Abstract
Purpose
To determine a relationship between adhesive and cohesive inter-particulate forces of interactions and in vitro performance in pressurised metered dose inhalers (pMDIs) suspension formulations.
Methods
Interparticulate forces of salbutamol sulphate (SS), budesonide (BUD) and formoterol fumarate dihydrate (FFD) were investigated by in situ atomic force microscopy (AFM) in a model propellant 2H, 3H perfluoropentane (HPFP). Experimental data were analysed using the recently developed cohesive/adhesive analysis method (CAB) and compared with in vitro deposition performances in pMDIs systems using Andersen cascade impactor (ACI).
Results
The in vitro investigation suggested that the micronised drug materials had significantly different aerosolisation profiles when manufactured as single or combination formulations. In general, the greatest significant differences were observed between SS single drug and SS-BUD and SS-FFD combinations. Analysis of the in vitro performance for the SS only formulation suggested that the cohesive nature of SS (as predicted by the CAB and observed with AFM) led to tightly bound flocs that did not fully deaggregate upon aerosolisation.
Conclusions
It is suggested that the relationship between interparticulate interactions and in vitro performance of pMDIs suspension systems, when compared to direct measurement of the adhesion/cohesion forces, indicated good correlation. This approach may be useful in expediting the development of pMDI formulation and predicting performance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma is a very common disease in Western countries affecting over 5% of adults and an even increasing number of children (1). The treatment of asthma by inhalation is a logical one, as the drug is delivered directly to the target organ, resulting in a rapid onset of action, lower dose when compared to the oral route, and a relative low incidence of side-effects (2). One method of inhalation delivery is by pressurised metered dose inhalers (pMDI).
Pressurised metered dose formulations consist of an active ingredient and one or more propellants. They may also contain additives, such as surfactants and co-solvents. The drug can either be homogeneously suspended or solubilised in a propellant (3). A well-formulated suspension should be physically and chemically stable and be readily redispersable after storage for prolonged periods. These criteria are particularly important as stability and uniformity are of utmost importance for safety and efficacy (4).
In a previous study (5), the authors investigated the relationship between atomic force microscopy (AFM) colloidal drug measurements and the interfacial behaviour of colloid particles used in pMDIs using a surface component approach (SCA) (5), derived from Fowkes, Good–Girifalco and van Oss (6–8).
In general, results indicated that direct measurements of interaction forces, using atomic force microscopy, responsible for the stability of colloid particles in pMDI formulations, were in direct correlation with the particles adhesive and cohesive tendencies. Furthermore, a relationship between the theoretical interfacial thermodynamics, derived from the SCA, and experimental force measurements were demonstrated (5).
The primary aim of this work was to combine in vitro drug delivery performance of three single and combination drug formulations with direct force measurement obtained using the AFM colloid probe technique reported previously (5) and analysed using the CAB analysis method (9). It is hoped that a greater understanding will be gained on the relationship between formulation performance and surface properties, which control particle–particle interactions in pMDIs.
There are numerous techniques available to evaluate lung deposition, including in vitro approaches. The Andersen cascade impactor (ACI) (10) is based on the assessment of the aerodynamic particle size and subsequent lung deposition of particles by inertial impaction. Based on the mass deposited on the different stages, an arbitrary division is made between ’respirable’ and ’non respirable’ fractions. Only fine particles (below approximately 5 μm) are thought to reach the lower airways. The relative ease of operation, the high power to detect differences and the relatively low variability in measurement makes in vitro impaction an attractive method in performance testing. The ACI is routinely used in the pharmaceutical industry for the evaluation of inhalation formulations and provides significant information during the development stage about deposition characteristic (11,12). In this study, using the ACI as the in vitro test of choice, the effects of adhesion and cohesion of three drug particulates (salbutamol sulphate, budesonide and formoterol fumarate dihydrate), formulated in single drug or combination drug pMDI suspension formulations, have been evaluated.
Materials and Methods
Materials
Micronised salbutamol sulphate, budesonide and formoterol fumarate dihydrate was supplied by AstraZeneca (R & D Charnwood, Loughborough, UK). The propellant 1,1,1, 2-tetrafluoroethane (Zephex 134a) was supplied by Ineos Fluor (Cheshire, UK). Metering valves (BK 357, nominal metered volume 50 μl) and actuator with orifice diameter of 0.3 mm were supplied by Bespack Europe Limited (Norfolk, UK). Cut edge pMDI aluminium cans (18 ml brim capacity) were supplied by Presspart (Lancashire, UK). Glass pMDI containers were supplied by Saint Gobain plc (London, UK). The aerosol formulations were pressure filled using a Pamasol Laboratory plant 02016 (Pamasol Willi Maäden AG, Pfaffikon, SZ).
The model propellant (HPFP, 2H, 3H perfluoropentane) was supplied by Apollo Scientific (Stockport, Derbyshire, UK). The purity of HPFP was in excess of 99.9%, with moisture content less than 9 ppm. All organic solvents used in the study were supplied by BDH (Poole, Dorset, UK) and were of analytical grade. Purified water was prepared by reverse osmosis (MilliQ, Molsheim, France).
Important Note Relating to Drug Names
Unless otherwise stated in the text, micronised salbutamol sulphate shall be designated as SS, budesonide as BUD and formoterol fumarate dihydrate as FFD.
Particle Size Measurement
Particle sizing of all drug samples were performed using a Malvern Mastersizer X (Malvern Instruments Ltd, Malvern, UK). The instrument was equipped with a small volume cell (with a capacity of approximately 20 ml) and a 100 mm lens, allowing particle detection in the size range of 0.5–120 μm. Cyclohexane was chosen as the dispersant. Approximately 10 mg of drug material was suspended in a 0.1% lecithin/cyclohexane solution and sonicated for 10 min at 25°C prior to each particle distribution analysis. Particle size distribution was characterised by the 10th, 50th and 90th percentile of the cumulative particle undersize frequency distribution. Results were collected in triplicate and corrected for reflective index using a built-in algorithm.
True Density Analysis
True density measurements were determined by helium pycnometry (Accupyc 1330 Gas Pycnometer, Micromeritics, Norcross, GA). Measurements were performed by measuring the pressure change of helium in a calibrated volume in relation to a known mass with unknown volume (13). Samples were prepared by drying in the pycnometer at 40°C for 24 h prior to analysis. The temperature was maintained at 27°C during out-gassing and analysis. Each sample was run ten times.
Preparation, Characterisation and Drug Crystal Morphology
As in the previous study (5), each crystal was heterogeneously nucleated and grown on a borosilicate glass substrate using a sitting drop technique, described elsewhere (14). This process produced planar crystals with large areas of sub-nanometre roughness. Prior to adhesion studies, the surface roughness on the dominant crystal face of each drug substrate was investigated. Root mean squared surface roughness (Rrms) analysis was conducted over 5 μm× 5 μm areas of each substrate (n = 25).
The general morphology of the drug crystals was investigated using optical microscopy, AFM tapping mode (in air) and computationally, via the use of a crystal shape prediction software. Optical photographs of each crystal were taken using a 200× long working distance microscope (Digital Instruments, Cambridge, UK) connected to CCD camera and associated software. The scale was determined by overlaying the image with a calibration grid (Digital Instruments, Cambridge, UK).
Predictive crystal morphology was conducted by inputting the crystal structure data, previously reported by others, for SS [Crystal system: monoclinic; Space group: Cc; Z = 8: a = 28.069 (5), b = 6.183 (1), c = 16.914 (2)], BUD [Crystal system: orthorhombic; Space group: P212121; Z = 4: a = 8.550 (1), b = 9.406 (1), c = 28.401 (3)] and FFD [Crystal system: triclinic; Space group: PĪ Z = 2: a = 6.737 (1), b = 10.384 (1), c = 16.571 (1)] (15–17), into SHAPE V 7.0 crystal computational software (Kingsport, USA ).
AFM Topographical, Colloidal Probe Measurements and Cohesion–Adhesion
Analysis of Drugs
The surface topography of drug crystal surfaces was investigated using the AFM in its conventional imaging Tapping Mode operation with a high-aspect-ratio silicon probe (OTESP, Digital Instruments, UK), at a scan rate of 0.7 Hz. Colloid probes were prepared by mounting an individual micronized drug particle (approximate diameter 5 μm) onto a V-shaped tipless cantilever (spring constant k = 0.32 N/m, DNP-020, DI, Cambridge, UK) using a quick-setting epoxy resin (18). The micromanipulation technique is described in detail elsewhere (19). The measurement of the forces of adhesion and cohesion between individual particles and their respective crystal surfaces were carried out with the in situ liquid AFM cell in purified HPFP (20,21). All AFM studies were performed using a commercially available Multi Mode AFM with a Nanoscope IIIa controller (Digital Instruments (DI), Cambridge, UK). The use of HPFP as a model system for studying the behaviour of pMDIs, has been extensively studied by Rogueda (22). AFM force distance measurements were performed according method described in Traini et al., (5) while the Cohesive/Adhesive balance (CAB) approach as described by Begat et al., (9).
Pressurised Metered Dose Inhalers Manufacture
Accurately, 25.0 mg of micronised drug material (12.5 mg of each drug for combination formulations) were weighted into aluminium canisters. Each canister was fitted with a 50 μl metering valve and crimped. 10 g of HFA134a was pressure filled into each canister. Calculated theoretical dose for each actuation was 125 μg. Cans were sonicated for 20 min and left to stabilise for 24 h at ambient temperature prior testing. All formulations manufactured for this study were produced under identical conditions.
To visually investigate the physical characteristics of the formulations, three glass containers with 25.0 mg of micronised single drug material SS, BUD and FFD and three containing the combination of micronised drugs (12.5 mg plus 12.5 mg) SS-BUD, SS-FFD and BUD-FFD were prepared, as described above. Containers were crimped with continuous valves and filled with 10 g of HFA 134a.
Suspension Sedimentation Behaviour
To evaluate the suspension properties, as with the aluminium containers, each of the glass containers was sonicated for 20 min and left to stand for at least 24 h before visual analysis.
Digital photographs were taken with a CCD 3 megapixel digital camera (Pentax, Slough, UK) to document any tendency of the suspension to cream, sediment or to detect adhesion/cohesion characteristics.
In Vitro Impaction Measurements
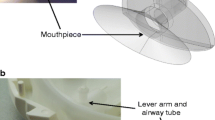
The influence of adhesion/cohesion on the aerosolisation of the micronised drug materials on in vitro performances was investigated using pharmacopoeia apparatus D, the Andersen cascade impactor [ACI, Copley Scientific, Nottingham, UK; (10)].
All experiments were conducted at ambient temperature and humidity (25°C/45% RH). The ACI is an eight stage cascade impactor designed for measuring the fine particle dose of aerosol clouds generated by pMDIs. Upon impaction, the aerosol is divided into seven size categories, according to its aerodynamic diameter. A pump (Model 1423-101Q-Q626X, GAST, Buckinghamshire, UK) generated a flow rate through the ACI of 28.3 L.min−1 (± 2 L.min−1), which was calibrated using a micromanometer (model FC012, Furness controls, Bexhill, UK) by adjustment of a needle valve flow regulator. For each analysis, the first five shots of each pMDI canister were shaken vigorously for 5 s and fired to waste. The manufactured pMDIs were inserted into a specially constructed mouthpiece and actuated in a fixed position into the throat of the cascade impactor for 10 s using the solenoid valve timer. A 3 s delay in activating the timer, after the pump was engaged, was invigilated to allow equilibrium of the pump. Ten consecutive doses (vigorous shaking in between each dose) for the single drug formulation and 20 for the combination formulation were released into the impactor.
The pMDI actuator, mouthpiece adaptor, throat assembly, stage zero to seven and filter stage were thoroughly rinsed into suitable volumetric flasks with dilution solvent [50:50 (V/V) CH3CN:H2O] and made up to the mark. The actuator and ACI components were then rinsed with distilled water followed by methanol, and dried at 40°C in an oven for 30 min. The ACI components were left to cool for 30 min, reassembled and re-used. For each single and combination drug formulations, ACI investigations were carried out in triplicate. All samples were analysed by high performance liquid chromatography (HPLC).
HPLC Assay
Simultaneous analyses of all the drug materials were performed using a reverse phase HPLC with the following settings: column oven temperature of 30°C, column flow rate of 1.75 ml/min, injection volume 100 μl, run time 6 mins and detector wavelength 248 nm. Samples elution times of: 2.42 min for BUD, 2.82 mins for SS and 4.68 mins for FFD were observed, respectively. The chromatographic system consisted of a deterctor (Jasco Model UV-970/975 Intelligent UV/VIS Detector) an autosampler (Jasco Model AS-950 Intelligent Auto-Sampler) a peristaltic pump (Jasco PU-90 Intelligent HPLC Pump) and a column oven (Jasco Model CO.965). Data were recorded and integrated using AZUR-OSIRIS Chromatography Software V 3.0 (Datalys, St Martin d’Hères, France).
Mobile phase was 50:50 (V/V) CH3CN: buffer. The buffer used in these studies was prepared by weighing 1.10 g of heptane sulphonic acid sodium salt into a 1 l volumetric flask which was diluted to volume with purified water and mixed well. The solution was adjusted to pH 3.0 using glacial acetic acid, using a calibrated pH meter (Activon, Model 209 pH/mV meter, Gladesville, NSW, Australia) and de-gassed prior to use. Dilution solvent, used throughout the study to recover drug deposits from the impactor and to dilute samples and standards was a 50:50 (V/V) CH3CN:H2O.
The amount of SS, BUD and FFD in the samples was established by means of a calibration curve prepared with the three drugs concomitantly present in the range of 0.1–10 μg.ml. The method was validated with regard to variability, recovery, linearity, detection limit and range, and proved to be suitable for this study. Each sample was analysed in duplicate. Graphical representations of calibration plots and chromatographs of SS, BUD and FFD mixed standards across low and high (0.1–10 μg.ml−1) concentration range are presented in Figs. 1, 2, 3, respectively.
Data Analysis
In the present study data are presented as cumulative particle undersize for various aereodynamic cut-offs (i.e., Stage 2-filter, Stage 3-filter etc).
The fine particle dose (FPD), defined as the amount of drug deposited on the stages below the stage with the cut-off diameter with the closest value to 5.0 μm, i.e., stage 2 to filter of the ACI. For each preparation the standard deviation (SD) was calculated. Emitted dose (ED) is presented as a percentage of the calculated emitted dose over the expected dose (125 μg).
Statistical Analysis
Data were subjected to analysis of variance (ANOVA) (Minitab 12.1, Minitab Ltd., Coventry, UK). Significant differences between formulations were analysed using multiple comparisons and p values of < 0.05 (Fisher Pair wise) were considered to be significant.
Results and Discussion
As previously discussed this study was conducted to investigate variation in particle deposition for single drug versus combination drug formulations and to establish a correlation between adhesion and cohesion of three micronised drug materials with their relative in vitro performances.
Particle Size
Micronised BUD was found to have a median equivalent volume diameter of 3.24 μm, with over 82% of particles below 5 μm. In comparison, micronised FFD was found to have a median equivalent volume diameter of 2.69 μm, with 93% of particles below 5 μm. Micronised SS was found to have the largest median equivalent volume diameter of 3.33 μm, with 74% of particles below 5 μm.
In general, particle size suggests all three micronised drugs were of similar size and were suitable for inhalation applications (23). Volume (% under) data are presented in Fig. 4.
True Density
True density measurements for SS, BUD and FFD were determined as 1.306 ± 0.001 g.cm−3, 1.240 ± 0.007 g.cm−3 and 1.295 ± 0.007 g.cm−3, respectively (n = 10). (Density of HFA 134a at 20°C, 1.226 g.cm−3).
Characterisation and Morphology Prediction of the Drug Crystals
Data collected by AFM indicated very smooth, crystals surfaces exhibiting a root mean squared roughness well below 2 nm over 5 μm × 5 μm areas deeming them suitable for AFM studies (24,25). Root mean square values were 1.33 nm ± 0.04 nm for SS, 0.68 nm±0.01 nm for BUD and 1.52 nm ± 0.01 nm for FFD (n=25) respectively (5). Fresh batches of drug crystals were prepared for each colloidal probe study.
The dominant crystal face predicted for each of the three drugs was the (111) face for SS, the (002) face for BUD, and the (100) face for FFD. These predicted dominant crystal faces were used throughout this investigation.
Representative optical micrographs of the re-crystallised SS, BUD and FFD and predicted crystal morphology derived from SHAPE V 7.0 crystal computational software (Kingsport, USA) are shown in Fig. 5 (top, middle, and bottom, respectively). In general, good correlation between the optical micrographs and predicted crystal morphology was observed for all drug materials.
Atomic Force Microscopy Colloid Probe Measurements and CAB Analysis
Direct measurements of the cohesion and adhesion between single drug particulates and the dominant crystal faces of each drug material combination were performed using the in situ AFM probe technique. For a comprehensive review of the data and experimental procedure, authors refer to a previously published paper (5).
In situ atomic force microscopy measurements were performed for each permutation of single and combination drug. Each study was performed with three probes of each drug. The AFM settings were as follows: force volume scan size 5 μm × 5 μm, approach retraction cycle 500 nm, cycle rate 4.07 Hz and constant compliance region 60 nm. Data was processed to produce force of separation values and number distribution of each data set indicated a normal distribution with low variability (a correlation coefficient of the linear relationship equal to R 2 = 0.95 ± 0.05 for SS tip, R 2 = 0.94 ± 0.07 for BUD and R 2 = 0.89 ± 0.06 for FFD. In order to characterise the adhesive and cohesive characteristics of each of the drugs, data were further analysed using the recent published Cohesive/Adhesive balance method (CAB) (9). The focal point of this method of analysis is that it allows quantification of the relationship between the theoretical works of cohesion and adhesion and corresponding AFM measurements without prior knowledge of the contact area between an irregular probe and atomically smooth model substrate surface.
For the SS probes (n = 3), the AFM data suggested that the SS-FFD interaction was approximately twice that of the SS-BUD adhesion. For the BUD probes (n = 3) the quantitative AFM data suggested that the adhesive BUD-SS interaction was nine times greater than the cohesive one. For FFD probes (n = 3) the AFM data suggested that the FFD-SS interaction was approximately five times greater than the force of cohesion. A graphical representation of the cohesive and adhesive characteristics of all drugs used in this study is presented in Fig. 6. Corroborating data can be found in Traini et al., (2005) (5).
Graphical representation of the cohesive or adhesive nature of an AFM drug probe with drug substrate. The first acronym for each series denotes the drug probe type. Each CAB value is based on linear regression analysis of three drug probes (R 2 > 0.9000). Values >1 indicate the drug probe has a cohesive bias, while values <1 present a more adhesive characteristic. Corroborating data can be found in Traini et al., (2005) (5).
In Situ Sedimentation of pMDI Formulations
Information about the physical stability and the adhesive/cohesive characteristics of the suspension pMDI formulations may be obtained by observing the sedimentation characteristic of the drug particulates after a specific settling time. Figures 7 and 8 show the settling characteristics of the sedimentation of the pMDI formulations at time zero and after 24 h.
Sedimentation of combination drug suspensions (SS-BUD = salbutamol sulphate in combination with budesonide; SS-FFD = salbutamol sulphate in combination with formoterol fumarate dihydrate and BUD-FFD = budesonide in combination with formoterol fumarate dihydrate). At T=0, just after shaking, (top image) and after 24 h (bottom image).
Directly after shaking, the formulations demonstrate a tendency to form heterogeneous floccules readily suspended for all micronised drugs, for both single drug and combination drug formulation. After standing for 24 h, SS single drug formulation presents the smallest sedimentation volume, correlating well with previous AFM findings where this β2 agonist has been shown to have strong cohesive characteristics (5). Similarly, BUD and FFD single drug formulations show a higher sedimentation volume with looser flocks, once more correlating with previous findings where both drugs have been found to exhibit more adhesive characteristics (5).
The cohesive and adhesive quality of the three micronised drugs is reflected, moreover, in the respective combination drug formulations. When the SS is present (in combination with BUD or FFD), system showed a lower sedimentation volume in comparison with combination drug formulations where the two drugs with adhesive characteristics are present (BUD and FFD). A possible explanation is the formation of strong interparticle bonds between SS-BUD and SS-FFD, thus inducing small interparticulate cavities and, consequently more compact sedimentation. In comparison, BUD-FFD form relatively weak interparticulate bonds due to their adhesive bias, inducing higher sediment characteristics.
In Vitro Analysis Results of pMDI Formulations
The particle size distribution, obtained by cascade impactor analysis, of the cumulative particle undersize for various aerodynamic cut-off stages (from stage 1 <9 μm to stage 4<3.3 μm) of SS, BUD and FFD delivered from the single drug pMDIs, were compared with particle size distribution of the combination drug formulation inhalers (SS-BUD, SS-FFD and BUD-FFD) for the same stages. Graphical representation for deposition of single drug in each stage of the ACI is presented in Fig. 9. The mean percentile deposition and the range of the mass on each stages for three replicates against the effective cut-off diameter of the stage for the single and combination formulations shows the variation in the amount of drug particulate observed on a given stage within the formulation. The total amount of drug collected from stage one to four obtained for the single and combination formulations are presented in Table I and II, respectively. Results indicate significant differences (p < 0.05) in the deposition pattern.
The emitted drug deposition of SS, BUD and FFD presented as percentage of the theoretical dose formulated as single drug and combination formulation were compared. Data are presented in Table III. Graphical representations of the emitted drug deposition of single drug formulations are shown in Fig. 10, while combination drug formulation data for SS-BUD, SS-FFD and BUD-FFD are shown in Figs. 11, 12, 13, respectively.
Delivered as single drug, SS presents very poor emitted dose performance, as shown in Table III (% emitted dose/theoretical dose 37.8% ± 11.1). It was evident that emitted dose of SS increased up to three times when delivered in a combination formulation, with both BUD ( 91.2% ± 5.6) and FFD ( 78.8% ± 23.9). Data are significantly different (p < 0.05, p = 0.013). The rationale behind this lies in the cohesive physical characteristic of this drug. Being predominantly cohesive, SS particles, when delivered as a homogenous system, will have a tendency to aggregate due to van der Waals attractive forces. Consequently, these homogeneous flocs formed by random collisions will be difficult to break apart during inhalation. Deaggregation involves the expenditure of work during actuation and it can only take place if there is sufficient kinetic energy to overcome the energy barrier associated with binding. Accordingly, cohesive drugs like SS will not be proficiently delivered to the target site but rather will impact in the upper stages of the ACI, giving poor drug delivery performances.
When combined with adhesive drugs like BUD and FFD, SS will tend to aggregate but, BUD-SS and FFD-SS flocs will be loosely bound, easy to re-disperse and, therefore be delivered with higher performances. These findings are confirmed not only by the drug delivery recovery but also by visual observations of sedimentation of the above drugs in the glass canisters. Sediments of combination drug formulations containing SS are, in all cases, more compact and have lower sedimentation volumes than formulations without such a cohesive drug.
As shown in Table III, budesonide delivered as single drug presents an experimental emitted dose of 79.4% ± 7.4. When delivered in a combination formulation, with both SS (69.8% ± 8.3) and formoterol (104.8% ± 15.5) data are still significantly different (p < 0.05, p = 0.02) variation between single drug and combination drug formulations of BUD is not as broad as is observed in the SS systems. The underlying principle behind this lies in the adhesive physical characteristic of this drug.
Budesonide, being predominantly adhesive, when delivered as homogeneous system, or combined with another adhesive drug like FFD, will have the tendency to form loose flocs, due to relatively weak particulate bonds. To elaborate, the adhesive nature of BUD and FFD will result in the formation of intraparticulate agglomerate, constituted of both drugs, which will easier to break during inhalation and thus be able to reach the deep lung.
On the contrary, when coupled with a cohesive drug like SS, BUD will tend to aggregate strongly resulting in decreased delivery performance. Visual observations of sedimentation of the above drugs in the glass canisters corroborate these findings. Sediments of combination formulations containing an adhesive–cohesive drug mixture, in all cases, showed more compact sedimentation volumes.
As shown in Table III, Formoterol delivered as single drug presents an experimental emitted dose of 88.8% ± 3.5. When delivered in a combination formulation, with both SS (emitted dose of 63.7% ± 23.9) and BUD (emitted dose of 90.1% ± 14.7) data are not significantly different (p > 0.05, p = 0.162). Like BUD, FFD is a drug with an adhesive characteristic, and, consequently, performs like the latter in the presence of adhesive or cohesive drugs.
Conclusions
An in vitro investigation of three micronised drug systems was undertaken to determine if the relationship between adhesive/cohesive forces, measured by AFM and CAB, could be correlated with in vitro performance.
Direct measurements of the interaction forces (via AFM measurements) responsible for the stability of colloidal particles in binary pMDI formulations indicate a fine balance between adhesive and cohesive tendencies.
The in vitro investigation suggested that the three micronised drug materials had significantly different aerosolisation profiles when manufactured as single or combination formulations. The relationship between aerosolisation performance of the micronised drugs can be attributed to the modification in the balance of forces acting between the particulates within the respective formulations.
In general, the greatest significant differences were observed between salbutamol single drug and combination systems. Analysis of the in vitro performance for the salbutamol-only formulation suggested that the cohesive nature of salbutamol (as predicted by the CAB and observed with AFM) led to tightly bound flocs that did not fully deaggregate upon aerosolisation. In comparison, the improved aerosolisation efficiency of salbutamol in combination with budesonide or formoterol showed the positive effect of the adhesive characteristics of the latter two drug particulates (also predicted by the CAB and observed with AFM). In summary, the relationship between inter-particulate interactions and aerosol performance indicated good correlation.
References
P. J. Barnes, M. M. Grunstein, A. R. Leff, and A. J. Woolcock. Asthma, Lippincott-Raven, Philadelphia, 1997.
R. N. Dalby and J. Suman. Inhalation therapy: technological milestones in asthma treatment. Adv. Drug Deliv. Rev. 55:779–791 (2003).
H. D. C. Smyth. Propellant-driven metered-dose inhalers for pulmonary drug delivery. Expert Opin. Drug Deliv. 2:53–74 (2005).
A. Brindley. The chlorofluorocarbon to hydrofluoroalkane transition: the effect on pressurised metered dose inhaler suspension stability. J. Allergy Clin. Immunol. 104:S221–S226 (1999).
D. Traini, P. Rogueda, P. M. Young, and R. Price. Surface energy and interparticle forces correlations in model pMDI formulations. Pharm. Res. 22:816–825 (2005).
R. J. Good and L. A. Girifalco. A theory for estimation of surface and interfacial energies. III. Estimation of surface energies of solids from contact angle data. J. Phys. Chem. 64:561–565 (1960).
F. M. Fowkes. Determination of interfacial tension, contact angles and dispersion forces in surface by assuming additivity of intermolecular interactions in surfaces. J. Phys. Chem. 66:382 (1962).
C. J. van Oss. Interfacial Forces in Aqueous Media. Marcel Dekker, New York, U.S.A., 1994.
P. Begat, D. A. V. Morton, J. N. Staniforth, and R. Price. The cohesive–adhesive balances in dry powder inhaler formulations I: direct quantification by atomic force microscopy. Pharm. Res. 21:1591–1597 (2004).
Apparatus D, British Pharmacopoeia. The Stationery Office on behalf of the Medicines and Healthcare Products Regulatory Agency (MHRA). London, UK, 2005.
N. J. C. Snell and D. Ganderton. Assessing lung deposition of inhaled medications: consensus statement from a workshop of the British Association for Lung Research. Respir. Med. 93:123–133 (1999).
C. G. Thiel. Can in vitro particle size measurements be used to predict pulmonary deposition of aerosol from inhalers? J. Aerosol Med. 11:S43–S52 (1998).
P. A. Webb and C. Orr. Analytical Methods in Fine Particle Technology, Micrometrics Instrument Corp., Norcross, Georgia, U.S.A., 1997.
G. Rhodes. Crystallography—Made Crystal Clear, Academic, New York, USA, 1993.
J. Albertsson, A. Oskarsson, and C. Svensson. X-ray study of budesonide: molecular structure and solid solution of the (22S) and (22R) epimers of 11B,21-dihydroxy-16alfa,17 alfa-propylmethylenedioxy-1,4-pregnadiene-3,20-dione. Acta Crystallogr. B34:3027–3036 (1978).
Ertan, B. Stensland, and I. Ymen. Crystal and molecular structure of formoterol fumarate dihydrate, Astra Production Chemicals AB, Confidential Report N. 117/97, 1997.
P. J. M. Leger, M. Goursolle, and M. Gadret. Structure cristalline du sulphate de salbutamol [ter-butylamino-2-(hydroxy-4hydroxymethyl-3 phenyl)-1 ethanol.1/2 H2SO4]. Acta Crystallogr. B34:1203–1208 (1978).
W. A. Ducker, T. J. Senden, and R. M. Pashley. Direct measurement of colloidal forces using an atomic force microscope. Nature 353:239–241 (1991).
P. M. Young. Characterisation of particle–particle interactions using the atomic force microscope, Pharmacy and Pharmacology, University of Bath, Bath, UK, 2002.
Y. Michael, M. J. Snowden, B. Z. Chowdhry, I. C. Ashurst, C. J. Davies-Cutting, and T. Ripley. Characterisation of the aggregation behaviour in a salmeterol and fluticasone propionate inhalation aerosol system. Int. J. Pharm. 221:165–174 (2001).
E. M. Phillips, P. R. Byron, and R. N. Dalby. Axial-ratio measurements for early detection of crystal-growth in suspension-type metered dose inhalers. Pharm. Res. 10:454–456 (1993).
P. G. A. Rogueda. HPFP, a model propellant for pMDIs. Drug Dev. Ind. Pharm. 29:39–49 (2003).
J. N. Pritchard. The influence of lung deposition on clinical response. J. Aerosol Med. 14:S19–S26 (2001).
W. Neumann, D. R. Renzow, H. Reumuth, and J. E. Richter. Vol. 55, Fortschr. Kolloide Polymere 49–54 (1971)
G. Buckton. Interfacial Phenomena in Drug Delivery and Targeting, Harwood Academic Publishers, Chur, Switzerland, 1995.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Traini, D., Young, P.M., Rogueda, P. et al. In Vitro Investigation of Drug Particulates Interactions and Aerosol Performance of Pressurised Metered Dose Inhalers. Pharm Res 24, 125–135 (2007). https://doi.org/10.1007/s11095-006-9130-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-006-9130-2