Abstract
A wealth of evidence demonstrates that a prodromal period of Alzheimer’s disease (AD) exists for some years prior to the appearance of significant cognitive and functional declines required for the clinical diagnosis. This prodromal period of decline is characterized by a number of different neuropsychological and brain changes, and reliable identification of individuals prior to the development of significant clinical symptoms remains a top priority of research. In this review we provide an overview of those neuropsychological changes. In particular, we examine specific domains of cognition that appear to be negatively affected during the prodromal period of AD, and we review newer analytic strategies designed to examine cognitive asymmetries or discrepancies between higher-order cognitive functions versus fundamental skills. Finally, we provide a critical examination of the clinical concept of Mild Cognitive Impairment and offer suggestions for an increased focus on the impact of cerebrovascular disease (CVD) and CVD risk during the prodromal period of AD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The search for antecedent markers of Alzheimer’s disease (AD), whether clinical or biological, is predicated on the notion that significant neural dysfunction and cell death occurs well in advance of the clinical diagnosis. From a treatment perspective, it is imperative to reliably identify individuals during the disease prodrome (i.e., prior to the development of significant clinical symptoms) in order to have a maximum impact on cognitive function and quality of life. A wealth of studies has identified neuropsychological and neuroimaging changes in older adults during this prodromal period. The focus of much of this research has been on the study of higher risk groups (e.g., those of advanced age, termed the Very-Old; those with genetic susceptibility such as carriers of the apolipoprotein E epsilon-4 [APOE ɛ4] allele; and those with mild cognitive impairments but relatively normal daily function), as well as the prospective tracking of individuals who progress to AD over time.
In this review, we will highlight and discuss important neuropsychological differences by age and genetic risk in the expression of cognitive and brain changes during the clinical and prodromal periods of AD. For a more specific review of neuroimaging changes in the prodromal period of AD, we refer the reader to another recent critical review (see Wierenga and Bondi 2007). However, much remains to be done in characterizing the progression to AD in the Very-Old, and further clarification of the evolution of these brain and behavioral differences through the use of emerging neuropsychological (e.g., cognitive discrepancy measures) and neuroimaging (e.g., functional magnetic resonance imaging [fMRI]) techniques is needed. Critical examination of another risk factor for progression to AD, Mild Cognitive Impairment (MCI; Petersen et al. 1999), is also needed, given its recent definitional modifications (see Petersen and Morris 2005). We will argue in this review for more rigorous criteria and knowledge of clinical outcomes to better characterize MCI as a risk factor of AD. Finally, the oft-neglected impact of cerebrovascular disease (CVD) and CVD risk on the prodromal period of AD will also be discussed. Overall, this exciting area of research will undoubtedly continue to lead to better and more cost-effective methods for early detection as well as to provide a better understanding of the underlying brain substrata and risk factors related to the earliest cognitive declines in AD.
Clinical And Neuropathologic Features Of Alzheimer’s Disease
Alzheimer’s disease is a progressive and degenerative brain disease that results in dementia. Of the more than 70 known causes of dementia (Cummings and Benson 1992), AD is the most common and accounts for roughly half of all dementias. Alzheimer’s disease is characterized by brain atrophy and the microscopic appearance of diffuse and neuritic plaques and neurofibrillary tangles (Alzheimer 1907). These neuropathologic accumulations are thought to begin primarily in the medial temporal lobes (e.g., entorhinal cortex, hippocampus) and then progress to the association cortices of the temporal, parietal and frontal lobes (Braak and Braak 1991). Primary sensory and motor cortices, and most subcortical structures are relatively spared (see Fig. 1). Degeneration in the basal forebrain results in a major reduction of acetylcholine (Whitehouse et al. 1982). Consistent with these widespread neuropathologic changes, the primary clinical manifestation of AD is a progressive dementia syndrome that usually begins in later life. Typically, the dementia syndrome is characterized by prominent amnesia with additional deficits in language and semantic knowledge, executive functions, attention, and constructional and visuospatial abilities (Salmon and Bondi 1999). These cognitive deficits and the decline in everyday function they produce are the core features of the AD dementia syndrome.
Evolution of neurofibrillary tangle pathology as originally conceived by Braak and Braak (1991). Prior to the appearance of significant clinical symptoms, neurofibrillary changes begin to accumulate in entorhinal and transentorhinal cortex (stages I and II) and may appear surprisingly early in life (e.g., in one’s thirties or forties). Increasing involvement of the medial temporal lobe and surrounding association cortices are then thought to coincide with the appearance of mild clinical symptoms (stages III and IV), followed by clinically apparent Alzheimer’s disease and correspondingly severe involvement of medial temporal and cortical association areas (stages V and VI; adapted from Braak and Braak 1991, 1995; Braak et al. 1998)
Risk Factors
Advancing age is the single most important risk factor for AD, and the prevalence of the disease rises in an approximately exponential fashion between the ages of 65 and 85. With respect to the Oldest-Old (age 85 and above), the fastest growing segment of our population, prevalence rates for dementia are high, ranging between 40% and 60%. A number of studies suggest that women have a slightly greater risk for AD than men (Zhang et al. 1990), although the increased prevalence of AD in women may be attributable to differential survival after the onset of dementia due to their longer life expectancy. For example, although the Framingham study of AD showed about a 3:1 prevalence ratio of women to men with AD (Bachman et al. 1992), no gender difference was found in the incidence of dementia or AD (Bachman et al. 1993). However, more recent incidence rates from the Cache County epidemiological study of dementia, a study that includes the very old, reveal that the incidence among women increases after age 80 and exceeds the risk among men by more than twofold in late old age (Miech et al. 2002).
Regarding environmental factors, numerous epidemiological and biological studies show that higher education, occupational work complexity, as well as a mentally and socially integrated lifestyle in late life postpones the onset of clinical dementia and AD (see also Kawas and Katzman 1999; Fratiglioni and Wang 2007, for reviews). Long-term benefits of exercise and cardiorespiratory fitness on cognition have also been established, and clinical trials of fitness training interventions show a positive impact on cognition (Barnes et al. 2003). Indeed, physical activity has been shown to reduce the risk for dementia and improve cognition (see Kramer & Erickson 2007, for review). Moreover, head injury has been identified as an important risk factor for AD (Jellinger 2004). Specifically, the risk of AD is doubled for individuals with a history of a single head injury that led to loss of consciousness or hospitalization (Mortimer et al. 1991). Similarly, retired professional football players with histories of recurrent concussions show greater cognitive impairments in late life than do retired players without concussion histories (Guskiewicz et al. 2005).
With respect to genetic risk, AD development is increased by a positive family history in a first-degree relative (van Duijn et al. 1991), and specific point mutations on the amyloid precursor protein gene of chromosome 21 as well as presenilin gene mutations on chromosomes’ 1 and 14 are deterministic gene mutations for AD. In addition, the APOE ɛ4 allele located on chromosome 19 is over-represented in AD and has been identified as the single most important susceptibility gene for the disease (Corder et al. 1993; Saunders et al. 1993; Strittmatter et al. 1993). Gene-environment interactions may also be evident. For example, when Mayeux et al. (1995) examined the interaction between the APOE ɛ4 allele and head injury, they found a tenfold increase in the risk of developing AD in people with both risk factors. In high-exposure professional boxers, Jordan et al. (1997) also found that possession of an APOE ɛ4 allele was associated with increased severity of chronic neurologic deficits.
Our understanding of the risk factors for AD is growing rapidly and now includes not only those risk factors imparted in late life but also those present across the entire lifespan. For example, perinatal conditions, brain development, body growth, socioeconomic conditions, environmental enrichment, and cognitive reserve have all been suggested as early life factors that influence the onset of AD (see Borenstein et al. 2006). To summarize, the literature suggests that risk for AD is not likely to be determined in any single time period but results from a complex interplay between genetic and environmental exposures throughout one’s life (Borenstein et al. 2006).
Neuropsychological Characteristics of Alzheimer’s Disease
Profile of Cognitive Deficits in Early AD
Prior research has characterized the pattern of cognitive deficits typically associated with early AD and related those deficits to the severity and distribution of AD brain pathology (Salmon and Bondi 1999). Better understanding of the profile of neuropsychological deficits associated with early AD has resulted in earlier and more reliable clinical diagnosis (Salmon et al. 2002), and it has improved the ability to better detect the disease in persons who are in a prodromal phase of the disease before the manifestation of obvious clinical symptoms (Bondi et al. 1995, 1999; Jacobson et al. 2002; Lange et al. 2002; Mickes et al. 2007).
Although the progression of neuropathologic changes in AD are not fully known, studies are consistent with the notion that the hippocampus and entorhinal cortex are involved in the earliest stage, and that frontal, temporal and parietal cortices become increasingly involved as the disease progresses (Braak and Braak 1991; Brewer and Moghekar 2002). Consistent with this progression, numerous studies have shown that medial temporal lobe (MTL)-dependent episodic memory tasks are usually affected earliest in the disease and are quite effective in differentiating between very mildly demented patients with AD and normal older adults (Salmon and Bondi 1999). In the typical case, as AD progresses the dementia syndrome is characterized by a prominent amnesia with rapid forgetting of material, marked executive dysfunction, and additional deficits in certain aspects of language, visuospatial abilities, and attention.
Brain and Behavioral Profiles of AD in the Very-Old
Despite gains in our understanding of the profile of early AD, much of this work is based on the study of AD with relatively young groups (e.g., individuals below the age of 70 or 80) and thus our understanding of the early expression of AD in those who are over the age of 80 (Very-Old) is more limited. In part, this is due to the boundaries between normal age-related cognitive changes and early signs of AD being particularly difficult to delineate in the Very-Old. Many of the early structural and functional changes of AD overlap with changes observed in normal aging or in the context of other diseases. Because there are age-related declines in information processing speed, executive functions, and efficiency of learning and recall, some investigators suggest that less AD pathology may be needed to produce pathologic cognitive decline in the Very-Old compared to the Young-Old (Terry et al. 1999). Consequently, dementia may also be more difficult to detect against the background of declining and more variable cognitive scores (Allen et al. 2005) relative to the appropriate age-matched normal reference group. Because normal aging can detrimentally affect many of the same cognitive abilities affected by AD, the prominence of specific deficits related to AD may be much less evident in the Very-Old than in the Young-Old. This would result in a less distinct and somewhat atypical cognitive deficit profile associated with AD in the Very-Old compared to that of the Young-Old.
Our neuropsychological work suggests that the profile of deficits associated with AD in the Very-Old differs in the severity and pattern of test performance from that of the Young-Old with AD (Bondi et al. 2003). Specifically, we compared the profile of neuropsychological deficits associated with AD in Young-Old (mean age < 70) and Very-Old (mean age > 80) patients. Young-Old AD and Very-Old AD groups were comparable in education, gender, dementia severity, and disease duration, and they achieved comparable raw scores on all the neuropsychological measures. However, when scores were standardized in relation to their age-appropriate control groups, the Young-Old AD patients were generally more impaired than the Very-Old patients and showed a typical AD profile. That is, they demonstrated pronounced deficits in executive functions and the retention of episodic memories (i.e., savings scores) that were greater than their deficits in other cognitive domains. By contrast, the Very-Old AD patients showed a similar level of impairment across all cognitive domains so that their deficit profile lacked the disproportionate saliency of memory and executive function deficits typical of the disease. Without consideration of these profile distinctions by age, there is the potential for greater false negative diagnoses if the diagnostician expects comparably impaired levels of memory and executive function deficits in the Very-Old patient.
In addition to neuropsychological differences, a similar age-related decline and increased inter-individual variability occurs in MRI-derived measures of regional brain volumes (Jernigan et al. 2001; Raz and Rodrigue 2006) and thus decreases the sensitivity of these measures for detecting mild AD in the Very-Old. It is known that normal aging is associated with mild brain atrophy on structural magnetic resonance (MR) imaging (Jack et al. 1998; Jernigan et al. 2001; Pfefferbaum et al. 1994), decreased hemodynamic response on functional MR imaging (D’Esposito et al. 1999), reduced synaptic density (Masliah et al. 1993), and increased white matter abnormalities (Guttman et al. 1998; Jernigan et al. 2001; Salat et al. 1999). Thus, an increased focus on neuropsychological and neuroimaging studies of the Very-Old is needed to improve upon our understanding of the evolution of AD in this fastest growing segment of the population.
Neuropsychological Studies of the Prodromal Period of Alzheimer’s Disease
One of the most active areas of clinical research on AD is the attempt to identify cognitive changes that occur during the prodromal phase that precedes the manifestation of the overt dementia syndrome. Evidence consistently suggests that subtle declines in episodic memory in the older adult presages the development of the dementia syndrome associated with AD (Jacobs et al. 1995; Grober and Kawas 1997; Bondi et al. 1999; Collie and Maruff 2000; Smith et al. 2007). In addition, recent work also highlights that an episodic memory deficit need not be the only affected cognitive domain during the AD prodrome (see Twamley et al. 2006, for review), a finding also emphasized in recent re-characterizations of the concept of Mild Cognitive Impairment (Petersen and Morris 2005).
The ability to identify cognitive declines prior to overt dementia has led to the adoption of the designation Mild Cognitive Impairment (MCI; Petersen et al. 1999, 2001) for those with impaired performance on objective memory tests, but with intact general cognition and daily functioning. As Petersen and Morris (2005) more recently noted, MCI can be characterized more broadly in terms of the specific profile of impairment (e.g., amnestic vs. non-amnestic). The MCI condition (particularly the amnestic type) is a risk factor for the development of AD. Unfortunately, the practice of defining MCI is idiosyncratic and has varied widely across studies in the decade since its inception. Moreover, we have argued (see Twamley et al. 2006) that much of the literature’s formulations of MCI might well be re-cast as early AD but for the use of antiquated psychometric cutoffs (e.g., MMSE ≥ 24 constituting “preserved general cognitive function”; see Salmon et al. 2002) and poor cognitive and functional (e.g., activities of daily living) characterizations. Thus, more rigorous criteria and knowledge of clinical outcomes are needed to better characterize this risk factor. We will address this further in the section on MCI below.
Another approach to identifying potential cognitive markers of AD during its prodromal phase has been to compare the neuropsychological changes of nondemented older adults who have an increased risk for developing the disease to that of individuals who do not have an increased risk. This approach assumes that a group of individuals with the risk factor will be more likely than one without this factor to contain individuals who are in the prodromal phase of the disease. These prodromal AD subjects will contribute to poor group performance on those tests that are particularly sensitive to early AD pathology. Studies that have adopted this approach to the search for cognitive markers of early AD, for the most part, have focused on increased risk due to a positive history of AD in a first degree relative (e.g., mother, father, or sibling) or the presence of a genetic marker for the disease, most commonly the ɛ4 allele type of apolipoprotein E (APOE), a low density lipoprotein cholesterol carrier.
A number of studies have shown that nondemented older adults with a positive family history for AD perform significantly worse than those with a negative family history on tests of episodic memory (Bondi et al. 1994; Caselli et al. 2004; La Rue et al. 1992; Levy et al. 2004). Our neuropsychological studies have also demonstrated that nondemented older adults who are at risk for developing AD by virtue of the APOE ɛ4 allele perform more poorly than those without this risk factor on tests of episodic memory, and that episodic memory measures are more effective for differentiating between these groups than are other cognitive measures of executive functions, attention, constructional ability, or psychomotor speed (Bondi et al. 1995, 1999; Lange et al. 2002; Mickes et al. 2007). Our research group has also shown that risk groups and those who convert to AD might be better characterized in terms of cognitive discrepancies between pairs of tests (see below), rather than through traditional methods of analyzing overall group means on individual cognitive tasks (Jacobson et al. 2002, 2005a, b; Houston et al. 2005; Wetter et al. 2005, 2006).
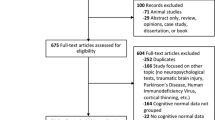
Reviews of the Prodromal Period of Alzheimer’s Disease
To better determine the neuropsychological and neuroimaging changes that may reflect prodromal AD, we critically reviewed these respective literatures (see Twamley et al. 2006; Wierenga and Bondi 2007). In doing so, we distinguished between prodromal AD and MCI. Whereas MCI has been traditionally defined as mild memory impairment without other cognitive or functional deficits, prodromal AD is conceptualized as a stage featuring subtle cognitive declines but not necessarily impairments—and not solely in the domain of memory—and no appreciable declines in daily functioning. Another distinction exists on autopsy where those with MCI may exhibit substantial AD pathology but prodromal AD patients may exhibit only minor changes (Bennett et al. 2006). In their review, Bäckman et al. (2005) found that neuropsychological tests of global cognition, delayed recall, perceptual speed, and executive functioning best discriminated subjects who developed AD from those who remained nondemented. However, of the 47 studies included in their meta-analysis, 27 investigated cognition in MCI, cognitively impaired, or memory clinic samples, thereby making memory measures the most likely to emerge as predictors of future AD. Our review (Twamley et al. 2006) excluded studies of subjects with MCI in favor of a more pure focus on prodromal AD. We systematically reviewed 91 studies of neuropsychological functioning, structural neuroimaging, or functional neuroimaging in prodromal AD. The neuropsychological studies indicated that prodromal AD is characterized by subtle deficits in a broad range of neuropsychological domains, particularly in learning and memory, executive functioning, processing speed, attention, and semantic knowledge. The neuroimaging research suggests that volume loss and cerebral blood flow or metabolic changes, particularly in the temporal lobe, may be detected before the onset of dementia. Thus, there exist several potential markers of a prodromal period of AD, in which specific cognitive and biomarker changes precede the clinical manifestations. Our reviews indicate that many possible cognitive domains and brain regions are susceptible in prodromal AD (and earlier than previously thought), and highlight the need for comprehensive measurement and integration of cognitive and brain changes in future studies.
Course of Cognitive Decline in Prodromal Alzheimer’s Disease
As is now evident, a subtle decline in episodic memory often occurs prior to the emergence of frank dementia (Bondi et al. 1999). The course of episodic memory change during the prodromal phase of AD has been the focus of a number of studies (Bäckman et al. 2001; Chen et al. 2001; Lange et al. 2002; Rubin et al. 1998; Small et al. 2000; Storandt et al. 2002). These studies suggest that memory performance may be poor but stable a number of years prior to the development of the dementia syndrome in those with AD, and then decline rapidly in the year or two immediately preceding the dementia diagnosis. For example, both Small et al. (2000) and Bäckman et al. (2001) found that episodic memory was mildly impaired 6 years prior to dementia onset, but changed little over the next 3 years. In contrast, Chen et al. (2001) and Lange et al. (2002) showed a significant and steady decline in episodic memory beginning about 2 to 3 years prior to the dementia diagnosis in individuals with prodromal AD. Taken together, findings suggest a plateau effect in the course of decline in episodic memory rather than a monotonic or linear course of decline. Such a plateau model (i.e., mild but stable episodic memory decline followed by more abrupt decline in the years proximal to diagnosis) was validated in a large-scale study by Smith et al. (2007) who found that a plateau was evident on tests of episodic memory but not for the other cognitive domains examined (see Fig. 2).
Linear versus plateau trajectories of episodic memory decline prior to a diagnosis of Alzheimer’s disease. The solid line (—) represents a linear trajectory of cognitive decline, whereas the dashed line (– –) represents individuals with an initial mild decline, then a period of stabilization, followed by a more abrupt decline in the year or two preceding an AD diagnosis. Evidence suggests that episodic memory may reflect a plateau model of decline, whereas other cognitive functions may not (adapted from Smith et al. 2007 and Twamley et al. 2006)
These results indicate that an abrupt decline in memory in an elderly individual might better predict the imminent onset of dementia than poor but stable memory ability. Also, the mild but stable episodic memory decrements in an early preclinical period, followed by more abrupt and severe declines during a late preclinical period, suggest the operation of compensatory brain changes in response to increasing neuropathologic encroachments. A variety of studies examining functional neuroimaging (Bookheimer et al. 2000; Bondi et al. 2005; Han et al. 2007), neurochemical (DeKosky et al. 2002) and neurotrophic (Durany et al. 2000; Egan et al. 2003) factors, support this notion.
Although the search for cognitive changes in prodromal AD has largely focused on episodic memory, several recent reviews and meta-analyses suggest that there is largely non-specific cognitive decline in the few years prior to a dementia diagnosis. Although a decline in episodic memory is consistently found in these studies, they also often reveal additional deficits in executive functions, perceptual speed, verbal ability, visuospatial skill, and attention during the prodromal phase of AD (Bäckman et al. 2005; Storandt et al. 2006; Twamley et al. 2006). This widespread decline in cognitive abilities mirrors evidence that multiple brain regions (e.g., medial and lateral temporal lobes, frontal lobes, anterior cingulate cortex) or connectivity between these regions are impaired in prodromal AD (Albert et al. 2001; Andrews-Hanna et al. 2007; Small et al. 2003) (see Table 1).
Consistent with this broader view, measures of semantic knowledge show significant declines during prodromal AD (Mickes et al. 2007; see also Cuetos et al. 2007; Powell et al. 2006), and this may be relatively independent of episodic memory deficits (Koenig et al. 2007). For example, Mickes et al. (2007) have shown in a detailed neuropsychological study of prodromal AD that both semantic memory and episodic memory functions declined rapidly in a 3-year period progressing to AD, whereas executive function deficits were not especially prominent (see Fig. 3). From these findings, the authors suggest that cognitive abilities thought to be subserved by the medial and lateral temporal lobes (episodic memory and semantic knowledge, respectively) may be substantially more impaired than cognitive functions subserved by the frontal lobes (executive functions). These findings map nicely onto the known neuropathologic encroachments of AD early on in the disease process (Braak and Braak 1991) and are also consistent with recent reports of decreased semantic access in nondemented APOE ɛ4 older adults (Rosen et al. 2005) and the ability of language tasks to predict pathologic AD 6 years later (Powell et al. 2006).
Control-referenced standard scores for prodromal AD patients on tests of episodic memory, semantic memory, and executive functions. Their neuropsychological profiles were examined 1 year (−1) and 2 years (−2) prior to the first year of their non-normal diagnosis (adapted from Mickes et al. 2007)
Cognitive Discrepancy Studies
The likelihood of a long prodromal period preceding the onset of AD is now well established. Although cognitive changes like those noted above appear to be the most common neuropsychological deficits prior to diagnosis, given the wide variability in domains initially affected it is unlikely that a single test or domain will be sufficient to accurately predict who will develop AD or to detect its earliest onset (Albert et al. 2007). A combination of methods that include a cognitive profile may prove more useful in defining a prodromal period in AD. Recent studies suggest that an asymmetric cognitive profile could improve our ability to characterize the earliest cognitive changes in AD.
Asymmetric cognitive profiles can capture relative intra-individual differences by comparing performance on dissimilar neuropsychological tests or domains such as verbal relative to visuospatial abilities. Infrequent or atypical performance discrepancies may signal a neurodegenerative process and are frequently used in both clinical and research settings to identify potential changes from premorbid levels of cognitive functioning (Dori and Chelune 2004; Lange and Chelune 2006; Wilde et al. 2001). Thus, asymmetric cognitive profiles may have utility for detecting a prodromal phase of AD for a number of reasons. Because AD has such a heterogeneous clinical presentation, there is a strong possibility that distinct cognitive subgroups exist within the larger at-risk population (Martin 1990). By averaging performance with a single test score across subjects, we may inadvertently obscure potential subgroups that exist within a larger group (Mitrushina et al. 1995). For example, an older adult subgroup with preserved verbal memory skills could mask the presence of a second subgroup with a subtle decline in verbal memory (see Demadura et al. 2001).
There is considerable evidence for cognitive asymmetry in the early stages of AD. EEG and SPECT studies show structural and functional asymmetries in early AD (Celsis et al. 1997). Studies using PET, MRI perfusion, and MRI morphometry also document increased left-right asymmetry associated with aging, cognitive decline, and early AD (Celsis et al. 1997; Small et al. 1995a, 1995b; Franceschi et al. 1995). Right versus left hemisphere reductions in glucose metabolism show correspondence with lateralized functional deficits in spatial and verbal skills, respectively (Haxby et al. 1985, 1990). Case studies describe unilateral neglect syndrome in AD patients and frequent asymmetric cerebral atrophy (Bugiani et al. 1991; Venneri et al. 1998). Interestingly, MRI brain morphometry studies suggest that a reduction of normal, structural asymmetry in hippocampal volume is a consequence of a neurodegenerative process in higher-risk older adults with APOE-ɛ4 genotype (Geroldi et al. 2000) and in older adults with increased cognitive dysfunction (Wolf et al. 2001). Bigler et al. (2002) found that, in general, significant hippocampal and parahippocampal asymmetries (i.e., greater volume in right versus left hemisphere) were associated with relatively more preserved cognitive functions in AD patients.
Many studies of asymmetric brain structure and function in early AD document lateralized cognitive changes with composite measures of language and visuospatial abilities. However, more detailed studies using cognitive neuroscience paradigms have further refined our knowledge of the component processes involved in cognitive asymmetry. Delis et al. (1992) suggested that the traditional verbal/spatial dichotomy could mask a more primary impairment in processing large, global forms relative to detailed, local stimuli. Subsequent studies using computerized global/local (Navon-type) visual stimuli identified specific impairments in disengaging and shifting attention (Filoteo et al. 1992) in early AD, possibly resulting from disconnection of posterior temporoparietal regions (Parasuraman et al. 1992).
Consequently, asymmetric cognitive profiles in early AD can be more discrete than a verbal/spatial dichotomy. For example, Cherry et al. (1996) proposed that the phonological loop and visuospatial scratchpad could be independently affected in AD, resulting in discrete deficits in auditory or visuospatial span, or discrepancies between memory span and supraspan ability (also see Collette et al. 1997). Although subgroups with relatively preserved “verbal” or “spatial” profiles have been confirmed in early stages of AD, a corresponding advantage does not always extend to more specific cognitive functions like verbal or visuospatial memory (Demadura et al. 2001) and may differ between genetic risk groups (Finton et al. 2003). Effects of handedness and motor asymmetry have also been documented in AD (Doody et al. 1999; Strite et al. 1997). Given this substantial evidence for cognitive asymmetry in the early stages of AD, it is likely that these profiles may exist in a more subtle form in a prodromal phase.
To directly investigate the possibility of cognitive asymmetry in a prodromal phase of AD, Jacobson et al. (2002) conducted a retrospective study of performance discrepancies between naming and visuoconstructive ability in cognitively intact, community dwelling older adults. A prodromal group was identified by a subsequent change in clinical diagnosis to AD approximately 2 years after the assessment. The control group consisted of age- and education-matched individuals with no subsequent cognitive decline (for a minimum of 4 years). Cognitive asymmetry was calculated as the difference (standardized-scores) between Boston Naming Test (BNT) and Block Design subtest (BD) scores. Although the groups showed comparable mean performance on the individual measures, an analysis of performance discrepancies revealed that the prodromal AD group had a significantly larger discrepancy between BNT and BD scores relative to those with no cognitive decline or change in diagnosis. Consistent with our predictions, the prodromal group had a significantly greater frequency of asymmetric profiles (greater than 1 SD discrepancy) compared to the control group (see Fig. 4).
Distribution of standard score differences between naming and visuospatial skills for each participant. Note that 50% of the prodromal AD patients demonstrated an asymmetry score greater than 1 SD, whereas only 25% of the normal control participants demonstrated an asymmetry 1 SD or more. (Adapted from Jacobson et al. 2002)
The stability of asymmetric cognitive profiles in the face of declining cognitive abilities has been questioned (Rasmusson and Brandt 1995). Many neuropsychological tests are subject to floor effects, and the probability of global cognitive decline would seem to predict decreasing frequency of asymmetric profiles over time. However, in a large sample of subjects with a range of cognitive deficits, distinct verbal and visuospatial subgroups were confirmed in mild through severe dementia severity levels based on neuropsychological deficits (Strite et al. 1997). Some models of normal aging suggest that reduction of functional asymmetry is a compensatory mechanism that preserves cognitive abilities (see Cabeza et al. 2002), rather than a sign of neurodegeneration. Other theories suggest that correlations between cognitive domains tend to be relatively symmetrical, and disruption of brain systems supporting cognition would actually increase measures of cognitive asymmetry (Andrews-Hanna et al. 2007). The debate surrounding “atypical” asymmetry is complicated by whether a given brain structure or function is symmetrical in normal, younger individuals without neurologic disease. Structural neuroimaging findings are also equivocal. Some investigations showing relatively little structural asymmetry in non-demented older adults (Mu et al. 1999; Raz et al. 2004), whereas other investigations using meta-analysis and multi-site legacy datasets confirm hippocampal asymmetry (right greater than left) in healthy older adults and possible reduction of asymmetry in prodromal AD (Pedraza et al. 2004; Fennema-Notestine et al. 2007).
To investigate the longitudinal course of cognitive asymmetry, Jacobson et al. (2002) examined six consecutive years of neuropsychological test scores for an individual in her eighties who ultimately received a clinical AD diagnosis. During the study period, however, she had intact learning and memory skills and no initial evidence of overall cognitive or functional decline. Cognitive asymmetry was examined with a discrepancy-score method, calculating age-adjusted z-score differences between opposing verbal and spatial tasks. Over 6 years, a pattern of increasing cognitive asymmetry was apparent with relatively preserved performance on non-verbal/visuospatial tests relative to declining scores on verbally mediated tasks (see Fig. 5). Her neuropsychological test scores revealed significant cognitive discrepancies on four verbal/spatial contrasts (tasks of memory, fluency, attention/memory span, naming/visuoconstruction) for all six assessments even while her individual test scores remained within normal limits for her age. In addition, there were significant discrepancies between higher-level cognitive skills and baseline skills (e.g., letter number sequencing/shifting relative to simple sequencing). Results from this case study (Jacobson et al. 2002) suggest that cognitive discrepancies can be a sensitive marker of prodromal neuropsychological changes, and they are apparent prior to changes in either memory or overall cognitive ability.
Six consecutive years of scores of an individual who progressed to a clinical diagnosis of AD at year 7. The graph depicts the discrepancy between verbal and visual recall measures (solid line), and the discrepancy between tests of naming and visuospatial skills (dashed line). Note the general increase in discrepancies between measures over time (adapted from Jacobson et al. 2002)
Other work in this area has focused on differences in cognitive discrepancies between genetic risk groups. Although only a subgroup of individuals who carry the APOE-ɛ4 allele go on to develop AD, this genotype has often served as a possible surrogate marker for prodromal AD when evaluating asymmetric cognitive profiles. For example, cognitively intact older adults with and without the APOE-ɛ4 allele were administered verbal and spatial tasks of working memory and attention span (Jacobson et al. 2005a). The APOE-ɛ4 genotype group showed significantly increased cognitive discrepancies between verbal and spatial attention span relative to the non-ɛ4 group despite comparable mean performance on the individual span tasks. In a follow-up study by Jacobson et al. (2005b), hierarchical (global/local) visual stimuli with documented sensitivity to lateralized hemispheric dysfunction (Delis et al. 1988) were used to investigate cognitive asymmetry. Despite similar levels of overall recall ability in normal elderly APOE-ɛ4 and non-ɛ4 groups, the APOE-ɛ4 group showed a significantly larger discrepancy between recall of global relative to local components. Houston et al. (2005) also found larger cognitive discrepancies in a normal elderly APOE-ɛ4 group compared to a non-ɛ4 group, but only when contrasting performance on a switching condition with baseline skills of verbal versus design fluency (Delis-Kaplan Executive Function Scale [D-KEFS]; Delis and Kaplan 2001). In addition, Wetter et al. (2005) found that, compared to non-ɛ4 elderly, the cognitively intact APOE-ɛ4 elderly group showed increased error-rate variance on a higher-level Stroop switching condition relative to baseline conditions. Wetter et al. (2006) also used a cognitive discrepancy approach to identify evidence of greater heterogeneity of variance in a non-demented APOE-ɛ4 group relative to a non-ɛ4 group on complex verbal memory measures, but not on fundamental verbal skills such as vocabulary.
Overall, recurring findings of structural and functional asymmetry in early AD have led to the confirmation of asymmetric cognitive profiles in a prodromal phase of the disease, as well as in cognitively intact older adults at genetic risk for AD. It is not yet clear whether these functional asymmetries reflect compensatory responses to aging, specific neuroanatomic changes related to the neurodegenerative process, or a more general loss of functional connectivity between brain regions. Nevertheless, it is evident that cognitive asymmetries are not restricted to verbal/spatial deficits but may include discrepancies between complex cognitive abilities and more basic skills, or discrepancies between component processes within a single domain. There is a growing consensus that accurate detection of prodromal AD may require combinations of neuropsychological tests and cognitive profiles, and the presence of atypical functional asymmetries could contribute to our ability to identify AD at its earliest stages.
Mild Cognitive Impairment
Another relevant concept related to the prodrome of AD is that of Mild Cognitive Impairment (MCI; Petersen et al. 1999; Petersen and Morris 2005). Although the definition of MCI has evolved considerably over time, MCI has generally been conceptualized as a transitional stage between normal aging and dementia. Individuals with MCI have an increased risk of future dementia, although it is not clear that all individuals with MCI will progress to dementia (Fisk and Rockwood 2005). As originally proposed by Petersen et al. (1999), MCI was characterized primarily as an amnestic disorder that represented a borderland between normal aging and AD. Criteria included a memory complaint corroborated by an informant, evidence of objective memory impairment, preservation of general cognitive functioning (commonly defined as an MMSE score at or above 24), and intact activities of daily living, all in the absence of dementia (Petersen et al. 2001). More recently, broader conceptualizations of MCI have emerged that encompass cognitive domains other than memory (Petersen and Morris 2005). These characterizations delineate clinical subtypes that include amnestic and non-amnestic forms and that involve single and multiple cognitive domains (Manly et al. 2005; Tabert et al. 2006). With the advent of these broader classification schemes, diagnostic challenges related to MCI have increased, and neuropsychological assessment will increasingly play a prominent role in resolving these challenges.
The lack of a universally accepted approach to the objective identification of cognitive impairment has likely played a pivotal role in inconsistencies in the literature with respect to prevalence rates of MCI, rates of progression from MCI to dementia, and general lack of stability of the diagnosis over time. Demonstration of objective neuropsychological impairment in the classification of MCI is perhaps the most variable and ill-defined component of the diagnosis (Portet et al. 2006). The application of a wide-range of conceptual and diagnostic approaches to MCI have led to highly variable prevalence rates ranging from 1–30%, and annual rates of conversion from MCI to dementia that vary drastically from 1–72% (Tuokko and McDowell 2006). There is also some concern over the apparent instability of the MCI diagnosis. For example, those who are diagnosed with MCI appear to revert back to normalcy at subsequent assessments in 10–40% of cases (Bickel et al. 2006; Petersen 2004). The instability of the diagnosis may be a function of MCI subtype, as one recent study showed that those classified as single domain MCI improved in more than 50% of cases, whereas those classified as multi-domain MCI improved in only 12% of cases (Bickel et al. 2006).
Diagnostic instability is also likely to be related to the use of cognitive test procedures that are not sufficient to reliably identify memory impairment or deficits broadly across other cognitive abilities. As an initial step in identifying MCI, evidence of preserved general cognition has commonly been based solely on an MMSE score of 24 or above and/or a Clinical Dementia Rating (CDR) of 0.5 (Hirao et al. 2006; DeCarli et al. 2001; Zanetti et al. 2006), although some groups incorporate clinical judgment into determinations (Grundman et al. 2004). These often-used MMSE criteria are problematic because the traditional MMSE cutoff score of 24 and below appears to be rather conservative. For example, individuals with MMSE scores greater than 24 are accurately diagnosed with AD (see Salmon et al. 2002). Also, MMSE scores do not consistently predict dementia (Tian et al. 2003), and MMSE scores are prone to regression to the mean and practice effects (Hensel et al. 2007). Similarly, use of the CDR, a disease severity rating scale, not a diagnostic measure, has limited utility in providing an operational definition for MCI, as a CDR of 0.5 may be indicative of either MCI or mild AD (Petersen 2004).
Another challenge to the neuropsychological contribution to identification of MCI is the level of performance to choose for the criterion of “objective impairment”. In the original criteria for MCI, now more specifically identified as amnestic MCI (aMCI), memory impairment was operationally defined as performance falling more than 1.5 standard deviations (SD) below the mean of age-matched normal elderly on tests of memory (see Tuokko et al. 2006, for discussion). Other researchers have utilized different cutoffs for what is considered impairment, ranging from 1 SD (Busse et al. 2006) to 1.96 SD (Bickel et al. 2006), or have suggested different cutoffs for different MCI subtypes (Zanetti et al. 2006). The use of clinical judgment of memory impairment informed by psychometrics has also been advocated (Smith et al. 2006; Heaton et al. 1991, 2004).
There is also limited consensus within the literature on what cognitive domains should be assessed when determining the presence or absence of MCI. Most studies of MCI have used verbal recall measures to document objective memory impairment (Tuokko et al. 2006). Specifically, the use of paragraph recall as the objective memory impairment measure has historically been the norm in identifying and tracking amnestic MCI (Grundman et al. 2004). However, investigators taking a broader view of memory have used both verbal and non-verbal memory tests (Kryscio et al. 2006; Larrieu et al. 2002) and have shown that a sizeable minority of aMCI cases are likely to be missed if visual memory is not examined (Alladi et al. 2006). Failing to fully examine cognitive domains other than memory has also likely led to improper characterization of so-called aMCI samples (Kramer et al. 2006). An isolated amnestic presentation in many early studies of MCI was not always clear or accurate given that memory was the only cognitive domain formally assessed.
Employing larger neuropsychological test batteries that formally assess multiple cognitive domains has been more helpful in determining preserved general cognition as well as in providing evidence of impaired performance in isolated cognitive domains. Unfortunately, many of these batteries may still lack rigor because many have defined impairment as a deficit (e.g., 1.5 SD below age-appropriate norms) on only one test in a particular domain (Tabert et al. 2006; Lopez et al. 2006). Inaccurate identification of MCI subtypes due to an insufficient evaluation is of significant concern as it has become clear that subtypes differ in diagnostic outcome and likelihood of conversion to AD (Busse et al. 2006; Yaffe et al. 2006). For example, Busse et al. (2006) have shown that non-amnestic multi-domain MCI is more likely to convert to a non-AD dementia than amnestic subtypes, and the single domain non-amnestic MCI is the most likely to revert back to normalcy.
Relying on more than one test within a cognitive domain to determine the presence or absence of “objective impairment” has not been the norm in MCI studies, despite the fact that it follows more closely with clinical decision-making processes. That is, clinicians typically examine multiple scores within a cognitive domain and base decisions on consistency of findings and patterns of impairment rather than isolated deficit scores. Our own recent work (Jak et al., unpublished) indicates that varying the number of neuropsychological measures used to determine objective impairment or the cutoffs used to define mildly impaired cognition in older adults can alter MCI classification rates substantially. Diagnoses of MCI ranged from 11–44% in a sample of non-demented older adults depending on which of three different operational definitions to determining objective cognitive impairment were employed.
Neuropsychological assessment is heavily relied upon both clinically and in research to contribute to identifying mild cognitive impairment and differentiating it from normal cognition and dementia. The literature to date demonstrates that varying the components of the objective cognitive assessment can significantly impact MCI case determination. Because there are no “gold standard” operational criteria for the cognitive component of the diagnosis for MCI, it is impossible to determine with certainty which diagnostic strategy is the most valid or has the highest sensitivity or specificity. Nonetheless, when examining the literature, it is important to bear in mind the vast range of criteria used to identify cognitive impairment in making the MCI diagnosis. Additionally, using comprehensive neuropsychological assessment when diagnosing MCI subtypes improves the stability and reliability of the diagnosis. Certainly, with the advent of identifying clinical subtypes of MCI, neuropsychological assessments that encompass more than memory and a global screening measure have become a requirement, not a suggestion.
Vascular Contributions to Alzheimer’s Disease and its Prodrome
The role of vascular risk factors such as stroke, heart disease, and hypertension in the development of cognitive impairments and vascular dementia (VaD) has been well established. By definition, vascular conditions are associated with VaD, and in general the relationship between various vascular risk factors and subsequent VaD are typically additive in nature (Hayden et al. 2006; Kivipelto et al. 2005). In contrast to VaD, the role of vascular risk factors in the development and progression of AD is much less clear, and historically there has been considerable debate and controversy surrounding this issue. For more than three decades AD has been characterized as primarily a neurodegenerative disorder with little to no vascular underpinnings (Blessed et al. 1968; American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 4th edition [DSM-IV]). However, within recent years, studies investigating the relationship between vascular risk and AD have burgeoned dramatically. Although the debate is certainly not a new one (see de la Torre 2002, for review), the pathophysiological links between vascular disease and AD is widely acknowledged and, increasingly, vascular risk factors are being implicated in the pathogenesis of MCI and AD.
There is a growing body of research to suggest that the relationship between vascular disease and AD is more complex than previously believed. For example, vascular risk factors have been associated with cerebral atrophy (Swan et al. 2000), and it has been suggested that brain atrophy can result from an ischemic process (Mentis et al. 1994). In addition, population-based postmortem studies have shown that the incidence of “pure” AD is much lower than once thought, perhaps below 50% (Snowdon et al. 1997; Etiene et al. 1998), although others suggest that significant vascular contributions are present in about 30–40% of AD cases (Knopman et al. 2001). Moreover, it is striking that, at autopsy, the vast majority of patients with AD demonstrate microvascular degeneration, and roughly a third of AD patients show frank stroke (Helbecque and Amouyel 2004). Finally, studies have shown that white matter lesion pathology appears to be associated with AD (Barber et al. 2000; Hirono et al. 2000), vascular factors predict rate of progression in AD (Mielke et al. 2007), and we have shown a particularly strong relationship between white matter lesions and MCI-related cognitive dysfunction (Delano-Wood et al. 2008). Given little clarity in the pathogenesis and treatment of AD, research has begun to focus more heavily on the identification of risk factors to both elucidate the pathophysiology of AD and provide new potential avenues for its prevention and treatment. With regard to the latter, vascular risk factors are quite modifiable and treatable (Bowler and Hachinski 2003), and thus it is plausible that secondary prevention of vascular risk factors may be helpful in delaying disease onset or progression in AD. Indeed, postponing the onset of clinical AD by 5 years would lead to a decrease in the prevalence of the disease by an astounding 50% (Brookmeyer et al. 1998).
Within the past decade, numerous population-based longitudinal studies have demonstrated links between several vascular factors and increased risk for the development of AD, including atherosclerosis (Hofman et al. 1997), atrial fibrillation (Ott et al. 1997), diabetes (Ott et al. 1999), hyperlipidemia (Jick et al. 2000), and stroke (Honig et al. 2003). Particularly strong longitudinal associations have been found between elevated blood pressure in midlife and higher risk for the development of AD in later life (Launer et al. 2000). Interestingly, Petrovich et al. (2000) showed that hypertension measured in midlife was related to significantly greater AD neuropathology (e.g., higher density of hippocampal neurofibrillary tangles) almost four decades later. Similarly, hypertension has been shown to be related to an increased risk for MCI, and this risk appears to be as strong as that imparted by the presence of the APOE ɛ4 genotype (DeCarli et al. 2001; Margaglione et al. 1998). Among the vascular risk factors, diabetes appears to provide strong evidence for a direct role in AD (Luchsinger and Mayeux 2004; Luchsinger et al. 2004, 2007) given its relationship to both cerebrovascular disease and hyperinsulinemia, which is thought to impair ß-amyloid clearance in the brain (Farris et al. 2003, 2004).
The possibility that reduced cerebral perfusion may be a marker for early AD is a current focus of investigation as well. In MCI patients who later progressed to AD, for example, hypoperfusion has been identified in several brain regions, including the temporoparietal cortex (Kogure et al. 2000), hippocampal and parahippocampal regions (Okamura et al. 2000), and the posterior cingulate (Rodriguez et al. 2000). Often a direct result of lowered cerebral perfusion, PET imaging studies have shown reduced cerebral glucose metabolism in the hippocampus of MCI patients (De Santi et al. 2001; Arnaiz et al. 2001). Similarly, this association has been detected in normally aging older adults who later converted to MCI (de Leon et al. 2001). Bangen et al. (2007) have also shown robust associations between resting cerebral blood flow in the medial temporal lobe and CVD risk in cognitively intact healthy older adults. Silvestrini et al. (2006) have also demonstrated that altered cerebrovascular hemodynamics (i.e., elevated cerebral vasomotor reactivity to hypercapnia) was associated with hastened cognitive decline in AD patients over 1 year. Indeed, although much research is required to enhance our understanding of the pathogenesis and pathophysiology of AD, the use of advanced neuroimaging techniques has shown promise in helping to reliably detect prodromal clinical features predictive of AD-related cognitive losses.
The interplay between vascular disease and AD neurodegenerative pathology is unclear, although many theories have been put forth touting a relationship. Perhaps the most commonly held view is that vascular pathology may exert an additive effect on the brain, increasing the overall burden of pathology as well as the rate of AD progression. In support of this theory, studies have shown that AD patients with concomitant stroke demonstrate more severe dementia (Snowdon et al. 1997; Honig et al. 2003), and the risk appears to be highest for those with other established vascular risk factors (e.g., hypertension, diabetes, heart disease; Honig et al. 2003; Luchsinger et al. 2005). Given brain tissue necrosis associated with stroke, Honig et al. (2003) suggested that this theory explains why a lesser amount of AD-related neuropathologic change may be necessary to produce dementia in patients who have suffered stroke. Another study supporting the vascular additive effects model showed that patients with low vascular risk do not decline cognitively or functionally over an 18-month period, whereas those with higher vascular burden demonstrate significantly greater AD-associated deterioration (Regan et al. 2006). The authors concluded that, although vascular risk factors are likely not part of the underlying etiologic process of AD, they contribute to the expression of the disease process in its very early stages.
A related prevalent theory states that pathogenic factors of AD and vascular disease may interact to produce synergistic effects on the brain and thus increase the likelihood of expressing cognitive impairment (Iadecola and Gorelick 2003; Bowler 2003; Chui et al. 2006). Proponents of this view argue that accumulation of ß-amyloid (an important mechanism implicated in neurodegeneration) may be both the cause and the consequence of cerebrovascular impairment. Indeed, as stated earlier, vascular risk factors have been shown to be associated with cerebral atrophy (Swan et al. 2000). In addition, animal studies have demonstrated that elevated cholesterol intake increases the deposition of ß-amyloid in the brains of transgenic mice expressing human amyloid precursor protein (Refolo et al. 2000). However, others argue that, at least in the case of stroke, only an additive effect on neurodegeneration appears to exist (Schneider et al. 2004; Silvestrini et al. 2006).
Some investigators have posited that a cerebrovascular component is seen in some AD brains as a consequence of incorrect diagnosis. For instance, these associations may stem from a misclassification of VaD as AD. Alternatively, given that vascular disease and AD pathology appears to exist co-morbidly in many cases, it has been argued that “mixed dementia” represents a separate clinical entity from that of “pure” dementia forms in which only neurodegeneration (AD) or cerebrovascular disease (VaD) are present. However, a number of studies show that vascular risk factors such as atherosclerosis, cardiac disease, and diabetes appear to be involved in progression to VaD just as often as AD (Breteler 1998, 2000; Ott et al. 1998, 1999; Tyas et al. 2001; Polvikoski et al. 2001).
Perhaps the most provocative and controversial theory holds that AD may itself be considered a vascular disorder. Along this vein, de la Torre (2002) put forth the term “vasculopathic complex” to describe how vascular-related factors negatively impact cerebral perfusion to a “critical level of dysfunction” (pg. 1157). de la Torre (2002) argues that there is mounting evidence to support this contention, including the observation that (1) epidemiological studies have demonstrated that known risk factors for AD have a vascular basis; (2) shared risk factors exist for both AD and VaD (e.g., APOE); (3) medications used to slow the development of AD improve cerebral perfusion; (4) regional cerebral perfusion deficits can predict preclinical AD; (5) there is often similar clinical symptomatology in AD and VaD; (6) cerebrovascular pathological lesions frequently overlap in AD and VaD; and (7) cerebral hypoperfusion may precede AD-related hypometabolic, neuropsychological, and neurodegenerative pathology. Clearly, additional research is needed to better characterize the cascade of neuropathologic events that precede and promote the development of AD.
Given the expected continued growth of the aging population, the prevalence of AD is projected to grow to 14 million or more by 2050 (Brookmeyer et al. 1998). Because of the possibility that vascular risk factors may increase the risk and promote the development of the disease process, greater emphasis is being placed on the detection of early, preclinical features that may be predictive of AD-related changes. Future work is needed to help elucidate whether vascular disease exerts an additive or synergistic effect with respect to AD, or whether vascular pathology is itself intrinsic to the pathogenesis of AD. Identification of the etiologic mechanisms underlying this disorder will greatly help delineate the pathophysiological underpinnings responsible for progressive cognitive and functional decline.
Summary
The identification of prodromal neuropsychological markers of Alzheimer’s disease is predicated on the notion that significant neural losses accrue well in advance of the clinical diagnosis. It is important that we reliably identify individuals while in this early stage of disease expression in order to treat them during a period that will have maximal impact in maintaining cognitive and functional abilities. The early diagnosis of AD in a prodromal stage remains an extremely important goal given the likelihood that this stage will be amenable to treatments designed either to halt or slow disease progression or treat cerebrovascular disease, if present. To identify and verify the accuracy of subtle neuropsychological abnormalities (e.g., poor delayed recall, cognitive asymmetry) in those non-demented older adults who are destined to develop dementia in the relatively near future will help maximize intervention efforts and ultimately preserve quality of life. Finally, the characterization of MCI and its subtypes will require better reliability and standardization of methods if it is to improve its applicability for accurate identification of the AD prodrome.
References
Albert, M., Blacker, D., Moss, M. B., Tanzi, R., & McArdle, J. J. (2007). Longitudinal change in cognitive performance among individuals with mild cognitive impairment. Neuropsychology, 21, 158–169.
Albert, M. S., Moss, M. B., Tanzi, R., & Jones, K. (2001). Preclinical prediction of AD using neuropsychological tests. Journal of the International Neuropsychological Society, 7, 631–639.
Alladi, S., Arnold, R., Mitchell, J., Nestor, P. J., & Hodges, J. R. (2006). Mild cognitive impairment: applicability of research criteria in a memory clinic and characterization of cognitive profile. Psychological Medicine, 36(4), 1–9.
Allen, J. S., Bruss, J., & Damasio, H. (2005). The aging brain: the cognitive reserve hypothesis and hominid evolution. American journal of human biology, 17(6), 673–689.
Alzheimer, A. (1907). Über eine eigenartige Erkrankung der Hirnrinde. Allgemeine Zeitschrift fuÉr Psychiatrie und psychisch-gerichtliche Medizin, 64, 146–148.
Andrews-Hanna, J. R., Snyder, A. Z., Vincent, J. L., et al. (2007). Disruption of large-scale brain systems in advanced aging. Neuron, 56, 924–935.
Arnaiz, E., Jelic, V., Almkvist, O., et al. (2001). Impaired cerebral glucose metabolism and cognitive functioning predict deterioration in mild cognitive impairment. Neuroreport, 12, 851–855.
Bachman, D. L., Wolf, P. A., Linn, R., Knoefel, J. E., Cobb, J. L., Belanger, A. J., et al. (1992). Prevalence of dementia and probable senile dementia of the Alzheimer type in the Framingham study. Neurology, 42, 115–119.
Bachman, D. L., Wolf, P. A., Linn, R., Knoefel, J. E., Cobb, J. L., Belanger, A. J., et al. (1993). Incidence of dementia and probable Alzheimer’s disease in a general population: The Framingham study. Neurology, 43, 515–519.
Bäckman, L., Small, B. J., & Fratiglioni, L. (2001). Stability of the preclinical episodic memory deficit in Alzheimer’s disease. Brain, 124, 96–102.
Bäckman, L., Jones, S., Berger, A., Laukka, E. J., & Small, B. J. (2005). Cognitive impairment in preclinical Alzheimer’s disease: A meta-analysis. Neuropsychology, 19, 520–531.
Bangen, K. J., Restom, K., Liu, T. T., Jak, A. J., Perthen, J. E., Wierenga, C. E., et al. (2007). Differential age effects on cerebral blood flow and BOLD response to encoding: Associations with cognition and stroke risk. Neurobiology of Aging (in press) DOI 10.1016/j.neurobiolaging.2007.11.012.
Barber, R., Gholkar, A., Scheltens, P., et al. (2000). MRI volumetric correlates of white matter lesions in dementia with Lewy bodies and Alzheimer’s disease. International Journal of Geriatric Psychiatry, 15(10), 911–916.
Barnes, D. E., Yaffe, K., Satariano, W. A., & Tager, I. B. (2003). A longitudinal study of cardiorespiratory fitness and cognitive function in healthy older adults. Journal of the American Geriatrics Society, 51(4), 459–465.
Bennett, D. A., Schneider, J. A., Arvanitakis, Z., Kelly, J. F., Aggarwal, N. T., Shah, R. C., et al. (2006). Neuropathology of older persons without cognitive impairment from two community-based studies. Neurology, 66(12), 1837–1844.
Bickel, H., Mösch, E., Seigerschmidt, E., Siemen, M., & Förstl, H. (2006). Prevalence and persistence of mild cognitive impairment among elderly patients in general hospitals. Dementia and Geriatric Cognitive Disorders, 21(4), 242–250.
Bigler, E. D., Tate, D. F., Miller, M. J., et al. (2002). Dementia, asymmetry of temporal lobe structures, and Apolipoprotein E genotype: Relationships to cerebral atrophy and neuropsychological impairment. Journal of the International Neuropsychological Society, 8, 925–933.
Blessed, G., Tomlinson, B. E., & Roth, M. (1968). The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. British journal of psychiatry, 114, 797–811.
Bondi, M. W., Houston, W. W., Eyler, L. T., & Brown, G. G. (2005). FMRI evidence of compensatory mechanisms in older adults at genetic risk for Alzheimer’s disease. Neurology, 64, 501–508.
Bondi, M. W., Houston, W. S., Salmon, D. P., Corey-Bloom, J., Katzman, R., Thal, L. J., et al. (2003). Neuropsychological deficits associated with Alzheimer’s disease in the very old: Discrepancies in raw vs. standardized scores. Journal of the International Neuropsychological Society, 9, 783–795.
Bondi, M. W., Monsch, A. U., Galasko, D., Butters, N., Salmon, D. P., & Delis, D. C. (1994). Preclinical cognitive markers of dementia of the Alzheimer type. Neuropsychology, 8, 374–384.
Bondi, M. W., Salmon, D. P., Galasko, D., Thomas, R. G., & Thal, L. J. (1999). Neuropsychological function and apolipoprotein E genotype in the preclinical detection of Alzheimer's disease. Psychology & Aging, 14, 295–303.
Bondi, M. W., Salmon, D. P., Monsch, A. U., Galasko, D., Butters, N., Klauber, M. R., et al. (1995). Episodic memory changes are associated with the ApoE-e4 allele in nondemented older adults. Neurology, 45, 2203–2206.
Bookheimer, S. Y., Strojwas, M. H., Cohen, M. S., Saunders, A. M., Pericak-Vance, M. A., Mazziotta, J. C., et al. (2000). Patterns of brain activation in people at risk for Alzheimer’s disease. New England journal of medicine, 343, 450–456.
Borenstein, A. R., Copenhaver, C. I., & Mortimer, J. A. (2006). Early-life risk factors for Alzheimer disease. Alzheimer disease and associated disorders, 20, 63–72.
Bowler, J. (2003). Epidemiology: Identifying vascular cognitive impairment. International psychogeriatrics, 15(Suppl1), 115–122.
Bowler, J. V., & Hachinski, V. (2003). Vascular Cognitive Impairment. Oxford, UK: Oxford University Press.
Braak, H., & Braak, E. (1991). Neuropathological staging of Alzheimer-related changes. Acta Neuropathologica, 82, 239–259.
Braak, H., & Braak, E. (1995). Staging of Alzheimer’s disease-related neurofibrillary changes. Neurobiol Aging, 16, 15–31.
Braak, H., Braak, E., Bohl, J., & Bratzke, H. (1998). Evolution of Alzheimer’s disease related cortical lesions. Journal of neural transmission, (Supplement), 54, 97–106.
Breteler, M. M. (1998). Epidemiological evidence of a connection between Alzheimer’s disease and vascular dementia. Neurobiol Aging, 19(Suppl 4), S150.
Breteler, M. M. (2000). Vascular involvement in cognitive decline and dementia: epidemiologic evidence from the Rotterdam Study and the Rotterdam Scan Study. Annals of the New York Academy of Sciences, 903, 457–465.
Brewer, J. B., & Moghekar, A. (2002). Imaging the medial temporal lobe: exploring new dimensions. Trends in cognitive sciences, 6, 217–223.
Brookmeyer, R., Gray, S., & Kawas, C. (1998). Projections of Alzheimer’s disease in the United States and the public health impact of delaying disease onset. American journal of public health, 88(9), 1337–1342.
Bugiani, O., Constantinidis, J., Ghetti, B., Bouras, C., & Tagliavini, F. (1991). Asymmetrical cerebral atrophy in Alzheimer’s disease. Clinical Neuropathology, 10, 55–60.
Busse, A., Hensel, A., Guhne, U., Angermeyer, M. C., & Riedel-Heller, S. G. (2006). Mild cognitive impairment: Long-term course of four clinical subtypes. Neurology, 67(12), 2176–2185.
Cabeza, R., Anderson, N. D., Locantore, J. K., & McIntosh, A. R. (2002). Aging gracefully: compensatory brain activity in high-performing older adults. Neuroimage, 17, 1394–1402.
Caselli, R. J., Reiman, E. M., Osborne, J. G., et al. (2004). Longitudinal changes in cognition and behavior in asymptomatic carriers of the APOE e4 allele. Neurology, 62, 1990–1995.
Celsis, P., Agniel, A., Cardebat, D., Demonet, J. F., Ousset, P. J., & Puel, M. (1997). Age related cognitive decline: a clinical entity? A longitudinal study of cerebral blood flow and memory performance. Journal of Neurology, Neurosurgery and Psychiatry, 62, 601–608.
Chen, P., Ratcliff, G., Belle, S. H., Cauley, J. A., DeKosky, S. T., & Ganguli, M. (2001). Patterns of cognitive decline in presymptomatic Alzheimer disease: A prospective community study. Archives of general psychiatry, 58, 853–858.
Cherry, B. J., Buckwalter, J. G., & Henderson, V. W. (1996). Memory span procedures in Alzheimer’s disease. Neuropsychology, 10, 286–293.
Chui, H. C., Zarow, C., Mack, W. J., et al. (2006). Cognitive impact of subcortical vascular and Alzheimer’s disease pathology. Annals of neurology, 60(6), 677–687.
Collette, F., Salmon, E., Van der Linden, M., Degueldre, C., & Franck, G. (1997). Functional anatomy of verbal and visuospatial span tasks in Alzheimer’s disease. Human brain mapping, 5, 110–118.
Collie, A., & Maruff, P. (2000). The neuropsychology of preclinical Alzheimer’s disease and mild cognitive impairment. Neuroscience and Biobehavioral Reviews, 24, 365–374.
Corder, E. H., Saunders, A. M., Strittmatter, W. J., et al. (1993). Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science, 261, 921–923.
Cuetos, R., Arango-Lasprilla, J. C., Uribe, C., Valencia, C., & Lopera, F. (2007). Linguistic changes in verbal expression: A preclinical marker of Alzheimer’s disease. Journal of the International Neuropsychological Society, 13, 433–439.
Cummings, J. L., & Benson, D. F. (1992). Dementia: A clinical approach (2nd ed.). Boston: Butterworth-Heinemann.
DeCarli, C., Miller, B. L., Swan, G. E., Reed, T., Wolf, P. A., & Carmelli, D. (2001). Cerebrovascular and brain morphologic correlates of Mild Cognitive Impairment in the National Heart, Lung, and Blood Institute Twin Study. Archives of neurology, 58(4), 643–647.
DeKosky, S. T., Ikonomovic, M. D., Styren, S. D., Beckett, L., Wisniewski, S., Bennett, D. A., et al. (2002). Up regulation of choline acetyltransferase activity in hippocampus and frontal cortex of elderly subjects with mild cognitive impairment. Annals of neurology, 51, 145–155.
Delano-Wood, L., Abeles, N., Sacco, J., et al. (2008). Regional white matter pathology in mild cognitive impairment: Differential influence of lesion type on neuropsychological functioning. Stroke (in press).
de la Torre, J. C. (2002). Alzheimer disease as a vascular disorder: Nosological evidence. Stroke, 33(4), 1152–1162.
Delis, D., & Kaplan, E. (2001). Manual for the Delis-Kaplan Executive Function System. San Antonio: Psychological Corporation.
Delis, D. C., Kiefner, M. G., & Fridlund, A. J. (1988). Visuospatial dysfunction following unilateral brain damage: Dissociations in hierarchical hemispatial analysis. Journal of Clinical & Experimental Neuropsychology, 10, 421–431.
Delis, D. C., Massman, P. J., Butters, N., Salmon, D. P., et al. (1992). Spatial cognition in Alzheimer’s disease: Subtypes of global–local impairment. Journal of Clinical & Experimental Neuropsychology, 14, 463–477.
de Leon, M., Convit, A., Wolf, O. T., et al. (2001). Prediction of cognitive decline in normal elderly subjects with 2-[(18)F] fluoro-2-deoxy-d-glucose/positron-emission tomography (FDG/PET). Proceedings of the National Academy of Sciences of the United States of America, 98, 10966–10971.
Demadura, T., Delis, D. C., Jacobson, M., & Salmon, D. (2001). Do subgroups of patients with Alzheimer’s disease exhibit asymmetric deficits on memory tests? Journal of Clinical & Experimental Neuropsychology, 23, 164–171.
De Santi, S., de Leon, M. J., Rusinek, H., et al. (2001). Hippocampal formation glucose metabolism and volume losses in MCI and AD. Neurobiology of aging, 22, 529–539.
D’Esposito, M., Zarahn, E., Aguirre, G. K., & Rypma, B. (1999). The effect of normal aging on the coupling of neural activity to the BOLD hemodynamic response. NeuroImage, 10, 6–14.
Doody, R. S., Vacca, J. L., Massman, P. J., & Liao, T. Y. (1999). The influence of handedness on the clinical presentation and neuropsychology of Alzheimer disease. Archives of neurology, 56, 1133–1137.
Dori, G. A., & Chelune, G. J. (2004). Education-stratified base-rate information on discrepancy scores within and between the Wechsler Adult Intelligence Scale—Third Edition and the Wechsler Memory Scale—Third Edition. Psychological assessment, 16, 146–154.
Durany, N., Michel, T., Kurt, J., Cruz-Sanchez, F. F., Crevos-Navarro, J., & Riederer, P. (2000). Brain-derived neurotrophic factor and neurotrophin-3 levels in Alzheimer’s disease brains. International Journal of Developmental Neuroscience, 18, 807–813.
Egan, M. F., Kojima, M., Callicott, J. H., Goldberg, T. E., Kolachana, B. S., Bertolino, E. Z., et al. (2003). The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell, 112, 257–269.
Etiene, D., Kraft, J., Ganju, N., et al. (1998). Cerebrovascular pathology contributes to the heterogeneity of Alzheimer’s disease. Journal of Alzheimer's disease, 1, 119–134.
Farris, W., Mansourian, S., Chang, Y., et al. (2003). Insulin-degrading enzyme regulates the levels of insulin, amyloid beta-protein, and the beta-amyloid precursor protein intracellular domain in vivo. Proceedings of the National Academy of Sciences, 100(7), 4162–4167.
Farris, W., Mansourian, S., Leissring, M. A., et al. (2004). Partial loss-of-function mutations in insulin-degrading enzyme that induce diabetes also impairs degradation of amyloid beta-protein. American journal of pathology, 164(4), 1425–1434.
Fennema-Notestine, C., Gamst, A. C., Quinn, B. T., et al. (2007). Feasibility of multi-site clinical structural neuroimaging studies of aging using legacy data. Neuroinformatics, 5, 235–245.
Filoteo, J. V., Delis, D. C., Massman, P. J., Demadura, T., et al. (1992). Directed and divided attention in Alzheimer’s disease: Impairment in shifting of attention to global and local stimuli. Journal of Clinical & Experimental Neuropsychology, 14, 871–883.
Finton, M. J., Lucas, J. A., Rippeth, J. D., et al. (2003). Cognitive asymmetries associated with apolipoprotein E genotype in patients with Alzheimer’s disease. Journal of the International Neuropsychological Society, 9, 751–759.
Fisk, J. D., & Rockwood, K. (2005). Outcomes of incident mild cognitive impairment in relation to case definition. Journal of Neurology, Neurosurgery and Psychiatry, 76(8), 1175–1177.
Franceschi, M., Alberoni, M., Bressi, S., et al. (1995). Correlations between cognitive impairment, middle cerebral artery flow velocity and cortical glucose metabolism in the early phase of Alzheimer’s disease. Dementia, 6, 32–38.
Fratiglioni, L., & Wang, H. X. (2007). Brain reserve hypothesis in dementia. Journal of Alzheimer's disease, 12, 11–22.
Geroldi, C., Laakso, M. P., DeCarli, C., et al. (2000). Apolipoprotein E genotype and hippocampal asymmetry in Alzheimer’s disease: A volumetric MRI study. Journal of Neurology, Neurosurgery & Psychiatry, 68, 93–96.
Grober, E., & Kawas, C. (1997). Learning and retention in preclinical and early Alzheimer’s disease. Psychology and Aging, 12, 183–188.
Grundman, M., Petersen, R. C., Ferris, S. H., et al. (2004). Mild cognitive impairment can be distinguished from Alzheimer disease and normal aging for clinical trials. Archives of neurology, 61(1), 59–66.
Guskiewicz, K. M., Marshall, S. W., Bailes, J., McCrea, M., Cantu, R. C., Randolph, C., et al. (2005). Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurg, 57(4), 719–726.
Guttman, C. R., Jolesz, F. A., Kikinis, R., Killiany, R. J., Moss, M. B., Sandor, T., et al. (1998). White matter changes with normal aging. Neurology, 50, 972–978.
Han, S. D., Houston, W. S., Jak, A. J., Eyler, L. T., Nagel, B. J., Fleisher, A. S., et al. (2007). Verbal paired-associate learning by APOE genotype in non-demented older adults: fMRI evidence of a right hemisphere compensatory response. Neurobiology of aging, 28, 238–247.
Haxby, J. V., Duara, R., Grady, C. L., & Cutler, N. R. (1985). Rapoport SI. Relations between neuropsychological and cerebral metabolic asymmetries in early Alzheimer’s disease. Journal of cerebral blood flow and metabolism, 5, 193–200.
Haxby, J. V., Grady, C. L., Koss, E., et al. (1990). Longitudinal study of cerebral metabolic asymmetries and associated neuropsychological patterns in early dementia of the Alzheimer type. Archives of neurology, 47, 753–760.
Hayden, K. M., Zandi, P. P., Lyketsos, C. G., et al. (2006). Vascular risk factors for incident Alzheimer disease and vascular dementia: The Cache county study. Alz Dis Assoc Disord, 20, 93–100.
Heaton, R. K., Grant, I., & Matthews, C. G. (1991). Comprehensive norms for an expanded Halstead-Reitan Battery: Demographic corrections, research findings, and clinical applications. Odessa, FL: Psychological Assessment Resources.
Heaton, R. K., Miller, S. W., Taylor, M. J., & Grant, I. (2004). Revised comprehensive norms for an expanded Halstead-Reitan Battery: Demographically adjusted neuropsychological norms for African American and Caucasian adults Scoring Program. Odessa, FL: Psychological Assessment Resources, Inc.
Helbecque, N., & Amouyel, P. (2004). Commonalities between genetics of cardiovascular disease and neurodegenerative disorders. Current opinion in lipidology, 15, 121–127.
Hensel, A., Angermeyer, M. C., & Riedel-Heller, S. G. (2007). Measuring cognitive change in older adults: Reliable change indices for the Mini-Mental State Examination. Journal of Neurology, Neurosurgery and Psychiatry, 78(12), 1298–1303.
Hirao, K., Ohnishi, T., Matsuda, H., et al. (2006). Functional interactions between entorhinal cortex and posterior cingulate cortex at the very early stage of Alzheimer’s disease using brain perfusion single-photon computed tomography. Nuclear Medicine, 27, 151–156.
Hirono, N., Kitagaki, H., Kazui, H., et al. (2000). Impact of white matter changes on clinical manifestation of Alzheimer’s disease. Stroke, 31, 2182–2188.
Hofman, A., Ott, A., & Breteler, M. M. (1997). Atherosclerosis, apolipoprotein E, and prevalence of dementia and Alzheimer’s disease in the Rotterdam Study. Lancet, 349, 151–154.
Honig, L. S., Tang, M.-X., Albert, S., et al. (2003). Stroke and the risk of Alzheimer disease. Archives of neurology, 60, 1707–1712.
Houston, W. S., Delis, D. C., Lansing, A., et al. (2005). Executive function asymmetry in older adults genetically at-risk for Alzheimer's disease: Verbal versus design fluency. Journal of the International Neuropsychological Society, 11, 863–870.
Iadecola, C., & Gorelick, P. B. (2003). Converging pathogenic mechanisms in vascular and neurodegenerative dementia. Stroke, 34(2), 335–337.
Jack, C. R., Petersen, R. C., Xu, Y. C., Waring, S. C., O’Brien, P. C., et al. (1998). Medial temporal atrophy on MRI in normal aging and very mild Alzheimer’s disease. Neurology, 49, 786–794.
Jacobs, D. M., Sano, M., Dooneief, G., Marder, K., Bell, K. L., & Stern, Y. (1995). Neuropsychological detection and characterization of preclinical Alzheimer’s disease. Neurology, 45, 957–962.
Jacobson, M. W., Delis, D. C., Bondi, M. W., & Salmon, D. P. (2002). Do neuropsychological tests detect preclinical Alzheimer’s disease: individual-test versus cognitive-discrepancy score analyses. Neuropsychology, 16, 132–139.
Jacobson, M. W., Delis, D. C., Bondi, M. W., & Salmon, D. P. (2005a). Asymmetry in auditory and spatial span attention in normal elderly genetically at risk for Alzheimer’s disease. Journal of Clinical & Experimental Neuropsychology, 27, 240–253.
Jacobson, M. W., Delis, D. C., Lansing, A., et al. (2005b). Asymmetries in global-local processing ability in elderly people with the apolipoprotein e-epsilon4 allele. Neuropsychology, 19, 822–829.
Jellinger, K. A. (2004). Head injury and dementia. Current opinion in neurology, 17, 719–723.
Jernigan, T. J., Archibald, S. L., Fennema-Notestine, C., Gamst, A. C., Stout, J. C., Bonner, J., et al. (2001). Effects of age on tissues and regions of the cerebrum and cerebellum. Neurobiology of aging, 22, 581–594.
Jick, H., Zornberg, G. L., Jick, S. S., et al. (2000). Statins and the risk of dementia. Lancet, 356(9242), 1627–1631.
Jordan, B. D., Relkin, N. R., Ravdin, L. D., Jacobs, A. R., Bennett, A., & Gandy, S. (1997). Apolipoprotein E epsilon4 associated with chronic traumatic brain injury in boxing. JAMA, 278, 136–140.
Kawas, C. H., & Katzman, R. (1999). Epidemiology of dementia and Alzheimer disease. In R. D. Terry, R. Katzman, K. L. Bick, & S. S. Sisodia (Eds.), Alzheimer disease, 2nd edition (pp 95–116).
Kivipelto, M., Ngandu, T., Fratiglioni, L., et al. (2005). Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Archives of neurology, 62, 1556–1560.
Knopman, D., Boland, L. L., Mosley, T., Howard, G., Liao, D., Szklo, M., et al. (2001). Cardiovascular risk factors and cognitive decline in middle-aged adults. Neurology, 56, 42–8.
Koenig, P., Smith, E. E., Moore, P., Glosser, G., & Grossman, M. (2007). Categorization of novel animals by patients with Alzheimer’s disease and corticobasal degeneration. Neuropsychology, 21, 193–206.
Kogure, D., Matsuda, H., Ohnishi, T., et al. (2000). Longitudinal evaluation of early Alzheimer’s disease using brain perfusion SPECT. Journal of nuclear medicine, 41, 1155–1162.
Kramer, A. F., & Erickson, K. I. (2007). Capitalizing on cortical plasticity: Influence of physical activity on cognition and brain function. Trends in cognitive Neurosciences, 11(8), 342–348.
Kramer, J. H., Nelson, A., Johnson, J. K., et al. (2006). Multiple cognitive deficits in amnestic mild cognitive impairment. Dementia and Geriatric Cognitive Disorders, 22(4), 306–311.
Kryscio, R. J., Schmitt, F. A., Salazar, J. C., Mendiondo, M. S., & Markesbery, W. R. (2006). Risk factors for transitions from normal to mild cognitive impairment and dementia. Neurology, 66(6), 828–832.
La Rue, A., Matsuyama, S. S., McPherson, S., et al. (1992). Cognitive performance in relatives of patients with probable Alzheimer’s disease: An age at onset effect? Journal of clinical and experimental neuropsychology, 14, 533–538.
Lange, K. L., Bondi, M. W., Galasko, D. G., Delis, D. C., Salmon, D. P., & Thal, L. J. (2002). Decline in verbal memory during preclinical Alzheimer’s disease: Examination of the effect of Apolipoprotein E genotype. Journal of the International Neuropsychological Society, 8, 943–955.
Lange, R. T., Chelune, G. J., & Tulsky, D. S. (2006). Development of WAIS-III General Ability Index Minus WMS-III memory discrepancy scores. Clinical neuropsychology, 20, 382–395.
Larrieu, S., Letenneur, L., Orgogozo, J. M., et al. (2002). Incidence and outcome of mild cognitive impairment in a population-based prospective cohort. Neurology, 59(10), 1594–1599.
Launer, L. J., Ross, G. W., Petrovich, H., et al. (2000). Midlife blood pressure and dementia: The Honolulu-Asia Aging Study. Neurobiology of aging, 21, 49–55.
Levy, J. A., Bergeson, J., Putnam, K., Rosen, V., Cohen, R., Lalonde, F., et al. (2004). Context-specific memory and apolipoprotein E (ApoE) e4: Cognitive evidence from the NIMH prospective study of risk for Alzheimer’s disease. Journal of the International Neuropsychological Society, 10, 362–370.
Lopez, O. L., Becker, J. T., Jagust, W. J., et al. (2006). Neuropsychological characteristics of mild cognitive impairment subgroups. Journal of Neurology, Neurosurgery and Psychiatry, 77(2), 159–165.
Luchsinger, J. A., & Mayeux, R. (2004). Cardiovascular risk factors and Alzheimer’s disease. Current atherosclerosis reports, 6(4), 261–266.
Luchsinger, J. A., Reitz, C., Honig, L. S., et al. (2005). Aggregation of vascular risk factors and risk of incident Alzheimer disease. Neurology, 65(4), 545–551.
Luchsinger, J. A., Reitz, C., Patel, B., et al. (2007). Relation of diabetes to mild cognitive impairment. Archives of neurology, 64(4), 570–575.
Luchsinger, J. A., Tang, M. X., Shea, S., et al. (2004). Hyperinsulinemia and risk of Alzheimer disease. Neurology, 63(7), 1187–1192.
Manly, J. J., Bell-McGinty, S., Tang, M., Schupf, N., Stern, Y., & Mayeux, R. (2005). Implementing diagnostic criteria and estimating frequency of mild cognitive impairment in an urban community. Archives of neurology, 62(11), 1739–1746.
Margaglione, M., Seripa, D., Gravina, C., et al. (1998). Prevalence of apolipoprotein E alleles in healthy subjects and survivors of ischemic stroke. Stroke, 29, 399–403.
Martin, A. (1990). Neuropsychology of Alzheimer’s disease: The case for subgroups. In M. F. Schwartz (Ed.) Modular deficits in Alzheimer-type dementia. Issues in the biology of language and cognition (pp. 143–175). Cambridge, MA: The MIT Press.
Masliah, E., Mallory, M., Hansen, L. A., DeTeresa, R., & Terry, R. D. (1993). Quantitative synaptic alterations in the human neocortex during normal aging. Neurology, 43, 192–197.
Mayeux, R., Ottman, R., Maestre, G., Ngai, C., Tang, M.-X., Ginsberg, H., Chun, M., Tycko, B., et al. (1995). Synergistic effects of traumatic head injury and apolipoprotein e4 in patients with Alzheimer’s disease. Neurology, 45, 555–557.
Mentis, M. J., Salerno, J., Horwitz, B., et al. (1994). Reduction of functional neuronal connectivity in long-term treated hypertension. Stroke, 25(3), 601–607.
Mickes, L., Wixted, J. T., Fennema-Notestine, C., Galasko, D., Bondi, M. W., Thal, L. J., et al. (2007). Progressive impairment on neuropsychological tasks in a longitudinal study of preclinical Alzheimer’s disease. Neuropsychology, 21, 696–705.
Miech, R. A., Breitner, J. C., Zandi, P. P., Khachaturian, A. S., Anthony, J. C., & Mayer, L. (2002). Incidence of AD may decline in the early 90s for men, later for women: The Cache County study. Neurology, 58, 209–218.
Mielke, M. M., Rosenberg, P. B., Tschanz, J., et al. (2007). Vascular factors predict rate of progression in Alzheimer disease. Neurology, 69, 1850–1858.
Mitrushina, M., Uchiyama, C., & Satz, P. (1995). Heterogeneity of cognitive profiles in normal aging: Implications for early manifestations of Alzheimer’s disease. Journal of clinical and experimental neuropsychology, 17, 374–382.
Mortimer, J. A., van Duijn, C. M., Chandra, V., Fratglioni, L., Graves, A. B., Heyman, A., et al. (1991). Head trauma as a risk factor for Alzheimer’s disease: A collaborative re-analysis of case-control studies. International journal of epidemiology, 20(suppl. 2), S28–35.
Mu, Q., Xie, J., Wen, Z., Weng, Y., & Shuyun, Z. (1999). A quantitative MR study of the hippocampal formation, the amygdala, and the temporal horn of the lateral ventricle in healthy subjects 40 to 90 years of age. AJNR American journal of neuroradiology, 20, 207–211.
Okamura, N., Shinkawa, M., Arai, H., et al. (2000). Prediction pf progression in patients with mild cognitive impairment using IMP-SPECT. Nippon Ronen Igakkai Zasshi, 37, 974–978.
Ott, A., Breteler, M. M., de Bruyne, M. C., et al. (1997). Atrial fibrillation and dementia in a population-based study: The Rotterdam Study. Stroke, 28, 316–321.
Ott, A., Slooter, A. J., Hofman, A., et al. (1998). Smoking and risk of dementia and Alzheimer’s disease in a population-based cohort study: the Rotterdam Study. Lancet, 351, 1840–1843.
Ott, A., Stolk, R. P., Hofman, A., et al. (1999). Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology, 53, 1907–1909.
Parasuraman, R., Greenwood, P. M., Haxby, J. V., & Grady, C. L. (1992). Visuospatial attention in dementia of the Alzheimer type. Brain, 115(Pt 3), 711–733.
Pedraza, O., Bowers, D., & Gilmore, R. (2004). Asymmetry of the hippocampus and amygdala in MRI volumetric measurements of normal adults. Journal of the International Neuropsychological Society, 10, 664–678.
Petersen, R. C. (2004). Mild cognitive impairment as a diagnostic entity. Journal of Internal Medicine, 256, 183–194.
Petersen, R. C., Doody, R. S., Kurz, A., et al. (2001). Current concepts in mild cognitive impairment. Archives of neurology, 58(12), 1985–1992.
Petersen, R. C., & Morris, J. C. (2005). Mild cognitive impairment as a clinical entity and treatment target. Archives of Neurology, 62, 1160–1163.
Petersen, R. C., Smith, G. E., Waring, S. C., Ivnik, R. J., Tangalos, E. G., & Kokmen, E. (1999). Mild cognitive impairment: Clinical characterization and outcome. Archives of neurology, 56(3), 303–308.
Petrovich, H., White, L. R., Izmirilian, G., et al. (2000). Midlife blood pressure and neuritic plaques, neurofibrillary tangles, and brain weight at death: the HAAS, Honolulu–Asia Aging Study. Neurobiology of aging, 21, 57–62.
Pfefferbaum, A., Mathalon, D. H., Sullivan, E. V., Rawles, J. M., Zipursky, R. B., & Lim, K. O. (1994). A quantitative magnetic resonance imaging study of changes in brain morphology from infancy to late adulthood. Archives of neurology, 51, 874–887.
Polvikoski, T., Sulkava, R., Myllykangas, L., et al. (2001). Prevalence of Alzheimer’s disease in very elderly people: A prospective neuropathological study. Neurology, 56, 1690–1696.
Portet, F., Ousset, P. J., Visser, P. J., et al. (2006). Mild cognitive impairment (MCI) in medical practice: a critical review of the concept and new diagnostic procedure. Report of the MCI Working Group of the European Consortium on Alzheimer’s Disease. Journal of Neurology, Neurosurgery and Psychiatry, 77(6), 714–718.
Powell, M. R., Smith, G. E., Knopman, D. S., et al. (2006). Cognitive measures predict pathologic Alzheimer disease. Archives of Neurology, 63, 865–868.
Rasmusson, D. X., & Brandt, J. (1995). Instability of cognitive asymmetry in Alzheimer’s Disease. Journal of Clinical and Experimental Neuropsychology, 17, 449–458.
Raz, N., Gunning-Dixon, F., Head, D., Rodrigue, K. M., Williamson, A., & Acker, J. D. (2004). Aging, sexual dimorphism, and hemispheric asymmetry of the cerebral cortex: replicability of regional differences in volume. Neurobiology of aging, 25, 377–396.
Raz, N., & Rodrigue, K. M. (2006). Differential aging of the brain: patterns, cognitive correlates and modifiers. Neuroscience and biobehavioral reviews, 30, 730–748.
Refolo, L. M., Malester, B., LaFrancois, J., et al. (2000). Hypercholestremia accelerates the Alzheimer’s amyloid pathology in a transgenic mouse model. Neurobiology of disease, 7(4), 321–331.
Regan, C., Katona, C., Walker, Z., et al. (2006). Relationship of vascular risk to the progression of Alzheimer’s disease. Neurology, 67, 1357–1362.
Rodriguez, G., Vitali, P., Calvini, P., et al. (2000). Hippocampal perfusion in mild cognitive impairment. Psychiatry research, 100, 65–74.
Rosen, V. M., Sunderland, T., Levy, J., Harwell, A., McGee, L., Hammond, C., et al. (2005). Apolipoprotein E and category fluency: evidence for reduced semantic access in healthy normal controls at risk for developing Alzheimer’s disease. Neuropsychologia, 43, 647–658.
Rubin, E. H., Storandt, M., Miller, P., Kinscherf, D. A., Grant, E. A., Morris, J. C., et al. (1998). A prospective study of cognitive function and onset of dementia in cognitively healthy elders. Archives of neurology, 55, 395–401.
Salat, D. H., Kaye, J. A., & Janowsky, J. S. (1999). Prefrontal gray and white matter volumes in healthy aging and Alzheimer disease. Archives of neurology, 56, 338–344.
Salmon, D. P., & Bondi, M. W. (1999). Neuropsychology of Alzheimer’s disease. In R. D. Terry, R. Katzman, K. L. Bick, & S. S. Sisodia (Eds.) Alzheimer Disease (pp. 39–56). Philadelphia: Lippincott Williams & Wilkens.
Salmon, D. P., Thomas, R. G., Pay, M. M., et al. (2002). Alzheimer’s disease can be accurately diagnosed in very mildly impaired individuals. Neurology, 59, 1022–1028.
Saunders, A. M., Strittmatter, W. J., Schmechel, D., St. George-Hyslop, P. H., Pericak-Vance, M. A., Joo, S. H., et al. (1993). Association of apolipoprotein E allele e4 with late-onset familial and sporadic Alzheimer’s disease. Neurology, 43, 1467–1472.
Schneider, J. A., Wilson, R. S., Bienias, J. L., et al. (2004). Cerebral infarctions and the likelihood of dementia from Alzheimer disease pathology. Neurology, 62(7), 1148–1155.
Silvestrini, M., Pasqualetti, P., Baruffaldi, R., et al. (2006). Cerebrovascular reactivity and cognitive decline in patients with Alzheimer disease. Stroke, 37(4), 1010–1015.
Small, B. J., Fratiglioni, L., Viitanen, M., Winblad, B., & Bäckman, L. (2000). The course of cognitive impairment in preclinical Alzheimer disease: Three- and 6-year follow-up of a population-based sample. Archives of neurology, 57, 839–844.
Small, G. W., La Rue, A., Komo, S., Kaplan, A., & Mandelkern, M. A. (1995a). Predictors of cognitive change in middle-aged and older adults with memory loss. American Journal of Psychiatry, 152, 1757–64.
Small, G. W., Mazziotta, J. C., Collins, M. T., Baxter, L. R., Phelps, M. E., Mandelkern, M. A., et al. (1995b). Apolipoprotein E type 4 allele and cerebral glucose metabolism in relatives at risk for familial Alzheimer disease. JAMA, 273, 942–947.
Small, B. J., Mobly, J. L., Laukka, E. J., Jones, S., & Bäckman, L. (2003). Cognitive deficits in preclinical Alzheimer’s disease. Acta Neurologica Scandinavica, Supplementum, 179, 29–33.
Smith, G., Machulda, M., & Kantarci, K. (2006). A perspective from the Mayo Clinic. In H. A. Tuokko, & D. F. Hultsch (Eds.) Mild Cognitive Impairment: International Perspectives (pp. 131–162). New York: Taylor & Francis.
Smith, G. E., Pankratz, V. S., Negash, S., et al. (2007). A plateau in pre-Alzheimer memory decline: Evidence for compensatory mechanisms? Neurology, 69, 133–139.
Snowdon, D. A., Greiner, L. H., Mortimer, J. A., et al. (1997). Brain infraction and the clinical expression of Alzheimer disease. The Nun Study. JAMA, 277, 813–817.
Storandt, M., Grant, E. A., Miller, J. P., & Morris, J. C. (2002). Rates of progression in mild cognitive impairment and early Alzheimer’s disease. Neurology, 59, 1034–1041.
Storandt, M., Grant, E. A., Miller, J. P., & Morris, J. C. (2006). Longitudinal course and neuropathologic outcomes in original vs revised MCI and in pre-MCI. Neurology, 67(3), 467–473.
Strite, D., Massman, P. J., Cooke, N., & Doody, R. S. (1997). Neuropsychological asymmetry in Alzheimer’s disease: verbal versus visuoconstructional deficits across stages of dementia. Journal of the International Neuropsychological Society, 3, 420–427.
Strittmatter, W. J., Saunders, A. M., Schmechel, D., Pericak-Vance, M., Enghild, J., Salvesen, G. S., et al. (1993). Apolipoprotein-E—High-avidity binding to B-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proceedings of the National Academy of Sciences [USA], 90, 9649–9653.
Swan, G. E., DeCarli, C., Miller, B. L., et al. (2000). Biobehavioral characteristics of nondemented older adults with subclinical brain atrophy. Neurology, 54(11), 2108–2114.
Tabert, M. H., Manly, J. J., Liu, X., et al. (2006). Neuropsychological prediction of conversion to Alzheimer disease in patients with mild cognitive impairment. Archives of General Psychiatry, 63(8), 916–924.
Terry, R. D., Katzman, R., Bick, K. L., & Sisodia, S. S. (Eds.) (1999). Alzheimer disease (2nd ed.). New York: Lippincott.
Tian, J., Bucks, R. S., Haworth, J., & Wilcock, G. (2003). Neuropsychological prediction of conversion to dementia from questionable dementia: Statistically significant but not yet clinically useful. Journal of Neurology, Neurosurgery and Psychiatry, 74(4), 433–438.
Tuokko, H. A., & McDowell, I. (2006). An overview of mild cognitive impairment. In H. A. Tuokko, & D. F. Hultsch (Eds.) Mild Cognitive Impairment: International Perspectives (pp. 3–28). New York: Taylor and Francis.
Twamley, E. W., Ropacki, S., & Bondi, M. W. (2006). Neuropsychological and neuroimaging changes in preclinical Alzheimer’s disease. Journal of the International Neuropsychological Society, 12, 707–735.
Tyas, S. L., Manfreda, J., Strain, L. A., et al. (2001). Risk factors for Alzheimer’s disease: a population-based, longitudinal study in Manitoba, Canada. International journal of epidemiology, 30, 590–597.
van Duijn, C. M., Hofman, A., & Kay, D. W. (1991). Risk factors for Alzheimer's disease: A collaborative re-analysis of case-control studies. International journal of epidemiology, 20(Suppl. 2).
Venneri, A., Pentore, R., Cotticelli, B., & Della Sala, S. (1998). Unilateral spatial neglect in the late stage of Alzheimer’s disease. Cortex, 34, 743–52.
Wetter, S. R., Delis, D. C., Houston, W. S., et al. (2006). Heterogeneity in verbal memory: A marker of preclinical Alzheimer’s disease? Neuropsychology, development, and cognition. Section B, Aging, neuropsychology and cognition, 13, 503–515.
Wetter, S. R., Delis, D. C., Houston, W. S., Jacobson, M. W., Lansing, A., Cobell, K., et al. (2005). Deficits in inhibition and flexibility are associated with the APOE-E4 allele in nondemented older adults. Journal of clinical and experimental neuropsychology, 27, 943–952.
Whitehouse, P. J., Price, D. L., Struble, R. G., Clark, A. W., Coyle, J. T., & DeLong, M. R. (1982). Alzheimer's disease and senile dementia: Loss of neurons in the basal forebrain. Science, 215, 1237–1239.
Wierenga, C. E., & Bondi, M. W. (2007). The use of functional magnetic resonance imaging in preclinical Alzheimer’s disease. Neuropsychology review, 17, 127–143.
Wilde, N., Strauss, E., Chelune, G., Loring, D., Martin, R., Hermann, B., et al. (2001). WMS-III performance in patients with temporal lobe epilepsy: Group differences and individual classification. Journal of the International Neuropsychological Society, 7, 881–891.
Wolf, H., Grunwald, M., Kruggel, F., et al. (2001). Hippocampal volume discriminates between normal cognition; questionable and mild dementia in the elderly. Neurobiology of aging, 22, 177–186.
Yaffe, K., Petersen, R. C., Lindquist, K., Kramer, J., & Miller, B. (2006). Subtype of mild cognitive impairment and progression to dementia and death. Dementia and Geriatric Cognitive Disorders, 22(4), 312–319.
Zanetti, M., Ballabio, C., Abbate, C., Cutaia, C., Vergani, C., & Bergamaschini, L. (2006). Mild Cognitive impairment subtypes and vascular dementia in community-dwelling elderly people: A 3-year follow-up study. Journal of the American Geriatrics Society, 54(4), 580–586.
Zhang, M., Katzman, R., Salmon, D. P., Jin, H., Cai, G., Wang, Z., et al. (1990). The prevalence of dementia and Alzheimer’s disease (AD) in Shanghai, China: Impact on age, gender and education. Annals of neurology, 27, 428–437.
Acknowledgements
This critical review was supported by funds from NIA grants P50 AG005131 (MWB, DPS), RO1 AG012674 (MWB), and K24 AG026431 (MWB) to the University of California San Diego and the Veterans Medical Research Foundation, by grants from the Department of Veterans Affairs (DCD, AJJ, MWJ), and by a grant from the Alzheimer’s Association (AJJ). The authors wish to thank our many collaborators and volunteers at the UCSD Alzheimer’s Disease Research Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bondi, M.W., Jak, A.J., Delano-Wood, L. et al. Neuropsychological Contributions to the Early Identification of Alzheimer’s Disease. Neuropsychol Rev 18, 73–90 (2008). https://doi.org/10.1007/s11065-008-9054-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-008-9054-1