Abstract
Purpose
The study was designed to evaluate the effect of delayed release (DR) on absorption and bioavailability of intestinally metabolized drugs after oral dosing, using the HMG-CoA reductase inhibitor simvastatin, a CYP3A substrate, as a model drug.
Materials and Methods
To target drug release and to assess regional gastrointestinal absorption of the CYP 3A substrate simvastatin from the distal parts of the intestine, delayed release film coated tableted oral dosage forms were developed. Simvastatin delayed release tablet, simvastatin immediate release capsule and simvastatin immediate release tablet Zocor® were administered as single doses (20 mg) to fasting healthy volunteers in a crossover design.
Results
Simvastatin bioavailability was increased by a factor of three, as compared to the reference formulation Zocor®. The overall metabolite levels from the immediate release capsules tended to be higher throughout the period studied than the metabolite levels following administration of Zocor® and simvastatin delayed release dosage form.
Conclusions
The interplay between gastrointestinal physiology (lower CYP 3A expression in the distal ileum and the colon) and formulation design (zero-order controlled release after a predetermined lag-time) resulted in successful absorption and bioavailability improvement and represent a viable strategy to reduce the dose of CYP 3A drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Enterocyte-based metabolism via cytochrome P450 complicate the predictability of drug absorption and bioavailability especially when administered in modified release dosage forms. Regional variations on CYP 3A expression contribute to changes in drug exposure—greater distal intestinal exposure with modified release compared with immediate release—as a function of variations in metabolism.
The enterocytes contain virtually all types of drug-metabolising enzymes that are found in the liver. The importance of hepatic metabolism for limiting systemic drug availability is well established; however intestinal drug metabolism can further diminish systemic availability. Using functional enzyme activity studies and immunoblot analysis, it was shown that the CYP 3A expression in mature enterocytes, located mainly in the villi tips, of jejunal mucosa is comparable or may even exceed the expression of CYP 3A in hepatocytes (1). Total CYP P450 content increased slightly in proceeding from the duodenum to the jejunum, and then decreased sharply towards to the ileum (2). Using in situ hybridisation with a probe specific for CYP 3A4, McKinnon confirmed CYP 3A expression throughout the entire small intestine, with highest levels in its proximal regions (3). The most abundant CYP isoenzymes in the intestine are 3A4 and 3A5. Many authors found higher CYP 3A4 mRNA and protein expression in the duodenum than in the stomach and the colon (4,5).
To overcome the limitations of presystemic metabolism, we propose a targeting approach for site-specific drug release in those segments in the gut where expression of the CYP 3A enzymes is minimal (6). We postulate that distal intestinal delivery can lead to elevated plasma levels and improved oral bioavailability for drugs that are substrates for the cytochrome P450 3A enzyme class, since their activity is lower in the mucosa of the distal small intestine and colon than of the proximal small intestine. Moreover, drug delivery to these regions of the intestine can be beneficial when an intentional time delay in absorption is required.
Drug absorption from the distal intestine is affected by the limited effective surface area available for absorption and the tight epithelium. Furthermore, the drug may become adsorbed to dietary residues, intestinal secretions, mucus or general faecal matter, thereby reducing the concentration of free drug. There is also less free fluid in the colon than in the small intestine; hence dissolution could be problematic for poorly water soluble drugs like nifedipine, simvastatin, spironolactone, and griseofulvin. In such instances, the drug may need to be delivered in a presolubilised form. The challenge for poorly soluble drugs is to control the rate of dissolution to minimize variations and maintain a well-dispersed system that allows the drug to become absorbed. The longer residence time in the colon may overcome some of the potential biopharmaceutically relevant constraints of this region of the gut (6–8).
Four strategies are currently being pursued to achieve drug release specifically in the lower segments of the gastrointestinal tract: time-controlled, pH-controlled, enzyme-controlled and pressure-controlled drug delivery. Time-based delivery systems that take advantage of the relatively constant transit time through the small intestine (approximately 3–4 h) seem to be most promising thus far (8).
Design of modified release systems for poorly soluble drugs that are additionally CYP 3A substrates such as simvastatin is challenging not only because of their low solubility and dissolution rate, but due to their high metabolic inactivation as well. The aqueous solubility of simvastatin at room temperature is 1.4 mg/l, resulting in the requirement of approximately 14 l of water for dissolution of a 20 mg dose. Efforts to enhance the aqueous dissolution rate of simvastatin include embedding of the API within a mixture of gelatin and lecithin. As previously demonstrated for the model substances cyclosporin and griseofulvin the lecithin/gelatin containing formulation greatly increased initial dissolution rate and total percentage dissolved (9).
The systemic availability of simvastatin is less than 5% caused by cytochrome P450 mediated enzymatic conversion in the gut and in the liver. The extensive oxidative metabolism of simvastatin in human liver is primarily mediated by CYP 3A (CYP 3A4 and CYP 3A5), with the remaining metabolism being attributed to CYP 2C8 (10,11), and CYP 2C9 (12). In addition to the CYP P450-mediated oxidation and ß-oxidation processes, glucuronidation constitutes a common metabolic pathway for statins (13). Simvastatin, administered as lactone, is metabolically activated to the open chain nonlactone simvastatin acid. This reversible conversion to the active form occurs by nonspecific carboxyesterases in the intestinal wall, liver and to some extent in plasma or by nonenzymatic hydrolysis.
The present study was a “proof of concept” human clinical trial to demonstrate the advantages of delayed release technology based on Hydrophilic Solubilisation Technology (HST) (14) and its effect on absorption and bioavailability of poorly soluble, intestinally metabolized drugs.
MATERIALS AND METHODS
Materials
All chemicals used for the preparation of the clinical batches of simvastatin dosage forms were of pharmaceutical grade. Simvastatin was supplied from Hovione FarmaCiencia SA (Loures, Portugal). Lecithin, gelatin, mannitol, magnesium stearate and sodium lauryl sulfate were from Caelo (Hilden, Germany). Precirol® was received from Gattefossé (Saint-Priest, France). Eudragit® RS 100 was from Röhm (Darmstadt, Germany) and Explotab® from JRS Pharma (Rosenberg, Germany). USP simvastatin reference standard was received from PHAST GmbH (Homburg/Saar, Germany). Solvents for HPLC and LC/MS/MS analysis were purchased from Merck (Darmstadt, Germany), Across Organics (Geel, Belgien), Spectrum Chemicals (Gradena, USA) and Fisher Scientific (Pittsburgh, USA). Lovastatin reference standard was supplied from US Pharmacopeia (Rockville MD, USA). Heparinized human control plasma was kindly provided by Biological Specialty Corporation (Landsdale PA, USA). Simvastatin immediate release tablets Zocor® 20 were a gift from MSD SHARP & DOHME (Haar, Germany).
The HPLC instrument consisted of an autosampler type AS 950 (Jasco Deutschland GmbH, Groß-Umstadt, Germany), a pump type PU 980 (Jasco, Deutschland GmbH, Groß-Umstadt, Germany), a UV–VIS detector model UV 975 (Jasco, Deutschland GmbH, Groß-Umstadt, Germany), and a column oven type Jetstream Plus. Chromatograms were evaluated using Borwin™ software, version 3 (JMBS Development, Le Fontanil, France). The LC/MS/MS system used for the analysis of simvastatin and simvastatin acid in plasma consisted of an HP 1100 HPLC system (Hewlett Packard, USA) and a Quattro II mass spectrometer (Micromass Beverly MA, USA) interfaced with the liquid chromatograph via an electrospray source. The turbo ion-spray temperature was optimized and maintained at 150°C. Data acquisition, peak integration and calculation were performed using MassLynx software (Micromass, version 1.4).
Formulation and Characterization of Simvastatin Solid Dosage Forms
Simvastatin delayed release tablets and simvastatin immediate release capsules were manufactured in compliance with Good Manufacturing Practice standards.
Coated delayed release tablets, containing 20 mg of simvastatin were designed to increase the solubility of the active pharmaceutical ingredient (API) and also to control the release rate of such dosage form for extended delivery to the lower small intestine and the proximal colon. The components and procedures for manufacturing of the simvastatin delayed release formulation, tested in humans, were described by Hilfinger et al. (14). Briefly, the manufacturing process consisted of preparation of a freeze-dried powder composed of simvastatin, gelatine, lecithin and mannitol (SGLM), tablet compression, and a tablet dip coating procedure.
Preparation of Simvastatin Immediate Release Capsules
The appropriate mass of sieved (through sieves number 4, 10, 20, 25 and 30 (USP)) freeze-dried powder (SGLM formulation) was filled into hard gelatine capsules of the size 00 using an Aponorm® capsule filling and closure device equipped with a suitable inlay for 00 capsule sizes.
Preparation of Simvastatin Delayed Release Tablets
Tablets consisted of freeze dried powder, Precirol®, magnesium stearate and Explotab® and were prepared by compressing the mixture for 15 s using a manual tablet press with a compression force of 30 kN. The punches (upper and lower punch diameter: 5.39 mm and die inner diameter: 5.40 mm) were lubricated with magnesium stearate before the compression process. The tablets were coated with Eudragit® RS until the desired coating level of 6 to 10 total weight percent was reached.
Dissolution of Simvastatin from Solid Dosage Forms
In vitro dissolution for all the formulations was performed employing USP apparatus II. The dissolution studies were carried out in 900 ml of 0.01M phosphate buffer solution at pH 7.0 containing 0.5% sodium lauryl sulphate at 37 ± 0.5°C at 50 rpm. Dissolution samples were collected at 0, 2, 4, 8, 12, 16, 20 and 24 h for simvastatin delayed release tablets and at 0, 5, 10, 20, 30 and 60 min for both immediate release dosage forms. After centrifugation, the dissolution samples were diluted with mobile phase (pH 2.8) 1:1 and quantified by HPLC.
HPLC Determination of Simvastatin in Dosage Forms and Dissolution Samples
The HPLC assay for determination of simvastatin in dosage forms and dissolution samples was based on the monographs of simvastatin in USP/NF and the method according to the reference (15). About 10 µl sample solution was injected into the HPLC and analyzed using a Phenomenex® Synergi 4 μm Hydro-RP 80 Å (150 × 4.6 mm) column (Phenomenex USA Torrance, CA) under isocratic conditions at 35°C and a flow rate of 1 ml/min. The mobile phase consisted of 14.8 mM phosphoric acid solution (pH 2.8): acetonitrile (75:25, v/v). Simvastatin concentration in the eluate was analysed by UV-absorption at 238 nm. The calibration curve for simvastatin was prepared in a concentration range from 0.1 μg/ml to 15 μg/ml. The correlation coefficient was always better than 0.9989. Intra-day and inter-day accuracy of the assay were in the range between −5.4% and 2.4% of the nominal values, precision was between 0.2% and 2.7%. The limit of quantification of 50 ng/ml was adequate for the dosage form development.
Clinical Study
Subjects Profiles
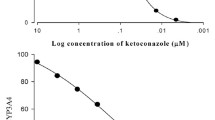
Seven volunteers (one female and six male subjects) were enrolled in the clinical study. The mean age was 30 years (range: 26–42), and the mean body weight was 77.3 kg (range: 70.5–84 kg). None of the subjects were smokers or used continuous medication (including CYP 3A enzymes inducers or inhibitors), except for one female subject who used oral contraceptives. Before entering the study, volunteers were ascertained to be healthy by scrutinizing their respective medical histories, physical examination, routine laboratory tests, and a standard electrocardiogram. None of the volunteers should exhibit any of the following exclusion criteria: disease of liver and/or kidney and/or gastrointestinal tract, prior gastrointestinal surgery, Crohn’s disease, ulcerative colitis, evidence of pelvic infection or cervical disease; concomitant chronic illness (diabetes mellitus, heart disease, renal insufficiency, hypertension, cancer, autoimmune diseases); unexplained persistent elevations of serum transaminase; creatine kinase different from the normal limit; current or previous treatment with systemic immunosuppressive medications (including cyclophosphamide, methotrexate, azathioprine); current treatment with potent inhibitors of CYP 3A4 (itraconazole, ketoconazole, nefazodone, erythromycin, clarithromycin). All study protocols were approved by the independent Ethics Committee Rheinland-Pfalz and reviewed by the German National Agency of Medicines. Before entering the study all subjects received both oral and written information and gave their written consent.
Study Design
The randomized, open, three phases, and single-dose study was carried out according to a crossover design with at least 1 week washout period between the phases. The following products were studied: simvastatin delayed release tablet (20 mg), simvastatin immediate release capsule (20 mg), and simvastatin immediate release tablet Zocor® (20 mg) as reference product. Each dose was administered, under the supervision of the investigator, with 200 ml of mineral water. Subjects were monitored to ensure that the tablets and capsule were swallowed intact and were not chewed. Volunteers were required to fast at least 10 h prior to drug administration, as well as not to undergo excessive physical exercise on the day before the trial. Consummation of cola, coffee, tea, orange and grapefruit juice was prohibited and use of alcohol was not allowed commencing 1 day prior to the study day, during the study day and up to 24 h thereafter.
After the volunteers had entered the clinical study unit, a forearm vein was cannulated and a blood sample was drawn 30 min before administration of the study drug. Thereafter, each subject was dosed with the study drug in the fasted state, according to the individual randomization scheme for each subject. All subjects, regardless of treatment assignment, were monitored in the clinic for 24 h following dosing (general condition, heart rate, blood pressure, ECG, occurrence of adverse reactions). Standard meals (CYP enzyme inducer-free, caffeine-free food and beverage) were given at 4 and 10 h after the drug administration in each study period. Venous blood samples (7 ml each) were drawn following administration of the simvastatin delayed release tablet at 0, 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 5, 6, 8, 10, 12, 16, 20, 24, and 30 h. Following treatment with immediate release dosage forms the sampling times were at 0, 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 5, 6, 8, 10, 12, 16, 20, and 24 h.
Determination of Simvastatin and Simvastatin Acid Concentrations in Plasma
An assay from Zhao et al. was adapted based on a LC/MS/MS method (16). The analyses were performed on a Kromasil C18 column 5 μm, 50 × 2.2 mm (Higgins Analytical Inc. Mountain View CA, USA) protected by a Kromasil C18, 5 μm, 20 × 2.2 mm (Higgins Analytical Inc Mountain View CA, USA) with liquid flow of 200 μl/min under ambient conditions. 1 mM ammonium acetate with pH adjusted to 4.5: acetonitrile (75:25, v/v) was used as mobile phase. Calibration standard solutions containing simvastatin and simvastatin acid at concentrations of 0.1, 0.5, 1.0, 5.0, 10.0 ng/ml were prepared by spiking working standard solutions into the tubes containing human control plasma. An internal standard solution containing lovastatin at 50 ng/ml was prepared by diluting and mixing stock solution of lovastatin with acetonitrile-water. Plasma quality control samples (8, 5, 0.5 ng/ml) were prepared by adding 400 μl of the appropriate quality control working solutions into 45 ml polypropylene screw-cap tubes containing 39.6 ml of human plasma.
Cryogenic tubes containing plasma samples, quality controls and working solutions were thawed in a refrigerator prior to analysis. Tubes were vortexed thoroughly and centrifuged for 10 min after being thawed. To each labelled microcentrifuge vial containing a 500 μl plasma sample, 50 μl of internal standard solution (50 ng/ml) was added, followed by the addition of 400 μl of ammonium acetate solution (100 mM) and 2.8 ml of methyl tert-butyl ether (MTBE). Vials were capped and immediately vortex-mixed at max speed for 10 s and centrifuged at 4°C for 15 min. Simvastatin and simvastatin acid were shown to be stable in plasma for at least 3 h at this temperature. Vials were placed on a dry ice-ethanol bath for 10 min to freeze the lower aqueous phase. The upper organic layers were transferred to labelled glass test tubes and the solvent was evaporated in a TurboVap evaporator at 37°C under a gentle nitrogen stream. The residues were reconstituted with 100 μl of 70:30 acetonitrile–ammonium acetate buffer, 1 mM, pH 4.5 and vortexed for 15 s. Volumes of 20 μl of each reconstituted sample in the microinserts were injected into the LC/MS/MS for analysis. The precursor/ product ion transitions were monitored at m/z 435.2 → m/z 319.1 for (simvastatin acid −H)—followed by m/z 419.1 → m/z 199.1 for (simvastatin+H) +and m/z 405.1.1 → m/z 199.1 for (lovastatin+H)+. The mass spectrometer was operated in the negative ion detection mode for the first 2 min with a dwell time of 500 ms, and then positive ion mode for the rest of the analytical run with dwell time of 600 ms. The cone voltage was set at 30 V and the collision energy was optimized at 15 V for both ion modes.
Acceptable precision (between 2.99 and 18.31% for simvastatin; between 1.84 and 18.26% for simvastatin acid) and accuracy (between −7.00 and 3.15% for simvastatin; between −3.08 and 11.25% for simvastatin acid) were obtained for concentrations over the linear calibration curve range (0.1–10 ng/ml).
Both simvastatin and simvastatin acid were stable after undergoing three freeze (−70°C)—thaw (+4°C) cycles and under autosampler storage conditions for at least 24 h at 4°C and in a reconstitution solution [70:30 acetonitrile–ammonium acetate (1 mM, pH 4.5)]. Both analytes were stable in plasma at −70°C for at least 6 months.
Pharmacokinetic Analysis
The pharmacokinetic parameters for simvastatin and simvastatin acid were determined from the plasma concentration-time profiles by the non-compartment method using Topfit® 2.0 software (17). Maximum plasma concentration (C max) and time to C max (t max) were determined directly from the individual plasma concentration versus time curves. The area under the curve was determined from zero up to the last quantifiable concentration AUC0–24 h, AUC0–30 h and extrapolated to infinity \(AUC_{0 \to \infty } \)(18). The terminal log-linear phase of the plasma concentration-time curve was visually identified for each subject. The elimination rate constant λz was estimated from the slope of the linear regression line of the log-transformed concentration versus time data in the terminal phase. The total clearance (CLtot) and the volume of distribution (Vd) were calculated from:
where in case of an oral administration f is the bioavailability, so that the term CL/f is the oral clearance.
Topfit® 2.0 and WinNonlin® program (Pharsight Corporation, NC, USA) were used to fit two and/or three compartment models to plasma concentration versus time data. In all subjects data were weighted by 1/c, where c is the plasma concentration. In a second approach, the same data sets were fitted using the same disposition function but including a two segment absorption model (Fig. 1). The decision on the appropriateness of the compartment model was based upon the Akaike criterion. Multifraction absorption models have been reported for drugs which give irregular or discontinuous absorption profiles (19). This approach provided a suitable alternative to the analysis of plasma concentrations of drugs such as simvastatin, which after oral administration, exhibited multiple peaks (20).
A three-segment two compartment absorption model. X 1, X 2—the amounts of the drug in compartment 1 and 2; D 1, D 2, D 3—fractions of the dose D absorbed from the gastrointestinal tract at different times after dosing; K a1, K a2, K a3—the rate of absorption in different segments of the GIT; K 12, K 21—rate constants for the movement of drug from the central compartment 1 to peripheral compartment 2 and from compartment 2 to 1; K 10—elimination rate constant from the central compartment.
Statistical Analysis
Results are expressed as mean values with standard deviations (SD) in tables and as mean values with standard error of mean (SEM) in plasma concentration profile figures. Statistical analysis was carried out using the ANOVA test, followed by Tukey-Kramer Multiple Comparisons Tests integrated in GraphPrism® version 3 (GraphPad Software, San Diego, USA) to assess the statistical significance of the differences between the results. Difference between two related parameters was considered to be statistically significant for p value equal or less than 0.05.
RESULTS AND DISCUSSION
Development of Solid Dosage Forms for Simvastatin
The newly developed dosage forms of simvastatin ensured an intimate contact of the low water soluble API with the mixture of gelatin and lecithin (1:1). As described in (14), gelatin, a naturally derived collagen extract carrying both positive and negative charges, most likely coats the particles of the API and prevents their aggregation or clumping. This results in an improved wettability of hydrophobic drug particles through polar interactions. In addition, the amphiphilic lecithin reduces surface tension between the dissolution fluid and the particle surface. Alternatively, it may form a microemulsion or micelles, which can entrap hydrophobic drug material and thus facilitate the dissolution of simvastatin. The aqueous solubility of simvastatin (less than 10 mg/l at 37°C), was increased by more than 5,000-fold (67.5 mg/l at 37°C) through embedding with gelatin and lecithin. After the coating process, the solvent (water) was removed by freeze-drying. The bulking agent mannitol has excellent cake forming properties, providing mechanical strength and attractive appearance for the matrix. Using this excipient, a good free-flowing product was obtained, containing only 0.5% residual water. The solution of butylhydroxytoluol was added in order to prevent oxidation of simvastatin (21).
The release of the water insoluble drug simvastatin was controlled by the addition of glyceryl palmitostearate (Precirol® ATO 5). Precirol® was chosen by virtue of its good stability at various pH values and low moisture levels, and well established safety-profile in humans (22). Tablets formulated with different levels of Precirol® yielded linear release of simvastatin for at least 12 h (14). It has been reported that the use of Precirol® ATO 5 can sometimes lead to unacceptable slow drug release due to its high hydrophobicity especially when the formulated drug is poorly soluble (22,23). For example, strong interaction between felodipine and lipophilic excipients, such as Precirol® resulted in prolonged and incomplete release of felodipine from the tablets (24). In order to prevent this, hydrophilic excipients such as mannitol, hydroxypropylmethylcelluose (25), Poloxamer® 407, Pluronic® F 127 (26) can be added to Precirol® in order to adjust the release of the API from the matrix. The combination of a lipid-based matrix and the hydrophilic mannitol may thus increase chances for complete dissolution in the lower parts of the gastrointestinal tract, where limited fluid volume is available (27). Rapid dissolution of mannitol will create channels in the lipophilic matrix that will allow the dissolution medium to penetrate the matrix and dissolve the drug.
The final delayed release dosage form tested in the human study was composed of a drug-containing core and a polymeric coating composed of polymethylmethacrylate (Eudragit® RS). Eudragit® RS is a water-insoluble, but swellable polymer independent of the pH of the dissolution fluid. In the swollen state the active pharmaceutical ingredient is gradually dissolved and diffuses through the polymer membrane thus ensuring a delayed release profile. The rate of drug release decreased by increasing coating thickness, due to the longer drug diffusion pathways and increased tortuosity at higher coating levels.
As can be seen in Fig. 2 the rate of release was inversely proportional to the thickness of the coat, implying that the film coat was controlling the release process. The increased lag time at the higher coating level demonstrated the effect of coating thickness on the dissolution rate.
The formulation at a 6% coating level was preferred over the 10% coating level to be included in the clinical trial since it was expected that strongly delayed and slow release rates might adversely affect dissolution of the low soluble simvastatin in the lower gastrointestinal tract where less fluid is available and viscosity is increased (28). Thus the advantage of decreased intestinal first pass effect might be lost due to a dissolution problem.
For comparison the in vitro release characteristics of the immediate release capsules and the reference formulation Zocor® are shown in Fig. 3.
Pharmacokinetic Study in Humans
Pharmacokinetic Analysis Based on Parent Compound
A single-dose pharmacokinetic study was performed in the Clinical Research Center (University of Mainz, Germany) according to the codes and guidelines of Good Clinical Practice and the Declaration of Helsinki in its revised form from 1996. Grapefruit juice, which is an inhibitor of CYP 3A4 (29), was prohibited for 2 weeks prior to each and during the study days. The possible effect of food or beverages on the pharmacokinetics of the study drug was minimised by a fasting period before ingestion of drugs and by serving standardised meals on all study days. Since in previous studies the menstrual cycle and use of oral contraceptives has not been found to affect the metabolism of CYP 3A4 substrates (30–33) both females and males were recruited as study volunteers. Simvastatin was well tolerated by all volunteers, unexpected incidents that could have influenced the outcome of the study did not occur. There was no drop out and all volunteers who started the study continued to the end and were discharged in good health.
Figure 4 shows the plot of mean simvastatin plasma concentrations versus time from the delayed release tablet, immediate release capsule and immediate release tablet Zocor®. Table I shows the pharmacokinetic parameters following administration of the formulations. Both immediate release formulations were rapidly absorbed from the gastrointestinal tract and simvastatin was measurable at the first sampling time (0.5 h) in all volunteers. Maximum simvastatin plasma concentrations of 2.46 ± 0.93 ng/ml and 2.68 ± 1.33 ng/ml were attained at 2.07 ± 1.62 h and 2.36 ± 1.65 h after administration of the immediate release capsule and Zocor®, respectively. After C
max was reached, concentrations declined rapidly until 5 h post dose and were detectable up to 24 h. In the case of the modified release formulation, the release was designed to commence after a predetermined lag time such that a continuous input over an extended period of time existed. In all subjects prolonged drug absorption was achieved with this delayed release formulation. The corresponding plasma concentration time profile of simvastatin following administration of delayed release tablets demonstrated a delayed, but higher peak concentration. There was no evidence of dose dumping or loss of rate control. Upon oral administration of delayed release tablets, simvastatin appeared in plasma after approximately 3 h, but the drug was released slowly from the tablet and reached peak concentrations at 6.29 ± 1.98 h. The mean C
max for simvastatin was found to be 4.21 ± 2.03 ng/ml. The tablet was formulated so as to release minimal amounts of simvastatin in the stomach and in the upper small intestine, yet to release the majority of the drug in the ileum and the proximal colon. The arithmetic mean CmaxIRcapsule/CmaxZocor® ratio was 0.92, the CmaxDR/CmaxZocor® ratio was 1.57. The \(AUC_{0 \to \infty } \) estimated after the single dose of 20 mg of the delayed release product was 44.92 ± 14.88 ng h/ml compared with 15.11 ± 9.13 ng h/ml for the immediate release capsule and 14.81 ± 7.28 ng h/ml for Zocor®. Less than 20% of the total \(AUC_{0 \to \infty } \) was extrapolated in all cases after oral administration. The  ratio based on arithmetic mean values was 1.02. The
ratio based on arithmetic mean values was 1.02. The  ratio based on arithmetic mean values was 3.03. Based on the analysis of variance of log-transformed data, the \(AUC_{0 \to \infty } \) for the delayed release was significantly higher than for Zocor® (p < 0.01). The \( AUC_{{0 \to \infty }} \) of simvastatin immediate release capsules was not significantly different from \(AUC_{0 \to \infty } \)of Zocor® (p > 0.05). The average half-life of simvastatin after administration of the delayed release formulation was 10.67 ± 3.44 h compared with 7.12 ± 2.17 h after immediate release capsules and 6.75 ± 2.67 h after Zocor®. The results showed a significant difference between the terminal rate constant following the delayed release dosage form compared to the IR reference formulations. The higher \(AUC_{0 \to \infty } \) and C
max values, later t
max and longer t
1/2 observed for the delayed and extended release formulation in comparison with the IR formulations are indicative of in vivo delayed release of simvastatin and reduced presystemic metabolism resulting in increased bioavailability from the modified release formulation.
ratio based on arithmetic mean values was 3.03. Based on the analysis of variance of log-transformed data, the \(AUC_{0 \to \infty } \) for the delayed release was significantly higher than for Zocor® (p < 0.01). The \( AUC_{{0 \to \infty }} \) of simvastatin immediate release capsules was not significantly different from \(AUC_{0 \to \infty } \)of Zocor® (p > 0.05). The average half-life of simvastatin after administration of the delayed release formulation was 10.67 ± 3.44 h compared with 7.12 ± 2.17 h after immediate release capsules and 6.75 ± 2.67 h after Zocor®. The results showed a significant difference between the terminal rate constant following the delayed release dosage form compared to the IR reference formulations. The higher \(AUC_{0 \to \infty } \) and C
max values, later t
max and longer t
1/2 observed for the delayed and extended release formulation in comparison with the IR formulations are indicative of in vivo delayed release of simvastatin and reduced presystemic metabolism resulting in increased bioavailability from the modified release formulation.
Double peaks were noted in the simvastatin plasma concentration-time curves. After administration of the immediate release formulations secondary peaks in individual concentration-time profiles occurred approximately 5 h after dosing. For some of the volunteers, the second peak was the C max. This may have contributed to the variability in mean t max. Several hypotheses based on region-dependent variation in absorption, enterohepatic circulation, variable gastric emptying, intestinal transit time, and intestinal bacterial reconversion of biliary metabolites have been proposed to account for these observations (34). Simvastatin metabolites are eliminated to a large extent through the biliary route. The glucuronide conjugate of simvastatin acid and its lactone have been recovered from bile. In principle, either the intestinal deconjugation of the glucuronide conjugates of simvastatin acid or the reabsorption of simvastatin as lactone would complete the enterohepatic cycle. It could be that enterohepatic circulation caused multiple peaking in plasma. Cheng at al. reported that secondary peaks were evident in the plasma profiles of most patients treated with simvastatin (20). Delayed release of simvastatin did not reduce the occurrence of double peaks in the plasma concentration-time curve. The number of peaks varied from subject to subject.
A significant difference in MRTabs of the drug was apparent when it was administered as immediate release in comparison to delayed release dosage forms (Table II). Similarly, there was a significant difference in the absorption rate constant (K01) of simvastatin when it was administered as an immediate versus delayed release dosage form. The decrease in K01 with increased Cmax and \(AUC_{0 \to \infty } \) after administration of delayed release compared with immediate release dosage forms might be due to the lower absorptive surface area of the colon and the slower release rate from the dosage form, resulting in slow, but complete absorption of intact simvastatin. The rapid release of the drug from the immediate release tablets ensures immediate absorption from the small intestine resulting in early tmax, but lower Cmax and \(AUC_{0 \to \infty } \) indicating significant metabolism of simvastatin in the upper small intestine.
Pharmacokinetic Analysis Based on Metabolite Simvastatin Acid
Mean plasma concentration-time profiles of simvastatin acid following administration of simvastatin immediate and delayed release formulations are presented in Fig. 5. Arithmetic means and standard deviations of pharmacokinetic parameters are given in Table III. The overall metabolite levels from the immediate release capsules tended to be higher throughout the period studied than following administration of Zocor®. Mean maximum concentration of simvastatin acid observed after the 20 mg dose of the delayed release formulation was 0.91 ± 0.3 ng/ml compared with 1.23 ± 0.51 ng/ml for the immediate release capsules and 0.73 ± 0.36 ng/ml for Zocor®. Based on the arithmetic means, the CmaxDR/CmaxZocor® ratio was 1.24 and the CmaxIRcapsules/CmaxZocor® ratio was 1.67. The corresponding t
max values were 6.86 ± 1.07 h for the delayed release product, 5.29 ± 0.76 h and 6.14 ± 1.35 h for immediate release capsules and Zocor®, respectively. The \(AUC_{0 \to \infty } \) estimated after single dose of the 20 mg delayed release product was 13.13 ± 4.77 ng h/ml compared with 12.03 ± 5.08 ng h/ml for the immediate release capsules and 7.27 ± 3.40 ng h/ml for Zocor®. The  ratio based on arithmetic mean values was 1.81 and
ratio based on arithmetic mean values was 1.81 and  was 1.65. These results illustrate approximately 65% to 80% higher systemic levels of simvastatin acid after administration of IR capsule and delayed release tablet compared to Zocor®.
was 1.65. These results illustrate approximately 65% to 80% higher systemic levels of simvastatin acid after administration of IR capsule and delayed release tablet compared to Zocor®.
Simvastatin acid/simvastatin \(AUC_{0 \to \infty } \)ratios after a single dose of IR formulation ranged from 0.48 to 2.13 (mean ± SD = 0.94 ± 0.56). Metabolite/parent compound \(AUC_{0 \to \infty } \)ratios after a single dose of the delayed release formulation ranged from 0.13 to 0.75 (mean ± SD = 0.35 ± 0.21). Thus the metabolite to parent drug AUC ratio was approximately threefold lower after the delayed release compared to the immediate release formulation indicating that the delayed release dosage form diminishes the extent of presystemic metabolism.
The comparison between Zocor® and immediate release simvastatin capsules in vivo showed no significant differences regarding pharmacokinetic parameters of the simvastatin lacton, yet plasma concentrations of the parent compound were lower following administration of the immediate release capsules as compared to Zocor®. On the other hand, C max and \(AUC_{0 \to \infty } \) data for simvastatin acid illustrated higher systemic concentrations of this metabolite for the immediate release capsules as compared to the reference formulation. It has been reported that within the stomach hydrolysis of the simvastatin lactone is very limited (35). Lack of hydrolytic enzymes and stomach acidity combine to favor the perpetuation of the closed low soluble lactone form as simvastatin enters the small intestine. The presence of gelatin, lecithin and mannitol in the freeze dried powder, filled in capsules, could increase solubilization and hydrolysis of the closed lactone form of simvastatin, converting it to the open hydroxyl acid in the stomach and the upper small intestine, and thereby increasing the amount of this metabolite. These results are in accordance with data published in WO Patent 2005/044258 A1, where the presence of surface active agent (e.g. SLS, Tween®) in the formulation resulted in increased conversion of the lacton form to the hydroxyl acid in a simulated gastric environment and significantly higher AUC for simvastatin acid compared with Zocor® (35).
Compared with Zocor®, the delayed release formulation exhibited delayed and extended release characteristics in terms of both simvastatin and simvastatin acid. The present study indicated that the administration of simvastatin in form of delayed release tablets increased simvastatin bioavailability by a factor of three, as compared to the reference formulation Zocor®. It is generally accepted that the measured overall systemic availability F, following an oral drug dose, is:
where FF is the fraction of the drug dose neither lost in the feces nor decomposed in the humans (36). Thus, when FG increases and FF as well FH remain constant, an increase in AUCparent will be expected for a dosage form that minimizes the intestinal first-pass loss of the delivered compound. An increased systemic availability of the parent drug should be followed by a decrease of the systemic availability of the metabolite which is generated by the first-pass metabolism. One explanation for the metabolite data (Table III), showing that AUCSA(delayed release) slightly exceed AUCSA(immediate release capsule), is given if one assumes that a fraction of the dissolved simvastatin hydrolyzes to simvastatin acid in the acidic environment of the stomach. The metabolite formed may be less efficiently absorbed from the intestine, due to its more polar properties or in addition, as CYP 3A substrate (10) may be further metabolized in the intestinal wall.
The cytochrome P450 3A4 and 3A5 enzymes, primarily responsible for the metabolism of simvastatin, are expressed both in the liver and in the gut (1,37). Studies of cyclosporine, diltiazem (38), and midazolam disposition indicated that CYP 3A metabolic activity in the intestinal mucosa may substantially contribute to the overall first-pass effect. In vivo and in vitro midazolam data suggested that the small intestine may represent a major source of interindividual variability in oral bioavailability (39). The large increase in AUC caused by grapefruit juice in addition suggests that intestinal wall metabolism is significant with respect to presystemic elimination of simvastatin (40). US Patent 6652865 described that simvastatin undergoes a strong first intestinal passage effect (41).
The localization of CYP 3A in the gut is not uniform (2,3) with higher levels of this enzyme in the jejunum, slightly lower levels in the duodenum, and significantly lower levels in the ileum, caecum, and colon. First-pass intestinal metabolic extraction may depend on the absorption characteristics of the drug formulation. Conventional IR formulations release drug predominantly in the stomach and upper small intestine, thereby presenting the drug to the region of the small intestine with the highest levels of CYP 3A. First-pass intestinal metabolism may be reduced when the drug is absorbed at more distal sites of the small intestine. Results reported by Homsy et al. confirmed that the first-pass effect of diltiazem in the distal portion of the small intestine of rabbits was at least half the value of that in the proximal intestine (42).
The delayed release formulation studied in the present investigation protected simvastatin from metabolism in either the lumen of the gut and/or during the absorption process. One part of the bioavailability enhancement represents the lower concentration of CYP isoforms in the distal gastrointestinal tract, which become more readily saturated by the simvastatin delayed release formulation. Therefore, more unmetabolized simvastatin is available for absorption and presentation to the site of cholesterol synthesis in the liver. Simvastatin metabolites may be absorbed less efficiently than the non-transformed parent compound. Moreover, even if the polar metabolites were absorbed, they would be extracted less efficiently into the hepatocytes due to their lower lipophilicity. The simvastatin lactone (logD7.0 = 4.4, pKa = 13.5) is more lipophilic than simvastatin acid (logD7.0 = 1.88, pKa = 4.3). As simvastatin acid is ionized in plasma and thus mildly lipophilic, it poorly penetrates the hepatocyte plasma membrane via passive diffusion and requires carrier-mediated uptake. Pasanen et al. showed that OATP1B1 polymorphism markedly affects the pharmacokinetics of simvastatin acid (43), suggesting that simvastatin acid undergoes transporter-mediated uptake in the human hepatocytes. The rate of transport-mediated hepatic uptake determinates the pharmacological effect of simvastatin acid. Simvastatin inhibits OAT1B1-mediated transport, suggesting that that it may also be a substrate of this transporter, but hepatic uptake was explained mainly by extensive passive diffusion. Conversion of simvastatin to its active metabolite should preferably take place in the liver at its pharmacologic target. Preclinical data have indicated that statins such as lovastatin and simvastatin are more efficiently extracted by the liver than their corresponding β-hydroxy acids, with subsequent minimization of systemic burden (44,45). Similarly, data obtained in various species have shown higher liver accumulation with simvastatin and lovastatin lactones than with their respective open acid forms due to their facilitated passive diffusion through hepatocyte membranes and selective accumulation in the liver (46).
CONCLUSIONS
Therapeutic Advantages
The human study presented here serves as in vivo confirmation that the site of absorption in the intestine can modulate the bioavailability of simvastatin. This could be mainly due to regional differences in the ability of the intestine to metabolize simvastatin. A combined strategy of controlled and delayed release within the distal small intestine and the proximal colon resulted in higher systemic plasma levels of simvastatin than immediate release dosing at equal doses. This would most likely allow reduced doses of API for the delayed release dosage form, thereby reducing also potential side effects of the drug and possible drug/drug interactions. The mechanism by which these drug/drug interactions can be prevented has been outlined previously by Sawada et al., who describes the use of a timed-release formulation to prevent drug–drug interactions between midazolam and diltiazem by modifying the release pattern of both drugs. By separating time and space of release of the two drugs their interaction can be minimized if not avoided (47). Similarly, a delayed release dosage form of simvastatin could be administered together with an immediate release dosage form of a CYP 3A inhibitor with minimum pharmacokinetic interaction of both drugs. Directly following oral administration of both dosage forms, the drug from the immediate release formulation would be released and absorbed while the release and absorption of simvastatin would not occur until 3 to 4 h later. Thus the patient benefits from the convenience of taking both dosage forms simultaneously without the risk of a potential drug–drug interaction.
The tested delayed release formulation in humans may be considered suitable for the use with drugs which are expected to exhibit therapeutic effects several hours after intake, e.g. from midnight to daybreak. Cholesterol synthesis follows a circadian rhythm, with peak synthesis occurring in late night and early morning hours. Modified release formulations, in which plasma drug levels peak a number of hours after administration, would yield peak plasma levels of the drug that coincide with peak cholesterol synthesis times, thereby increasing the efficacy of the drug. Additional studies are needed to evaluate the same lipid lowering response with reduced dose of simvastatin delayed release dosage form.
The same formulation principle as illustrated in this article may also be used for the formulation development of other CYP 3A substrates (e.g. midazolam, felodipine, terfenadine, tamoxifen, taxol). Keeping in mind the metabolic activity of the intestine when designing modified release formulations of drugs highly extracted by this organ it should be feasible by combined delayed and controlled release to achieve equal efficacy with a reduced dose of CYP 3A substrate.
References
P. Watkins. Drug metabolism by cytochromes P450 in the liver and small bowel. Gastroenterol. Clin. North Am. 21:511–526 (1992).
Q. Zhang, D. Dunbar, A. Ostrowska, S. Zeisloft, J. Yang, and L. Kaminsky. Characterization of human small intestinal cytochromes P-450. Drug Metab. Dispos. 27:804–809 (1999).
R. McKinnonand, and M. McManus. Localization of cytochromes P450 in human tissues: Implications for chemical toxicity. Pathology 28:148–155 (1996).
M. Thorn, N. Finnstrom, S. Lundgren, A. Rane, and L. Loof. Cytochromes P450 and MDR1 mRNA expression along the human gastrointestinal tract. Br. J. Clin. Pharmacol. 60:54–60 (2005).
O. von Richter, O. Burk, M. Fromm, K. Thon, M. Eichelbaum, and K. Kivistö. Cytochrome P450 3A4 and P-glycoprotein expression in human small intestinal enterocytes and hepatocytes: a comparative analysis in paired tissue specimens. Clin. Pharmacol. Ther.172–183 (2004).
A. Basit. Advances in colonic drug delivery. Drugs 65:1991–2007 (2005).
D. R. Friend. Oral colon-specific drug delivery, CRC Press, Boca Raton, FL, 1992.
G. Patel. Oral colon-specific drug delivery: an overview. Drug Delivery Techno. 6:62–71 (2006).
G. Amidon and J. Crison. Water soluble pharmaceutical coating and method for producing coated pharmaceuticals, US Patent, 1998.
T. Prueksaritanont, B. Ma, and N. Yu. The human hepatic metabolism of simvastatin hydroxy acid is mediated primarily by CYP3A, and not CYP2D6. Br. J. Clin. Pharmacol. 56:120–124 (2003).
A. Tornio, M. Pasanen, J. Laitila, P. Neuvonen, and J. Backman. Comparison of 3-hydroxy-3-methylglutaryl Coenzyme A (HMG-CoA) reductase inhibitors (statins) as inhibitors of cytochrome P450 2C8. Basic Clin. Pharmacol. Toxicol. 97:104–108 (2005).
C. Transon, T. Leemann, and P. Dayer. In vitro comparative inhibition profiles of major human drug metabolising cytochrome P450 isozymes (CYP2C9, CYP2D6 and CYP3A4) by HMG-CoA reductase inhibitors. Eur. J. Clin. Pharmacol. 50:209–215 (1996).
T. Prueksaritanont, R. Subramanian, X. Fang, M. Bennett, Y. Qiu, J. Lin, P. Pearson, and T. Baillie. Glucuronidation of statins in animals and humans: a novel mechanism of statin lactonization. Drug Metab. Dispos. 30:505–512 (2002).
J. Hilfinger, J. Kim, and P. Kijek. Methods and composition of extended delivery of water insoluble drugs. In U. P. A. Publication (ed.) (U. P. A. Publication, ed.), USA, 2005.
L. Schmuff. HPLC Method for Pharmaceutical Analysis. John Willey & Sohns, New York, 1997.
J. Zhao, I. H. Xie, A. Yang, B. Roadcap, and J. Rogers. Quantitation of simvastatin and its ß-hydroxy acid in human plasma by liquid–liquid cartridge extraction and liquid chromatography/tandem mass spectrometry. J. Mass Spectrom. 35:1133–1143 (2000).
G. Heinzel, R. Woloszczak, and P. Thomann. TopFit, Version 2.0: Pharmacokinetic and pharmacodynamic data analysis system for the PC, G. Fischer: VCH Publishers, 1993.
M. Gibaldi, and D. Perrier. Pharmacokinetics. Marcel Dekker, New York, 1982.
I. Mahmood. Pharmacokinetic analysis of the absorption characteristics of diclofenac sodium in man by use of a multi-segment absorption model. J. Pharm. Pharmacol. 48:1260–1263 (1996).
H. Cheng, J. Rogers, A. Sweany, M. Dobrinska, E. Stein, A. Tate, R. Amin, and H. Quan. Influence of age and gender on the plasma profiles of 3-hydroxy-3-methylglutaryl-Coenzyme A (HMG-CoA) reductase inhibitory activity following multiple doses of lovastatin and simvastatin. Pharm. Res. 9:1629–1633 (1992).
M. Kaufman. Applications of oxygen polarography to drug stability testing and formulation development: solution-phase oxidation of hydroxymethylglutaryl Coenzyme A (HMG-CoA) reductase inhibitors. Pharm. Res. 7:289–292 (1990).
M. Ozyazici, E. Gokce, and G. Ertan. Release and diffusional modeling of metronidazole lipid matrices. Eur. J. Pharm. Biopharm. 63:331–339 (2006).
V. Jannin, E. Pochard, and O. Chambin. Influence of poloxamers on the dissolution performance and stability of controlled-release formulations containing Precirol ATO 5. Int. J. Pharm. 309:6–15 (2006).
M. Savolainen, C. Khoo, H. Glad, C. Dahlqvist, and A. Juppo. Evaluation of controlled-release polar lipid microparticles. Int. J. Pharm. 244:151–161 (2002).
P. Parab, C. Oh, and W. Ritschel. Sustained release from Precirol (glycerol palmito-stearate) matrix: effect of mannitol and hydroxypropyl methylcellulose on the release of theophylline. Drug Dev. Ind. Pharm. 12:1309–1327 (1986).
M. Savolainen, J. Herder, C. Khoo, K. Lovqvist, C. Dahlqvist, H. Glad, and A. Juppo. Evaluation of polar lipid-hydrophilic polymer microparticles. Int. J. Pharm. 262:47–62 (2003).
J. Sousa, A. Sousa, M. Moura, F. Podczeck, and J. Newton. The influence of core materials and film coating on the drug release from coated pellets. Int. J. Pharm. 233:111–122 (2002).
H. Stevens, C. Wilson, P. Welling, M. Bakhshaee, J. Binns, A. Perkins, M. Frier, E. Blackshaw, M. Frame, and D. Nichols. Evaluation of Pulsincap to provide regional delivery of dofetilide to the human GI tract. Int. J. Pharm. 236:27–34 (2002).
D. Bailey, J. Kreeft, C. Munoz, D. Freeman, and J. Bend. Grapefruit juice-felodipine interaction: Effect of naringin and 6. ,7. -dihydroxybergamottin in humans. Clin. Pharmacol. Ther. 64:284–256 (1998).
A. Kashuba, J. J. Bertino, M. Rocci, R. Kulawy, D. Beck, and A. Nafziger. Quantification of 3-month intraindividual variability and the influence of sex and menstrual cycle phase on CYP3A activity as measured by phenotyping with intravenous midazolam. Clin. Pharmacol. Ther. 64:269–277 (1998).
E. Kharasch, M. Russell, K. Garton, G. Lentz, T. Bowdle, and K. Cox. Assessment of cytochrome P450 3A4 activity during the menstrual cycle using alfentanil as a noninvasive probe. Anesthesiology 87:26–35 (1997).
J. Scavone, D. Greenblatt, A. Locniskar, and R. Shader. Alprazolam pharmacokinetics in women on low-dose oral contraceptives. J. Clin. Pharmacol. 28:454–457 (1988).
G. Stoehr, P. Kroboth, R. Juhl, D. Wender, J. Phillips, and R. Smith. Effects of oral contraceptives on trizolam, temazepam, alprazolam, and lorazepam kinetics. Clin. Pharmacol. Ther. 36:683–690 (1984).
H. Lennernäs, and C. Regardh. Evidence for an interaction between the beta-blocker pafenolol and bile salts in the intestinal lumen of the rat leading to dose-dependent oral absorption and double peaks in the plasma concentration-time profile. Pharm. Res. 10:879–883 (1993).
M. Flash-Ner-Barak, I. Lerner, V. Rosenberger, and N. Moldavski. Simvastatin formulations and methods of making same. In T. p. i. ltd. (ed.), Vol. WO 2005/044254 A1 (T. p. i. ltd., ed.), Israel, 2005, pp. 1–32.
T. N. Tozerand, and M. Rowland. Introduction to Pharmacokinetics and Pharmacodynamics: The Quantitative Basis of Drug Therapy. Lippincott Williams & Wilkins, USA, 2006.
J. Kolars, K. Lown, P. Schmiedlin-Ren, M. Ghosh, C. Fang, S. Wrighton, R. Merion, and P. Watkins. CYP3A gene expression in human gut epithelium. Pharmacogenetics 4:247–259 (1994).
O. Mousa, D. Brater, K. Sundblad, and S. Hall. The interaction of diltiazem with simvastatin. Clin. Pharmacol. Ther. 67:267–274 (2000).
K. Thummel, D. O’Shea, M. Paine, D. Shen, K. Kunze, J. Perkins, and G. Wikinson. Oral first-pass elimination of midazolam involves both gastrointestinal and hepatic CYP3A-mediated metabolism. Clin. Pharmacol. Ther. 59:491–502 (1996).
J. Lilja, K. Kivisto, and P. Neuvonen. Grapefruit juice-simvastatin interaction: effect on serum concentrations of simvastatin, simvastatin acid, and HMG-CoA reductase inhibitors. Clin. Pharmacol. Ther. 64:477–483 (1998).
H. Benameur, V. Jannin, and D. Roulot. Method and formulation for decreasing statin metabolism. In F. Gattefosse Holding (ed.), Vol. US 6,652,865 B2 (F. Gattefosse Holding, ed.), USA, 2003.
W. Homsy, G. Caille, and P. du Souich. The site of absorption in the small intestine determines diltiazem bioavailability in the rabbit. Pharm. Res. 12:1722–1726 (1995).
M. Pasanen, M. Neuvonen, P. Neuvonen, and M. Niemi. SLCO1B1 polymorphism markedly affects the pharmacokinetics of simvastatin acid. Pharmacogenetics and Genomics 16:873–879 (2006).
M. Davidson. A look to the future: new treatment guidelines and a perspective on statins. Am. J. Med. 112 (Suppl 8A):34S–41S (2002).
M. Davidson, P. Lukacsko, J. Sun, G. Phillips, E. Walters, A. Sterman, R. Niecestro, and L. Friedhoff. A multiple-dose pharmacodynamic, safety, and pharmacokinetic comparison of extended- and immediate-release formulations of lovastatin. Clin. Ther. 24:112–125 (2002).
B. Hamelinand, and J. Turgeon. Hydrophilicity/lipophilicity:relevance for the pharmacology and clinical effects of HMG-CoA reductase inhibitors. TiPS 19:26–37 (1998).
T. Sawada, K. Sako, K. Yoshihara, K. Nakamura, S. Yokohama, and M. Hayashi. Timed-release formulation to avoid drug–drug interaction between diltiazem and midazolam. J. Pharm. Sci. 92:790–797 (2003).
Acknowledgements
The authors wish to thank Dr. Elke Lipka, TSRL Inc. for kindly revising the manuscript and Ute Hartung, Johannes Gutenberg-University Mainz, for helpful technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tubic-Grozdanis, M., Hilfinger, J.M., Amidon, G.L. et al. Pharmacokinetics of the CYP 3A Substrate Simvastatin following Administration of Delayed Versus Immediate Release Oral Dosage Forms. Pharm Res 25, 1591–1600 (2008). https://doi.org/10.1007/s11095-007-9519-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-007-9519-6