Abstract
In the past two decades, there has been an increased interest in the assessment and treatment of preschool children presenting with concerns about attention problems. This article reviews the research and clinical literature involving assessment of attention and related skills in the preschool years. While inattention among preschoolers is common, symptoms alone do not necessarily indicate a disorder, and most often represent a normal variation in typical preschool child development. Thus, accurate identification of “disordered” attention in preschoolers can be challenging, and development of appropriate, norm-referenced tests of attention for preschoolers is also difficult. The current review suggests that comprehensive assessment of attention and related functions in the preschool child should include thorough review of the child’s history, planned observations, and formal psychometric testing. The three primary methods of psychometric assessment that have been used to characterize attentional functioning in preschool children include performance-based tests, structured caregiver interviews, and rating scales (parent, teacher, and clinician). Among performance-based methods for measurement of attention in the preschool years, tests have been developed to assess sustained attention, selective (focused) attention, span of attention (encoding/manipulation), and (top-down) controlled attention—including freedom from distractibility and set shifting. Many of these tests remain experimental in nature, and review of published methods yields relatively few commercially available, nationally normed tests of attention for preschoolers, and an overall dearth of reliability and validity studies on the available measures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Attention Problems in Preschoolers
Attention problems are common among preschool children. By the age of 4 years, as many as 40 % of children have sufficient problems with attention to be of concern to parents and preschool teachers (Palfrey et al. 1985). Symptoms of inattention, even those falling short of formal diagnosis of Attention-deficit/Hyperactivity Disorder (ADHD) are observed to be as high as 3 to 15 % in community samples and 50 % or higher among clinical referrals (Christophersen and Mortweet 2003). For example, the number of preschoolers described as “always on the go/driven by a motor” is as high as 72.7 % (Pavuluri et al. 1999). Inattention among preschoolers is not always indicative of ADHD, and may represent a variety of alternative or co-existing conditions, including language disorders, hearing loss, low intellectual functioning, or other forms of psychopathology. Most often, though, inattention is a normal variation observed in typical preschool child development, making identification of “disordered” attention more problematic (Mahone 2005), especially given the tremendous variability in caregiver ratings of attention and endorsed symptoms of ADHD in this age group (Stefanatos and Baron 2007). In the past two decades, there has been an increased interest in the assessment and treatment of preschool children presenting with attention problems, especially those associated with symptoms of ADHD, i.e., distractibility and hyperactivity (Shelton and Barkley 1993). It has been asserted that earlier identification and treatment of attention problems may minimize the harmful impact of childhood disorders, and facilitate appropriate diagnosis, or just as importantly, non-diagnosis (Wilens et al. 2002b).
In the preschool years, ADHD is now the most commonly diagnosed form of psychopathology (Armstrong and Nettleton 2004), and the prevalence estimates appear to be increasing. For example, DeBar and colleagues (DeBar et al. 2003) reported the occurrence of ADHD to be 2 % in a sample of 38,664 general pediatric patients under the age of 5 years, while Conners and Staff (2000) reported that the incidence might be as high as 59 % in child psychiatry clinics. In another sample of 200 children age 6 years and younger referred to an outpatient psychiatric clinic, 86 % met diagnostic criteria for ADHD (Wilens et al. 2002a). The preponderance of research findings suggest that preschool children presenting with disrupted attentional skills are at significant risk for social (Rapport et al. 1999), developmental (Newborg et al. 1988), and academic difficulties (Stefanatos and Baron 2007), relative to typically developing children (American Academy of Pediatrics 2000), including multiple developmental deficits (Yochman et al. 2006) as well as diagnosis of ADHD and/or other psychopathology in the school-age years (Lahey et al. 2004; 2006; Massetti, et al. 2007; McGee et al. 1991; Wilens et al. 2002b). Attention problems in preschool are also associated with poor social adjustment and frequent emergency medical visits during adolescence (Greenhill et al. 2008). Even sub-threshold ADHD in early childhood has been shown to be associated with later academic failure and grade retention (Bussing et al. 2010). Preschool children who actually meet formal diagnostic criteria for ADHD are at even higher risk for behavior problems 6 years later (Lahey et al. 2006), as well as depression and suicidal behavior by age 18 (Chronis-Tuscano, et al. 2010). The Centers for Disease Control estimated that between 1998 and 2009, nearly 9 % of children in the US (1 in 11 children between the ages of 5 and 17) have ADHD, with boys receiving the diagnosis approximately twice as often as girls (Akinbami et al. 2011). Nevertheless, the proportion of girls exhibiting attention problems has also increased rapidly over the past two decades. A recent large epidemiological study of 3,907 children found that of the 8.7 % who met DSM-IV-TR criteria for ADHD, 51 % were boys and 49 % were girls (Froehlich et al. 2007).
While early identification and treatment of attention problems in preschoolers may minimize the adverse impact (Sonuga-Barke et al. 2011), prior to age 4 years, it is difficult to characterize the behavioral features specifically associated with ADHD (or other co-existing disorders), and to distinguish them from attentional difficulties that occur in typically developing children (Smidts and Oosterlaan 2007). Some researchers have noted that preschool children who meet criteria for the Inattentive ADHD subtype are actually more likely to go on to have reading, spelling, and mathematics problems compared with those presenting with primarily hyperactive/impulsive behaviors, who are more likely to go on to develop ADHD (Massetti et al. 2007). Other investigators have questioned whether the Inattentive subtype of ADHD is meaningful at all in the preschool years; Egger and colleagues noted that the Inattentive subtype of ADHD occurs in fewer than 1 in 1,000 preschoolers in the general population (Egger et al. 2006). Given these considerations, development of valid objective methods for assessing attention in preschool children is particularly important. Since diagnostic thresholds tend to be viewed though the expectations of those applying the standards (i.e., parents, teachers), what is considered a “disorder” can change over time (Sonuga-Barke et al. 2011), and relying on parent or teacher reports of child symptoms in isolation can lead to over-identification of disorders (Gimpel and Kuhn 2000). Further, when impairment criteria from the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR; American Psychiatric Association–APA 2000) are used carefully in diagnosing preschoolers, fewer children actually meet formal diagnostic criteria for ADHD (Healey et al. 2008).
Additionally, while ADHD is presently treated as a categorical phenomenon for the purposes of DSM-IV-TR, the syndrome more likely represents dimensional variations rather than a categorical entity (Sonuga-Barke et al. 2011), and the DSM-V is likely to reflect these changes (APA 2012; Stefanatos and Baron 2007). Thus, psychometrically sound assessment methods can help quantify these dimensions more accurately, and can facilitate diagnostic accuracy in young children.
Risk Factors for Attention Problems in Preschoolers
Early developmental differences involving attentional control in preschoolers are considered to arise from a variety of influences, including genetic (Biederman and Faraone 2002), temperamental (Nigg et al. 2004), and environmental (Pauli-Pott and Becker 2011) factors. A recent longitudinal study of over 2,000 children from Canada, who were followed from age 5 months to 8 years, showed that the strongest early predictors of attention problems included premature birth, low birth weight, prenatal tobacco exposure, non-intact family, young maternal age, paternal history of antisocial behavior, and maternal depression (Galera et al. 2011). Similarly, a recent study conducted in Israel found that several parameters observed during infancy (birth-1 month) were significantly associated with later development of ADHD: advanced maternal age, lower maternal education, family history of ADHD, and family history of social problems. Between 3 and 18 months, decrease in head circumference, delay in motor and language milestones, and difficult temperament were all significantly associated with later onset of ADHD, suggesting that temperament, family environment, and early developmental delays are significant risk factors in the preschool years (Gurevitz et al. 2012). As part of the Family Life Project, researchers evaluated behavior and associated risk factors for attention problems among preschoolers ages 3–5 years. They observed that symptoms of inattention and hyperactivity occurred along a single latent factor that did not vary over the preschool years. Further, they observed that low caregiver educational level was the single best predictor of symptom severity (Willoughby et al. 2012).
In the past decade, there has also been increasing concern regarding the amount of screen media used by young children and its relationship with early attention problems. Using retrospective data from the National Longitudinal Survey of Youth, researchers found that number of hours of television watched per day at age 1 and 3 years was associated with attention problems at age 7 years (Christakis et al. 2004). There may even be immediate cognitive effects of short-term television viewing in young children. In a recently published study, children who watched a fast-paced television show (specifically a popular fantastical cartoon about an animated sponge that lives under the sea), performed more poorly on a Tower of Hanoi test immediately after viewing than those who had not watched the show (Lillard and Peterson 2011). These associations remain controversial, however, and there is still a question of whether inattention, per se, represents a cause or an effect of increased television viewing. Nevertheless, the American Academy of Pediatrics (AAP) has taken a conservative approach to television viewing by young children, and has recommended no screen time for children under age 2 years and no more than 1–2 h a day of quality television and media for older children (AAP 2011).
Neuropsychological Models of Attention
Attention encompasses several important neuropsychological processes that develop rapidly during the preschool years, including the ability to focus on and attend to stimuli over a period of time and the capacity to take in and report back stimuli immediately after presentation (White et al. 2009). Attention can be considered the foundation on which most other cognitive and neuropsychological functions develop (Cooley and Morris 1990). Multiple models of attention in the adult brain have been articulated; however, fewer have been translated to apply clinically to the assessment of children (Mahone 2005). When attentional models are applied to younger children, there exists greater overlap with other developing skills, e.g., executive function, language, visuospatial skills (White et al. 2009), and tests designed to measure attention are affected by (and dependent on) skill development in these other neurobehavioral domains. The prominent neuropsychological models of attention, and their relationship to behavior among preschoolers, are outlined below.
Selective Attention
As humans, our senses are constantly bombarded by stimuli. Because there are limits to the capacity of human information processing, development of goal-directed behavior requires a high degree of selectivity within the attentional system (Lachter et al. 2004). To this end, Broadbent (1958) proposed a selective filter model of attention in which stimuli are selected via top-down control to be processed further, while non-selected (filtered) information is not processed beyond the extraction of its basic physical features. This filtering mechanism becomes more efficient over the course of early development as children use a larger proportion of their attentional capacities to focus on relevant tasks or stimuli (Lane and Pearson 1982). Broadbent’s theory provided the basis for other contemporary attentional theories (described below), especially those involving selective attention. The selective attention system includes two competing processes: bottom-up and top-down. Bottom-up attention occurs when the brain automatically orients or attends to sensory features in the environment that stand out in some way. Conversely, top-down attention involves conscious (effortful) control of attention toward some target (including shifting of attention). Bottom-up attention has long been considered to be dependent on the posterior parietal cortex, whereas top-down attention is considered to be dependent on the prefrontal cortex and its connections. However, more recent evidence from studies in primates suggests that the dorsolateral prefrontal cortex is also involved in visually based bottom-up selective attention (Katsuki and Constantinidis 2012).
Pribram and McGuinness (1975) proposed a related theory in which arousal, activation, and effort act as essential elements in controlled attention. In their model, arousal is defined by the orienting response to sensory input (bottom-up), and is considered dependent on the brainstem, reticular system, and hypothalamus. As children mature beyond the preschool years toward adolescence, forebrain control over this system (top-down) is exerted by the amygdala and frontal cortex—which regulate arousal (phasic, short term attention), and by the basal ganglia—which regulate activation (tonic, longer lasting attention). Pribram and McGuinness highlighted the importance of automatic and effortful cognitive processes in understanding attentional control. In their model, automatic processing is performed without intention. It is necessarily brief, not limited by short-term memory, and preferentially processed by the left cerebral hemisphere. Conversely, effortful (conscious, top-down, frontally-mediated) processing, which invokes limitations on one’s capacity, is necessarily slower, uses serial processing, and is used for novel information (Goldberg and Costa 1981).
Posner and Peterson (Peterson and Posner 2012; Posner and Peterson 1990) have asserted that attention is not carried out in a single section of the brain, but rather in a network of regions that complete different, complementary functions. This attentional network is considered separate from the systems of the brain that process data. In the Posner and Peterson model, three primary functions of the attention network are sensory orientation, detection and conscious processing of signals, and maintaining a state of alertness. Visual orienting, which is probably the most relevant to performance-based tests of attention in children, is considered a primary function of the posterior parietal cortex, as well as the lateral pulvinar nucleus of the postereolateral thalamus, and the superior colliculus, with each part carrying out a specific function important in disengaging from a previous focus, shifting, and encoding information from the new stimuli. Posner has asserted that when a target is detected, the brain disengages from a general state of alertness, orients in order to process specific information from that target, and prepares to respond to those specific signals. The brain then maintains a more specific pattern of alertness in order to continue processing (or orienting to) signals with a higher priority. This activation appears to occur primarily in the right hemisphere and involves the noradrenergic system, which is considered to increase the rate of selection of high priority visual information.
Selective or focused attention as described in the models above is often measured using paradigms in which an individual is given two or more concurrent stimuli (or dimensions of stimuli) and must attend to one and ignore the others (Cooley and Morris 1990). Examples of selective attention measures include: perceptual matching tasks, in which individuals are shown pictures or objects and asked to indicate if a picture is same or different than another; central-incidental learning tasks, in which individuals are given stimuli representing two or more categories, with one designated as central (or important), and then asked to recall both central and non-central (incidental) details; and, visual search or cancellation tasks (described below) in which individuals are asked to search a visual display for a predetermined target.
Divided Attention
A criticism of the Broadbent (1958) and other theories of selective attention is that they do not adequately account for simultaneous or parallel processing, requiring divided attention (Lachter et al. 2004). Divided attention is required when one is given two concurrent tasks or stimuli and instructed to respond to both components. Tasks requiring divided attention differ from selective attention tasks by virtue of the additional demand for number of items attended to, thus requiring additional top-down control (Cooley and Morris 1990). A common method for assessing divided attention is the dual-task interference paradigm, in which (for example) performance on a task is carried out alone, and then contrasted with performance on the same task performed at the same time as a competing task. NEPSY Statue (described below) is an example of a divided attention task that can be used in preschoolers.
Sustained Attention
Sustained attention or vigilance involves the maintenance of attention over time, and is often based on paradigms that require individuals to detect changes in stimuli over longer periods of time, such as continuous performance tests (Cooley and Morris 1990). In a model based primarily on factor analytic methods applied to neuropsychological measures in adults and children, Mirsky and colleagues (Mirsky et al. 1991) were among the first to use continuous performance tests to measure sustained attention. In their studies, Mirsky and colleagues suggested that there are at least four distinct attention functions. These four functions included: focus-execute (i.e., target selection and response—similar to selective attention), sustain (i.e., vigilance, persistence), shift (i.e., flexibility of attentional focus), and encode (i.e., registration, mental manipulation, and recall of information). Similar factors were observed in adults and in children. The authors suggested that while each factor was localized to a different part of the brain, the regions work together as an organized system. “Sustained” attention was dependent on midbrain and brainstem; shifting with the prefrontal cortex; focused attention with the superior temporal cortex, inferior parietal cortex, and corpus striatum; and, encoding with the hippocampus and amygdala. Since Mirsky’s model was based on performance-based tests of attention, it translates easily to the clinical setting, and several computerized continuous performance tests for preschoolers have been developed and normed (see descriptions of tests below).
Attention and Executive Control Functions
There has been a concurrent interest in characterizing problems with attention and executive control functions in preschool children, driven in part by the increase in early identification of psychiatric and neurodevelopmental conditions (Espy 2004). In the preschool years, these executive function skills have significant overlap with the developmental constructs measured in assessment of attention (Mahone 2005; Mahone et al. 2001; Mahone et al. 2005). Like their school-age counterparts, preschool children with attention problems may also present with significant executive dysfunction, although the pattern and trajectory of these behaviors in preschoolers may be different than that observed in school-age children (Arons et al. 2002; Byrne et al. 1998), with hyperactivity and impulse control (more than inattention and organization) observed as the primary problems (Byrne et al. 2000; Mahone et al. 2005; Mahone and Hoffman 2007). This profile, however, may simply reflect what is demanded or expected of a preschool child. Like attention, individual characteristics of executive dysfunction change and are exhibited differently throughout development, from preschool through adult life (Root and Resnick 2003), and are elicited by environmental demands. Among preschoolers, however, both attention and executive function skills can be directly facilitated by provision of externally guided, attention-directing behaviors, usually initiated by the parent (Conway and Stifter 2012).
A number of theories have attempted to capture the developmental overlap between attention and executive function. For example, Knudsen’s model of attention (Knudsen 2007) emphasized the role of top-down control of both attention and behavior. The model suggests that there are four essential components of attention: working memory, competitive selection, top-down sensitivity control, and salience filters. Sensory information is filtered for what are either behaviorally important, instinctive stimuli, or infrequent stimuli in a bottom-up approach. The stimuli are encoded and go through competitive selection based on relative signal strength in order to determine what gets access to working memory. Working memory (a core executive function) uses the information to direct subsequent behaviors, as well as direct attention using a frontally mediated, top-down approach. The sensitivity of the information is regulated to improve signal-to-noise and attend only to the information relative to stimuli involved in necessary actions or judgments, and to selectively direct the necessary stimuli to be further encoded. Knudson argued that these tasks are dependent on the development of the prefrontal cortex.
Barkley’s model of executive function (Barkley 2011a) also highlights the dynamic overlap between executive control and elements of attention. His theory emphasized the developmental unfolding of self-regulation and top-down control of behavior as a marker of prefrontal cortex development, and cites at least six key executive functions: self-restraint (executive inhibition), self-directed sensory-motor action (nonverbal working memory), self-directed private speech (verbal working memory), self-directed emotion/motivation (inhibition of strong emotions), self-directed play (planning, innovation, generativity), and self-directed attention (self-awareness). As a theory with a more direct link to top-down control, Barkley’s model has been linked more directly to ADHD than to disorders in which bottom-up or posterior attention systems are more affected. While performance-based tests of the model have been developed, their ecological validity has been criticized, and Barkley has emphasized the importance of rating scales for measuring elements of the model (Barkley 2011b).
Recently, Dennis and colleagues (Dennis et al. 2008) highlighted the importance of situational factors in determining the relationship between attention and executive function. Their model considered the integrated nature of stimulus orienting and response control, by considering the elements of each that are more related to attention networks (i.e., bottom-up), or to executive control networks (i.e., top-down). In their model, orientation to stimuli can occur as a result of a bottom-up (passive, external stimulus driven) or top-down (task driven, internally directed) approach. Response to stimuli can occur in a preprogramed, model-driven, performance and reward-based approach (bottom-up), or in a more top-down approach using instructions and attention priorities. In both stimulus orientating and response control, the individual is involved in three (potentially simultaneous) cognitive processes: activation (directing specific attention), inhibition (voluntary or automatic avoidance or cessation of response), and adjustment (performance monitoring and contingency adjustment), all of which interact dynamically to produce goal-directed behaviors.
Attention and Brain Development in Preschoolers
Development of the human nervous system begins 2–3 weeks after conception (Black et al. 1990). Brain systems underlying attentional control are among the earliest to develop, with continued maturation into at least early adulthood (Gogtay et al. 2004). The trajectory of functional development, however, is nonlinear, and progresses in a region-specific manner that coincides with maturation of different brain systems (Halperin and Schulz 2006). By age 2 years, the brain is approximately 80 % of its adult size (Giedd et al. 1999). Subsequently, synapse formation (Huttenlocher and Dabholkar 1997) and myelination (Kinney et al. 1988) proceed rapidly up to age 2 years, followed by a plateau phase, during which neurons begin to form complex dendritic trees (Mrzljak et al. 1990). Maximum synaptic density (i.e., synaptic overproduction) is observed at age 3 months in the primary auditory cortex, but not until age 15 months in the prefrontal cortex (Huttenlocher and Dabholkar 1997). After age 5 years, brain development is marked by continued neuronal growth, experience-dependent pruning of inefficient synapses, and cortical organization (Gogtay et al. 2004), with eventual reduction of synaptic density to 60 % of its earlier maximum (Huttenlocher and Dabholkar 1997).
Functional development of attention in the preschool years occurs via a process of active neural development—largely genetically determined—but also through a dynamic process of shaping and constraining abilities through experience, potentially modifying genetic expression (Blair and Raver 2012). The idea of experiential canalization, described by Gottlieb (1991), notes that functional development is shaped concurrently by biology as well as experience (or opportunity). In normal development, this “shaping” occurs via progressive myelination and associated cortical thinning, and is associated with improvements in attentional control. Conversely, pathological pruning (affected in part by experience) may contribute to the disrupted development of attentional skills (Kotrla and Weinberger 2000; Marsh et al. 2008), including ADHD (Sowell et al. 2003; Shaw et al. 2007).
The prefrontal cortex, which has a prominent role in the development of controlled (top-down) attention, has a protracted period of development, with rapid changes beginning in the first year of life (Diamond 2002), that continue into young adulthood (Luna et al. 2001). There is evidence that maturation of the prefrontal cortex and its connections during infancy sets the stage for emergence of many “higher” cognitive processes, including top-down control of attention (Columbo and Cheatham 2006; Kraybill and Bell 2012). Prefrontal development in infancy and toddlerhood has been most commonly measured via electrophysiology (EEG; Fox et al. 2007), such that frontal EEG power (considered a measure of neuronal excitability) is observed to be associated with controlled attention in toddlers (Morasch and Bell 2011).
Over the first year of life, the development of attention is most commonly assessed behaviorally using visual attention paradigms (Columbo 2001). In the first 3 months of life, infants are visually attracted to objects with contours and/or edges (e.g., faces, checkerboards), and exhibit long visual fixations. During this period, infants have difficulty disengaging visual attention from objects. This difficulty is likely because the pathways from the basal ganglia to the superior colliculus have begun to develop at that time, whereas the parietal lobes have yet to mature (Hood and Atkinson 1993). Experimental paradigms used in infancy often include habituation and paired comparison, variants of which have been incorporated into infant development scales (e.g., Bayley Scales of Infant and Toddler Development, Third Edition; Bayley 2006). Object novelty preference typically begins to emerge in infants around age 4–6 months, and is thought to coincide with the maturation of the cortical visual system and the parietal cortex. During this period, infants’ visual gaze time decreases and visual disengagement occurs. By 7–12 months, gaze time begins to increase again, and is accompanied by a shift from involuntary to more voluntary control, which continues to develop throughout toddlerhood and the preschool years (Columbo 2001).
The development of neural systems supporting attentional control occurs at different rates in boys and girls (De Bellis et al. 2001). At birth, girls are already considered to be 3 weeks ahead of boys in terms of physical maturation; 1 year ahead by school entry (Eme 1992). Although there are few reported sex differences in problem behavior in infancy and early childhood; sex differences appear to emerge by age 4 years, with boys showing more aggressive and impulsive behaviors. The change in behavior among girls may be a function of more rapid neurobiological, cognitive, motor, and social development, which, in preschool, may be protective against the manifestation of some ADHD symptoms in early childhood (Biederman et al. 2008). Sexual dimorphism in cerebral development may also contribute to the observed differences in attention problems. Giedd and colleagues compiled normative growth curves, demonstrating the sexual dimorphism in brain development (Lenroot et al. 2007). From age 4 to 20 years, linear increases in white matter volume with age were observed, whereas age-related changes in gray matter were nonlinear, regionally specific, and differed for boys and girls. Total cerebral gray matter volume was 10 % larger in boys, but peaked much earlier in girls than boys (10.5 years vs. 14 years). The trajectory was identical for the caudate, which also showed peak at age 10.5 for girls and 14 for boys. Frontal lobe gray matter volume peaked around 10.5 years for boys (9.5 years for girls), and declined during post-adolescence resulting in an overall net decrease across the age span. Results were similar for parietal lobe volumes and differed only in that the slope of the curve was steeper and volumes peaked 1.5 years earlier for each sex (9.0 years for boys, 7.5 years for girls). Similarly, temporal lobe volumes peaked age 11 years for boys and 10 years for girls.
Interventions for Attention Problems in Preschoolers
Behavioral Interventions
A variety of programs have been developed to target improvements in behaviors associated with ADHD, including inattention and self-control. Two such programs, Triple P (Bor et al. 2002) and The Incredible Years (Jones et al. 2008), which emphasize parent training, have been shown to be effective in reducing disruptive behaviors, more so than behaviors associated with attentional control (Halperin et al. 2012a). Similarly, in a randomized control trial of a treatment program for preschoolers focusing on self-regulation and mother-child interactions (i.e., the Revised New Forest Parent Programme), the authors reported a reduction in symptoms associated with ADHD up to 9 weeks after conclusion of treatment (Thompson et al. 2009). More recently, Halperin and colleagues (Halperin et al. 2012b) developed a novel method for training attention and other cognitive skills in preschoolers that has shown initial promise. Their Training Executive, Attention, and Motor Skills program utilized parent-directed small groups (3–4 parent–child dyads), that employed “games” emphasizing attention, inhibitory control, working memory, planning, visuospatial skills, and motor skills. Groups occurred daily for 30–45 min, and treatments lasted approximately 5–8 weeks. Preliminary evidence suggested that parent and teacher ratings of attention improved (relative to baseline) after completion of treatment, with gains maintained at three-month follow up (Halperin et al. 2012a).
Pharmacotherapy
The practice of prescribing psychotropic medications for very young children has increased in both the US and Europe (Connor 2002). For example, Rappley et al. (2002) reported on 223 children age 3 years and younger who were receiving treatment for attention problems. More than half of their sample received treatment in an idiosyncratic manner, and had monitoring less than once every 3 months. In an attempt to improve knowledge about assessment and treatment of attention problems in young children, the NIMH began a clinical trial in 2000 to study the effects of methylphenidate in preschoolers (ages 3–6 years) with ADHD. This study, known as the Preschool ADHD Treatment Study (PATS) has begun to shed light on diagnostic methods and treatments for ADHD and other attentional disorders in the preschool years (Vitiello et al. 2007), including safety of stimulants (Greenhill et al. 2006), short-term (Abikoff et al. 2007) and long-term effectiveness (Vitiello et al. 2007), and associated side effects (Ghuman et al. 2001), including reduced growth rates among preschoolers treated with stimulants (Swanson et al. 2006). In one sample of preschoolers with ADHD treated with stimulant medication, more than 82 % of the sample saw improvement in behavior ratings by at least one standard deviation (Short et al. 2004). The presumed mechanism of action of stimulants, which has been established via studies of older children and adults (but not among preschoolers), is by increasing the availability of catecholamines (especially dopamine and norepinephrine) in the synaptic cleft (Pliszka 2007). Given the preponderance of these neurotransmitters in the fronto-striatal circuitry, stimulants have primary action on attentional functions affecting top down control, and improvement in these skills has been observed in preschool children (Abikoff et al. 2007). From these studies, the American Academy of Pediatrics has recently addressed the use of stimulant medication in preschool children (ages 4–5 years), and has recommended using stimulant medications only in those preschool-aged children with symptoms of ADHD who have moderate-to-severe symptoms that have persisted for at least 9 months, with dysfunction manifested in both the home and other settings such as preschool or child care, and who have not responded adequately to behavior therapy (AAP 2011).
To date, there have been only two published studies of pharmacological treatment of preschool children with non-stimulant medication—both with atomoxetine, a selective norepinephrine reuptake inhibitor. An open-label study of atomoxetine (titrated to 1.8 mg/kg/day) with 12 preschool children ages 3–5 years showed adequate tolerability and reduction of parent reported hyperactivity and impulsivity from baseline (Ghuman et al. 2009). More recently, a larger, 8-week, double blind, placebo-controlled, randomized clinical trial of atomoxetine (titrated to 1.8 mg/kg/day) in 101 children with ADHD (ages 5–6 years) led to significant reductions in core symptoms of inattention (observed by parents and teachers) and hyperactivity (observed by parents), although functional impairment was not significantly affected (Kratochvil et al. 2011). Given the findings from pharmacological studies of preschoolers, it is clear that behavioral treatments are necessary to augment any medication therapy treatment in this age range.
Methods for Assessing Attention in Preschoolers
Comprehensive assessment of attention and related functions in children should include thorough review of the child’s history, planned observations, and formal psychometric testing (Mahone and Slomine 2008). The three primary methods of psychometric assessment that have been used to characterize attentional functioning in preschool children include performance-based tests, rating scales (parent, teacher, clinician), and structured interviews. Performance-based methods for measurement of attention in the preschool years have been developed to address most of the salient components of attention described by Mirsky, Dennis, and Posner, and include sustained attention, selective (focused) attention, span of attention (encoding/maintaining), and top-down controlled attention, including freedom from distractibility and set-shifting. A review of published methods is provided below, and includes measures that are commercially available, and those that have been published only in the research literature.
Performance-Based Tests
Continuous Performance Tests
Kiddie Continuous Performance Test (K-CPT)
The K-CPT (Conners 2001) is a computerized test of attention for children ages 4 and 5 years. The task lasts 7.5 min and uses 11 black and white pictures of common objects (10 targets, 1 non-targets). The child must respond by clicking a mouse or pressing space bar as quickly as possible following all pictures except for the non-target (a soccer ball). Data regarding omissions, commissions, perseverations, hit reaction time, and standard error are collected. Response time data are also used to determine response consistency as the task progresses, as well as in response to the two interstimulus intervals. The normative sample included 454 four- and five-year-old children, of whom 314 were classified as nonclinical, 100 as having ADHD, and 40 as clinical cases without ADHD. The nonclinical sample was relatively even in regard to sex distribution (48 % boys, 52 % girls); however, the majority of the ADHD sample was boys (75 %). Split-half reliability ranged from 0.72 to 0.83 (Conners 2001).
Despite its publication over a decade ago, there have been relatively few validity studies using the K-CPT. In one study combining the K-CPT (ages 3–5) and the CPT-II (Conners and Staff 2000; ages 6–7), omission errors were significantly correlated with the Conners’ Parent Rating Scale-Revised (CPRS-R) Cognitive Problems and Inattention scales; although, commission errors were not found to be associated with the Hyperactivity scale (Rezazadeh et al. 2011). Preschool children without behavioral difficulties are observed to have fewer omissions, lower reaction time standard error, less variability and less deterioration in performance over time than children with hyperactive and oppositional behaviors (Youngwirth et al. 2007). The K-CPT has also been used as an attention measure with healthy preschoolers in research comparing effects of DHA supplements on cognitive functioning (Ryan and Nelson 2008).
Auditory Continuous Performance Test for Preschoolers (ACPT-P) (Mahone et al. 2001)
The ACPT-P is a computerized go/no-go test developed for use in children ages 36 to 78 months. Omissions, commissions, response latency, and variability of response time are the primary performance indices. This is a true go/no-go test, with only two stimuli—one target (dog bark) and one non-target (bell). Auditory stimuli are presented for 690 msec, with a fixed ISI of 5,000 msec. During this five-minute test, 15 target and 15 non-target stimuli are presented. The child presses the space bar immediately following the target stimulus, and ignores the non-target. Initial studies showed no significant differences between typically developing boys and girls on any of the indices. Performance (omissions, response latency, and variability) improved with age from age 3–4 years, leveling off by age 5 years and was correlated with parent ratings on the CPRS-R (Mahone et al. 2001). Preschool children with ADHD demonstrate significantly poorer performance on the ACPT-P with regard to omissions, mean response time, and variability (Mahone et al. 2005). Among preschoolers with ADHD, the ACPT-P omissions, response time, and variability were significantly associated with performance on the NEPSY Statue test (Mahone et al. 2005). Among typically developing preschool children, amount of nighttime sleep was significantly (inversely) associated with number of commission errors on the ACPT-P (Lam et al. 2011).
Continuous Performance Task for Preschoolers (CPTP) (Corkum et al. 1995)
The CPTP is a computerized test designed for children ages 3–5 years. The CPTP uses pictures for stimuli, includes targets and distractors, a sequential presentation of stimuli in a quasi-random fashion, a slowed rate of presentation to allow for longer viewing time, a longer response window, fewer trials to reduce total task duration, and a training phase (Corkum et al. 1995). All six stimuli (1 target, 5 non-targets) are black and white, hand drawn (and scanned) figures with the same basic circular shape. Non-targets include pictures of a girl’s face, the sun, an ice cream cone, a lollipop, and a flower; the target is a pig face. The test presents 240 stimuli (40 targets) in pseudorandom order in which the target and each non-target occur once every six trials. For evaluation purposes, the session is divided into four 60-trial blocks, and the total test is 9 min long. Omissions, commissions and response latency are recorded.
In a sample of 60 typically developing preschoolers, an increase in omissions was observed over the 9-minute course of the CPTP. In all blocks, 3-year-olds showed more omissions than 4- and 5-year-olds; however, only in the last three blocks did 4-year-olds display more omissions than 5-year-olds. A greater number of commissions were displayed by 3-year-olds than by the other two groups, and boys displayed more commissions than girls. The sensitivity to target discrimination improved with age as well. When compared with other measures of preschool attention, commissions and omissions on the CPTP were significantly correlated with performance on a preschool picture cancellation test (Corkum et al. 1995).
Hagelthorn and colleagues (Hagelthorn et al. 2003) adapted the CPTP by shortening the length to 3 min and reducing the number of non-targets to one to facilitate more direct comparison with a preschool auditory CPT (i.e., the ACPT-P described above). In this adaptation, stimulus duration and interstimulus intervals remained identical to those described by Corkum et al. (1995). In this sample, typically developing children displayed a significantly higher rate of omissions and commissions on the visual task than on the auditory task. Mean reaction time and omissions errors decreased with age. Of note, the findings from the Hagelthorn study suggested that 3-year olds likely require interstimulus intervals as long as 5,000 msec in order to respond within the allotted interval (and not to the preceding stimulus).
The CPTP has also been used in preschool children with ADHD. In a sample of 50 children ages 3–6 years, children with ADHD made more errors of omission and commission than age-matched typically developing peers (DeWolfe et al. 1999). Preschoolers with ADHD who had not been treated with stimulant medications had significantly more omissions and commissions on the CPTP than matched controls; however, once treated, group differences were eliminated (Byrne et al. 1998). Noland and colleagues also used the CPTP to investigate attention in 4-year-olds who had experienced prenatal substance exposure (Noland et al. 2005). The authors reported that children with prenatal cocaine exposure “passed” the pretest portion of the CPTP at a significantly lower rate than non-exposed children. Additionally, cocaine-exposed and cigarette-exposed children display significantly more commission errors than non-exposed children, and increased exposure to cigarettes was associated with a higher rate of commission errors. Severity of marijuana exposure showed a positive, but non-significant correlation with omission errors.
Zoo Runner
Zoo Runner was developed by Prather et al. (1995) to assess sustained attention in children ages 3 to 6 years. It has two components: an auditory attention task and a visual task. On the auditory test, animal sounds are presented to the child for 1,000 msec, and with an ISI of 1,000 msec. There are a total of 215 trials, and the task takes 7.2 min. There is 1 target and 11 non-target stimuli. Children are asked to press a button when they hear the word “tiger.” Mean reaction time, omissions, and commission errors were recorded. The auditory version of Zoo Runner has been used in both clinical and nonclinical samples. In a sample of 50 children ages 3–6, children with ADHD had similar rates of omissions and commissions on this task compared with typically developing peers (DeWolfe et al. 1999). Similar to the CPTP, preschoolers with ADHD who had not been pharmacologically treated displayed significantly more omissions on the auditory Zoo Runner task than matched controls; however, once treated, this difference was eliminated (Byrne et al. 1998).
The visual version of Zoo Runner requires the child to respond after seeing a picture of a cat. Stimulus presentation time, interstimulus intervals, total number of trials, number of targets and non-targets, and total task duration are the same as in the auditory version. In both tasks, typically developing children were noted to improve with age on omissions, commissions, and reaction times. Children at age 3 years demonstrated a higher number of omissions on both tasks, suggesting that the tasks may be too difficult for typical children of that age. After age 5.5 years, little further improvement is observed (Prather et al. 1995).
Children’s Continuous Performance Test (C-CPT) (Kerns and Rondeau 1998)
The C-CPT is a computerized CPT that uses a combined visual/auditory format. Stimuli are presented at 1,500 msec intervals—one target for every six non-targets, for a total duration of 5 min. Familiar animal pictures are paired with the common noise associated with those animals. Familiarization to the pictures and sounds are completed prior to test administration, and a practice trial is administered until 100 % accuracy is obtained. Correct hits, omission errors, commission errors, and reaction times are recorded. Three subtests can be administered to each participant, for a total of 200 stimuli, including 29 randomly presented targets. Task 1 presents the visual and auditory pairing, during which the child is asked to respond to the sheep. Task 2 presents only the audio stimuli (with an X on the screen), and the child is again asked to respond to the sheep sound. Task 3 pairs the visual and auditory stimuli incorrectly, and the child is asked to respond to the picture of the sheep, regardless of the accompanying animal sound.
When administered to typically developing children ages 40 through 64 months, a significant age effect was found for correct hits on all three tasks, and for commission errors on Task 1. Correct hits increased as age increased, while commission errors decreased with age. As a group, children displayed fewer overall hits on Task 2 (auditory only) than on Tasks 1 and 3, suggesting that the task may have been more difficult. More commission errors were made on Task 3 (incorrect pairings) than on Tasks 1 or 2. Reaction times across all three tasks were faster for commission errors than for correct hits. No significant effects of sex were identified (Kerns and Rondeau 1998). Among clinically-referred preschoolers with attention problems, only 39 % had successful completion of all three C-CPT trials (compared with 98.9 % control completion), despite all clinical participants being able to complete the practice trial successfully, suggesting that only Task 1 is appropriate for use in clinical groups (Kerns and Rondeau 1998).
The Preschool-Continuous Performance Test (P-CPT) is a modification of the C-CPT, and includes only Task 1. The child is told that he or she is responsible for feeding the sheep, and must do so by touching the sheep when it appears on the computer screen. The child is not supposed to touch any of the other animals. The task is 5 min in duration, includes 200 stimulus presentations, of which 29 are sheep. Omission errors, commission errors, and reaction times are recorded. In a sample of typically developing children ages 3–5 years from private preschools in a socio-economically disadvantaged area of Canada, correct hits (.65), omissions (.63), and reaction time (.77) were all found to display modest test-retest reliability while commission errors had less stability (.44) (Muller et al. 2012). Preschool children with both early and late pre-term birth made significantly more errors of omission and commission than age-matched term birth children (Baron et al. 2011).
Gordon Diagnostic System (GDS) (Gordon et al. 1986)
The GDS is a self-contained computerized CPT that is most often used with children of school age or adults; however, it can also be used with 4-and 5-year-old children. Normative data for the GDS were collected during the mid-1980s., with data based on more than 1,250 children aged 4 to 16 years old (Gordon and Mettelman 1987). Preschool children (4–5 years-old) are asked to complete two tasks—Delay and Vigilance. On the Delay task, the child is instructed to earn maximum points by pushing a button; however, a delay between presses is required in order to earn points. The child must determine how long to wait, as well as be able to wait that amount of time between presses in order to earn points. Typically, a 6-second delay is required; however, this is decreased to 4 s for preschool children. If the child responds sooner than 4 s, a buzzer sounds and the timer is reset; however if they wait the 4 s before responding, a light flashes and a point is earned. The delay task is 6 min in duration. The percentage of correct responses (efficiency ratio) is used to determine the child’s level of impulsivity. The Vigilance task is also modified for children ages 4 and 5 years. Rather than the standard 1/9 combination required for response with older children, the preschool task assesses sustained attention by flashing numbers quickly on the screen and asking the child to respond when a 1 appears. The presentation interval is 2 s, and the entire task lasts 6 min. Performance is evaluated using the total correct and the total number of commissions.
Mariani and Barkley (1997) used a version of this task with 4- and 5-year old boys in which they extended the standard duration time from 6 min to 9 min and used the single digit target of 7. Boys with ADHD performed significantly worse on the total correct responses, but not on commission errors. Similarly, Pulsifer and colleagues used the GDS to assess attention in 5-year-old children living in an urban environment, with and without prenatal drug exposure. The authors reported that the drug exposed group had significantly fewer commission errors, although both groups performed below average in regard to sustained attention (Pulsifer et al. 2008).
Preschool Vigilance Task (PVT) (Harper and Ottinger 1992)
The PVT is a computerized task that presents a picture of a tree with an extended right-side branch. A bird appears on the branch for 0.5 s 25 times at intermittent intervals ranging from 10 to 60 s, for total task duration of 14.5 min. The ISIs are chosen randomly, but each participant receives the same sequence. The child is instructed to press the response button only when the bird appears on the tree. The computer records errors of commission, errors of omission, and reaction time. This task was evaluated on a sample of 20 hyperactive 4–6 year olds, predominantly boys, and 20 controls matched on gender and age. Errors of omission demonstrated high test-retest reliability (0.80); however, commission errors and reaction time did not. Hyperactive children tended to make more errors of omission, but not commission, on the PVT. The PVT was able to correctly classify hyperactive versus typically developing with 82.5 % accuracy (Harper and Ottinger 1992).
Additional Issues with Preschool CPT Tests
Other continuous performance tasks have been developed that assess sustained attention in preschoolers with and without ADHD, as well as with and without other childhood disorders. Some researchers have adapted tasks designed for older children to be more appropriate for preschool groups, for example, by decreasing the total task duration and using more basic stimuli (Finneran et al. 2009). Even with these adaptations, other factors, such as ISI can impact performance (Finneran et al. 2009; Hagelthorn et al. 2003). In a study of preschool children described as low or high risk for ADHD Berwid and colleagues manipulated the ratio of targets to non-targets in a computerized test. Across groups, rates of omission and commission errors decreased with age and the youngest group displayed significantly more errors than the middle and oldest age groups (which did not differ). An interaction effect was observed, such that group differences in commission errors diminished with age. High-risk children also displayed longer and more variable reaction times, though again, mean response time and response time standard deviation decreased with age when comparing the youngest group (ages 3.44 to 4.54) to the older two groups (ages 4.54–5.57, and 5.58–6.95). The greatest response time discrepancies between risk groups were found to be present in the youngest age groups (Berwid et al. 2005). Another common problem is that some CPT tasks for preschoolers use letters or numbers as stimuli (Harper and Ottinger 1992), which presumes the children taking the test have automaticity of recognition of their letters and numbers.
A summary of the CPT tests reviewed is provided in Table 1.
Visual Cancellation Tasks
Picture Deletion Test for Preschoolers (PDTP) (Corkum et al. 1995)
The PDTP presents a quasi-randomized matrix of picture targets and non-targets, and reduces fine motor demands (compared with traditional paper and pencil tasks) via use of a self-inking “bingo” stamper (Corkum et al. 1995). Normative data were collected on 60 Caucasian children ages 3–5 years. Sex distribution in each age group was relatively equal. The PDTP requires the child to search a visual array of targets and non-targets to locate and mark the targets as quickly as possible. The training phase involves teaching the child to identify and mark the appropriate target. The test phase involves four tasks: Geometric Shape Deletion, Cat Deletion, Fish Deletion, and Motor Deletion. The total test phase lasts approximately 10 min. The first three tasks include one Discrimination and two Deletion phases. The Discrimination phase is used to determine that the child is able to identify an example of each distractor and the target. In the Deletion phase, the child is presented with two adjacent 10-inch × 6-inch arrays of 15 target and 45 non-target pictures, with an example of the target at the top, and asked to mark the targets as quickly as possible. Performance is measured in time to completion (speed), errors of omission, and errors of commission (accuracy). The Motor Deletion Task assessed the speed of marker use by presenting a single 10-inch × 6-inch array of circles and asking the child to mark all of the circles as quickly as possible.
Across the three age groups, more commissions were observed on the Fish trial than the Cat trial. Three-year olds made more omissions on the Cat trial than on the Shape trial. No significant differences between age groups were observed in regard for omissions and commissions on the Shape trial; however, 3-year olds made more omissions than 4-year-olds on the Cat trial, and the number of omissions decreased on the Fish trial as children got older. Similarly, commissions decreased with age on the Fish trial as well. Age effects were observed in regard to commissions on the Cat trial in the younger two groups as well, with 4-year-olds performing better than 3-year-olds. Performance on the Cat and Fish trials of the PDTP were significantly associated with commission and omission error rates on the CPTP (Corkum et al. 1995).
A revised version of the PDTP has been published, with removal of the Fish trial, an increase in the number of Cat trial arrays, and change in the printed layout of the task (Byrne et al. 1998). Using the revised task in a clinical sample of 50 children with ADHD, ages 3–6 years, there were no group differences (compared with age-matched controls) on the PDTP for omission errors; however, the ADHD group made significantly more commission errors and displayed a longer latency to task completion (DeWolfe et al. 1999). Additionally, preschoolers with ADHD who had not been treated with stimulant medications displayed significantly more commission errors on the PDTP than matched controls; however, once treated, there were no longer group differences (Byrne et al. 1998). The PDTP has more recently been used to assess attention in 4-year-old children with prenatal substance exposure. The children with prenatal cocaine exposure “passed” the pretest portion of this task at a significantly lower rate than non-exposed children. Additionally, preschool children with prenatal tobacco exposure produced a higher rate of commission errors than non-exposed children (Noland et al. 2005).
NEPSY Visual Attention (Korkman et al. 1998)
The original version of the NEPSY was designed to assess neuropsychological development of children ages 3 to 12 years. NEPSY subtests were divided into five content Cores—one of which one was Attention/Executive Functions. The Visual Attention subtest was included in this Core. Only two of the subtests on the NEPSY Attention/Executive Function Core were designed for use with preschool children—Visual Attention and Statue. Both of these measures have been used in studies of preschoolers with symptoms of ADHD (Mahone et al. 2005; Youngwirth et al. 2007), and in evaluating attention in other clinical groups, such as those with exposure to gestational diabetes mellitus (Nomura et al. 2012). The NEPSY Visual Attention subtest is a visual cancellation task that assesses the child’s ability to use selective focus and attention, along with speed and accuracy. The task requires the child to identify and mark the target stimulus among an array of distractors as quickly as possible. For preschoolers, there are two trials: bunnies (arranged in rows) and cats (arranged in random order). The child is required to search the pages and mark each target (which is represented at the top of the page) with a red crayon. Each trial is 120 s. Published reliability coefficients for children ages 3–5 years ranged from 0.68 to 0.76. In a sample of 184 typically developing children ages 3½ to 6 years, a moderate association was observed between the NEPSY Visual Attention and Statue subtests in children with a verbal span of ≤3 digits, but no relation in children with digit span of ≥5 (Espy 2004). Unfortunately, the Visual Attention subtest was not included in the second edition of the NEPSY due to concerns about insufficient clinical sensitivity (Korkman et al. 1998).
Visual Search Task (Visearch; Wilding et al. 2001)
This is a visual selection task designed for children ages 3–7 years. The task has two conditions, the single-target search condition and the dual-target search condition. In this task, participants were seated in front of a screen showing a display of black and brown color “holes” of different shapes on a green background with a river and some trees. In the single-target search condition, participants were instructed to touch a hole of prior specified shape and color (e.g., black vertical ellipse or a brown horizontal ellipse) in order to uncover the “king of monsters.” Participants are instructed that small monsters (which are blue for black vertical ellipses and yellow for brown horizontal ellipses) will pop from the target holes, but they have to continue looking until the king of monsters was found. The king always appears on the twentieth target touched. Performance is assessed using the number of false alarms to non-target holes and mean response time per hit. A modified version of the original task was used by Wilding et al. in which the “holes” were larger than in the original version, measuring 8 mm or 6 mm in diameter, with the same measurements for the longer and shorter axes of the ellipses. There were 20 targets in the single-target searches and 15 for each target in the dual-target search. Non-targets were large or small circles and ellipses in both colors; there were 50 non-targets in the single search conditions and 40 non-targets in the dual search condition, making 70 objects in all (Wilding et al. 2001).
Additional Performance-Based Tests of Attention
Statue (Korkman et al. 1998; Korkman et al. 2007)
The NEPSY Statue subtest assesses motor persistence and inhibition by asking the child to close his or her eyes, remain in a specified body position, and refrain from speaking or laughing for 75 s while the examiner performs potential distractions (e.g., dropping a pencil). The published reliability coefficient for the original NEPSY among children ages 3 to 4 years was only 0.50; nevertheless, the Statue test has been found to be highly sensitive in clinical groups. Preschoolers (ages 3–5 years) with ADHD were observed to have lower Statue scores than age- and sex-matched controls (Mahone et al. 2005), while preschoolers with behavior problems had lower Statue performance than those without behavior problems (Youngwirth et al. 2007). In the revised NEPSY (NEPSY-II; Korkman et al. 2007), normative data have been updated and the Statue subtest is administered in exactly the same manner as in the first edition. In the NEPSY-II, the reliability coefficient for children ages 3–4 years on the Statue subtest is considerably improved (0.82) (Korkman et al. 2007).
Recognition of Pictures (Differential Ability Scales-Second Edition—DAS-II; Elliot 2007)
The DAS-II was standardized on a sample of 3,480 children, ages 2:6 through 17:11, stratified by six-month age groups for ages 2, 3, and 4, and one-year age groups for ages 5 through 17. A total of 880 children between the ages of 2:6 and 4:11 were included. On the Recognition of Pictures subtest, the child is presented with pictures of common objects for 5 s. This is followed by presentation of a different page, on which the target object(s) is presented with similar distractor items. The task requires the child only to point to the target object(s) to identify the target. The number of target items gradually increases, as does the similarity of the targets to the distractor items. Reliability coefficients for the Recognition of Pictures task for children ages 2:6–5:11 range from 0.77 to 0.85 (Elliot 2007). The task assesses short-term recognition memory, which is highly dependent on focused (selective) attention and visual attention span. School-age children with ADHD have been shown to have poorer performance on the Recognition of Pictures test, compared to controls (Weisen 2008); however, there is little literature supporting its validity among preschoolers.
Digit Span Measures
There are two similar digit span measures that have been published and normed for preschool aged children. Both assess auditory verbal attention span (i.e., the “encode” component of attention described by Mirsky and colleagues). The first is Number Recall (Kaufman Assessment Battery for Children—KABC-II; Kaufman and Kaufman 2004). The KABC-II was standardized on a sample of 3,025 children, stratified by six-month age groups in ages 3 and 4, and one-year age groups for ages 5 through 18. The Number Recall task requires the child to repeat series of single syllable numbers of increasing length. The numbers in the series are presented orally at a rate of one per second. The series of numbers on the original KABC ranged from two to eight, but was expanded to include nine-digit sequences on the KABC-II. Reliability coefficients for the Number Recall task of the KABC-II for children ages four and five are 0.87 and 0.79, respectively (Kaufman and Kaufman 2004). There is significant improvement in performance among typically developing controls between ages 3–4 years; with slower rate of improvement between 4 and 5 years (Lam et al. 2011). Mariani and Barkley (1997) reported that preschool boys with ADHD (ages 4–5 years) had significantly lower scores on the Number Recall subtest compared to controls. Among typically developing preschool children in fulltime daycare, the amount of daytime napping was significantly associated with performance on Number Recall (Lam et al. 2011).
The second digit span test for preschoolers is the Recall of Digits Forward (Differential Ability Scales - Second Edition- DAS-II; Elliot 2007). The DAS-II was standardized on a sample of 3,480 children, ages 2:6 through 17:11, stratified by six-month age groups for ages 2, 3, and 4, and one-year age groups for ages 5 through 17. A total of 880 children between the ages of 2:6 and 4:11 were included. Similar to the KABC-II Number Recall task, the Recall of Digits Forward task requires the child to repeat a series of digits of increasing length. The numbers in the series are presented orally at a rate of two per second in order to prevent rehearsal. The series length begins with 2 digits and gradually increases to 10 digits. There are five trials of each series length. Reliability coefficients for the Recall of Digits Forward task for children ages 2:6–5:11 range from 0.88 to 0.91. (Elliot 2007). Differences have been observed on this task, such that children who were born premature at an extremely low birth weight perform more poorly on this task at age 3 than children who were born at term (Baron et al. 2011).
Other Verbal Span Tasks
Adaptations to verbal span tasks that have been used in school-age children (Brocki and Bohlin 2004; Brocki et al. 2008; Thorell 2007) have been used for preschool children. In these adaptations, the child is typically presented with two words or digits and asked to repeat verbatim for two trials. The span is then increased by a single digit/word every other trial until the child responds incorrectly to at least one of two trials at that span length (Wahlstedt et al. 2008), or failure on both items (Muller et al. 2012). Among preschool children, these tasks typically show moderate test-retest reliability, e.g., forward digit span (0.70) and forward word span (0.57) (Muller et al. 2012). Muller and colleagues also identified significant practice effects (over a 21-day interval) for forward digit span but not the forward word span task. Wahlstedt and colleagues (Wahlstedt et al. 2008) used forward and backward verbal span tasks consisting of familiar nouns (e.g., cat, rabbit, clown) in which the child was initially presented with two words, which sequence length increased by a single word every other trial until the child responded incorrectly to at least one of the two trials at that span length. Children with high rates of ADHD symptoms showed significantly lower performance on this verbal span test only if they also had poor performance on other executive function tests (Muller et al. 2012).
Hand Movements (KABC-II) (Kaufman and Kaufman 2004)
The Hand Movements subtest of the KABC and KABC-II requires that the child replicate an exact series of palm, fist, and side hand taps on the table. The task has not changed between the first and second version of the KABC. This task is short in duration (approximately 5 min or less), and normative data are available for children ages 4 and 5 years. Split-half reliability coefficients for the Hand Movements subtest of the KABC-II for children ages 4 and 5 years was 0.57 and 0.75, respectively, while test-retest reliability in this age group is 0.58. Barkley and colleagues also found significant group differences between preschool boys with and without ADHD on the Hand Movement subtest (Mariani and Barkley 1997).
Xylophone Task (Muller et al. 2012)
Another example of a visual span task is the Xylophone Task, in which an onscreen xylophone displays a sequence of lit bars, and the child is asked to replicate the series on the touch screen monitor. The trials start with sequences of two notes and progress to series of five notes, with the task discontinuing after errors on both trials at a given length. In the backward condition, the child is asked to repeat the sequence in reverse. Forward xylophone was shown to have poor test-retest reliability (0.26); however, test-retest reliability of the backward condition was slightly better, although still low (0.34).
Spatial Span
An adaptation of the Spatial Span task has also been developed for preschoolers (Wahlstedt et al. 2008). In this version, a 4 × 4 matrix appears on a computer screen and is described as “windows” on a house. Pigs appear in the windows for 1,000 msec with a 75 msec ISI. The child is asked to remember the sequence of windows in which the pigs appeared. Two trials are administered at each span length until the child responds incorrectly to at least one of the trials at that length. Preschool children with high levels of ADHD symptoms were shown to have poorer performance on this version of the Spatial Span task, compared to age-matched controls (Wahlstedt et al. 2008).
“Simple” Reaction Time Tasks
Simple reaction time tasks require that the examinee respond as quickly as possible when a stimulus appears. In this most basic format, only one stimulus is included, and the child must always respond. In a sample of typically developing, Russian children (ages 4–6 years), response accuracy for all age groups was found to be high, with no significant effect of sex. Young children required greater response latency (compared to adults), and response times decrease steadily with age through childhood (Kiselev et al. 2009). This type of task may be useful as a control task in behavioral experiments with preschool children (contrasted with go/no-go or choice reaction time tasks), since median “basic” response time does not appear to differ between typically developing preschoolers (ages 3–4), preschoolers with ADHD, and preschoolers with ADHD and ODD (Gopin et al. 2012). A summary of visual cancellation and additional performance-based tests of attention is provided in Table 2.
Rating Scales
Child Behavior Checklist for Ages 1.5 to 5 (CBCL 1.5–5) (Achenbach and Rescorla 2000)
The CBCL for ages 1.5 to 5 assesses a wide range of internalizing and externalizing problems in young children, including a scale pertaining specifically to attention problems. There are 100 behavioral items that are rated on a scale from 0 (not true) to 2 (very/often true). There is also a version available for completion by a child’s teacher or caregiver (Caregiver-Teacher Report Form; C-TRF) that includes items that pertain to group situations and removes items most specifically related to the home or family environment. Scales included on both the CBCL and the C-TRF include Emotionally Reactive, Somatic Complaints, Aggressive Behavior, Anxious/Depressed, Withdrawn, and Attention Problems, while a Sleep Problems scale is included only on the CBCL. Internalizing, Externalizing, and Total Problems scales are also included. Test retest reliability is high for the majority of scales on both the CBCL and the C-TRF. Mean reliability was 0.85 and 0.81 respectively. Reliability for the Attention Problems scale is 0.78 for the CBCL and 0.84 for the C-TRF (Achenbach and Rescorla 2000).
The CBCL has been used in preschoolers for general behavioral screening (Corkum et al. 1995; DeWolfe et al. 1999; Egger et al. 2006; Posner et al. 2007) and to determine correlations with other measures (Kadesjo et al. 2003). When used to specifically evaluate the behavior of children with and without ADHD, parent ratings on the Attention Problems scale were significantly higher than parent ratings of matched controls for an untreated ADHD group; however, once the ADHD group was treated, parent reports on the CBCL Attention Problems scale for the ADHD group were not different than parent ratings of controls (Byrne et al. 1998).
Behavior Assessment Scale for Children-2 (BASC-2) (Reynolds and Kamphaus 2004)
The BASC-2 is a broad band caregiver rating scale for children that was designed to assess a wide range of child behavior problems and psychopathology, including attention problems, hyperactivity, and aggression. The BASC-2 is often used as a general screener of behavioral, emotional, and some adaptive function, as well as to specifically identify hyperactivity and inattention (Gopin et al. 2010; Gopin et al. 2012; Youngwirth et al. 2007) The Preschool version of the BASC-2 consists of a parent and teacher report. Behaviors such as hyperactivity, aggression, anxiety, depression, somatization, withdrawal, attention problems, ability to adapt, social and communication skills, and daily living skills are included on these scales.
Conners-Early Childhood Scales (Conners and Staff 2000)
In the current revision of the Conners Rating Scales, a new measure, the Conners Early Childhood (Conners EC; Conners 2009) was developed for use in children ages 2 to 6 years. As with the previous Conners’ scales, parent and teacher forms are available. The Conners EC behavioral scales include Inattention/Hyperactivity, Defiant/Aggressive Behaviors, Anxiety, Mood and Affect, and Physical Symptoms. Developmental Milestone scales include Adaptive Skills, Communication, Motor Skills, Play, and Pre-Academic/Cognitive. The Conners EC can be completed at its full length (behavioral and developmental scales), or these areas can be assessed separately. Validity scales are only included on the full length and Behavior forms. The Conners-EC as standardized on a group of 1,600 cases randomly selected (with consideration of racial/ethnic distribution) from a total of 3,281 assessments collected. Reliability for the Conners-EC Parent Behavior Scales was as follows: internal consistency 0.86, test- retest 0.87, and inter-rater 0.72. For the Conners EC-Teacher Behavior Scales, reliability was as follows: internal consistency 0.89 and test- retest 0.93. The Conners-EC Behavior subscales are highly correlated with similar subscales on the BASC-2 and the CBCL 1.5–5 (Conners and Staff 2000).
ADHD Rating Scale-IV—Preschool Version (DuPaul et al. 1998; McGoey et al. 2007)
The ADHD-RS-IV includes the 18 behavioral descriptors of ADHD as determined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; APA 1994). Raters can consist of parents and teachers who respond to each question on a 4-point scale. Use of this questionnaire tends to consider ratings as 2 (pretty much) or 3 (very much) to reflect symptom presence (DuPaul et al. 1998; Kadesjo et al. 2001; Marks et al. 2005).
McGoey and colleagues (McGoey et al. 2007) adapted the instrument and established clinical utility in preschool children. Parent ratings were collected on 902 children ages 3: to 5:11 (53 % boys, 47 % girls) and teacher data were collected on 977 children (51 % boys, 49 % girls). Test-retest reliability and concurrent validity were determined by having a subsample of 42 parents and 41 teachers complete the ADHD-RS-IV Preschool Version and the Conners’ Teacher or Parent Rating Scale-Revised 4 weeks after initial completion. Symptom statements were modified to be more appropriate to the developmental level of preschoolers. Statements are rated on a Likert scale of 0 (not at all) to 3 (very often) to reflect the child’s behavior. Scores can be obtained for Inattention, Hyperactive/Impulsive, and Total Scales. Internal consistency for the three scales ranged from 0.92 to 0.95 on the School Version and from 0.85 to 0.92 on the Home Version. Test-retest reliability correlations for the three scales ranged from 0.93 to 0.96 for the School Version and between 0.80 and 0.87 for the Home Version. Correlations between the ADHD-RS-IV Preschool Version- teacher report and the CTRS-R Oppositional, Cognitive Problems/Inattention, Hyperactivity, and ADHD Index scales were all significant. Correlations between the same scales on the CPRS-R and the parent report were also significant.
The ADHD-RS-IV rating scale has been used as a screener for entry for preschool ADHD studies (Gopin et al. 2012; Nomura et al. 2012), to classify preschoolers as “high risk” or “low risk” of ADHD based on parent and teacher ratings (Berwid et al. 2005), and to assess parent perception of ADHD-related symptoms in the context of other problem behaviors (Kadesjo et al. 2003). Other researchers have adapted an 18-item list of symptoms to be more appropriate for the preschool population (e.g., loss of interest during story time or rolling on the floor during circle time) so that care providers can rate the behaviors on a Likert scale (e.g., PATS Diagnostic Interview). Internal consistency of this rating scale is reported at 0.84 (Posner et al. 2007).
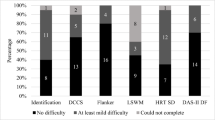
Behavior Rating Inventory for Children (BRIC) (Gopin et al. 2010)
The BRIC was designed to be a brief clinician rating scale that assesses core ADHD symptoms and associated behaviors in preschool children (ages 3–4 years). The BRIC is a 5-item scale that takes only 1–2 min to complete. Items are rated on a 5-point Likert Scale that provides behavioral examples at points 1, 3, and 5 in order to assist with clinician reliability. There are two scales: the ADHD Symptom Triad and the Mood/Sociability Factor. The ADHD Symptom Triad is comprised of three items, each one assessing one of the three core ADHD symptoms-inattention, hyperactivity, and impulsivity. The two items on the Mood/Sociability Factor assess social and mood impairment associated with ADHD. Lower scores reflect more positive behaviors. When used with preschool children, the ADHD Symptom Triad demonstrated adequate test-retest reliability when rated by the same examiner on both occasions (0.78), although reliability declined when rated by different clinicians (0.59). The Mood/Sociability Factor demonstrated only moderate results when rated by the same clinician (0.55) and when rated by different clinicians (0.50). Scores on the ADHD Symptom Triad reflected significant differences between hyperactive/inattentive children and a control group; however, differences on the Mood/Sociability Factor were not observed. There is a moderate association between the ADHD Symptom Triad and the BASC-2 PRS-P and the BASC-2 TRS-P inattention and hyperactivity scales. BRIC clinician ratings were correlated as well with parent and teacher reports (i.e., ADHD-RS-IV) as the parent and teacher reports were with one another. Significant correlations were also observed between the ADHD Symptom Triad and actigraph scores. Overall, the BRIC demonstrated high specificity, but limited sensitivity (Gopin et al. 2010).
Early Child Inventory-4 (ECI-4) (Sprafkin and Gadow 1996)
The ECI-4 is a DSM-IV-based rating scale designed for use with children ages 3–6 years to assess behaviors and emotions. Completion time is approximately 10–15 min. The parent version contains 108 items, 77 of which are also included on the teacher version. Behaviors unlikely to occur in the school setting are not included on the teacher version. On both versions, items are rated on a 4-point scale, “never” through “very often.” Scoring is completed in two ways, count (categorical) and severity (dimensional). Symptom count is a categorical score that is obtained from the number of symptoms of particular disorder that are rated as “often” or “very often.” This is compared to the symptom criterion score, which is the minimum symptom count necessary to meet DSM-IV diagnostic criteria. If the symptom count is equal or greater, the screening cutoff score is received for that disorder. Symptom severity is a dimensional score obtained by adding the values (0–4) of each response related to a particular disorder. ADHD Inattentive subtype, ADHD Hyperactive-Impulsive subtype, and ADHD Combined subtype are included on this measure. Other diagnoses include ODD, Conduct Disorder, PDD, Dysthymic Disorder, Major Depressive Disorder, Generalized Anxiety Disorder, and Social Phobia, as well as questions regarding tics, sleeping problems, feeding problems, posttraumatic stress disorder, selective mutism, and other problematic behaviors. The parent form also includes items symptomatic of Separation Anxiety Disorder.
The ECI-4 also includes a Developmental Deficits Index that includes 12 items about language motor, self-help, play behavior, and responsiveness to adults. Items are summed to a total. The parent version contains 12 items rated on a 4-point scale, while the teacher version contains 8 items on a 5 point scale. Internal consistency was high in regard to ADHD (ADHD-I = 0.91, ADHD-HI = 0.90). Sensitivity for ADHD was similar between parent (0.66) and teacher (0.68) forms, but increased when these forms were considered together (0.90). Specificity also improved when the measures were combined (0.41). The ECI-4 demonstrates internal consistency, criterion validity, and convergent/divergent validity with the CBCL and TRF (Sprafkin et al. 2002). The ECI-4 has also been used to establish the discriminant validity of other measures, such as the K-SADS (Birmaher et al. 2009).
The ECI-4 has been used to identify prevalence rates of psychiatric disorders in a community sample of preschoolers (Gadow et al. 2001). ADHD was one of the most prevalent disorders, and all three subtypes of ADHD were rated as experiencing higher levels of developmental deficits, according to parents. Teacher ratings suggest that only Combined-Type ADHD experiences a significantly lower level of developmental progress. In another study of prevalence rates using the ECI-4, Nolan et al. (Nolan et al. 2001) reported that although Combined type ADHD saw a significant difference in prevalence between genders (boys > girls), this was not the case for ADHD-I or ADHD-HI within the preschool population, although boys tend to display more severe symptoms in all categories. Preschoolers with Combined type also displayed more severe social problems than children with just Inattentive or Hyperactive-Impulsive alone. In general, preschoolers with ADHD tended to display higher severity symptoms than older children (Nolan et al. 2001).
A strength of the ECI-4 is that it has been used internationally. In a prevalence study of children in Spain that compared parent and teacher ratings, ADHD Inattentive subtype was determined to be the highest prevalence disorder as rated by teachers; however, the ADHD Hyperactive/Impulsive (HI) subtype was the most prevalent according to parents. Significant differences between urban and rural teacher reports did not occur for ADHD; however, parent ratings reflected significantly more ADHD-HI in urban settings than in rural (Jané et al. 2006). In a small pilot study of 10 Mexican children with a mean age of 51 months, parent and teacher Symptom Severity scores were significantly correlated; however, in a small subsection of that group who had been diagnosed as having ADHD, no correlation was found between the ECI-4 and the Conners’ Rating Scale-Revised. When compared with diagnosis based on psychiatric interview, the ECI-4 failed to demonstrate strong sensitivity and specificity (Poblano and Romero 2006).
A summary of the reviewed preschool rating scales is listed in Table 3.
Structured Interviews
Kiddie-Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (K-SADS-PL) (Kaufman et al. 1997)
The KSADS-PL is a semi-structured clinical interview developed for children ages 6 to 18 years that can be used to determine the presence of psychiatric disorders in children. Administration to parents of typically developing children takes approximately 45 min; however, increased psychopathology can result in a more extended interview, averaging approximately 75 min. ADHD was not a part of previous versions of the K-SADS, but was added when the K-SADS-PL was developed. Inter-rater reliability was above 98 %, test-retest reliability for ADHD was 0.59 to 0.63, and concurrent validity was established with the Conners’ Parent Rating Scale in children screened positive for ADHD.
The K-SADS was not initially designed for use with very young children; however, Birmaher and colleagues suggested that the measure can be useful in the preschool population (ages 2 to 5; Birmaher et al. 2009). In establishing psychometric properties, comparisons were made between the K-SADS-PL and the Child Behavior Checklist (CBCL), Early Childhood Inventory-4 (ECI-4) and Preschool Age Psychiatric Assessment (PAPA). Convergent validity and discriminant validity were established to be strong for diagnosis of ADHD. Inter-rater reliability reached significance for all diagnoses (ranging from 0.80 to 0.90). Few diagnostic differences were observed when compared to the results of a subsequently administered PAPA interview. Thus, while not specifically designed for preschoolers, the K-SADS has been used to assist in establishing appropriate study inclusion and participant groupings, in conjunction with other measures (Gopin et al. 2012; Nomura et al. 2012).
Preschool Age Psychiatric Assessment (PAPA) (Egger and Angold 2004)
The PAPA is a semi-structured interview that is completed by trained interviewers with the parents of children ages 2 to 5 years. The questions focus on the 3 months immediately preceding interview. There are 25 modules that generate symptom, scaled scores, and diagnoses. Clinicians can choose to administer only some of the modules. The PAPA includes developmentally appropriate questions about behaviors that are not a part of diagnostic criteria, such as temper tantrums and toilet training. The measure has been determined to be reliable and valid for preschool age children (Egger et al. 2006). The reported test-retest reliability for the ADHD module is 0.74. The PAPA has been used to determine diagnosis and/or group placement of participants. When the PAPA is used as the diagnostic instrument, significant stability of ADHD diagnosis has been observed between the preschool and school age years (Tandon et al. 2011).
Diagnostic Interview Schedule, Young Children (DISC-YC) (Fisher and Lucas 2006)
The current NIMH Diagnostic Interview Schedule for Children-IV (NIMH-DISC-IV) is designed to be a highly structured diagnostic instrument that can be used by non-clinicians to assess children ages 6 to 17 years (Shaffer et al. 2000). There are two versions, the parent (DISC-P) and the youth (DISC-Y, ages 9–17), both of which ask the same questions but differ in the pronouns and structure of the question dependent on respondent. The NIMH DISC-IV–P has been determined to be a reliable and valid measure of psychiatric disorders (McGrath et al. 2004; Shaffer et al. 2000). The DISC-YC (Fisher and Lucas 2006) is an adaptation of the DISC-P. It is a structured parent interview that asks a series of questions about the child’s behavior in yes/no format. Additional questions are posed (or not) within each module depending on initial parent responses. Follow-up questions about age of onset, level of impairment, parental concern, and treatment are asked in cases when parents have responded to the presence of clinically significant levels of symptomatic behaviors. Because the DISC-YC is a computerized, fully structured interview, it can be conducted by trained individuals who have limited clinical experience, as it does not require the same level of clinical judgment of some other parent interviews (e.g., K-SADS, PAPA).
Lavigne and colleagues (Lavigne et al. 2009) compared the prevalence rates of ADHD in 4-year-olds, as determined by the DISC-YC and the Child Symptom Inventory (CSI), and found the DISC-YC resulted in a similar prevalence of ADHD-Combined Subtype, but not of Inattentive or Hyperactive-Impulsive subtypes. Overall presence of any type of ADHD was similar between the two measures. When considering only severe impairment levels (i.e., those that met minimum diagnostic criteria, with at least one symptom meeting severe impairment criteria), the rates of ADHD obtained using the DISC-YC were similar to that of the K-SADS, but higher than those obtained when using the PAPA.
A summary of the reviewed structured psychiatric interviews is listed in Table 4.
Summary and Conclusions
Despite the increased interest in assessment of preschool age children, the development of formal measures of attention that are appropriate and valid for use in this age range has been slow. The majority of published assessment methods remain experimental and not commercially available, making access to appropriate tests more difficult for the practicing clinician. Review of the published literature highlights three primary methods for assessing attention in preschool age children: performance-based tests, structured parent interviews, and rating scales. Performance-based tests include a variety of continuous performance tests, aimed at assessing sustained attention, inhibitory control, and consistency of response. Among the CPTs, only the Conners Kiddie CPT (K-CPT) is commercially available in this age range; however, there are remarkably few published validity studies using the K-CPT. Among published CPT tests for preschoolers, those employing a fixed ISI of greater than 2,000 msec, and those whose overall length is 5–7 min or less, have shown greatest utility in preschool age children. Conversely, preschool children have much more difficulty completing tests with ISI of 1,500 msec or less, those whose length is 9 min or more, and those in which the pairing of auditory and visual stimuli are not congruent. Additional performance based tests are available to assess other components of attention, including visual selective attention (e.g., cancellation tests), motor persistence (i.e., NEPSY-II Statue), and encoding, working memory, and auditory/visual attention span (e.g., digit and spatial span tests). Compared to the preschool CPTs, these measures have more published validity studies, and also have the advantage of ease of administration, time efficiency, and (in many tests) nationally-representative standardization samples.
Rating scales for preschool children remain a viable and highly practical assessment method. There are a variety of commercially published instruments (e.g., Conners Early Childhood; BASC-2; CBCL) and methods that can be used by parents, teachers, and clinicians. The published rating scales more consistently have nationally-representative standardization samples, and most have scales specific to attention problems in preschool age children. The benefit of the rating scales is that the severity of inattention symptoms can be directly compared to “typical” attention problems observed in this age range, thus helping the clinician distinguish disordered attention in this age range, and to differentiate it from other cognitive and behavioral problems. The rating scale methods also provide data that complement the information obtained via performance-based methods.
Among the three structured psychiatric interviews reviewed, none are commercially available, making them largely impractical for clinical use outside of research settings. Further, all three (K-SADS, PAPA, DISC-YC) require considerable clinician training, which in some cases (e.g., PAPA) is available only through the author. Nevertheless, the PAPA and the DISC-YC, which were developed specifically for preschool children, show considerable promise in characterizing problematic behaviors in preschool age children, and linking them specifically to DSM-IV diagnostic categories.
In conclusion, while there are now more methods available for assessing attention in preschool age children, the research characterizing the validity and utility of these measures remains limited. Future studies are encouraged to broaden the range of skills assessed, and to clarify which methods work best with which children.
References
Abikoff, H. B., Vitiello, B., Riddle, M. A., Cunningham, C., Greenhill, L. L., Swanson, J. M., et al. (2007). Methylphenidate effects on functional outcomes in the Preschoolers with Attention-Deficit/Hyperactivity Disorder Treatment Study (PATS). Journal of Child and Adolescent Psychopharmacology, 17, 581–592.
Achenbach, T. M., & Rescorla, L. A. (2000). Manual for the ASEBA preschool forms and profiles. Burlington: University of Vermont, Research Center for Children, Youth, & Families.
Akinbami, L. J., Liu, X., Pastor, P. N., & Reuben, C. A. (2011). Attention deficit hyperactivity disorder among children aged 5–17 years in the United States, 1998–2009. NCHS data brief, 70. Hyattsville: National Center for Health Statistics.
American Academy of Pediatrics. (2000). Clinical practice guideline: diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. Pediatrics, 105, 1158–1170.
American Academy of Pediatrics (2011). Policy statement: media use by children younger than 2 years. Pediatrics, 128, doi:10.1542/peds.2011-1753.
American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders, Fourth Edition. Washington, DC: Author.
American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders, Fourth Edition. Text Revision. Washington, DC: Author.
American Psychiatric Association (2012, May 1). Attention deficit/hyperactivity disorder. DSM-5 Development Website (www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=383). Washington, DC: Author.
Armstrong, M. B., & Nettleton, S. K. (2004). Attention deficit hyperactivity disorder and preschool children. Seminars in Speech and Language, 25, 225–232.
Arons, B. S., Katz-Leavy, J., Wittig, A. C., & Wayne Holden, E. (2002). Too young for ADHD: the potential role of systems of care. Journal of Developmental and Behavioral Pediatrics, 23(1 Suppl), S57–S63.
Barkley, R. A. (2011a). Executive functioning and self-regulation: integration, extended phenotype, and clinical implications. New York: Guilford Press.
Barkley, R. A. (2011b). The Barkley deficits in executive functioning scale: rating scales, norms, and interpretive guide. New York: Guilford Press.
Baron, I. S., Kerns, K. A., Muller, U., Ahronovich, M. D., & Litman, F. (2011). Executive functions in extremely low birth weight and late preterm preschoolers: effects on working memory and response inhibition. Neuropsychology. doi:10.1080/09297049.2011.631906.
Bayley, N. (2006). Bayley scales of infant and toddler development-third edition. San Antonio: Harcourt Assessment.
Berwid, O., Curko Kera, E. A., Marks, D. J., Santra, A., Bender, H. A., & Halperin, J. M. (2005). Sustained attention and response inhibition in young children at risk for attention deficit/hyperactivity disorder. Journal of Child Psychology and Psychiatry, 46, 1219–1229.
Biederman, J., & Faraone, S. V. (2002). Current concepts on the neurobiology of attention-deficit/hyperactivity disorder. Journal of Attention Disorders, 6(Suppl. 1), S7–S16.
Biederman, J., Petty, C. R., Monuteaux, M. C., Mick, E., Parcell, T., Westerberg, D., & Faraone, S. V. (2008). The longitudinal course of comorbid oppositional defiant disorder in girls with attention-deficit/hyperactivity disorder: findings from a controlled 5-year prospective longitudinal follow-up study. Journal of Developmental & Behavioral Pediatrics, 6, 501–507.
Birmaher, B., Ehman, M., Axelson, D. A., Goldstein, B. I., Monk, K., Kalas, C., et al. (2009). Schedule for affective disorders and schizophrenia for school-age children (K-SADS-PL) for the assessment for preschool children - a preliminary psychometric study. Journal of Psychiatric Research, 43, 680–686.
Black, I. B., DiCicco-Bloom, E., & Dreyfus, C. F. (1990). Nerve growth factor and the issue of mitosis in the nervous system. Current Topics in Developmental Biology, 24, 161–192.
Blair, C., & Raver, C. C. (2012). Child development in the context of adversity: experiential canalization of brain and behavior. American Psychologist, 67, 309–318.
Bor, W., Sanders, M. R., & Markie-Dadds, C. (2002). The effects of the Triple P Positive Parenting Program on preschool children with co-occurring disruptive behavior and attentional/hyperactive difficulties. Journal of Abnormal Child Psychology, 30, 571–587.
Broadbent, D. E. (1958). Perception and communication. New York: Pergammon.
Brocki, K. C., & Bohlin, G. (2004). Executive functions in children aged 6 to 13: a dimensional and developmental study. Deveopmental Neuropsychology, 26, 571–593.
Brocki, K. C., Randall, K. D., Bohlin, G., & Kerns, K. A. (2008). Working memory in school-aged children with attention-deficit/hyperactivity disorder combined type: are deficits modality specific and are they independent of impaired inhibitory control? Journal of Clinical and Experimental Neuropsychology, 30, 749–759.
Bussing, R., Mason, D. M., Bell, L., Porter, P., & Garvan, C. (2010). Adolescent outcomes of childhood attention-deficit/hyperactivity disorder in a diverse community sample. Journal of the American Academy of Child and Adolescent Psychiatry, 49, 595–605.
Byrne, J. M., Bawden, H. N., Beattie, T. L., & DeWolfe, N. A. (2000). Preschoolers classified as having attention-deficit hyperactivity disorder (ADHD): DSM-IV symptom endorsement pattern. Journal of Child Neurology, 15, 533–538.
Byrne, J. M., DeWolfe, N. A., & Bawden, H. N. (1998). Assessment of attention-deficit hyperactivity disorder in preschoolers. Child Neuropsychology, 4, 49–66.
Christakis, D. A., Zimmerman, F. J., DiGiuseppe, D. L., & McCarty, C. A. (2004). Early television exposure and subsequent attentional problems in children. Pediatrics, 113, 708–713.
Christophersen, E. R., & Mortweet, S. L. (2003). Treatments that work with children: empirically supported strategies for managing childhood problems. Washington D.C.: American Psychological Association.
Chronis-Tuscano, A., Molina, B. S., Pelham, W. E., Applegate, B., Dahlke, A., Overmyer, M., & Lahey, B. B. (2010). Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry, 67, 1044–1051.
Columbo, J. (2001). The development of visual attention in infancy. Annual Review of Psychology, 52, 337–367.
Columbo, J., & Cheatham, C. L. (2006). The emergence and basis of endogenous attention in infancy and early childhood. Advances in Child Development and Behavior, 34, 283–322.
Conners, C. K. (2001). Conners’ Kiddie Continuous Performance Test (K-CPT). North Tonawanda: Multi-Health Systems, Inc.
Conners, C. K. (2009). Conners early childhood. North Tonawanda: Multi-Health Systems, Inc.
Conners, C. K., & Staff, M. H. S. (2000). Conners’ Continuous Performance Test-II (CPT-II). North Tonawanda: Multi-Health Systems, Inc.
Connor, D. F. (2002). Preschool attention deficit hyperactivity disorder: a review of prevalence, diagnosis, neurobiology, and stimulant treatment. Journal of Developmental and Behavioral Pediatrics, 23, S1–S9.
Conway, A., & Stifter, C. A. (2012). Longitudinal antecedents of executive function in preschoolers. Child Development, 83, 1022–1036.
Cooley, E. L., & Morris, R. D. (1990). Attention in children: a neuropsychologically based model for assessment. Developmental Neuropsychology, 6, 239–274.
Corkum, V., Byrne, J. M., & Ellsworth, C. (1995). Clinical assessment of sustained attention in preschoolers. Child Neuropsychology, 1, 3–18.
DeBar, L. L., Lynch, F., Powell, J., & Gale, J. (2003). Use of psychotropic agents in preschool children: associated symptoms, diagnoses, and health care services in a health maintenance organization. Archives of Pediatrics & Adolescent Medicine, 157, 150–157.
De Bellis, M. D., Keshavan, M. S., Beers, S. R., Hall, J., Frustaci, K., Masalehdan, A., et al. (2001). Sex differences in brain maturation during childhood and adolescence. Cerebral Cortex, 11, 552–557.
Dennis, M., Sinopoli, K. J., Fletcher, J. M., & Schachar, R. (2008). Puppets, robots, critics, and actors within a taxonomy of attention in developmental disorders. Journal of the International Neuropsychological Society, 14, 673–690.
DeWolfe, N. A., Byrne, J. M., & Bawden, H. N. (1999). Early clinical assessment of attention. The Clinical Neuropsychologist, 13, 458–473.
Diamond, A. (2002). Normal development of prefrontal cortex from birth to young adulthood: Cognitive functions, anatomy, and biochemistry. In D. T. Stuss & R. T. Knight (Eds.), Principles of frontal lobe function (pp. 466–503). New York: Oxford University Press.
DuPaul, G. J., Power, T. J., Anastopoulos, A. D., & Reid, R. (1998). ADHD rating scale-IV. New York: Guilford Press.
Egger, H., & Angold, A. (2004). The preschool age psychiatric assessment (PAPA): A structured parent interview for diagnosing psychiatric disorders in preschool children. In R. DelCarmen-Wiggins & A. Carter (Eds.), Handbook of infant, toddler, and preschool mental health assessment. New York: Oxford University Press.
Egger, H. L., Erkanli, A., Keeler, G., Potts, E., Walter, B. K., & Angold, A. (2006). Test-retest reliability of the preschool age psychiatric assessment (PAPS). Journal of the American Academy of Child and Adolescent Psychiatry, 45, 538–549.
Egger, H. L., Kondo, D., & Angold, A. (2006). The epidemiology and diagnostic issues in preschool attention-deficit/hyperactivity disorder: a review. Infants and Young Children, 19, 109–122.
Elliot, C. D. (2007). Differential ability scales (2nd ed.). San Antonio: Harcourt Assessment, Inc.
Eme, R. F. (1992). Selective female affliction in the developmental disorders of childhood: a review. Journal of Clinical Child Psychology, 21, 354–364.
Espy, K. A. (2004). Using developmental, cognitive, and neuroscience approaches to understand executive control in young children. Developmental Neuropsychology, 26, 379–384.
Finneran, D., Francis, A., & Leonard, L. (2009). Sustained attention in children with specific language impairment (SLI). Journal of Speech, Lanuage, and Hearing Research, 52, 915–929.
Fisher, P., & Lucas, C. (2006). Diagnostic interview schedule for children (DISC-IV)-young child. New York: Columbia University.
Fox, N. A., Schmidt, L. A., Henderson, H. A., & Marshall, P. (2007). Developmental psychophysiology: Conceptual and methodological issues. In J. T. Cacioppo, L. G. Tassinary, & G. G. Berntson (Eds.), Handbook of psychophysiology (3rd ed., pp. 453–481). Cambridge: Cambridge University Press.
Froehlich, T. E., Lanphear, B. P., Epstein, J. N., Barbaresi, W. J., Katusic, S. K., & Kahn, R. S. (2007). Prevalence, recognition, and treatment of attention-deficit/hyperactivity disorder in a national sample of US children. Archives of Pediatric and Adolescent Medicine, 161, 857–864.
Gadow, K. D., Sprafkin, J., & Nolan, E. E. (2001). DSM-IVSymptoms in community and clinic preschool children. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1383–1392.
Galera, C., Cote, S. M., Bouvard, M. P., Pingault, J., Melchoir, M., Michel, G., Boivin, M., & Tremblay, R. E. (2011). Early risk factors for hyperactivity-impulsivity and inattention from 17 months to 18 years. Archives of General Psychiatry, 68, 1267–1275.
Ghuman, J. K., Aman, M. G., Ghuman, H. S., Reichenbacher, T., Gelenberg, A., Wright, R., Rice, S., & Fort, C. (2009). Prospective, naturalistic, pilot study of open-label atomoxetine treatment in preschool children with attention-deficit/hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology, 19, 155–166.
Ghuman, J. K., Ginsburg, G. S., Subramaniam, G., Ghuman, H. S., Kau, A. S., & Riddle, M. A. (2001). Psychostimulants in preschool children with attention-deficit/hyperactivity disorder: clinical evidence from a developmental disorders institution. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 516–524.
Giedd, J. N., Blumenthal, J., Jeffries, N. O., Rajapakse, J. C., Vaituzis, A. C., Liu, H., et al. (1999). Development of the human corpus callosum during childhood and adolescence: a longitudinal MRI study. Progress in Neuropsychopharmacology & Biological Psychiatry, 23, 571–588.
Gimpel, G. A., & Kuhn, B. R. (2000). Maternal report of attention deficit hyperactivity disorder symptoms in preschool children. Child: Care, Health and Development, 26, 163–176. discussion 176–169.
Gogtay, N., Giedd, J. N., Lusk, L., Hayashi, K. M., Greenstein, D., Vaituzis, A. C., et al. (2004). Dynamic mapping of human cortical development during childhood through early adulthood. Proceedings of the National Academy of Sciences of the United States of America, 101, 8174–8179.
Goldberg, E., & Costa, L. D. (1981). Hemispheric differences in the acquisition and use of descriptive systems. Brain and Language, 14, 144–173.
Gopin, C.B., Berwid, O., Mark, D.J., Mlodnicka, A., Halperin, J.M. (2012). ADHD preschoolers with and without ODD: do they act differently depending on degree of task engagement/reward? Journal of Attention Disorders, (published online Feb 8 prior to publication).
Gopin, C., Healey, D., Castelli, K., Marks, D., & Halperin, J. M. (2010). Usefulness of a clinician rating scale in identifying preschool children with ADHD. Journal of Attention Disorders, 13, 479–488.
Gordon, M., McClure, F. D., & Post, E. M. (1986). Interpretive guide to the Gordon diagnostic system. Syracuse, NY: Gordon Systems.
Gordon, M., & Mettelman, B. B. (1987). Technical guide to the Gordon diagnostic system. Syracuse, NY: Gordon Systems, Inc.
Gottlieb, G. (1991). Experiential canalization of behavioral development: theory. Developmental Psychology, 27, 4–13.
Greenhill, L. L., Muniz, R., Ball, R. R., Levine, A., Pestreich, L., & Jiang, H. (2006). Efficacy and safety if dexmethylphenidate extended-release capsules in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 817–823.
Greenhill, L. L., Posner, K., Vaughan, B. S., & Kratochvil, C. J. (2008). Attention deficit hyperactivity disorder in preschool children. Child and Adolescent Psychiatry Clinics of North America, 17, 347–366.
Gurevitz, M., Geva, R., Varon, M., & Leitner, Y. (2012). Early markers in infants and toddlers for development of ADHD. Journal of Attention Disorders. doi:10.1177/1087054712447858.
Hagelthorn, K. M., Hiemenz, J. R., Pillion, J. P., & Mahone, E. M. (2003). Age and performance parameters in continuous performance tests for preschoolers. Perceptual and Motor Skills, 96(3 Pt 1), 975–989.
Halperin, J. M., Bedard, A. V., & Curchack-Lichtin, J. T. (2012a). Preventive interventions for ADHD: a neurodevelopmental perspective. Neurotherapeutics. doi:10.1007/s13311-012-0123-z.
Halperin, J. M., Marks, D. J., Bedard, A. V., Chacko, A., Curchack, J. T., Yoon, C. A., & Healy, D. M. (2012b). Training executive, attention, and motor skills: a proof-of-concept study in preschool children with ADHD. Journal of Attention Disorders. doi:10.1177/1087054711435681.
Halperin, J. M., & Schulz, K. P. (2006). Revisiting the role of the prefrontal cortex in the pathophysiology of attention-deficit/hyperactivity disorder. Psychological Bulletin, 132, 560–581.
Harper, G. W., & Ottinger, D. R. (1992). The performance of hyperactive and control preschoolers on a new computerized measure of visual vigilance: the preschool vigilance task. Journal of Child Psychology and Psychiatry, 33, 1365–1372.
Healey, D., Miller, C., Castelli, K., Marks, D., & Halperin, J. (2008). The impact of impairment criteria on rates of ADHD diagnoses in preschoolers. Journal of Abnormal Child Psychology, 36, 771–778.
Hood, B. M., & Atkinson, J. (1993). Disengaging visual attention in the infant and adult. Infant Behavior & Development, 16, 405–422.
Huttenlocher, P. R., & Dabholkar, A. S. (1997). Regional differences in synaptogenesis in human cerebral cortex. The Journal of Comparative Neurology, 387, 167–178.
Jané, M. C., Canals, J., Ballespí, S., Viñas, F., Esparó, G., & Domènech, E. (2006). Parents and teachers reports of DSM-IV psychopathological symptoms in preschool children: differences between urban-rural Spanish areas. Social Psychiatry and Psychiatric Epidemiology, 41, 386–393.
Jones, K., Daley, D., Hutchings, J., Bywater, T., & Eames, C. (2008). Efficacy of the incredible years programme as an early intervention for children with conduct problems and ADHD: long-term follow-up. Child: Care, Health and Development, 34, 380–390.
Kadesjo, C., Kadesjo, B., Hagglof, B., & Gillberg, C. (2001). ADHD in Swedish 3- to 7- year old children. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1021–1028.
Kadesjo, C., Hagglof, B., Kadesjo, B., & Gillberg, C. (2003). Attention-deficit-hyperactivity disorder with and without oppositional defiant disorder in 3- to 7-year-old children. Developmental Medicine and Child Neurology, 45, 693–699.
Katsuki, F., & Constantinidis, C. (2012). Early involvement of prefrontal cortex in visual bottom-up attention. Nature Neuroscience, 15, 1160–1166.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., et al. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 980–988.
Kaufman, A. S., & Kaufman, N. L. (2004). Kaufman assessment battery for children-II. Circle Pines: American Guidance Service.
Kerns, K., & Rondeau, L. (1998). Development of a continuous performance test for preschool children. Journal of Attention Disorders, 2, 229–238.
Kinney, H. C., Brody, B. A., Kloman, A. S., & Gilles, F. H. (1988). Sequence of central nervous system myelination in human infancy II: patterns of myelination in autopsied infants. Journal of Neuropathology and Experimental Neurology, 47, 217–234.
Kiselev, S., Espy, K. A., & Sheffield, T. (2009). Age-related differences in reaction time task performance in young children. Journal of Experimental Child Psychology, 102, 150–166.
Knudsen, E. I. (2007). Fundamental components of attention. Annual Review of Neuroscience, 30, 57–78.
Korkman, M., Kirk, U., & Kemp, S. (1998). NEPSY clinical and intrepretative manual. San Antonio: Harcourt Assessment, Inc.
Korkman, M., Kirk, U., & Kemp, S. (2007). NEPSY: second edition clinical and interpretive manual. San Antonio: Pearson.
Kotrla, K. J., & Weinberger, D. R. (2000). Developmental neurobiology. In B. J. Sadock & V. A. Sadock (Eds.), Comprehensive textbook of psychiatry (7th ed., pp. 32–40). Philadelphia: Lippincott Williams & Wilkins.
Kratochvil, C. J., Vaughan, B. S., Stoner, J. A., Daughton, J. M., Lubberstedt, B. D., et al. (2011). A double blind, placeob-controlled study of atomoxetine in young children with ADHD. Pediatrics, 127, e862–e868.
Kraybill, J. H., & Bell, M. A. (2012). Infant predictors of preschool and post-kindergarten executive function. Developmental Psychobiology. doi:10.1002/dev.21057.
Lachter, J., Forster, K. I., & Ruthruff, E. (2004). Forty-five years after Broadbent (1958): still no identification without attention. Psychological Review, 111, 880–913.
Lahey, B. B., Pelham, W. E., Chronis, A., Massetti, G., Kipp, H., Ehrhardt, A., & Lee, S. S. (2006). Predictive validity of ICD-10 hyperkenetic disorder relative to DSM-IV attention-deficit/hyperactivity disorder among younger children. Journal of Child Psychology and Psychiatry, 47, 472–479.
Lahey, B. B., Pelham, W. E., Loney, J., Kipp, H., Ehrhardt, A., Lee, S. S., et al. (2004). Three-year predictive validity of DSM-IV attention deficit hyperactivity disorder in children diagnosed at 4–6 years. The American Journal of Psychiatry, 161, 2014–2020.
Lam, J. C., Mahone, E. M., Mason, E. B. A., & Schraf, S. M. (2011). The effects of napping on cognitive function in preschoolers. Journal of Developmental and Behavioral Pediatrics, 32, 90–97.
Lane, D. M., & Pearson, D. A. (1982). The development of selective attention. Merrill-Palmer Quarterly, 28, 317–337.
Lavigne, J. V., LeBailly, S. A., Hopkins, J., Gouze, K. R., & Binns, H. J. (2009). The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. Journal of Clinical Child and Adolescent Psychology, 38, 315–328.
Lenroot, R. K., Gogtay, N., Greenstein, D. K., Wells, E. M., Wallace, G. L., Clasen, L. S., et al. (2007). Sexual dimorphism of brain developmental trajectories during childhood and adolescence. Neuroimaging, 36, 1065–1073.
Lillard, A. S., & Peterson, J. (2011). The immedicate impact of different types of television on young children’s executive function. Pediatrics, 128, 644–649.
Luna, B., Thulborn, K. R., Munoz, D. P., Merriam, E. P., Carver, K. E., Minshew, N. J., & Sweeney, J. A. (2001). Maturation of widely distributed brain function subserves cognitive development. NeuroImage, 13, 786–793.
Mahone, E. M. (2005). Measurement of attention and related functions in the preschool child. Mental Retardation Developmental Disabilities Research Review, 11, 216–225.
Mahone, E. M., & Hoffman, J. (2007). Behavior ratings of executive function among preschoolers with ADHD. Clinical Neuropsychology, 21, 569–586.
Mahone, E. M., Pillion, J. P., & Hiemenz, J. R. (2001). Initial development of an auditory continuous performance test for preschoolers. Journal of Attention Disorders, 5, 93–106.
Mahone, E. M., Pillion, J. P., Hoffman, J., Hiemenz, J. R., & Denckla, M. B. (2005). Construct validity of the auditory continuous performance test for preschoolers. Developmental Neuropsychology, 27, 11–33.
Mahone, E. M., & Slomine, B. S. (2008). Neurodevelopmental disorders. In J. Morgan & J. Ricker (Eds.), Textbook of clinical neuropsychology (pp. 105–127). New York: Taylor and Francis.
Mariani, M. A., & Barkley, R. A. (1997). Neuropsychological and academic functioning in preschool boys with attention deficit hyperactivity disorder. Developmental Neuropsychology, 13, 111–129.
Marks, D. J., Berwid, O. G., Santra, A., Kera, E. C., Cyrulnik, S. E., & Halperin, J. M. (2005). Neuropsychological correlates of ADHD symptoms in preschoolers. Neuropsychology, 19, 446–455.
Marsh, R., Gerber, A. J., & Peterson, B. S. (2008). Neuroimaging studies of normal brain development and their relevance for understanding childhood neuropsychiatric disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 1233–1251.
Massetti, G. M., Lahey, B. B., Pelham, W. E., Loney, J., Ehrhardt, A., Lee, S. S., & Kipp, H. (2007). Academic achievement over 8 years among children who met modified criteria for attention-deficit/hyperactivity disorder at 4–6 years of age. Journal of Abnormal Child Psychology, 36, 399–410.
McGee, R., Partridge, F., Williams, S., & Silva, P. A. (1991). A twelve-year follow-up of preschool hyperactive children. Journal of the American Academy of Child and Adolescent Psychiatry, 30, 224–232.
McGoey, K. E., DuPaul, G. J., Haley, E., & Shleton, T. L. (2007). Parent and teacher ratings of attention deficit/hyperactivity disorder in preschool: the ADHD rating scale-IV preschool version. Journal of Psychopathology and Behavioral Assessment, 29, 269–276.
McGrath, A. M., Handwerk, M. L., Armstrong, K. J., Lucas, C. P., & Friman, P. C. (2004). The validity of the ADHD section of the diagnostic interview for children. Behavioral Modification, 28, 349–374.
Mirsky, A. F., Anthony, B. J., Duncan, C. C., Ahern, M. B., & Kellam, S. G. (1991). Analysis of the elements of attention: a neuropsychological approach. Neuropsychology Review, 2, 109–145.
Morasch, K. C., & Bell, M. A. (2011). The role of inhibitory control in behavioral and physiological expressions of toddler executive function. Journal of Experimental Child Psychology, 108, 593–606.
Mrzljak, L., Uylings, H. B., Van Eden, C. G., & Judas, M. (1990). Neuronal development in human prefrontal cortex in prenatal and postnatal stages. Progress in Brain Research, 85, 185–222.
Muller, U., Kerns, K. A., & Konkin, K. (2012). Test-retest reliability and practice effects of executive function tasks in preschool children. The Clinical Neuropsychologist, 26, 271–287.
Newborg, J., Stock, J. R., & Wnek, L. (1988). The manual for the Battell Developmental Inventory. Boston: Houghton Mifflin.
Nigg, J. T., Goldsmith, H. H., & Sachek, J. (2004). Temperament and attention deficit hyperactivity disorder: the development of a multiple pathway model. Journal of Clinical Child and Adolescent Psychology, 33, 42–53.
Nolan, E. E., Gadow, K. D., & Sprafkin, J. (2001). Teacher reports of DSM-IV ADHD, ODD, and CD symptoms in schoolchildren. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 241–249.
Noland, J. S., Singer, L. T., Short, E. J., Minnes, S., Arendt, R. E., Kirchner, H. L., & Bearer, C. (2005). Prenatal drug exposure and selective attention in preschoolers. Neurotoxicology and Teratology, 27, 429–438.
Nomura, Y., Marks, D. J., Grossman, B., Yoon, M., Loudon, H., Stone, J., & Halperin, J. M. (2012). Exposure to gestational diabetes mellitus and low socioeconomic status: effects on neurocognitive development and risk of attention-deficit/hyperactivity disorder in offspring. Archives of Pediatrics & Adolescent Medicine, 166, 337–343.
Palfrey, J. S., Levine, M. D., Walker, D. K., & Sullivan, M. (1985). The emergence of attention deficits in early childhood: a prospective study. Journal of Developmental and Behavioral Pediatrics, 6, 339–348.
Pauli-Pott, U., & Becker, K. (2011). Neuropsychological basic deficits in preschoolers at risk for ADHD: a meta-analysis. Clinical Psychology Review, 31, 626–637.
Pavuluri, M. N., Luk, S. L., & McGee, R. (1999). Parent reported preschool attention deficit hyperactivity: measurement and validity. European Child & Adolescent Psychiatry, 8, 126–133.
Peterson, S. E., & Posner, M. I. (2012). The attention system of the human brain: 20 years after. Annual Review of Neuroscience, 35, 73–89.
Pliszka, S. R. (2007). Pharmacologic treatment of attention-deficit/hyperactivity disorder: efficacy, safety, and mechanisms of action. Neuropsychology Review, 17, 61–72.
Poblano, A., & Romero, E. (2006). ECI-4 screening of attention deficit-hyperactivity disorder and co-morbidity in Mexican preschool children. Arquivos de Neuro-Psiquiatria, 64, 932–936.
Posner, K., Melvin, G. A., Murray, D. W., Gugga, S. S., Fisher, P., Skrobala, A., et al. (2007). Clinical presentation of attention-deficit/hyperactivity disorder in preschool children: the Preschoolers with Attention-Deficit/Hyperactivity Disorder Treatment Study (PATS). Journal of Child and Adolescent Psychopharmacology, 17, 547–562.
Posner, M. I., & Peterson, S. E. (1990). The attention system of the human brain. Annual Review of Neuroscience, 13, 25–42.
Prather, P. A., Sarmento, N., & Alexander, A. (1995). Development of vigilance in preschoolers [Abstract]. Journal of the International Neuropsychological Society, 1, 153.
Pribram, K. H., & McGuinness, D. (1975). Arousal, activation, and effort in the control of attention. Psychological Review, 2, 116–149.
Pulsifer, M. B., Butz, A. M., O’Reilley Foran, M., & Belcher, H. M. E. (2008). Prenatal drug exposure: effects on cognitive functioning at 5 years of age. Clinical Pediatrics, 47, 58–65.
Rappley, M., Eneli, I., & Mullan, P. (2002). Patterns of psychotropic medication use in very young children with attention-deficit hyperactivity disorder. Journal of Developmental and Behavioral Pediatrics, 23, 23–30.
Rapport, M. D., Scanlan, S. W., & Denney, C. B. (1999). Attentiondeficit/hyperactivity disorder and scholastic achievement: a model of dual developmental pathways. Journal of Child Psychology and Psychiatry, 40, 1169–1183.
Reynolds, C., & Kamphaus, R. (2004). Behavior assessment system for children-2. Circle Pines: American Guidance Systems, Inc.
Rezazadeh, S. M., Wilding, J., & Cornish, K. (2011). The relationship between measures of cognitive attention and behavioral ratings of attention in typically developing children. Child Neuropsychology, 17, 197–208.
Root, R. W., II, & Resnick, R. J. (2003). An update on the diagnosis and treatment of attention-deficit/hyperactivity disorder in children. Professional Psychology: Research and Practice, 34, 34–41.
Ryan, A. S., & Nelson, E. B. (2008). Assessing the effect of docosahexaenoic acid on cognitive functions in healthy, preschool children: a randomized, placebo-controlled, double-blind study. Clinical Pediatrics, 47, 355–362.
Shaffer, D., Fisher, P., Lucas, C. P., Dulcan, M. K., & Schwab-Stone, M. E. (2000). NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 28–38.
Shaw, P., Eckstrand, K., Sharp, W., Blumenthal, J., Lerch, J. P., Greenstein, D., et al. (2007). Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proceedings of the National Academy of Sciences of the United States of America, 104, 19649–19654.
Shelton, T., & Barkley, R. (1993). Assessment of attention deficit hyperactivity disorder in young children. In J. Culbertson & D. Willis (Eds.), Testing young children (pp. 290–318). Austin: Pro-Ed.
Short, E. J., Manos, M. J., Findling, R. L., & Schubel, E. A. (2004). A prospective study of stimulant response in preschool children: insights from ROC analyses. Journal of the American Academy of Child and Adolescent Psychiatry, 43, 251–259.
Smidts, D. P., & Oosterlaan, J. (2007). How common are symptoms of ADHD in typically developing preschoolers? a study on prevalence rates and prenatal/demographic risk factors. Cortex, 43, 710–717.
Sonuga-Barke, E. J. S., Koerting, J., Smith, E., McCann, D. C., & Thompson, M. (2011). Early detection and intervention for attention-deficit/hyperactivity disorder. Expert Reviews Neurotheapeutics, 11, 557–563.
Sowell, E. R., Thompson, P. M., Welcome, S. E., Henkenius, A. L., Toga, A. W., & Peterson, B. S. (2003). Cortical abnormalities in children and adolescents with attention-deficit hyperactivity disorder. Lancet, 362, 1699–1707.
Sprafkin, J., & Gadow, K. D. (1996). Early childhood symptom inventories. Stony Brook: Checkmate Plus.
Sprafkin, J., Volpe, R. J., Gadow, K. D., Nolan, E. E., & Kelly, K. (2002). A DSM-IV-referenced screening instrument for preschool children: the early childhood inventory-4. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 604–612.
Stefanatos, G. A., & Baron, I. S. (2007). Attention deficit/hyperactivity disorder: a neuropsychological perspective toward DSM-V. Neuropsychology Review, 17, 5–38.
Swanson, J., Greenhill, L., Wigal, T., Kollins, S., Stehli, A., Davies, M., et al. (2006). Stimulant-related reductions of growth rates in the PATS. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 1304–1313.
Tandon, M., Xuemei, S., & Luby, J. (2011). Preschool onset ADHD: course and predictors of stability over 24 m. Journal of Child and Adolescent Psychopharmacology, 21, 321–330.
Thompson, M. J., Laver-Bradbury, C., Ayres, M., Le Poidevin, E., Mead, S., Dodds, C., et al. (2009). A small scale randomized controlled trial of the revised new forest parenting programme for preschoolers with attention deficit hyperactivity disorder. European Journal of Child and Adolescent Psychiatry, 18, 605–616.
Thorell, L. B. (2007). Do delay aversion and executive function deficits make distinct contributions to the functional impact of ADHD symptoms? a study of early academic skill deficits. Journal of Child Psychological Psychiatry, 48, 1061–1070.
Vitiello, B., Abikoff, H. B., Chuang, S. Z., Kollins, S. H., McCracken, J. T., Riddle, M. A., et al. (2007). Effectiveness of methylphenidate in the 10-month continuation phase of the Preschoolers with Attention-Deficit/Hyperactivity Disorder Treatment Study (PATS). Journal of Child and Adolescent Psychopharmacology, 17, 593–604.
Wahlstedt, C., Thorell, L. B., & Bohlin, G. (2008). ADHD symptoms and executive function impairment: early predictors of later behavior problems. Developmental Psychology, 33, 160–178.
Weisen, S. (2008). Clinical use of the Differential Abilities Scales-second edition (DAS-II) for children with attention deficit/hyperactivity disorder [Abstract]. Dissertation Abstracts International, Section B: Sciences and Engineering, 69(6-B), 3863.
White, R. F., Campbell, R., Echeverria, D., Knox, S. S., & Janulewicz, P. (2009). Assessment of neuropsychological trajectories in longitudinal population-based studies of children. Journal of Epidemiology and Community Health, 63(suppl 1), i15–i26.
Wilding, J., Munir, F., & Cornish, K. (2001). The nature of attentional differences between groups of children differentiated by teacher ratings of attention and hyperactivity. British Journal of Psychology Bulletin, 92, 357–371.
Wilens, T. E., Biederman, J., Brown, S., Monuteaux, M., Prince, J., & Spencer, T. J. (2002). Patterns of psychopathology and dysfunction in clinically referred preschoolers. Journal of Developmental and Behavioral Pediatrics, 23(1 Suppl), S31–S36.
Wilens, T. E., Biederman, J., Brown, S., Tanguay, S., Monuteaux, M. C., Blake, C., & Spencer, T. J. (2002). Psychiatric comorbidity and functioning in clinically referred preschool children and school-age youths with ADHD. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 262–268.
Willoughby, M. T., Pek, J., Greenberg, M. G., et al. (2012). Journal of Abnormal Child Psychology. doi:10.1007/s10802-012-9641-8.
Yochman, A., Ornoy, A., & Parush, S. (2006). Co-occurrence of developmental delays among preschool children with attention-deficit-hyperactivity disorder. Developmental Medicine and Child Neurology, 48, 483–488.
Youngwirth, S. D., Harvey, E. A., Gates, E. C., Hashim, R. L., & Friedman-Weieneth, J. L. (2007). Neuropsychological abilities of preschool-aged children who display hyperactivity and/or oppositional defiant behavior problems. Child Neuropsychology, 13, 422–443.
Acknowledgments
This work was supported by the National Institutes of Health Grants R01 HD068425, P30 HD 24061 (Intellectual and Developmental Disabilities Research Center), the Johns Hopkins Brain Sciences Institute, and the Johns Hopkins University School of Medicine Institute for Clinical and Translational Research, an NIH/NCRR CTSA Program, UL1-RR025005.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mahone, E.M., Schneider, H.E. Assessment of Attention in Preschoolers. Neuropsychol Rev 22, 361–383 (2012). https://doi.org/10.1007/s11065-012-9217-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-012-9217-y