Abstract
Functional neuroimaging offers the opportunity to understand the effect of prenatal alcohol exposure on the activities of the brain as well as providing a window into the relationship between neural activation and the behavioral outcomes that have been described in affected individuals. Several different methodologies have been used to examine the neurophysiological signal changes associated with different brain functions in prenatally exposed individuals and those diagnosed with fetal alcohol syndrome (FAS) or other fetal alcohol spectrum disorders (FASD). These include electroencephalography (EEG), positron emission tomography (PET), single-photon emission computed tomography (SPECT), and functional magnetic resonance imaging (fMRI). These studies demonstrate that it is feasible to use these technologies with this clinical population and that the damage to the central nervous system associated with prenatal alcohol exposure has widespread functional implications; however, currently, the literature in these areas is limited and unsystematic. Functional MRI with this clinical population has just begun to explore the implications of prenatal alcohol exposure with the first paper published in 2005. Other methodologies are similarly limited in scope. Nonetheless, these functional neuroimaging studies suggest that prenatal alcohol exposure, or a diagnosis of FAS, may lead to restrictions in neural efficiency or a global decrement in processing resources.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol is a potent teratogenic agent that affects the development of the brain in individuals exposed prenatally. Neurodevelopmental consequences have been documented through behavioral studies of exposed children and young adults since the fetal alcohol syndrome (FAS) was first described in the 1970’s (Jones and Smith 1973). Both individuals who meet criteria for FAS and those who fall on what is called the fetal alcohol spectrum (fetal alcohol spectrum disorders: FASD) show numerous behavior alterations and cognitive deficits. Microcephaly is used as a diagnostic criterion for FAS. Human (Spadoni et al. 2007) and animal studies (Sulik et al., this volume) have documented both global and specific alterations in brain anatomy. For instance, alcohol exposure is often associated with smaller intracranial volume as well as volume deficits in specific brain regions over and above those accounted for by small intracranial volume (Archibald et al. 2001; Chen et al. 2011). Given this evidence of neurological and neurobehavioral impact, it is highly probable that functional neuroimaging, which enables observation and recording of brain activation in human samples, also will identify alterations associated with prenatal alcohol exposure whether or not accompanied by structural differences. A second finding may be the demonstration of relationships between functional alterations and observable cognitive deficits or behavioral abnormalities, which could have diagnostic implications. Finally, investigation of such relationships can add significantly to our general understanding of the relationship between brain and behavior over development. This paper will review what is still a limited body of research that has used functional neuroimaging to examine the nature and extent of alcohol’s effects on the developing brain. In addition, we will note the constraints that currently exist on interpretation of these results and indicate directions for future research.
Methods for Functional Neuroimaging
Functional neuroimaging includes those techniques that measure the neurophysiological signal changes associated with different brain functions. These signal changes are usually caused by performing a specific task or by switching between different task states, but recordings can also be made during sleep or during what is called “resting state” when no specific task is occurring. The results are thought to provide information about the neuromechanisms underlying the brain functions that are associated with various sensory and cognitive activities. A number of functional neuroimaging approaches have been used in studies of the effects of prenatal alcohol exposure. These include electroencephalography (EEG), positron emission tomography (PET), single-photon emission computed tomography (SPECT), and functional magnetic resonance imaging (fMRI). Each of these techniques has its own advantages and limitations and these are summarized in the next section.
Electroencephalography (EEG) uses scalp electrodes to detect and measure gross field potentials caused by synchronized synaptic activities in the brain (Nunez and Srinivasan 2006). Thus, unlike other imaging methods, EEG provides relatively direct measurement of electric neuronal activity and it offers the best temporal resolution (~microsecond) among functional neuroimaging approaches. However, as the neuronal activation sources are usually separated from the electrodes by inactivated tissues, like cerebrospinal fluid, skull and scalp, the spatial resolution of EEG is relatively low in relation to other neuroimaging approaches. In addition, due to scalp recording and noise, there are limitations in the brain regions that can be measured, especially for those sources deep within the brain (Whittingstall et al. 2003). EEG is the oldest of the modern functional brain imaging techniques. As a result it is probably the best understood in terms of its relationship with behavioral correlates. For example, early ERP (event-related potential) components, like P1—a positive voltage deflection around 100 ms after stimulus onset, usually represent perceptual responses while late ERP components, like P3, usually represent attention-demanding cognitive processing. Besides the early and late components, two negative components—N2 and ERN, appearing around 200 ms, are often reported in studies of cognitive functions. N2 reflects conflict monitoring and executive control while ERN is related to error detection. A general introduction to various ERP components and associated brain processes can be found in (Fabiani et al. 2000).
Single-photon emission computed tomography (SPECT) is a nuclear medical tomographic technique that uses gamma rays to evaluate blood flow or concentration of various neurotransmitters. Following injection of a radioisotope, a gamma camera is used to acquire, from different angles, 2D projections of a 3D distribution of radioactive tracers. These 2D projections are fed into a subsequent algorithm of 3D reconstruction to produce 3D images. As blood flow is coupled to metabolic activity, SPECT can be used to evaluate brain metabolism regionally. As a well-established technique, SPECT is widely available and used with inexpensive radio tracer. However, low image resolution, signal attenuation and non-quantifiable blood flow measure are its traditional disadvantages.
Positron emission tomography (PET) also relies on radioactive materials and gamma ray detection. However, instead of direct gamma radiations, PET tracers emit positrons that annihilate with electrons thus generating two gamma photons travelling in opposite directions. A PET scanner detects these emission “coincidences” that can provide images in a higher resolution than SPECT (Wernick and Aarsvold 2004). PET is often used to quantitatively evaluate glucose metabolism and blood flow that is associated with brain activity. In addition, it is possible to radiolabel compounds that bind selectively to specific neuroreceptors (e.g., dopamine and serotonin receptors); therefore, metabolic activity of many neurotransmitters can be examined by PET as well. PET and SPECT are widely used to measure changes of blood flow and brain metabolism; but due to the reliance on radioactive materials, both are considered “invasive” approaches and are more often used in clinical samples than for research purposes.
Functional magnetic resonance imaging (fMRI) is now commonly used in the study of human brain function. This specialized form of magnetic resonance imaging was developed in the early 1990’s. Employing the different magnetic susceptibility of oxygenated and deoxygenated hemoglobin and the concentration changes caused by local neural activation (Cohen and Bookheimer 1994), most fMRI studies measure blood oxygen level dependent (BOLD) magnetic resonance signals. Specifically, local neural activation is associated with increased consumption of energy and increased blood oxygen levels; and oxygenated hemoglobin has a different MR signal from that produced by deoxygenated hemoglobin. The BOLD fMRI signal is often termed the hemodynamic response. This response is characterized by an initial delay of a few seconds, a peak over 4–6 s and then a signal recovery over more than 10 s. Compared with other volumetric functional imaging techniques, fMRI is fast in imaging speed. The acquisition of a 3 × 3 × 3 mm3 resolution brain volume regularly only takes 2–3 s (typical fMRI scan needs repetitive volume measurements and takes several minutes). Besides BOLD fMRI, there are also other fMRI approaches. For instance, arterial spin labeling can directly measure cerebral blood flow (CBF) and provide similar information to PET but without the disadvantage of using radioactive materials (Aguirre et al. 2005; Feng et al. 2004).
There are several advantages to fMRI over other forms of functioning imaging. In addition to its high availability and its noninvasive nature, is the high spatial resolution that can distinguish brain structures at millimeter scale. Further, with this technique it is possible to examine the whole brain area as it is engaged with a particular task. With these advantages, fMRI has become the primary tool in volumetric functional neuroimaging and its application has exhibited a increasing trend in studies of prenatal drug exposure (Derauf et al. 2009; Norman et al. 2009).
While being the most effective neuroimaging approach currently available, fMRI does have limitations. In contrast to EEG, which has a high temporal resolution, the relatively slow hemodynamic response limits its capability in capturing fast changes in temporal domain. Its spatial specificity is subject to distribution of local vascular structure and susceptibility artifacts. Most importantly, the BOLD response is only a surrogate signal of local neuronal activations; that is, it is an indirect assessment of neuronal activity. Other limitations of fMRI include the complexity of experiment designs required as well as data interpretation when such designs are used. Finally, this methodology is sensitive to motion artifacts that can limit the use of the technique with children and clinical populations. More details about advantages/disadvantages of fMRI and about how to use this technique appropriately in basic neuroscience research are reviewed extensively by Logothetis (2008).
Functional Imaging to Study Fetal Alcohol Spectrum Disorders and Effects of Prenatal Alcohol Exposure
Early applications of functional neuroimaging studies in samples of children exposed to alcohol due to maternal use during gestation were carried out with EEG, SPECT and PET (see Table 1). With SPECT, differences in cerebral blood perfusion were reported in the temporal (Bhatara et al. 2002) as well as parieto-occipital and prefrontal (Riikonen et al. 1999) regions of alcohol-affected subjects. A SPECT study also showed a group difference in medial-frontal serotonin transporter binding and increased striatal dopamine transporter binding in alcohol-exposed individuals (Riikonen et al. 2005). With PET, differences associated with alcohol exposure were found in the regional cerebral metabolic rates in thalamus and basal ganglia (Clark et al. 2000). However, though they employed functional neuroimaging approaches, all of these early SPECT and PET studies simply focused on the “resting-state” brain. As a result, they do not provide direct insights into the effects on specific behavioral deficits (e.g., attention deficit or memory problems) that have been found to be associated with prenatal exposure or with the diagnosis of FAS. In addition, compared with recent studies, some of these early studies have methodological issues that may limit interpretation. These issues include relatively small sample sizes and less sophisticated methods for data handling than are used currently (e.g., data simply being visually inspected).
EEG Studies of FASD also revealed alterations associated with prenatal alcohol exposure (D’Angiulli et al. 2006). The earliest work, carried out in the 1970’s and 1980’s, used exposure samples rather than the clinically identified samples that have characterized much later work. Exposure samples are composed of individuals identified through maternal drinking, usually during the prenatal period, and followed longitudinally. These early studies focused on outcome in infancy, particularly on arousal regulation, sleep and sensory processing (see Table 1). Studies of older children and adolescents, discussed below, have examined attention and cognition and have identified reductions in mean power of alpha frequencies (Kaneko et al. 1996; Mattson et al. 1992).
EEG studies of the impact of prenatal alcohol exposure on sleep during infancy (Chernick et al. 1983; Havlicek et al. 1977; Ioffe et al. 1984) found that, in comparison to non-exposed infants, infants of drinking mothers showed generalized EEG hypersynchroncy in all stages of sleep. In at least one longitudinal study, these power increases were found to be correlated with later developmental outcomes in the same children (Ioffe and Chernick 1990) with those showing increased EEG power having lower motor and mental development scores. In another sample, alcohol-exposed infants were found to have more disturbed sleep and more frequent arousals (Scher et al. 1988) than unexposed controls. Studies of sensory processes (that is auditory, visual and somatosensory evoked potentials) in alcohol exposed and affected children have also been done using EEG responses to specific stimuli (Church and Gerkin 1988; Olegård et al. 1979; Pettigrew and Hutchinson 1984; Rössig et al. 1994; Scher et al. 1998). Auditory brainstem responses (ABR) are used to evaluate initial sensory processing of auditory stimuli and in studies using this methodology, alcohol exposure is associated with slower perception of auditory information (that is with prolonged latencies) (Church and Gerkin 1988; Kable et al. 2009; Pettigrew and Hutchinson 1984). Similarly, visual processing was assessed by Scher et al. (1998) who found that certain wave latencies (i.e., N1, P1, at 1 month, and N2, at 4 months) were prolonged early in infancy in a manner suggesting developmental delays.
Studies of older children and adults with FASD using EEG have focused on attention and cognitive function. Kaneko et al. (1996) used an evoked-potential, oddball paradigm that was passive in nature; that is, it did not require an active response, and found that at least half of the alcohol-affected children tested had EEGs that could be classified as “abnormal”. This was one of the only studies to compare alcohol-affected children to both unexposed controls and another clinical group, those with Down syndrome. FAS diagnosis was found to be associated with slower P3 latencies than were shown by either contrast group. However, in this sample of older children, the N1 wave, noted to be altered by Scher et al. (1998) in infants, did not discriminate alcohol exposed from the other groups. Both N1 and P3 are believed to be associated with attentional responses.
Several recent studies also employed event-related potential (Burden et al. 2009, 2010, 2011). Two of these studies examined the effect of alcohol exposure on inhibitory control with similar task paradigms (Go/No-Go) administered to two samples recruited from Cape Town, South Africa and Detroit, Michigan. The Cape Town sample, whose mean age was 11.7 years (Burden et al. 2009), had a much higher level of prenatal alcohol exposure than the Detroit sample. The Cape Town sample used alcohol 42.8% of days during the month in contrast to the 13.6% in Detroit. In addition, in Cape Town, the mean ounces of absolute alcohol consumed per day (oz AA/dy) was 2.9 (SD = 3.0) versus 0.3 (SD = 0.7) in Detroit. In this Cape Town sample, prolonged latency of P2, and diminished Go vs. No-go amplitude difference of P2 and N2 components were observed in the alcohol-exposed children. These alterations reflect inefficient visual processing (prolonged P2), impaired early discrimination between conditions (P2 amplitude), and less controlled response inhibition (N2 amplitude).
In addition, the exposed group showed a long lasting P3 component, suggesting increased cognitive effort (Fig. 1). The data from the less heavily alcohol-exposed Detroit sample (Burden et al. 2010), who were adolescents rather than school-aged children, did not replicate these alcohol-related difference in group response suggesting that there may be more evidence of effects of exposure with higher doses. However, the focus of the Detroit study was a comparison of the characteristics of alcohol-exposed children with and without attention deficit hyperactivity disorder (ADHD). Responses of participants with ADHD were found to be uniquely associated with diminished P3 difference between the “Go” and “No-Go” condition. Such diminished response was not associated with alcohol exposure. P3 is believed to reflect both response inhibition and persistent cognitive effort and often is found to be diminished in individuals with attentional disorders. The investigators interpreted this result as suggesting that alcohol-affected individuals and those with ADHD, though sharing similar symptomatology, are different in certain aspects of their neural basis. In a third study (Burden et al. 2011), these investigators carried out a large scale EEG study in Inuit children, mean age 11.3 years, using the same Go/No-Go paradigm as well as a measure of continuous recognition memory. Maternal binge drinking during pregnancy was found to be associated with alterations in EEG responses, with the alcohol-exposed group showing slower P2 latencies on the inhibition task, suggesting slower visual processing, and reduced amplitudes on the memory protocol in components associated with item familiarity and retrieval. It is of interest that, when behavior was measured, both accuracy and reaction time on these tasks were equivalent for both groups despite differences in EEG response. The authors of these papers interpreted all of these results in light of the “dose” of alcohol associated with each group to suggest that more extensive exposure had more comprehensive effects on EEG results.
Event related potentials recorded in the prenatal alcohol exposed and control subjects in a Go/No-go task. The ERP waveforms are displayed on the left and the components with significant group differences are topographically displayed on the right. This figure is adapted from (Burden et al. 2009) with permission
Review of these EEG studies indicates that there are alterations in response associated with alcohol exposure but that outcomes may be affected by dose, comorbidity and development changes that make effects more or less apparent as individuals grow older. Changes over age in EEG results in alcohol-affected samples were noted previously by Spohr and Steinhausen (1987) and are reviewed by D’Angiulli et al. (2006).
Functional MRI is the technique most commonly employed in functional neuroimaging studies of the effects of prenatal alcohol exposure, although the body of research in this area remains limited. The first research paper using this methodology appeared in 2005 (Malisza et al. 2005) and there are currently nine published papers in this area (See Table 2). Of these, four concerned working memory, one verbal paired associate learning, two math processing, one inhibitory control and one visual sustained attention. Of those that have examined working memory, two focused on spatial memory (Malisza et al. 2005; Spadoni et al. 2009), one on verbal working memory (O’Hare et al. 2009) and one on facial recognition (Astley et al. 2009). A review of these papers (below) suggests that there are a variety of outcomes found whose results cannot be easily synthesized. For this reason, the information from these studies is provided followed by a discussion of the challenges associated with research in this area with reference to the cited studies.
Malisza et al. (2005) used clinically recruited samples of both children and adults to examined spatial working memory function. Their hypothesis was that, using fMRI, differences would be noted in brain regions associated with working memory performance, particularly in frontal areas, which support efficient working memory. No structural MR (or brain volume) differences were found in either children or adults although there were behavioral differences on cognitive task performance. The fMRI results were complex. BOLD activation was found to be affected by group status (FASD versus controls), age, and task difficulty. In the FASD group, there was increased activation in the inferior and middle frontal regions during spatial memory tasks. In controls, more parietal activation was observed. Different patterns of outcomes were found in children and adults. In children, the control group showed increased frontal lobe activity as the task difficulty increased while those with FASD showed an opposite effect. That is, they showed increased activation relative to controls on easier tasks but reduced response on more difficult cognitive tasks. In the adults (age range: 18–33 years), the FASD group generally showed less brain activation than the controls. With increasing task difficulty, both the child and adult controls, exhibited increasing brain activation in frontal regions, but the children and adults with FASD did not. The authors suggest that alcohol diagnosis is associated with “improper” functioning in the prefrontal areas of the brain that affects working memory skills.
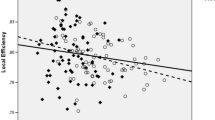
Another fMRI study focused on spatial working memory in clinically-recruited children and adolescents (mean age 13.6–14.7 years) (Spadoni et al. 2009). Data analysis was restricted to those participants who were able to perform behavioral tasks within the scanner to acceptable criteria (total accuracy 69–100%). In this study, as well, overall brain size did not differ between groups. The authors reported that, for the FASD group, greater frontal BOLD response was noted during the spatial working memory tasks but not during the simple vigilance task. That is, this study observed “greater-activations” in the alcohol group in extended brain regions during the spatial working memory task (Fig. 2). In an analysis comparing brain activation with task efficiency, greater activation in right middle frontal gyrus (Brodmann Areas 8 & 6), medial frontal and superior frontal gyri were found to be related to a shorter reaction time in task for the contrast group but not for the alcohol-affected group. The authors suggest that findings may indicate a delay in achieving mature information processing by the alcohol-affected children.
Functional brain activation differences (bottom frame) between the prenatal alcohol exposed (top-left frame) and control (top-right frame) subjects in a spatial working memory task. The exposed group exhibited greater activation in extended brain regions. This figure is adapted from (Spadoni et al. 2009) with permission
Interpretation of results can be difficult as inconsistencies in study results could be due to a number of factors, including the experimental group difference on behavior performance. In the study of Malisza et al., the exposed group was generally impaired in behavioral performance while in that of Spadoni et al. the group difference was not significant. However, differences in results could also be related to a number of other sources of variability including task characteristics (that is, difficulty), ability differences (IQ), or comorbid psychiatric conditions. Variations in brain structure can also affect activation (see Bookheimer and Sowell 2005 for a commentary on these issues).
In addition to spatial working memory, fMRI has been used to examine working memory for verbal information (O’Hare et al. 2009) and faces (Astley et al. 2009). For verbal working memory, O’Hare and colleagues, reported increased brain activation in the alcohol group (mean age 10.7 years) in the left dorsal frontal, left inferior parietal and bilateral posterior temporal regions even when behavioral performance did not differ. This increase in activation is consistent with the findings of this group in their study of spatial working memory discussed above (Spadoni et al. 2009).
In a study that used working memory for facial recognition, Astley et al. (2009) reported lower brain activation in the exposed group in extended prefrontal and parietal regions, particularly in the right hemisphere and particularly on tasks requiring more “mental effort”. Participants were clinically identified children with FASD and controls (age range: 8–15.9 years) and neuroactivation was assessed in seven brain regions include anterior cingulate, anterior and posterior parietal lobes and several frontal regions, including dorsolateral prefrontal, inferior frontal, middle frontal and precentral regions. During an “N-back” facial recognition task, the right inferior frontal gyrus, right posterior parietal lobe, right dorsal lateral prefrontal cortex, and right middle frontal gyrus, were found to exhibit greater activation by controls but not by those most affected by alcohol exposure. On an easier version of this task (1-back versus 2-back), there were no group differences in activation.
Inconsistency can be noticed between the findings of these two studies of working memory with the exposed group showing generally higher activation in the verbal study but generally lower activation in the face study. Certainly, differences may be the result of differences associated with task difficulty; however, group difference on behavior performance may contribute to these results, as well. In the face recognition study, those in the FASD group showed impaired behavior performances as well as IQ scores that are significantly lower than those in the control group while in the verbal memory study, those in the alcohol group performed at a comparable level on the in-scanner task although they also had lower mean ability scores than the controls.
Two recent fMRI studies examined functional alterations associated with number processing (Meintjes et al. 2010; Santhanam et al. 2009) based on behavioral research that suggests that number processing and math are areas of specific deficit in alcohol-exposed individuals (Kable and Coles 2004). Using a subtraction task, with a sample of prenatally exposed young adults and controls (Mean age: 23.2 years) with similar ability level and demographic characteristics, Santhanam and colleagues (2009) reported lower activation by alcohol-affected individuals in parietal and prefrontal regions known to be involved in arithmetic processing (Dehaene et al. 2004). In this study, which employed a longitudinal cohort identified prenatally, whole brain size was significantly smaller in alcohol-exposed adults. To reduce potential distortions associated with normalization of brain images to standardized templates, ROIs were defined in the standard space (template) but back-projected into the native space of each individual. Activation intensity and number of activated voxels of each ROI then were calculated in native space. In addition, activated voxel numbers for each ROI were individually normalized to the size of the ROI mask for each individual. This approach makes the group comparison less sensitive to normalizing distortions than typical procedures. In this study, behavioral performance on the subtraction task also was poorer in the alcohol groups but these results were not correlated with activation outcomes.
Meintjes and colleagues used tasks of exact addition and proximity judgment to examine brain activation associated with number processing (Meintjes et al. 2010). Participants were school-aged South African children (8–12 years) who had been exposed prenatally to heavy alcohol use. Control children were born to nonusers or to women drinking fewer than 7 drinks a week. Behavioral performance in the scanner was equalized by controlling task difficulty and excluding the data of children who could not meet accuracy criteria (for proximity judgment, 8 of 15 participants in the FASD group were excluded); more exacting neuropsychological tasks performed outside the scanner did show significant differences with the group heavily exposed to alcohol performing more poorly. Functional MRI results indicated additional or more widespread activation by the exposed group rather than activation that was specific to the regions that were identified as active in math processing. In contract, such specific activation was characteristic of the controls.
Functional MRI was used in three other studies examining brain alterations associated with inhibitory control (Fryer et al. 2007), verbal paired associate learning (Sowell et al. 2007) and sustained visual attention (Li et al. 2008). As the research designs and experimental tasks varied significantly, they must be considered separately.
Executive functioning has been identified as an area of concern in alcohol-affected individuals and inhibitory control is considered a major component of the behavioral pathology reported in individuals with FASD. To study inhibitory control, Fryer and colleagues (2007) used a “Go/No-Go” task with clinically identified children and adolescents (ages: 8–18) and controls. In this sample, brain size did not differ and there was similar behavioral performance between the alcohol group and the controls. However, greater BOLD response was noted in the alcohol group versus the control group in the left medial and right middle frontal gyri with less activation in the right caudate nucleus. The authors attribute these results to altered frontral-striatal activation patterns in the alcohol group that may require greater activation of frontal regions during inhibition.
To study verbal paired associate learning, Sowell et al. compared clinically diagnosed children, ages 8–13, with a contrast group (Sowell et al. 2007). Both groups had mean ability (IQ) scores in the average range but there remained a 20 point IQ differences between these two groups. A paired association task was done during the scan but behavioral performance was not recorded to avoid motion artifacts associated with a verbal response. The imaging finding was that the FASD group showed less activation in the left medial and posterior temporal regions but more activation in the right dorsal frontal cortex. The areas of underactiviation relative to controls are those usually thought to be associated with memory function.
The single study of sustained visual attention (Li et al. 2008) focused on the occipital-temporal region, which resides at the receiving end of attention modulation. The adult participants in this study were members of a longitudinal cohort identified prenatally. Alcohol-exposed participants showed both impairments of sustained attention on the behavioral task as well as structural volume reduction in the occipital-temporal region. Examination of white matter alterations in this area and of functional activation associated with this task indicated correspondence between the two measures. The authors hypothesized that, in the alcohol-exposed participants, functional activation patterns were altered due to structural impairment in this region.
These functional neuroimaging studies suggest that prenatal alcohol exposure and FASD diagnosis are associated with alterations in brain function in widespread cortical and subcortical regions. In addition, there are suggestions of a general association between functional brain activation and behavioral outcomes. In some cases, these functional alterations have been correlated with impairments in several different cognitive and behavioral outcomes. It is apparent, however, that there are a number of factors that affect the specific patterns of both behavior performance and BOLD activation across these studies. Results can vary depending not only on experimental group differences but also due to subject characteristics and task parameters.
Methodological Issues for Functional Neuroimaging Studies of FASD
The brief review of fMRI studies presented above does not provide a clear and consistent pattern associated with FASD or prenatal alcohol exposure. We suggest that, in addition to the general limitations that affect the interpretation of functional imaging studies, there are also specific issues associated with the study of FASD that should be noted.
Artifact/inaccuracy in image registration due to microcephaly generally affects the results of fMRI studies. To perform group analysis, fMRI data usually requires spatial normalization of each individual’s structural and functional images so that anatomical variability across different brains can be minimized. This spatial normalization is achieved by warping individual brain images to match a standard template in stereotaxic space (Friston et al. 1995). However, as the widely-available and commonly-used templates (e.g., ICBM452) are all built from brains of healthy adults, using these templates may introduce systematic bias in the results of group comparison (Bookheimer and Sowell 2005). Such bias is particularly likely in the case of FAS where severely affected individuals typically have smaller brain size than non-exposed controls or those representing the spectrum of alcohol effects (FASD); therefore, a different amount of image deformation and intensity modulation may be introduced into the data of these groups. Although quantitative assessment of the normalization-induced group difference has not yet been reported in studies of prental alcohol exposure, data from pediatric studies (which are complicated by a similar situation of smaller brain size in children) do suggest extra caution in interpreting imaging results with a biased normalization template (Wilke et al. 2002, 2003; Yoon et al. 2009). For future functional and structural studies of FASD, using a customized template with contributions from both the exposed and control sample would be preferable. Alternatively, using local structural measurements (e.g., gray matter volume) as covariates in statistics of group comparison can also provide effective control of this normalization bias (Oakes et al. 2007).
Group difference of cognitive ability level is a specific challenge for all kinds of functional neuroimaging studies of FASD. Due to the neurodevelopmental compromise, exposed and affected individuals often have lower ability levels (IQ) and widespread neuropsychological deficits. Such deficits are required for the diagnosis of FAS or associated disorders, which are a prerequisite to inclusion in most clinical studies. Thus, the individuals being studied tend to show reduced behavioral performances relative to controls in the experimental tasks that are required for functional neuroimaging. This can be the case even when controls are matched for socioeconomic status (SES) and other relevant factors. Different behavioral performance between groups may complicate the interpretation of functional imaging data. Even when there is no clinical condition, activation difference can be observed between groups of healthy subjects who show different behavior performance (Grabner et al. 2007). Thus, in a particular research paradigm, observed brain activation difference could either reflect neuronal alterations associated with alcohol exposure, or reflect results associated with the ability differences between groups. To deal with this issue, some of the cited studies matched behavioral performance between groups (Burden et al. 2009; Fryer et al. 2007; Meintjes et al. 2010; O’Hare et al. 2009) either by using a easy experimental task (so that both group can perform fairly well), or by a post-hoc select-and-match of subjects based on their performance. Obviously, both strategies limit the generalizibility of the results: the former strategy by restricting the kinds of cognitive tasks and the performance range that can be examined and the latter, by excluding the most affected individuals from participation.
An alternative approach to minimizing this effect of ability difference is to parametrically manipulate the task difficulty in the experiment (Amaro and Barker 2006; Kotsoni et al. 2006). With this design, brain activations do not need to be directly compared between groups at any specific level of task difficulty; instead, researchers can examine how brain activation changes with difficulty, and it is this change that will be compared between groups. For example, in a working memory study, the memory load can be parametrically manipulated to require subjects to perform the task at different levels of difficulty. With increasing task difficulty, control subjects may show increasing brain activation in memory-related regions, but individuals with FASDs may exhibit limited increment of this brain activation in the same regions. This approach was used by Sowell et al. (2007) in their study of verbal learning.
Developmental outcomes of prenatal alcohol exposure have not been directly examined by functional neuroimaging. The majority of the studies reviewed were carried out in children of late school age or adolescence. This age group is probably being studied most commonly because of access to samples and because children at that age are more cooperative with experimental protocols. However, development of cognition and behavior proceeds throughout the lifespan and as we know from functional neuroimaging studies of typical individuals and from other clinical groups, there are significant changes throughout the lifespan in brain function. When there are “developmental” delays or deficits, it can be difficult to understand whether these are truly delays and, therefore, eventually resolvable or whether these are deficits and represent permanent alterations in function. Currently, the functional neuroimaging studies of the effects of prenatal alcohol exposure that have been done are limited in number and in terms of the ages of the individuals who have been included in these studies. Thus, interpretation of “developmental” effects of prenatal alcohol exposure on brain function cannot be done as yet.
Sample characteristics and conditions of comorbidity vary between studies. Using samples drawn from populations with different characteristics may produce different results. In this literature, there are two methods commonly used to identify effects of alcohol exposure. The first is to identify women who use alcohol in pregnancy and to examine their offspring, in comparison with a non-exposed group whose mothers did not use alcohol. The second method is to recruit from clinical settings where alcohol-exposed individuals may apply for care and to compare their behavior or other characteristics to that of a contrast group. However, longitudinally followed alcohol-exposed individuals and individuals applying for mental health services usually have different characteristics. Clinical samples, in fact, represent a subset of the exposure population. When samples are recruited from clinical populations, as must often be the case, it is difficult to avoid questions about the effects of social and other factors that have brought them to the attention of clinicians. One paper (Spadoni et al. 2009) in discussing potential study limitation commented on the questions inherent in studying a sample recruited from a clinical population. As these authors noted, “Because of the high incidence of psychiatric co- morbidities in individuals with prenatal alcohol exposure, excluding medicated subjects would limit the generalizability of …results.”(p. 2074) However, it also seems likely that including subjects medicated with stimulants and antipsychotics, two common prescriptions for older children identified with alcohol-related behavioral disorders and FASD (Frankel et al. 2006; O’Malley and Nanson 2002), may also affect outcomes of activation studies. Similarly, when using adolescent and adult populations, controlling for alcohol and other drug use by participants may be important to avoid effects of concurrent exposure.
Discussion
Studies of functional neuroimaging suggest that prenatal alcohol exposure, or a diagnosis of FAS, may lead to a general decrease in neural efficiency or a global decrement in processing resources. Depending on the task requirements, compensation mechanisms may be needed for the exposed individuals to achieve a behavioral performance comparable to their peers. This view is supported by fMRI studies that report comparable behavioral performance (Fryer et al. 2007; Meintjes et al. 2010; O’Hare et al. 2009; Spadoni et al. 2009) and show increased activation in the task-associated brain regions. However, there may be conditions under which such “compensation” cannot occur, when the task is particularly challenging, or when exposure level was higher. Studies reporting impaired behavioral performance (Astley et al. 2009; Malisza et al. 2005; Santhanam et al. 2009) support such an argument as they show decreased activation in the associated brain regions. EEG studies also suggest a dose/response gradient (Burden et al. 2009, 2010, 2011).
Most of the currently available neuroimaging studies have used a “regional” approach to show which part of the brain is activating differently between the groups during task performance. With increasing imaging data available on whole brain that can describe alterations of neural activation, future studies of functional neuroimaging in alcohol-exposed populations will progress by applying knowledge available from previous studies of neuropsychology and functional neuroimaging to the understanding of functional networks. For example, recent fMRI studies have shown that besides functional activations, attention-demanding tasks usually also induce deactivation in several brain regions termed as the “default mode network (DMN)”. This network includes brain regions active when the individual is awake and alert but not focused on external stimuli or tasks. (Raichle and Snyder 2007). Typically comprising the anterior and posterior cingulate as well as bilateral inferior parietal cortices (Fig. 3), the DMN should be considered in future studies of prenatal alcohol exposure due to its significant relevance to attention/arousal regulation (Sonuga-Barke and Castellanos 2007), which are known being impaired in FASD (Mattson et al. 2006). Interactions of the DMN with task-positive brain networks should be of interest to most researchers as in many other psychiatric situations (Buckner et al. 2008) including prenatal cocaine exposure (Li et al. 2010) and attention deficits/hyperactivity disorder (Liddle et al. 2010).
The default mode brain network (the blue regions) shown in lateral (top) and midsagittal (bottom) view. This figure is adapted from (Buckner et al. 2008) with permission
Similarly, it would be valuable to explore brain networks beyond the prefrontal-parietal system that has received the bulk of experimental attention. The published functional neuroimaging studies so far focus on functions that are cognitively demanding (working memory, attention, number processing and inhibitory control), largely involving the prefrontal-parietal executive system (Jones and Smith 1973). However, the completion of a complex cognitive task requires cooperative effort across different neural networks and impaired behavioral outcome may reflect not only functional changes in the executive system but also in neural networks that processing information at relatively early stages (e.g., visual system). Comprehensive understanding of the impact of prenatal exposure needs imaging data from both aspects.
Finally, in examining functional outcomes, connectivity is of prime importance as different brain regions do not work in isolation. With fMRI, neural connections can be examined through two different aspects, functional and effective connectivity. Functional connectivity measures temporal signal correlations between regions and effective connectivity measures causal influence exerted by one region over another. Both approaches have made exceptional contributions to studies in populations with different pathologies (Whittingstall et al. 2003) and it is likely that this approach will be equally fruitful in future studies of effects of alcohol exposure. A recent example of this approach used “resting-state” data and found lower inter-hemispheric functional connectivity between para-central regions in the exposed group (Wozniak et al. 2011). Future studies will benefit from joint use of activation and connectivity approaches to examine the effects of prenatal alcohol exposure on both the nodes and margins of brain networks.
References
Aguirre, G. K., Detre, J. A., & Wang, J. (2005). Perfusion fMRI for functional neuroimaging. International Review of Neurobiology, 66, 213–236.
Amaro, E., & Barker, G. J. (2006). Study design in fMRI: basic principles. Brain and Cognition, 60, 220–232.
Archibald, S. L., Fennema-Notestine, C., Gamst, A., Riley, E. P., Mattson, S. N., & Jernigan, T. L. (2001). Brain dysmorphology in individuals with severe prenatal alcohol exposure. Developmental Medicine and Child Neurology, 43(3), 148–154.
Astley, S. J., Aylward, E. H., Olson, H. C., Kerns, K., Brooks, A., Coggins, T. E., et al. (2009). Functional magnetic resonance imaging outcomes from a comprehensive magnetic resonance study of children with fatal alcohol spectrum disorders. Journal of Neurodevelopmental Disorders, 1(1), 61–80.
Bhatara, V. S., Lovrein, F., Kirkeby, J., Swayze, V., Unruh, E., & Johnson, V. (2002). Brain function in fetal alcohol syndrome assessed by single photon emission computed tomography. South Dakota Journal of Medicine, 55(2), 59–62.
Bookheimer, S. Y., & Sowell, E. R. (2005). Brain imaging in FAS commentary on the article by Malisza et al. Pediatric Research, 58(6), 1148–1149.
Buckner, R. L., Andrews-Hanna, J. R., & Schacter, D. L. (2008). The brain’s default network: anatomy, function, and relevance to disease. Annals of the New York Academy of Science, 1124, 1–38.
Burden, M. J., Andrew, C., Saint-Amour, D., Meintjes, E. M., Molteno, C. D., Hoyme, H. E., et al. (2009). The effects of fetal alcohol syndrome on response execution and inhibition: an event-related potential study. Alcoholism: Clinical and Experimental Research, 33(11), 1994–2004.
Burden, M. J., Jacobson, J. L., Westerlund, A., Lundahl, L. H., Morrison, A., Dodge, N. C., et al. (2010). An event-related potential study of response inhibition in ADHD with and without prenatal alcohol exposure. Alcoholism: Clinical and Experimental Research, 34(4), 617–627.
Burden, M. J., Westerlund, A., Muckle, G., Dodge, N., Dewailly, E., Nelson, C. A., et al. (2011). The effects of maternal binge drinking during pregnancy on neural correlates of response inhibition and memory in childhood. Alcoholism: Clinical and Experimental Research, 35(1), 69–82.
Chen, X., Coles, C. D., Lynch, M. E., & Hu, X. (2011). Understanding specific effects of prenatal alcohol exposure on brain structure in young adults. Human Bran Mapping, In press.
Chernick, V., Childiaeva, R., & Ioffe, S. (1983). Effects of maternal alcohol intake and smoking on neonatal electroencephalogram and anthropometric measurements. American Journal of Obstetrics and Gynecology, 146(1), 41–47.
Church, M. W., & Gerkin, K. P. (1988). Hearing disorders in children with fetal alcohol syndrome: findings from case reports. Pediatrics, 82(2), 147–154.
Clark, C. M., Li, D., Conry, J., Conry, R., & Loock, C. (2000). Structural and functional brain integrity of fetal alcohol syndrome in nonretarded cases. Pediatrics, 105(5), 1096–1099.
Cohen, M. S., & Bookheimer, S. Y. (1994). Localization of brain function using magnetic resonance imaging. Trends in Neurosciences, 17(7), 268–277.
D’Angiulli, A., Grunau, P., Maggi, S., & Herdman, A. (2006). Electroencephalographic correlates of prenatal exposure to alcohol in infants and children: a review of findings and implications for neurocognitive development. Alcohol Research & Health, 40(2), 127–133.
Dehaene, S., Molko, N., Cohen, L., & Wilson, A. J. (2004). Arithmetic and the brain. Current Opinion in Neurobiology, 14, 218–224.
Derauf, C., Kekatpure, M., Neyzi, N., Lester, B., & Kosofsky, B. (2009). Neuroimaging of children following prenatal drug exposure. Seminars in Cell & Developmental Biology, 20, 441–454.
Fabiani, M., Gratton, G., & Coles, M. G. H. (2000). Event-related brain potentials methods, theory, and applications. In J. T. Cacioppo, L. G. Tassinary, & G. G. Berntson (Eds.), Handbook of psychophysiology (pp. 53–84). Cambridge: Cambridge University Press.
Feng, C.-M., Narayana, S., Lancaster, J. L., Jerabek, P. A., Arnow, T. L., Zhu, F., et al. (2004). CBF changes during brain activation: fMRI vs. PET. Neuroimage, 22, 443–446.
Frankel, F., Paley, B., Marquardt, R., & O’Connor, M. (2006). Stimulants, neuroleptics, and children’s friendship training for children with fetal alcohol spectrum disorders. Journal of Child and Adolescent Psychopharmacology, 16(6), 777–789.
Friston, K. J., Ashburner, J., Frith, C. D., Poline, J.-B., Heather, J. D., & Frackowiak, R. S. J. (1995). Spatial registration and normalization of images. Human Brain Mapping, 3(3), 165–189.
Fryer, S. L., Tapert, S. F., Mattson, S. N., Paulus, M. P., Spadoni, A. D., & Riley, E. P. (2007). Prenatal alcohol exposure affects frontal-striatal BOLD response during inhibitory control. Alcoholism: Clinical and Experimental Research, 31(8), 1415–1424.
Grabner, R. H., Ansari, D., Reishofer, G., Stern, E., Ebner, F., & Neuper, C. (2007). Individual differences in mathematical competence predict parietal brain activation during mental calculation. Neuroimage, 38, 346–356.
Havlicek, V., Childiaeva, R., & Chernick, V. (1977). EEG frequency spectrum characteristics of sleep states in infants of alcoholic mothers. Neuropädiatrie, 8(4), 360–373.
Ioffe, S., & Chernick, V. (1990). Prediction of subsequent motor and mental retardation in newborn infants exposed to alcohol in utero by computerized EEG analysis. Neuropediatrics, 21(1), 11–17.
Ioffe, S., Childiaeva, R., & Chernick, V. (1984). Prolonged effects of maternal alcohol ingestion on the neonatal electroencephalogram. Pediatrics, 74(3), 330–335.
Jones, K. L., & Smith, D. W. (1973). Recognition of the fetal alcohol syndrome in early infancy. Lancet, 302(7836), 999–1001.
Kable, J. A., & Coles, C. D. (2004). Teratology of alcohol: Implications for school settings. In R. T. Brown (Ed.), Handbook of pediatric psychology in school settings. Mahwah: Lawrence Erlbaum Associates Publishers.
Kable, J. A., Coles, C. D., Lynch, M. E., & Carroll, J. (2009). The impact of maternal smoking on fast auditory brainstem responses. Neurotoxicology and Teratology, 31(4), 216–224.
Kaneko, W. M., Phillips, E. L., Riley, E. P., & Ehlers, C. L. (1996). EEG findings in fetal alcohol syndrome and Down syndrome children. Electroencephalography and Clinical Neurophysiology, 98, 20–28.
Kotsoni, E., Byrd, D., & Casey, B. J. (2006). Special considerations for functional magnetic resonance imaging of pediatric populations. Journal of Magnetic Resonance Imaging, 23, 877–886.
Li, Z., Coles, C. D., Lynch, M. E., Ma, X., Peltier, S., & Hu, X. (2008). Occipital-temporal reduction and sustained visual attention deficit in prenatal alcohol exposed adults. Brain Imaging and Behavior, 2, 39–48.
Li, Z., Santhanam, P., Coles, C. D., Lynch, M. E., Hamann, S., Peltier, S., et al. (2010). Increased default mode activity in adolescents prenatally exposed to cocaine. Human Bran Mapping, In press, doi:10.1002/hbm.21059.
Liddle, E. B., Hollis, C., Batty, M. J., Groom, M. J., Totman, J. J., Liotti, M., et al. (2010). Task-related default mode network modulation and inhibitory control in ADHD: effects of motivation and methylphenidate. Journal of Child Psychology and Psychiatry, In press, doi:10.1111/j.1469-7610.2010.02333.x.
Logothetis, N. K. (2008). What we can do and what we cannot do with fMRI. Nature, 453, 869–878.
Malisza, K. L., Allman, A.-A., Shiloff, D., Jakobson, L., Longstaffe, S., & Chudley, A. E. (2005). Evaluation of spatial working memory function in children and adults with fetal alcohol spectrum disorders: a functional magnetic resonance imaging study. Pediatric Research, 58, 1150–1157.
Mattson, S. N., Riley, E. P., Jernigan, T. L., Ehlers, C. L., Delis, D. C., Jones, K. L., et al. (1992). Fetal alcohol syndrome: a case report of neuropsychological, MRI and EEG assessment of two children. Alcoholism: Clinical and Experimental Research, 16(5), 1001–1003.
Mattson, S. N., Calarco, K. E., & Lang, A. R. (2006). Focused and shifting attention in children with heavy prenatal alcohol exposure. Neuropsychology, 20(3), 361–369.
Meintjes, E. M., Jacobson, J. L., Molteno, C. D., Gatenby, J. C., Warton, C., Cannistraci, C. J., et al. (2010). An fMRI study of number processing in children with fetal alcohol syndrome. Alcoholism: Clinical and Experimental Research, 34(8), 1450–1464.
Norman, A. L., Crocker, N., Mattson, S. N., & Riley, E. P. (2009). Neuroimaging and fetal alcohol spectrum disorders. Developmental Disabilities Research Reviews, 15(3), 209–217.
Nunez, P. L., & Srinivasan, R. (2006). Electric fields of the brain: The neurophysis of EEG (2nd ed.). New York: Oxford University Press.
Oakes, T. R., Fox, A. S., Johnstone, T., Chung, M. K., Kalin, N., & Davidson, R. J. (2007). Integrating VBM into the general linear model with voxelwise anatomical covariates. Neuroimage, 34, 500–508.
O’Hare, E. D., Lu, L. H., Houston, S. M., Bookheimer, S. Y., Mattson, S. N., O’Connor, M. J., et al. (2009). Altered frontal-parietal functioning during verbal working memory in children and adolescents with heavy prenatal alcohol exposure. Human Brain Mapping, 30, 3200–3208.
Olegård, R., Sabel, K.-G., Aronsson, M., Sandin, B., Johansson, P. R., Carlsson, C., et al. (1979). Effects on the child of alcohol abuse during pregnancy. Retrospective and prospective studies. Acta Paediatrica, 68(Supplement S275), 112–121.
O’Malley, K. D., & Nanson, J. (2002). Clinical implications of a link between fetal alcohol spectrum disorder and attention-deficit hyperactivity disorder. Canadian Journal of Psychiatry, 47(4), 349–354.
Pettigrew, A. G., & Hutchinson, I. (1984). Effects of alcohol on functional development of the auditory pathway in the brainstem of infants and chick embryos. Ciba Foundation Symposium, 105, 26–46.
Raichle, M. E., & Snyder, A. Z. (2007). A default mode of brain function: a brief history of an evolving idea. Neuroimage, 37, 1083–1090.
Riikonen, R., Salonen, I., Partanen, K., & Verho, S. (1999). Brain perfusion SPECT and MRI in foetal alcohol syndrome. Developmental Medicine and Child Neurology, 41, 652–659.
Riikonen, R. S., Nokelainen, P., Valkonen, K., Kolehmainen, A. I., Kumpulainen, K. I., Könönen, M., et al. (2005). Deep serotonergic and dopaminergic structures in fetal alcoholic syndrome: a study with nor-beta-CIT-single-photon emission computed tomography and magnetic resonance imaging volumetry. Biological Psychiatry, 57, 1565–1572.
Rössig, C., Wässer, S., & Oppermann, P. (1994). Audiologic manifestations in fetal alcohol syndrome assessed by brainstem auditory-evoked potentials. Neuropediatrics, 25(5), 245–249.
Santhanam, P., Li, Z., Hu, X., Lynch, M. E., & Coles, C. D. (2009). Effects of prenatal alcohol exposure on brain activation during an arithmetic task: an fMRI study. Alcoholism: Clinical and Experimental Research, 33(11), 1901–1908.
Scher, M. S., Richardson, G. A., Coble, P. A., Day, N. L., & Stoffer, D. S. (1988). The effects of prenatal alcohol and marijuana exposure: disturbances in neonatal sleep cycling and arousal. Pediatric Research, 24(1), 101–105.
Scher, M. S., Richardson, G. A., Robles, N., Geva, D., Goldschmidt, L., Dahl, R. E., et al. (1998). Effects of prenatal substance exposure: altered maturation of visual evoked potentials. Pediatric Neurology, 18(3), 236–243.
Sonuga-Barke, E. J. S., & Castellanos, F. X. (2007). Spontaneous attentional fluctuations in impaired states and pathological conditions: a neurobiological hypothesis. Neuroscience and Biobehavioral Reviews, 31, 977–986.
Sowell, E. R., Lu, L. H., O’Hare, E. D., McCourt, S. T., Mattson, S. N., O’Connor, M. J., et al. (2007). Functional magnetic resonance imaging of verbal learning in children with heavy prenatal alcohol exposure. Neuroreport, 18(7), 635–639.
Spadoni, A. D., McGee, C. L., Fryer, S. L., & Riley, E. P. (2007). Neuroimaging and fetal alcohol spectrum disorders. Neuroscience and Biobehavioral Reviews, 31(2), 239–245.
Spadoni, A. D., Bazinet, A. D., Fryer, S. L., Tapert, S. F., Mattson, S. N., & Riley, E. P. (2009). BOLD response during spatial working memory in youth with heavy prenatal alcohol exposure. Alcoholism: Clinical and Experimental Research, 33(12), 2067–2076.
Spohr, H. L., & Steinhausen, H. C. (1987). Follow-up studies of children with fetal alcohol syndrome. Neuropediatrics, 18(1), 13–17.
Wernick, M. N., & Aarsvold, J. N. (2004). Emission tomography: The fundamentals of PET and SPECT. San Diego: Elsevier Academic Press.
Whittingstall, K., Stroink, G., Gates, L., Connolly, J., & Finley, A. (2003). Effects of dipole position, orientation and noise on the accuracy of EEG source localization. Biomedical Engineering Online, 2, 14.
Wilke, M., Schmithorst, V. J., & Holland, S. K. (2002). Assessment of spatial normalization of whole-brain magnetic resonance images in children. Human Brain Mapping, 17, 48–60.
Wilke, M., Schmithorst, V. J., & Holland, S. K. (2003). Normative pediatric brain data for spatial normalization and segmentation differs from standard adult data. Magnetic Resonance in Medicine, 50, 749–757.
Wozniak, J. R., Mueller, B. A., Muetzel, R. L., Bell, C. J., Hoecker, H. L., Nelson, M. L., et al. (2011). Inter-hemispheric functional connectivity disruption in children with prenatal alcohol exposure. Alcoholism: Clinical and Experimental Research, 35(5), 1–13.
Yoon, U., Fonov, V. S., Perusse, D., & Evans, A. C. (2009). The effect of template choice on morphometric analysis of pediatric brain data. Neuroimage, 45, 769–777.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Coles, C.D., Li, Z. Functional Neuroimaging in the Examination of Effects of Prenatal Alcohol Exposure. Neuropsychol Rev 21, 119–132 (2011). https://doi.org/10.1007/s11065-011-9165-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-011-9165-y