Abstract
Premature birth incidence and survival rates are increasing steadily due to advances in obstetric and neonatal intensive care. Those born at the limits of viability are highly at-risk of adverse neurocognitive function over their lifespan, leading to current controversy regarding aggressive resuscitation efforts for these extremely preterm children. However, data from earlier generation cohorts who were born in substantially different eras of neonatal intensive care cannot be relied on to predict outcome of today’s newborn. Our review by the crucial variable of birth cohort year shows a changing developmental trajectory in which today’s extremely preterm survivor is likely to have fewer severe medical complications, better neurological outcomes, and fewer adverse cognitive late effects. Such data further underscore the importance of concurrently considering medical, familial, socioenvironmental, and neurobiological factors in combination with individual neonatal intensive care center protocols when studying outcomes of the preterm child. This complex, interrelated range of factors directly affects the immature, rapidly developing premature brain. However, ongoing surveillance to detect subsequent delay or impairment and to apply interventional strategies early in the developmental course holds promise for further enhancement of functional outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Steadily rising premature birth rates signify an escalating pediatric public health problem (Ashton et al. 2009). Survivors of early birth incur immediate medical morbidities as well as long-term neuromotor, neurocognitive, and behavioral impairments (Tyson and Saigal 2005). Adverse effects have been found across the preterm spectrum, from extremely preterm (<28 weeks gestation) to late-preterm (34–36 weeks) birth (Engle et al. 2007). Although moderate to severe impairments are well-documented following extremely preterm birth (Aarnoudse-Moens et al. 2009), even late-preterm birth may result in subtle and specific neurocognitive deficits (Baron et al. 2009b). Neonates born weighing <750 g or at <26 weeks, i.e., micropremature (MacDonald 2002), represent a rapidly increasing extremely preterm subpopulation at risk of high mortality and morbidity rates, and lifespan impairments (American College of Obstetricians and Gynecologists 2002). Therefore, aggressive delivery resuscitation efforts have not been universally endorsed for these earliest born neonates, although consensus has been reached to support intensive care for those born ≥26 weeks (Vavasseur et al. 2007).
Cohort birth year is a crucial variable to be considered when evaluating the literature since substantially different intensive care medical management was applied across different neonatal care eras. The course and subsequent outcome of extremely preterm neonates born since 2000 appears to be changing relative to earlier generation cohorts. Although data continue to be published regarding cohorts born and cared for in earlier decades, these data do not usefully guide resuscitation and treatment recommendations for today’s neonate, or aid counseling of today’s new parents regarding their child’s future. Reports of fewer severe medical complications, better neurological outcomes, and less adverse cognitive late effects suggest a more optimistic prognosis is warranted for the neonate born today (Fawke 2007; Lorenz et al. 1998; Stjernqvist and Svenningsen 1993). Outcomes for the extremely preterm population, and whether they are changing, may be best appreciated by a review of studies published over the decades since inception of neonatal intensive care in the 1970s. Thus, the goals of this review are to: 1) provide a brief clinical context for discussion of extremely preterm birth, including basic terminology, incidence rates, and risk factors; 2) review effects of extreme prematurity on the immature but rapidly developing brain; 3) summarize reports of cognitive and neuropsychological outcome following extremely preterm birth by cohort birth year, extracting data on those born <26 weeks whenever possible; and, 4) describe intervention strategies that have begun to be applied to this at-risk population, concluding with suggestions for future directions. MEDLINE and PubMed were used to search the English literature for studies published since 1970 reporting on both mortality and disability in extremely preterm infants, i.e., those born <28 weeks gestational age or with a birth weight <1,000 g. Reference lists from literature retrieved were used to identify additional articles.
Preterm Birth Terminology, Incidence, and Risk Factors
Terminology
After a long history of inconsistent prematurity definitions (Lorenz et al. 1998), standard birth weight and gestational age designations now ensure classification uniformity (Engle 2004). Table 1 lists terms and definitions in standard usage. Although some report birth weight to be a reliable predictor of neonatal course and outcome (Cole et al. 2002), and others gestational age (Cooke 2005; Foster-Cohen et al. 2007; Saigal and Doyle 2008), neither birth weight or gestational age alone has been a sufficient predictor of outcome (Tyson et al. 2008). A complex array of medical and non-medical risk factors contributes to eventual function. Multifactorial methods may best aid identification of the most predictive factors, and more sophisticated decision parameters are needed (Tyson et al. 2008). Nevertheless, a clear inverse relationship exists between birth weight or gestational age and impairment, with greater disability incidence found with lower birth weight or earlier gestational age (Bhutta et al. 2002). Each additional week of gestational age or gram birth weight decreases the likelihood of impairment (Synnes et al. 1994) and improves functional outcome (MacDonald 2002), including of cognition (Fily et al. 2006; Piecuch et al. 1997).
The neonate’s size according to standardized age and growth curves is referred to as “appropriate for gestational age” (25–75th percentile) or “small for gestational age” (<10th percentile). The latter term has been used interchangeably with intrauterine growth delay and intrauterine growth retardation or restriction (Kok et al. 1998).
To account for ex-utero neurodevelopmental immaturity, preterm infants are routinely accorded a “corrected age”, i.e., chronological age minus the number of weeks born before full-term (40 weeks) (Engle 2004). In clinical practice, age correction has generally been made only until around 24 to 30 chronological months based on older data. However, survival at current lower viability limits is associated with more immature brain development than for survivable birth in past decades. Therefore, researchers tend to endorse use of age correction further along the developmental spectrum (Anderson and Doyle 2003; Raz et al. 2009). Empirical evidence remains lacking for when age correction is no longer necessary.
Preterm Birth Incidence
There has been a 21% increase in rates of low birth weight incidence since 1980, and of birth <37 weeks since 1990 (Hamilton et al. 2006; Martin et al. 2008). Until the latest (2008) report indicating a 12.3% incidence of preterm birth, rates had risen to 12.8% in the United States. Of the most recent statistics for U.S. livebirths, 8.3% were at low BW, approximately 1% at <1,000 g, 0.3–0.4% at <750 g, and .002% at 24–25 weeks (Hamilton et al. 2009; Martin et al. 2005; Martin et al. 2008; Ment et al. 2006; Vavasseur et al. 2007). Ethnicity/racial group differences include that births <33 weeks and <1,500 g for African/African-American women are double those of other groups (Behrman and Butler 2007).
Medical Risk Factors
Although pregnancy complications may emerge early in gestation, preterm birth is often the unexpected consequence of sudden maternal or fetal distress. Modern obstetric practices and in-hospital prenatal care for at-risk pregnancies have improved newborn overall health and survival (Skrablin et al. 2002), but not all at-risk pregnant women have access to those factors that significantly reduce complications, such as prenatal care, antenatal corticosteroids, or hospitalization in a tertiary care facility with in-house neonatal specialists (O’Shea 2008). The combination of antenatal and postnatal factors that contributes most to optimal outcome remains to be determined.
Severity rates have lessened for several common adverse effects related to extremely preterm birth. A significant turning point was the introduction of surfactant in the mid-1980s, which improved neonatal lung function, decreased the incidence of disabling conditions, and greatly enhanced survival rates of those born ≤26 weeks (Ferrara et al. 1994; The Victorian Infant Collaborative Study Group 1997). Antenatal corticosteroids, prophylactic infection control, and better modes of ventilation were also introduced. Additionally, nutritional supplements while in intensive care have had a significant effect on early neurodevelopment and growth (Ehrenkranz et al. 2006). Medical care in the first hours of life appears especially critical, and attempts to develop indices that are predictive continue. For example, standardized illness severity scores assessing physiologic instability in the first 12 postnatal hours provided risk information regarding brain damage and neurodevelopmental dysfunction (Dammann et al. 2009). Length of hospital stay is another indicator of neonatal course severity, related to such common perinatal risk factors as bronchopulmonary dysplasia, sepsis, necrotizing enterocolitis, patent ductus arteriosus, retinopathy of prematurity, and neurological complications. As a consequence of many treatment and procedural advances, rates of cerebral palsy, hydrocephalus, deafness, blindness, seizures, and mental retardation have declined, but adverse late effects still occur at unacceptably high rates in those currently born (Lorenz et al. 1998). Along with these advances, assessment of brain lesion presence and severity has been enabled by routine imaging surveillance with head ultrasonography and increasingly sophisticated neuroimaging techniques (Flodmark and Barkovich 2002; Papile et al. 1978; Volpe 2008). Magnetic resonance imaging at term equivalent, though insensitive to subtle microstructure abnormalities, was found to predict neurodevelopmental outcome (Woodward et al. 2006). Even preterm children at low risk for neurodevelopmental deficits (born at 30–34 weeks gestation) had decreased regional cortical gray matter unilaterally at age 9 in the parietal lobe and bilaterally in the temporal lobe (especially of the middle temporal gyrus), which correlated strongly with intelligence score and smaller white matter volumes (Soria-Pastor et al. 2009)
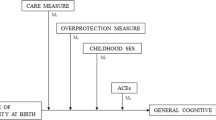
Familial, Socioenvironmental, and Neurobiological Risk Factors
Familial factors such as parental literacy, educational achievement, occupation, socioeconomic status, maternal substance use, ethnicity/culture, family adversity, and parental/caregiver attitudes influence preterm birth outcomes (Collaborative Group on Antenatal Steroid Therapy 1984; Fily et al. 2006; Landry et al. 2006; Laptook et al. 2005; Stjernqvist 1992; Vohr et al. 2003a; Washington and Craig 1992). Maternal education is an especially strong predictor (Breslau et al. 2004; Kesler et al. 2004). Relatedly, a relatively homogenous population of 1996–1997 extremely low birth weight (ELBW; <1,000 g) infants that benefited from maternal prenatal health care in Finland had 11% intraventricular hemorrhage incidence (Mikkola et al. 2005), contrasting with 32% intraventricular hemorrhage incidence for a heterogeneous United States population born <25 weeks and <751 g between 1993 and 1999, that included those disadvantaged by low maternal education, poor prenatal care, and low socioeconomic status (Shankaran et al. 2004). While it remains unclear which combination of factors will best predict good cognitive outcome (McCormick et al. 2006; Msall 2005), later learning difficulties were found to be predicted better by socioenvironmental than perinatal medical risk factors (Aylward et al. 1989; Teplin et al. 1991), cognitive development was better predicted by early environmental factors than genetic factors (Koeppen-Schomerus et al. 2000), and higher socioeconomic status was advantageous (Kilbride et al. 2004).
Negative socioenvironmental risk factors include multiple gestation, which also lowers survival odds, and adverse social conditions (Kesler et al. 2008; Castro et al. 2004; Marlow et al. 2005). The latter has been associated with poorer behavioral, attentional, and adaptive functioning (Chapieski and Evankovich 1997), and effects may be identified early (Delobel-Ayoub et al. 2006).
Male gender is a significant risk factor for brain maturational and neurobehavioral dysfunction (Brothwood et al. 1986; Fily et al. 2006; Hille et al. 1994; Kesler et al. 2008; Tyson et al. 2008; Vohr et al. 2003b). Imaging studies support these findings. Preterm children had smaller gray and white matter cerebral volumes than all controls, and white matter volumes were not significantly different between preterm and term females. However, preterm males were especially vulnerable to adverse effects on white matter development compared with term males (Reiss et al. 2004), and preterm males had greater hippocampal volume reduction than controls (Lodygensky et al. 2005). Furthermore, higher female than male representation in a majority of clinical studies likely reflects higher female survival rates or less attrition in female cohorts.
Neonatal Intensive Care Unit Factors
Neonatal intensive care unit factors have been understudied but account for significant variance across preterm studies (Vohr et al. 2004). Disparities in neonatal intensive care unit complication rates, survival rates, and long-term outcome are affected by preferred delivery method, inborn-outborn proportion (outborns disadvantaged by transport time), care level (tertiary or less specialized), preterm patient volume, and neonatal specialist staffing patterns (Bartels et al. 2005; Doyle 2004; Hakansson et al. 2004; Hoekstra et al. 2004; International Neonatal Network 2000; Tommiska et al. 2007). Medical complication rates vary greatly across neonatal intensive care units, including for crucial complications of intraventricular hemorrhage, periventricular leukomalacia, chronic lung disease, and retinopathy of prematurity (Daniel et al. 2003; McCormick 1994; Msall et al. 2004). Improvements to the neonatal intensive care environment that have had a positive effect on acute care and eventual outcome continue to be introduced, such as waterbeds, dimmed light, reduced sound levels, and private rooms (Gross et al. 2005; Jobe 2004; Maayan-Metzger et al. 2002), but are not uniformly similar across neonatal intensive care units. Furthermore, while parent satisfaction about the child’s adaptive and behavioral function is measurable (Hille et al. 2001; Szatmari et al. 1990), physician attitude is not easily quantified despite its importance in determining the care provided to borderline viable infants (see Hakansson et al. 2004 for North and South Sweden care practices and outcome differences). Overall, an institution’s outcome statistics require cautious interpretation based on care practices. For example, survival rates and outcomes of a neonatal intensive care unit that aggressively resuscitates a high volume of medically severe neonates is not easily compared with those of a neonatal intensive care unit that provides less aggressive care for infants born <26 weeks or <750 g, whose survival rates and outcomes may be inflated because their survivors were born at later gestational age or with heavier birth weight.
Unintended negative consequences may result when neurodevelopmental risk is weighed against medical gain (O’Shea et al. 2007). For example, systemic corticosteroid use introduced to reduce prematurity associated complications remains controversial. In an animal study, cholinergic neurons were more vulnerable to later learning challenges after prenatal dexamethasone treatment (Emgard et al. 2006), and in human studies, postnatal corticosteroid use was associated with poor early growth and negative cognitive effects (Wood et al. 2003). Studies caution about potential negative psychological effects detectable by the preschool years (Barrington 2001; Short et al. 2003; Yeh et al. 2004), although not all agree (Gross et al. 2005; Lodygensky et al. 2005; Meyer-Bahlburg et al. 2004; Trautman et al. 1995; Wilson et al. 2006). Conclusions based on preschool performance parameters need further longitudinal studies that extend outcome measurement further along the maturational course, consider the broad range of risk factors inherent to this population, and examine rate of maturational development to resolve these concerns.
In summary, the range and complexity of risk factors affecting neuropsychological outcome in extremely preterm children confounds attempts to interpret this large literature consisting of diverse cohort demographic and medical characteristics. In addition to medical, developmental, and psychosocial variables, differences in neonatal intensive care unit practices and environment appear to have a substantial impact on later outcome.
Effects of Prematurity on the Developmentally Immature Central Nervous System
Neurological status and stage along the brain developmental continuum are important risk factors (Jenkins et al. 2009). A full-term infant brain is very different from the maturation-dependent preterm brain whose growth has been interrupted at a critical neurodevelopmental stage. There are both general and specific consequences of the impact of preterm birth on brain development that may affect psychological function over the lifespan. Multiple immature body systems are present in a preterm child, but central nervous system (CNS) in-utero and ex-utero effects are especially predictive of later neurocognitive impairment (Patra et al. 2006; Piecuch et al. 1997; Selzer et al. 1992).
In-utero Effects
Prevalent in-utero cortical and neuronal effects include disproportionately enlarged frontal and parietal gray matter volumes, and smaller temporal and subcortical region volumes (Kesler et al. 2004; Kesler et al. 2006) related to enhanced apoptosis or excitotoxic damage of susceptible immature neurons (Bhutta and Anand 2001; Edgin et al. 2008). A higher likelihood of brain and lateral ventricular volume alterations has been associated with supratentorial lesions, including of sensorimotor and parieto-occipital regions (Peterson et al. 2003). Abnormalities also involve the hippocampus (Gimenez et al. 2004; Gimenez et al. 2008; Isaacs et al. 2000; Thompson et al. 2008), and cerebellum, including hemorrhagic cerebellar injury (Limperopoulos et al. 2005) and abnormal cerebellar growth (Allin et al. 2001). Immature cerebrovascular systems compromise cerebral blood flow autoregulation, supply, and perfusion, including to cerebral white matter (Volpe 2008). This leaves the developing brain vulnerable to hypoxic ischemic injury and white matter progenitor cell damage, as well as gray matter maldevelopment (Allin et al. 2004; Back et al. 2007; Khwaja and Volpe 2008). Hypoxic ischemic injury involves metabolic cascades in response to ischemia and reperfusion, contributing to oligodendrocyte progenitor cell (myelin precursor) damage due to these cells’ heightened vulnerability to oxidative stress early in development (Ferriero 2004; Volpe 2008). Additionally, immature astrocytes appear vulnerable to injury at early stages in development, which further compromises white matter development related to hypoxic ischemia (Sen and Levison 2006). Disturbances of axonal maturation and cell-to-cell interaction secondary to diffuse periventricular white matter damage (Barrett et al. 2007; Volpe 2005) have the additional effect of resulting in smaller thalamic and lentiform nucleus volumes (Gimenez et al. 2006; Srinivasan et al. 2007). The consequences of diffuse white matter degradation also involve cortical, basal ganglia, and cerebellar abnormalities (Counsell et al. 2003; Kesler et al. 2006). Notably, white matter injury appears to be the most common brain abnormality in preterm infants, and a major predictor of smaller volumes along with gestational age (Martinussen et al. 2009).
Another in-utero complication that may lead to preterm birth is intrauterine infection. e.g., chorioamnionitis or maternal infection. Cytokines and their receptors, found in central nervous system cells, are important for brain development and function. They influence inflammatory response as well as neuron and glial cell development. Elevated levels of proinflammatory cytokines in amniotic fluid, cord blood, or neonatal blood indicate the presence of a systemic fetal inflammatory response. A persistent neuroinflammatory response may result when the inflammation signal is transmitted across the blood-brain barrier (Malaeb and Dammann 2009). This has been associated with intraventricular hemorrhage, white matter damage, and cerebral palsy (Tauscher et al. 2003; Yoon et al. 1997). When associated with hypoxic events, cytokines negatively affect functional outcome such as of early psychomotor development (Hansen-Pupp et al. 2008). High concentrations of such specific cytokines as interleukin-1-beta, interleukin-6, and interleukin-8 have been associated with abnormal neurodevelopment at 6 months, 12-months, and 30 months of age (Bartha et al. 2004; Okazaki et al. 2006; Rezaie and Dean 2002).
Brain development proceeds according to a complex plan that unfolds in response to intrinsic and extrinsic factors, and the timing of events is critical (Stiles 2008). The second half of gestation is an active period of cell migration, neuronal differentiation, synapse formation, and glial cell proliferation (de Graaf-Peters and Hadders-Algra 2006). Oligodendrocyte progenitor cells in the periventricular white matter and microglia are in activated stages of development during this period and are more vulnerable to injury (Volpe 2008). Similarly, neurotransmitters and neuromodulatory substances affect development in different ways at different stages in brain development; gamma-aminobutyric acid, an inhibitory neurotransmitter, has an excitatory role until the last trimester and glutamate receptors are over-expressed in regions of the developing brain susceptible to injury. Consequently, mechanisms and effects of neurological insults differ between preterm and term infants (Back 2006; Dyet et al. 2006; Ferriero 2004; McQuillen and Ferriero 2004; Okereafor et al. 2008). For example, while severe hypoxic ischemia preferentially damages deep gray matter in preterm and term neonates, perirolandic involvement is more frequent in term neonates. Less profound insult tends to result in intraventricular hemorrhage and periventricular white matter injury in preterm neonates while term neonates have a greater likelihood of parasagittal watershed territory infarcts (Huang and Castillo 2008).
Ex-utero Effects
Preterm birth perturbs the trajectory of cerebral development into adolescence, with preterm children showing both less gray matter reduction and less white matter gain over time compared with term controls, and relative sparing of the perirolandic cortex and structures supplied by the posterior circulation (Ment et al. 2009). Abnormalities in perirolandic gyri magnetic resonance signal intensity may indicate degree of myelination and development of nerve cells, and be a marker of degree of brain maturation (Korogi et al. 1996). Although conventional imaging findings may be subtle or absent in the acute stage in neonates (Huang and Castillo 2008), the effects of severe hypoxic ischemia are apparent in deep gray matter nuclei, cortices, hippocampi, and cerebellum when these infants reach later childhood and adulthood. Ex-utero neonatal neurological complications include hypoxic ischemic encephalopathy, intraventricular hemorrhage, periventricular leukomalacia, periventricular hemorrhagic infarction, ventriculomegaly, and white matter dysgenesis (Papile et al. 1978; Volpe 2008); their prevalence inversely related to gestational age (Hamrick et al. 2004). Of these, severe intraventricular hemorrhage and periventricular leukomalacia have been strongly associated with neurodevelopmental impairment (Laptook et al. 2005; Sherlock et al. 2005). Severe intraventricular hemorrhage occurs in approximately 25% of very low birth weight infants (Inder and Volpe 2000), and 0.3–0.4% of those born with extremely low birth weight (Hack et al. 2000a; Martin et al. 2005), and leads to smaller subcortical gray matter volumes (Kesler et al. 2004). Periventricular leukomalacia occurs in 5–15% of very low birth weight infants. When severe, periventricular cystic lesions develop, often in occipital and frontoparietal white matter (Flodmark and Barkovich 2002). Although the incidence of severe insult has declined consequent to the many medical advances, poor outcomes still may result after lower grade insults (Patra et al. 2006). Intraventricular hemorrhage and periventricular leukomalacia have been good predictors of cerebral palsy, other neurological complications, and neurobehavioral dysfunction (Dammann and Leviton 2006; Inder and Volpe 2000; Stjernqvist and Svenningsen 1990). For example, an increased incidence of cerebral palsy, hearing impairment, maladaptive daily living skills, and cognitive deficit for 600–1,250 g survivors with intraventricular hemorrhage at age 8 years contrasted with intact neurological, intellectual, and educational outcomes in 92–94% of those who had no intraventricular hemorrhage (Vohr et al. 2003b).
Such extensive cortical and subcortical regional dysmorphologies and volumetric changes negatively affect neurocognition long-term (Martinussen et al. 2009; Nosarti et al. 2002; Peterson et al. 2000). This is exemplified by report of executive, visuospatial, and language dysfunction in adolescents with smaller lateral cerebellar and white matter volumes (Allin et al. 2005), and language dysfunction in association with posterior corpus callosum thinning (Nosarti et al. 2004). Furthermore, areas of smaller white and gray matter volume mediated these cognitive impairments (Nosarti et al. 2008). The finding of white matter loss in the centrum semiovale and posterior periventricular regions in preterm adolescents is intriguing as a potential explanation for the frequently observed effects on processing speed and nonverbal/spatial function (Soria-Pastor et al. 2008). Additionally, preterm adolescents with low birth weight had both smaller total brain size and smaller specific brain volumes, particularly of the thalamus and cerebellar white matter (Martinussen et al. 2009). More optimal neurodevelopmental and neuropsychological outcomes have been reported in recent cohorts when neonatal neurological complications were mild or absent (Ahronovich et al. 2007; Baron et al. 2009a; Edgin et al. 2008; Wilson-Costello et al. 2007).
Neurocognitive Outcome by Birth Year
The profound cognitive morbidities of extremely preterm and micropremature birth have been documented across international studies (Hack and Fanaroff 1999; Marlow et al. 2005; Shankaran et al. 2004; Vanhaesebrouck et al. 2004; Wood et al. 2000). Yet, prediction of clinical course on an individual basis has been limited. Reports of unexpected intact outcome in individual children born <500 g (Coccia et al. 1992; Gidley Larson et al. 2010), as well as well-documented highly variable neurocognitive competence across cohorts with similar medical characteristics, underscore how difficult it is to predict outcome reliably. Cohort studies have been relied on but cross-center methodological and demographic differences make it difficult to generalize findings. Moreover, cohort selection bias effects may overestimate adverse cognitive outcomes, as data may be obtained principally for children whose parents have concerns about their child’s development and are thus more likely to continue to participate in follow-up care and assessments (Castro et al. 2004).
Studies that reported cognitive outcomes of extremely preterm children are listed in Table 2, along with summary findings. Table 2 presents a summary of data extracted from studies of extremely preterm cohorts born from 1977 to 2005. Studies are listed chronologically by cohort birth year, with number of subjects, country, age at testing, and inclusion birth weight or gestational age indicated. Studies employed various cognitive metrics to evaluate cognitive function; these findings are summarized under “Cognitive Outcome”, followed by some additional reported outcomes. Individual studies provide more detailed information regarding outcomes. Outcomes by decade are summarized below for the broad patterns that were found.
Pre-1980 Births: The Pre-surfactant Era
Preterm birth before 1980 occurred in an era of exceptionally high mortality rates. It was not until 1986 that pulmonary surfactant was introduced, a substance that improves neonatal lung function, reduces the incidence of severely disabling conditions, and improves survival (Halliday 2008), especially for those born at 23–27 weeks (Ferrara et al. 1994; The Victorian Infant Collaborative Study Group 1997). Aggressive resuscitation efforts were not yet endorsed. Marginally viable birth weight in these early years was defined as around 1,500 g, quite a different cut-point than current viability boundaries of 400 g and 23 weeks. Neuropsychological evaluation was not conducted routinely. Instead, subjective clinical impressions, broad measures of neuromotor efficiency, and standardized infant neurodevelopmental tests, or general intelligence tests at school age, were the principal functional outcome measures in studies of survival, medical complication incidence rates, and functional outcomes.
Before 1980, surviving extremely preterm infants often had severe medical and psychological complications (Hack and Fanaroff 1989; Roth et al. 1993; Saigal et al. 2006; Vohr and Garcia Coll 1985). For example, 28% of those surviving birth <1,000 g in 1960–1972 had major neurological or sensory deficit, 72% fell below grade level at age 10, and 64% required special education (Nickel et al. 1982). High rates of microcephaly, ophthalmological problems, growth retardation, cerebral palsy, and neurosensory impairment were reported in the few (19%) who survived birth <1,000 g in 1976–1979; of these, 27% subsequently had IQ <85 and 64% had academic problems (Lefebvre et al. 1988). Poor neurocognitive and behavioral outcomes extended to adolescence in those born <750 g in 1977–1982 (Saigal et al. 2000), and in those born <1,000 g and <33 weeks in 1979–1980 (Stewart et al. 1999). Good outcomes were rarely reported. However, an outlier Australian study found adolescents born <32 weeks in 1970–1980 performed within normal limits on tests of attention, memory, perception, visuomotor skill, or executive function, suggesting only minor neuropsychological consequences of very preterm brain damage were present in this cohort (Rushe et al. 2001).
1980–1989 Births: Transition to Surfactant Treatment
Birth in the 1980s was a time of transition from the “pre-surfactant era” of high mortality and disability incidence (Lumley et al. 1988), to the “surfactant era” of rising survival rates. Mortality and severe neurodevelopmental disability data from 42 mostly pre-surfactant studies of birth ≤26 weeks or with birth weight ≤800 g published between 1969–1997 were reviewed. Mental retardation was reported in about 14% of survivors, 22–24% had major disability, and disability prevalence reached 52% (Lorenz et al. 1998). Since aggressive resuscitation efforts for the smallest and earliest born were often not endorsed, extremely preterm survival was less assured. Consequently, mean birth weight and gestational age were greater in these reports than in cohorts born in subsequent decades (Hansen and Greisen 2004; Teplin et al. 1991). Substantial negative effects persisted in these years. Of those born <1,000 g in 1983, only 13.5%, and 3.5% of those born at 25–26 weeks, survived to 19 years in one cohort; of these, 36–39% experienced moderate to severe impairment (Hille et al. 2007). For birth in 1983–1989, survival and morbidity rates improved for each successive birth week from 23 to 25 weeks; survival rate increased from 16% to 53%, morbidity decreased from 67% to 32%, and mental developmental index scores <−2SD at 18-months corrected age decreased from 10% to 1%. A single major impairment was present in 36%, and multiple deficits in 38% (Synnes et al. 1994).
Intellectual Outcome
The intelligence quotient (IQ), a principal psychological outcome index in the 1980s, was often reported to be below average in extremely preterm children. A meta-analysis of reports for 1980–2001 births after age 5 found mean cognitive performance directly proportional to birth weight and gestational age (Bhutta et al. 2002); only five case-control studies had reported cognitive and behavioral data for births <1,001 g, and all five were pre-1987 (pre-surfactant) cohorts (Hall et al. 1995; Portnoy et al. 1988; Saigal et al. 2000; Taylor et al. 2000; Teplin et al. 1991). At one center, mean IQ <85 was reported for 39% of those born <1,500 g in 1982–1986 and pre-surfactant, and 50% of those born <750 g (Hack et al. 1994; Taylor et al. 2000; Taylor et al. 2004); at 11 years of age, those born <750 g had persistent low average-to-average IQ, and mean scores below 750–1,499 g preterm children (Taylor et al. 2000).
Educational Outcome
Greater attention was directed toward assessing educational impairments in extremely preterm children during this decade. Swedish extremely preterm children born in 1985–1986 who had average IQ at 10 years also had learning disabilities, behavioral problems, and attentional disorder (Stjernqvist and Svenningsen 1999). In 1984, children born <1,000 g had a mean IQ of 90.4 compared with 102.5 for controls; 15% had cognitive deficits or met criteria for learning disability, and 52% received support services compared with only 16% of controls (Hall et al. 1995). One fourth of a 1985–1990 cohort (26%) was disabled at 8 years (10% severe), 27% were below grade level in reading or mathematics, and 43% required special education services. Only 30% were at grade level without academic support. Of the 74% children who had IQ ≥ 85 and no neurosensory deficit, i.e., “non-disabled”, 48% functioned below grade level and 25% received academic support (Bowen et al. 2002). Of those born ≤800 g in 1982–1987 and who were neurologically normal with average intelligence (VIQ or PIQ ≥ 85), 65% met LD criteria at 8–9 years compared with 13% of controls (Grunau et al. 2002). Thus, deficits were commonly found, even in association with average IQ.
Mid-1980s Trends
An early trend toward improved outcome emerged in the mid-1980s. An Australian study reported fewer severely disabled children at 5 years in those born in 1985–1987 compared with their 1977–1982 cohort (Doyle et al. 1994). Notably, it was suggested that the emergence of a positive impact of nationalized health care patterns as well as medical advances, such as surfactant, had a positive impact on extremely preterm outcomes. Several reports emerged from countries that provided comprehensive prenatal and postnatal care, and socioenvironmental supports such as teacher consistency and parental counseling. Nevertheless, their extremely preterm children were not insulated from deficit. For example, 50% of Swedish extremely preterm children born <29 weeks in 1985–1986 survived to 10 years, 92% without major neurological disability. However, their mean IQ and visuomotor scores, which were within the normal range, fell significantly below controls; 38% were below grade level, 32% had behavioral problems, and 20% were diagnosed with attention-deficit/ hyperactivity disorder. Of a subgroup born 500–900 g at 24–30 weeks, 80% had normal growth and development at 1 year but 17% had neurological abnormalities, 8.7% had post-hemorrhagic shunted hydrocephalus, and 13% had vision deficits (Stjernqvist and Svenningsen 1999).
1990–1999 Birth: Rising Survival Rates Post-surfactant
Survival rates increased for children born at the limits of viability following the introduction of surfactant, and as other medical advances became available. For example, survival rates rose from 2% to 35% for those born at 23 weeks, 17% to 58% for those born at 24 weeks, and from 35% to 85% for those born at 25 weeks (Hack and Fanaroff 1999). A survival rate of 73% was reported for those born at 26 weeks at another center (Tommiska et al. 2007). Yet, extremely preterm birth after 1990 did not confer substantial advantage over birth in the 1980s with respect to overall functional outcomes. High rates of neuromotor, neurological, neuropsychological, and behavioral impairments continued to be reported well into the 1990s (Anderson and Doyle 2003; Daniel et al. 2003; Delobel-Ayoub et al. 2006; Hack et al. 2000b; Taylor et al. 2006; Vohr et al. 2000), especially for children born <750 g or <26 weeks (De Groote et al. 2007; Mikkola et al. 2005; Rijken et al. 2003). As lower gestational age survival rates increased, a negative impact on morbidity was observed. In a 1982–1988 pre-surfactant cohort, only 23% survived birth <750 g compared with 43% of this center’s 1990–1992 cohort, but 20% of each cohort had a mental developmental index <70 at 20 months (Hack et al. 1996).
Disability and Educational Outcomes
A review of four international cohorts born in this decade found more than 50% of preterm survivors required special education or repeated a grade by age 8 to 11, and only 44–62% had IQ >84 (Saigal et al. 2003). A 38% disability rate in 1984–1989 survivors increased to 68% in 1990–1994 survivors, attributed to increased survival of those especially fragile children born at 23–24 weeks (Emsley et al. 1998). Report of health and educational needs of a 1992–1995 cohort at age 8 compared with controls noted elevated rates of cerebral palsy (14%), vision impairment (10%), and motor impairments (47%), and low IQ (i.e., <85; 38% v. 14% controls), academic limitations (37% vs. 15% controls), and poor adaptive function (69% vs. 34% controls) (Hack et al. 2005). Notably, this study’s control group’s higher than expected impairment rates highlighted the variability inherent in many control populations, and reinforces cautions to consider methodology and cohort characteristics stringently.
A Focus on Longitudinal Study
In the 1990s, attempts were made to determine longitudinal course and outcomes in later childhood. Neurofunctional assessment at 12 months of extremely low birth weight infants born in 1996–2001, along with magnetic resonance imaging status and chronic lung disease, predicted cognitive function at 36 months (Gianni et al. 2007). Children born <26 weeks in 1995 had a mean mental developmental index of 84 and a psychomotor developmental index of 87 at 30 months; 49% had cognitive or neurologic disability and 23% were severely disabled (Wood et al. 2000). At 6 years of age, 80% of this cohort was disabled (34% mildly, 24% moderately, and 22% severely). A 21% cognitive impairment rate increased to 41% when classmates, not normative data, were the comparison group. It was concluded that severe disability at 30-months strongly predicted developmental problems at 6 years, with 86% remaining moderately to severely impaired (Marlow et al. 2005).
Less dire outcomes characterized some birth cohorts in this decade. When 1990s extremely low birth weight survivors in Denmark were compared with 1980s very low birth weight survivors at 4–5 years, it was found that greater survival of the smallest in the 1980s and 1990s occurred without increased intellectual deficit, even though the 1990s cohort had lower mean birth weight (Hansen and Greisen 2004). Also, children born at 23–25 weeks in Sweden between 1990 and 1992 who had been evaluated at 36 months corrected age were studied again between 10 and 12 years and compared with controls on behavioral, emotion, social competency, and adaptive function measures. Parents and teachers reported more internalizing behavioral problems (anxiety/depression, withdrawn, and somatic) along with attention, thinking, and social problems. Child self-reports showed a trend toward increased depression symptoms. Teachers rated extremely preterm children less well adjusted than controls. However, a majority, 85%, were mainstreamed without adjustment problems (Farooqi et al. 2007).
Neuropsychological Measures Introduced
Studies of children born in the 1990s began to extend measurement beyond broad neurodevelopmental or general intellectual instruments to include neuropsychological tests. An early 1990s cohort demonstrated poorer performance compared with controls on all neuropsychological measures at 12 years, and severe brain injury and unfavorable social factors were the most important predictors of adverse cognitive outcomes (Luu et al. 2009). In a 1996–1997 extremely low birth weight cohort from Finland, 26% were normally developing at 5 years but 9% were impaired in all five assessed neuropsychological domains; 20% had major disabilities, 19% had minor disabilities, and 61% had no functional developmental abnormalities although subtle abnormalities were suggested. The overall extremely low birth weight group mean IQ was 96 ± 19 and cerebral palsy rate was 14% whereas in the 22–26 weeks subgroup mean IQ was 94 ± 19 and cerebral palsy rate was 19% (Mikkola et al. 2005).
Executive function and attention, broad capacities subsuming more specific subcomponents essential for overall cognitive development and adaptive efficiency, came under increased scrutiny post-1990 (Carmody et al. 2006). Preterm associated white matter pathology, prefrontal cortical dysfunction, and fronto-subcortical neural network disruption presumptively underlie executive deficits (Anderson et al. 2005; Chen and Desmond 2005; Edgin et al. 2008). Studies began to examine the stepwise development of executive subcomponents in normal children and adolescents using measures that ranged in degree of required cognitive control (Conklin et al. 2007; Luciana et al. 2005). In preterm studies, at-risk very low birth weight and extremely low birth weight survivors performed poorly on working memory, verbal fluency, set shifting, interference suppression, inhibition, and behavioral regulation measures, despite average range intelligence (Bohm et al. 2004; Caravale et al. 2005; Harvey et al. 1999; Vicari et al. 2004). A prospective longitudinal study of young high-risk preterm children with white matter abnormality detected by magnetic resonance imaging at term equivalent found poor inhibitory control and mental inflexibility persisted from 2 to 4 years of age, even after controlling for IQ, socioeconomic status, and medical variables (Edgin et al. 2008). Australian extremely preterm survivors born in 1991–1992 also exhibited executive dysfunction, even after adjustment for sociodemographic variables and when those with substantial sensorineural impairment were excluded from analyses (Anderson and Doyle 2004). However, in a Danish national cohort at 5 years, case-control group differences were not found for memory and executive measures after controlling for IQ, suggesting a global cognitive impact of preterm birth (Hoff Esbjorn et al. 2006). The accumulating literature suggests that early executive dysfunction detection is both possible and necessary to permit timely diagnosis and intervention for fundamental capacities.
As neuropsychology clinical practice and research methods become increasingly sophisticated the opportunities to address more specific hypotheses about neurocognitive function are possible. Clinical assessments need to more effectively adapt strategies used in research to clinical assessment paradigms in order to examine more specific functions than general intelligence and broad achievement. A long history of reliance on global measures will necessarily be strengthened by more fine-tuned longitudinal studies of the development of specific neuropsychological domains in these at-risk children. Simultaneously, assessment of parental and environmental factors that contribute to the very young child’s growth and development need to be considered in such long-term studies. Establishing the foundational importance of thorough assessment should benefit these children as they mature and enter adolescence and young adulthood.
Post-2000 Birth: An Era of Tentative Optimism
Opinion persists that the long-term adverse effects of preterm birth cannot be lessened despite medical advances that have substantially improved survival (Tommiska et al. 2007; Tyson and Saigal 2005). However, reports of more optimal outcome have begun to be reported for recent births. Extremely preterm survival rates continue their upward trend post-2000, along with variable reports about medical complications and associated long-term morbidities. A reduction of adverse neurodevelopmental outcome has not always been found in conjunction with increased survival rates (O’Shea et al. 1997; Riley et al. 2008), but reduced morbidity was reported for infants born at 22–27 weeks gestational age in 1999–2000 (Markestad et al. 2005), and in 1990–2000 (Washburn et al. 2007). While post-2000 extremely preterm birth has not yet dramatically changed expectation for poor outcome (De Groote et al. 2007; Tyson and Saigal 2005), gradual gains have been noted for young survivors. In a 1988–2001 extremely low birth weight multicenter cohort who survived to NICU discharge, 27% had unimpaired outcomes at 18–22 months (Gargus et al. 2009). Identification of those factors that contribute most to successful long-term outcome remains a primary concern. Decisions about when to aggressively resuscitate the borderline viable infant remain individualized and care center-specific, with few published guidelines (Batton 2009; Kaempf et al. 2006).
Although post-2000 extremely preterm data allow for reserved optimism, comparisons with older cohort studies remain limited as recent survivors are still too young for researchers to appreciate their full outcome. Besides earlier reports, such as those that found 85% of a Swedish extremely low birth weight cohort had normal range cognitive development at 4 years of age (Stjernqvist and Svenningsen 1995), age-appropriate neurodevelopmental and cognitive outcomes are only just beginning to be reported, e.g., at 18–20 months (Wilson-Costello et al. 2007), and at early school age (Baron et al. 2009a). The extremely preterm survival rates in the former study increased from 49% to 68% to 71% for birth in 1982–1989, 1990–1999, and 2000–2002. Major neurologic and sensorineural impairment rates and mental developmental index scores <70, decreased for their 2000–2002 cohort at 20 months of age, i.e., 28%, 35%, to 23%. Better outcome was attributed to increased Cesarean delivery, increased antenatal steroid use, decreased postnatal steroid use, decreased intraventricular hemorrhage incidence, less sepsis, and a lowered moderate to severe cerebral palsy rate (Wilson-Costello et al. 2007). The significant decline in severe intraventricular hemorrhage may have particular relevance, as low intraventricular hemorrhage incidence but high incidence for other risk factors was present in the 1998–2001 cohort that had low average-to-average function in most respects, and no impaired scores (i.e., <−2 SD) (Ahronovich et al. 2007; Baron et al. 2009a). Reduced neonatal complication incidence is not sufficiently explanatory of favorable outcomes and more fine-grained analyses of both antenatal and postnatal factors are expected to lead to a more comprehensive understanding of risk and outcome of extremely preterm birth in future decades (Eichenwald and Stark 2008).
In summary, an examination of outcome studies by birth decades reveals the effects of progressively improving intensive care, with slight but consistent change in a positive direction beginning to be documented (Table 2). Nevertheless, cohort variability and the absence of a uniform metric to assess disability necessarily limited cross-study comparisons in this review. In the future, meta-analytic techniques should be applied to compare temporal trends in outcomes and to evaluate methodological quality, with particular emphasis on effect sizes.
Intervention and Future Directions
Prevention of preterm birth is the principal means of reducing mortality and morbidity (McCormick 1994). Yet, preterm incidence rates are rising steadily (Behrman and Butler 2007). Consequently, there is a need for strong advocacy, proactive measures, and enhanced inter-disciplinary collaboration among obstetrics/gynecology and neonatology practitioners, geneticists, immunologists, endocrinologists, and others to improve preterm risk assessment strategies and to devise appropriate interventions (Lamont 2003). Progress in antenatal and neonatal intensive care is evident in improving medical outcomes, and decreased mortality and severe morbidity rates. Molecular and cellular mechanisms associated with neonatal brain injury risk and injury prevention are the subject of intense study, which aids formulation of a rationale for developing specific strategies (Back et al. 2007). Early identification and management of cerebral circulation and autoregulation problems that increase the risk of ischemia in preterm neonates may prevent damage to white matter precursor cells by replenishing anti-oxidant defenses and preventing free radical generation, and protective agents may enable excitotoxic pathways to prevent oligodendrocyte precursor cell damage (Back et al. 2007; Khwaja and Volpe 2008).
Targeted intervention strategies uniquely suited for at-risk preterm neonates are likely to evolve with greater understanding of brain development, and of the mechanisms and progression of injury in the immature brain. Plasticity, the capacity for reorganization associated with an immature brain, becomes a fundamental consideration (Stiles 2008), along with the potential for greater vulnerability to brain injury (de Haan and Johnson 2003; Johnston 2009). Specific interventions are needed to support reparative processes as well as preventive strategies. Such studies will likely include analysis of biomarkers and interactions with other risk factors (Ferriero 2009).
Early postnatal intervention is crucial to ensure more optimal outcomes, particularly for mental development (Spittle et al. 2007). A stimulating home environment and early intervention lessened cognitive deficit in preschool very low birth weight (VLBW; <1,500 g) children, while increased deficit was found in those from less stimulating homes (Weisglas-Kuperus et al. 1993). Interventions can begin within the neonatal intensive care unit. Adaptation of the neonatal care environment prior to term using the Newborn Individualized Developmental Care and Assessment Program (NIDCAP) enhanced brain structure and function, and may promote the preterm infant’s self-regulatory capacity, leading to more optimal overall outcome (Als et al. 2003). Efforts to optimize preterm infant management through individualized developmentally informed approaches has encouragingly improved neurocognitive function (Westrup et al. 2002) and enhanced brain development, as documented with diffusion tensor imaging (Als et al. 2004). At 1 year, children born at <32 weeks and enrolled in a family centered developmentally supportive intervention program had a mean mental developmental index 10 points higher than those not enrolled, although psychomotor developmental index scores did not differ (Kleberg et al. 2002). Positive effects of this program were also reported for children at 3 years and born very low birth weight in 1992–1993 (Kleberg et al. 2000) and at age 18 months for children born in 1999–2004 (Peters et al. 2009), although not all centers have been able to demonstrate the effectiveness of this type of intervention (Maguire et al. 2009).
Concurrent with learning more about specific neuropsychological developmental processes and their susceptibility to disruption after early birth, timely and targeted interventions need to be devised and applied as preventive as well as remedial measures. It is concerning that those with mild-to-moderate disability and adverse social risk do not access those early intervention resources as consistently as those more impaired (Roberts et al. 2008), since it is these children who likely will benefit greatly from such treatments. Furthermore, enrollment in early intervention may be inconsistent, despite availability of services (Wang et al. 2009).
Cognitive rehabilitation strategies adapted for the cognitive late effects of childhood cancers that also affect cerebral white matter development and result in neuropsychological impairment are showing promise in addressing attention and cognitive processing deficits. These may be applicable to children born extremely preterm (Butler and Copeland 2002; Butler et al. 2008; Mulhern et al. 1992). Strategies that promote self-regulatory capacities and preserve the integrity of emerging neuropsychological capacities hold promise, as do structured “follow-along” intervention programs that customize support to the family and social and educational environments. Ongoing care post-neonatal unit discharge may be especially critical for both the preterm child and stressed family (Drotar et al. 2006; Kaaresen et al. 2006). The potential efficacy of pharmacological strategies has yet to be studied through clinical trial investigations. As more is learned about the unique vulnerable periods in development, interventions will need to be devised and implemented according to specific windows of opportunity. Multi-faceted approaches that integrate medical, cognitive, familial, and psychosocial needs within a community context will be required.
Intervention programs will also need to include an educational component to aid parents and educators in understanding the unique developmental needs of this vulnerable population. As more children survive into preschool and adolescence, educational systems need to be prepared to provide the types of interventions required to support optimal progress and overall adjustment.
Conclusions
A review of research on extremely preterm birth cognitive outcomes since the 1960’s to the present reveals that those extremely preterm children born post-2000 are more likely to demonstrate greater cognitive strengths than those survivors born in earlier eras of prenatal and neonatal intensive care. However, even children who have average general intelligence remain at risk for subtle to more profound neuropsychological and behavioral problems that will impact academic and personal functioning over their lifespan. Guarded optimism about the outcomes of today’s neonate appears appropriate, although discrepancies are seen across NICUs related to complex interrelated factors. It is necessary to identify those factors that promote resilience and best guide future intervention and prevention efforts. Access to ongoing care, follow-up surveillance, and interventional treatments appear critical. The vast literature on this population needs to be interpreted with an appreciation of the complex systemic interactions among biological, medical, social, familial, cultural, and environmental factors, and their influence on the dynamic and adaptive maturational process of brain development. Assessment strategies need to be more theory-driven and developmentally referenced, addressing specific neurobehavioral domains and subdomains of functioning. Furthermore, more consistent and comprehensive methods for describing overall outcome are needed so that interventions can be targeted appropriately and findings across studies can be directly compared. These assessment methods would need to address the impact of disability on overall functioning in the context of specific environmental and personal factors. The International Classification of Functioning (ICF) model has been suggested as a useful way of understanding the spectrum of issues affecting a child’s overall adjustment and adaptation (Msall and Park 2008). Greater use of sophisticated imaging techniques integrated with knowledge about developmental stage holds great promise to better inform about the developing child and the effects of too early birth on brain structure and function. These findings in turn will serve to guide advances in prevention and rehabilitation efforts.
References
Aarnoudse-Moens, C. S., Weisglas-Kuperus, N., van Goudoever, J. B., & Oosterlaan, J. (2009). Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics, 124(2), 717–728.
Adams-Chapman, I., Hansen, N. I., Stoll, B. J., & Higgins, R. (2008). Neurodevelopmental outcome of extremely low birth weight Infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics, 121, e1167–e1177.
Agustines, L. A., Lin, Y. G., Rumney, P. J., Lu, M. C., Bonebrake, R., Asrat, T., et al. (2000). Outcomes of extremely low-birth-wieight infants between 500 and 750 g. American Journal of Obstetrics and Gynecology, 182, 1113–1116.
Ahronovich, M., Baron, I. S., & Litman, F. (2007). Improved outcomes of extremely low birth weight infants. Pediatrics, 119, 1044.
Allin, M., Matsumoto, H., Santhouse, A. M., Nosarti, C., AlSady, M. H. S., Stewart, A. L., et al. (2001). Cognitive and motor function and the size of the cerebellum in adolescents born very pre-term. Brain, 124, 60–66.
Allin, M., Henderson, M., Suckling, J., Nosarti, C., Rushe, T., Fearon, P., et al. (2004). Effects of very low birthweight on brain structure in adulthood. Developmental Medicine and Child Neurology, 46, 46–53.
Allin, M., Salaria, S., Nosarti, C., Wyatt, J., Rifkin, L., & Murray, R. M. (2005). Vermis and lateral lobes of the cerebellum in adolescents born very preterm. NeuroReport, 16, 1821–1824.
Als, H., Gilkerson, L., Duffy, F. H., McAnulty, G. B., Buehler, D. M., Vandenberg, K., et al. (2003). A three-center, randomized, controlled trial of individualized developmental care for very low birth weight preterm infants: medical, neurodevelopmental, parenting, and caregiving effects. Journal of Developmental and Behavioral Pediatrics: JDBP, 24, 399–408.
Als, H., Duffy, F. H., McAnulty, G. B., Rivkin, M. J., Vajapeyam, S., Mulkern, R. V., et al. (2004). Early experience alters brain function and structure. Pediatrics, 113, 846–857.
American College of Obstetricians and Gynecologists. (2002). ACOG practice bulletin 38: perinatal care at the threshold of viability. Obstetrics and Gynecology, 100, 617–624.
Anderson, P., & Doyle, L. W. (2003). Neurobehavioral outcomes of school-age children born extremely low birth weight or very preterm in the 1990s. Journal of the American Medical Association, 289, 3264–3272.
Anderson, P., & Doyle, L. W. (2004). Executive functioning in school-aged children who were born very preterm or with extremely low birth weight in the 1990s. Pediatrics, 114, 50–57.
Anderson, V., Jacobs, R., & Harvey, A. S. (2005). Prefrontal lesions and attentional skills in childhood. Journal of the International Neuropsychological Society, 11, 817–831.
Ashton, D. M., Lawrence, H. C., 3rd, Adams, N. L., 3rd, & Fleischman, A. R. (2009). Surgeon General’s Conference on the Prevention of Preterm Birth. Obstetrics and Gynecology, 113, 925–930.
Aylward, G. P., Pfeiffer, S. L., Wright, A., & Verhulst, S. J. (1989). Outcome studies of low birth weight infants published in the last decade: a meta-analysis. Journal of Pediatrics, 115, 515–520.
Back, S. A. (2006). Perinatal white matter injury: the changing spectrum of pathology and emerging insights into pathogenetic mechanisms. Mental Retardation and Developmental Disabilities Research Reviews, 12, 129–140.
Back, S. A., Riddle, A., & McClure, M. M. (2007). Maturation-dependent vulnerability of perinatal white matter in premature birth. Stroke, 38(2 Suppl), 724–730.
Baron, I. S., Ahronovich, M. D., Erickson, K., Gidley Larson, J. C., & Litman, F. R. (2009a). Age-appropriate early school age neurobehavioral outcomes of extremely preterm birth without severe intraventricular hemorrhage: A single center experience. Early Human Development, 85, 191–196.
Baron, I. S., Erickson, K., Ahronovich, M., Coulehan, K., Baker, R., & Litman, F. (2009b). Visuospatial and verbal fluency relative deficits in ‘complicated’ late-preterm preschool children. Early Human Development, 85, 751–754.
Barrett, R. D., Bennet, L., Davidson, J., Dean, J. M., George, S., Emerald, B. S., et al. (2007). Destruction and reconstruction: hypoxia and the developing brain. Birth Defects Research. Part C: Embryo Today, 81, 163–176.
Barrington, K. J. (2001). The adverse neuro-developmental effects of postnatal steroids in the preterm infant: a systematic review of RCTs. BioMed Central Pediatrics, 1, 1.
Bartels, D. B., Kreienbrock, L., Dammann, O., Wenzlaff, P., & Poets, C. F. (2005). Population based study on the outcome of small for gestational age newborns. Archives of Disease in Childhood: Fetal and Neonatal Edition Archive, 90, F53–F59.
Bartha, A. I., Foster-Barber, A., Miller, S. P., Vigneron, D. B., Glidden, D. V., Barkovich, A. J., et al. (2004). Neonatal encephalopathy: association of cytokines with MR spectroscopy and outcome. Pediatric Research, 56, 960–966.
Batton, D. G. (2009). Clinical report–Antenatal counseling regarding resuscitation at an extremely low gestational age. Pediatrics, 124, 422–427.
Behrman, R., & Butler, A. (2007). Preterm birth: causes, consequences, and prevention. Washington, D.C.: National Academies Press.
Bhutta, A. T., & Anand, K. J. (2001). Abnormal cognition and behavior in preterm neonates linked to smaller brain volumes. Trends in Neuroscience, 24, 129–130. discussion 131–122.
Bhutta, A. T., Cleves, M. A., Casey, P. H., Cradock, M. M., & Anand, K. J. (2002). Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. Journal of the American Medical Association, 288, 728–737.
Bohin, S., Draper, E. S., & Field, D. J. (1999). Health status of a population of infants born before 26 weeks gestation derived from routine data collected between 21 and 27 months post-delivery. Early Human Development, 55, 9–18.
Bohm, B., Smedler, A. C., & Forssberg, H. (2004). Impulse control, working memory and other executive functions in preterm children when starting school. Acta Paediatrica, 93, 1363–1371.
Bowen, J. R., Gibson, F. L., & Hand, P. J. (2002). Educational outcome at 8 years for children who were born extremely prematurely: a controlled study. Journal of Paediatrics and Child Health, 38, 438–444.
Breslau, N., Paneth, N. S., & Lucia, V. C. (2004). The lingering academic deficits of low birth weight children. Pediatrics, 114, 1035–1040.
Brothwood, M., Wolke, D., Gamsu, H., Benson, J., & Cooper, D. (1986). Prognosis of the very low birthweight baby in relation to gender. Archives of Disease in Childhood, 61, 559–564.
Butler, R. W., & Copeland, D. R. (2002). Attentional processes and their remediation in children treated for cancer: a literature review and the development of a therapeutic approach. Journal of the International Neuropsychological Society, 8, 115–124.
Butler, R. W., Copeland, D. R., Fairclough, D. L., Mulhern, R. K., Katz, E. R., Kazak, A. E., et al. (2008). A multicenter, randomized clinical trial of a cognitive remediation program for childhood survivors of a pediatric malignancy. Journal of Consulting and Clinical Psychology, 76, 367–378.
Caravale, B., Tozzi, C., Albino, G., & Vicari, S. (2005). Cognitive development in low risk preterm infants at 3–4 years of life. Archives of Disease in Childhood. Fetal and Neonatal Edition, 90, F474–F479.
Carmody, D. P., Bendersky, M., Dunn, S. M., DeMarco, J. K., Hegyi, T., Hiatt, M., et al. (2006). Early risk, attention, and brain activation in adolescents born preterm. Child Development, 77, 384–394.
Castro, L., Yolton, K., Haberman, B., Roberto, N., Hansen, N. I., Ambalavanan, N., et al. (2004). Bias in reported neurodevelopmental outcomes among extremely low birth weight survivors. Pediatrics, 114, 404–410.
Chapieski, M. L., & Evankovich, K. D. (1997). Behavioral effects of prematurity. Seminars in Perinatology, 21, 221–239.
Chen, S. H., & Desmond, J. E. (2005). Cerebrocerebellar networks during articulatory rehearsal and verbal working memory tasks. Neuroimage, 24, 332–338.
Coccia, C., Pezzani, M., Moro, G. E., & Minoli, I. (1992). Management of extremely low-birth-weight infants. Acta Paediatrica. Supplement, 382, 10–12.
Cole, C., Hagadorn, J., & Kim, C. (2002). Criteria for determining disability in infants and children: Low birth weight. Evidence report/Technology Assessment No. 70, Publication No. 03-E010. Rockville: Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services.
Collaborative Group on Antenatal Steroid Therapy. (1984). Effects of antenatal dexamethasone administration in the infant: long-term follow-up. Journal of Pediatrics, 104, 259–267.
Conklin, H. M., Luciana, M., Hooper, C. J., & Yarger, R. S. (2007). Working memory performance in typically developing children and adolescents: behavioral evidence of protracted frontal lobe development. Developmental Neuropsychology, 31, 103–128.
Conom, D. H., Thomas, C., Evans, J., & Tan, K. I. (2006). Surfactant era (1990–2002) 2-year outcomes of infants less than 1500 g from a Community Level 3 Neonatal Intensive Care Unit. Journal of Perinatology, 26, 605–613.
Cooke, R. W. (2005). Perinatal and postnatal factors in very preterm infants and subsequent cognitive and motor abilities. Archives of Disease in Childhood. Fetal and Neonatal Edition Archive, 90, F60–F63.
Counsell, S. J., Allsop, J. M., Harrison, M. C., Larkman, D. J., Kennea, N. L., Kapellou, O., et al. (2003). Diffusion-weighted imaging of the brain in preterm infants with focal and diffuse white matter abnormality. Pediatrics, 112(1 Pt 1), 1–7.
Dammann, O., & Leviton, A. (2006). Neuroimaging and the prediction of outcomes in preterm infants. The New England Journal of Medicine, 355, 727–729.
Dammann, O., Naples, M., Bednarek, F., Shah, B., Kuban, K. C., O’Shea, T. M., et al. (2009). SNAP-II and SNAPPE-II and the risk of structural and functional brain disorders in extremely low gestational age newborns: The ELGAN study. Neonatology, 97, 71–82.
Daniel, L. M., Lim, S. B., & Clarke, L. (2003). Eight-year outcome of very-low-birth-weight infants born in KK hospital. Annals of the Academy of Medicine, Singapore, 32, 354–361.
de Graaf-Peters, V. B., & Hadders-Algra, M. (2006). Ontogeny of the human central nervous system: what is happening when? Early Human Development, 82, 257–266.
De Groote, I., Vanhaesebrouck, P., Bruneel, E., Dom, L., Durein, I., Hasaerts, D., et al. (2007). Outcome at 3 years of age in a population-based cohort of extremely preterm infants. Obstetrics and Gynecology, 110, 855–864.
de Haan, M., & Johnson, M. (2003). Mechanisms and theories of brain development. In M. de Haan & M. Johnson (Eds.), The cognitive neuroscience of development (pp. 1–18). New York: Psychology Press.
Delobel-Ayoub, M., Kaminski, M., Marret, S., Burguet, A., Marchand, L., N’Guyen, S., et al. (2006). Behavioral outcome at 3 years of age in very preterm infants: the EPIPAGE study. Pediatrics, 117, 1996–2005.
Doyle, L. W. (2004). Changing availability of neonatal intensive care for extremely low birthweight infants in Victoria over two decades. The Medical Journal of Australia, 181, 136–139.
Doyle, L. W., Permezel, M., Ford, G. W., Knoches, A. M., Rickards, A. L., Kelly, E. A., et al. (1994). The obstetrician and the extremely immature fetus (24–26 weeks): outcome to 5 years of age. The Australian & New Zealand Journal of Obstetrics & Gynaecology, 34, 421–424.
Drotar, D., Hack, M., Taylor, G., Schluchter, M., Andreias, L., & Klein, N. (2006). The impact of extremely low birth weight on the families of school-aged children. Pediatrics, 117, 2006–2013.
Dyet, L. E., Kennea, N., Counsell, S. J., Maalouf, E. F., Ajayi-Obe, M., Duggan, P. J., et al. (2006). Natural history of brain lesions in extremely preterm infants studied with serial magnetic resonance imaging from birth and neurodevelopmental assessment. Pediatrics, 118, 536–548.
Edgin, J. O., Inder, T. E., Anderson, P. J., Hood, K. M., Clark, C. A., & Woodward, L. J. (2008). Executive functioning in preschool children born very preterm: Relationship with early white matter pathology. Journal of the International Neuropsychological Society, 14, 90–101.
Ehrenkranz, R. A., Dusick, A. M., Vohr, B. R., Wright, L. L., Wrage, L. A., & Poole, W. K. (2006). Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics, 117, 1253–1261.
Eichenwald, E. C., & Stark, A. R. (2008). Management and outcomes of very low birth weight. The New England Journal of Medicine, 358, 1700–1711.
Emgard, M., Paradisi, M., Pirondi, S., Fernandez, M., Giardino, L., & Calza, L. (2006). Prenatal glucocorticoid exposure affects learning and vulnerability of cholinergic neurons. Neurobiology of Aging, 28, 112–121.
Emsley, H. C., Wardle, S. P., Sims, D. G., Chiswick, M. L., & D’Souza, S. W. (1998). Increased survival and deteriorating developmental outcome in 23 to 25 week old gestation infants, 1990–4 compared with 1984–9. Archives of Disease in Childhood. Fetal and Neonatal Edition Archive, 78, F99–F104.
Engle, W. A. (2004). Age terminology during the perinatal period. Pediatrics, 114, 1362–1364.
Engle, W. A., Tomashek, K. M., & Wallman, C. (2007). “Late-preterm” infants: a population at risk. Pediatrics, 120, 1390–1401.
Farooqi, A., Hagglof, B., Sedin, G., Gothefors, L., & Serenius, F. (2007). Mental health and social competencies of 10- to 12-year-old children born at 23 to 25 weeks of gestation in the 1990s: a Swedish national prospective follow-up study. Pediatrics, 120, 118–133.
Fawke, J. (2007). Neurological outcomes following preterm birth. Seminars in Fetal & Neonatal Medicine, 12, 374–382.
Ferrara, T. B., Hoekstra, R. E., Couser, R. J., Gaziano, E. P., Calvin, S. E., Payne, N. R., et al. (1994). Survival and follow-up of infants born at 23 to 26 weeks of gestational age: effects of surfactant therapy. Journal of Pediatrics, 124, 119–124.
Ferriero, D. M. (2004). Neonatal brain injury. The New England Journal of Medicine, 351, 1985–1995.
Ferriero, D. M. (2009). Controversies and advances in neonatal neurology: introduction. Pediatric Neurology, 40, 145–146.
Fily, A., Pierrat, V., Delporte, V., Breart, G., & Truffert, P. (2006). Factors associated with neurodevelopmental outcome at 2 years after very preterm birth: the population-based Nord-Pas-de-Calais EPIPAGE cohort. Pediatrics, 117, 357–366.
Flodmark, O., & Barkovich, A. J. (2002). Imaging of the infant brain. In H. Lagercrantz, M. Hanson, P. Evrard, & C. Rodeck (Eds.), The newborn brain: Neuroscience and clinical applications (pp. 289–316). Cambridge: Cambridge University Press.
Foster-Cohen, S., Edgin, J. O., Champion, P. R., & Woodward, L. J. (2007). Early delayed language development in very preterm infants: evidence from the MacArthur-Bates CDI. Journal of Child Language, 34, 655–675.
Gargus, R. A., Vohr, B. R., Tyson, J. E., High, P., Higgins, R. D., Wrage, L. A., et al. (2009). Unimpaired outcomes for extremely low birth weight infants at 18 to 22 months. Pediatrics, 124, 112–121.
Gianni, M. L., Picciolini, O., Vegni, C., Gardon, L., Fumagalli, M., & Mosca, F. (2007). Twelve-month neurofunctional assessment and cognitive performance at 36 months of age in extremely low birth weight infants. Pediatrics, 120, 1012–1019.
Gidley Larson, J. C., Baron, I. S., Ahronovich, M., & Iamipetro, M. (2010). Birth below 500 grams. In J. Morgan, I. S. Baron, & J. Ricker (Eds.), Casebook of clinical neuropsychology. New York: Oxford University Press.
Gimenez, M., Junque, C., Narberhaus, A., Caldu, X., Salgado-Pineda, P., Bargallo, N., et al. (2004). Hippocampal gray matter reduction associates with memory deficits in adolescents with history of prematurity. Neuroimage, 23, 869–877.
Gimenez, M., Junque, C., Narberhaus, A., Botet, F., Bargallo, N., & Mercader, J. M. (2006). Correlations of thalamic reductions with verbal fluency impairment in those born prematurely. NeuroReport, 17, 463–466.
Gimenez, M., Soria-Pastor, S., Junque, C., Caldu, X., Narberhaus, A., Botet, F., et al. (2008). Proton magnetic resonance spectroscopy reveals medial temporal metabolic abnormalities in adolescents with history of preterm birth. Pediatric Research, 64, 572–577.
Gross, S. J., Anbar, R. D., & Mettelman, B. B. (2005). Follow-up at 15 years of preterm infants from a controlled trial of moderately early dexamethasone for the prevention of chronic lung disease. Pediatrics, 115, 681–687.
Grunau, R. E., Whitfield, M. F., & Davis, C. (2002). Pattern of learning disabilities in children with extremely low birth weight and broadly average intelligence. Archives of Pediatrics & Adolescent Medicine, 156, 615–620.
Hack, M., & Fanaroff, A. A. (1989). Outcomes of extremely-low-birth-weight infants between 1982 and 1988. The New England Journal of Medicine, 321, 1642–1647.
Hack, M., & Fanaroff, A. A. (1999). Outcomes of children of extremely low birthweight and gestational age in the 1990’s. Early Human Development, 53, 193–218.
Hack, M., Taylor, H. G., Klein, N., Eiben, R., Schatschneider, C., & Mercuri-Minich, N. (1994). School-age outcomes in children with birth weights under 750 g. The New England Journal of Medicine, 331, 753–759.
Hack, M., Friedman, H., & Fanaroff, A. A. (1996). Outcomes of extremely low birth weight infants. Pediatrics, 98, 931–937.
Hack, M., Taylor, H. G., Klein, N., & Minich, N. (2000a). Functional limitations and special health care needs of 10- to 14-year-old children weighing less than 750 grams at birth. Pediatrics, 106, 554–559.
Hack, M., Wilson-Costello, D., Friedman, H., Taylor, H. G., Schluchter, M., & Fanaroff, A. A. (2000b). Neurodevelopment and predictors of outcomes of children with birth weights of less than 1000 g. Archives of Pediatrics & Adolescent Medicine, 154, 725–731.
Hack, M., Taylor, H. G., Drotar, D., Schluchter, M., Cartar, L., Andreias, L., et al. (2005). Chronic conditions, functional limitations, and special health care needs of school-aged children born with extremely low-birth-weight in the 1990s. Journal of the American Medical Association, 294, 318–325.
Hakansson, S., Farooqi, A., Holmgren, P. A., Serenius, F., & Hogberg, U. (2004). Proactive management promotes outcome in extremely preterm infants: A population-based comparison of two perinatal management strategies. Pediatrics, 114, 58–64.
Hall, A., McLeod, A., Counsell, C., Thomson, L., & Mutch, L. (1995). School attainment, cognitive ability and motor function in a total Scottish very-low-birthweight population at eight years: a controlled study. Developmental Medicine and Child Neurology, 37, 1037–1050.
Halliday, H. L. (2008). Surfactants: past, present and future. Journal of Perinatology, 28(Suppl 1), S47–S56.
Hamilton, B. E., Martin, J. A., & Ventura, S. J. (2006). Births: preliminary data for 2005. National Vital Statistics Reports, 55, 1–18.
Hamilton, B. E., Martin, J. A., & Ventura, S. J. (2009). Births: Preliminary data for 2007. National Vital Statistics Reports, 57.
Hamrick, S. E. G., Miller, S. P., Leonard, C., Glidden, D. V., Goldstein, R., Ramaswamy, V., et al. (2004). Trends in severe brain injury and neurodevelopmental outcome in premature newborn infants: The role of cystic periventricular leukomalacia. The Journal of Pediatrics, 145, 593–599.
Hansen, B. M., & Greisen, G. (2004). Is improved survival of very-low-birthweight infants in the 1980s and 1990s associated with increasing intellectual deficit in surviving children? Developmental Medicine and Child Neurology, 46, 812–815.
Hansen-Pupp, I., Hallin, A. L., Hellstrom-Westas, L., Cilio, C., Berg, A. C., Stjernqvist, K., et al. (2008). Inflammation at birth is associated with subnormal development in very preterm infants. Pediatric Research, 64, 183–188.
Harvey, J. M., O’Callaghan, M. J., & Mohay, H. (1999). Executive function of children with extremely low birthweight: a case control study. Developmental Medicine and Child Neurology, 41, 292–297.
Hille, E. T., den Ouden, A. L., Bauer, L., van den Oudenrijn, C., Brand, R., & Verloove-Vanhorick, S. P. (1994). School performance at nine years of age in very premature and very low birth weight infants: perinatal risk factors and predictors at five years of age. Collaborative Project on Preterm and Small for Gestational Age (POPS) Infants in The Netherlands. The Journal of Pediatrics, 125, 426–434.
Hille, E. T., den Ouden, A. L., Saigal, S., Wolke, D., Lambert, M., Whitaker, A., et al. (2001). Behavioural problems in children who weigh 1000 g or less at birth in four countries. Lancet, 357, 1641–1643.
Hille, E. T., Weisglas-Kuperus, N., van Goudoever, J. B., Jacobusse, G. W., Ens-Dokkum, M. H., de Groot, L., et al. (2007). Functional outcomes and participation in young adulthood for very preterm and very low birth weight infants: the Dutch Project on Preterm and Small for Gestational Age Infants at 19 years of age. Pediatrics, 120, e587–e595.
Hintz, S. R., Kendrick, D. E., Vohr, B. R., Poole, W. K., & Higgins, R. D. (2005). Changes in neurodevelopmental outcomes at 18 to 22 month’s corrected age among infants of less than 25 weeks’ gestational age born in 1993–1999. Pediatrics, 115, 1645–1651.
Hoekstra, R. E., Ferrara, T. B., Couser, R. J., Payne, N. R., & Connett, J. E. (2004). Survival and long-term neurodevelopmental outcome of extremely premature infants born at 23–26 weeks’ gestational age at a tertiary center. Pediatrics, 113(1 Pt 1), e1–e6.
Hoff Esbjorn, B., Hansen, B. M., Greisen, G., & Mortensen, E. L. (2006). Intellectual development in a danish cohort of prematurely born preschool children: specific or general difficulties? Journal of Developmental and Behavioral Pediatrics, 27, 477–484.
Huang, B. Y., & Castillo, M. (2008). Hypoxic-ischemic brain injury: imaging findings from birth to adulthood. Radiographics, 28, 417–439. quiz 617.
Inder, T. E., & Volpe, J. J. (2000). Mechanisms of perinatal brain injury. Seminars in Neonatology, 5, 3–16.
International Neonatal Network, S. N. C., Nurses Collaborative Study Group, (2000). Risk adjusted and population based studies of the outcome for high risk infants in Scotland and Australia: Archives of Disease in Childhood: Fetal and Neonatal Edition, 82, 118–123.
Isaacs, E. B., Lucas, A., Chong, W. K., Wood, S. J., Johnson, C. L., Marshall, C., et al. (2000). Hippocampal volume and everyday memory in children of very low birth weight. Pediatric Research, 47, 713–720.
Jenkins, D. D., Chang, E., & Singh, I. (2009). Neuroprotective interventions: is it too late? Journal of Child Neurology, 24, 1212–1219.
Jeyaseelan, D., O’Callaghan, M., Neulinger, K., Shum, D., & Burns, Y. (2006). The association between early minor motor difficulties in extreme low birth weight infants and school age attentional difficulties. Early Human Development, 82, 249–255.
Jobe, A. H. (2004). Postnatal corticosteroids for preterm infants—do what we say, not what we do. The New England Journal of Medicine, 350, 1349–1351.
Johnson, S., Fawke, J., Hennessy, E., Rowell, V., Thomas, S., Wolke, D., et al. (2009). Neurodevelopmental disability through 11 years of age in children born before 26 weeks of gestation. Pediatrics, 124, e249–e257.
Johnston, M. V. (2009). Plasticity in the developing brain: implications for rehabilitation. Developmental Disabilities Research Reviews, 15, 94–101.
Kaaresen, P. I., Ronning, J. A., Ulvund, S. E., & Dahl, L. B. (2006). A randomized, controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics, 118, e9–e19.
Kaempf, J. W., Tomlinson, M., Arduza, C., Anderson, S., Campbell, B., Ferguson, L. A., et al. (2006). Medical staff guidelines for periviability pregnancy counseling and medical treatment of extremely premature infants. Pediatrics, 117, 22–29.
Kesler, S. R., Ment, L. R., Vohr, B., Pajot, S. K., Schneider, K. C., Katz, K. H., et al. (2004). Volumetric analysis of regional cerebral development in preterm children. Pediatric Neurology, 31, 318–325.
Kesler, S. R., Vohr, B., Schneider, K. C., Katz, K. H., Makuch, R. W., Reiss, A. L., et al. (2006). Increased temporal lobe gyrification in preterm children. Neuropsychologia, 44, 445–453.
Kesler, S. R., Reiss, A. L., Vohr, B., Watson, C., Schneider, K. C., Katz, K. H., et al. (2008). Brain volume reductions within multiple cognitive systems in male preterm children at age twelve. Journal of Pediatrics, 152, 513–520. 520 e511.
Khwaja, O., & Volpe, J. J. (2008). Pathogenesis of cerebral white matter injury of prematurity. Archives of Disease in Childhood. Fetal and Neonatal Edition, 93, F153–F161.
Kilbride, H. W., Thorstad, K., & Daily, D. K. (2004). Preschool outcome of less than 801-gram preterm infants compared with full-term siblings. Pediatrics, 113, 742–747.
Kleberg, A., Westrup, B., & Stjernqvist, K. (2000). Developmental outcome, child behaviour and mother-child interaction at 3 years of age following Newborn Individualized Developmental Care and Intervention Program (NIDCAP) intervention. Early Human Development, 60, 123–135.
Kleberg, A., Westrup, B., Stjernqvist, K., & Lagercrantz, H. (2002). Indications of improved cognitive development at one year of age among infants born very prematurely who received care based on the Newborn Individualized Developmental Care and Assessment Program (NIDCAP). Early Human Development, 68, 83–91.
Koeppen-Schomerus, G., Eley, T. C., Wolke, D., Gringras, P., & Plomin, R. (2000). The interaction of prematurity with genetic and environmental influences on cognitive development in twins. Journal of Pediatrics, 137, 527–533.
Kok, J. H., den Ouden, A. L., Verloove-Vanhorick, S. P., & Brand, R. (1998). Outcome of very preterm small for gestational age infants: the first nine years of life. British Journal of Obstetrics and Gynecology, 105, 162–168.
Korogi, Y., Takahashi, M., Sumi, M., Hirai, T., Sakamoto, Y., Ikushima, I., et al. (1996). MR signal intensity of the perirolandic cortex in the neonate and infant. Paediatric Neuroradiology, 38, 578–584.
Lamont, R. F. (2003). Looking to the future. BJOG: An International Journal of Obstetrics And Gynaecology, 110(Suppl 20), 131–135.
Landry, S. H., Smith, K. E., & Swank, P. R. (2006). Responsive parenting: establishing early foundations for social, communication, and independent problem-solving skills. Developmental Psychology, 42, 627–642.
Laptook, A. R., O’Shea, M., Shankaran, S., Bhaskar, B., & Network, N. N. (2005). Adverse neurodevelopmental outcomes among extremely low birth weight infants with a normal head ultrasound: prevalence and antecedents. Pediatrics, 115, 673–680.
Larroque, B., Ancel, P. Y., Marret, S., Marchand, L., Andre, M., Arnaud, C., et al. (2008). Neurodevelopmental disabilities and special care of 5-year-old children born before 33 weeks of gestation (the EPIPAGE study): a longitudinal cohort study. Lancet, 371, 813–820.
Lefebvre, F., Bard, H., Veilleux, A., & Martel, C. (1988). Outcome at school age of children with birthweights of 1000 grams or less. Developmental Medicine and Child Neurology, 30, 170–180.
Limperopoulos, C., Soul, J. S., Gauvreau, K., Huppi, P. S., Warfield, S. K., Bassan, H., et al. (2005). Late gestation cerebellar growth is rapid and impeded by premature birth. Pediatrics, 115, 688–695.
Lodygensky, G. A., Rademaker, K., Zimine, S., Gex-Fabry, M., Lieftink, A. F., Lazeyras, F., et al. (2005). Structural and functional brain development after hydrocortisone treatment for neonatal chronic lung disease. Pediatrics, 116, 1–7.
Lorenz, J. M., Wooliever, D. E., Jetton, J. R., & Paneth, N. (1998). A quantitative review of mortality and developmental disability in extremely premature newborns. Archives of Pediatrics & Adolescent Medicine, 152, 425–435.
Luciana, M., Conklin, H. M., Hooper, C. J., & Yarger, R. S. (2005). The development of nonverbal working memory and executive control processes in adolescents. Child Development, 76, 697–712.
Lumley, J., Kitchen, W. H., Roy, R. N., Yu, V. Y., & Drew, J. H. (1988). The survival of extremely-low-birthweight infants in Victoria: 1982–1985. The Medical Journal of Australia, 149(242), 244–246.
Luu, T. M., Ment, L. R., Schneider, K. C., Katz, K. H., Allan, W. C., & Vohr, B. R. (2009). Lasting effects of preterm birth and neonatal brain hemorrhage at 12 years of age. Pediatrics, 123, 1037–1044.
Maayan-Metzger, A., Naor, N., & Sirota, L. (2002). Comparative outcome study between triplet and singleton preterm newborns. Acta Paediatrica, 91, 1208–1211.
MacDonald, H. (2002). Perinatal care at the threshold of viability. Pediatrics, 110, 1024–1027.
Maguire, C. M., Walther, F. J., Sprij, A. J., Le Cessie, S., Wit, J. M., & Veen, S. (2009). Effects of individualized developmental care in a randomized trial of preterm infants <32 weeks. Pediatrics, 124, 1021–1030.
Malaeb, S., & Dammann, O. (2009). Fetal inflammatory response and brain injury in the preterm newborn. Journal of Child Neurology, 24(9), 1119–1126.
Markestad, T., Kaaresen, P. I., Ronnestad, A., Reigstad, H., Lossius, K., Medbo, S., et al. (2005). Early death, morbidity, and need of treatment among extremely premature infants. Pediatrics, 115, 1289–1298.
Marlow, N., Wolke, D., Bracewell, M. A., & Samara, M. (2005). Neurologic and developmental disability at six years of age after extremely preterm birth. The New England Journal of Medicine, 352, 9–19.
Martin, J. A., Hamilton, B. E., Sutton, P. D., Ventura, S. J., Menacker, F., & Munson, M. L. (2005). Births: final data for 2003. National Vital Statistics Reports, 54, 1–116.
Martin, J. A., Kung, H. C., Mathews, T. J., Hoyert, D. L., Strobino, D. M., Guyer, B., et al. (2008). Annual summary of vital statistics: 2006. Pediatrics, 121, 788–801.
Martinussen, M., Flanders, D. W., Fischl, B., Busa, E., Lohaugen, G. C., Skranes, J., et al. (2009). Segmental brain volumes and cognitive and perceptual correlates in 15-year-old adolescents with low birth weight. Journal of Pediatrics, 155(848–853), e841.
McCormick, M. C. (1994). Survival of very tiny babies-good news and bad news. The New England Journal of Medicine, 331, 802–803.
McCormick, M. C., Brooks-Gunn, J., Buka, S. L., Goldman, J., Yu, J., Salganik, M., et al. (2006). Early intervention in low birth weight premature infants: results at 18 years of age for the Infant Health and Development Program. Pediatrics, 117, 771–780.
McQuillen, P. S., & Ferriero, D. M. (2004). Selective vulnerability in the developing central nervous system. Pediatric Neurology, 30, 227–235.
Ment, L. R., Peterson, B. S., Meltzer, J. A., Vohr, B., Allan, W., Katz, K. H., et al. (2006). A functional magnetic resonance imaging study of the long-term influences of early indomethacin exposure on language processing in the brains of prematurely born children. Pediatrics, 118, 961–970.
Ment, L. R., Kesler, S., Vohr, B., Katz, K. H., Baumgartner, H., Schneider, K. C., et al. (2009). Longitudinal brain volume changes in preterm and term control subjects during late childhood and adolescence. Pediatrics, 123, 503–511.
Meyer-Bahlburg, H. F., Dolezal, C., Baker, S. W., Carlson, A. D., Obeid, J. S., & New, M. I. (2004). Cognitive and motor development of children with and without congenital adrenal hyperplasia after early-prenatal dexamethasone. The Journal of Clinical Endocrinology and Metabolism, 89, 610–614.
Mikkola, K., Ritari, N., Tommiska, V., Salokorpi, T., Lehtonen, L., Tammela, O., et al. (2005). Neurodevelopmental outcome at 5 years of age of a national cohort of extremely low birth weight infants who were born in 1996–1997. Pediatrics, 116, 1391–1400.
Msall, M. E. (2005). Measuring functional skills in preschool children at risk for neurodevelopmental disabilities. Mental Retardation and Developmental Disabilities Research Reviews, 11, 263–273.
Msall, M. E., & Park, J. J. (2008). The spectrum of behavioral outcomes after extreme prematurity: regulatory, attention, social, and adaptive dimensions. Seminars in Perinatology, 32, 42–50.
Msall, M. E., Phelps, D. L., Hardy, R. J., Dobson, V., Quinn, G. E., Summers, C. G., et al. (2004). Educational and social competencies at 8 years in children with threshold retinopathy of prematurity in the CRYO-ROP multicenter study. Pediatrics, 113, 790–799.
Mulhern, R. K., Hancock, J., Fairclough, D., & Kun, L. (1992). Neuropsychological status of children treated for brain tumors: a critical review and integrative analysis. Medical and Pediatric Oncology, 20, 181–191.
Neubauer, A. P., Voss, W., & Kattner, E. (2008). Outcome of extremely low birth weight survivors at school age: The influence of perinatal parameters on neurodevelopment. European Journal of Pediatrics, 167, 87–95.
Nickel, R. E., Bennett, F. C., & Lamson, F. N. (1982). School performance of children with birth weights of 1,000 g or less. Amercan Journal of Diseases of Children, 136, 105–110.
Nosarti, C., Al-Asady, M. H., Frangou, S., Stewart, A. L., Rifkin, L., & Murray, R. M. (2002). Adolescents who were born very preterm have decreased brain volumes. Brain, 125(Pt 7), 1616–1623.
Nosarti, C., Rushe, T. M., Woodruff, P. W., Stewart, A. L., Rifkin, L., & Murray, R. M. (2004). Corpus callosum size and very preterm birth: relationship to neuropsychological outcome. Brain, 127(Pt 9), 2080–2089.
Nosarti, C., Giouroukou, E., Healy, E., Rifkin, L., Walshe, M., Reichenberg, A., et al. (2008). Grey and white matter distribution in very preterm adolescents mediates neurodevelopmental outcome. Brain, 131(Pt 1), 205–217.
Okazaki, K., Nishida, A., Kato, M., Kozawa, K., Uga, N., & Kimura, H. (2006). Elevation of cytokine concentrations in asphyxiated neonates. Biology of the Neonate, 89, 183–189.
Okereafor, A., Allsop, J., Counsell, S. J., Fitzpatrick, J., Azzopardi, D., Rutherford, M. A., et al. (2008). Patterns of brain injury in neonates exposed to perinatal sentinel events. Pediatrics, 121, 906–914.
O’Shea, M. (2008). Cerebral palsy. Seminars in Perinatology, 32, 35–41.
O’Shea, T. M., Klinepeter, K. L., Goldstein, D. J., Jackson, B. W., & Dillard, R. G. (1997). Survival and developmental disability in infants with birth weights of 501 to 800 grams, born between 1979 and 1994. Pediatrics, 100, 982–986.
O’Shea, T. M., Washburn, L. K., Nixon, P. A., & Goldstein, D. J. (2007). Follow-up of a randomized, placebo-controlled trial of dexamethasone to decrease the duration of ventilator dependency in very low birth weight infants: neurodevelopmental outcomes at 4 to 11 years of age. Pediatrics, 120, 594–602.
Papile, L.-A., Burstein, J., Burstein, R., & Koffler, H. (1978). Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infants with birth weight less than 1500 g. Journal of Pediatrics, 92, 529–534.
Patra, K., Wilson-Costello, D., Taylor, H. G., Mercuri-Minich, N., & Hack, M. (2006). Grades I–II intraventricular hemorrhage in extremely low birth weight infants: Effects on neurodevelopment. Journal of Pediatrics, 149, 169–173.
Peters, K. L., Rosychuk, R. J., Hendson, L., Cote, J. J., McPherson, C., & Tyebkhan, J. M. (2009). Improvement of short- and long-term outcomes for very low birth weight infants: Edmonton NIDCAP trial. Pediatrics, 124, 1009–1020.
Peterson, B. S., Vohr, B. R., Staib, L. H., Cannistraci, C. J., Dolberg, A., Schneider, K. C., et al. (2000). Regional brain volume abnormalities and long-term cognitive outcome in preterm infants. Journal of the American Medical Association, 284, 1939–1947.
Peterson, B. S., Anderson, A. W., Ehrenkranz, R., Staib, L. H., Tageldin, M., Colson, E., et al. (2003). Regional brain volumes and their later neurodevelopmental correlates in term and preterm infants. Pediatrics, 111(5 Pt 1), 939–948.
Piecuch, R. E., Leonard, C. H., Cooper, B. A., Kilpatrick, S. J., Schlueter, M. A., & Sola, A. (1997). Outcome of infants born at 24–26 weeks’ gestation: II. Neurodevelopmental outcome. Obstetrics and Gynecology, 90, 809–814.
Portnoy, S., Callias, M., Wolke, D., & Gamsu, H. (1988). Five-year follow-up study of extremely low-birthweight infants. Developmental Medicine and Child Neurology, 30, 590–598.
Raz, S., Debastos, A. K., Newman, J. B., & Batton, D. (2009). Extreme prematurity and neuropsychological outcome in the preschool years. Journal of the International Neuropsychological Society, 1–11
Reiss, A. L., Kesler, S. R., Vohr, B., Duncan, C. C., Katz, K. H., Pajot, S., et al. (2004). Sex differences in cerebral volumes of 8-year-olds born preterm. Journal of Pediatrics, 145, 242–249.
Rezaie, P., & Dean, A. (2002). Periventricular leukomalacia, inflammation and white matter lesions within the developing nervous system. Neuropathology, 22, 106–132.
Rijken, M., Stoelhorst, G. M., Martens, S. E., van Zwieten, P. H., Brand, R., Wit, J. M., et al. (2003). Mortality and neurologic, mental, and psychomotor development at 2 years in infants born less than 27 weeks’ gestation: the Leiden follow-up project on prematurity. Pediatrics, 112, 351–358.
Riley, K., Roth, S., Sellwood, M., & Wyatt, J. S. (2008). Survival and neurodevelopmental morbidity at 1 year of age following extremely preterm delivery over a 20-year period: a single centre cohort study. Acta Paediatrica, 97, 159–165.
Roberts, G., Howard, K., Spittle, A. J., Brown, N. C., Anderson, P. J., & Doyle, L. W. (2008). Rates of early intervention services in very preterm children with developmental disabilities at age 2 years. Journal of Paediatrics and Child Health, 44, 276–280.
Roth, S. C., Baudin, J., McCormick, D. C., Edwards, A. D., Townsend, J., Stewart, A. L., et al. (1993). Relation between ultrasound appearance of the brain of very preterm infants and neurodevelopmental impairment at eight years. Developmental Medicine and Child Neurology, 35, 755–768.
Rushe, T. M., Rifkin, L., Stewart, A. L., Townsend, J. P., Roth, S. C., Wyatt, J. S., et al. (2001). Neuropsychological outcome at adolescence of very preterm birth and its relation to brain structure. Developmental Medicine and Child Neurology, 43, 226–233.
Saigal, S., & Doyle, L. W. (2008). An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet, 371, 261–269.
Saigal, S., Hoult, L. A., Streiner, D. L., Stoskopf, B. L., & Rosenbaum, P. L. (2000). School difficulties at adolescence in a regional cohort of children who were extremely low birth weight. Pediatrics, 105, 325–331.
Saigal, S., den Ouden, L., Wolke, D., Hoult, L., Paneth, N., Streiner, D. L., et al. (2003). School-age outcomes in children who were extremely low birth weight from four international population-based cohorts. Pediatrics, 112, 943–950.
Saigal, S., Stoskopf, B., Streiner, D., Boyle, M., Pinelli, J., Paneth, N., et al. (2006). Transition of extremely low-birth-weight infants from adolescence to young adulthood: comparison with normal birth-weight controls. Journal of the American Medical Association, 295, 667–675.
Selzer, S. C., Lindgren, S. D., & Blackman, J. A. (1992). Long-term neuropsychological outcome of high risk infants with intracranial hemorrhage. Journal of Pediatric Psychology, 17, 407–422.
Sen, E., & Levison, S. W. (2006). Astrocytes and developmental white matter disorders. Mental Retardation and Developmental Disabilities Research Reviews, 12, 97–104.
Shankaran, S., Johnson, Y., Langer, J. C., Vohr, B. R., Fanaroff, A. A., Wright, L. L., et al. (2004). Outcome of extremely-low-birth-weight infants at highest risk: gestational age < or =24 weeks, birth weight < or =750 g, and 1-minute Apgar < or =3. American Journal of Obstetrics and Gynecology, 191, 1084–1091.
Sherlock, R. L., Anderson, P. J., & Doyle, L. W. (2005). Neurodevelopmental sequelae of intraventricular haemorrhage at 8 years of age in a regional cohort of ELBW/very preterm infants. Early Human Development, 81, 909–916.
Short, E. J., Klein, N. K., Lewis, B. A., Fulton, S., Eisengart, S., Kercsmar, C., et al. (2003). Cognitive and academic consequences of bronchopulmonary dysplasia and very low birth weight: 8-year-old outcomes. Pediatrics, 112, e359.
Skrablin, S., Kuvacic, I., Kalafatic, D., Peter, B., Gveric-Ahmetasevic, S., Letica-Protega, N., et al. (2002). Perinatal care improves the outcome of triplets. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 10, 26–31.
Soria-Pastor, S., Gimenez, M., Narberhaus, A., Falcon, C., Botet, F., Bargallo, N., et al. (2008). Patterns of cerebral white matter damage and cognitive impairment in adolescents born very preterm. International Journal of Developmental Neuroscience, 26, 647–654.
Soria-Pastor, S., Padilla, N., Zubiaurre-Elorza, L., Ibarretxe-Bilbao, N., Botet, F., Costas-Moragas, C., et al. (2009). Decreased regional brain volume and cognitive impairment in preterm children at low risk. Pediatrics, 124, e1161–e1170.
Spittle, A. J., Orton, J., Doyle, L. W., & Boyd, R. (2007). Early developmental intervention programs post hospital discharge to prevent motor and cognitive impairments in preterm infants. Cochrane Database of Systematic Reviews (2), CD005495.
Srinivasan, L., Dutta, R., Counsell, S. J., Allsop, J. M., Boardman, J. P., Rutherford, M. A., et al. (2007). Quantification of deep gray matter in preterm infants at term-equivalent age using manual volumetry of 3-tesla magnetic resonance images. Pediatrics, 119, 759–765.
Steinmacher, J., Pohlandt, F., Bode, H., Sander, S., Kron, M., & Franz, A. R. (2008). Neurodevelopmental follow-up of very preterm infants after proactive treatment at a gestational age of >=23 Weeks. Journal of Pediatrics, 152, 771–776.
Stewart, A. L., Rifkin, L., Amess, P. N., Kirkbride, V., Townsend, J. P., Miller, D. H., et al. (1999). Brain structure and neurocognitive and behavioural function in adolescents who were born very preterm. Lancet, 353, 1653–1657.
Stiles, J. (2008). The fundamentals of brain development: Integrating nature and nurture. Cambridge: Harvard University Press.
Stjernqvist, K. (1992). Extremely low birth weight infants less than 901 g. Impact on the family during the first year. Scandinavian Journal of Social Medicine, 20, 226–233.
Stjernqvist, K., & Svenningsen, N. W. (1990). Neurobehavioural development at term of extremely low-birthweight infants (less than 901 g). Developmental Medicine and Child Neurology, 32, 679–688.
Stjernqvist, K., & Svenningsen, N. W. (1993). Extremely low-birth-weight infants less than 901 g. Growth and development after one year of life. Acta Paediatrica, 82, 40–44.
Stjernqvist, K., & Svenningsen, N. W. (1995). Extremely low-birth-weight infants less than 901 g: Development and behaviour after 4 years of life. Acta Paediatrica, 84, 500–506.
Stjernqvist, K., & Svenningsen, N. W. (1999). Ten-year follow-up of children born before 29 gestational weeks: health, cognitive development, behaviour and school achievement. Acta Paediatrica, 88, 557–562.
Sutton, L., & Bajuk, B. (1999). Population-based study of infants born at less than 28 weeks’ gestation in New South Wales, Australia, in 1992–3. New South Wales Neonatal Intensive Care Unit Study Group. Paediatric and Perinatal Epidemiology, 13, 288–301.
Synnes, A. R., Ling, E. W., Whitfield, M. F., Mackinnon, M., Lopes, L., Wong, G., et al. (1994). Perinatal outcomes of a large cohort of extremely low gestational age infants (twenty-three to twenty-eight completed weeks of gestation). Journal of Pediatrics, 125(6 Pt 1), 952–960.
Szatmari, P., Saigal, S., Rosenbaum, P., Campbell, D., & King, S. (1990). Psychiatric disorders at five years among children with birthweights less than 1000 g: a regional perspective. Developmental Medicine and Child Neurology, 32, 954–962.
Tauscher, M. K., Berg, D., Brockmann, M., Seidenspinner, S., Speer, C. P., & Groneck, P. (2003). Association of histologic chorioamnionitis, increased levels of cord blood cytokines, and intracerebral hemorrhage in preterm neonates. Biology of the Neonate, 83, 166–170.
Taylor, H. G., Hack, M., & Klein, N. K. (1998). Attention deficits in children with <750 gm birth weight. Child Neuropsychology, 4, 21–34.
Taylor, H. G., Klein, N., Minich, N., & Hack, M. (2000). Middle-school-age outcomes in children with very low birthweight. Child Development, 71, 1495–1511.
Taylor, H. G., Minich, N. M., Klein, M., & Hack, M. (2004). Longitudinal outcomes of very low birth weight: neuropsychological findings. Journal of the International Neuropsychological Society, 10, 149–163.
Taylor, H. G., Klein, N., Drotar, D., Schluchter, M., & Hack, M. (2006). Consequences and risks of <1000-g birth weight for neuropsychological skills, achievement, and adaptive functioning. Journal of Developmental and Behavioral Pediatrics, 27, 459–469.
Teplin, S. W., Burchinal, M., Johnson-Martin, N., Humphry, R. A., & Kraybill, E. N. (1991). Neurodevelopmental, health, and growth status at age 6 years of children with birth weights less than 1001 grams. Journal of Pediatrics, 118, 768–777.
The Victorian Infant Collaborative Study Group. (1997). Outcome at 2 years of children 23–27 weeks’ gestation born in Victoria in 1991–92. The Victorian Infant Collaborative Study Group. Journal of Paediatrics and Child Health, 33, 161–165.
Thompson, D. K., Wood, S. J., Doyle, L. W., Warfield, S. K., Lodygensky, G. A., Anderson, P. J., et al. (2008). Neonate hippocampal volumes: prematurity, perinatal predictors, and 2-year outcome. Annals of Neurology, 63, 642–651.
Tommiska, V., Heinonen, K., Lehtonen, L., Renlund, M., Saarela, T., Tammela, O., et al. (2007). No improvement in outcome of nationwide extremely low birth weight infant populations between 1996–1997 and 1999–2000. Pediatrics, 119, 29–36.
Trautman, P. D., Meyer-Bahlburg, H. F., Postelnek, J., & New, M. I. (1995). Effects of early prenatal dexamethasone on the cognitive and behavioral development of young children: results of a pilot study. Psychoneuroendocrinology, 20, 439–449.
Tyson, J. E., & Saigal, S. (2005). Outcomes for extremely low-birth-weight infants: Disappointing news. Journal of the American Medical Association, 294, 371–373.
Tyson, J. E., Parikh, N. A., Langer, J., Green, C., & Higgins, R. D. (2008). Intensive care for extreme prematurity—moving beyond gestational age. The New England Journal of Medicine, 358, 1672–1681.
Vanhaesebrouck, P., Allegaert, K., Bottu, J., Debauche, C., Devlieger, H., Docx, M., et al. (2004). The EPIBEL study: outcomes to discharge from hospital for extremely preterm infants in Belgium. Pediatrics, 114, 663–675.
Vavasseur, C., Foran, A., & Murphy, J. F. (2007). Consensus statements on the borderlands of neonatal viability: from uncertainty to grey areas. Irish Medical Journal, 100, 561–564.
Vicari, S., Caravale, B., Carlesimo, G. A., Casadei, A. M., & Allemand, F. (2004). Spatial working memory deficits in children at ages 3–4 who were low birth weight, preterm infants. Neuropsychology, 18, 673–678.
Vohr, B. R., & Garcia Coll, C. T. (1985). Neurodevelopmental and school performance of very low-birth weight infants: A seven year longitudinal study. Pediatrics, 76, 345–350.
Vohr, B. R., Wright, L., Dusick, A., Mele, L., Verter, J., Steichen, J. J., et al. (2000). Neurodevelopmental and functional outcomes of extremely low birth weight infants iin the National Institute of Child Health and Human Development Neonatal Research Network, 1993–1994. Pediatrics, 105, 1216–1226.
Vohr, B. R., Allan, W., Westerveld, M., Schneider, K., Katz, K., Makuch, R. W., et al. (2003a). School-age outcomes of very low birth weight infants in the indomethacin intraventricular hemorrhage prevention trial. Pediatrics, 111, e340–e346.
Vohr, B. R., Allan, W. C., Westerveld, M., Schneider, K. C., Katz, K. H., Makuch, R. W., et al. (2003b). School-age outcomes of very low birth weight infants in the indomethacin intraventricular hemorrhage prevention trial. Pediatrics, 111(4 Pt 1), e340–e346.
Vohr, B. R., Wright, L. L., Dusick, A. M., Perritt, R., Poole, W. K., Tyson, J. E., et al. (2004). Center differences and outcomes of extremely low birth weight infants. Pediatrics, 113, 781–789.
Vohr, B. R., Wright, L. L., Poole, W. K., & McDonald, S. A. (2005). Neurodevelopmental outcomes of extremely low birth weight infants <32 weeks’ gestation between 1993 and 1998. Pediatrics, 116, 635–643.
Volpe, J. J. (2005). Encephalopathy of prematurity includes neuronal abnormalities. Pediatrics, 116, 221–225.
Volpe, J. J. (2008). Neurology of the newborn (5th ed.). Philadelphia: Saunders Elsevier.
Wang, C. J., Elliott, M. N., Rogowski, J., Lim, N., Ratner, J. A., & Schuster, M. A. (2009). Factors influencing the enrollment of eligible extremely-low-birth-weight children in the part C early intervention program. Academic Pediatrics, 9, 283–287.
Washburn, L. K., Dillard, R. G., Goldstein, D. J., Klinepeter, K. L., deRegnier, R. A., & O’Shea, T. M. (2007). Survival and major neurodevelopmental impairment in extremely low gestational age newborns born 1990–2000: a retrospective cohort study. BMC Pediatrics, 7, 20.
Washington, J. A., & Craig, H. A. (1992). Performances of low-income, African-American preschool and kindergarten children on the Peabody Picture Vocabulary Test-Revised. Language, Speech, and Hearing Services in Schools, 23, 329–333.
Weisglas-Kuperus, N., Baerts, W., Smrkovsky, M., & Sauer, P. J. (1993). Effects of biological and social factors on the cognitive development of very low birth weight children. Pediatrics, 92, 658–665.
Westrup, B., Stjernqvist, K., Kleberg, A., Hellstrom-Westas, L., & Lagercrantz, H. (2002). Neonatal individualized care in practice: a Swedish experience. Seminars in Neonatology, 7, 447–457.
Wilson, T. T., Waters, L., Patterson, C. C., McCusker, C. G., Rooney, N. M., Marlow, N., et al. (2006). Neurodevelopmental and respiratory follow-up results at 7 years for children from the United Kingdom and Ireland enrolled in a randomized trial of early and late postnatal corticosteroid treatment, systemic and inhaled (the Open Study of Early Corticosteroid Treatment). Pediatrics, 117, 2196–2205.
Wilson-Costello, D., Friedman, H., Minich, N., Siner, B., Taylor, G., Schluchter, M., et al. (2007). Improved neurodevelopmental outcomes for extremely low birth weight infants in 2000–2002. Pediatrics, 119, 37–45.
Wolke, D., Samara, M., Bracewell, M., & Marlow, N. (2008). Specific language difficulties and school achievement in children born at 25 weeks of gestation or less. Journal of Pediatrics, 152, 256–262.
Wood, N. S., Marlow, N., Costeloe, K., Gibson, A. T., & Wilkinson, A. R. (2000). Neurologic and developmental disability after extremely preterm birth. The New England Journal of Medicine, 343, 378–384.
Wood, N. S., Costeloe, K., Gibson, A. T., Hennessy, E. M., Marlow, N., & Wilkinson, A. R. (2003). The EPICure study: growth and associated problems in children born at 25 weeks of gestational age or less. Archives of Disease in Childhood. Fetal and Neonatal Edition Archive, 88, F492–F500.
Woodward, L. J., Anderson, P. J., Austin, N. C., Howard, K., & Inder, T. E. (2006). Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. The New England Journal of Medicine, 355, 685–694.
Yeh, T. F., Lin, Y. J., Lin, H. C., Huang, C. C., Hsieh, W. S., Lin, C. H., et al. (2004). Outcomes at school age after postnatal dexamethasone therapy for lung disease of prematurity. The New England Journal of Medicine, 350, 1304–1313.
Yoon, B. H., Jun, J. K., Romero, R., Park, K. H., Gomez, R., Choi, J. H., et al. (1997). Amniotic fluid inflammatory cytokines (interleukin-6, interleukin-1beta, and tumor necrosis factor-alpha), neonatal brain white matter lesions, and cerebral palsy. American Journal of Obstetrics and Gynecology, 177, 19–26.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no financial or other relationships that could be interpreted as a conflict of interest affecting this manuscript.
Rights and permissions
About this article
Cite this article
Baron, I.S., Rey-Casserly, C. Extremely Preterm Birth Outcome: A Review of Four Decades of Cognitive Research. Neuropsychol Rev 20, 430–452 (2010). https://doi.org/10.1007/s11065-010-9132-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-010-9132-z