Purpose
Very few chemical enhancers for transdermal drug delivery have been approved for clinical use due to irritancy and toxicity concerns. Novel chemical enhancers (iminosulfuranes) were synthesized and studied for their activity and toxicity.
Methods
Skin was treated with 0.4 M 1–5 for 1 h before hydrocortisone was applied. Samples were taken over 24 h and analyzed by high-performance liquid chromatography. Dermal fibroblasts and epidermal keratinocytes were treated with 0–1.2 M 1–5 for 24 h and cytotoxicity assay [3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT)] was performed. Furthermore, enhancement activity of 0–0.4 M 2 was studied. Partition coefficient of the model drugs into stratum corneum (SC) was measured and confocal Raman microscopy was used to study the penetration process and possible mechanisms of action of the enhancers. Quantitative structure–activity relationship (QSAR) was analyzed to study the contribution of different intramolecular descriptors to enhancement activity.
Results
Iminosulfurane 2 showed the highest enhancement activity. All compounds below 0.2 M were safe to skin cells, and 2 was effective at the concentration of 0.1 and 0.2 M. Mechanisms of action of 2 may include increasing partition coefficient of the model drug into SC and interaction between the enhancer and lipids and protein in the SC. QSAR study indicated contribution of several factors to activity: partition coefficient, hydrogen-bond acceptor, and optimal molecular size.
Conclusions
Enhancement activity of 2 was achieved without any cytotoxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The transdermal route for systemic drug delivery has been extensively studied in the past 20 years. The advantages offered by this route of administration include, but are not limited to, avoidance of the hepatic first pass effect, zero-order absorption, controlled drug release, noninvasive drug delivery, and improved patient compliance. However, the drug candidates for transdermal administration are quite limited because of the significant barrier that the skin presents to most penetrants. The stratum corneum (SC) plays the key role in limiting the diffusion of various agents into deeper layer of the skin. Many different approaches have been used to overcome this barrier and facilitate drug permeation through the skin, including chemical modification (i.e., chemical enhancers) and physical disruption (e.g., iontophoresis, phonophoresis, electroporation, microneedles, etc.) (1–5).
One of the most promising and the most extensively studied techniques is the use of chemical enhancers. Many studies have investigated the mechanisms of action of chemical enhancers and the following have been suggested as possible explanations for activity: (1) interaction with intercellular lipids of the SC resulting in disorganization of the highly ordered structures thus enhancing the paracellular diffusivity through the SC; (2) interaction with intracellular proteins of the corneocytes to increase transcellular permeation; and (3) increasing partitioning of the drug into the SC.
The potent enhancing effect of dimethyl sulfoxide (DMSO) on skin penetration was first reported in 1964 (6), and the mechanisms of action may include solvent effect, lipid extraction and disruption, and protein configuration change (7, 8). The enhancement effect of DMSO was found to be concentration-dependent. It has been shown that when the DMSO concentration is 60% or above, the permeants can penetrate to the lowest layer of the SC within several minutes to several hours (9, 10). DMSO has been associated with a number of toxicity issues and irritancy problems, the extent of which were also concentration-dependent (11–13), and this made DMSO undesirable for further development as a percutaneous penetration enhancer.
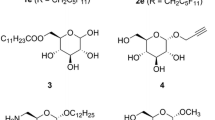
Studies on structure–activity relationships showed that the presence of a cyclic structure in the molecule plays an important role in determining the enhancement activity. Azone® (1-dodecylazacycloheptan-2-one), a derivative of caprolactam, is a very potent enhancer. Molecular modeling studies have suggested that the polar lactam functionality may interact with the lipid polar head groups. These groups would then be forced apart, an action that not only efficiently disrupts the lipid packing in the head group region, but alsoin the acyl chain region. In previous studies (14), 19 novel potential penetration enhancers were synthesized by introducing modifications to the DMSO molecule where the oxygen atom of DMSO was replaced by a nitrogen atom, which in turn was substituted with an arylsulfonyl, aroyl, or aryl group. Thus a cyclic structure was introduced to the molecule, which could potentially interact with the lipids in the stratum corneum such as Azone®. The polarity of these novel compounds could additionally be modulated by placing different substituents into the aromatic core of the molecule. As DMSO may cause irritancy at higher concentrations, these novel compounds were designed to be effective atlower concentrations, which would potentially result in less untoward side effects. Permeation studies using hairless mouse skinwere performed and the highest enhancement activity was obtained with N-(4-bromobenzoyl)-S,S-dimethyliminosulfurane (2) (14, 15). In the current study, further analogs of 2(Fig. 1) were synthesized and their enhancement effects and cytotoxicity were investigated.
Materials and Methods
Iminosulfuranes 1–5
Iminosulfurane 2 has been reported previously (14, 15). The analogs 1, 3–5 were synthesized in a similar way by treatment of DMSO with trifluoroacetic anhydride followed by the reaction of the resultant reagent [S,S-dimethyl-S-(trifluoroacetoxy)sulfonium trifluoroacetate] with an appropriate 4-substituted benzamide. After a general workup (14), compounds were purified by chromatography on silica gel eluting with dichloromethane/ethanol (up to 5% of ethanol) and crystallized: 1, dichloromethane; 3 and 4, dichloromethane/ether; and 5, hexanes. Iminosulfuranes 1–5 are crystalline colorless compounds. They are soluble in a variety of polar and nonpolar solvents, and their solutions remain stable for several months when stored under normal laboratory conditions. Elemental analyses given below were obtained at the Department of Chemistry, Georgia State University, on a Perkin-Elmer 240 CHN instrument. 1H NMR spectra were recorded at 400 MHz in deuteriochloroform.
N-(4-Fluorobenzoyl)-S,S-dimethyliminosulfurane (1)
This compound was obtained from 4-fluorobenzamide: yield, 80%; mp 128–130°C; 1H NMR δ 2.77 (s, 6H), 7.03 (m, 2H), 8.10 (m, 2H). Analysis: C9 H10 FNOS requires C, 54.27; H, 5.03; N, 7.04. Found: C, 54.25; H, 5.06; N, 7.03.
N-(4-Iodobenzoyl)-S,S-dimethyliminosulfurane (3)
This compound was obtained from 4-iodobenzamide: yield, 40%; mp 103–105°C; 1H NMR δ 2.77 (s, 6H), 7.70 (d, J = 9 Hz, 2H), 7.81 (d, J = 9 Hz, 2H). Analysis: C9 H10 INOS requires C, 35.19; H, 3.28: N, 4.56. Found: C, 35.50; H, 3.35; N, 4.67.
N-(4-Butylbenzoyl)-S,S-dimethyliminosulfurane (4)
This compound was obtained from 4-butylbenzamide: yield, 30%; mp 83–84°C; 1H NMR δ 0.92 (t, J = 7 Hz, 3H), 1.35 (m, 2H), 1.60 (m, 2H), 2.64 (t, J = 7 Hz, 2H), 2.77 (s, 6H), 7.17 (d, J = 8 Hz, 2H), 7.98 (d, J = 8 Hz, 2H). Analysis: C13 H19 NOS requires C, 65.78; H, 8.07; N, 5.90. Found: C, 65.60; H, 8.05; N, 5.95.
N-(4-Hexylbenzoyl)-S,S-dimethyliminosulfurane (5)
This compound was obtained from 4-hexylbenzamide: yield, 53%; mp 90–92°C; 1H NMR δ 0.92 (t, J = 7 Hz, 3H), 1.20–1.60 (m, 8H), 2.64 (t, J = 7 Hz, 2H), 2.77 (s, 6H), 7.19 (d, J = 8 Hz, 2H), 7.98 (d, J = 8 Hz, 2H). Analysis: C15 H23 NOS requires C, 67.88; H, 8.73; N, 5.28. Found: C, 67.99; H, 8.80; N, 5.21.
In Vitro Skin Permeation Studies with Enhancer Treatment
Male hairless mice of strain SKH1, 8 weeks old were obtained from Charles River Laboratories (Wilmington, MA, USA). Mice were euthanized with CO2 asphyxiation and their skins were excised and stored at −20°C until use. Dermatomed human cadaver skin (500 μm thick), collected from the abdominal region of different Caucasian donors, was obtained from the National Disease Research Interchange (Philadelphia, PA, USA) and stored at −80°C until use. Vertical Franz diffusion cells were purchased from Permegear, Inc. (Bethlehem, PA, USA), with a diffusional area of 0.64 cm2 and a receptor compartment volume of 5.1 mL.
The receptor compartment of Franz cells was filled with isotonic phosphate buffer (pH 7.4), which contained 2.68 mM KCl, 1.47 mM KH2 PO4, 136.89 mM NaCl, and 8.10 mM Na2 HPO4, with the temperature maintained at 32 ± 0.5°C. Skin was allowed to hydrate for 1 h followed by treatment with 2 μL of varying concentrations of enhancer solution in propylene glycol (PG) for 1 h. Then, 16.5 μL saturated suspension of the model drug (hydrocortisone or caffeine) in PG was applied to the skin. Saturated suspensions of model drugs were used to insure maximum thermodynamic activity and maintain sink conditions. Samples (300 μL) were taken from the receptor compartment over 24 h and were immediately replaced by the same volume of buffer solution. The samples were kept frozen at −20°C prior to high-performance liquid chromatography (HPLC) analysis. For all experiments, n = 5.
HPLC Methodology of Model Drugs
Samples were analyzed using a Hewlett Packard 1100 HPLC system with a diode array detector and a reverse phase C18-Microsorb column (15 cm × 4.6 mm, 5 μm; Varian, Inc., Palo Alto, CA, USA) operating at room temperature. For hydrocortisone, the mobile phase was a mixture of acetonitrile/water (40:60, v/v) with the flow rate of 1 mL min−1. Hydrocortisone was detected at 242 nm with the retention time of 3.5 min. For caffeine, the mobile phase was a mixture of methanol/water/acetonitrile (20:70:10, v/v/v) with the flow rate of 1 mL min−1. Caffeine was detected at 210 nm with the retention time of 3.5 min. The calibration curve was linear over the concentration range 0.5–500 μg mL−1 (R2 = 0.9999). The coefficient of variation for intra- and interday variation was below 3%.
Data Analysis for Permeation Studies
The parameters of the in vitro skin permeation studies were calculated by plotting the cumulative drug amount permeated through the skin vs. time. The slope of the linear portion of the permeation curve provided the flux value (J, μg cm−2 h−1) at steady state. The lag time (Tlag) was determined by extrapolating the linear portion of the curve to the X-axis. The cumulative drug amount in the receptor compartment after 24 h was defined as Q24 (μg cm−2). Enhancement ratio (ER) for flux were calculated using the following equation:
Statistical analysis of the data was performed using one-way analysis of variance (ANOVA, α = 0.05). A least significant different test (LSD) was followed if the ANOVA indicated that a difference existed. Log P values of the model drugs were determined using ACD program (Advanced Chemistry Inc., Ontario, Canada).
Cytotoxicity Assay
The 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay was used to determine the toxic effects of iminosulfuranes on dermal fibroblasts and epidermal keratinocytes in vitro. The MTT assay kit was purchased from Sigma (St. Louis, MO). The tetrazolium ring of MTT can be cleaved by mitochondial dehydrogenases in living cells and gives purple formazan crystals (16, 17). Skin cells (fibroblasts or keratinocytes) were transferred to the 96-well plate at 5000 cells in 200 μL medium per well. After 24 h, the cells were treated with varying concentrations of enhancer solution in culture medium with 1% DMSO (as vehicle) and incubated for 24 h at 37°C. The cells that were treated with culture medium containing 1% DMSO were used as control. Then the medium was replaced by fresh medium with 20 μL MTT solution (5 mg mL−1 in phosphate buffer) and the cells were incubated for 3 h. Then the medium was removed and 200 μL solubilization solution was added to dissolve the formazan crystals. The plate was incubated for 30 min while shaking. A plate reader (DV990; Zylux Corp., Oak Ridge, TN, USA) was used to measure absorbance at 595 nm.
Partition Coefficient of Model Drugs into the SC
The partition coefficient of model drugs into SC with or without enhancer treatment was determined following the method of Wester et al. (18). The epidermis was prepared by soaking dermatomed human cadaver skin in water at 60°C for 45 s (19). The skin was removed from water and the intact epidermis was teased off from the dermis. The SC was prepared by floating the epidermis (the SC side up) on an aqueous solution of trypsin (0.1% w/v) and sodium hydrogen carbonate (0.5% w/v) for 3 h at 37°C (20). The SC was then removed, rinsed with distilled water, dried, and was ready to use. The SC was pulverized in a mortar with a pestle containing dry ice. 10 mg ground SC was mixed by vortexing with 1 mL of 0.4 M 2 in PG containing 5% (w/v) of model drug. The control was treated with vehicle (PG) only. The mixture was shaken for 10 h at 37°C, centrifuged and the supernatant removed. The sediment was again resuspended in 1 mL of enhancer solution and immediately centrifuged to remove material adsorbed on the surface. The amount of drug in the supernatant was determined by HPLC. The amount of drug bound to the SC was obtained by subtracting the amount of drug in the supernatant from the total amount added. The partition coefficient, K, of model drug was calculated using the following equation:
Confocal Raman Microscopy for Enhancer Treated Human Cadaver Skin
Dermatomed human cadaver skin was treated with 0.4 M 2 in PG for 1 h and then cleaned by addition of hexane to remove any chemicals left on the surface. The skin was gently pressed into a cyclindrical opening machined in a brass block. The human cadaver skin without enhancer treatment was used as control. The spectra of 2 powder and 2 solution in PG were also recorded and used as references for band assignment.
Raman spectra were obtained with a Kaiser Optical Systems Raman Microprobe (Kaiser Optical Systems, Inc., Ann Arbor, MI, USA). The samples were placed under a Leica DMLP optical microscope. The excitation wavelength and the laser power on the samples were 785 nm and ∼4 mW, respectively, with a nominal spot size of ∼2 μm. A microscope objective (100×) was used to focus the laser light on the sample and to collect scattered light. A confocal mask was inserted into the collection fiber optic. The collected light was then filtered through a holographic notch filter and passed through a transmission grating. The spectra were recorded with a back-illuminated, deep depletion charge-coupled device (CCD) camera (1024 × 128 pixels; ANDOR Technology, South Windsor, CT, USA). The spectral coverage was 100–3450 cm−1. A video image of the sample was used to control the positioning of the laser spot on the sample. The exposure time was 60 s. The obtained data were converted into a multifile format using GRAMS/32 (Galactic Industries Corporation, Salem, NH, USA) and then loaded into Isys 3.0 (Spectral Dimensions, Olney, MD, USA) for analysis. Baseline corrections were made before peak heights were determined.
Quantitative Structure–Activity Relationship Study on Enhancers
Data from current and previous studies (14) with hydrocortisone as the model drug through hairless mouse skin were used as the training data set, and the enhancement ratio for flux was used as the dependent variable in quantitative structure–activity relationship (QSAR) analysis. A total of 77 intramolecular descriptors used in building QSAR models were calculated using Cerius2 (21). All QSAR models were built and optimized using multidimensional linear regression fitting and genetic function approximation (GFA), which is a multidimensional optimization method based on the genetic algorithm paradigm (22, 23). Linear representations of each of the descriptor values were included in the trial descriptor pool, and QSAR models were built as a function of the number of descriptor terms in a model. Statistical significance in the optimization of a QSAR model was judged by the correlation coefficient of fit, r2. In addition, GFA uses the Friedman's lack of fit (LOF) measure to resist overfitting, a problem often encountered in constructing statistical models (24). A total of 10,000 GFA generated calculations were conducted. Each GFA generation had partial least squares (PLS) applied to it instead of multiple linear regressions, and so each model could have more terms in it without danger of overfitting.
Results
Effects of Iminosulfuranes 1–5 on Percutaneous Permeation
In the preliminary study, male hairless mouse skin was used for comparison with the previous study. Compounds 1–5 (0.4 M) in PG were used as penetration enhancer and hydrocortisone was the model drug. A control experiment was run without any enhancer but with PG as the vehicle. The permeation parameters (flux, Q24, and lag time) are shown in Table I. Iminosulfuranes 2 and 5 showed statistically higher Q24 and flux values compared to those of the control (p < 0.05). Compound 2 produced the highest activity of all compounds tested in this study (ER = 11.9) and the lowest Tlag value. The permeation profile of the cumulative amounts of hydrocortisone penetrated through male hairless mouse skin over 24 h is presented in Fig. 2. It indicates that the enhancement effect of 2 was significant throughout the 24 h of the study. Mouse skin has been thought to be more permeable than human skin due to the differences in lipid composition and structure, and hence differs in permeability from human skin (25). The study with mouse skin was a preliminary study and was followed by a more detailed investigation using human cadaver skin.
The experimental conditions for the permeation study using human cadaver skin were the same as those used in the mouse study, and results are presented in Table II. Consistent with the results from hairless mouse skin, the results from human cadaver skin also showed that 2 and 5 produced statistically higher Q24 and flux values compared to those of control (p < 0.05). Compound 2 showed the highest activity (ER = 17.0) and the lowest Tlag value. Interestingly, 1 showed a slightly retardant effect in that the flux was statistically lower than that of control, whereas Q24 was not. The permeation profiles of hydrocortisone through human cadaver skin with 0.4 M enhancer treatment over 24 h are shown in Fig. 3. Similar to data from hairless mouse skin, 2 showed a significant enhancement effect over 24 h.
Cytotoxicity Effects of 1–5 on Skin Cells
Most penetration enhancers have been shown to produce skin irritation, hence few of them have been approved for clinical use. The cytotoxicity of 1–5 on epidermal keratinocytes and dermal fibroblasts was studied using MTT assay. Cells without treatment of enhancers were used as control and represented 100% viability. Results were expressed as percent of control. The results of fibroblasts and keratinocytes treated with various concentrations of 1–5 are shown in Fig. 4. Iminosulfuranes showed concentration-dependent cytotoxicity on both fibroblasts and keratinocytes. Except for 4, there was no significant decrease (p > 0.05) in cell viability for iminosulfuranes concentrations below 0.2 M, and 0.7–0.9 M solution produced 50% cell viability (IC50). The study indicated that concentrations below 0.2 M would produce negligible cytotoxicity for 1, 2, 3, and 5.
Further Studies on Penetration Enhancement Activity of Iminosulfurane 2
Lower concentrations of 2 within the safety limit (0.2 M) were chosen for permeation study using human cadaver skin. Meanwhile, the enhancement effects for both hydrophobic (hydrocortisone) and hydrophilic (caffeine) model drugs were tested. The log P values of hydrocortisone and caffeine were 1.43 ± 0.47 and −0.07 ± 0.35, respectively. The enhancement effects of different concentrations of 2 on percutaneous permeation of hydrocortisone and caffeine are presented in Fig. 5. Permeation profiles over 24 h are shown in Fig. 6. In summary, 2 showed a statistically significant enhancement effect for hydrocortisone at lower concentrations of 0.1 and 0.2 M, with ER of 1.7 and 6.0, respectively. For caffeine, 2 also showed an enhancement effect at low concentrations, but with a considerably lower enhancement ratio compared to hydrocortisone. This suggested that the enhancement effect of 2 could be obtained at lower concentrations without any accompanying major irritancy problem. Additionally, 2 was more potent in the case of the hydrophobic drug rather than the hydrophilic drug.
Effects of 2 on Partitioning of Model Drugs to the SC
The effects of 0.4 M 2 on partitioning of hydrocortisone and caffeine into the SC were studied to investigate the mechanisms of action of the enhancer. Results are shown in Table III. With 2 treatment, the partitioning of hydrocortisone and caffeine into the SC was 5.4- and 1.4-fold higher than control, respectively, which would indicate increased permeation.
Confocal Raman Microscopy of Human Cadaver Skin Treated with 2
Confocal Raman microscopy was used to study the penetration process and shed light on the possible mechanisms of action of the enhancer. Figure 7 shows the Raman spectra of full-thickness human cadaver skin, powder of 2, PG, and human cadaver skin treated with 0.4 M 2 in PG for 1 h over the range of 640–1050 cm−1. The peak at 1002 cm−1 arises from the ring stretching modes of phenylalanine and was used to identify skin, whereas the peak at 670 cm−1 was used to identify 2. Figure 8 plots intensity vs. penetration depth into the skin from the surface. The dotted line shows the intensity of the iminosulfurane normalized to the intensity of the Amide I vibration (mostly peptide bond C = O stretch) of the skin proteins. This parameter is assumed to be constant as one moves from the SC toward the epidermis. The similarity of the depth variation of this parameter to that of the solid line (iminosulfurane alone) shows that the observed intensity variation of the iminosulfurane is not an artifact of the confocal measurement, but a real diminution in concentration as the material progresses through the surface of the SC. The factor of 400 is introduced to obtain the ratio measurement on scale. The intensity of the skin Amide I mode is much greater than the iminosulfurane band. It shows that 2 penetrated through the SC (to depth of about 20 μm) with a maximum concentration at 5–10 μm from the skin surface. There was no significant penetration of 2 below 25 μm, indicating that: (1) the enhancer was probably bound to lipids and/or protein in the SC; (2) the enhancer did not penetrate into viable epidermis, which would indicate that if applied topically it may not be highly irritant because irritancy occurs only when chemicals are present in the viable epidermis and dermis.
QSAR Study on Enhancers
The optimized four-term linear QSAR models are given below. The definitions of the descriptors used in the models are given in Table IV.
There are four major structural factors of enhancer that seem to determine enhancement activity and reveal features of the enhancement mechanisms: (1) partition coefficient (AlogP), which indicates that skin penetration enhancement increases with increasing AlogP; (2) H-bond acceptor, which indicates that skin penetration enhancement increases with increasing the number of hydrogen bonding acceptors; (3) size, shape, and molecular flexibility of enhancers as represented by CHI, Shadow, and PHI descriptors that present both positive and negative contributions to enhancement in the QSAR models and indicate that there is a range of optimal molecular size that controls the maximum skin penetration enhancement; and (4) electrostatic, represented by Jurs partial charge surface area descriptors, Jurs-RNCG, and Jurs-RPCS, which relate to both polar properties and size of the enhancer molecule.
By inspecting the r2 values of QSAR models, two compounds were identified as outliers from the rest of training set. The major issue might come from the observation value range. These two compounds had ER value greater than 10; however, the ER value of other compounds was below 4. Further molecular similarity study is required to select representative compounds from the lower value pool to build a new QSAR model.
Discussion
Several new 4-substituted N-benzoyl-S,S-dimethyliminosulfuranes were synthesized. Among them, a bromo-substituted iminosulfurane 2 and a hexyl-substituted analog 5 are the most effective enhancers in both hairless mouse skin and human cadaver skin. The cytotoxicity study indicates that the enhancement action is independent of the toxic effect of the enhancer at lower concentrations (0.2 and 0.1 M), whereas for higher concentrations (0.4 M) the enhancers show only slightly cytotoxic effects. At nontoxic concentrations (0.2 and 0.1 M), 2 shows significant enhancement effects for both caffeine and hydrocortisone, although less for the former.
The solvent effect of 2 was examined and the results indicate that with enhancer treatment the partitioning of both the hydrophobic and hydrophilic drug tested in skin is increased. For hydrocortisone, the partition coefficient was increased by 5.4-fold by 0.4 M 2, whereas the flux was increased by 17.0-fold. Because flux is directly related with permeability coefficient, which in turn is proportional to partition coefficient and diffusion coefficient, the enhancement effect is partially a result of the solvent effect of the enhancer, and the other contribution may include the change in diffusivity across the skin, which can be affected by structural alteration of lipid and protein in the SC caused by enhancers. Tlag can also be related to diffusivity:
where h is the length of the permeation path and D is the diffusion coefficient. For hydrocortisone, Tlag was decreased by 7.4-fold by 0.4 M 2, which reflected changes in both h and D and suggested interaction of the enhancer with lipid and protein in the SC.
The key to promoting the permeation of drugs across the skin is to modify the properties of the principal pathways associated with drug penetration through the SC, i.e., the lipoidal intercellular pathway and the polar transcellular pathway. Hydrocortisone, which is a hydrophobic compound, favors the lipoidal intercellular pathway rather than the polar transcellular pathway, hence the results from the partitioning studies using hydrocortisone indicate that the enhancer interacts with the lipids of the SC. For caffeine, the partition coefficient was increased 1.4-fold by 0.4 M 2, whereas the flux increased by 5.3-fold. These results suggest that other mechanisms of action of the enhancer exist in addition to the solvent effect. As caffeine is a moderately hydrophilic drug, its permeation is probably taking place through the transcellular pathway. Results from partitioning studies using caffeine indicate possible interaction of the enhancer with the SC proteins.
Iminosulfurane 2 is a small, polar molecule. It may interact with lipids in the SC with the aromatic ring lying in the plane of the lipid polar head groups. These groups would then be forced apart, which not only efficiently disrupts the lipid packing at the head group region but also in the acyl chain region. It has been thought that the enhancement effect of DMSO is related to its polar O–S bond, which enables the compound to interact strongly with water by forming hydrogen bonds. This interaction with water is believed to be one of the key elements in the mechanism of action of DMSO as a penetration enhancer. It is thought that DMSO at low concentrations displaces protein bound water, and at high concentrations it displaces water surrounding the polar head groups of intercellular lipids of SC leading to poorer packing of the lipid hydrocarbon tails (27). The S–O functionality of DMSO and the S–N functionality of iminosulfuranes are isoelectronic. Due to the similarity in the structure of DMSO and 2, it was expected that these compounds might exert their action by similar mechanisms. The interaction of 2 with protein in the SC could be caused by replacing water molecules bound to polar protein side chains, resulting in conformational alterations of the keratinized proteins from α-helix to β-sheet.
The penetration of 2 was examined by confocal Raman microscopy. The results indicate that compound 2 penetrates through the SC (to a depth of about 20 μm), whereas the maximum concentration is observed at 5–10 μm from the skin surface. They also show that the enhancer remains primarily in the SC without any significant penetration into the viable epidermis. Studies by Fourier transform Raman spectroscopy of the interaction between DMSO and human SC have shown that the enhancement produced by DMSO not only changes the protein structure, but may also be related to alterations in SC lipid organization, in addition to any increased drug partitioning effects (28). Similar effects were expected for 2; however, further studies on molecular structure changes need to be performed.
The pilot QSAR analysis was conducted with compounds 1–5 and other iminosulfuranes previously studied (14, 15). Results revealed that enhancement activity is paralleled by hydrophobicity of the iminosulfuranes and the number of hydrogen bonding acceptors in the molecules. In addition, there is a range of optimal molecular size that controls the maximum enhancement.
Conclusions
In summary, the enhancement activity of iminosulfurane 2 is not accompanied by any cytotoxic effect. The mechanisms of action of dimethyliminosulfuranes probably include the solzvent effect that increases drug partitioning in the SC, interaction with lipids in the SC, and interaction with protein in the SC.
References
C. S. Asbill A. F. El-Kattan B. Michniak (2000) ArticleTitleEnhancement of transdermal drug delivery: chemical and physical approaches Crit. Rev. Ther. Drug Carrier Syst. 17 621–658 Occurrence Handle11204737
R. H. Guy (1998) ArticleTitleIontophoresis—recent developments J. Pharm. Pharmacol. 50 371–374 Occurrence Handle9625480
S. Henry D. V. McAllister M. G. Allen M. R. Prausnitz (1998) ArticleTitleMicrofabricated microneedles: a novel approach to transdermal drug delivery J. Pharm. Sci. 87 922–925 Occurrence Handle10.1021/js980042+ Occurrence Handle9687334
S. Mitragotri D. A. Edwards D. Blankschtein R. Langer (1995) ArticleTitleA mechanistic study of ultrasonically-enhanced transdermal drug delivery J. Pharm. Sci. 84 697–706 Occurrence Handle7562407
J. C. Weaver T. E. Vaughan Y. Chizmadzhev (1999) ArticleTitleTheory of electrical creation of aqueous pathways across skin transport barriers Adv. Drug Deliv. Rev. 35 21–39 Occurrence Handle10.1016/S0169-409X(98)00061-1 Occurrence Handle10837687
R. B. Stoughton W. Fritsch (1964) ArticleTitleInfluence of dimethylsulfoxide (DMSO) on human percutaneous absorption Arch. Dermatol. 90 512–517 Occurrence Handle14200645
T. Kurihara-Bergstrom G. L. Flynn W. I. Higuchi (1986) ArticleTitlePhysicochemical study of percutaneous absorption enhancement by dimethyl sulfoxide: kinetic and thermodynamic determinants of dimethyl sulfoxide mediated mass transfer of alkanols J. Pharm. Sci. 75 479–486 Occurrence Handle3735087
B. W. Barry (1987) ArticleTitleMode of action of penetration enhancers in human skin J. Control. Release 6 85–97 Occurrence Handle10.1016/0168-3659(87)90066-6
A. M. Kligman (1965) ArticleTitleTopical pharmacology and toxicology of dimethyl sulfoxide. 1 JAMA 193 796–804 Occurrence Handle14329978
T. M. Sweeney A. M. Downes A. G. Matoltsy (1966) ArticleTitleThe effect of dimethyl sulfoxide on the epidermal water barrier J. Invest. Dermatol. 46 300–302 Occurrence Handle5930898
E. Skog J. E. Wahlberg (1967) ArticleTitleEffect of dimethyl sulfoxide on skin. A macroscopic and microscopic investigation on human skin Acta Derm.-Venereol. 47 426–434 Occurrence Handle4168806
L. F. Montes J. L. Day C. J. Wand L. Kennedy (1967) ArticleTitleUltrastructural changes in the horny layer following local application of dimethyl sulfoxide J. Invest. Dermatol. 48 184–196 Occurrence Handle6020683
J. M. Shackleford K. L. Yielding (1984) ArticleTitleUltrastructural studies of barrier restoration in epidermis of hairless mice following dimethyl sulfoxide application J. Cutaneous Pathol. 11 259–268
N. Kim M. El-Khalili M. M. Henary L. Strekowski B. B. Michniak (1999) ArticleTitlePercutaneous penetration enhancement activity of aromatic S,S-dimethyliminosulfuranes Int. J. Pharm. 187 219–229 Occurrence Handle10.1016/S0378-5173(99)00194-5 Occurrence Handle10502628
L. Strekowski M. Henary N. Kim B. B. Michniak (1999) ArticleTitleN-(4-Bromobenzoyl)-S,S-dimethyliminosulfurane, a potent dermal penetration enhancer Bioorg. Med. Chem. Lett. 9 1033–1034 Occurrence Handle10.1016/S0960-894X(99)00131-6 Occurrence Handle10230634
T. Mossman (1983) ArticleTitleRapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays J. Immunol. Methods 65 55–63 Occurrence Handle10.1016/0022-1759(83)90303-4 Occurrence Handle6606682
T. Watanabe T. Hasegawa H. Takahashi T. Ishibashi H. Itagaki K. Sugibayashi (2002) ArticleTitleUtility of MTT assay in three-dimensional cultured human skin model as an alternative for draize skin irritation test: approach using diffusion law of irritant in skin and toxicokinetics–toxicodynamics correlation Pharm. Res. 19 669–675 Occurrence Handle10.1023/A:1015366331634 Occurrence Handle12069171
R. C. Wester H. I. Maibach L. Sedik J. Melendres S. DiZio M. Wade (1992) ArticleTitleIn vitro percutaneous absorption of cadmium from water and soil into human skin Fundam. Appl. Toxicol. 19 1–5 Occurrence Handle10.1016/0272-0590(92)90021-9 Occurrence Handle1397789
A. M. Kligman E. Christophers (1963) ArticleTitlePreparation of isolated sheets of human stratum corneum Arch. Dermatol. 88 70–73
H. K. Vaddi P. C. Ho S. Y. Chan (2002) ArticleTitleTerpenes in propylene glycol as skin-penetration enhancers: permeation and partition of haloperidol, Fourier transform infrared spectroscopy, and differential scanning calorimetry J. Pharm. Sci. 91 1639–1651 Occurrence Handle10.1002/jps.10160 Occurrence Handle12115825
Accelrys Inc. Cerius2 Molecular Simulation Users Guide, Version 4.6, San Diego, 2001.
D. Rogers A. J. Hopfinger (1994) ArticleTitleApplications of genetic function approximation to quantitative structure–activity relationships and quantitative structure–property relationships J. Chem. Inf. Comput. Sci. 34 854–866 Occurrence Handle10.1021/ci00020a020
D. Rogers (1994) WOLF 6.2 GFA Program Molecular Simulation Inc. San Diego
J. Friedman (1988) Multivariate Adaptive Regression Splines Stanford University Stanford
L. C. Fuhrman B. Michniak C. R. Behl A. W. Malick (1997) ArticleTitleEffect of novel penetration enhancers on the transdermal delivery of hydrocortisone: an in vitro species comparison J. Control. Release 45 199–206 Occurrence Handle10.1016/S0168-3659(96)01573-8
A. K. Ghose V. N. Viswanadhan J. J. Wendoloski (1998) ArticleTitlePrediction of hydrophobic (lipophilic) properties of small organic molecules using fragmental methods: an analysis of ALOGP and CLOGP methods J. Phys. Chem. 102 3762–3772
E. W. Smith H. I. Maibach (1995) Percutaneous Penetration Enhancers CRC Press Boca Raton
A. N. C. Anigbogu A. C. Williams B. W. Barry H. G. M. Edwards (1995) ArticleTitleFourier transform Raman spectroscopy of interactions between the penetration enhancer dimethylsulfoxide and human SC Int. J. Pharm. 125 265–282 Occurrence Handle10.1016/0378-5173(95)00141-5
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Song, Y., Xiao, C., Mendelsohn, R. et al. Investigation of Iminosulfuranes as Novel Transdermal Penetration Enhancers: Enhancement Activity and Cytotoxicity. Pharm Res 22, 1918–1925 (2005). https://doi.org/10.1007/s11095-005-7416-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-005-7416-4