ABSTRACT
Purpose
To assess the feasibility of hot-melt extrusion (HME) for preparing implants based on protein/poly(lactide-co-glycolide) (PLGA) formulations with special emphasis on protein stability, burst release and release completeness.
Method
Model protein (lysozyme)-loaded PLGA implants were prepared with a screw extruder and a self-built syringe-die device as a rapid screening tool for HME formulation optimization. Lysozyme stability was determined using DSC, FTIR, HPLC and biological activity. The simultaneous effect of lysozyme and PEG loadings was investigated to obtain optimized formulations with high drug loading but low initial release.
Results
Lysozyme was recovered from implants with full biological activity after HME. The release from all implants reached the 100% value in 60–80 days with nearly complete enzymatic activity of the last fraction of released lysozyme. Pure PLGA implants with up to 20% lysozyme loading could be formulated without initial burst. The incorporation of PEG 400 reduced the initial burst at drug loadings in excess of 20%.
Conclusion
A complete lysozyme recovery in active form with a burst-free and complete release from PLGA implants prepared by hot-melt extrusion was obtained. This is in contrast to many reported microparticulate lysozyme-PLGA systems and suggests the great potential of hot-melt extrusion for the preparation of protein-PLGA implants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Maintenance of protein stability during formulation process, storage and release is one of the main challenges for the effective delivery of protein drugs. Growing attention has been paid to the parenteral delivery of proteins in biodegradable injectable delivery systems in order to protect them from degradation and to allow for their controlled delivery (1).
Poly(lactide-co-glycolide) (PLGA) has been successfully used as biodegradable carrier material in controlled-release systems of low-molecular-weight drugs and peptides. The application of PLGA for the delivery of protein drugs, which have a much higher structural and functional complexity compared to small molecules and peptides, has been less successful. This is mostly due to incomplete recovery and release of native proteins.
In this study, hen egg white lysozyme, a glycosidase with a molecular weight of approximately 14.7 kDa and an isoelectric point around 11, was chosen as the model protein. Lysozyme is a popular model protein in pharmaceutical research, and its incorporation into PLGA-based delivery systems has been reported extensively (2–7). Although lysozyme has sometimes been referred to be a relatively stable protein, its low recovery in the presence of PLGA was remarkable (3,8). The low recovery of lysozyme as well as its incomplete release from PLGA-based delivery systems has been related to the protein instability during manufacturing of the delivery system and during release (2,4,9).
Biodegradable drug delivery systems based on PLGA can be in the form of microparticles or implants (10). Microparticles, which are often preferred to single unit implants because of easier administration, can be prepared by different microencapsulation techniques, including solvent evaporation/extraction, organic phase separation and spray drying (10). However, for protein drugs, the formation of large interfaces during microencapsulation (for example between the organic polymer phase and the aqueous protein phase) is a common destabilizing factor because of interfacial adsorption followed by denaturation and aggregation of proteins (11). Additionally, hydrophobic interaction of PLGA with proteins during emulsification or co-dissolution with PLGA may lead to protein unfolding and subsequent aggregation (12). Additionally, it can compromise the secondary structure of proteins, leading to partially unfolded and aggregate-prone conformations (13). Instability of lysozyme during microencapsulation has been addressed by several studies (5–7,14,15).
PLGA implants can be prepared with solvent-free processes, such as melt compression, injection/compression molding and melt extrusion. Accordingly, these promising methods for protein formulations can avoid potential stress during the incorporation of a protein drug with regard to the exposure of its dissolved form to surfaces and interfaces. Conformational stability of proteins is inversely related to their hydration level, being higher in the solid state (16,17). Similarly, chemical reactions proceed at a much lower rate in the solid than in the dissolved state (18).
Hot-melt extrusion is a single-step process which potentially offers many advantages for pharmaceutical applications over various microencapsulation processing techniques. It can result in large drug loadings, avoids water and organic solvents and does not require additional excipients such as surfactants. However, protein exposure to high temperature and shear force or high pressure can potentially cause unfolding, even in the dry state, leading to irreversible aggregation or covalent modifications of proteins (19). Accordingly, lysozyme was incorporated into PLGA implants by hot-melt extrusion to examine whether this solvent-free process can provide a better lysozyme stability during processing and also during release.
One of the biggest issues for protein delivery appears during rehydration of the protein upon contact of delivery systems with aqueous in vitro or vivo medium (13). The increased protein mobility upon hydration and the close vicinity of the molecules can initiate (non-)covalent aggregation. Special emphasis was therefore put on characterizing the quality of lysozyme during the initial drug release phase in order to differentiate rehydration-induced changes from other potential changes, which can, for example, arise upon polymer degradation through acidification of the implant interior. These instabilities can result in incomplete release of lysozyme (3,4,20,21).
Hydrophilic additives have been used to improve protein release from polymeric matrices. They can facilitate release of PLGA degradation products by increasing pore formation and hence prevent acidification of the matrix core. Low-molecular-weight polyethylene glycols (PEG) are hydrophilic additives with a plasticizing effect on PLGA. PEG generally increases the release during the initial burst and the diffusion-controlled release phases (22,23) and has no adverse effect on lysozyme structure and activity (24). Therefore, PEGs with average molecular weights of 400 and 1500 Da were incorporated into lysozyme-loaded implants, and their effects on lysozyme release were investigated.
MATERIALS AND METHODS
Materials
Poly(lactide-co-glycolide) (Resomer® RG 502, end-capped 50:50 PLGA, inherent viscosity 0.2 dlg−1, Boehringer-Ingelheim, Ingelheim, Germany); acetonitrile (HPLC gradient grade), lyophilized hen egg white lysozyme, sodium hydroxide (Carl Roth GmbH & Co. KG, Karlsruhe, Germany); polyethylene glycol 400 and 1500 (Lutrol® E, BASF AG, Ludwigshafen, Germany); acetic acid, ethyl acetate, sodium acetate, sodium azide, sodium dihydrogen phosphate, trifluoroacetic acid (Merck KGaA, Darmstadt, Germany); Micrococcus lysodeikticus (Sigma–Aldrich Chemie GmbH, Steinheim, Germany), medium chain triglyceride (MCT, Fagron Ltd., Barsbüttel, Germany).
Hot Melt Extrusion
Hot-Melt Extrusion with a Twin-Screw Extruder (HME)
The extrusion process was performed using a HAAKE MiniLab Rheomex CTW5 co-rotating twin-screw extruder at 20 rpm screw speed. Powder blends (>4 g) of PLGA and lysozyme were manually fed into the preheated barrel (90–105°C). A 1 mm cylindrical die was used, resulting in matrices of 1.1–1.2 mm in diameter. Implant fractions were collected from the beginning, middle and end of the process. All experiments were performed with at least 3 replicates using one piece implant (≈3 mm length and 3 mg weight) from each process fraction.
Hot-Melt Extrusion with a Syringe-Die Device (S-HME)
In order to have a higher throughput and less material use in HME formulation optimization, melt-extrusion with a syringe-die device was used as a screening tool.
Properly mixed formulation blends (∼200 mg) of PLGA and lysozyme (plus additive if mentioned) were charged into 1 ml polypropylene syringes (LUER LOK™, B–D®, Singapore). The syringes were fixed with a self-built die (Fig. 1), having similar dimensions as the HME-die, and heated at 105°C in an oven for 10 min. The molten blends were then extruded manually, producing cylindrical matrices with diameters of 1.1–1.2 mm. The matrices were cut into 3 mm length for recovery and dissolution experiments (n ≥ 3).
Protein Recovery from Implants
The implants (∼3 mm) were dissolved in 1.5 ml ethyl acetate (protein nonsolvent/polymer solvent) and then centrifuged for 20 min at 25°C and 28,110 g (Heraeus Biofuge stratos Haemo, Heraeus Instruments, Osterode, Germany) as described previously (25). About 1 ml of the supernatant was removed, and the washing cycle was repeated two more times. The protein precipitates were then dried under vacuum for 30 min (Heraeus oven VT 5042 EKP, Hanau, Germany, coupled with a chemistry hybrid pump, Vacuubrand GmbH, Wertheim, Germany) to remove residual ethyl acetate. The dried protein pellets were dissolved in 1 ml release medium (33 mM sodium acetate buffer pH 5 containing 0.01% sodium azide). The pH of the release medium of 5 was chosen according to the stability optimum of lysozyme (26). The concentration of soluble protein was quantified by BCA assay kit (Pierce, Rockford, USA). These protein solutions were also used to determine the concentration of active protein after extraction and also for HPLC.
To study lysozyme recovery upon rehydration, implants were incubated in the release medium for one day before extraction.
Biological Activity of Lysozyme
The biological activity of lysozyme was measured with a modified turbidimetric assay (27). The corrected linear rate of the absorbance decrease at 450 nm of a Micrococcus lysodeikticus cell suspension in 66 mM phosphate buffer (pH 6.24) at 25°C was used to estimate the concentration of active enzyme.
The initial absorbance of the filtered cell suspension was adjusted to values between 0.6 and 0.7. The aqueous lysozyme solution (100 μl) was added to 2.5 ml suspension of the bacteria. Turbidity was measured for 2 min using a diode array UV-spectrophotometer with a Peltier thermostatted cell holder (Agilent 8453, Agilent Technologies Inc., Palo Alto, USA) equipped with a UV-Chemstation biochemical analysis software. The slope of the linear portion was used for the quantification of active lysozyme concentration in the sample based on a freshly prepared standard curve (0–30 μg/ml).
HPLC
Extracted lysozyme from implants was characterized for possible oxidation of the protein by HPLC (SCL-10A VP, Shimadazu, Japan) using a C4 reversed phase column (Eurosphere-100, 7 μm, 125 mm × 4 mm, Knauer, Berlin, Germany). The solvent system consisted of water/acetonitrile/trifluoroacetic acid (A: 100/0/0.1, B: 0/100/0.1, V/V). A linear gradient method was applied (0-11-12 min 18.5-59-18.5%B) at a flow rate of 2 ml/min for 14 min and a column temperature of 25°C. Samples (25 μl) were injected, and chromatograms obtained with a diode-array UV-detector (SPD M-10A, Shimadazu, Japan) were quantified at 281 nm.
Differential Scanning Calorimetry (DSC)
DSC studies of protein powder or implants were performed with a DSC821e (Mettler Toledo) coupled with a Mettler TC15 TA-controller. Samples of ∼10 mg were accurately weighed in closed 40 µl aluminum crucibles. When measuring above 100°C, a pinhole was introduced into the lid for the escape of water vapor. DSC scans were recorded using a heating rate of 20 K/min under nitrogen atmosphere. Thermographs were normalized for sample weight. There was a negligible effect of DSC scan rate on lysozyme Tm from 10–20 K/min (Tm = 202°C–204°C).
Fourier Transform Infrared Spectroscopy (FTIR)
FTIR spectra were generated with an Excalibur 3100 FTIR spectrophotometer (Varian Inc., Palo Alto, USA). The spectra from protein powder or ground implants (with mortar and pestle) were collected using a horizontal ATR accessory with a single reflection diamond crystal (Pike Miracle, Pike Technologies, Madison, USA). Sixty-four scans at 4 cm−1 resolution were averaged, and spectral contributions coming from water vapor in the light pass were subtracted using Varian software (Resolution Pro 4.0). Second derivative data were processed with the same software. Finally, all spectra were treated with a 13-point smoothing function.
EDX-SEM
Lysozyme distribution was examined by elemental mapping of the cross sections of implants for the characteristic X-ray peak of sulfur. The elemental distributions were investigated by scanning electron microscopy (Hitachi S-2700, Tokyo, Japan) combined with energy-dispersive X-ray (EDX) spectroscopy using a Röntec XFlash-SDD-detector. The implants were coated with carbon to make them conductive.
In order to depict the radial distribution of proteins in the implants, pixel intensities in EDX pictures were analyzed using a MATLAB® function (see Supplementary Material 1). First, the RGB pictures were converted to the grayscale format. Then, for each of the L concentric layers of the implant, the average pixel intensity and the 95% confidence interval of each distribution were computed.
Density Measurement
In order to compare the porosity of implants, their apparent densities were estimated. Glass pipettes (1 ml) filled with medium chain triglyceride (MCT) (a nonsolvent for the implant ingredients) were used for volume measurement. Several pieces of implants from different fractions of the extrusion process were weighed and put together into the oil-filled pipette to achieve significant changes in the oil volume. Densities were calculated by dividing the total weight by the volume change.
Lysozyme Release
Implants (3 mm long) were placed in screw-cap-sealed test tubes filled with 4 ml of 33 mM pH 5 sodium acetate buffer containing 0.01% sodium azide as preservative to determine the lysozyme release (one implant per vial, n = 3). The vials were incubated in vertical position in a horizontal shaker (80 rpm, 37°C; Gemeinschaft für Labortechnik, Burgwedel, Germany). The release medium was replaced with fresh medium at each sampling time point. Lysozyme concentrations in release samples were quantified by Micro BCA assay (Pierce, Rockford, USA) using a freshly prepared standard curve (0–20 μg/ml).
Uptake of Release Medium and Mass Loss of Implants During Release Studies
S-HME implants were weighed in the initial dry form (t0). Medium uptake of implants was determined by their weight gain during release (Eq. 1). At predetermined time points (ti), the implants were removed from the release medium, blotted with tissue paper to remove surface medium and then weighed. The weight gain values were corrected for the amount of released lysozyme. The studies were stopped when the implants turned into very soft matrices.
After 1 day release (t1), the water content of S-HME implants (lysozyme:PEG:PLGA, 10:9:81) was measured using thermogravimetric analysis (TGA) with a Mettler TC15 TA-controller (Mettler Toledo). Total mass loss and the amount of released PEG were calculated according to Eqs. 2 and 3, respectively.
RESULTS AND DISCUSSION
Lysozyme Stability During Hot-Melt Extrusion Process
Protein instability during manufacturing of different PLGA delivery systems has been addressed by several studies (14,15,28). In hot-melt extrusion, there are some stress factors (e.g., elevated temperature in combination with shear forces), which can potentially affect protein integrity via physical and/or chemical modifications and consequently can lead to their inactivation. Systematic studies about the stress factors exerted on protein drugs during hot-melt extrusion are still missing. Therefore, the physical and chemical stability of lysozyme after hot-melt extrusion with extruder (HME) at 105°C were evaluated.
Differential scanning calorimetry showed a denaturation temperature (Tm) of 204°C for both native lysozyme and lysozyme-loaded hot melt extruded PLGA implants (Fig. 2). This is in agreement with previous results on native lysozyme in solid state (29). The presence of the melting peak in the DSC scan can indicate conservation of protein conformation after extrusion at 105°C (30).
Conformational stability of lysozyme in HME implants was confirmed by ATR-FTIR. The spectra of implants containing 25% lysozyme were comparable to the lyophilized lysozyme powder used to prepare the implants (Fig. 3a). Thus, there was no indication for denaturation (shifts or distortion of bands) or aggregation (intermolecular β-sheet formation) as a consequence of the exposure to elevated temperature and pressure during the extrusion at 105°C based on these data. The second derivative spectra of the Amide I band (Fig. 3b) suggested a negligible red-shift of the bands above 1,660 cm−1, assigned to turns and β-sheet (21), which can be caused by subtraction of PLGA background or small loosening of the turn structures.
Lysozyme was completely recovered (99 ± 1.1% based on initial loading) from the implants showing 98 ± 5.9% biological activity. HPLC analysis of extracted protein showed that no oxidation of lysozyme occurred during the HME process. Chromatograms showed the same peak ratio of native (retention time 7.0 min) to oxidized lysozyme (retention time 6.7 min) as freshly prepared solution of unprocessed lysozyme powder (data not shown).
In conclusion, lysozyme can be incorporated into PLGA implants in its active form.
Lysozyme Release
Lysozyme Recovery upon Contact with Release Medium
Moisture-induced degradation/aggregation is one major reason for the incomplete release of proteins (31). Therefore, the effect of the initial hydration on protein recovery from the implant was examined after one day release.
Lysozyme was fully recoverable from the HME implants produced at 100 and 105°C after one day release. For implants prepared at 105°C, approximately 42% of the totally recovered amount was released within one day (burst release) (Table I). The unreleased fraction (approx. 58%) of total protein remained in the fully active form in the implant. However, the released fraction showed some activity loss which summed up to an overall activity of 84%. Considering the native character of lysozyme found in the dry implants, the perturbation appears to occur during the rehydration step upon contact with aqueous release medium.
Interestingly, no enzyme activity was lost when the hot-melt extrusion was conducted at 100°C. This observation coincided with a lower burst release from 100°C HME-implants (27% vs. 42%) compared to the 105°C ones. Reduction of process temperature from 105°C to 100°C increased the density of the matrices from 1.04 gcm−3 to 1.45 gcm−3, respectively. A lower process temperature can increase the density of the product because of a higher melt viscosity (32). In fact, the higher melt viscosity results in a higher pressure (33) and thus a lower free volume (34).
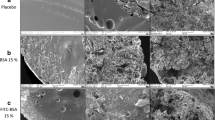
Elemental mapping of implant cross-sections showed an overall homogeneous distribution of lysozyme particles in implants produced at 105°C and at 100°C (Fig. 4a and 4b). Nevertheless, the radial distribution plots showed that in the outer layers of implants produced at 100°C, the protein concentration was lower than the average total concentration (Fig. 4d). The lower surface concentration of proteins compared to implants prepared at 105°C (Fig. 4c) correlated with the lower burst release of implants prepared at 100°C.
Lysozyme distribution illustrated with EDX-SEM elemental mapping of sulfur (yellow/white spots) on cross-section of 25% lysozyme containing PLGA implants prepared by hot-melt extrusion at a 105°C and b 100°C. The corresponding radial distribution plots, c 105°C and d 100°C, depict average of pixels intensity in each layer form inside (layer 1) to outside (layer 24). The gray arrows show the averaged total intensity.
The coincidence of surface accumulation and loss of activity might suggest a relationship of protein distribution and its susceptibility to undergo rehydration-induced alterations (e.g., aggregation and/or structural changes via a higher local protein concentration). However, a more detailed study is required to address this question.
In addition to hydration, another stress factor which might cause incomplete protein release from PLGA controlled-release systems is the pH-drop inside the matrix due to trapped acidic polymer degradation products (12). Exposure of the protein to the acidic environment during prolonged release can promote perturbation of protein structure and aggregation [28]. Hence, lysozyme release from melt-extruded implants was followed, and the achievable release patterns as well as the fate of the protein in the formulations were investigated.
Hot-Melt vs. Syringe-Hot-Melt Extruded Implants
Melt-extrusion with a syringe-die device was used as a small-scale screening tool.
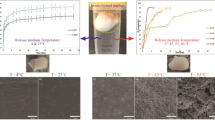
The release of lysozyme from both types of melt-extruded PLGA implants showed a typical multiphasic pattern. The release profiles consisted of an initial burst followed by a period of negligible lysozyme release and an erosion-controlled release thereafter (Fig. 5). The initial release at 10% lysozyme loading was similar for HME and S-HME implants. Increasing the lysozyme loading from 10% to 25% increased the initial release. The slightly higher burst with the 25% lysozyme-containing S-HME implant can be attributed to its lower density (higher porosity) compared to the HME matrix (1.15 gcm−3 vs. 1.45 gcm−3). The lower variability in lysozyme release from HME compared to S-HME implants reflects a better homogeneity resulting from a better mixing of the formulations in the screw-type extruder than with the syringe-die device.
In all cases, the main protein fraction was released during the polymer erosion phase. The release rates of the S-HME and the HME implants were comparable, resulting in a completion of the release from 25% lysozyme-loaded implants between 40 and 50 days (t90%). The residual amount was released between 50–60 days with full biological activity (96.7 ± 1.2%). However, deamidation, which can occur as a consequence of a pH decrease within the implant, cannot be excluded based on these data. At low pHs, deamidation has been shown to result in formation of protein derivatives with hyperactivity (35).
Implants containing 10% lysozyme completed the release at about 80 days for both S-HME and HME. Thus, melt-extrusion with the syringe-die device was used as screening tool for HME formulations in the following studies.
Effect of Drug Loading
The initial release phases were comparably small (<10%) for the 10% and 17.5% lysozyme-containing implants (Fig. 6). Increasing the drug loading to 25%, however, increased the fraction released within the first week to about 40%. This suggests that the drug percolation threshold is around 20%, above which some drug particles are in contact to form an interconnected network with access to the implant surface, resulting in drug release by diffusion through water-filled pores.
The erosion-controlled release phase for lysozyme particles not on the surface and not in contact with each other started at about day 20 for all three drug loadings. The release rates increased with increasing drug loading. As a result, release periods for 90% drug released of about 36, 63 and 73 days were obtained for the 25%, 17.5% and 10% drug loadings, respectively. The dependence of the release rate on drug loading might be related to a fraction of remaining lysozyme particles in the matrix which can form an interconnected network. In addition, a higher lysozyme loading means a lesser PLGA content to be eroded. Also, a higher initial burst results in a more porous matrix which can accelerate both drug release and matrix erosion.
Effect of PEG Incorporation
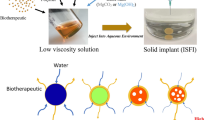
PEGs with average molecular weights of 400 or 1500 Da and lysozyme were co-incorporated into S-HME implants in order to overcome the multiphasic release behavior of the protein implants through an increase of the diffusional drug release.
Incorporation of 10% PEG (based on polymer) into 10% lysozyme-containing implants increased the rate and extent of lysozyme release during the first 14 days (Fig. 7). The release approximated linear characteristics against time to the power of 0.45, which reflects a diffusion-controlled release for cylindrical shape matrices (36) without an uncontrolled burst. The accelerating effect of PEG on the initial release of lysozyme correlated with an increased weight gain of the implants during incubation due to the uptake of release medium (Fig. 8). Corresponding to the osmotic activity of drug and additive, the water uptake upon incorporation of PEG 400 was the highest, followed by PEG 1500 and the formulation without PEG. However, the release-accelerating effect of PEG 400 was less pronounced compared to PEG 1500. This might be correlated to higher pore formation ability of PEG 1500.
Similar differences in protein release between PEG 400 and PEG 1500 were reported (7,37). To better understand this difference and to obtain an optimized formulation with a high drug loading but low burst, the simultaneous effect of lysozyme and PEG loading on first day release was investigated. Implant formulations with loadings of 10%, 17.5% and 25% lysozyme (based on total) and 0%, 5% or 10% PEG 400 or 1500 (based on polymer) were prepared. The initial lysozyme release of the PEG-free formulations increased with increasing drug loading (Figs. 9a and 10a). The increase was pronounced when the drug loading was increased above 17.5%, which can be attributed to the drug percolation threshold.
Incorporation of PEG 400 reduced the effect of the protein loading on the initial release (Fig. 9a). On the other hand, depiction of first day release vs. PEG 400 content showed that the effect of PEG on the release depended also on drug loading (Fig. 10a). Below 22.5% drug loading, a slight increase in the release as a function of PEG concentration was noticed. This might be explained by a pore-formation through PEG. The amount of released protein from these formulations within the first day, however, was still low.
A more complex effect was seen above the percolation threshold of lysozyme. PEG appeared to decrease the initial burst release. The decrease might be explained by a PEG-induced viscosity increase which reduces diffusion through water-filled pores. When high levels of lysozyme (27.5%) and PEG (10%) were combined, however, the viscosity effect was diminished, probably by an increased pore formation through further PEG addition. The result was a local minimum seen for the 27.5% lysozyme loading (Fig. 10a).
The higher molecular weight PEG, however, increased the initial release at low lysozyme loadings (Fig. 9b). Mass loss study showed nearly similar leaching of PEG 400 and 1500 from the matrix (6.3 ± 0.5 and 6.8 ± 1.2%, respectively) within the first day. A stronger pore-formation effect through the formation of larger pores might have led to an acceleration of the initial lysozyme release with PEG 1500. Indeed, PEG 400 is a solvent for PLGA and mixes well with PLGA, while PEG 1500 is mixed in particulate form. Although being molten during melt extrusion, islands of PEG 1500 could potentially form in the PLGA matrix after extrusion, since it does not dissolve PLGA.
As discussed here, the effect of PEG varied not only with size and concentration of PEG, but also with protein concentration. Lysozyme could be formulated with HME up to 20% loading without initial burst. Incorporation of 10% PEG 400 reduced the initial burst at 25% drug loading.
CONCLUSION
In this study, the feasibility of hot-melt extrusion for processing of proteins was examined with regard to the main challenges in the field, i.e. protein instability during manufacture and release, as well as the release incompleteness.
Nearly complete recovery of active lysozyme as a model protein illustrated that the melt extrusion process did not damage the protein integrity.
Melt-extrusion with syringe could be applied as a screening tool for optimizing hot-melt extrusion formulations. Lysozyme was completely released from all formulations whereby the initial release as well as release rate were controlled by lysozyme loading and additives. Drug release was also dependent on matrix properties, including matrix density and drug distribution. Nearly complete enzymatic activity was obtained with the last fraction of released lysozyme from HME implants.
In summary, hot-melt extrusion is a promising method for the effective delivery of protein therapeutics because of its relatively simple, single step formulation process and good protein stability.
REFERENCES
Giteau A, Venier-Julienne MC, Aubert-Pouëssel A, Benoit JP. How to achieve sustained and complete protein release from PLGA-based microparticles? Int J Pharm. 2008;350:14–26.
Aubert-Pouëssel A, Bibby DC, Venier-Julienne MC, Hindre F, Benoît JP. A novel in vitro delivery system for assessing the biological integrity of protein upon release from PLGA microspheres. Pharm Res. 2002;19:1046–51.
Ghassemi AH, van Steenbergen MJ, Talsma H, van Nostrum CF, Jiskoot W, Crommelin DJA, et al. Preparation and characterization of protein loaded microspheres based on a hydroxylated aliphatic polyester, poly(lactic-co-hydroxymethyl glycolic acid). J Control Release. 2009;138:57–63.
Giteau A, Venier-Julienne MC, Marchal S, Courthaudon JL, Sergent M, Montero-Menei C, et al. Reversible protein precipitation to ensure stability during encapsulation within PLGA microspheres. Eur J Pharm Biopharm. 2008;70:127–36.
Kokai LE, Tan H, Jhunjhunwala S, Little SR, Frank JW, Marra KG. Protein bioactivity and polymer orientation is affected by stabilizer incorporation for double-walled microspheres. J Control Release. In Press, Uncorrected Proof.
Lee ES, Park KH, Park IS, Na K. Glycol chitosan as a stabilizer for protein encapsulated into poly(lactide-co-glycolide) microparticle. Int J Pharm. 2007;338:310–6.
Taluja A, Bae YH. Role of a novel multifunctional excipient poly(ethylene glycol)-block-oligo(vinyl sulfadimethoxine) in controlled release of lysozyme from PLGA microspheres. Int J Pharm. 2008;358:50–9.
Van De Weert M, Hoechstetter J, Hennink WE, Crommelin DJA. The effect of a water/organic solvent interface on the structural stability of lysozyme. J Control Release. 2000;68:351–9.
Diwan M, Park TG. Pegylation enhances protein stability during encapsulation in PLGA microspheres. J Control Release. 2001;73:233–44.
Jain RA. The manufacturing techniques of various drug loaded biodegradable poly(lactide-co-glycolide) (PLGA) devices. Biomaterials. 2000;21:2475–90.
Pérez C, Griebenow K. Improved activity and stability of lysozyme at the water/CH2Cl2 interface: enzyme unfolding and aggregation and its prevention by polyols. J Pharm Pharmacol. 2001;53:1217–26.
Van De Weert M, Hennink WE, Jiskoot W. Protein instability in poly(lactic-co-glycolic acid) microparticles. Pharm Res. 2000;17:1159–67.
Prestrelski SJ, Tedeschi N, Arakawa T, Carpenter JF. Dehydration-induced conformational transitions in proteins and their inhibition by stabilizers. Biophys J. 1993;65:661–71.
Ghaderi R, Carlfors J. Biological activity of lysozyme after entrapment in poly (d, l-lactide-co-glycolide)-microspheres. Pharm Res. 1997;14:1556–62.
Pérez C, Castellanos IJ, Costantino HR, Al-Azzam W, Griebenow K. Recent trends in stabilizing protein structure upon encapsulation and release from bioerodible polymers. J Pharm Pharmacol. 2002;54:301–13.
Hageman MJ. The role of moisture in protein stability. Drug Dev Ind Pharm. 1988;14:2047–70.
Bell LN, Hageman MJ, Muraoka LM. Thermally induced denaturation of lyophilized bovine somatotropin and lysozyme as impacted by moisture and excipients. J Pharm Sci. 1995;84:707–12.
Chien-Hua N, Yuan-Yuan C. FDA perspective on peptide formulation and stability issues. J Pharm Sci. 1998;87:1331–4.
Rothen-Weinhold A, Oudry N, Schwach-Abdellaoui K, Frutiger-Hughes S, Hughes GJ, Jeannerat D, et al. Formation of peptide impurities in polyester matrices during implant manufacturing. Eur J Pharm Biopharm. 2000;49:253–7.
Park TG, Lee HY, Nam YS. A new preparation method for protein loaded poly(D, L-lactic-co-glycolic acid) microspheres and protein release mechanism study. J Control Release. 1998;55:181–91.
Van De Weert M, Van’T Hof R, Van Der Weerd J, Heeren RMA, Posthuma G, Hennink WE, et al. Lysozyme distribution and conformation in a biodegradable polymer matrix as determined by FTIR techniques. J Control Release. 2000;68:31–40.
Kang F, Singh J. Effect of additives on the release of a model protein from PLGA microspheres. AAPS PharmSciTech. 2001;2.
Jiang W, Schwendeman SP. Stabilization and controlled release of bovine serum albumin encapsulated in poly(D, L-lactide) and poly(ethylene glycol) microsphere blends. Pharm Res. 2001;18:878–85.
Malzert A, Boury F, Renard D, Robert P, Lavenant L, Benoît JP, et al. Spectroscopic studies on poly(ethylene glycol)-lysozyme interactions. Int J Pharm. 2003;260:175–86.
Körber M, Bodmeier R. Development of an in situ forming PLGA drug delivery system. I. Characterization of a non-aqueous protein precipitation. Eur J Pharm Sci. 2008;35:283–92.
Claudy P, Letoffe JM, Bayol A, Bonnet MC, Maurizot JC. Denaturation versus pH of lysozyme and biosynthetic human growth hormone by differential scanning calorimetry and circular dichroism: a comparative study. Thermochim Acta. 1992;207:227–37.
Shugar D. The measurement of lysozyme activity and the ultra-violet inactivation of lysozyme. BBA–Biochim Biophys Acta. 1952;8:302–9.
Wang J, Chua KM, Wang CH. Stabilization and encapsulation of human immunoglobulin G into biodegradable microspheres. J Colloid Interface Sci. 2004;271:92–101.
Elkordy AA, Forbes RT, Barry BW. Integrity of crystalline lysozyme exceeds that of a spray-dried form. Int J Pharm. 2002;247:79–90.
Hill JJ, Shalaev EY, Zografi G. Thermodynamic and dynamic factors involved in the stability of native protein structure in amorphous solids in relation to levels of hydration. J Pharm Sci. 2005;94:1636–67.
Schwendeman SP, Costantino HR, Gupta RK, Langer R. Peptide, protein and vaccine delivery from implantable polymeric systems: Progress and challenges. Controlled Drug Delivery: Challenges and Strategies; 1997. p. 229–267.
Ding QB, Ainsworth P, Plunkett A, Tucker G, Marson H. The effect of extrusion conditions on the functional and physical properties of wheat-based expanded snacks. J Food Eng. 2006;73:142–8.
Akdogan H. Pressure, torque, and energy responses of a twin screw extruder at high moisture contents. Food Res Int. 1996;29:423–9.
Warfield RW. Compressibility of bulk polymers. Polym Eng Sci. 1966;6:176–80.
Tomizawa H, Yamada H, Ueda T, Imoto T. Isolation and characterization of 101-succinimide lysozyme that possesses the cyclic imide at Asp101-Gly102. Biochemistry. 1994;33:8770–4.
Ritger P, Peppas N. A simple equation for description of solute release I. Fickian and non-fickian release from non-swellable devices in the form of slabs, spheres, cylinders or discs. J Control Release. 1987;5:23–36.
Bezemer JM, Radersma R, Grijpma DW, Dijkstra PJ, Van Blitterswijk CA, Feijen J. Microspheres for protein delivery prepared from amphiphilic multiblock copolymers 2. Modulation of release rate. J Control Release. 2000;67:249–60.
ACKNOWLEDGMENT
The financial support of the German Academic Exchange Service (DAAD) for Zahra Ghalanbor Ph.D. studies and the support of Laszlo David (Department of Mathematics and Informatics, Freie Universität Berlin) with the MATLAB® code are acknowledged.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 303 kb)
Rights and permissions
About this article
Cite this article
Ghalanbor, Z., Körber, M. & Bodmeier, R. Improved Lysozyme Stability and Release Properties of Poly(lactide-co-glycolide) Implants Prepared by Hot-Melt Extrusion. Pharm Res 27, 371–379 (2010). https://doi.org/10.1007/s11095-009-0033-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-009-0033-x