Purpose
To determine the roles of blood–brain barrier (BBB) transport and plasma protein binding in brain uptake of nonsteroidal anti-inflammatory drugs (NSAIDs)—ibuprofen, flurbiprofen, and indomethacin.
Methods
Brain uptake was measured using in situ rat brain perfusion technique.
Results
[14C]Ibuprofen, [3H]flurbiprofen, and [14C]indomethacin were rapidly taken up into the brain in the absence of plasma protein with BBB permeability–surface area products (PSu) to free drug of (2.63 ± 0.11) × 10−2, (1.60 ± 0.08) × 10−2, and (0.64 ± 0.05) × 10−2 mL s−1 g−1 (n = 9–11), respectively. BBB [14C]ibuprofen uptake was inhibited by unlabeled ibuprofen (K m = 0.85 ± 0.02 mM, V max = 13.5 ± 0.4 nmol s−1 g−1) and indomethacin, but not by pyruvate, probenecid, digoxin, or valproate. No evidence was found for saturable BBB uptake of [3H]flurbiprofen or [14C]indomethacin. Initial brain uptake for all three NSAIDs was reduced by the addition of albumin to the perfusion buffer. The magnitude of the brain uptake reduction correlated with the NSAID free fraction in the perfusate.
Conclusions
Free ibuprofen, flurbiprofen, and indomethacin rapidly cross the BBB, with ibuprofen exhibiting a saturable component of transport. Plasma protein binding limits brain NSAID uptake by reducing the free fraction of NSAID in the circulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Considerable evidence exists that supports a neuroprotective role for nonsteroidal anti-inflammatory drugs (NSAIDs) in Alzheimer's disease (AD) and other neurodegenerative disorders. Epidemiologic studies have consistently linked long-term NSAID use with a reduced risk for AD (1). Invitro, NSAIDs inhibit β-amyloid (Aβ) aggregation, decrease Aβ formation, and limit microglial and astrocytic activation (2). In vivo, long-term high-dose NSAID administration to Tg2576 transgenic AD mice is associated with reduced Aβ plaques and cerebral Aβ42 levels (3,4). Both cyclooxygenase (COX)-dependent and -independent mechanisms have been linked to these actions. However, NSAID concentrations required for some COX-independent pathways (20–150 μM) markedly exceed brain NSAID concentrations obtained in vivo at normal doses (0.4–3 μM) (2–4).
Most NSAIDs that exhibit good activity against AD models, such as ibuprofen, flurbiprofen, and indomethacin, distribute poorly to the brain. For ibuprofen, the vascular-corrected brain concentration at steady state is only 1–2% of that of the total plasma concentration (5). Similar low values have been reported for flurbiprofen, ketoprofen, and naproxen (4). Cerebrospinal fluid (CSF) distribution is also minimal (<1–5% of plasma) for many NSAIDs (6,7). Together, these results suggest that some barrier exists that limits brain uptake of acidic NSAIDs.
Brain delivery for many agents is restricted by the blood–brain barrier (BBB), which is formed by tight junctions between brain endothelial cells (8,9). These junctions block paracellular transfer and force most agents to cross the BBB either by lipophilic transcellular diffusion or by specialized carrier- or receptor-mediated transport mechanisms. Most NSAIDs are lipophilic (log D oct −1 to +2) and thus might be expected to cross the BBB readily by passive diffusion (10). However, the majority of NSAIDs circulate in plasma as organic anions (>99% charged), such that the small neutral (un-ionized) fraction may prove limiting to brain uptake. Furthermore, the BBB expresses a large number of organic anion transporters (11) that are capable of restricting brain uptake for a broad array of solutes. A number of these transporters are known to interact with NSAIDs either as substrates or inhibitors (12,13). Moreover, many NSAIDs bind with high affinity to serum albumin, thus reducing the free fraction in the circulation to ≤5% (14). In several tissues, drug uptake markedly exceeds that predicted by the plasma free drug concentration and mass action exchange between free and bound pools as plasma transits the capillary from the arterial to the venous end (15). Thus, the contribution of plasma protein binding to brain NSAID availability remains to be determined experimentally.
In the present study, we examined the roles of BBB permeability, saturable transport, and plasma protein binding in the initial passage of NSAIDs into the brain. Three nonselective NSAIDs, ibuprofen, flurbiprofen, and indomethacin, which have been linked to central nervous system (CNS) AD protection in vitro and in vivo, were studied. Brain NSAID uptake was measured using the in situ rat brain perfusion technique (16), which allows ready control of perfusion fluid composition (e.g., concentrations of drug, plasma protein, and transport inhibitors) and accurately measures brain uptake over a 104 range.
Methods
Chemicals
R,S-[carboxyl-14C]Ibuprofen (55 mCi mmol−1), [3H(G)] flurbiprofen (400 mCi mmol−1), [N-methyl-3H]diazepam (85 Ci mmol−1), [methoxy-14C]inulin (3.75 mCi g−1), and [methoxy-3H]minulin (2.25 mCi g−1) were purchased from American Radiolabeled Chemicals Inc. (St. Louis, MO, USA). [14C]Diazepam (56 mCi mmol−1) was obtained from Amersham Biosciences (Piscataway, NJ, USA). [2-14C]Indomethacin (20 mCi mmol−1) was procured from PerkinElmer Life Sciences (Boston, MA, USA). NSAID radiochemical purity was confirmed by reverse-phase high-performance liquid chromatography (HPLC) using a C18 column and acetonitrile/1% aqueous acetic acid mobile phase. Unlabeled ibuprofen, indomethacin, flurbiprofen, digoxin, probenecid, pyruvic acid, valproate, and bovine albumin (fraction V, A3059, γ-globulin free) were purchased from Sigma-Aldrich (St. Louis, MO, USA).
Brain Perfusion Method
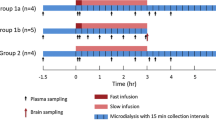
Brain NSAID uptake was measured using the in situ rat brain perfusion technique (16,17). Adult male rats (Sprague–Dawley strain, 250–350 g) obtained from Charles River Laboratories (Wilmington, MA, USA) were anesthetized with sodium pentobarbital (Nembutal, 40 mg kg−1 i.p., Abbott Laboratories, North Chicago, IL, USA). The neck region was shaved, and a ventral midline incision was made in the skin. The left common carotid artery was gently exposed and catheterized with PE-60 tubing filled with heparinized 0.9% NaCl (100 U mL−1). The left external carotid artery was ligated with surgical silk, but the pterygopalatine artery was left open (17). Body temperature was maintained at 37°C using a heating pad linked to a YSI Indicating Controller (Yellow Springs Instruments, Yellow Springs, OH, USA). The catheter was attached to a four-way stopcock connected to a dual-syringe Harvard infusion pump (Harvard Bioscience, South Natick, MA, USA). Both syringes of the infusion pump were filled with bicarbonate-buffered physiologic saline containing 128 mM NaCl, 24 mM NaHCO3, 4.2 mM KCl, 2.4 mM NaH2PO4, 1.5 mM CaCl2, 0.9 mM MgSO4, and 9 mM d-glucose (17). The perfusion fluid was oxygenated with 95% O2–5% CO2 and maintained at 37°C using a heating coil. In some experiments, unlabeled NSAID (1–20 mM), transport competitor (e.g., probenecid, digoxin, pyruvate, or valproate), or albumin (0.027, 0.27, or 2.7 g per 100 mL) was added to the perfusate. The perfusion fluid in the second syringe was identical to the first with the exception that it contained 3H- or 14C-labeled NSAID (0.01–0.8 μCi mL−1), diazepam, or inulin. Radiolabeled diazepam was used to measure cerebral perfusion fluid flow rate, whereas brain vascular volume was quantitated using labeled inulin (16,17). Most experiments were of dual-label type (3H/14C), with one tracer used for NSAID and the other for either vascular volume or flow. Perfusate tracer concentrations were chosen to maintain tissue 3H/14C disintegrations per minute (dpm) ratios of >3:1 for accurate counting statistics.
To start the perfusion, the heart was severed (2–3 s), and then tracer-free fluid was infused into the common carotid artery for 30 s at a rate of 5 or 20 mL min−1. After 30 s of tracer-free perfusion, the perfusion fluid was switched using the four-way valve to matching fluid containing radiolabeled NSAID and either the flow or vascular volume marker. After 10–30 s of tracer perfusion, the animal was decapitated and the pump was turned off. The left brain was dissected into different regions and the samples were weighed. In addition, duplicate samples of perfusion fluid were obtained. Samples were digested overnight at 55°C in 1 mL of Solvable tissue solubilizer (Packard, Meriden, CT, USA). The following morning, 10 mL Scintisafe™ 30% scintillation cocktail (Fischer Scientific, Fair Lawn, NJ, USA) was added and the samples were assayed for radioactivity by dual-label liquid scintillation counting (LSC; Beckman LS 6500, Fullerton, CA, USA). Counts per minute were converted to dpm after appropriate correction for background, quench, spillover, and efficiency.
Plasma Protein Binding
The unbound fraction of radiolabeled NSAID in perfusion fluid was measured by ultrafiltration and equilibrium dialysis. Ultrafiltration was performed using a Microcon centrifugal filter device (10-kDa MW cutoff, Amicon Bioseperations, Bedford, MA, USA). Briefly, perfusate fluid collected immediately at the end of perfusion (0.5 mL) was placed in an ultrafiltration tube and spun at 4000 rpm at 37°C for 7 min under 95% O2 and 5% CO2. Conditions were set so that the temperature was maintained at 37°C and only 10–15% of perfusion fluid sample was filtered. Tracer NSAID concentration in the initial fluid as well as filtrate and retentate was measured using LSC. Matching protein-free perfusion samples were also run to correct for binding of drug to filter membrane.
Equilibrium dialysis was performed at 37°C using acrylic equilibrium dialysis cells (1 mL) with a dialysis membrane MW cutoff of 6 kDa (Bel-Art Products, Pequannock, NJ, USA). The equilibration time for free drug (∼4 h) was determined for each agent tested. At the end of the dialysis period, samples were collected from both chambers (protein containing and protein free) and concentrations were determined by LSC.
Distribution Coefficient
The octanol–water distribution coefficient (Doct 7.4) was measured using the shake flask technique. Briefly, radiolabeled NSAID was dissolved in 0.5 mL phosphate buffer (0.1 M, pH 7.4) to which an equal volume of water-saturated n-octanol was added. The mixture was vortexed for 1 min and then allowed to separate into two phases. Aliquots were sampled from each phase and analyzed via LSC for tracer NSAID concentration.
Calculations
Unidirectional transfer constants (K in) for initial brain uptake of [14C]ibuprofen, [3H]flurbiprofen, and [14C] indomethacin were calculated as previously described (16,18):
where Q*tot is the measured quantity of radiolabeled NSAID in the brain (vascular and extravascular) at the end of the perfusion (disintegrations per minute per gram), V v is the cerebral vascular volume measured using radiolabeled inulin (milliliters per gram), C*tot is the total perfusate concentration of radiolabeled NSAID (disintegrations per minute per milliliter), and T is the net perfusion time. In Eq. (1), Q*tot was corrected for residual vascular tracer (V v C*tot) to obtain the quantity of labeled NSAID tracer that was predicted to have crossed the BBB (Q*br = Q*tot − V v × C*tot). Equation (1) assumes that uptake is linear with time and that metabolic loss is negligible. Linearity was confirmed by examining the initial time course (0–30 s) of NSAID uptake into brain. V v was calculated as the brain-to-perfusion fluid ratio of labeled inulin(16).
For a number of solutes that do not bind appreciably to plasma proteins, K in has been shown to depend on cerebral perfusion fluid flow (F, milliliters per second per gram) and the apparent BBB permeability–surface area product (PSu) as given by the Kety-Crone-Renkin equation (18):
For solutes that bind reversibly and rapidly to plasma proteins, Eq. (2) has been adapted as follows, assuming that bound and free drug are in equilibrium at all points in the fluid as it transits the cerebral capillary (19):
where f u is the free fraction of drug in the saline perfusion fluid or plasma.
PSu was determined for each NSAID from measured K in, F, and f u by rearranging Eqs. (2) and (3) as
where F was determined from brain uptake of [3H]diazepam or [14C]diazepam in the absence of albumin (16).
The concentration dependence of ibuprofen uptake into the brain was analyzed with a model containing a saturable and a nonsaturable component as,
where V max and K m, respectively, are the maximal transport rate (nanomoles per second per gram) and half saturation constant (millimolar) of the saturable component and K d is the coefficient of nonsaturable transfer (milliliters per second per gram).
Statistics
All the values are means ± SEM unless otherwise noted. One-way analysis of variance (ANOVA) was used to determine statistical significance with either Dunnet's or Tukey's post hoc test for multiple comparisons (Prism 4, GraphPad Software, San Diego, CA, USA). Regression analysis was also performed using Prism.
Results
Time Course of Brain Uptake of NSAIDs from Protein-Free Saline
Figure 1 illustrates the time course of [14C]ibuprofen, [3H]flurbiprofen, and [14C]indomethacin uptake into the brain (i.e., left cerebral hemisphere) at tracer concentration during perfusion with protein-free bicarbonate-buffered saline (20 mL min−1 infusion rate). Uptake was linear for each NSAID from 10 to 30 s with a y-axis intercept that did not differ significantly (p>0.05) from zero after vascular correction using labeled inulin. Best-fit BBB K in obtained from linear regression equaled (2.31±0.07)×10−2, (1.41± 0.08)×10−2, and (0.60±0.02)×10−2 mL s−1 g−1, respectively, for [14C]ibuprofen, [3H]flurbiprofen, and [14C]indomethacin. Based upon these data, a 30-s uptake time was used in all subsequent experiments. Brain V v equaled (0.66±0.04)×10−2 mL g−1 with inulin, comparable to values in previous reports (16).
Time profile of brain (A) [14C]ibuprofen (♦), (B) [3H]flurbiprofen (⋄), and (C) [14C]indomethacin (○) uptake during perfusion with protein-free saline. Data represent mean ± SEM (n = 3–5) values of average brain samples collected after brain perfusion. Measured brain NSAID radioactivity (disintegrations per minute per gram) was corrected for residual vascular tracer by subtracting the product of the inulin vascular volume (milliliters per gram) and perfusate NSAID concentration (disintegrations per minute per milliliter). Perfusate NSAID concentration equaled 0.54, 0.15, and 2.5 μM for [14C]ibuprofen, [3H]flurbiprofen, and [14C]indomethacin, respectively.
Regional Brain Uptake of NSAIDs
Dissection of the perfused left cerebral hemisphere into eight separate areas demonstrated minimal regional differences in BBB drug transport (Fig. 2). Calculated BBB PSu in different brain regions varied by only 10–30% among regions with the highest values in the frontal and parietal cerebral cortex and the lowest values in the hippocampus or midbrain colliculus. F followed a similar pattern but was significantly lower (40–60%) in the cerebellum, which gets most of its flow from the basilar artery and is not perfused well with the carotid artery in situ brain perfusion technique (16,17). Therefore, the cerebellum was not included in subsequent analyses, and data were presented as a pooled left cerebral hemisphere value excluding cerebellum.
Rapid Uptake of Free NSAIDs from Saline
BBB PSu, calculated from F and K in at the 20-mL min−1 infusion rate using Eq. (2), equaled (2.63±0.10)×10−2 (ibuprofen), (1.60±0.12) × 10−2 (flurbiprofen), and (0.64± 0.05)×10−2 mL s−1 g−1 (indomethacin). Experiments demonstrated that BBB PSu differed by <8% (p>0.05) between carotid artery infusion rates of 5 and 20 mL min−1, which provided cerebral perfusion fluid flows (F) of (2.8 ± 0.2)×10−2 mL s−1 g−1 (n = 11) and (9.8 ± 0.8) × 10−2 mL s−1 g−1 (n = 9), respectively. Given that F at the 5-mL min−1 infusion rate more closely matches normal cerebral blood flow [(1.6–3.3) × 10−2 mL s−1 g−1; (16)], the 5-mL min−1 infusion rate was used in most subsequent experiments.
Figure 3 illustrates the plot of BBB log PSu vs. log D oct7.4 for the three NSAIDs expressed relative to established markers of BBB PSu (18). Consistent with the high NSAID PSu values, the log PSu values for the three NSAIDs fall in the upper right-hand corner of the graph. The NSAID log PSu values are ∼2 log units greater than those associated with low BBB permeability (log PSu < −4) and suggest that the free NSAIDs rapidly cross the BBB at physiologic pH. The measured NSAID log PSu values, however, fell slightly under those predicted by the measured log D oct7.4 and the empirical relation obtained for the BBB permeability markers (Fig. 3). The difference was ∼1 log unit low for ibuprofen and flurbiprofen and 2 log units low for indomethacin. Measured log D oct 7.4 equaled 1.09 ± 0.05 (ibuprofen), 0.92 ± 07 (flurbiprofen), and 1.17 ± 0.06 (indomethacin).
Relationship of BBB log PSu vs. log D oct 7.4 for [14C]ibuprofen (♦), [3H]flurbiprofen (▴), and [14C]indomethacin (•) in comparison with those of established values of permeating compounds (□) (18). Values represent means for at least three determinations.
Brain Uptake in the Presence of Inhibitory Transport Substrates
To evaluate the relative contribution of carrier-mediated transport to brain NSAID uptake, BBB PSu to each tracer NSAID was determined in the presence of elevated concentrations of matching unlabeled NSAID (Fig. 4). Brain [14C]ibuprofen PSu fell by 60% (p < 0.01) as perfusate unlabeled ibuprofen concentration was raised to 20 mM, demonstrating self-saturation. Best-fit kinetic parameters using a model with one Michaelis-Menten saturable and one nonsaturable component equaled V max = 13.5 ± 0.4 nmol s−1 g−1, K m = 0.85 ± 0.02 mM, and K d = (9.36 ± 0.05) × 10−3 mL s−1 g−1 (r 2 = 0.9998) for ibuprofen transport across BBB. Addition of anion transport competitors, such as 100 μM digoxin, 10 mM probenecid, 20 mM valproate, or 20 mM pyruvate, did not significantly lower BBB [14C]ibuprofen PSu. However, 10 mM indomethacin reduced brain [14C]ibuprofen uptake by 42% (p < 0.05), suggesting that brain ibuprofen uptake was mediated in part by a saturable system that was inhibited by indomethacin.
Concentration dependence and effect of unlabeled transport substrates/inhibitors. (A) [14C]Ibuprofen, (B) [3H]flurbiprofen, and (C) [14C]indomethacin. Control represents uptake of radiolabeled NSAID in the absence of unlabeled compound. Values represent mean ± SEM (n = 3–5). *Differs significantly from matching control (p < 0.05 by one-way ANOVA and Dunnett's multiple comparison). The highest concentration of unlabeled flurbiprofen tested due to solubility limitations was 1 mM.
In contrast, brain uptake of [3H]flurbiprofen and [14C]indomethacin showed no evidence for self-saturation over the concentrations tested and did not show cross-inhibition with 20 mM ibuprofen (Fig. 4). Thus, the carrier system may be selective for ibuprofen. No regional difference was observed in PSu response in the self-saturation and competitor experiments, such that the pooled brain hemisphere value represented the pattern for all sampled brain regions.
Because the NSAIDs and transport inhibitors at elevated concentrations may alter brain vascular responsivity or BBB integrity, brain F and V v were also measured in these experiments. Table I summarizes the obtained values. F and V v did not differ significantly from control for any of the groups, suggesting that BBB integrity and F were maintained throughout the experiments.
Influence of Plasma Protein Binding on Brain Uptake of NSAIDs
All three NSAIDs that were examined bind highly to albumin. Therefore, the influence of plasma protein binding on brain uptake K in and PSu was also assessed. Figure 5 illustrates the effect of 0.027, 0.27, or 2.7% bovine serum albumin (BSA) on brain uptake K in of [14C]ibuprofen. Perfusate albumin levels roughly matched 1, 10, and 100% of those in serum, as the normal rat plasma level of albumin is 2.5–3.0 mg dL−1 (%) (20). For these experiments, F equaled (2.4 ± 0.2) × 10−2 mL s−1 g−1 (n = 9) and matched that in the normal rat (21). As shown in Fig. 5, unidirectional K in for [14C]ibuprofen decreased sharply by >20-fold with increasing albumin concentration. Comparable reductions were noted in perfusate [14C]ibuprofen f u. Albumin did not affect calculated BBB [14C]ibuprofen PSu (p>0.05). Measured [14C]ibuprofen K in in the presence of albumin matched that predicted from perfusate f u and F and the separate PSu measured in the absence of protein (± 10%). A comparable pattern was seen for [3H]flurbiprofen (Fig. 6) and [14C]indomethacin (Fig. 7). The influence of plasma protein binding was pronounced, decreasing brain uptake of [14C]ibuprofen and [3H]flurbiprofen at the 2.7 and 0.27% albumin concentration by >95 and 92%, respectively. Thus, in addition to BBB transport, plasma protein binding critically influences BBB NSAID K in.
Effect of BSA (0.027–2.7%) on brain K in, perfusate f u, and BBB PSu to [14C]ibuprofen (tracer concentration). (A) K in measured (□) and predicted (▴). (B) Free fraction measured (□) and predicted (▴). (C) BBB PSu calculated from the measured K in corrected for F and f u using Eq. (3). Values represent mean ± SEM (n = 3–5). Infusion rate = 5 mL min−1. All K in and f u values measured in the presence of albumin differed significantly (p < 0.01) from matching controls (no albumin).
Effect of BSA (0.027–2.7%) on brain K in, perfusate f u, and BBB PSu to [3H]flurbiprofen (tracer concentration). (A) K in measured (□) and predicted (▴). (B) Free fraction measured (□) and predicted (▴). (C) BBB PSu calculated from the measured K in corrected for F and f u using Eq. (3). Values represent mean ± SEM (n = 3–5). Infusion rate = 5 mL min−1. All K in and f u values measured in the presence of albumin differed significantly (p < 0.01) from matching controls (no albumin).
Effect of BSA (0.027–2.7%) on brain K in, perfusate f u, and BBB PSu to [14C]indomethacin (tracer concentration). (A) K in measured (□) and predicted (▴). (B) Free fraction measured (□) and predicted (▴). (C) BBB PSu calculated from the measured K in corrected for F and f u using Eq. (3). Values represent mean ± SEM (n = 3–5). Infusion rate = 5 mL min−1. All K in and f u values measured in the presence of albumin differed significantly (p < 0.01) from matching controls (no albumin).
Discussion
The present study demonstrates that the NSAIDs ibuprofen, flurbiprofen, and indomethacin readily cross the BBB with cerebrovascular PSu values approaching or exceeding that of rapidly penetrating solutes, such as [3H]water and [14C]antipyrine (18,21). No evidence was found for saturable brain uptake of flurbiprofen and indomethacin over the concentration range tested. In contrast, BBB ibuprofen transport was in part saturable with a K m of 0.85 mM, a V max of 13.5 nmol s−1 g−1, and a K d of 9.3 × 10−3 mL s−1 g−1. Brain ibuprofen uptake was inhibited by indomethacin but not by pyruvate, probenecid, valproate, or digoxin. This suggests that at least part of BBB ibuprofen uptake is carrier mediated. Furthermore, plasma protein binding was found to have a dramatic effect on brain uptake for all three NSAIDs. Measured NSAID K in followed that predicted using the modified Kety-Crone-Renkin equation with no significant change in PSu. The results suggest that brain distribution of ibuprofen, flurbiprofen, and indomethacin is limited in part by plasma protein binding, which reduces the plasma free fraction in vivo by >90%.
BBB drug penetration has long been known to be strongly influenced by solute lipophilicity (16,21). In addition, the presence of charge (22), ionization, and hydrogen bonding have also been shown to have significant effects (10). Ibuprofen, flurbiprofen, and indomethacin are fairly lipophilic and thus might be expected to show good brain uptake. Most NSAIDs meet the five simple rules of thumb outlined by Clark (8) for good probability of entering brain. As shown in this study, their BBB PSu for brain NSAID uptake is actually quite high and approximates that predicted by the log D oct 7.4. The fact that the values fall slightly below those predicted for passive diffusion may hint at an active efflux process. In support of this, Fukuda et al. (23) reported that probenecid increased brain-to-plasma concentration ratio of two NSAIDs, diclofenac and mefenamic acid, suggesting an active efflux process. The dislocation between steady-state brain–plasma concentration ratios for NSAIDs (0.01–0.08) and their appreciable BBB PSu values, as reported here, highlights the fact that multiple parameters impact drug uptake and distribution into the brain beyond simple BBB permeability. For these NSAIDs, something additional is going on that appreciably limits brain NSAID distribution in vivo. This can include active efflux transport, poor brain distribution volume, rapid brain drug metabolism, and/or plasma protein binding.
NSAIDs are known to interact with a number of transport carriers (12,24,25). The demonstration of a saturable component of [14C]ibuprofen uptake into the brain with a K m of 0.85 mM suggests that one or more carriers may facilitate ibuprofen influx into the brain at the BBB. Brain capillaries have been shown to express a number of transporters that accept organic anions (11). The fact that brain [14C]ibuprofen uptake was not inhibited by pyruvate, probenecid, or digoxin casts doubt on the contributions of BBB monocarboxylate transporter 1 (MCT1) (pyruvate), organic anion transporter 3 (OAT3) (probenecid), organic anion transporting polypeptides (oatp) 1a4, 1a5, or 1c1 (probenecid and/or digoxin), and multidrug resistance protein (MRP), 4, or 5 (probenecid) (24,26). Ibuprofen and salicylic acid have been shown to inhibit MCT1 (27,28). However, it is possible that ibuprofen is too large to be an appreciable substrate for that transporter. OAT3 and members of the MRP family transport solutes out of the brain, and therefore their contributions to saturable influx would be expected to be small. Several members of the oatp family mediate bidirectional transport of organic solutes at the BBB (11). Ibuprofen and indomethacin inhibit rat oatp2 with K i values of ∼1.3 and 0.17 mM, respectively (12). However, the absence of BBB [14C]ibuprofen uptake inhibition by either digoxin or probenecid, which are known inhibitors of oatp 1a4 (11), and the fact that indomethacin had a weaker inhibitory effect on brain [14C]ibuprofen uptake than ibuprofen, contrary to their oatp 1a4 K i values, argue against the role of oatp 1a4 in brain [14C]ibuprofen influx. Similarly, probenecid has been shown to inhibit oatp 1a5 and 1c1 (29,30). The fact that 20 mM valproate did not significantly reduce brain [14C]ibuprofen PSu suggests that the saturable ibuprofen carrier is not mediated by the BBB valproate transporter (31). Thus, brain ibuprofen uptake may be mediated by an as yet unidentified BBB carrier, or it may be that multiple transport mechanisms contribute and determinations at single concentrations with a few inhibitors are not adequate to unravel the roles of influx and efflux components. In contrast, neither [3H]flurbiprofen nor [14C]indomethacin exhibited clear evidence of a saturable component over the range tested.
Most acidic NSAIDs bind tightly to plasma albumin (Sudlow site II), decreasing the available free fraction in plasma for brain uptake (20). Conventionally, free drug has been thought to be the driving force for the drug uptake into tissues. However, many studies have found that in the presence of plasma protein, the net exchangeable fraction of drug in the brain capillaries markedly exceeds that measured in vitro even when correction for exchange between bound and free drug (Eq. 3) is incorporated (15,32). Our results suggest that brain influx for ibuprofen, flurbiprofen, and indomethacin correlated well with the measured free drug fraction with no evidence for a significant contribution of induced or enhanced dissociation. Upon addition of albumin to the perfusion fluid, brain NSAID uptake K in fell in accordance to the decrease in measured free fraction. This result is consistent with studies showing good agreement between plasma unbound concentration and CSF or brain drug concentrations (33).
Plasma protein binding plays a major role in restricting brain uptake of NSAIDs, reducing K in by more than 10-fold from PSu. Prior to this study, this concept had not been clearly elucidated. In fact, in several initial studies of CSF and brain NSAID uptake, plasma protein binding was noted to have a minor role (7,34) and the BBB permeability of NSAIDs was reported to be quite low (35,36). Many studies have concluded that CNS uptake of most nonselective NSAIDs is quite limited. However, the exact mechanisms limiting CNS NSAID uptake were unclear. Given the role that plasma protein plays in unidirectional brain NSAID uptake, it may be possible to transiently increase brain NSAID delivery via administration of a plasma protein binding inhibitor, as proposed by Haradahira et al. (37) for a radioligand. However, such an approach would not be expected to appreciably change brain exposure with long-term administration.
There is a widespread interest in NSAIDs regarding the role of COX in CNS disorders. Many traditional acidic NSAIDs show poor delivery to brain based on low brain-to-plasma ratios and plasma protein binding. In contrast, several neutral NSAIDs, including acetaminophen, antipyrine, and the newer COX-2 inhibitors, show markedly improved CNS distribution. The newer neuroprotective effects recently ascribed to a subset of nonselective NSAIDs, including ibuprofen, indomethacin, and flurbiprofen, and not seen with better penetrating COX-2 or nonselective analogs, suggest that improved brain delivery may be of interest for these poorly distributing NSAIDs to enhance CNS activity and reduce peripheral toxicity (2,4,5). Brain drug delivery in AD is complicated by a number of alterations in the BBB and CSF system leading to decrease in CSF production rate, enhanced CSF volume, and altered expression and function of transporters (38,39). Our results suggest that at least one NSAID, ibuprofen, may be taken up into the brain by a saturable carrier that is sensitive to indomethacin. Design of NSAIDs with less plasma protein binding, less efflux transport, enhanced cellular uptake, and greater free drug distribution to brain may aid in CNS efficacy.
Abbreviations
- BBB:
-
blood–brain barrier
- COX:
-
cyclooxygenase
- F :
-
perfusion fluid flow
- f u :
-
free fraction
- K in :
-
transfer constant for unidirectional uptake
- K m :
-
half saturation constant
- NSAIDs:
-
nonsteroidal anti-inflammatory drugs
- PSu :
-
permeability–surface area product
- V max :
-
maximal transport rate of saturable component
- V v :
-
vascular volume
References
B. A. in t'Veld A. Ruitenberg A. Hofman L. J. Launer C. M. Duijn Particlevan T. Stijnen M. M. Breteler B. H. Stricker (2001) ArticleTitleNon-steroidal antiinflammatory drugs and the risk of Alzheimer's disease N. Engl. J. Med. 345 1515–1521 Occurrence Handle10.1056/NEJMoa010178
L. Gasparini E. Ongini G. Wenk (2004) ArticleTitleNon-steroidal anti-inflammatory drugs (NSAIDs) in Alzheimer's disease: old and new mechanisms of action J. Neurochem. 91 521–536 Occurrence Handle15485484 Occurrence Handle1:CAS:528:DC%2BD2cXpsFelsLo%3D Occurrence Handle10.1111/j.1471-4159.2004.02743.x
S. Weggen J. L. Eriksen S. A. Sagi C. U. Pietrzik V. Ozols A. Fauq T. E. Golde E. H. Koo (2003) ArticleTitleEvidence that nonsteroidal anti-inflammatory drugs decrease amyloid beta 42 production by direct modulation of gamma-secretase activity J. Biol. Chem. 278 31831–31837 Occurrence Handle12805356 Occurrence Handle1:CAS:528:DC%2BD3sXmsVOntbY%3D Occurrence Handle10.1074/jbc.M303592200
J. L. Eriksen S. A. Sagi T. E. Smith S. Weggen P. Das D. C. McLendon V. V. Ozols K. W. Jessing K. H. Zavitz E. H. Koo T. E. Golde (2003) ArticleTitleNSAIDs and enantiomers of flurbiprofen target gamma-secretase and lower Abeta 42 in vivo J. Clin. Invest. 112 440–449 Occurrence Handle12897211 Occurrence Handle1:CAS:528:DC%2BD3sXmtFemtrY%3D Occurrence Handle10.1172/JCI200318162
A. Mannila J. Rautio M. Lehtonen T. Jarvinen J. Savolainen (2005) ArticleTitleInefficient central nervous system delivery limits the use of ibuprofen in neurodegenerative diseases Eur. J. Pharm. Sci. 24 101–105 Occurrence Handle15626583 Occurrence Handle1:CAS:528:DC%2BD2MXjtlCh Occurrence Handle10.1016/j.ejps.2004.10.004
B. Bannwarth F. Lapicque F. Pehourcq P. Gillet T. Schaeverbeke C. Laborde J. Dehais A. Gaucher P. Netter (1995) ArticleTitleStereoselective disposition of ibuprofen enantiomers in human cerebrospinal fluid Br. J. Clin. Pharmacol. 40 266–269 Occurrence Handle8527289 Occurrence Handle1:CAS:528:DyaK2MXosl2ltr8%3D
M. Matoga F. Pehourcq F. Lagrange G. Tramu B. Bannwarth (1999) ArticleTitleInfluence of molecular lipophilicity on the diffusion of arylpropionate non-steroidal anti-inflammatory drugs into the cerebrospinal fluid Arzneim.-Forsch. 49 477–482 Occurrence Handle1:CAS:528:DyaK1MXktF2ksrg%3D
D. E. Clark (2003) ArticleTitle In silico prediction of blood–brain barrier permeation Drug Discov. Today 8 927–933 Occurrence Handle14554156 Occurrence Handle1:CAS:528:DC%2BD3sXnvFSiu70%3D Occurrence Handle10.1016/S1359-6446(03)02827-7
D. J. Begley M. W. Brightman (2003) ArticleTitleStructural and functional aspects of the blood–brain barrier Prog. Drug Res. 61 39–78 Occurrence Handle14674608 Occurrence Handle1:CAS:528:DC%2BD3sXpvFert7c%3D
M. D. Habgood D. J. Begley N. J. Abbott (2000) ArticleTitleDeterminants of passive drug entry into the central nervous system Cell. Mol. Neurobiol. 20 231–253 Occurrence Handle10696512 Occurrence Handle1:STN:280:DC%2BD3c7mtFGjsA%3D%3D Occurrence Handle10.1023/A:1007001923498
H. Kusuhara Y. Sugiyama (2005) ArticleTitleActive efflux across the blood–brain barrier: Role of the solute carrier family NeuroRx 2 73–85 Occurrence Handle15717059 Occurrence Handle10.1602/neurorx.2.1.73
Y. Shitara D. Sugiyama H. Kusuhara Y. Kato T. Abe P. J. Meier T. Itoh Y. Sugiyama (2002) ArticleTitleComparative inhibitory effects of different compounds on rat oatpl (slc21a1)- and Oatp2 (Slc21a5)-mediated transport Pharm. Res. 19 147–153 Occurrence Handle11883641 Occurrence Handle1:CAS:528:DC%2BD38XitVSmu7Y%3D Occurrence Handle10.1023/A:1014264614637
Y. Nozaki H. Kusuhara H. Endou Y. Sugiyama (2004) ArticleTitleQuantitative evaluation of the drug–drug interactions between methotrexate and nonsteroidal anti-inflammatory drugs in the renal uptake process based on the contribution of organic anion transporters and reduced folate carrier J. Pharmacol. Exp. Ther. 309 226–234 Occurrence Handle14722319 Occurrence Handle1:CAS:528:DC%2BD2cXivFamtLg%3D Occurrence Handle10.1124/jpet.103.061812
N. M. Davies N. M. Skjodt (2000) ArticleTitleChoosing the right nonsteroidal anti-inflammatory drug for the right patient: a pharmacokinetic approach Clin. Pharmacokinet. 38 377–392 Occurrence Handle10843458 Occurrence Handle1:CAS:528:DC%2BD3cXktFGqsLk%3D Occurrence Handle10.2165/00003088-200038050-00001
H. Tanaka K. Mizojiri (1999) ArticleTitleDrug–protein binding and blood–brain barrier permeability J. Pharmacol. Exp. Ther. 288 912–918 Occurrence Handle10027826 Occurrence Handle1:CAS:528:DyaK1MXhs1Kjtbo%3D
Y. Takasato S. I. Rapoport Q. R. Smith (1984) ArticleTitleAn in situ brain perfusion technique to study cerebrovascular transport in the rat Am. J. Physiol. 247 H484–H493 Occurrence Handle6476141 Occurrence Handle1:CAS:528:DyaL2cXmtVOis7g%3D
Q. R. Smith (1996) ArticleTitleBrain perfusion systems for studies of drug uptake and metabolism in the central nervous system Pharm. Biotechnol. 8 285–307 Occurrence Handle8791815 Occurrence Handle1:CAS:528:DyaK2sXosVWjtg%3D%3D
Q. R. Smith (2003) ArticleTitleA review of blood–brain barrier transport techniques Methods Mol. Med. 89 193–208 Occurrence Handle12958421 Occurrence Handle1:CAS:528:DC%2BD3sXntlKnsbo%3D
D. J. Morgan J. L. Huang (1993) ArticleTitleEffect of plasma protein binding on kinetics of capillary uptake and efflux Pharm. Res. 10 300–304 Occurrence Handle8456081 Occurrence Handle1:CAS:528:DyaK3sXhs1SmsLk%3D Occurrence Handle10.1023/A:1018959415963
T. J. Peters (1996) All About Albumin Academic Press, Inc. San Diego, CA
S. I. Rapoport K. Ohno K. D. Pettigrew (1979) ArticleTitleDrug entry into the brain Brain Res. 172 354–359 Occurrence Handle466480 Occurrence Handle1:CAS:528:DyaE1MXls1yitb4%3D Occurrence Handle10.1016/0006-8993(79)90546-8
W. H. Oldendorf B. E. Stoller F. L. Harris (1993) ArticleTitleBlood–brain barrier penetration abolished by N-methyl quaternization of nicotine Proc. Natl. Acad. Sci. USA 90 307–311 Occurrence Handle8419935 Occurrence Handle1:STN:280:ByyC38njs1E%3D
M. Fukuda K. Kitaichi F. Abe Y. Fujimoto K. Takagi T. Morishima T. Hasegawa (2005) ArticleTitleAltered brain penetration of diclofenac and mefenamic acid, but not acetaminophen, in Shiga-like toxin II-treated mice J. Pharmacol. Sci. 97 525–532 Occurrence Handle15821337 Occurrence Handle1:CAS:528:DC%2BD2MXjslGgsbY%3D Occurrence Handle10.1254/jphs.FP0040752
F. G. Russel R. Masereeuw R. A. Aubel Particlevan (2002) ArticleTitleMolecular aspects of renal anionic drug transport Annu. Rev. Physiol. 64 563–594 Occurrence Handle11826280 Occurrence Handle1:CAS:528:DC%2BD38XisFGmsbo%3D Occurrence Handle10.1146/annurev.physiol.64.081501.155913
S. Ohtsuki T. Kikkawa S. Mori S. Hori H. Takanaga M. Otagiri T. Terasaki (2004) ArticleTitleMouse reduced in osteosclerosis transporter functions as an organic anion transporter 3 and is localized at abluminal membrane of blood–brain barrier J. Pharmacol. Exp. Ther. 309 1273–1281 Occurrence Handle14762099 Occurrence Handle1:CAS:528:DC%2BD2cXksFCntbo%3D Occurrence Handle10.1124/jpet.103.063370
B. E. Enerson L. R. Drewes (2003) ArticleTitleMolecular features, regulation, and function of monocarboxylate transporters: implications for drug delivery J. Pharm. Sci. 92 1531–1544 Occurrence Handle12884241 Occurrence Handle1:CAS:528:DC%2BD3sXmtFeksbs%3D Occurrence Handle10.1002/jps.10389
I. Tamai H. Takanaga H. Maeda Y. Sai T. Ogihara H. Higashida A. Tsuji (1995) ArticleTitleParticipation of a proton-cotransporter, MCT1, in the intestinal transport of monocarboxylic acids Biochem. Biophys. Res. Commun. 214 482–489 Occurrence Handle7677755 Occurrence Handle1:CAS:528:DyaK2MXotV2hsbY%3D Occurrence Handle10.1006/bbrc.1995.2312
A. Tsuji (2005) ArticleTitleSmall molecular drug transfer across the blood–brain barrier via carrier-mediated transport systems NeuroRx 2 54–62 Occurrence Handle15717057 Occurrence Handle10.1602/neurorx.2.1.54
S. Ohtsuki T. Takizawa H. Takanaga N. Terasaki T. Kitazawa M. Sasaki T. Abe K. Hosoya T. Terasaki (2003) ArticleTitle In vitro study of the functional expression of organic anion transporting polypeptide 3 at rat choroid plexus epithelial cells and its involvement in the cerebrospinal fluid-to-blood transport of estrone-3-sulfate Mol. Pharmacol. 63 532–537 Occurrence Handle12606759 Occurrence Handle1:CAS:528:DC%2BD3sXitFyrs7c%3D Occurrence Handle10.1124/mol.63.3.532
K. Tohyama H. Kusuhara Y. Sugiyama (2004) ArticleTitleInvolvement of multispecific organic anion transporter, Oatp14 (Slc21a14), in the transport of thyroxine across the blood–brain barrier Endocrinology 145 4384–4391 Occurrence Handle15166123 Occurrence Handle1:CAS:528:DC%2BD2cXnt1Citb8%3D Occurrence Handle10.1210/en.2004-0058
K. D. Adkison D. D. Shen (1996) ArticleTitleUptake of valproic acid into rat brain is mediated by a medium-chain fatty acid transporter J. Pharmacol. Exp. Ther. 276 1189–1200 Occurrence Handle8786552 Occurrence Handle1:CAS:528:DyaK28XhslSgur8%3D
W. M. Pardridge (1998) Targeted delivery of hormones to tissues by plasma proteins P. M. conn (Eds) Handbook of Physiology Section 7: The Endocrine System Oxford University Press New York 335–382
M. Hammarlund-Udenaes L. K. Paalzow E. C. Lange Particlede (1997) ArticleTitleDrug equilibration across the blood–brain barrier—pharmacokinetic considerations based on the microdialysis method Pharm. Res. 14 128–134 Occurrence Handle9090698 Occurrence Handle1:CAS:528:DyaK2sXitFyrsbc%3D Occurrence Handle10.1023/A:1012080106490
B. Bannwarth P. Netter J. Pourel R. J. Royer A. Gaucher (1989) ArticleTitleClinical pharmacokinetics of nonsteroidal anti-inflammatory drugs in the cerebrospinal fluid Biomed. Pharmacother. 43 121–126 Occurrence Handle2660917 Occurrence Handle1:CAS:528:DyaL1MXktVSjsrY%3D Occurrence Handle10.1016/0753-3322(89)90140-6
Y. Deguchi H. Hayashi S. Fujii T. Naito Y. Yokoyama S. Yamada R. Kimura (2000) ArticleTitleImproved brain delivery of a nonsteroidal anti-inflammatory drug with a synthetic glyceride ester: a preliminary attempt at a CNS drug delivery system for the therapy of Alzheimer's disease J. Drug Target 8 371–381 Occurrence Handle11328663 Occurrence Handle1:CAS:528:DC%2BD3MXjtVOlsLc%3D Occurrence Handle10.3109/10611860008997913
X. Liu M. Tu R. S. Kelly C. Chen B. J. Smith (2004) ArticleTitleDevelopment of a computational approach to predict blood– brain barrier permeability Drug Metab. Dispos. 32 132–139 Occurrence Handle14709630 Occurrence Handle1:CAS:528:DC%2BD2cXnsFWqs7k%3D Occurrence Handle10.1124/dmd.32.1.132
T. Haradahira M. Zhang J. Maeda T. Okauchi K. Kawabe T. Kida K. Suzuki T. Suhara (2000) ArticleTitleA strategy for increasing the brain uptake of a radioligand in animals: use of a drug that inhibits plasma protein binding Nucl. Med. Biol. 27 357–360 Occurrence Handle10938470 Occurrence Handle1:CAS:528:DC%2BD3cXlsFCgtro%3D Occurrence Handle10.1016/S0969-8051(00)00096-2
C. Johanson P. McMillan R. Tavares A. Spangengerger J. Duncan G. Silverberg E. Stopa (2004) ArticleTitleHomeostatic capabilities of the choroids plexus epithelium in Alzheimer's disease Cerebrospinal Fluid Res. 1 1–16 Occurrence Handle10.1186/1743-8454-1-3 Occurrence Handle1:CAS:528:DC%2BD2MXjs1eltrs%3D
G. D. Silverberg G. Heit S. Huhn R. A. Jaffe S. D. Chang H. Bronte-Stewart E. Rubenstein K. Possin T. A. Saul (2001) ArticleTitleThe cerebrospinal fluid rate is reduced in dementia of the Alzheimer type Neurology 57 1763–1766 Occurrence Handle11723260 Occurrence Handle1:STN:280:DC%2BD3Mnnslehuw%3D%3D
Acknowledgment
This work was supported in part by grant NS052484 from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parepally, J.M.R., Mandula, H. & Smith, Q.R. Brain Uptake of Nonsteroidal Anti-Inflammatory Drugs: Ibuprofen, Flurbiprofen, and Indomethacin. Pharm Res 23, 873–881 (2006). https://doi.org/10.1007/s11095-006-9905-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-006-9905-5