Abstract
Purpose
To determine the contribution of the lymphatics to the systemic availability of darbepoetin alfa (DA) using an established sheep model.
Materials and Methods
DA was administered either by intravenous (IV) injection (0.2, 0.5 or 2 μg/kg) or by subcutaneous (SC) administration (2 μg/kg) into the interdigital space of the hind leg. A SC control group was used to determine the absolute bioavailability (F sys). Cannulation of the peripheral lymphatics in a parallel SC group allowed the continuous collection of lymph draining the injection site and determination of the cumulative amount of DA absorbed via the lymphatics. Serum and lymph concentrations of DA were determined by ELISA. The fraction of the dose absorbed into the lymphatics (F lymph) relative to the fraction absorbed directly into the blood (F blood) was determined using a compartmental approach.
Results
Dose-linear pharmacokinetics was observed within the dose range investigated. The bioavailability was virtually complete following SC injection into the interdigital space (88.4 ± 15.7%). A high proportion of the administered dose was recovered in peripheral lymph (90.2 ± 4.4%) resulting in a substantial reduction in the systemic availability in lymph cannulated animals (3.7%).
Conclusion
The high recovery of DA in the peripheral lymph demonstrated near complete absorption of this recombinant protein via the lymphatics in a lymph cannulated sheep model.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Darbepoetin alfa (Aranesp®, novel erythropoiesis stimulating protein) is a hyperglycosylated analogue of recombinant human epoetin alfa (rHuEPO). Darbepoetin alfa (DA) stimulates red cell production and proliferation via the same mechanism as rHuEPO (1) and is approved for the treatment of anaemia associated with chronic renal failure and chemotherapy-induced anaemia in patients with non-myeloid malignancies. DA provides an advantage over rHuEPO in that it displays an extended serum half-life allowing dosing at a less frequent interval compared with rHuEPO (2). DA is produced in Chinese hamster ovary (CHO) cells and contains amino acid modifications at five positions to allow the attachment of two additional N-linked sialic acid carbohydrate chains in comparison to rHuEPO (1,2). The increased carbohydrate content in the hyperglycosylated analogue increases the molecular weight of darbepoetin alfa (37.0 kDa compared to 30.4 kDa for rHuEPO) and the overall anionic charge which modulates the systemic pharmacokinetics (1,2) resulting in an approximately three-fold longer serum terminal half-life compared to rHuEPO (25.3 versus 8.5 h) after intravenous (IV) administration in dialysis patients (3).
The increased circulating half-life of the DA relative to rHuEPO is a consequence of a reduction in serum clearance as opposed to changes in the volume of distribution which can be approximated to plasma volume for both proteins (2,3). While the clearance of rHuEPO in humans and other species has shown marked dose-dependence (4–7), DA has apparent dose-linear pharmacokinetics in humans (8). Pharmacokinetic assessment of DA in different animal species (mice, rats, dogs and humans) has demonstrated that allometric scaling provides adequate predictions of human IV clearance and volume of distribution (9).
Following subcutaneous (SC) administration, absorption of DA is significantly slower than that of rHuEPO across a range of SC injection sites with the time to maximal concentration occurring between 36 and 49 h in humans for the hyperglycosylated analogue (3,10) compared with 10–18 h for rHuEPO (11,12). The bioavailability of DA after SC injection in humans is incomplete (36.9 ± 3.0%) (3). DA demonstrates “flip-flop” pharmacokinetics with a longer half-life after SC administration relative to IV administration (approximately 70 h (10) and 25.3 h (3), respectively) which is also consistent with slow absorption. The slower absorption of the hyperglycosylated analogue has been attributed to the larger molecular size of the protein (3), however, the increased negative charge of DA (pI ∼3.3) compared to rHuEPO (pI ∼4.0) may also influence the SC absorption rate and bioavailability (2,13).
Given the pharmacokinetic differences between DA and rHuEPO, and the understanding that these differences are related both to differences in clearance and absorption rate, the current study was initiated to explore the influence of hyperglycosylation on the rate and extent of SC absorption of DA in a sheep model. Previous studies which have quantified the relative roles of the lymphatics and vasculature in the absorption of SC administered recombinant proteins have demonstrated an increasing contribution of the lymphatics to overall absorption with increasing molecular weight (14–17). A recent mechanistic assessment of rHuEPO absorption in sheep revealed preferential absorption via the lymphatics (83.9% of the administered dose) with a minimal contribution of direct vascular absorption after SC administration (18). Furthermore, these studies indicated no loss of rHuEPO upon transport through the lymphatics. On the basis of these previously published findings, it was predicted that the lymphatics would also play a major role in the overall SC bioavailability of DA, however given the current information, it was not possible to predict the effect of hyperglycosylation and increased net negative charge on the rate and extent of lymphatic absorption, and the potential for retention at the injection site and/or lymphatic clearance.
Materials and Methods
Materials
Recombinant DA solution and placebo formulation were provided by Amgen Inc. (Thousand Oaks, CA, USA). Adult male merino sheep (40–60 kg) were obtained from the Victorian Institute of Animal Science (Werribee, Australia). Intravenous 16-gauge catheters (133 mm, Angiocath™, Becton Dickinson, Australia) were used to facilitate blood sampling. Peripheral lymphatic ducts were cannulated using sterilized medical grade polyvinyl cannulae of 0.58 mm internal diameter and 0.96 mm external diameter (W.F Scientific, Victoria, Australia). Blood samples and peripheral lymph were collected into glass collection tubes containing no anticoagulant (Vacutainer®, Becton Dickinson). Commercial Quantikine® In Vitro Diagnostic® human erythropoietin ELISA kits were from R&D Systems (Minneapolis, USA). Horse serum was purchased from Life Technologies (GibcoBRL®, Auckland, New Zealand).
Study Design and Surgical Procedures
The animal studies were approved by The University of Melbourne Animal Experimentation Ethics Sub-Committee and were conducted in accordance with the “Principles of Laboratory Animal Care” (NIH publication #85-23, revised 1985). Doses were administered to three parallel groups of sheep according to Table I. DA stock solution (494 μg/ml) was diluted with placebo formulation to provide a nominal dose volume of between 1.0 and 1.5 ml for all animals. A range of intravenous (IV) bolus doses (0.2, 0.5 and 2 μg/kg) were administered by venipuncture into the jugular vein of animals in the IV control groups to assist in characterising pharmacokinetic linearity. Subcutaneous (SC) doses (2 μg/kg) were administered into the interdigital space of the hindleg for non-lymph cannulated SC control and lymph cannulated animals.
Serum was sampled from all animals via a catheter inserted in the jugular vein. Peripheral lymph was continuously and quantitatively collected from the lymph cannulated group via a cannula inserted in the efferent popliteal lymph duct. Lymphatic cannulations were performed according to published methods (19) and peripheral lymph flow rates greater than 3 ml/h were used as an indication of the absence of collateral lymphatic vessels which would have prohibited quantitative lymph collection. Animals were housed in metabolism cages during the experimental period and food and water were available ad libitum.
Sample Collection
Blood samples were withdrawn prior to dosing and 1, 5, 10, 15, 30 min, 1, 2, 4, 6, 8, 10, 12, 18, 24, 30, 48, 54, 72, 78, 96 and 102 h post-dosing for the IV treatment groups. Additional blood samples were withdrawn at 168 and 174 h post-dosing for the 2 μg/kg IV control group. Blood samples were withdrawn prior to dosing and 0.5, 1, 4, 8, 12, 24, 30, 48, 54, 72, 96, 120 and 168 h post-dosing for the SC control and lymph cannulated groups. Lymph samples for the lymph cannulated group were collected at hourly intervals for the first 12 h and then at 12-hourly intervals up to 36 h post-dosing.
All blood samples were withdrawn via the IV catheter inserted in the jugular vein. One millilitre of blood was initially withdrawn and discarded to flush the catheter and to ensure collection of circulating blood. Five millilitres of blood was subsequently withdrawn and transferred into serum collection tubes. The jugular vein catheter was flushed with a small volume of heparinized saline (10 IU/ml) immediately following blood withdrawal to ensure patency. Blood and lymph samples were allowed to clot for 60 min at ambient temperature prior to centrifugation at 2,576 × g for 10 min. Aliquots of the supernatant were taken and frozen at −80°C until analysis.
Assay Methodology
DA concentrations in serum and lymph samples were determined using a commercial human erythropoietin ELISA kit. All the reagents from the kit were used according to the prescribed instructions. Reference standards and three quality control samples (QCs) were prepared using DA solution provided by Amgen Inc. (Thousand Oaks, CA, USA). Calibration curves consisted of seven standards and provided an analytical range of 0.13–6.25 ng/ml. The lower limit of quantitation for the DA assay was 0.25 ng/ml. QCs were prepared at three final concentrations (0.99, 2.74 and 5.49 ng/ml) and were stored along with the study samples to monitor sample stability and routine assay performance. Serum samples were diluted with pooled sheep serum if necessary to fall within the assay range and concentrations were determined relative to calibration curves prepared using pooled sheep serum. Lymph samples were diluted with horse serum due to the large dilution factors required and the commercial availability of horse serum. Lymph concentrations were determined against calibration curves prepared using horse serum and a minimum dilution factor of 1:10 was adopted to minimise matrix interference. QCs prepared in peripheral lymph were diluted 1:10 with horse serum prior to assaying to reflect and validate sample preparation. The precision of the assays was <15% and the accuracy of measured QC concentrations were consistently within ±15% of the nominal concentrations. There were no cross-reacting species (including endogenous erythropoietin) present in the pre-dose samples or in the pooled sheep or horse serum used for sample dilution.
Pharmacokinetic Analysis
Non-compartmental analysis was performed using WinNonlin (v. 3.2, Pharsight Corporation, Mountain View, CA, USA) for individual serum profiles. The terminal elimination half life (t 1/2), area under the serum concentration–time curve extrapolated to infinity (\( {\text{AUC}}_{{{\text{0 - }}\infty }} \)), steady-state volume of distribution (V ss) and serum clearance (CL) were calculated using standard pharmacokinetic approaches for the IV treatment groups (20). For the SC treatment groups, the peak serum concentrations (C max) and time to reach the peak concentration (T max) were taken directly from experimental data. The terminal t 1/2 for the SC treatment groups and bioavailability (F sys) calculated relative to the 2 μg/kg IV treatment group, were determined using standard pharmacokinetic approaches. For the lymph cannulated group, non-compartmental analysis was conducted on mean serum concentrations due to variability and low serum concentrations. The mass of DA collected in each lymph sampling interval was calculated by taking the product of the measured sample concentration and the lymph sample volume. Lymph recovery was calculated as a percentage of the administered dose. The total fraction of the dose absorbed (F abs) for the SC lymph-cannulated group was calculated through summation of F sys and the lymph recovery.
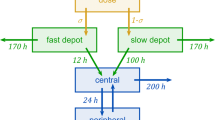
Compartmental analysis was performed using SAAM II (v. 1.2, SAAM Institute, University of Washington, Seattle, USA). Compartmental modelling was undertaken using a simplified adaptation of a model recently described for rHuEPO (18). The non-linear clearance process required to describe rHuEPO disposition was not necessary for the modelling of DA due to the apparent linear pharmacokinetics across the dose and plasma concentration range investigated. A two compartmental model incorporating first order absorption via the lymph and blood pathways (Fig. 1) was utilised to simultaneously describe mean serum concentrations for the 0.5 μg/kg IV and 2 μg/kg SC groups, and the mean cumulative recovery in the peripheral lymph SC group (equations outlined in Appendix). Modeling was conducted using mean treatment group data and was optimised using the fractional standard deviation (FSD) based on the coefficient of variance corresponding to each mean data point. The goodness of fit was assessed by the absence of systematic deviations in the weighted residuals and the precision of parameter estimates was demonstrated by the coefficient of variation. Data for the 0.2 and 2 μg/kg IV dose levels (n = 2 for each) was utilised for the non-compartmental assessment of linear pharmacokinetics for DA although were not included in the compartmental model due to low animal numbers.
Proposed pharmacokinetic model for DA administered by IV or SC bolus injection. For the IV treatment groups, the blood and lymph absorption pathways are not relevant. For the non-lymph cannulated SC group, DA was absorbed via the blood pathway (k blood) or via the peripheral and central lymph (k lymph) into the systemic circulation. For the peripheral lymph cannulated group, the proportion of the dose absorbed from the SC injection site into the lymph was quantitatively collected prior to transferral into central lymph.
Results
Serum concentrations of DA declined biexponentially following IV administration (Fig. 2A). There were no apparent differences between the terminal t 1/2, V ss or CL for the three IV doses (0.2, 0.5 and 2 μg/kg) suggesting linear pharmacokinetics within this dose and concentration range (Table II). The mean serum profiles for the SC control and lymph cannulated groups are shown in Fig. 2A. Absorption following SC administration was slow with T max in serum for the SC control and lymph cannulated groups occurring at 6 and 8 h, respectively (Table II). The terminal t 1/2 for the SC control (30.2 ± 4.4 h) and lymph cannulated (29.4 h) groups were comparable to the terminal t 1/2 observed after IV administration (∼33 h across the dose range).
Serum DA concentration versus time profiles (Panel A) and cumulative recovery of DA in peripheral lymph versus time profile (Panel B) following IV administration of 0.5 μg/kg to the non-lymph cannulated IV control sheep (filled square, Panel A only), and SC administration of 2 μg/kg to the non-lymph cannulated SC control (filled triangle, Panel A only) and SC lymph cannulated (filled circle) groups (mean ± SD, n = 4). Symbols represent the experimental data and the model predicted fits for the mean observed data are shown by the solid lines. The dashed line in Panel B represents the mean absolute dose (μg) administered to lymph cannulated animals.
The collection of peripheral lymph resulted in substantial reductions in serum C max and \( {\text{AUC}}_{{{\text{0 - }}\infty }} \)for the lymph cannulated group compared to the SC control group (Table II). Non-compartmental analysis was conducted using individual serum profiles for the SC control group and mean serum concentrations for the lymph cannulated group given the very low serum concentrations. The systemic bioavailability (F sys) for the SC control group, calculated relative to the mean IV data at 2 μg/kg, was 88.4 ± 15.7% and was reduced to approximately 3.7% for the lymph cannulated group. The cumulative recovery of DA in peripheral lymph was 90.2 ± 4.4% of the administered dose. The total fraction of the dose absorbed (F abs) for the lymph cannulated group was 93.9 ± 4.4% which was not statistically different to F sys for the SC control group (88.4 ± 15.7%).
The two compartmental model incorporating first order absorption via blood and lymph pathways adequately predicted serum concentrations for the 0.5 μg/kg IV and 2 μg/kg SC treatment groups, and the cumulative recovery in peripheral lymph for the SC lymph cannulated group. The model predicted fits for the serum concentrations are shown in Fig. 2A and the model predicted fit for cumulative recovery in lymph is shown in Fig. 2B. The distribution parameters k 12 and k 21 were constrained to be equivalent for each of the different treatment groups, however improved fits were observed for the SC groups when the parameter k 10 was not constrained to the corresponding rate constant in the mean IV control group. Variability was more evident in the terminal serum concentrations of the SC control profiles and constraining k 10 led to a systematic underestimation in the elimination portion of the profile. Nonetheless, the parameter estimates for k 10 for the IV and SC groups were comparable. The validity of the compartmental estimates is supported by the low coefficient of variation (Table III) and consistency between estimates for CL and F abs obtained using compartmental and non-compartmental approaches (Table II).
Discussion
In contrast to previous results for rHuEPO (18), there was no evidence of nonlinear kinetics for DA in sheep within the dose range studied as demonstrated by dose-proportional \( {\text{AUC}}_{{{\text{0 - }}\infty }} \)and similar estimates for the other non-compartmental parameters (t 1/2, V ss and CL). The resulting serum concentrations of DA after IV administration (0.2, 0.5 and 2 μg/kg) were within the same range of serum concentrations after SC administration (2 μg/kg). The V ss in sheep (mean 73.6 ml/kg) indicated that like rHuEPO, DA does not distribute extensively outside the vasculature (estimated plasma volume of sheep is 39 ml/kg (21). Serum CL was observed to be low (mean 1.60 ml/h/kg) and independent of dose.
The serum CL of DA at 0.5 μg/kg was significantly lower than that for rHuEPO at an equivalent 100 IU/kg dose resulting in an approximately four-fold longer serum t 1/2 (Table IV). The V c for the two proteins was comparable in sheep which was consistent with observations in other species which have demonstrated that hyperglycosylation modulates the circulating t 1/2 via a reduction in CL without altering the volume of distribution (2,3). Clearance of DA was also observed to be independent of dose in contrast to marked dose-dependency for rHuEPO in sheep (18). The mechanistic basis for this pharmacokinetic difference is not currently understood.
The bioavailability of DA was nearly complete after SC administration to sheep with an estimated F sys of 88.4 ± 15.7% for the SC control group. Mass balance was achieved for the lymph cannulated group as demonstrated by F abs of 93.9 ± 4.4%. The systemic availability of DA was considerably higher in sheep (88.4 ± 15.7%) when compared to the reported bioavailability in humans (36.9 ± 3.0%) (3). The SC absorption of DA was also significantly faster in sheep (T max 4–12 h) than in humans (T max 36–49 h) (3,10) and the apparent differences in T max for DA and rHuEPO seen in humans was not evident in sheep (T max for rHuEPO was 4–12 h in sheep (18)). In humans, “flip-flop” kinetics after SC injection of DA has been described (3) but this was not evident in sheep as demonstrated by the similar terminal t 1/2 values after IV and SC administration, presumably due to the more rapid absorption rate. These differences may reflect the use of different SC injection sites (interdigital space of the hind leg in sheep and upper thigh, abdomen or arm in humans) or potential differences in the absorption mechanisms in sheep and humans. The influence of the injection site on the rate and extent of lymphatic uptake for DA and other proteins remains largely undefined.
DA was preferentially absorbed via the lymphatics following SC administration to sheep as demonstrated by 90.2 ± 4.4% of the administered dose being recovered in the peripheral lymph from the lymph cannulated group. Preferential absorption of DA via the lymphatics in the lymph cannulated group was also independently verified by the reduced F sys (3.7%) compared with the SC control group (88.4 ± 15.7%). Similarity between F abs for the peripheral lymph cannulated group (93.9 ± 4.4%) and F sys in the non-lymph cannulated SC control group (88.4 ± 15.7%) suggested that there was minimal clearance during transfer of DA within the lymphatics. The recovery of 90.2 ± 4.4% of the SC administered dose of DA in peripheral lymph was comparable to 83.9 ± 6.6% recovery of rHuEPO in peripheral lymph (18).
For both DA and rHuEPO, the lymphatics would appear to be the predominant absorption pathway after SC administration in the cannulated sheep model. In these studies, the interdigital injection site of the hindleg was chosen due to the technical feasibility of quantitatively collecting the peripheral lymph draining the administration site. To date, little has been reported regarding the similarity between the interdigital space and other SC injection sites, especially with regard to the absorption of macromolecules. Variations in topology and blood/lymph flow characteristics at different injection sites are likely to influence the absorption rate of macromolecules and proteins administered via the SC route ((22) and references within). Future studies to investigate the rate and extent of lymphatic uptake from different anatomical sites may assist in explaining the difference in the apparent absorption rates for DA in sheep and humans as well as differences between the rates of absorption for DA and rHuEPO.
Summation of compartmental estimates of transfer rate constants into the blood (k blood) and lymph (k lymph) for DA and rHuEPO in sheep (Table IV) indicated a slightly faster absorption rate for DA than rHuEPO (0.30 and 0.18 h−1, respectively) despite the higher molecular weight for the hyperglycosylated analogue. Faster absorption of DA in the sheep model may, in part, reflect greater diffusivity within the aqueous regions of the SC injection site due to presence of additional hydrophilic negatively charged carbohydrate chains which could potentially reduce electrostatic interactions with negatively charged glycosaminoglycans within the interstitium (22). The contribution of species variability and differences in injection sites, however, cannot be excluded and additional studies are required to further explore the effect of protein glycosylation on SC absorption mechanisms.
In summary, the structurally related proteins, DA and rHuEPO demonstrated marked differences in pharmacokinetic disposition in sheep, consistent with previous observations in humans and other species. The hyperglycosylated analogue exhibited dose-linear pharmacokinetics across a ten-fold dose range in comparison to dose-dependency observed previously for rHuEPO in this animal model (18). The increased molecular weight and overall negative charge imparted by hyperglycosylation increased the circulating t 1/2 of DA by a reduction in serum CL but did not affect the extent of SC absorption and there was no evidence of retention of DA at the injection site. As for rHuEPO, the lymphatics was the predominant absorption route for DA and the relative distribution between the blood and lymphatic absorptive pathways in the sheep model did not appear to be affected by hyperglycosylation. While compartmental modelling predicted a marginally faster rate of absorption rate for DA in the sheep model, additional studies are required to confirm this trend and examine the role of the SC injection site which will provide additional mechanistic insight into the factors affecting the SC absorption of this important protein.
Notations
- \( {\text{AUC}}_{{{\text{0 - }}\infty }} \) :
-
Area under the serum concentration–time curve extrapolated to infinity
- CL:
-
Serum clearance
- C max :
-
Maximum serum concentration
- C s :
-
Serum concentration
- F abs :
-
Total fraction of the dose absorbed in the lymph cannulated animals
- F blood :
-
Fraction of the absorbed dose taken up via the blood pathway
- F lymph :
-
Fraction of the absorbed dose taken up via the lymph pathway
- F sys :
-
Fraction of the dose absorbed into systemic circulation
- IV:
-
Intravenous
- k blood :
-
Transfer rate constant into blood
- k lymph :
-
Transfer rate constant into lymph
- rHuEPO:
-
Recombinant human erythropoietin
- SC:
-
Subcutaneous
- t 1/2 :
-
Terminal half-life
- T max :
-
Time at which maximum serum concentration occurs
- V c :
-
Volume of distribution of central compartment
- V ss :
-
Volume of distribution at steady state
References
I. C. Macdougall. Novel erythropoiesis stimulating protein. Semin. Neurol. 20:375–381 (2000).
J. C. Egrie and J. K. Browne. Development and characterization of novel erythropoiesis stimulating protein (NESP). Nephrol. Dial. Transplant. 16(Suppl 3):3–13 (2001).
I. C. Macdougall, S. J. Gray, O. Elston, C. Breen, B. Jenkins, J. Browne, and J. Egrie. Pharmacokinetics of novel erythropoiesis stimulating protein compared with epoetin alfa in dialysis patients. J. Am. Soc. Nephrol. 10:2392–2395 (1999).
K. K. Flaharty, J. Caro, A. Erslev, J. J. Whalen, E. M. Morris, T. D. Bjornsson, and P. H. Vlasses. Pharmacokinetics and erythropoietic response to human recombinant erythropoietin in healthy men. Clin. Pharmacol. Ther. 47:557–564 (1990).
P. Veng-Pedersen, J. A. Widness, L. M. Pereira, C. Peters, R. L. Schmidt, and L. S. Lowe. Kinetic evaluation of nonlinear drug elimination by a disposition decomposition analysis. Application to the analysis of the nonlinear elimination kinetics of erythropoietin in adult humans. J. Pharm. Sci. 84:760–767 (1995).
P. Veng-Pedersen, J. A. Widness, L. M. Pereira, R. L. Schmidt, and L. S. Lowe. A comparison of nonlinear pharmacokinetics of erythropoietin in sheep and humans. Biopharm. Drug Dispos. 20:217–223 (1999).
M. Kato, H. Kamiyama, A. Okazaki, K. Kumaki, Y. Kato, and Y. Sugiyama. Mechanism for the nonlinear pharmacokinetics of erythropoietin in rats. J. Pharmacol. Exp. Ther. 283:520–527 (1997).
M. Allon, K. Kleinman, M. Walczyk, C. Kaupke, L. Messer-Mann, K. Olson, A. C. Heatherington, and B. J. Maroni. Pharmacokinetics and pharmacodynamics of darbepoetin alfa and epoetin in patients undergoing dialysis. Clin. Pharmacol. Ther. 72:546–555 (2002).
A. Heatherington, D. Robi, J. Young, and S. Baughman. Pharmacokinetic (PK) Properties of Aranesp™ Scale Allometrically. American Association of Pharmaceutical Scientists National Biotechnology Conference, San Diego, 2002.
G. Jang, R. Marino, B. Cooke, and D. Padhi. Darbepoetin Alfa (Aranesp) Pharmacokinetics is Comparable in Chronic Kidney Disease (CKD) Patients Receiving and not Receiving dialysis, in Pediatric CKD Patients, and in Healthy Adults. The American Society of Nephrology, Philadelphia, 2005.
D. Kampf, A. Kahl, J. Passlick, A. Pustelnik, K. U. Eckardt, B. Ehmer, C. Jacobs, A. Baumelou, B. Grabensee, and G. M. Gahl. Single-dose kinetics of recombinant human erythropoietin after intravenous, subcutaneous and intraperitoneal administration: preliminary results. Contrib. Nephrol. 76:106–111 (1989).
J. D. Jensen, L. W. Jensen, and J. K. Madsen. The pharmacokinetics of recombinant human erythropoietin after subcutaneous injection at different sites. Eur. J. Clin. Pharmacol. 46:333–337 (1994).
J. C. Egrie, E. Dwyer, J. K. Browne, A. Hitz, and M. A. Lykos. Darbepoetin alfa has a longer circulating half-life and greater in vivo potency than recombinant human erythropoietin. Exp. Hematol. 31:290–299 (2003).
A. Supersaxo, W. R. Hein, and H. Steffen. Effect of molecular weight on the lymphatic absorption of water-soluble compounds following subcutaneous administration. Pharm. Res. 7:167–169 (1990).
S. A. Charman, A. M. Segrave, G. A. Edwards, and C. J. H. Porter. Systemic availability and lymphatic transport of human growth hormone administered by subcutaneous injection. J. Pharm. Sci. 89:168–177 (2000).
C. J. Porter and S. A. Charman. Lymphatic transport of proteins after subcutaneous administration. J. Pharm. Sci. 89:297–310 (2000).
S. A. Charman, D. N. McLennan, G. A. Edwards, and C. J. H. Porter. Lymphatic absorption is a significant contributor to the subcutaneous bioavailability of insulin in a sheep model. Pharm. Res. 18:1620–1626 (2001).
D. N. McLennan, C. J. H. Porter, G. A. Edwards, S. W. Martin, A. C. Heatherington, and S. A. Charman. Lymphatic absorption is the primary contributor to the systemic availability of epoetin alfa following subcutaneous administration to sheep. J. Pharmacol. Exp. Ther. 313:345–351 (2005).
C. J. H. Porter, G. A. Edwards, and S. A. Charman. Lymphatic transport of proteins after s.c. injection: implications of animal model selection. Adv. Drug Deliv. Rev. 50:157–171 (2001).
M. Gibaldi and D. Perrier. Pharmacokinetics. Marcel Dekker, New York, 1982.
D. Adams and M. McKinley. The sheep. ANZCCART News 8:1–4 (1995).
D. N. McLennan, C. J. H. Porter, and S. A. Charman. Subcutaneous drug delivery and the role of the lymphatics. Drug. Discov. Today Technol. 2:89–96 (2005).
Acknowledgments
The technical assistance of Ms. Majella Snelling is gratefully acknowledged. Financial support for this study was provided by Amgen Inc., Thousand Oaks, California.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
C s | Serum concentration |
A sc | The amount at the SC injection site |
A pl | The amount in peripheral lymph |
A e | The amount in the extravascular compartment |
Secondary parameters estimated:
Rights and permissions
About this article
Cite this article
McLennan, D.N., Porter, C.J.H., Edwards, G.A. et al. The Absorption of Darbepoetin Alfa Occurs Predominantly via the Lymphatics Following Subcutaneous Administration to Sheep. Pharm Res 23, 2060–2066 (2006). https://doi.org/10.1007/s11095-006-9064-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-006-9064-8