Abstract
Purpose
To quantify the effects of the ratio of indomethacin to Neusilin US2 and the processing humidity on the amorphization kinetics, stability and nature of the interaction.
Materials and Methods
A porcelain jar mill with zirconia balls was used to affect conversion of the physical mixtures (48 g) of indomethacin and Neusilin US2 (in the ratios 1:1 to 1:5) to amorphous states at room temperature (25°C) employing either 0% RH or 75% RH. The percent crystallinity in the samples was determined from ATR-FTIR scans chemometrically. The physical stability of these co-ground amorphous powders was evaluated at 40°C/75% RH and 40°C/0% RH.
Results
The lower the ratio of indomethacin to Neusilin US2, the faster is the amorphization during co-grinding. Higher humidity facilitates amorphization with a more pronounced effect at the lower ratio of indomethacin to Neusilin US2. There is further amorphization of some of the partially amorphized samples on storage at 40°C/75% RH for 3 months. Hydrogen bonding and surface interaction between metal ions of Neusilin US2 and indomethacin can explain changes in the FTIR spectra.
Conclusions
The processing humidity and the ratio of indomethacin to Neusilin US2 are important factors to be considered to affect amorphization during ball milling. Amorphous indomethacin can be stabilized by co-grinding with Neusilin US2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
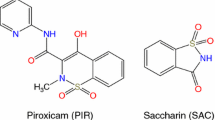
The increase in the number of poorly water soluble drug candidates has heightened interest in methods to improve water-solubility. There are several physical approaches which have been employed to improve drug solubility such as size reduction, melt adsorption (1), melt quenching (2), solvent deposition (3), spray drying (4), and freeze drying (5). These techniques often lead to the formation of amorphous solids. The key reason to form amorphous drugs is to increase the solubility and therefore the bioavailability of the poorly water-soluble compounds. Hancock and Parks (6) found that the experimental solubilities of the amorphous solids are at least 2–4 times greater than their crystalline counterparts. Watanabe et al., reported higher apparent equilibrium solubility of indomethacin co-ground with silica (7). There have been reports of increased solubility of indomethacin when spray dried with silica (8) and when co-ground with crospovidone (9). However, Yang et al., reported that the enhancement of drug dissolution by interaction with silicates is drug and silicate specific (3).
Co-grinding drugs with excipients has been employed for making amorphous solids. Watanabe et al., showed that amorphization of indomethacin could be achieved by milling it with polyvinylpyrrolidone or silica (10). Ali et al., used a vibration mill to prepare amorphous co-ground mixtures of flufenamic acid with amorphous calcium silicate and silicon-dioxide (11). Volatile compounds such as naphthalene, d-camphor and p-cresol amorphized reported lost their volatility when co-ground with microcrystalline cellulose (MCC) (12). Amorphization of ibuprofen, sulfathiazole, phenothiazine, acridine, chloranil and vitamin K3 has been achieved by co-grinding with polyvinylpyrrolidone (13–15). Amobarbital amorphized in the presence of variety of excipients such as carbon black, ethyl cellulose, precipitated silica and activated charcoal (16). A variety of excipients such as β-cyclodextrins, dextrans, chitin, chitosan, gelatin, polyethylene glycol, methyl cellulose, hydroxy propyl cellulose, calcium silicate and silicon dioxide used to amorphize structurally diverse drugs resulted in various degrees of amorphization (8–18).
The amorphous solids generally revert to their lower energy, more stable, crystalline forms. There have been contradictory reports in the literature regarding the physical stabilization of amorphous solids using silicates. Kinoshita et al., showed that melt adsorption of a drug on Florite (amorphous calcium silicate) led to the formation of its amorphous state which was stable for 3 days at 60°C/80% RH and at least 2 years at ambient temperature and humidity (1). Watanabe et al., however, reported the reversion of amorphous indomethacin co-ground with silica at 30°C/11% RH in 10 days (2). Gupta et al. found that the amorphous drugs formed by co-grinding with Neusilin US2 (magnesium aluminometasilicate) were physically stable for at least 4 weeks at 40°C/75% RH (19).
Konno et al. have reported spontaneous amorphization of crystalline drugs stored (as a physical mixture) with silica (20). Since the amorphous form of the drug is associated with higher energy than its crystalline counterpart, spontaneous amorphization is an intriguing phenomenon. Attempts have been made to correlate the amorphization of the drugs by co-grinding, simple mixing and fusion with the porous nature of the excipients (21,22). Kim et al. used porous and non-porous silicas to make amorphous solids by physical mixing and fusion. They suggested that amorphization and the subsequent stabilization of the amorphous state is dependent upon the porosity of the silicate (21). However, the silicates used in their study differed from each other with respect to pH and surface area as well as porosity.
Neusilin US2 is amorphous magnesium aluminometasilicate with a high specific surface area (300 m2/g) (23). Like many complex silicates, the surface of Neusilin US2 has different types of silanols, which make it a potential proton donor as well as a proton acceptor. The hydrogen bonding potential of silanols on Neusilin US2 (19,24,25) and of silicas (2,26,27) in general, has been reported. The hydrogen bonding interaction between drugs and silanols seems to be facilitated during co-grinding (2,19).
In the present study, we report on the effects of the ratio of indomethacin to Neusilin US2 and the processing humidity on the amorphization kinetics during co-grinding. The percent crystallinity of the resulting co-ground powders was monitored by attenuated total reflectance Fourier transform infrared (ATR-FTIR) spectroscopy. Changes in the ATR-FTIR spectra also provided insight into the nature of the indomethacin-silicate interaction. The physical stability of the co-ground powders was studied at 40°C/75% RH and 40°C/0% RH.
Materials
Indomethacin USP, 1-(p-chlorobenzoyl)-5-methoxy-2-methylindole-3-acetic acid, as the γ-polymorph, was purchased from Spectrum Chemicals (New Brunswick, NJ). Neusilin US2, amorphous magnesium aluminometasilicate, was obtained as a gift sample from Fuji Chemicals (Englewood, NJ).
Methods
General Description of the Co-Grinding Process
A rolling jar mill (Model #202421, Paul O. Abbe Inc., Little Falls, NJ) consisting of a cylindrical porcelain jar (outer diameter = 5.25”; internal volume = 1,000 ml) and zirconia balls (outer diameter = 0.25”) was used to affect conversion of the physical mixtures of indomethacin and Neusilin US2. The cylindrical jar was filled with zirconia balls up to 600 ml of its total internal volume which gives a ball charge of ∼40% v/v. The gasket between the lid and the jar ensured a well-sealed system during co-grinding. The speed of rotation of the cylindrical jar was 85 rpm. In each experiment 48 g of powder (indomethacin-Neusilin US2) was added to the jar. This jar milling process is a much less energy intensive in comparison to high energy ball milling. No increase in the temperature was noted within the sensitivity of ±1°C during the grinding process.
All co-grinding experiments were performed in triplicate at room temperature utilizing the two processing humidities. At 0% RH, the porcelain jar, zirconia balls and Neusilin US2 were stored in an oven at 175°C for 24 h followed by equilibration at room temperature at 0% RH in a glove box for 24 h. Indomethacin was equilibrated at room temperature at 0% RH in a glove box for 36 h. Nitrogen gas was purged in the glove box to maintain 0% RH. At 75% RH, indomethacin, Neusilin US2, porcelain jar and zirconia balls were equilibrated at room temperature at 75% RH in a glove box for 36 h using a saturated NaCl solution to maintain 75% RH. The humidity inside the glove box was monitored using a hygrometer (Model LAM 880D, Mannix, Lynbrook, NY).
Preparation of Melt-Quenched Amorphous Indomethacin
The melting point of the γ-polymorph of indomethacin is 162°C (28). The amorphous state of γ-indomethacin was prepared by melting indomethacin at 168°C and holding the melt at 168°C for 2 min followed by quench-cooling in liquid nitrogen. The amorphous state was confirmed by absence of birefringence under cross-polarized light and by powder X-ray diffraction (PXRD) studies.
Powder X-Ray Diffraction (PXRD) Studies
X-ray diffraction patterns of pure crystalline γ-indomethacin, melt-quenched amorphous indomethacin and indomethacin co-ground with Neusilin US2 were obtained using a diffractometer (Model D5005, Bruker AXS Inc., Madison, WI) using CuKα radiation, a voltage of 40 kV, and a current of 40 mA. The scanning rate was 20/min over a 2θ range of 10–400 with a sampling interval of 0.020.
Quantification of Indomethacin Crystallinity in the Presence of Neusilin US2 using Attenuated Total Reflectance Fourier Transform Infrared (ATR-FTIR) Spectroscopy
Co-grinding indomethacin with Neusilin in the ratio 1:5 at 75% RH completely amorphized indomethacin in 5 days. Further co-grinding for an additional 5 days did not result in any change in crystallinity of indomethacin. Therefore, indomethacin co-ground with Neusilin US2 in the ratio 1:5 at 75% RH for 10 days was used as a standard for co-ground amorphous indomethacin. Mixtures of this co-ground amorphous indomethacin and crystalline indomethacin (0, 10, 30, 50, 70, 90 and 100% w/w crystallinity) with Neusilin US2 in the weight ratio of indomethacin to Neusilin US2 1:5 were used to generate a standard curve. All samples were prepared in triplicate. One hundred scans were recorded and averaged on an IR spectrophotometer (Model Magna IR 560, Nicolet Instruments Technologies Inc.,Westbury, WI) with golden gate ATR assembly equipped with diamond-ZnSe crystal using OMNIC® software. The scans were collected at 1 cm−1 resolution over a wave number region 4000–650 cm−1 using a mercury-cadmium-telluride (MCT) detector. Dry CO2 free air was purged throughout data acquisition. A chemometric technique (partial least squares) was utilized to generate the standard curve using TQ-ANALYST® software. Each infrared (IR) spectrum obtained was corrected for baseline and divided by the height (intensity) of the peak at 1477 cm−1. The changes in the regions 1727–1700, 1492–1479, 1476–1463 and 1367–1356 cm−1 were used to quantify percent crystallinity. The standard curve was validated and cross-validated to check its accuracy and precision. The predicted and actual percent crystallinities of the validation samples along with the standard deviations are given in Table I. Content uniformity of the standards was confirmed for samples corresponding to 10, 50 and 90% crystallinity. The standard deviation among samples withdrawn from the top, middle, and bottom of the sampling vials ranged from 0.2 to 1.2% crystallinity.
Investigation of the Effect of Ratio of Indomethacin to Neusilin US2
Powder mixtures of indomethacin to Neusilin US2 (n = 3) in ratios of 1:0.1, 1:0.15, 1:0.3, 1:0.5, 1:1, 1:2, 1:3, 1:4 and 1:5 by weight were co-ground at 75% RH condition. The powders were sampled every 2 h for 6 h followed by every 6 h for 24 h followed by every 24 h for 3 days and then at suitable time points until complete amorphization of indomethacin was achieved. The samples were analyzed by ATR-FTIR and PXRD as described above.
Investigation of the Effect of Processing Humidity
Powder mixtures of indomethacin to Neusilin US2 (n = 3) in ratios of 1:1, and 1:5 by weight were co-ground at 0% RH condition for 3 days. The powders were sampled every 2 h for 6 h followed by every 6 h for 24 h and then every 24 h until 3 days of co-grinding. Quantification of the percent crystalline fraction remaining in the samples was performed chemometrically using ATR-FTIR.
Physical Stability of Stored Samples
Samples co-ground to various extents of amorphization were studied to evaluate the effect of incomplete versus complete amorphization on physical stability of the co-ground powders. Samples co-ground at 75% RH were stored in open glass vials in jars in an oven (Model 1350 FM, VWR Scientific Products, Cornelius, OR) maintained at 40°C for 3 months. A saturated NaCl solution was used to maintain 75% RH in the jars. The samples co-ground at 0% RH condition were stored in open vials in jar in oven maintained at 40°C for 6 months. Phosphorous pentoxide was used to maintain 0% RH in those jars. Samples were taken periodically and analyzed for percent crystallinity by ATR-FTIR. PXRD of the initial and stored co-ground powders were compared to evaluate corresponding changes in X-ray diffraction pattern.
Results and Discussion
Evaluation of Amorphized Indomethacin by PXRD and FTIR
Figure 1A shows the X-ray powder diffraction patterns of crystalline indomethacin, melt-quenched amorphous indomethacin, co-ground amorphous indomethacin and Neusilin US2. The diffraction peaks for crystalline indomethacin are in accordance with the γ-polymorph (28). A broad halo at ∼20° 2θ for both melt-quenched indomethacin as well as co-ground indomethacin confirmed their amorphous nature. Preliminary experiments were performed to evaluate the feasibility of using powder X-ray diffraction (PXRD) as a technique for quantification of the percent crystallinity of indomethacin in the mixture of indomethacin and Neusilin US2 (magnesium aluminometasilicate). The results (Fig. 2) indicated significant attenuation of the X-ray diffraction intensity of crystalline indomethacin by Neusilin US2. For example, PXRD scans could not differentiate 1 day co-ground indomethacin from 2 days co-ground indomethacin. Thus PXRD lacked sensitivity required for quantification of crystalline fraction of indomethacin in the presence of the amorphous silicate.
The FTIR scans of crystalline indomethacin, melt-quenched amorphous indomethacin, co-ground amorphous indomethacin and Neusilin US2 are shown in Fig. 1B. Indomethacin exists as dimers in both crystalline and melt-quenched amorphous states. The dimer peak for crystalline and melt-quenched amorphous state of indomethacin is at 1710−1 and 1704 cm−1, respectively, while the benzoyl carbonyl peak occurs at 1690−1 and 1676 cm−1, respectively. In addition the melt-quenched amorphous indomethacin exhibits the free acid carbonyl peak at 1735 cm−1. These findings are consistent with previous reports (29). For co-ground amorphous indomethacin, the peaks corresponding to the dimer as well as the free acid carbonyl were absent. Thus ATR-FTIR technique differentiated between the two states of amorphous indomethacin that both appeared X-ray amorphous (Fig. 1B) The inability to differentiate between the two types of amorphous states coupled with the poor sensitivity of PXRD led us to utilize attenuated total reflectance Fourier transform infrared (ATR-FTIR) spectroscopy to quantify percent crystallinity of indomethacin in mixtures with Neusilin US2. The ATR-FTIR technique proved to be a more sensitive for quantification of crystalline fraction of drug. Figure 2 shows that FTIR was far better at distinguishing between the various degrees of amorphization during grinding. Furthermore, Neusilin US2 does not absorb in the carbonyl region of the FTIR spectrum. These two observations may lead to the increased sensitivity of FTIR over PXRD in the presence of the amorphous silicate.
Effect of Ratio of Indomethacin to Neusilin US2 on Amorphization Kinetics during Co-Grinding
Indomethacin was co-ground with Neusilin US2 in a 1:5 weight ratio at 75% RH. Figure 2 shows that the crystallinity of indomethacin decreased with time of co-grinding. Complete amorphization of indomethacin was achieved by co-grinding with Neusilin US2 for 5 days. A stability-indicating HPLC assay on a sample of indomethacin co-ground with Neusilin US2 in the ratio 1:5 for 12 days (more than twice the time for complete amorphization) showed 97.4% indomethacin remaining. So, it is unlikely that the 2.6% of degradation products affects the amorphization process or FTIR spectra significantly. While complete amorphization of indomethacin co-ground in 1:5 mixture with Neusilin US2 was achieved in 5 days, no amorphization was achieved by grinding indomethacin in the absence of Neusilin US2 for 14 days either at 75% RH or at 0% RH. In the absence of Neusilin US2, recrystallization of any disordered indomethacin due to low Tg (42°C) and long grinding time (14 days) is possible. However, Neusilin US2 appeared to stabilize any amorphous indomethacin formed during co-grinding. It is also possible that amorphization of indomethacin by co-grinding with Neusilin US2 could be mediated by vapor-phase transport of the drug to the surface of Neusilin US2 as found by other investigators (20). In either case, the presence of Neusilin US2 is key to the stable amorphization that we observe. It is also worth noting that there was significant densification of the powder on co-grinding indomethacin with Neusilin US2 along with a reduction of specific surface of the powder from 300 initially to 30 m2/g after 5 days of co-grinding.
The plots of percent crystallinity versus time for various ratios of indomethacin to Neusilin US2 co-ground at 75% RH are shown in Fig. 3a and b. Amorphization is faster in the presence of larger proportions of Neusilin. A faster initial amorphization rate (within the first 6 h) followed by slower amorphization kinetics was observed when the amount of Neusilin was greater (Fig. 3a). This two step amorphization was also reported by Kim and co-workers when a low melting point (∼53°C) NSAID was gently mixed with porous silica and stored at 25°C (21). Biphasic amorphization suggests a change in the mechanism of interaction of the drug with the silicate. An examination of the “goodness of fit” parameters for each FTIR spectrum with the standards (crystalline and co-ground amorphous indomethacin) showed no significant differences in fit parameters as a function of co-grinding time. This initial examination by FTIR did not reveal any differences in the interactions of indomethacin with Neusilin US2 in the fast and slow amorphization phases. The possibility of high and low energy sites on silicates will be investigated. It should be noted that this biphasic amorphization behavior was not observed when lower amounts of Neusilin were co-ground with indomethacin (Fig. 3b).
The time taken to achieve 0% crystallinity increased from 5 to 10 days as the ratio of indomethacin co-ground with Neusilin US2 was changed from 1:5 to 1:0.5. The dependence of amorphization time on indomethacin to Neusilin US2 ratio is a key factor in optimizing both the formulation and processing time to reliably produce X-ray amorphous indomethacin using Neusilin US2. Degradation, as determined by a stability-indicating HPLC assay on a sample of indomethacin co-ground with Neusilin US2 in the ratio 1:0.5 for 17 days (70% longer than the time for complete amorphization) was below the limits of detection, so the phenomenon is not complicated by chemical degradation. A critical ratio of indomethacin to Neusilin US2 above which complete amorphization is not possible appears to lie between 1:0.3 and 1:0.5 (Fig. 3b). This ratio is a measure of the total amorphization capacity of the Neusilin US2 (including the apparent “high energy sites” occupied initially and the remaining sites on the silicate that are more slowly filled assuming an adsorption mechanism).
The extent of amorphization during the initial fast amorphization phase increased with increasing level of Neusilin US2 suggesting a capacity of the presumably high energy sites. Table II shows the capacity of Neusilin US2 to rapidly amorphize indomethacin appears to be about 1–2 g of indomethacin per 10 grams of Neusilin US2 regardless of the initial ratio. The determination of both the critical ratio beyond which complete amorphization does not occur and the fast amorphization capacity further aid in the optimization of formulation design and reduction in processing time of the co-ground drug silicate mixtures.
Effect of Processing Humidity on Amorphization Kinetics during Co-Grinding
The effect of processing humidity on amorphization kinetics during co-grinding indomethacin with Neusilin US2 in the ratio 1:1 and 1:5 is shown in Fig. 4a and b. The results indicate facilitation of amorphization at higher humidity. The effect is more pronounced at the lower ratio of indomethacin to Neusilin US2. Water is known to act as a plasticizer and increase the mobility of amorphous solids, usually causing reversion to lower energy crystalline forms (30,31). However, since the present system is not a neat amorphous system, moisture may simply increase the mobility of indomethacin (32), thereby facilitating its interaction with Neusilin US2. Since there is no apparent reversion to the crystalline state during processing, one might conjecture that the co-ground amorphous (presumably Neusilin-bound) state is a lower free energy state than the crystalline state. However, preliminary studies show that solubility of the co-ground amorphous indomethacin is higher than crystalline indomethacin. Watanabe and co-workers similarly reported enhanced solubility of indomethacin co-ground with Aerosil-200 (7).
It should be noted that sometimes during co-grinding, the powder formed a cake at one end of the jar or the other, rather than remaining in the interstices between the zirconia balls. When it appeared, the cake was broken by applying gentle pressure with a spatula before co-grinding further. Cake formation was, however, not dependent on the processing humidity or the ratio of indomethacin to Neusilin US2. No significant differences in amorphization kinetics were noted for those samples in which there was cake formation. Konno and co-workers suggested that the amorphization of drugs was mediated by vapor phase mass transfer (20). This mechanism is further supported by the spontaneous amorphization of drugs physically mixed with silicates reported by Kim et al. (21) and Gupta et al. (19). The lack of a significant change in amorphization kinetics associated with cake formation in the present system also suggests that the amorphization could be mediated at least in part by vapor phase mass transfer. However, if vapor phase mass transfer alone were the sole means of amorphization, it is unlikely that the humidity would have resulted in an increase in amorphization kinetics. Indeed, Gupta and co-workers found that humidity increased the amorphization of ketoprofen physically mixed with Neusilin US2. They suggested that water was the medium for amorphization even in the static sample, presumably by particle–particle surface migration of drug. Thus, three pathways for amorphization are possible: 1) plasticization of transiently amorphous drug to allow easier mechanical transfer of drug to the silicate; 2) vapor-phase mass transfer; and 3) particle–particle surface migration of drug to the silicate.
Stability Studies
Indomethacin co-ground with Neusilin US2 in a 1:1 ratio at 75% RH condition was stored at 40°C/75% RH. The results over a period of 3 months of storage are shown in Fig. 5a. The 1:1 co-ground amorphous indomethacin was stable for 3 months. XRPD of 1:1 co-ground amorphous indomethacin did not show any peaks in the stored samples, further confirming the absence of reversion to the crystalline state. However, samples corresponding to ∼30% initial crystallinity (co-ground for 3 days) showed reversion to ∼60% crystallinity in 1 month and thereafter remained unchanged. The sample corresponding to ∼70% initial crystallinity (co-ground for 12 h) also plateaus around ∼60% crystallinity. Samples with ratios of 1:4 and 1:5 were similarly co-ground at 75% RH and stored at 40°C/75% RH. However, partially amorphous 1:4 and 1:5 samples showed further spontaneous amorphization upon storage. It appears that the ratio of drug to silicate dictates whether any remaining crystalline drug serves to seed reversion or is spontaneously amorphized. It should be noted that the standard deviations of the partially crystalline samples (Fig. 5) stored at 40°C/75% RH are higher than the standard deviations inherent in the method (Table I). The high standard deviation (Table III) is due to batch to batch variability of percent crystallinity among three batches. When individual batches were followed (Table III), the spontaneous amorphization of the 3-day co-ground sample is unambiguous. Similar spontaneous amorphization has been reported for crystalline mixtures of both aspirin and phenacetin mixed with Neusilin UFL2 in the ratio 1:4 within 14 days at 25°C (20). There are no obvious molecular-level explanations for these observations.
The stability data for indomethacin co-ground with Neusilin US2 in 1:1 ratio at 0% RH and stored at 40°C/0% RH are shown in Fig. 6. There is a decrease in the crystallinity of partially amorphized samples on storage for 2 months. However, between 2 and 6 months, there is an increase in the crystallinity. It is not clear at this point whether the reversion to crystallinity is due to the processing condition, the storage condition, or the initial extent of amorphization.
The powders which were completely amorphous remained stable irrespective of the ratio of indomethacin to Neusilin US2. This is in contrast to the findings by Watanabe et al. where reversion of indomethacin co-ground at a ratio of 1:1 with Aerosil-200 (specific surface of 200 m2/g) was observed at 30°C/11% RH (2). They attributed incomplete grinding to be the cause of recrystallization whereby the remaining crystalline indomethacin served as seeds for recrystallization. However, in a later study, similarly processed samples were shown to be fully amorphous by 29Si solid state NMR (7). In addition, the specific surface and nature of the silicate were different in those studies than in the present study. Still, it is notable that Watanabe and co-workers reported 10% reversion of a presumably completely amorphized sample at 60 days of storage at 30°C/11% RH, whereas the present findings are no reversion at 90 days of storage at a more extreme condition of 40°C/75% RH.
Interaction of Indomethacin with Neusilin US2
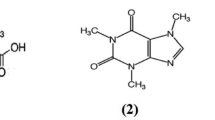
ATR-FTIR was used to investigate the interaction between indomethacin and Neusilin US2. In the region 1727–1700 cm−1, the absorbance of the dimer peak of indomethacin at 1710 cm−1 decreased upon co-grinding. The dimer peak was absent in completely amorphous indomethacin obtained by co-grinding (Fig. 8). Zografi et al., reported an absence of the peak in the 1710 cm−1 region for the sodium salt of indomethacin (33,34). A similar absence of the peak in the 1710 cm−1 region for indomethacin co-ground with Neusilin US2 might suggest the possibility of salt formation. However, interactions between tetracycline and metal ions present at the surface of an aluminum or iron hydrous oxide are well documented (35). Thus, in the present system, an ion-dipole interaction (rather than salt formation) between the Mg2+ and/or Al3+ ions at the surface of Neusilin US2 and the carboxyl group of the indomethacin could explain the changes in the 1727–1700 cm−1 region of the FTIR spectrum. Alternatively, the interaction with the carboxyl group could simply be a hydrogen bond with the silanols that are known to populate the surfaces of silicates (20). In addition, there are changes in the 1367–1356 cm−1 region of the spectrum (Fig. 8) which have been assigned to the C9H34,35 wagging (refer to Fig. 7) (36). Interaction of Neusilin with the carboxyl group (C36) would affect the charge densities of C–H bonds at C9H34,35, thereby causing the absorbance in 1367–1356 cm−1 region to change. This further suggests an interaction with the carboxyl group.
There is a shoulder in the FTIR spectrum of crystalline indomethacin at 1471 cm−1 which has been assigned to C12–C17 deformation (Fig. 8) (36). The absorbance of this shoulder decreased as a function of time of co-grinding. Hydrogen bonding between the benzoyl carbonyl and silanols of Neusilin US2 has the potential to affect the charge distribution at C12–C17. This implies that the benzoyl carbonyl is another possible site of interaction with Neusilin US2. Furthermore, the 1492–1479 cm−1 region in the FTIR spectrum is attributed to in plane C–H stretching for C13, C14, C16 and C17 of indomethacin (Fig. 7) (36). A change in the absorbance in this region was also observed upon co-grinding indomethacin with Neusilin US2 (Fig. 8). This provides additional evidence for an interaction of silanols of Neusilin US2 with the benzoyl carbonyl group.
Conclusion
Amorphous drugs, while more soluble, are often less preferred over their crystalline counterparts due to issues of poor chemical and physical stability. This, in turn, has reduced their commercial utility. In the present study various aspects relating to the successful manufacture of amorphous drugs have been investigated. Increasing the amount of Neusilin US2 with respect to indomethacin was shown to reduce the amorphization time. Further higher humidity facilitated amorphization. Most notably, indomethacin co-ground with Neusilin in three ratios (1:1, 1:4, and 1:5) were stable over a period of 3 months at 40°C/75% RH. Thus co-grinding with Neusilin US2 has been shown as a potential strategy to manufacture physically stable indomethacin. Several potential interactions between indomethacin and the surface of Neusilin are responsible for the physical stabilization of amorphous indomethacin co-ground with Neusilin US2.
The spontaneity of amorphization of indomethacin with Neusilin US2 suggests that the chemical potential of indomethacin is lower in co-ground mixtures than in pure indomethacin. Therefore, the term “amorphization” may not be appropriate for drug-silicate solid dispersion since the neat amorphous state is a higher energy state. However, co-ground indomethacin is X-ray amorphous and leads to higher solubility as compared to crystalline indomethacin; this is consistent with the amorphous form. There are two explanations in the literature for the phenomenon currently denoted “amorphization” in drug-silicate solid dispersions, adsorption (2,19,37,38) and confinement in mesopores (21,22). The term amorphous would certainly be more appropriate for stabilization of disordered drugs in mesopores than simple adsorption. More research is necessary to clarify the nature of the co-ground X-ray amorphous state.
References
M. Kinoshita, K. Baba, A. Nagayasu, K. Yamabe, T. Shimooka, Y. Takeichi, M. Azuma, H. Houchi, and K. Minakuchi. Improvement of solubility and oral bioavailability of a poorly water soluble drug, TAS-301, by its melt-adsorption on a porous calcium silicate. J. Pharm. Sci. 91:362–370 (2002).
T. Watanabe, N. Wakiyama, F. Usui, M. Ikeda, T. Isobe, and M. Senna. Stability of amorphous indomethacin compounded with silica. Int. J. Pharm. 226:81–91 (2001).
K. Y. Yang, R. Glemza, and C. I. Jarowski. Effects of amorphous silicon dioxides on drug dissolution. J. Pharm. Sci. 68:560–565 (1979).
E. Yonemochi, S. Kitahara, S. Maeda, S. Yamamura, T. Oguchi, and K. Yamamoto. Physicochemical properties of amorphous clarithromycin obtained by grinding and spray drying. Eur. J. Pharm. Sci. 7:331–338 (1999).
S. Byrn et al., Solid State Chemistry of Drugs, Second ed., 25, 1999.
B. C. Hancock,and M. Parks. What is the true solubility advantage for amorphous pharmaceuticals. Pharm. Res. 17:397–404 (2000).
T. Watanabe, S. Hasegawa, N. Wakiyama, A. Kusai, and M. Senna. Prediction of apparent equilibrium solubility of indomethacin compounded with silica by C13 solid state NMR. Int. J. Pharm. 248:123–129 (2002).
H. Takeuchi, S. Nagira, H. Yamamoto, and Y. Kawashima. Solid dispersion particles of amorphous indomethacin with fine porous silica particles by using spray drying method. Int. J. Pharm. 293:155–164 (2005).
M. Fujii, H. Okada, Y. Shibata, H. Teramachi, M. Kondoh, and Y. Watanabe. Preparation, characterization, and tabletting of a solid dispersion of indomethacin with crospovidone. Int. J. Pharm. 293:145–153 (2005).
T. Watanabe, S. Hasegawa, N. Wakiyama, A. Kusai, and M. Senna. Comparison of polyvinylpyrrolidone and silica nanoparticles as carriers for indomethacin in a solid state dispersion. Int. J. Pharm. 250:283–286 (2003).
A. S. Ali, K. Yamamoto, A. M. El-sayed, F. S. Habib, and Y. Nakai. Molecular behavior of flufenamic acid in physical and ground mixtures with florite. Chem. Pharm. Bull. 40:1289–1294 (1992).
Y. Nakai, E. Fukuoka, S. Nakajima, and Y. Iida. Effect of grinding on physical and chemical properties of crystalline medicinals with microcrystalline cellulose. II. Retention of volatile medicinals in ground mixture.Chem. Pharm. Bull. 26:2983–2989 (1978).
H. Sekizaki, K. Danjo, H. Eguchi, Y. Yonezawa, H. Sunada, and A. Otsuka. Solid-state interaction of ibuprofen with polyvinylpyrrolidone. Chem. Pharm. Bull. 43:988–993 (1995).
V. V. Boldyrev, T. P. Shakhtshneider, L. P. Burleva, and V. A. Severtsev. Preparation of the disperse systems of sulfathiazole-polyvinylpyrrolidone by mechanical activation. Drug Dev. Ind. Pharm. 20:1103–1114 (1994).
N. Kaneniwa and A. Ikekawa. Solubilization of water insoluble organic powders by ball milling in the presence of polyvinylpyrrolidone. Chem. Pharm. Bull. 23:2973–2986 (1975).
N. Kaneniwa, A. Ikekawa, and M. Sumi. A decrease in crystallinity of amobarbital by mechanical treatment in the presence of the diluents. Chem. Pharm. Bull. 26:2734–2743 (1978).
M. Cirri, F. Maestrelli, S. Furlanetto, and P. Mura. Solid state characterization of glyburide cyclodextrin co-ground products. J. Therm. Anal. Calorim. 77:413–422 (2004).
T. P. Shakhtshneider, M. A. Vasiltchenko, A. A. Politov, and V. V. Boldyrev. The mechanochemical preparation of solid disperse systems of ibuprofen-polyethylene glycol. Int. J. Pharm. 130:25–32 (1996).
M. K. Gupta, A. Vanwert, and R. H. Bogner. Formation of physically stable amorphous drugs by milling with Neusilin. J. Pharm. Sci. 92:502–517 (2003).
T. Konno, K. Kinuno, and K. Kataoka. Physical and chemical changes of medicinals in mixtures with adsorbents in the solid state. I. Effect of vapor pressure of the medicinals on changes in crystalline properties. Chem. Pharm. Bull. 34:301–307 (1986).
K. H. Kim, M. J. Frank, and N. L. Henderson. Application of differential scanning calorimetery to the study of solid drug dispersions. J. Pharm. Sci. 74:283–289 (1985).
T. Oguchi, et al., Improved dissolution of naproxen from solid dispersions with porous additives. Yakuzaigaku 57:168–173 (1997).
C. Fuji. Company Literature on Neusilin. Fuji Chemical Industry, Toyama, Japan, 1997, pp 3–4.
M. K. Gupta, R. H. Bogner, D. Goldman, and Y. C. Tseng. Mechanism for further enhancement in drug dissolution from solid-dispersion granules upon storage. Pharm. Dev. Technol. 7:103–112 (2002).
M. K. Gupta, Y. C. Tseng, D. Goldman, and R. H. Bogner. Hydrogen bonding with adsorbent during storage governs drug dissolution from solid-dispersion granules. Pharm. Res. 19:1663–1672 (2002).
I. S. Chuang and G. E. Maciel. Probing hydrogen bonding and the local environment of silanols on silica surfaces via nuclear spin cross polarization dynamics. J. Am. Chem. Soc. 118:401–406 (1996).
I. S. Chuang and G. E. Maciel. A detailed model of local structure and silanol hydrogen bonding of silica gel surfaces. J. Phys. Chem. B 101:3052–3064 (1997).
M. O'Brien, J. McCauley, and E. Cohen. Indomethacin. In H. G. Brittain (ed.), Analytical Profiles of Drug Substances, Volume 13, Academic, London, UK, 1984, pp. 211–238.
L. S. Taylor and G. Zografi. Spectroscopic characterization of interactions between PVP and indomethacin in amorphous molecular dispersions. Pharm. Res. 14:1691–1698 (1997).
K. J. Crowley and G. Zografi. Water vapor absorption into amorphous hydrophobic drug/poly(vinylpyrrolidone) dispersions. J. Pharm. Sci. 91:2150–2165 (2002).
E. Y. Shalaev and G. Zografi. How does residual water affect the solid-state degradation of drugs in the amorphous state?. J. Pharm. Sci. 85:1137–1141 (1996).
V. Andronis and G. Zografi. The molecular mobility of supercooled amorphous indomethacin as a function of temperature and relative humidity. Pharm. Res. 15:835–842 (1998).
P. Tong and G. Zografi. Solid state characteristics of amorphous sodium indomethacin relative to its free acid. Pharm. Res. 16:1186–1192 (1999).
P. Tong and G. Zografi. A study of amorphous molecular dispersions of indomethacin and its sodium salt. J. Pharm. Sci. 90:1991–2004 (2001).
C. Gu and K. G. Kartikeyan. Interaction of tetracycline with aluminum and iron hydrous oxides. Environ. Sci. Technol. 39:2660–2667 (2005).
A. Jubert, N. E. Massa, L. L. Tevez and N. B. Okulik. Vibrational and theoretical studies of the non-steroidal anti-inflamatory drugs Niflumic [2-3((3-trifluoromethy;)phenylamino)-3-pyridinecarboxylic acid]; Diclofenac [[2-(2,6-dichlorophenyl)amino]-benzeneacetic acid] and Indometacin acids [1-(4-chlorobenzoyl)-5-methoxy-2-methyl-1H-indole-3-acetic acid]. Vibr. Spectrosc. 37:161–178 (2005).
P. Mura, et al., Investigation of the effects of grinding and co-grinding on physicochemical properties of glisentide. J. Pharm. Biomed. Anal. 30(2):227–237 (2002).
A. E. Aboutaleb et al., Enhancement of dissolution rate of meclozine HCl by co-grinding and loading onto certain adsorbents. Bull. Pharm. Sci. Assiut University, 25(1):7–14 (2002).
Acknowledgments
The authors gratefully acknowledge financial support from the Dane O. Kildsig Center for Pharmaceutical Processing Research. We are thankful to Mr. Gary Lavigne and Dr. Jack Gromek at the Institute of Material Sciences, University of Connecticut for assistance with FTIR instrument and X-ray diffractometer, respectively. We also want to thank Mr. Sharad Murdande at Pfizer, Groton, CT for his help with HPLC analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bahl, D., Bogner, R.H. Amorphization of Indomethacin by Co-Grinding with Neusilin US2: Amorphization Kinetics, Physical Stability and Mechanism. Pharm Res 23, 2317–2325 (2006). https://doi.org/10.1007/s11095-006-9062-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-006-9062-x






 1:1,
1:1,  1:4
1:4  1:5 B
1:5 B
 1:0.5,
1:0.5,  1:0.3,
1:0.3,  1:0.15
1:0.15  1:0.1.
1:0.1.
 0% RH
0% RH 
 12 h co-ground
12 h co-ground 
 72 h co-ground.
72 h co-ground.
