Abstract
ASD and ADHD are regarded as distinct disorders in the current DSM-5. However, recent research and the RDoC initiative are recognizing considerable overlap in the clinical presentation of ASD, ADHD, and other neurodevelopmental disorders. In spite of numerous neuroimaging findings in ASD and ADHD, the extent to which either of the above views are supported remains equivocal. Here we compare structural MRI and DTI literature in ASD and ADHD. Our main findings reveal both distinct and shared neural features. Distinct expressions were in total brain volume (ASD: increased volume, ADHD: decreased volume), amygdala (ASD: overgrowth, ADHD: normal), and internal capsule (ASD: unclear, ADHD: reduced FA in DTI). Considerable overlap was noted in the corpus callosum and cerebellum (lower volume in structural MRI and decreased FA in DTI), and superior longitudinal fasciculus (reduced FA in DTI). In addition, we identify brain regions which have not been studied in depth and require more research. We discuss relationships between brain features and symptomatology. We conclude by addressing limitations of current neuroimaging research and offer approaches that account for clinical heterogeneity to better distinguish brain-behavior relationships.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the DSM-5, autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD) are each distinguished by a separate set of core symptoms. For ADHD these include inattentiveness, hyperactivity and impulsivity, and for ASD social impairment, communication impairment and restricted interests and repetitive behavior (American Psychiatric Association 2013). Recent research efforts, however, are beginning to reveal significant overlap in clinical presentation between these two disorders. Subtle manifestations of these core symptoms along with high rates of comorbidity often blur the lines between diagnostic categories.
In those diagnosed with ASD, epidemiological research indicates that ADHD symptoms commonly co-occur. One such study found that 28 % of individuals diagnosed with ASD also have comorbid ADHD (Simonoff et al. 2008). ADHD symptoms such as inattentiveness, impulsivity, and hyperactivity are often present in ASD with one study even failing to find ASD subjects without these symptoms (Mayes et al. 2012; van der Meer et al. 2012).
In ADHD, studies have indicated that up to 70 % of individuals with ADHD exhibit ASD symptoms (Mulligan et al. 2009). Symptoms such as hyperactivity, inattentiveness, language delay, irritability, and social impairment can appear in both disorders (Mayes et al. 2012). Evidence indicates that children with ADHD exhibit increased rates of ASD symptoms such as social impairment which are not accounted for by ADHD traits like impulsivity and inattention (Grzadzinski et al. 2011). ADHD subjects exhibiting motor problems have also been found to exhibit increased levels of autistic traits (Reiersen et al. 2008).
Shared symptomatology and comorbidity have significant clinical implications. In children in whom both ASD and ADHD co-occur, cognitive and social impairment may be more severe than those without comorbidity (Leitner 2014). One study found that individuals with comorbid ASD and ADHD were more than twice as likely to be considered cognitively delayed than those with ASD alone (Rao and Landa 2014).
For these reasons there is significant controversy regarding whether ASD and ADHD represent distinct diagnostic categories, a single disorder, or lie on a continuum of brain dysfunction. To date, few imaging studies have directly compared ASD and ADHD structural features (Lim et al. 2015; Brieber et al. 2007). Given this scarcity of previous research, the extent to which these two disorders overlap at the level of brain features or represent distinct diagnostic categories remains unclear. We therefore present a review of neuroimaging findings in these two highly co-morbid conditions in order to examine and compare the neural structures and resultant symptoms that are implicated across ASD and ADHD diagnostic categories. We aim to build on some of the findings of a previous broad review encompassing many separate fields of research in ASD and ADHD by Rommelse et al. (2011) by focusing specifically on structural neuroimaging, including recent research, and by addressing additional regions of interest. We have chosen to focus specifically on structural findings as functional studies add the additional confound of task, making it difficult to accurately compare ASD and ADHD across studies. We conclude our review, by offering suggestions for future research in the neuroimaging of ASD and ADHD as well as other neurodevelopmental disorders.
We conducted our literature search using Pubmed and Google Scholar search engines. Our search terms included “ASD”, “ADHD”, “autism”, ‘autism spectrum disorder’ or “attention-deficit hyperactivity disorder”, combined with “neuroimaging”, “diffusion tensor imaging”, “DTI”, or “structural MRI”. Articles were also chosen from the reference lists of articles found through the above search methods. Brain regions of interest were then chosen based on the frequency with which they were implicated in the ASD and ADHD neuroimaging literature found through the above search. Several brain regions of interest (brain volume, cortical thickness, corpus callosum, and cerebellum) chosen by our methodology were discussed by a previous review (Rommelse et al. 2011). Articles included in the final reference list were chosen based on their relevance to the selected brain regions of interest. Articles which did not include an analysis on the selected brain regions of interest were excluded. Publication year of the articles included in the final reference list range from 1992 to 2015.
The first section of this paper addresses structural magnetic resonance imaging (sMRI) findings while the second will focus on structural connectivity studies that use diffusion tensor imaging (DTI). In the final section we will present a summary of our findings and discuss directions for future research.
Structural Magnetic Resonance Imaging (sMRI)
Structural magnetic resonance imaging (sMRI) takes advantage of the differing magnetic properties of brain tissues to non-invasively map the spatial distribution of the structural properties of the human brain. Spatial distribution of different brain tissues (gray and white matter) and cortical and sub-cortical structures of the brain can be accurately mapped using sMRI. Images obtained from sMRI are used to quantify and compare brain structures for both research and diagnostic purposes. In this section, in regions in which volumetric findings are reported on a specific structure, we have indicated if original studies have not controlled for total brain volume using methods such as calculating volume ratios or regressing total brain volume when groups significantly differ on this measure. A summary of sMRI findings is depicted in Fig. 1.
A summary of ASD and ADHD structural MRI findings. Light blue indicates regions where ASD predominately shows volumetric increases compared to controls and ADHD shows decreases; these regions include the prefrontal cortex and basal ganglia. Green indicates regions where ASD and ADHD display similar abnormalities including cerebellum and corpus callosum. Red indicates regions implicated predominately in ASD. These regions include the amygdala and temporal lobe. (Figure 1 regions were defined using AAL and Brodmann's atlases and generated using WFU Pickatlas and MRIcron)
Brain Volume
Total brain volume is usually calculated by adding total grey matter, white matter and cerebrospinal fluid. In the case of ASD there has been interest in brain volume and head circumference because it is believed that these may serve as an early marker for possible risk for ASD. As such, many studies have sought to determine the extent to which brain overgrowth is associated with ASD status.
In ASD it is believed that shortly after birth brain size is normal or smaller than average (Courchesne et al. 2003; Hazlett et al. 2005; Nordahl et al. 2011). However, a period of increased brain growth has been found to occur thereafter (Langen et al. 2014). The age of onset for this period of growth is speculated to occur prior to 4 years of age (Langen et al. 2014), but others have indicated that overgrowth may begin as young as 4 to 6 months (Nordahl et al. 2011). The exact cause of this sudden increase in brain growth is unknown, but overgrowth appears to be due to both grey matter (GM) and white matter (WM) increases (Carper et al. 2002). Schumann et al. (2010) found that grey and white matter overgrowth are present during the first year of life and occur in all lobes of the brain except the occipital. This period of increased brain growth appears to arrest around adolescence and may even begin to transition into a period of degeneration (Courchesne et al. 2007). It is suspected that brain overgrowth may be due to failure of dendritic pruning or excessive dendritic arborization (Hazlett et al. 2005).
In contrast, ADHD appears to be characterized by decreased brain volume (Batty et al. 2010; Hill et al. 2003; Mostofsky et al. 2002). A study by Durston et al. (2004) found a 4 % reduction in intracranial volume in children with ADHD aged 7 to 19 years compared to controls and a trend for reduced volume in unaffected siblings, indicating a possible genetic susceptibility for brain volume. Other studies have estimated up to 7 % reductions in brain volume in children with ADHD (Wolosin et al. 2009). Reductions in total WM volume or cerebral volume only have been reported as well (Sowell et al. 2003; Valera et al. 2007). Seidman et al. (2011) found no differences in total brain volume in a data set of individuals aged 18 to 59 but speculate this may be due to the above average IQ of the ADHD subject cohort. Some previous studies reporting lower brain volume have used subjects with average IQ (Batty et al. 2010; Hill et al. 2003) or have not matched or covaried for IQ (Mostofsky et al. 2002). Researchers have hypothesized that abnormalities in ADHD may be due to a delay in brain maturation whereby individuals with ADHD experience the same steps of cortical maturation but slower than unaffected individuals (Shaw et al. 2007). This hypothesis offers an explanation for studies which indicate a normalization of brain volume in adulthood. But findings regarding total brain volume after childhood remain equivocal with some suggesting persistent deficits into adolescence or even adulthood (Castellanos et al. 2002).
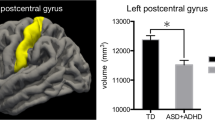
Cortical Thickness
Another metric of interest in ASD and ADHD is cortical thickness. Cortical grey matter volume is calculated as the product of both surface area (SA) and cortical thickness (CT). Studies have found evidence that these two facets of brain morphology are determined by different genetic factors and as such may be dissociable brain features (Panizzon et al. 2009). Because of this, an increase in SA may not necessarily entail an increase in CT and vice versa. Therefore it is not clear how these metrics individually contribute to cortical grey matter volume in ASD and ADHD. It may be possible that mutations in various genes independently control cortical SA and CT (Panizzon et al. 2009). Many researchers have sought to examine these features individually in both ASD and ADHD. By examining these features independently, it may be possible to infer the etiology of brain abnormalities in various disorders.
Studies examining CT and SA in ASD have found mixed results. Hardan et al. (2006) found increased gyral and sulcal thickness as well as increased thickness in temporal and frontal lobes in children with ASD and in a later longitudinal study decreases in GM thickness over time (Hardan et al. 2009). But a study by Raznahan et al. (2009) in a cohort of 127 males with ASD aged 10 to 60 found that more cortical thinning was present during childhood. By middle to late adulthood, however, patients exhibited increased cortical thickness compared to controls. Focal differences in cortical thickness were found and were pronounced in temporal regions including middle temporal gyrus and fusiform gyrus. This report of cortical thinning in childhood was consistent with a previous study (Chung et al. 2005). Inconsistencies in findings between Hardan et al. (2009) and Raznahan et al. (2009) may be due to differences in sample size. The former study only included 34 participants while the latter included 127. In addition, Raznahan et al. (2009) used a cross-sectional as opposed to longitudinal data set. Other studies have indicated no differences in cortical thickness in children with ASD, but report increases in surface area across all four lobes which the authors hypothesized may underlie increased cortical volume in ASD (Hazlett et al. 2011).
In adults with ASD, some studies have reported thinning throughout regions of the mirror neuron system and other areas responsible for social cognition such as middle and inferior temporal gyrus (Hadjikhani et al. 2006) and posterior superior temporal sulcus in high functioning individuals (Scheel et al. 2011). Others report increases which occur in the frontal lobe with reductions in surface area in orbitofrontal cortex (Ecker et al. 2013). A recent study making use of a large publicly available data set consisting of over 1000 subjects, however, found that there was no significant differences in overall cortical thickness or surface area in subjects with ASD compared to controls (Haar et al. 2014). It is possible that observed differences in cortical thickness vary with developmental stage or even by region (Zielinski et al. 2014). This in turn may account for some of the inconsistency observed across studies.
Fewer studies have focused on cortical morphology in ADHD than in ASD especially in adults. Reductions in thickness have been reported throughout parietal and frontal regions responsible for attention and executive function in children as well as in adults with ADHD (Hoekzema et al. 2012; Makris et al. 2007; Proal et al. 2011). Longitudinal studies of brain development in ADHD show delayed development of cortex which occurs significantly later than in typical developing controls. Shaw and colleagues examined cortical development in two separate studies. In the former, cortical thinning was found to mature more slowly relative to typically developing individuals while the later study found that peak surface area in prefrontal regions doesn’t occur until 14.6 years on average in ADHD in comparison to 12.7 years in typically developing individuals (Shaw et al. 2007, 2012). At least one study found no differences in cortical thickness in children with ADHD, but instead reported reductions in surface area and cortical folding (Wolosin et al. 2009).
Temporal Lobe
The temporal lobe as a whole is involved in processing sensory information. Areas responsible for language, face recognition, and audition are located in this region in addition to regions which are involved in memory. Temporal lobe abnormalities have frequently been reported in ASD while findings are less numerous in ADHD.
In the temporal lobe there have been reports of abnormalities in both GM and WM in ASD. A study by Boddaert et al. (2004) found reduced white matter in right temporal pole and reduced grey matter in the superior temporal sulcus in children with ASD, but did not control for brain volume. Other studies report only grey matter deficits in left temporal lobe (Brun et al. 2009; McAlonan et al. 2005) or only white matter deficits in left temporal lobe (McAlonan et al. 2002). In contrast, studies in very young children with ASD appear to indicate volumetric increases in temporal regions although without controlling for brain volume. Carper et al. (2002) found increased grey matter in temporal lobe and a trend toward significant increases in temporal lobe WM in children under the age of four. This finding has been replicated by Hazlett et al. (2005) and Schumann et al. (2010) which report grey and white matter hyperplasia and grey matter hyperplasia, respectively, in temporal lobe regions in children under the age of three.
Growth rates in temporal region WM have been found to be decreased compared to controls in adolescents (Hua et al. 2013)—a finding which is consistent with the hypothesized trajectory of brain growth in ASD. In addition to abnormal growth of temporal lobe regions, some studies report abnormalities in temporal sulci and gyri. Levitt et al. (2003) reports shifting of temporal sulci in children and adolescents with ASD compared to controls. Increased gyrification in bilateral posterior temporal regions and lateral occipital regions has been reported in adolescents and adults with ASD as well (Wallace et al. 2013).
Studies in adults with ASD are less frequent. Some studies report thinning in middle and inferior temporal lobe, regions responsible for facial processing and social cognition (Hadjikhani et al. 2006). Interestingly, a study of typically developing adults was able to find a negative correlation between posterior superior temporal sulcus WM and degree of autistic symptoms as measured by autism-spectrum quotient (von dem Hagen et al. 2011).
ADHD studies report mixed findings in temporal lobe regions. Some studies report reductions in white matter in bilateral temporal lobes and reduced grey matter in anterior temporal lobe in individuals at high risk for ADHD (Van’t Ent et al. 2007). Researchers have found decreased cortical volume in temporal lobes in children (Wolosin et al. 2009) as well as decreased WM (McAlonan et al. 2007). Additionally, some studies report both increases and decreases. Sowell et al. (2003) found reductions in anterior temporal regions and grey matter increases in posterior temporal regions in children and adolescents with ADHD without controlling for brain volume. Seidman et al. (2011) report decreases in right temporal lobe grey matter and increases in left temporal lobe in adults. In the above study, differences were not significant after correcting for multiple comparisons.
Prefrontal Cortex
Involvement of the prefrontal cortex has long been implicated in both ADHD and ASD due to its role in attentional regulation, impulse control, cognitive set-shifting, working memory and theory of mind (Arnsten 2009; Evans et al. 2004; Shallice 2001). The prefrontal cortex may be subdivided into the dorsolateral prefrontal cortex (DLPFC), ventrolateral prefrontal cortex (VLPFC), and orbitofrontal (OFC) or ventromedial prefrontal cortex (VMPFC).
The frontal lobe as a whole has been found to exhibit increased volume in ASD although findings do not necessarily indicate increased volume across all frontal lobe sub-regions. Evidence from studies by Carper et al. (2002) and Brun et al. (2009) indicate early hyperplasia in frontal regions although in the latter study hyperplasia was not evident when scaling for brain volume. Studies reveal that early hyperplasia or overgrowth in some frontal regions is transient such that brain growth decreased to slower than normal by age two with group differences disappearing by middle to late childhood (Carper and Courchesne 2005). Specific areas of abnormality include the OFC—which has been implicated in social cognition and theory of mind (Girgis et al. 2007). Studies examining the OFC have found decreased volume and thickness in individuals with ASD (Chung et al. 2005; Girgis et al. 2007; Jiao et al. 2010). Carper and Courchesne (2005) reported a slight increase in OFC in children under five and a slight decrease in children aged five to nine, although this finding was not statistically significant. Abnormalities in the dorsolateral and medial frontal regions have been found as well in ASD, with children exhibiting increased volume in these regions (Carper and Courchesne 2005) and in prefrontal cortex white matter (Herbert et al. 2004). Of the aforementioned ASD studies only Girgis et al. (2007) and Chung et al. (2005) have controlled for brain volume. Histological analysis has offered insight into abnormalities in these regions in ASD. Prefrontal regions have shown increased neuron counts in prefrontal and dorsolateral prefrontal areas (Courchesne et al. 2011) and axonal abnormalities with reduction of large axons involved in long distance connectivity and increases of thin axons involved in short local connectivity (Zikopoulos and Barbas 2010).
In ADHD it is suspected there is a delay in prefrontal cortex development in individuals with ADHD (Shaw et al. 2007, 2012). Studies report volumetric reductions throughout the frontal lobe (Castellanos et al. 2002) and prefrontal cortex (Mostofsky et al. 2002) although Castellanos et al. found that this difference disappeared when controlling for brain volume. Other studies not controlling for brain volume have reported reductions bilaterally in inferior portions of the prefrontal cortex as well in areas thought to underlie functions such as working memory and response inhibition (Sowell et al. 2003). A study of twin pairs at low and high risk for ADHD and concordant or discordant for scores on the Child Behavior Checklist Attention Problem scale found volume loss in orbitofrontal areas in concordant twin pairs and volume reductions in the inferior DLPFC in discordant pairs—demonstrating a possible differential effect of genetics and environment (Van’t Ent et al. 2007). At least one study has reported increased volume in regions of the DLPFC (Seidman et al. 2011). A meta-analysis, however, found no significant differences in grey matter volumes in frontal regions (Ellison-Wright et al. 2008).
Amygdala
Another candidate brain region that may differentiate ASD and ADHD is the amygdala. This subcortical structure inferior to the temporal lobe maintains diverse connections with the neocortex, basal ganglia, hippocampus and thalamus (Baron-Cohen et al. 2000). The amygdala has been robustly linked to fear, anxiety, and a range of social behaviors (Davis 1992; Adolphs et al. 1998). The amygdala has been a major region of interest in ASD, but fewer structural imaging studies of the amygdala in ADHD have been conducted.
Most ASD studies have shown amygdala overgrowth. Toddlers have exhibited bilateral amygdala overgrowth which correlates with severity of social impairment (Cynthia Mills Schumann et al. 2009). Amygdalar enlargement has been found to be present at ages 2 to 4 (Nordahl et al. 2012) and some evidence indicates that amygdalar volume may normalize in adolescence (Barnea-Goraly et al. 2014). Post-mortem histological analyses examining the amygdala in ASD brains ranging from ages 10 to 44 have reported fewer neurons in this region, but given the large age range of the cohort used in this study caution must be used in interpreting this result (Cynthia Mills Schumann and Amaral 2006).
By contrast, in ADHD, the amygdala has been found to be relatively normal given the current evidence. Plessen et al. (2006) found normal amygdala volumes in subjects with ADHD ages 6 to 18, but did note possible reduced size in the basolateral region of the amygdala. Perlov et al. (2008) examined adults and also failed to find differences in amygdala size. Frodl et al. (2010), however, found bilaterally reduced amygdala volumes in adults with ADHD. In this study, smaller right amygdala volume was associated with less inattention and greater hyperactivity.
Corpus Callosum (CC)
The corpus callosum (CC) has been of particular interest to researchers as it represents the largest white matter bundle in the brain and is responsible for interhemispheric communication. In addition, DTI studies have used the CC as an index of cortical connectivity (Lewis et al. 2009). From anterior to posterior, the corpus callosum consists of the genu, midbody, and splenium. The CC is organized in a manner such that the anterior region connects to frontal areas while the posterior region contains connections to temporal, parietal, and occipital regions containing premotor, supplementary motor, motor and sensory areas (Gilliam et al. 2011). Because of these connections to areas essential for cognition and motor skills there has been a great deal of interest in the corpus callosum particularly in ASD as it is a source of many long-range connections within the brain (Cascio et al. 2006).
Findings in individuals with ASD reveal significantly reduced volume or area compared to controls (Alexander et al. 2007; Frazier and Hardan 2009; Freitag et al. 2009; Haar et al. 2014; Hardan et al. 2000; Manes et al. 1999; Vidal et al. 2006). Although CC volume reductions in ASD are well established, the trajectory of CC growth remains undefined and to date very few longitudinal studies examining the growth of the CC in ASD have been conducted. Preliminary evidence indicates that while reductions in CC volume persist into adulthood they do not worsen (Frazier et al. 2012). The anterior portions of the CC, however, may normalize in adolescence and this normalization may underlie the motor and emotional regulation improvements seen in adolescence (Frazier et al. 2012).
Recent studies examining the CC in ADHD are relatively few. Those studies examining CC volume in ADHD have mostly found volumetric reductions or reduced area (Hill et al. 2003; Van’t Ent et al. 2007). Additionally, the aforementioned study by Van’t Ent et al. (2007) found that CC volume reduction in individuals at high risk for ADHD was localized to the splenium compared to those at low risk. Splenium reductions have been the most replicated finding across ADHD structural studies (Valera et al. 2007). Schnoebelen et al. (2010) failed to find differences in total CC volume, but the study did find a reduction in the area of the splenium in treatment naïve ADHD subjects that was not present in those who had been receiving stimulant treatment. Few studies have examined the trajectory of CC growth in ADHD. A preliminary study by Gilliam et al. (2011) examining the CC in children and adolescents found increased growth rates in the anterior portion of the CC in subjects with ADHD which may be related to prefrontal abnormalities given the anterior CC’s connections with this region.
Basal Ganglia
The basal ganglia are a group of subcortical structures which include the globus pallidus, subthalamic nucleus, nucleus accumbens, substantia nigra, and neostriatum. The basal ganglia as a whole are believed to be integral in coordinating goal-directed behavior (Shadmehr and Krakauer 2008). The neostriatum consists of the caudate and putamen, two structures implicated in the pathophysiology of both ASD and ADHD (Di Martino et al. 2011; Seidman et al. 2011). The striatum is responsible for coordinating motivation and motor movement and has the highest concentration of dopamine in the brain (Castellanos and Tannock 2002). Given its role in motor movement and motivation, it is thought that the striatum may underlie the hyperactivity in ADHD and repetitive and stereotyped behavior seen in ASD. Abnormalities such as rightward globus pallidus asymmetry have been implicated in repetitive behavior as well (Evans et al. 2014).
In ASD, basal ganglia abnormalities have been put forth as a possible cause of the repetitive behaviors that are a core symptom (McAlonan et al. 2002). In a longitudinal study of children with ASD average ages 9.9 to 12.3 the caudate nucleus was found to have twice the growth rate of controls (Langen et al. 2014). This increased growth rate was correlated with the severity of repetitive behavior symptoms as measured by the Autism Diagnostic Interview – Revised (Langen et al. 2014). Increased caudate volume has been shown to correlate with repetitive behaviors in adults with ASD as well (Hollander et al. 2005). A recent longitudinal study by Hua et al. (2013) did not find caudate abnormalities, but findings did reveal increased rates of putamen growth in adolescents. A meta-analysis of structural findings indicated caudate overgrowth as the most common basal ganglia finding in ASD (Stanfield et al. 2008).
In contrast, some studies indicate reductions in basal ganglia volume; for example Ecker et al. (2010) report reductions in right caudate and right putamen volume in ASD adults compared to controls, but only at a very lenient threshold of p < 0.1. A study by Estes et al. (2011) initially found enlargement in basal ganglia structures, but this failed to remain significant after controlling for brain volume. In this study, it was also found that reductions in basal ganglia structures including the striatum, putamen, and globus pallidus were correlated with repetitive and stereotyped behavior in children with ASD ages 3 to 4 (Estes et al. 2011). Other studies have found widespread grey matter reductions within the frontostriatal network as a whole in both adults and children (McAlonan et al. 2002; McAlonan et al. 2005).
Studies examining the striatum in ADHD have found volume reductions in the caudate (Seidman et al. 2011; Pliszka et al. 2006) and caudate and globus pallidus (Castellanos et al. 1996). Possible gender difference in these structures may exist. One study reports that basal ganglia abnormalities in caudate, putamen and globus pallidus are present in boys but not girls (Qiu et al. 2009). Meta-analyses of structural studies support findings of basal ganglia abnormalities with one such analysis by Ellison-Wright et al. (2008) finding reduced volume in the right putamen and the region surrounding the globus pallidus. A more recent meta-analysis (Frodl and Skokauskas 2012) arrived at similar conclusions, noting reduced caudate volume in ADHD compared to controls. Further, Frodl and Skokauskas (2012) report that caudate abnormalities in ADHD may diminish with age and methylphenidate treatment. Castellanos et al. (2002) also reported that caudate differences diminish in adolescence.
Cerebellum
Initially known for its role in execution of motor skills, the cerebellum has recently been shown to play an important role in cognitive processes as well via connections to frontal cortical areas (Seidman et al. 2005). For example, the cerebellum has been identified as a node in a network subserving attention (Bush 2011). In ASD and ADHD, the cerebellum has been found to be one of the most consistent sites of abnormality (Allen et al. 2004; Fatemi et al. 2012). The cerebellum is divided into ten separate cerebellar lobules and a midline structure known as the vermis. The exact function of all cerebellar lobules is not known, but lobules I-V and VIII are believed to have sensorimotor functions, lobules VI and VII are involved in cognitive processes, lobule IX is used in visual guidance and lobule X is involved in the vestibular system (Stoodley and Schmahmann 2010).
Studies of the cerebellum in ASD have mostly noted reductions in the cerebellum as a whole or cerebellar sub-regions. Adults with high functioning ASD are reported to exhibit reduced grey matter volume in cerebellar regions (McAlonan et al. 2002) and children have been found to exhibit reduced white matter volume (Boddaert et al. 2004; McAlonan et al. 2005). Work examining the relationship between structural volume of the cerebellum and functional activation during a STOP/GO task, revealed a reduced (but not statistically significant) volume of the cerebellum in ASD subjects, and a correlation between the level of abnormality in cerebellar structure with the degree of cerebellar motor activation during the STOP/GO task (Allen et al. 2004). Of these studies Allen et al. (2004) and Boddaert et al. (2004) appear not to have controlled for brain volume.
In ASD specific lobules have been examined with one report of reduced area of lobules VI-VII in children (Carper and Courchesne 2000). More recently, reduced volume of the cerebellar vermis as a whole was reported in high functioning individuals with ASD aged 7.5 to 18.5 but with no significant differences in lobule subgroups (Scott et al. 2009). A meta-analysis of structural MRI studies in ASD (Stanfield et al. 2008) found reduced volume of cerebellar vermis lobules VI-VII and VIII to X but increased overall cerebellar volume. Finally, a recent study found increased volume of cerebellar lobules V, VII and IX and decreased volume in lobules III and VIII in children (Brun et al. 2009). It is thought one source of these volumetric reductions may be reduced purkinje cell numbers in the cerebellum. Post-mortem histological studies have indicated that ASD subjects exhibit significantly reduced purkinje cell numbers in the cerebellum perhaps indicating a decrease in inhibitory output to cortical areas (Carper et al. 2002).
An early study by Berquin et al. (1998) found that cerebellar volume was reduced in young boys with ADHD in lobules VIII to X of the inferior lobe and hypothesized that a cerebello-thalamo-prefrontal circuit could underlie ADHD symptoms involving motor control, inhibition, and executive function. Reductions in lobules VIII to X have been replicated in other studies in young boys with ADHD as well (Mostofsky et al. 1998). Similarly, a study by Hill et al. (2003) found a smaller area rather than volume in cerebellar lobules VIII to X and I to V in cohort of boys and girls diagnosed with ADHD. Further studies have noted reduced cerebellar volume in the inferior vermis, but not overall cerebellar volume, in children which was correlated with parent ratings of hyperactivity, impulsivity, and attention (Bledsoe et al. 2011). Seidman et al. (2011) reported reductions in areas of bilateral cerebellum as well, but these failed to remain significant after FWE correction. In a longitudinal work (Mackie et al. 2007) examining the cerebellum in ADHD, a non-progressive reduction in superior vermis was found compared to controls which was present regardless of clinical outcome. In comparison, the study found a progressive loss of total cerebellar volume with age which was related to negative clinical outcome (Mackie et al. 2007).
Diffusion Tensor Imaging (DTI)
Diffusion tensor imaging (DTI) has given researchers a way to non-invasively investigate the macrostructural integrity and orientation of white matter fiber bundles. DTI measures the directional diffusion of water molecules along neuronal membranes, allowing researchers to map white matter pathways within the brain. One measure frequently derived in DTI is fractional anisotropy (FA). FA is measured on a scale from 0 to 1; with 0 indicating complete isotropy and 1 indicating complete anisotropy. Anisotropy would indicate that diffusion occurs in a directional manner whereas isotropy would indicate diffusion in all directions. Other measures include mean diffusivity (MD) which is an average of axial diffusivity (λ1) and the perpendicular diffusivities (λ2, λ3), radial diffusivity (RD) which is the average of perpendicular diffusivities, and apparent diffusion coefficient which indicates the magnitude of diffusion.
While numerous DTI studies have investigated ASD, few have been conducted in ADHD. Based on the studies to date a few regions have been found to be abnormal in both disorders. In particular, abnormalities in the corpus callosum and superior longitudinal fasciculus have been frequent findings in addition to possible abnormalities in areas such as the cingulum, cerebellum and internal and external capsules. A summary of the DTI findings in this section is depicted in Fig. 2.
A summary of DTI findings in ASD and ADHD. Purple indicates regions of possible abnormality for ASD and ADHD for which contradictory findings or insufficient research prevents drawing firm conclusions. These regions include the cingulum, cerebellar peduncles, and external capsules. Blue indicates regions of similar abnormalities in both ASD and ADHD. These regions include the corpus callosum and superior longitudinal fasciculus. Red indicates regions implicated in ADHD only. These regions include the internal capsule. (Figure 2 generated using Johns Hopkins University White Matter Atlas and MRIcron)
Corpus Callosum (CC)
Overall reductions in volume and increased mean diffusivity have been reported in the CC in ASD, but studies have differed regarding the exact nature of the abnormalities in sub-regions. Varying methods are employed to subdivide the corpus callosum to detect regional abnormalities, which further complicates comparisons. Reduced FA in the corpus callosum as a whole is noted in children (Kumar et al. 2010; Shukla et al. 2010) and adults (Gibbard et al. 2013). Others (Alexander et al. 2007) report reduced FA in the genu and splenium only, while still others detect reduced FA in the body and genu (Barnea-Goraly et al. 2004), and the body alone after controlling for IQ (Barnea-Goraly et al. 2010) in children with ASD. Abnormalities in the CC in FA, radial diffusivity, and mean diffusivity have been found to correlate with processing speed on an IQ test (Alexander et al. 2007). Overall, DTI measures of white matter integrity in the corpus callosum in subjects with ASD have predominately revealed reduced FA and increased diffusivity (Alexander et al. 2007; Aoki et al. 2013; Barnea-Goraly et al. 2004, 2010; Gibbard et al. 2013; Shukla et al. 2010, 2011), although notable exceptions of increased FA findings in children with ASD do exist (Weinstein et al. 2011).
As discussed previously, ADHD studies have found volumetric reductions in CC as well – particularly in the splenium. Studies using DTI to examine the CC predominately indicate FA reductions in children, with some reports of reduced FA in frontal regions (Langevin et al. 2014), and posterior regions (Cao et al. 2010) while Hamilton et al. (2008) found no differences. Langevin et al. (2014) report a correlations between CC FA and scores on measures of attention and motor function with reduced FA predicting poorer performance in children in some sub-regions. Dramsdahl et al. (2012) examined adults with ADHD and found reduced FA in the splenium of the CC, but were unable to detect volumetric abnormalities.
Internal and External Capsules
The internal and external capsules are white matter association tracts located adjacent to the basal ganglia. The internal capsule contains connections to cortical areas and subcortical areas such as the brain stem, thalamus, and basal ganglia in addition to connections with the corticospinal tract which conducts nerve impulses from motor cortex to the spinal cord (Ara and Islam 2010; Axer and Keyserlingk 2000). The external capsule also contains connections to cortical and subcortical regions (Dictionary of Biological Psychology 2003).
In ASD increased MD in bilateral external capsules and bilateral retrolenticular internal capsules are reported in adults (Gibbard et al. 2013). Increased MD in the anterior and posterior limbs of the internal capsule have been reported in children (Shukla et al. 2010) along with reduced FA; moreover MD in the posterior limb of the internal capsule was found to correlate negatively with age. In contrast, the posterior limb of the left internal capsule and external capsule has been found to exhibit increased FA in very young children compared to controls (Bashat et al. 2007). A study examining a cohort of individuals with large age range (10 to 35) found that the right retrolenticular portion of the internal capsule exhibits decreased FA (Keller et al. 2007).
In children and adolescents with ADHD, a study by Adisetiyo et al. (2014) found increased mean kurtosis (MK) in external and internal capsules indicating greater white matter complexity. A large cohort study of over 100 individuals by Cortese et al. (2013) found decreased FA in children in the retrolenticular area of the internal capsule. A 33 year follow up indicated that FA reductions in some regions may persist into adulthood. Abnormalities in other regions of the internal capsule have been reported as well with findings of reduced FA or increased diffusivity in anterior, superior, and posterior portions of the internal capsule (Pavuluri et al. 2009). A recent meta-analysis of DTI studies indicates that the internal capsule is an area most commonly found to exhibit altered white matter integrity in ADHD (van Ewijk et al. 2012).
Cerebellum
Although the cerebellum has been a major region of interest in ADHD and ASD using sMRI, few DTI studies examining cerebellar white matter currently exist. Studies in ASD have found decreased FA in the middle cerebellar peduncle in children (Shukla et al. 2010) and increased FA in adolescents (Cheng et al. 2010). Others report decreased FA in right superior cerebellar peduncle in adults (Catani et al. 2008). Furthermore, this study revealed a negative correlation between diffusion anisotropy in the right superior cerebellar peduncle and social impairment.
Preliminary studies in ADHD indicate lower FA in right middle cerebellar peduncle (Bechtel et al. 2009) as well as right cerebral peduncle, left middle cerebellar peduncle, and left cerebellum in children (Ashtari et al. 2005). Decreased white matter connectivity is reported in cerebellar regions as well in children and adolescents with ADHD (Hong et al. 2014).
Superior Longitudinal Fasciculus
Another consistent area of white matter abnormality in both disorders is the superior longitudinal fasciculus (SLF). The SLF is a white matter bundle spanning the posterior and anterior regions of the cerebrum and is known to contain connections to frontal, temporal, parietal and occipital lobes (Hong et al. 2014). It is subdivided into four regions – the SLF I, II, III and arcuate fasciculus. The SLF is involved in higher order motor behavior, spatial attention, somatosensory processing as well as auditory functions (Makris et al. 2005). In addition, the left SLF also connects Broca’s and Wernicke’s areas which are responsible for language comprehension and production (Hoppenbrouwers et al. 2014).
Studies in ASD have indicated reduced FA along this tract and/or increased diffusivity in children and adolescents (Groen et al. 2011; Jou et al. 2011a, b; Shukla et al. 2011) and adults (Gibbard et al. 2013). Weinstein et al. indicate increased FA in this tract in very young children, however (Weinstein et al. 2011). A meta-analysis of DTI studies in ASD found reduced FA in SLF as well (Aoki et al. 2013).
Reduced FA in the SLF in children with ADHD has been indicated in several studies with findings in a subsection of the right SLF (Cortese et al. 2013) as well as bilaterally (Hamilton et al. 2008) although no differences have been reported as well (Langevin et al. 2014). Studies of adults have reported similar findings in right SLF (Makris et al. 2008). Pavuluri et al. (2009) did not find reduced FA in the SLF in children; however, results did indicate an increased apparent diffusion coefficient in ADHD compared to controls.
Cingulum
The cingulum is a white matter tract located superior to the corpus callosum and spans its entire length. It contains connections to prefrontal cortex and medial parietal and temporal lobes. Some evidence suggests it is involved in cognitive control (Metzler-Baddeley et al. 2012) or possibly in sustained attention (Takahashi et al. 2010). While it has often been a region of interest in both disorders, current evidence is contradictory.
In ASD the cingulum has been found to exhibit increased density (Kumar et al. 2010) and increased FA (Weinstein et al. 2011) as well as decreased FA (Jou et al. 2011a, b) in children. This discrepancy may possibly be explained by the fact the former study used young cohorts under the age of six while the latter two studies used adolescents. At least one study found reduced cingulum FA to be significantly correlated with behavioral regulation in ASD (Ikuta et al. 2014). In ADHD, investigations of the cingulum bundle have been inconclusive and have yielded higher apparent diffusion coefficients in adolescents (Pavuluri et al. 2009), increased FA (Silk et al. 2009), as well as no differences (Hamilton et al. 2008; Langevin et al. 2014), and in adults reduced FA (Makris et al. 2008).
Discussion
Summary of Findings and Directions for Imaging
From the research discussed in this review (see Table 1 for a summary) it appears abnormalities in brain volume are one of the more consistent features of ASD and ADHD. While ASD exhibits brain overgrowth starting in early childhood through adolescence, ADHD appears to exhibit smaller brain volumes. In addition, it appears that ADHD exhibits cortical thinning throughout childhood and possibly into adulthood. Findings regarding cortical thickness in ASD are equivocal with some studies indicating cortical thinning and thickening in both childhood and adulthood.
Overgrowth and cortical thinning extends to many regions in the prefrontal cortex for ASD and ADHD, respectively. Prefrontal abnormalities may underlie deficits in social functioning, attention, and impulsivity in both disorders. The exact cause of these abnormalities is unknown, but it appears that grey and white matter abnormalities are implicated in both disorders but to different extents. In the case of ASD, non-neuronal tissue growth may underlie volumetric increases (Aoki et al. 2012).
Temporal lobe findings in ASD are quite numerous. In children under the age of three, studies seem to indicate an increase in both GM and WM volume in temporal regions. From the research discussed, there may be a trend for decreased temporal lobe volume with age. In adults, findings are mixed with reports of increases and decreases in GM and WM. In ADHD, fewer studies have examined temporal lobe regions and no conclusions can be drawn although some abnormalities have been reported.
Current evidence appears to more strongly implicate the amygdala in ASD than ADHD. Although the amygdala hasn’t been a major region of interest in ADHD structural studies, the majority of studies report few or no differences from controls. Based on this review it is possible that the amygdala may differentiate ASD and ADHD. Because of this the amygdala may serve as a possible imaging marker for discerning the two disorders, but more evidence from structural ADHD studies are required to draw firm conclusions.
The corpus callosum is another consistently implicated structure in both ASD and ADHD and exhibits volumetric reductions in both disorders. DTI studies in both disorders have mainly found decreased FA and increased diffusivity in this region. Attempts have been made to identify specific regions of callosal abnormality, but results are often contradictory. ADHD studies consistently report decreased FA and diffusivity in CC although specific sub regions (such as genu, body, or splenium) are contradictory. Current evidence appears to indicate that deficits in callosal subregions may mirror deficits in the cortical regions they subserve. Overall, there is ample evidence of volumetric reductions and decreased white matter integrity in the CC in both disorders, but how these abnormalities relate to brain behavior is not known and more research is needed.
Evidence for basal ganglia abnormalities is present in both disorders as well. ASD studies appear to indicate caudate overgrowth most often with abnormalities in the putamen as well. ADHD studies report volumetric reductions in caudate with possible reductions in other basal ganglia regions such as the globus pallidus and putamen. Basal ganglia abnormalities are thought to underlie hyperactivity, impulsivity, and repetitive and stereotyped behavior.
Another region that consistently exhibits abnormalities in both ASD and ADHD is the cerebellum. In addition, these abnormalities appear to be very specific in ADHD with evidence often indicating volumetric reductions in cerebellar lobules VIII to X in children with ADHD as well as possible volumetric reductions in cerebellar vermis. In ASD, volumetric reductions are present as well with most reports in children, but these appear to be more wide spread. A recent meta-analysis did report reductions specifically in lobules VIII to X, however (Stanfield et al. 2008).
Evidence of white matter abnormality in the cerebellum is limited and future research is needed in this area. A few DTI studies offer preliminary evidence of cerebellar white matter abnormality in both disorders in the form of reduced FA in the cerebellar peduncles, but no firm conclusions can be drawn given that only a few studies have been conducted (Ashtari et al. 2005; Bechtel et al. 2009; Cheng et al. 2010; Catani et al. 2008; Hong et al. 2014; Shukla et al. 2010). It is not clear how specific lobule abnormalities relate to behavioral phenotypes, but volumetric abnormalities may underlie both cognitive and motor dysfunction in both disorders.
DTI studies have implicated possible deficits in a few white matter tracts—namely internal and external capsules, superior longitudinal fasciculus, and cingulum. The internal and external capsules in ASD and ADHD have exhibited white matter abnormalities in both disorders although evidence for abnormality is more robust in ADHD and how these relate to symptomatology is unclear. The superior longitudinal fasciculus is another possible region of interest as it has been found to exhibit measures of decreased white matter integrity in both disorders; whether this is exhibited bilaterally is less clear. Although the cingulum has been a region of interest quite frequently, evidence for cingulum abnormality is contradictory with findings of both increased and decreased FA in both disorders. In summary, evidence seems to support the notion that white matter integrity appears to be affected in ASD and ADHD with studies implicating widespread abnormalities throughout the brain.
To our knowledge only two structural studies directly comparing ASD and ADHD have been done. Both studies compared children and adolescents. Several findings in these studies lend support to some of the conclusions presented in this paper. A direct comparison of patients with ASD and ADHD revealed that ADHD exhibited significantly smaller total brain volume and GM volume than ASD and controls (Lim et al. 2015) although Brieber et al. (2007) reported no difference in total GM volume with a smaller sample size. In temporal lobe regions both studies have reported abnormalities in ASD and ADHD although the nature of these differences varies. Lim et al. (2015) report GM increases in left middle/superior temporal gyrus and medial frontal gyrus in ASD compared to ADHD and controls, but this only held true for the comparison with the ADHD group without correcting for multiple comparisons (Lim et al. 2015). In contrast, Brieber et al. (2007) report shared reductions compared to controls in left medial temporal regions in ASD and ADHD as well as ASD specific increases in GM near temporo-parietal junction compared to controls and subjects with ADHD. Additionally, Lim et al. (2015) reported smaller posterior cerebellum in ADHD compared to ASD and controls (Lim et al. 2015). The findings from these studies lend some support to the notion that temporal, frontal, and cerebellar abnormalities may be present in both disorders in addition to possible differences in total brain volume.
In our review we have arrived at some similar conclusions for some of the regions put forth previously by Rommelse et al. (2011). Specifically, we have found similar conclusions for total brain volume, corpus callosum, and cerebellum, although we report additional evidence for sub-region specific abnormalities in the splenium of the corpus callosum in ADHD as well as lobules VIII to X in the cerebellum. By contrast, Rommelse et al. (2011) found that ASD exhibits focal differences in cortical thickness especially in regions responsible for social cognition, however, current evidence for regional abnormalities in cortical thickness in ASD is inconsistent. Additionally, recent studies indicate that cortical thickness is dynamic and region-specific (Zielinski et al. 2014) hence studies of cortical thickness should examine its trajectory as comparisons at a specific time point fail to accurately capture the developmental nature of cortical regions.
Limitations of this Review
The studies reported in this review differ in the statistical parameters and techniques used to analyze study data and here we discuss an overall summary of these inconsistencies. Choice of statistical threshold can result in more subtle differences being dismissed as non-significant. Most studies use a p-value threshold of 0.05 but a few use more strict thresholds. In addition, some studies correct for multiple comparisons. Other differences can be found in the statistical model applied. Many studies choose to regress IQ, or control for age, gender (when applicable), and in some instances brain volume when examining specific regions. There is currently controversy as to whether studies should control for IQ with some suggesting IQ should only be considered a covariate when samples are unrepresentative of the disorder in question (Dennis et al. 2009). Given the developmental nature of these disorders covarying for age is prudent and is widely practiced, but there is no current consensus on whether IQ should be considered a covariate.
Another important consideration, especially in DTI studies, is subject motion. A recent study, indicated many of the reported widespread abnormalities in ASD disappear when accounting for head motion and data quality with only the inferior longitudinal fasciculus remaining significant (Koldewyn et al. 2014). In contrast, several studies reviewed which quantitatively examined and controlled for differences in motion still report widespread white matter abnormalities in ASD (Shukla et al. 2010; Gibbard et al. 2013; Groen et al. 2011). The findings of the Koldewyn et al. study do emphasize the importance of correcting for head motion and controlling for data quality in DTI studies. The majority of DTI studies reviewed in this paper account for at least some level of motion. Across studies, this ranges from simple head immobilization, sedation, data quality inspection, to examination of group differences in head translation and rotation in x, y, and z axes. Most studies do not quantify the degree of motion observed in groups, however, and we therefore cannot comment on whether motion played a role in observed group differences; we can only emphasize the importance of rigorously controlling for motion in DTI studies to prevent any spurious group differences.
Another factor that must be acknowledged in reviewing studies on developmental disorders is the bias in neurodevelopmental imaging literature toward higher functioning individuals. Because it is difficult to scan lower functioning individuals with developmental disorders due to movement and/or non-compliance, studies often exclude individuals with IQs below 70. The majority of studies examined in our review do not include subjects with IQ less than 70. As such brain features of lower functioning individuals are not as well characterized. This makes it difficult to speculate how inclusion of lower functioning individuals would affect group differences. We can only hypothesize that more severely impaired individuals would manifest brains which exhibit greater deviance from normal.
It is worth noting that although some abnormalities may be common to both disorders, these findings were derived from ASD versus control and ADHD versus control studies. Further support for these findings would need to be made using direct ADHD versus ASD studies. Very few studies have directly compared ASD and ADHD (Brieber et al. 2007; Christakou et al. 2013; Di Martino et al. 2013; Lim et al. 2015) and to our knowledge only two have examined structural features (Brieber et al. 2007; Lim et al. 2015). Additionally, with the current literature it is not possible to examine these disorders at all stages of development. We have therefore attempted to indicate overall developmental trends in these regions throughout the paper when possible.
All studies reviewed in this article do not necessarily follow the exact same set of image acquisition (scanner, pulse sequence, etc.), image processing and statistical analyses techniques. As such, in addition to the heterogeneity in subject inclusion criteria there are technical differences between the studies reviewed here and this is a limitation. Although there can be technical variability between studies, what is reported in the review are the common findings that emerge across studies.
Finally, the findings presented in this review reflect results from studies which look at differences in group means and do not necessarily indicate a finding is absent or present across all subjects.
Direction for Future Research
A recent area of interest in the study of neurodevelopmental disorders is the significant rate of comorbidity and symptom overlap among disorders regarded as distinct. Several models have attempted to explain this overlap and comorbidity. Gillberg, for example, has coined the concept of ESSENCE (Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Evaluations) to describe the multitude of overlapping clinical conditions such as ASD, ADHD, language disorder, developmental coordination disorder, intellectual disability, and tic disorders, among others (Gillberg and Fernell 2014; Gillberg et al. 2013). In our own previous work (Moreno-De-Luca et al. 2013) we proposed that, rather than being regarded as causally and pathophysiologically distinct, neurodevelopmental disorders should be thought of as different patterns of symptoms reflecting a common underlying neurodevelopmental continuum, resulting in a host of disorders we refer to as Developmental Brain Dysfunction, or DBD.
Similarly, the recent Research Domain Criteria project (RDoC) initiative by the NIMH proposes a new dimensional paradigm for the study of psychopathology (National Institute of Mental Health 2011). In this initiative diagnostic categories are not used as the basis of investigation, rather, observable behaviors and neural measures are used to work toward a classification system which relates to clinical phenomena. This new system for conducting research poses an advantage over diagnostic systems which fail to account for the significant heterogeneity in clinical presentation demonstrated by a group of individuals who bear the same diagnosis. In addition, the RDoC approach provides a better alternative for diagnoses that have overlapping clinical presentations by quantifying the domains of dysfunction as in ASD and ADHD. Symptoms such as hyperactivity, inattentiveness, language delay, irritability, and social impairment appear in both disorders and blur diagnostic distinctions (Mayes et al. 2012).
The majority of studies used in this review use traditional diagnostic categories to form study cohorts. We therefore acknowledge the limitations of this review in this respect and present our findings as a starting point for further investigation. We suggest that future neuroimaging studies should focus more on domains of dysfunction and recognize that symptoms/phenotypes are distributed on a continuum with significant variance within diagnoses. It is highly likely that subsets of individuals within an ASD diagnostic category have ADHD symptoms and vice versa. Each of these subcategories may have unique neural profiles. This failure to account for comorbidity may contribute to the mixed and sometimes contradictory results (see “unclear” in Table 1) that exist in current neuroimaging literature.
To this end we suggest that rather than combine diverse symptom expressions into one diagnostic category, research would be better served if symptoms were given precedence as stated in the RDoC. Study cohorts formed based on diagnostic categories can incorrectly dichotomize subjects into ASD and not ASD or ADHD and not ADHD. Instead, acknowledging that behavioral traits exist on spectrums from healthy to pathological, can better discern relationships between neural substrates and behaviors. For example, if the goal of a study is to determine the neural substrates of a behavior, merely searching for group differences may hide important brain-behavior relationships.
In Fig. 3 we present an illustrative example to demonstrate the advantages of correlating across an entire phenotypic spectrum over calculating t-test between two groups. Suppose Feature 1 is a behavioral phenotype and Feature 2 a brain feature. In Fig. 3a, two groups clearly segregate based on Feature 1. A t-test is then performed to determine if there is a significant difference in Feature 2 between groups which results in a significant p-value (p = 1.2E-4) and correlation coefficient across both groups (r = .66, p = 6.3E-6). In this instance this approach works well because Feature 1 is clearly separated between groups and there is not much overlap in Feature 2. In Fig. 3b, however, we show a case (using the original data from Fig. 3a with additional subjects) where features may not be clearly separated such as in ASD and ADHD. In this instance a t-test searching for group differences in Feature 2 fails to retain significance (p = .053). Instead, if we search for a correlation between Feature 1 and Feature 2 across groups we see an increase in the correlation coefficient (r = .76, p = 1.6E-9).
A comparison of t-test between two groups versus correlation across a spectrum. a Demonstrates a significant correlation between Feature 1 (a behavioral phenotype) and Feature 2 (a brain feature) as well as significant group differences in Feature 2. b In b, however, it can be demonstrated, that when Features 1 and 2 are not clearly separated, group differences can fail to remain significant in spite of the presence of highly significant correlations between Features 1 and 2 across the entire phenotype. Because of this, searching only for group differences may miss significant brain-behavior relationships. (Figure 3 generated in MATLAB R2013b)
For this reason, significant heterogeneity between two groups may lead to non-significant t-values; but when the entire spectrum of a specific phenotype is considered, significant correlations between brain features and behavior may emerge. In our opinion, studies should search for brain imaging markers that display significant associations with the severity of dysfunction, instead of dichotomizing the subjects to seek brain imaging differences. Diagnostic categories can be crude approximations which fail to account for heterogeneity and comorbidity hence a great degree of overlap may occur and confound results. Because diagnostic categories serve a useful clinical purpose it has become accepted practice to classify participants in clinical research in a similar manner. But increasingly it is becoming apparent that controls and patients in studies are not as dichotomous as previously thought. By focusing on domains of dysfunction rather than diagnostic categories our ability to detect which brain profiles lead to which behavioral phenotypes would be greatly enhanced.
Another factor that should be acknowledged is the fact that ASD and ADHD may have the same or different genetic etiologies. Current knowledge of ASD and ADHD genes is limited, but a few copy number variants (CNV) such as 1q21.1, 5p13, 9q33, 15q13.3, 16p13, 16p11.2 have been put forth as candidates for shared etiology (A. Moreno-De-Luca et al. 2013; Rommelse et al. 2010). Different genetic mutations may lead to important differences among ADHD and ASD individuals. By controlling for multiple genetic etiologies it may be possible to define clinical subgroups which display phenotypic differences within ASD and ADHD as well as other neurodevelopmental disorders (Simons VIP Consortium 2012). Examining specific genetic mutations may offer another way of delineating the overlap in neurodevelopmental disorders. In addition, this approach may allow for targeted treatments that produce better outcomes for patients. As our knowledge of the genetic etiologies of neurodevelopmental disorders increases, forming cohorts based on specific genetic etiologies may help reduce the significant heterogeneity in these and other neurodevelopmental disorders and further aid our understanding of their diverse nature.
A final consideration when performing research on neurodevelopmental disorders is the fact that neurodevelopmental disorders are by their very nature in a state of flux. Studies which make use of heterogeneous age groups are unlikely to produce informative results given that a subject with ASD or ADHD at age five presents with different neural substrates than adults at eighteen. Efforts should be made to recruit subjects with little variance in age to prevent developmental confounds and produce more informative results. In addition to this, more longitudinal studies would also aid this process and make it much easier to determine the developmental trajectory of various substrates not only in ASD and ADHD, but across neurodevelopmental disorders. From our review only limited research has been done on the longitudinal development of various neural substrates such as the corpus callosum, amygdala, basal ganglia, and prefrontal cortex. Even less is known about the development of the white matter tracts mentioned in this paper. It is therefore not possible to rule out the possibility of age specific abnormalities in these and other neurodevelopmental disorders. A given brain structure or feature may be found to be abnormal in childhood, but these differences may disappear with age.
Conclusion
The nature of co-morbidity in various neurodevelopmental and neuropsychiatric disorders has been a challenge to researchers and clinicians alike. Rather than viewing co-morbidity as the expression of multiple separate and distinct disorders, recent work emphasizes that such occurrences may be better explained by a variety of factors: problems with reliability and discriminant validity of certain diagnoses; the overlap in symptom expression across disorders; the fact that different symptoms or diagnoses may represent alternative phenotypes of a common genotype, and conversely, that similar symptom expression may result across a number of copy number variations (Gillberg 2010; Pettersson et al. 2013; Moreno-De-Luca et al. 2013, 2014).
Future neuroimaging studies of neurodevelopmental disorders should approach these disorders from the perspective of symptom-to-brain relationships rather than disorder-to-brain relationships. Similarly, a focus on genetic etiology may also eliminate heterogeneity and allow researchers to determine if specific genetic mutations produce specific brain profiles. We offer the findings in this review as a starting point for future efforts which can further describe the diverse nature of both disorders. Differentiating disorders based on brain-symptom relationships will be an important step in understanding the similarities and differences across neurodevelopmental disorders and may eventually offer new targets for individualized treatment.
References
Adisetiyo, V., Tabesh, A., Di Martino, A., Falangola, M. F., Castellanos, F. X., Jensen, J. H., et al. (2014). Attention‐deficit/hyperactivity disorder without comorbidity is associated with distinct atypical patterns of cerebral microstructural development. Human Brain Mapping, 35(5), 2148–2162.
Adolphs, R., Tranel, D., & Damasio, A. R. (1998). The human amygdala in social judgment. Nature, 393(6684), 470–474.
Alexander, A. L., Lee, J. E., Lazar, M., Boudos, R., DuBray, M. B., Oakes, T. R., et al. (2007). Diffusion tensor imaging of the corpus callosum in Autism. NeuroImage, 34(1), 61–73.
Allen, G., Müller, R.-A., & Courchesne, E. (2004). Cerebellar function in autism: functional magnetic resonance image activation during a simple motor task. Biological Psychiatry, 56(4), 269–278.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington: American Psychiatric Publishing.
Aoki, Y., Kasai, K., & Yamasue, H. (2012). Age-related change in brain metabolite abnormalities in autism: a meta-analysis of proton magnetic resonance spectroscopy studies. Translational Psychiatry, 2(1), e69.
Aoki, Y., Abe, O., Nippashi, Y., & Yamasue, H. (2013). Comparison of white matter integrity between autism spectrum disorder subjects and typically developing individuals: a meta-analysis of diffusion tensor imaging tractography studies. Molecular Autism, 4(1), 25.
Ara, S., & Islam, M. (2010). White fiber dissection of brain; the internal capsule: a cadaveric study. Turkish Neurosurgery, 20(3), 314–322.
Arnsten, A. F. (2009). The emerging neurobiology of attention deficit hyperactivity disorder: the key role of the prefrontal association cortex. The Journal of Pediatrics, 154(5), I.
Ashtari, M., Kumra, S., Bhaskar, S. L., Clarke, T., Thaden, E., Cervellione, K. L., et al. (2005). Attention-deficit/hyperactivity disorder: a preliminary diffusion tensor imaging study. Biological Psychiatry, 57(5), 448–455.
Axer, H., & Keyserlingk, D. G. (2000). Mapping of fiber orientation in human internal capsule by means of polarized light and confocal scanning laser microscopy. Journal of Neuroscience Methods, 94(2), 165–175.
Barnea-Goraly, N., Kwon, H., Menon, V., Eliez, S., Lotspeich, L., & Reiss, A. L. (2004). White matter structure in autism: preliminary evidence from diffusion tensor imaging. Biological Psychiatry, 55(3), 323–326.
Barnea-Goraly, N., Lotspeich, L. J., & Reiss, A. L. (2010). Similar white matter aberrations in children with autism and their unaffected siblings: a diffusion tensor imaging study using tract-based spatial statistics. Archives of General Psychiatry, 67(10), 1052–1060.
Barnea-Goraly, N., Frazier, T. W., Piacenza, L., Minshew, N. J., Keshavan, M. S., Reiss, A. L., et al. (2014). A preliminary longitudinal volumetric MRI study of amygdala and hippocampal volumes in autism. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 48, 124–128.
Baron-Cohen, S., Ring, H. A., Bullmore, E. T., Wheelwright, S., Ashwin, C., & Williams, S. (2000). The amygdala theory of autism. Neuroscience & Biobehavioral Reviews, 24(3), 355–364.
Bashat, D. B., Kronfeld-Duenias, V., Zachor, D. A., Ekstein, P. M., Hendler, T., Tarrasch, R., et al. (2007). Accelerated maturation of white matter in young children with autism: a high b value DWI study. NeuroImage, 37(1), 40–47.
Batty, M. J., Liddle, E. B., Pitiot, A., Toro, R., Groom, M. J., Scerif, G., et al. (2010). Cortical gray matter in attention-deficit/hyperactivity disorder: a structural magnetic resonance imaging study. Journal of the American Academy of Child and Adolescent Psychiatry, 49(3), 229–238.
Bechtel, N., Kobel, M., Penner, I.-K., Klarhöfer, M., Scheffler, K., Opwis, K., et al. (2009). Decreased fractional anisotropy in the middle cerebellar peduncle in children with epilepsy and/or attention deficit/hyperactivity disorder: a preliminary study. Epilepsy & Behavior, 15(3), 294–298.
Berquin, P., Giedd, J., Jacobsen, L., Hamburger, S., Krain, A., Rapoport, J., et al. (1998). Cerebellum in attention-deficit hyperactivity disorder A morphometric MRI study. Neurology, 50(4), 1087–1093.
Bledsoe, J. C., Semrud-Clikeman, M., & Pliszka, S. R. (2011). Neuroanatomical and neuropsychological correlates of the cerebellum in children with attention-deficit/hyperactivity disorder–combined type. Journal of the American Academy of Child and Adolescent Psychiatry, 50(6), 593–601.
Boddaert, N., Chabane, N., Gervais, H., Good, C., Bourgeois, M., Plumet, M., et al. (2004). Superior temporal sulcus anatomical abnormalities in childhood autism: a voxel-based morphometry MRI study. NeuroImage, 23(1), 364–369.
Brieber, S., Neufang, S., Bruning, N., Kamp‐Becker, I., Remschmidt, H., Herpertz‐Dahlmann, B., et al. (2007). Structural brain abnormalities in adolescents with autism spectrum disorder and patients with attention deficit/hyperactivity disorder. Journal of Child Psychology and Psychiatry, 48(12), 1251–1258.
Brun, C. C., Nicolson, R., Leporé, N., Chou, Y. Y., Vidal, C. N., DeVito, T. J., et al. (2009). Mapping brain abnormalities in boys with autism. Human Brain Mapping, 30(12), 3887–3900.
Bush, G. (2011). Cingulate, frontal, and parietal cortical dysfunction in attention-deficit/hyperactivity disorder. Biological Psychiatry, 69(12), 1160–1167.
Cao, Q., Sun, L., Gong, G., Lv, Y., Cao, X., Shuai, L., et al. (2010). The macrostructural and microstructural abnormalities of corpus callosum in children with attention deficit/hyperactivity disorder: a combined morphometric and diffusion tensor MRI study. Brain Research, 1310, 172–180.
Carper, R. A., & Courchesne, E. (2000). Inverse correlation between frontal lobe and cerebellum sizes in children with autism. Brain, 123(4), 836–844.
Carper, R. A., & Courchesne, E. (2005). Localized enlargement of the frontal cortex in early autism. Biological Psychiatry, 57(2), 126–133.
Carper, R. A., Moses, P., Tigue, Z. D., & Courchesne, E. (2002). Cerebral lobes in autism: early hyperplasia and abnormal age effects. NeuroImage, 16(4), 1038–1051.
Cascio, C., Styner, M., Smith, R. G., Poe, M. D., Gerig, G., Hazlett, H. C., et al. (2006). Reduced relationship to cortical white matter volume revealed by tractography-based segmentation of the corpus callosum in young children with developmental delay. American Journal of Psychiatry, 163(12), 2157–2163.
Castellanos, F. X., & Tannock, R. (2002). Neuroscience of attention-deficit/hyperactivity disorder: the search for endophenotypes. Nature Reviews Neuroscience, 3(8), 617–628.
Castellanos, F. X., Giedd, J. N., Marsh, W. L., Hamburger, S. D., Vaituzis, A. C., Dickstein, D. P., et al. (1996). Quantitative brain magnetic resonance imaging in attention-deficit hyperactivity disorder. Archives of General Psychiatry, 53(7), 607–616.
Castellanos, F. X., Lee, P. P., Sharp, W., Jeffries, N. O., Greenstein, D. K., Clasen, L. S., et al. (2002). Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. JAMA, 288(14), 1740–1748.
Catani, M., Jones, D. K., Daly, E., Embiricos, N., Deeley, Q., Pugliese, L., et al. (2008). Altered cerebellar feedback projections in Asperger syndrome. NeuroImage, 41(4), 1184–1191.
Cheng, Y., Chou, K.-H., Chen, I.-Y., Fan, Y.-T., Decety, J., & Lin, C.-P. (2010). Atypical development of white matter microstructure in adolescents with autism spectrum disorders. NeuroImage, 50(3), 873–882.
Christakou, A., Murphy, C., Chantiluke, K., Cubillo, A., Smith, A., Giampietro, V., et al. (2013). Disorder-specific functional abnormalities during sustained attention in youth with attention deficit hyperactivity disorder (ADHD) and with autism. Molecular Psychiatry, 18(2), 236–244.
Chung, M. K., Robbins, S. M., Dalton, K. M., Davidson, R. J., Alexander, A. L., & Evans, A. C. (2005). Cortical thickness analysis in autism with heat kernel smoothing. NeuroImage, 25(4), 1256–1265.
Cortese, S., Imperati, D., Zhou, J., Proal, E., Klein, R. G., Mannuzza, S., et al. (2013). White matter alterations at 33-year follow-up in adults with childhood attention-deficit/hyperactivity disorder. Biological Psychiatry, 74(8), 591–598.
Courchesne, E., Carper, R., & Akshoomoff, N. (2003). Evidence of brain overgrowth in the first year of life in autism. JAMA, 290(3), 337–344.
Courchesne, E., Pierce, K., Schumann, C. M., Redcay, E., Buckwalter, J. A., Kennedy, D. P., et al. (2007). Mapping early brain development in autism. Neuron, 56(2), 399–413.
Courchesne, E., Mouton, P. R., Calhoun, M. E., Semendeferi, K., Ahrens-Barbeau, C., Hallet, M. J., et al. (2011). Neuron number and size in prefrontal cortex of children with autism. JAMA, 306(18), 2001–2010.
Davis, M. (1992). The role of the amygdala in fear and anxiety. Annual Review of Neuroscience, 15(1), 353–375.
Dennis, M., Francis, D. J., Cirino, P. T., Schachar, R., Barnes, M. A., & Fletcher, J. M. (2009). Why IQ is not a covariate in cognitive studies of neurodevelopmental disorders. Journal of the International Neuropsychological Society, 15(03), 331–343.
Di Martino, A., Kelly, C., Grzadzinski, R., Zuo, X.-N., Mennes, M., Mairena, M. A., et al. (2011). Aberrant striatal functional connectivity in children with autism. Biological Psychiatry, 69(9), 847–856.
Di Martino, A., Zuo, X.-N., Kelly, C., Grzadzinski, R., Mennes, M., Schvarcz, A., et al. (2013). Shared and distinct intrinsic functional network centrality in autism and attention-deficit/hyperactivity disorder. Biological Psychiatry, 74(8), 623–632.
Dictionary of Biological Psychology (2003). London: Routledge.
Dramsdahl, M., Westerhausen, R., Haavik, J., Hugdahl, K., & Plessen, K. J. (2012). Adults with attention-deficit/hyperactivity disorder—a diffusion-tensor imaging study of the corpus callosum. Psychiatry Research: Neuroimaging, 201(2), 168–173.
Durston, S., Pol, H. E. H., Schnack, H. G., Buitelaar, J. K., Steenhuis, M. P., Minderaa, R. B., et al. (2004). Magnetic resonance imaging of boys with attention-deficit/hyperactivity disorder and their unaffected siblings. Journal of the American Academy of Child and Adolescent Psychiatry, 43(3), 332–340.
Ecker, C., Rocha-Rego, V., Johnston, P., Mourao-Miranda, J., Marquand, A., Daly, E. M., et al. (2010). Investigating the predictive value of whole-brain structural MR scans in autism: a pattern classification approach. NeuroImage, 49(1), 44–56.
Ecker, C., Ginestet, C., Feng, Y., Johnston, P., Lombardo, M. V., Lai, M.-C., et al. (2013). Brain surface anatomy in adults with autism: the relationship between surface area, cortical thickness, and autistic symptoms. JAMA Psychiatry, 70(1), 59–70.
Ellison-Wright, I., Ellison-Wright, Z., & Bullmore, E. (2008). Structural brain change in attention deficit hyperactivity disorder identified by meta-analysis. BMC Psychiatry, 8(1), 51.
Estes, A., Shaw, D. W., Sparks, B. F., Friedman, S., Giedd, J. N., Dawson, G., et al. (2011). Basal ganglia morphometry and repetitive behavior in young children with autism spectrum disorder. Autism Research, 4(3), 212–220.
Evans, D. W., Lewis, M. D., & Iobst, E. (2004). The role of the orbitofrontal cortex in normally developing compulsive-like behaviors and obsessive–compulsive disorder. Brain and Cognition, 55(1), 220–234.
Evans, D. W., Lazar, S. M., Boomer, K., Mitchel, A. D., Michael, A. M., & Moore, G. J. (2014). Social cognition and brain morphology: implications for developmental brain dysfunction. Brain Imaging and Behavior, 9(2), 264–274.
Fatemi, S. H., Aldinger, K. A., Ashwood, P., Bauman, M. L., Blaha, C. D., Blatt, G. J., et al. (2012). Consensus paper: pathological role of the cerebellum in autism. The Cerebellum, 11(3), 777–807.
Frazier, T. W., & Hardan, A. Y. (2009). A meta-analysis of the corpus callosum in autism. Biological Psychiatry, 66(10), 935–941.
Frazier, T. W., Keshavan, M. S., Minshew, N. J., & Hardan, A. Y. (2012). A two-year longitudinal MRI study of the corpus callosum in autism. Journal of Autism and Developmental Disorders, 42(11), 2312–2322.
Freitag, C. M., Luders, E., Hulst, H. E., Narr, K. L., Thompson, P. M., Toga, A. W., et al. (2009). Total brain volume and corpus callosum size in medication-naive adolescents and young adults with autism spectrum disorder. Biological Psychiatry, 66(4), 316–319.
Frodl, T., & Skokauskas, N. (2012). Meta‐analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects. Acta Psychiatrica Scandinavica, 125(2), 114–126.
Frodl, T., Stauber, J., Schaaff, N., Koutsouleris, N., Scheuerecker, J., Ewers, M., et al. (2010). Amygdala reduction in patients with ADHD compared with major depression and healthy volunteers. Acta Psychiatrica Scandinavica, 121(2), 111–118.
Gibbard, C. R., Ren, J., Seunarine, K. K., Clayden, J. D., Skuse, D. H., & Clark, C. A. (2013). White matter microstructure correlates with autism trait severity in a combined clinical–control sample of high-functioning adults. NeuroImage, 3, 106–114.
Gillberg, C. (2010). The ESSENCE in child psychiatry: early symptomatic syndromes eliciting neurodevelopmental clinical examinations. Research in Developmental Disabilities, 31(6), 1543–1551.
Gillberg, C., & Fernell, E. (2014). Autism plus versus autism pure. Journal of Autism and Developmental Disorders, 44(12), 3274–3276.
Gillberg, C., Fernell, E., & Minnis, H. (2013). Early symptomatic syndromes eliciting neurodevelopmental clinical examinations. The Scientific World Journal, 2013.
Gilliam, M., Stockman, M., Malek, M., Sharp, W., Greenstein, D., Lalonde, F., et al. (2011). Developmental trajectories of the corpus callosum in attention-deficit/hyperactivity disorder. Biological Psychiatry, 69(9), 839–846.
Girgis, R. R., Minshew, N. J., Melhem, N. M., Nutche, J. J., Keshavan, M. S., & Hardan, A. Y. (2007). Volumetric alterations of the orbitofrontal cortex in autism. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 31(1), 41–45.
Groen, W. B., Buitelaar, J. K., Van Der Gaag, R. J., & Zwiers, M. P. (2011). Pervasive microstructural abnormalities in autism: a DTI study. Journal of Psychiatry & Neuroscience, 36(1), 32.
Grzadzinski, R., Di Martino, A., Brady, E., Mairena, M. A., O’Neale, M., Petkova, E., et al. (2011). Examining autistic traits in children with ADHD: does the autism spectrum extend to ADHD? Journal of Autism and Developmental Disorders, 41(9), 1178–1191.
Haar, S., Berman, S., Behrmann, M., & Dinstein, I. (2014). Anatomical abnormalities in autism? Cerebral Cortex, bhu242.
Hadjikhani, N., Joseph, R. M., Snyder, J., & Tager-Flusberg, H. (2006). Anatomical differences in the mirror neuron system and social cognition network in autism. Cerebral Cortex, 16(9), 1276–1282.
Hamilton, L. S., Levitt, J. G., O’Neill, J., Alger, J. R., Luders, E., Phillips, O. R., et al. (2008). Reduced white matter integrity in attention-deficit hyperactivity disorder. Neuroreport, 19(17), 1705.
Hardan, A., Minshew, N. J., & Keshavan, M. S. (2000). Corpus callosum size in autism. Neurology, 55(7), 1033–1036.
Hardan, A., Muddasani, S., Vemulapalli, M., Keshavan, M. S., & Minshew, N. J. (2006). An MRI study of increased cortical thickness in autism. American Journal of Psychiatry, 163(7), 1290–1292.
Hardan, A., Libove, R., Keshavan, M., Melhem, N., & Minshew, N. (2009). A preliminary longitudinal magnetic resonance imaging study of brain volume and cortical thickness in autism. Biological Psychiatry, 66(4), 320–326.
Hazlett, H. C., Poe, M., Gerig, G., Smith, R. G., Provenzale, J., Ross, A., et al. (2005). Magnetic resonance imaging and head circumference study of brain size in autism: birth through age 2 years. Archives of General Psychiatry, 62(12), 1366–1376.
Hazlett, H. C., Poe, M. D., Gerig, G., Styner, M., Chappell, C., Smith, R. G., et al. (2011). Early brain overgrowth in autism associated with an increase in cortical surface area before age 2 years. Archives of General Psychiatry, 68(5), 467–476.
Herbert, M. R., Ziegler, D. A., Makris, N., Filipek, P. A., Kemper, T. L., Normandin, J. J., et al. (2004). Localization of white matter volume increase in autism and developmental language disorder. Annals of Neurology, 55(4), 530–540.
Hill, D. E., Yeo, R. A., Campbell, R. A., Hart, B., Vigil, J., & Brooks, W. (2003). Magnetic resonance imaging correlates of attention-deficit/hyperactivity disorder in children. Neuropsychology, 17(3), 496.
Hoekzema, E., Carmona, S., Ramos-Quiroga, J. A., Fernández, V. R., Picado, M., Bosch, R., et al. (2012). Laminar thickness alterations in the fronto-parietal cortical mantle of patients with attention-deficit/hyperactivity disorder.
Hollander, E., Anagnostou, E., Chaplin, W., Esposito, K., Haznedar, M. M., Licalzi, E., et al. (2005). Striatal volume on magnetic resonance imaging and repetitive behaviors in autism. Biological Psychiatry, 58(3), 226–232.
Hong, S.-B., Zalesky, A., Fornito, A., Park, S., Yang, Y.-H., Park, M.-H., et al. (2014). Connectomic disturbances in attention-deficit/hyperactivity disorder: a whole-brain tractography analysis. Biological Psychiatry, 76(8), 656–663.
Hoppenbrouwers, M., Vandermosten, M., & Boets, B. (2014). Autism as a disconnection syndrome: a qualitative and quantitative review of diffusion tensor imaging studies. Research in Autism Spectrum Disorders, 8(4), 387–412.
Hua, X., Thompson, P. M., Leow, A. D., Madsen, S. K., Caplan, R., Alger, J. R., et al. (2013). Brain growth rate abnormalities visualized in adolescents with autism. Human Brain Mapping, 34(2), 425–436.
Ikuta, T., Shafritz, K. M., Bregman, J., Peters, B. D., Gruner, P., Malhotra, A. K., et al. (2014). Abnormal cingulum bundle development in autism: a probabilistic tractography study. Psychiatry Research: Neuroimaging, 221(1), 63–68.
Jiao, Y., Chen, R., Ke, X., Chu, K., Lu, Z., & Herskovits, E. H. (2010). Predictive models of autism spectrum disorder based on brain regional cortical thickness. NeuroImage, 50(2), 589–599.
Jou, R., Mateljevic, N., Kaiser, M., Sugrue, D., Volkmar, F., & Pelphrey, K. (2011a). Structural neural phenotype of autism: preliminary evidence from a diffusion tensor imaging study using tract-based spatial statistics. American Journal of Neuroradiology, 32(9), 1607–1613.
Jou, R. J., Jackowski, A. P., Papademetris, X., Rajeevan, N., Staib, L. H., & Volkmar, F. R. (2011b). Diffusion tensor imaging in autism spectrum disorders: preliminary evidence of abnormal neural connectivity. Australian and New Zealand Journal of Psychiatry, 45(2), 153–162.
Keller, T. A., Kana, R. K., & Just, M. A. (2007). A developmental study of the structural integrity of white matter in autism. Neuroreport, 18(1), 23–27.
Koldewyn, K., Yendiki, A., Weigelt, S., Gweon, H., Julian, J., Richardson, H., et al. (2014). Differences in the right inferior longitudinal fasciculus but no general disruption of white matter tracts in children with autism spectrum disorder. Proceedings of the National Academy of Sciences, 111(5), 1981–1986.
Kumar, A., Sundaram, S. K., Sivaswamy, L., Behen, M. E., Makki, M. I., Ager, J., et al. (2010). Alterations in frontal lobe tracts and corpus callosum in young children with autism spectrum disorder. Cerebral Cortex, 20(9), 2103–2113.
Langen, M., Bos, D., Noordermeer, S. D., Nederveen, H., van Engeland, H., & Durston, S. (2014). Changes in the development of striatum are involved in repetitive behavior in autism. Biological Psychiatry, 76(5), 405–411.
Langevin, L. M., MacMaster, F. P., Crawford, S., Lebel, C., & Dewey, D. (2014). Common white matter microstructure alterations in pediatric motor and attention disorders. The Journal of Pediatrics, 164(5), 1157–1164. e1151.
Leitner, Y. (2014). The co-occurrence of autism and attention deficit hyperactivity disorder in children–what do we know? Frontiers in Human Neuroscience, 8.
Levitt, J. G., Blanton, R. E., Smalley, S., Thompson, P., Guthrie, D., McCracken, J. T., et al. (2003). Cortical sulcal maps in autism. Cerebral Cortex, 13(7), 728–735.
Lewis, J. D., Theilmann, R. J., Sereno, M. I., & Townsend, J. (2009). The relation between connection length and degree of connectivity in young adults: a DTI analysis. Cerebral Cortex, 19(3), 554–562.
Lim, L., Chantiluke, K., Cubillo, A., Smith, A., Simmons, A., Mehta, M., et al. (2015). Disorder-specific grey matter deficits in attention deficit hyperactivity disorder relative to autism spectrum disorder. Psychological Medicine, 45(05), 965–976.
Mackie, S., Shaw, P., Lenroot, R., Pierson, R., Greenstein, D. K., Nugent, T. F., III, et al. (2007). Cerebellar development and clinical outcome in attention deficit hyperactivity disorder. The American Journal of Psychiatry, 164(4), 647–655.
Makris, N., Kennedy, D. N., McInerney, S., Sorensen, A. G., Wang, R., Caviness, V. S., et al. (2005). Segmentation of subcomponents within the superior longitudinal fascicle in humans: a quantitative, in vivo, DT-MRI study. Cerebral Cortex, 15(6), 854–869.
Makris, N., Biederman, J., Valera, E. M., Bush, G., Kaiser, J., Kennedy, D. N., et al. (2007). Cortical thinning of the attention and executive function networks in adults with attention-deficit/hyperactivity disorder. Cerebral Cortex, 17(6), 1364–1375.
Makris, N., Buka, S. L., Biederman, J., Papadimitriou, G. M., Hodge, S. M., Valera, E. M., et al. (2008). Attention and executive systems abnormalities in adults with childhood ADHD: a DT-MRI study of connections. Cerebral Cortex, 18(5), 1210–1220.
Manes, F., Piven, J., Vrancic, D., Nanclares, V., Plebst, C., & Starkstein, S. E. (1999). An MRI study of the corpus callosum and cerebellum in mentally retarded autistic individuals. The Journal of Neuropsychiatry and Clinical Neurosciences, 11(4), 470–474.
Mayes, S. D., Calhoun, S. L., Mayes, R. D., & Molitoris, S. (2012). Autism and ADHD: overlapping and discriminating symptoms. Research in Autism Spectrum Disorders, 6(1), 277–285.
McAlonan, G., Daly, E., Kumari, V., Critchley, H. D., van Amelsvoort, T., Suckling, J., et al. (2002). Brain anatomy and sensorimotor gating in Asperger’s syndrome. Brain, 125(7), 1594–1606.
McAlonan, G., Cheung, V., Cheung, C., Suckling, J., Lam, G. Y., Tai, K., et al. (2005). Mapping the brain in autism. A voxel-based MRI study of volumetric differences and intercorrelations in autism. Brain, 128(2), 268–276.
McAlonan, G., Cheung, V., Cheung, C., Chua, S. E., Murphy, D. G., Suckling, J., et al. (2007). Mapping brain structure in attention deficit-hyperactivity disorder: a voxel-based MRI study of regional grey and white matter volume. Psychiatry Research: Neuroimaging, 154(2), 171–180.
Metzler-Baddeley, C., Jones, D. K., Steventon, J., Westacott, L., Aggleton, J. P., & O’Sullivan, M. J. (2012). Cingulum microstructure predicts cognitive control in older age and mild cognitive impairment. The Journal of Neuroscience, 32(49), 17612–17619.
Moreno-De-Luca, A., Myers, S. M., Challman, T. D., Moreno-De-Luca, D., Evans, D. W., & Ledbetter, D. H. (2013). Developmental brain dysfunction: revival and expansion of old concepts based on new genetic evidence. Lancet Neurology, 12(4), 406–414.
Moreno-De-Luca, D., Moreno-De-Luca, A., Cubells, J. F., & Sanders, S. J. (2014). Cross-disorder comparison of four neuropsychiatric CNV Loci. Current Genetic Medicine Reports, 2(3), 151–161.
Mostofsky, S. H., Reiss, A. L., Lockhart, P., & Denckla, M. B. (1998). Evaluation of cerebellar size in attention-deficit hyperactivity disorder. Journal of Child Neurology, 13(9), 434–439.
Mostofsky, S. H., Cooper, K. L., Kates, W. R., Denckla, M. B., & Kaufmann, W. E. (2002). Smaller prefrontal and premotor volumes in boys with attention-deficit/hyperactivity disorder. Biological Psychiatry, 52(8), 785–794.
Mulligan, A., Anney, R. J., O’Regan, M., Chen, W., Butler, L., Fitzgerald, M., et al. (2009). Autism symptoms in attention-deficit/hyperactivity disorder: a familial trait which correlates with conduct, oppositional defiant, language and motor disorders. Journal of Autism and Developmental Disorders, 39(2), 197–209.
National Institute of Mental Health (2011). NIMH: Research Domain Criteria (RDoC). http://www.nimh.nih.gov/research-priorities/rdoc/nimh-research-domain-criteria-rdoc.shtml.
Nordahl, C. W., Lange, N., Li, D. D., Barnett, L. A., Lee, A., Buonocore, M. H., et al. (2011). Brain enlargement is associated with regression in preschool-age boys with autism spectrum disorders. Proceedings of the National Academy of Sciences, 108(50), 20195–20200.
Nordahl, C. W., Scholz, R., Yang, X., Buonocore, M. H., Simon, T., Rogers, S., et al. (2012). Increased rate of amygdala growth in children aged 2 to 4 years with autism spectrum disorders: a longitudinal study. Archives of General Psychiatry, 69(1), 53–61.
Panizzon, M. S., Fennema-Notestine, C., Eyler, L. T., Jernigan, T. L., Prom-Wormley, E., Neale, M., et al. (2009). Distinct genetic influences on cortical surface area and cortical thickness. Cerebral Cortex, bhp026.
Pavuluri, M. N., Yang, S., Kamineni, K., Passarotti, A. M., Srinivasan, G., Harral, E. M., et al. (2009). Diffusion tensor imaging study of white matter fiber tracts in pediatric bipolar disorder and attention-deficit/hyperactivity disorder. Biological Psychiatry, 65(7), 586–593.
Perlov, E., Philipsen, A., van Elst, L. T., Ebert, D., Henning, J., Maier, S., et al. (2008). Hippocampus and amygdala morphology in adults with attention-deficit hyperactivity disorder. Journal of Psychiatry & Neuroscience, 33(6), 509.
Pettersson, E., Anckarsäter, H., Gillberg, C., & Lichtenstein, P. (2013). Different neurodevelopmental symptoms have a common genetic etiology. Journal of Child Psychology and Psychiatry, 54(12), 1356–1365.
Plessen, K. J., Bansal, R., Zhu, H., Whiteman, R., Amat, J., Quackenbush, G. A., et al. (2006). Hippocampus and amygdala morphology in attention-deficit/hyperactivity disorder. Archives of General Psychiatry, 63(7), 795–807.
Pliszka, S. R., Lancaster, J., Liotti, M., & Semrud-Clikeman, M. (2006). Volumetric MRI differences in treatment-naive vs chronically treated children with ADHD. Neurology, 67(6), 1023–1027.
Proal, E., Reiss, P. T., Klein, R. G., Mannuzza, S., Gotimer, K., Ramos-Olazagasti, M. A., et al. (2011). Brain gray matter deficits at 33-year follow-up in adults with attention-deficit/hyperactivity disorder established in childhood. Archives of General Psychiatry, 68(11), 1122–1134.
Qiu, A., Crocetti, D., Adler, M., Mahone, E. M., Denckla, M. B., Miller, M. I., et al. (2009). Basal ganglia volume and shape in children with attention deficit hyperactivity disorder.
Rao, P. A., & Landa, R. J. (2014). Association between severity of behavioral phenotype and comorbid attention deficit hyperactivity disorder symptoms in children with autism spectrum disorders. Autism, 18(3), 272–280.
Raznahan, A., Toro, R., Daly, E., Robertson, D., Murphy, C., Deeley, Q., et al. (2009). Cortical anatomy in autism spectrum disorder: an in vivo MRI study on the effect of age. Cerebral Cortex, bhp198.
Reiersen, A. M., Constantino, J. N., & Todd, R. D. (2008). Co-occurrence of motor problems and autistic symptoms in attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 47(6), 662–672.
Rommelse, N. N., Franke, B., Geurts, H. M., Hartman, C. A., & Buitelaar, J. K. (2010). Shared heritability of attention-deficit/hyperactivity disorder and autism spectrum disorder. European Child & Adolescent Psychiatry, 19(3), 281–295.
Rommelse, N. N., Geurts, H. M., Franke, B., Buitelaar, J. K., & Hartman, C. A. (2011). A review on cognitive and brain endophenotypes that may be common in autism spectrum disorder and attention-deficit/hyperactivity disorder and facilitate the search for pleiotropic genes. Neuroscience & Biobehavioral Reviews, 35(6), 1363–1396.
Scheel, C., Rotarska-Jagiela, A., Schilbach, L., Lehnhardt, F. G., Krug, B., Vogeley, K., et al. (2011). Imaging derived cortical thickness reduction in high-functioning autism: key regions and temporal slope. NeuroImage, 58(2), 391–400.
Schnoebelen, S., Semrud-Clikeman, M., & Pliszka, S. R. (2010). Corpus callosum anatomy in chronically treated and stimulant naive ADHD. Journal of Attention Disorders, 14(3), 256–266.
Schumann, C. M., & Amaral, D. G. (2006). Stereological analysis of amygdala neuron number in autism. The Journal of Neuroscience, 26(29), 7674–7679.
Schumann, C. M., Barnes, C. C., Lord, C., & Courchesne, E. (2009). Amygdala enlargement in toddlers with autism related to severity of social and communication impairments. Biological Psychiatry, 66(10), 942–949.
Schumann, C. M., Bloss, C. S., Barnes, C. C., Wideman, G. M., Carper, R. A., Akshoomoff, N., et al. (2010). Longitudinal magnetic resonance imaging study of cortical development through early childhood in autism. The Journal of Neuroscience, 30(12), 4419–4427.
Scott, J. A., Schumann, C. M., Goodlin‐Jones, B. L., & Amaral, D. G. (2009). A comprehensive volumetric analysis of the cerebellum in children and adolescents with autism spectrum disorder. Autism Research, 2(5), 246–257.
Seidman, L. J., Valera, E. M., & Makris, N. (2005). Structural brain imaging of attention-deficit/hyperactivity disorder. Biological Psychiatry, 57(11), 1263–1272.
Seidman, L. J., Biederman, J., Liang, L., Valera, E. M., Monuteaux, M. C., Brown, A., et al. (2011). Gray matter alterations in adults with attention-deficit/hyperactivity disorder identified by voxel based morphometry. Biological Psychiatry, 69(9), 857–866.
Shadmehr, R., & Krakauer, J. W. (2008). A computational neuroanatomy for motor control. Experimental Brain Research, 185(3), 359–381.
Shallice, T. (2001). Theory of mind’ and the prefrontal cortex. Brain, 124(2), 247–248.
Shaw, P., Eckstrand, K., Sharp, W., Blumenthal, J., Lerch, J., Greenstein, D., et al. (2007). Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proceedings of the National Academy of Sciences, 104(49), 19649–19654.
Shaw, P., Malek, M., Watson, B., Sharp, W., Evans, A., & Greenstein, D. (2012). Development of cortical surface area and gyrification in attention-deficit/hyperactivity disorder. Biological Psychiatry, 72(3), 191–197.
Shukla, D. K., Keehn, B., Lincoln, A. J., & Müller, R.-A. (2010). White matter compromise of callosal and subcortical fiber tracts in children with autism spectrum disorder: a diffusion tensor imaging study. Journal of the American Academy of Child & Adolescent Psychiatry, 49(12), 1269–1278. e1262.
Shukla, D. K., Keehn, B., & Müller, R. A. (2011). Tract‐specific analyses of diffusion tensor imaging show widespread white matter compromise in autism spectrum disorder. Journal of Child Psychology and Psychiatry, 52(3), 286–295.
Silk, T. J., Vance, A., Rinehart, N., Bradshaw, J. L., & Cunnington, R. (2009). White‐matter abnormalities in attention deficit hyperactivity disorder: a diffusion tensor imaging study. Human Brain Mapping, 30(9), 2757–2765.
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47(8), 921–929.
Simons VIP Consortium. (2012). Simons Variation in Individuals Project (Simons VIP): a genetics-first approach to studying autism spectrum and related neurodevelopmental disorders. Neuron, 73(6), 1063–1067.
Sowell, E. R., Thompson, P. M., Welcome, S. E., Henkenius, A. L., Toga, A. W., & Peterson, B. S. (2003). Cortical abnormalities in children and adolescents with attention-deficit hyperactivity disorder. The Lancet, 362(9397), 1699–1707.
Stanfield, A. C., McIntosh, A. M., Spencer, M. D., Philip, R., Gaur, S., & Lawrie, S. M. (2008). Towards a neuroanatomy of autism: a systematic review and meta-analysis of structural magnetic resonance imaging studies. European Psychiatry, 23(4), 289–299.
Stoodley, C. J., & Schmahmann, J. D. (2010). Evidence for topographic organization in the cerebellum of motor control versus cognitive and affective processing. Cortex, 46(7), 831–844.
Takahashi, M., Iwamoto, K., Fukatsu, H., Naganawa, S., Iidaka, T., & Ozaki, N. (2010). White matter microstructure of the cingulum and cerebellar peduncle is related to sustained attention and working memory: a diffusion tensor imaging study. Neuroscience Letters, 477(2), 72–76.
Valera, E. M., Faraone, S. V., Murray, K. E., & Seidman, L. J. (2007). Meta-analysis of structural imaging findings in attention-deficit/hyperactivity disorder. Biological Psychiatry, 61(12), 1361–1369.
van der Meer, J. M., Oerlemans, A. M., van Steijn, D. J., Lappenschaar, M. G., de Sonneville, L. M., Buitelaar, J. K., et al. (2012). Are autism spectrum disorder and attention-deficit/hyperactivity disorder different manifestations of one overarching disorder? Cognitive and symptom evidence from a clinical and population-based sample. Journal of the American Academy of Child and Adolescent Psychiatry, 51(11), 1160–1172. e1163.
van Ewijk, H., Heslenfeld, D. J., Zwiers, M. P., Buitelaar, J. K., & Oosterlaan, J. (2012). Diffusion tensor imaging in attention deficit/hyperactivity disorder: a systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 36(4), 1093–1106.
Van’t Ent, D., Lehn, H., Derks, E., Hudziak, J., Van Strien, N., Veltman, D., et al. (2007). A structural MRI study in monozygotic twins concordant or discordant for attention/hyperactivity problems: evidence for genetic and environmental heterogeneity in the developing brain. NeuroImage, 35(3), 1004–1020.
Vidal, C. N., Nicolson, R., DeVito, T. J., Hayashi, K. M., Geaga, J. A., Drost, D. J., et al. (2006). Mapping corpus callosum deficits in autism: an index of aberrant cortical connectivity. Biological Psychiatry, 60(3), 218–225.
von dem Hagen, E. A., Nummenmaa, L., Yu, R., Engell, A. D., Ewbank, M. P., & Calder, A. J. (2011). Autism spectrum traits in the typical population predict structure and function in the posterior superior temporal sulcus. Cerebral Cortex, 21(3), 493–500.
Wallace, G. L., Robustelli, B., Dankner, N., Kenworthy, L., Giedd, J. N., & Martin, A. (2013). Increased gyrification, but comparable surface area in adolescents with autism spectrum disorders. Brain, awt106.
Weinstein, M., Ben‐Sira, L., Levy, Y., Zachor, D. A., Itzhak, E. B., Artzi, M., et al. (2011). Abnormal white matter integrity in young children with autism. Human Brain Mapping, 32(4), 534–543.
Wolosin, S. M., Richardson, M. E., Hennessey, J. G., Denckla, M. B., & Mostofsky, S. H. (2009). Abnormal cerebral cortex structure in children with ADHD. Human Brain Mapping, 30(1), 175–184.
Zielinski, B. A., Prigge, M. B., Nielsen, J. A., Froehlich, A. L., Abildskov, T. J., Anderson, J. S., et al. (2014). Longitudinal changes in cortical thickness in autism and typical development. Brain, 137(6), 1799–1812.
Zikopoulos, B., & Barbas, H. (2010). Changes in prefrontal axons may disrupt the network in autism. The Journal of Neuroscience, 30(44), 14595–14609.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dougherty, C.C., Evans, D.W., Myers, S.M. et al. A Comparison of Structural Brain Imaging Findings in Autism Spectrum Disorder and Attention-Deficit Hyperactivity Disorder. Neuropsychol Rev 26, 25–43 (2016). https://doi.org/10.1007/s11065-015-9300-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-015-9300-2