Abstract
Cannabis has an ancient history of human use and is currently one of the most commonly used drugs worldwide. Understanding its impact on neurobehavioral functioning is of significant public health concern. In recent decades, substantial progress has been made in understanding the impact of cannabis use on neurobehavioral functioning. This has been fueled, in part, by characterization of an endocannabinoid signaling system in the brain through which cannabis exerts its psychoactive effects. Acute intoxication with cannabis causes marked changes in subjective mental status, brain functioning, and neuropsychological performance. Some of these changes are consistently detected and well characterized, yet others are not. Changes in brain functioning and neuropsychological performance are also reported after abstinence, but appear to be mild, circumscribed, and transient. On the other hand, functional neuroimaging often reveals subtle differences in the brain functioning of abstinent cannabis users compared with controls. The persistence and clinical significance of these differences, however, remains to be determined. Neuropsychological deficits and differences in brain functioning are most consistently observed only among frequent, heavy users, who are those most likely addicted to cannabis. The dire impact of drug addiction on a person’s life and everyday functioning suggests that the large number of individuals addicted to cannabis experience substantial negative effects from its use. This manuscript reviews the scientific literature on the aforementioned topics in detail, providing evidence for converging findings, and highlighting areas in need of further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction to Cannabis Use and Abuse
Cannabis is one of the most commonly used psychoactive substances in the world and has the disreputable status of being the most popular illicit drug in the United States. From 2001 through 2003, approximately 3.7% of the world’s population (ages 15–64 years old) reported ever having used cannabis (United Nations Office on Drugs and Crimes 2004). By contrast, substantially fewer individuals worldwide use cocaine (0.3%) and opiates (0.4%). Prevalence of cannabis use varies considerably across countries. In Europe, estimates of lifetime use between 1999 and 2003 ranged from 31% in the United Kingdom to 5% in Belgium (European Monitoring Centre for Drugs and Drug Addiction 2004). Sweden boasts the lowest rate (1%) of individuals reporting cannabis use “in the last 12 months,” whereas Switzerland reports the highest (22.1%). By comparison, rates of reported use in the past year were 20% in the United Kingdom and 11.8% in the Netherlands. In the United States, 40.1% of the population over 12 years of age reported using cannabis at least once in their life and 10.4% reported use in the past year (Substance Abuse and Mental Health Service Administration 2005). Cannabis use appears to be popular with the nation’s youth, with 42.3% of 12th graders in the U.S. reporting having tried cannabis during 2006 (Johnston et al. 2006). Only 17.8% of 12th graders perceived trying cannabis once or twice as harmful, but perceived harm increased to 57.9% when asked about frequent use (Johnston et al. 2006).
Of more concern is the number of individuals in the U.S. that have cannabis-related substance use disorders. Estimates from 2004 and 2005 indicate that 1.7% of the U.S. population met DSM-IV criteria for cannabis abuse or dependence during the “past year,” which is substantially more than for any other drug (Substance Abuse and Mental Health Service Administration 2005). For example, less than half the number of people have a substance use disorder for cocaine and considerably fewer for heroin. Lifetime prevalence rates for cannabis dependence are estimated to be much greater, at 4.2% (Anthony et al. 1994). Moreover, Compton et al. (2004) found that prevalence of cannabis use remained stable from 1992 to 2002, but rates of substance-use disorders for cannabis showed statistically significant increases (1.2% to 1.5%). Anthony et al. (1994) found that 9.1% of people that reported lifetime use of cannabis transitioned to dependence. The percentage of individuals transitioning to dependence for other drugs was reported to be higher for alcohol (15.4%), cocaine (16.7%), heroin (23.1%), and tobacco (31.9%). Thus, the high prevalence of cannabis substance use disorders compared with other substances likely reflects its popularity rather than an inherent greater liability for dependence.
Cannabis sativa is an annual plant that grows wild in many temperate and tropical climates throughout the world. The flowers and surrounding leaves of this plant are often dried and processed for use as a psychoactive drug. One reason why cannabis has enjoyed a high prevalence of use may stem from its ancient history of use by humans for varied purposes, including textiles, food, medicine, spiritual rituals, and as a recreational drug (Jiang et al. 2006; Merlin 2003; Zuardi 2006). The cannabis plant contains 489 known compounds representing almost all classes of chemicals, including 70 cannabinoids, of which delta-9-tetrahydrocannabinol (THC) is the most psychoactive (ElSohly and Slade 2005).
It was not until the 1960s that THC was fully characterized and found to be the main psychoactive compound in cannabis (Mechoulam and Gaoni 1967). This was a milestone for cannabis research, in part because it allowed standardized dosing of the key psychoactive ingredient, enabling scientists to better understand the mechanisms for its effects. Nonetheless, the mechanisms by which THC caused a mind-altering experience remained elusive. Because of its chemical properties, many hypothesized that THC produced its effects through its actions on cell membranes, thus avoiding need to speculate on a specific neurotransmitter site to which it might bind (Mechoulam and Hanus 2000).
The Endocannabinoid Signaling System
Approximately 25 years transpired from the discovery of THC until the recognition that it bound to a specific receptor in mammalian brain tissue, identified as CB1 (Devane et al. 1988; Matsuda et al. 1990). CB1 receptors are also found in human peripheral tissue, but in much lower concentrations. On the other hand, a second type of cannabinoid receptor, CB2 (Munro et al. 1993), is present mainly in immune tissues and cells (Galiegue et al. 1995; Munro et al. 1993), with more recent evidence showing that it may also be present in CNS (Onaivi et al. 2006). Some evidence argues for a third cannabinoid receptor (Breivogel et al. 2001; Di Marzo et al. 2000; Fride et al. 2003) that is also present in the CNS but has yet to be well characterized.
Cannabinoid receptors are in the family of G-protein-coupled receptors, which are involved in second messenger signaling, and modulate chemical reactions in cells (Childers et al. 1993). CB1 is found on presynaptic terminals and modulates neurotransmission through inhibiting adenylyl cyclase and modulating cAMP production, decreasing Ca2+ influx, and increasing K+ conductance (McAllister and Glass 2002; Pertwee 1997). Several endogenous metabolites of arachidonic acid (an essential fatty acid found in cell membranes and the brain) that are active at cannabinoid receptors were later identified (termed endocannabinoids) and an endogenous cannabinoid signaling system was further characterized (De Petrocellis et al. 2004). The earliest discovered and most studied molecules are anandamide (N-arachidonoyl-ethanolamine) (Devane et al. 1992) and 2-AG (2-arachidonoyl-glycerol) (Mechoulam et al. 1995; Sugiura et al. 1995), which are both endogenous cannabinoid receptor agonists with similar binding activity to THC. Since then, several additional endogenous compounds that are active at cannabinoid receptors have been identified (Hanus et al. 2001; Porter et al. 2002).
CB1 receptors are diversely and often densely distributed throughout mammalian brain tissue. Quantitative autoradiography has shown that across several mammalian species (including humans), CB1 receptors are most plentiful in the substantia nigra pars reticulata, globus pallidus, cerebellum, and hippocampus (Glass et al. 1997b; Herkenham et al. 1990). Several functional roles have been ascribed to the endocannabinoid system within these different brain regions. For example, in the hippocampus, cannabinoid receptors are important in long-term potentiation (LTP) (Chevaleyre and Castillo 2004) and other processes thought critical for memory function, such as GABAergic retrograde (postsynaptic to presynaptic) rapid signaling (termed depolarization-induced suppression of inhibition: DSI), as well as a depolarization-induced suppression of excitation (DSE) through glutamatergic neurons (Davies et al. 2002; Maejima et al. 2001). In the basal ganglia, cannabinoid receptors are thought to play an important role in motor control through modulating both excitatory and inhibitory circuits via glutamatergic, dopaminergic, and GABAergic neurons (Glass et al. 1997a). Cannabinoid receptors are abundant in the brain’s “reward pathways,” which are implicated in the neuropathophysiology of addiction. Through modulating neurotransmission in mesolimbic circuits, mounting evidence implicates the endocannabinoid system in various aspects of drug addiction, including affecting the rewarding properties of drugs, drug-seeking behavior, and craving/relapse (Maldonado et al. 2006).
Clearly, stimulating cannabinoid receptors by smoking cannabis should have profound neurobehavioral effects. Alteration of neural systems, however, does not imply inevitable neurotoxicity, and this issue is particularly complicated for cannabis. Under certain circumstances, several animal studies have shown changes in brain morphology and neuronal death in the hippocampus with administration of CB1 agonists (Landfield et al. 1988; Lawston et al. 2000; Scallet et al. 1987). Yet, ample literature documents the strong antioxidative properties of THC and neuroprotective effects of cannabinoid agonists (Grundy 2002; Guzman et al. 2001; Hampson et al. 2000; Marsicano et al. 2002; Mechoulam 2002), which are being developed into neuroprotective pharmaceuticals (Mechoulam et al. 2002). Interestingly, cannabinoids have also been found protective in the neuropathology of Alzheimer’s disease (Eubanks et al. 2006; Milton 2002; Ramirez et al. 2005), a neurodegenerative illness that damages hippocampal structures and impairs memory. Although descriptive in nature, one study found that individuals dependent on the CNS stimulant methamphetamine (which appears to damage neurons through oxidative stress, cerebrovascular injury, and release of glutamate) who also had significant history of cannabis use showed fewer neuropsychological deficits than those with a history primarily for methamphetamine alone (Gonzalez et al. 2004). However, similar findings have not been found in the setting of “ecstasy” use (Fisk et al. 2006). These seemingly paradoxical mechanisms by which cannabinoids may be neurotoxic and neuroprotective to brain tissue have been the focus of recent reviews (Sarne and Keren 2004; Sarne and Mechoulam 2005).
Acute Effects of Cannabis Use
Basic Pharmacokinetics and Subjective Experience
To produce its psychoactive effects, cannabis is usually smoked. Smoking cannabis is a very efficient method of delivery, producing levels of THC in blood plasma that can be detected within seconds and reach peak concentrations in fewer than 10 min (Agurell et al. 1986; Grotenhermen 2003). In contrast, when cannabis is ingested orally, peak plasma concentrations take much longer to be reached (generally within 60–120 min), may vary substantially across individuals (as much as 6 h), and may peak multiple times. Thus, absorption and time course of psychoactive effects are more variable through the oral route. However, even when smoked, bioavailability of THC can vary based on the experience of cannabis smokers and how they smoke. By adjusting the duration of inhalation, frequency of puffs, and other smoking parameters, individuals titrate the amount of THC they consume and the subjective effects they experience (Block et al. 1998; Heishman et al. 1989; Herning et al. 1986).
THC is soluble in fat and is thus stored in adipose tissue after repeated use, with slow release into the bloodstream. Presence of THC and its metabolites in plasma can vary based on several factors, including potency of last dose, frequency of administration, and body composition, but can be detected from a couple of days to several weeks after last use (Agurell et al. 1986; Grotenhermen 2003). In urine, the time frame during which THC and its metabolites can be detected have been reported to range from 3 days up to 46 days for regular users, with toxicology test results often alternating from positive to negative during this time (Ellis et al. 1985; Huestis et al. 1996).
It must be noted that the amount of THC in cannabis differs widely, based on agricultural techniques, plant strains, and preparation. Cigarette paper and a variety of pipes are often used to smoke the dried cannabis leaves and flowing tops, which typically have THC contents ranging from 0.5 to 4%. However, some plant varieties, such as “sinsemilla,” may contain up to 20%. Further, much higher concentrations of THC can be found in special preparations of cannabis, such as hashish, oils, and tinctures. Some evidence suggests that the potency of street cannabis has increased over the years. Seized cannabis in the United States has shown steady increases in THC content, with samples seized in 1980 averaging about 1.5% THC and those seized in 1997 averaging 4.47% (ElSohly et al. 2000). These trends appear to persist, with estimates of THC content in commercial grade cannabis in the United States during 2002 averaging 5.11% (National Drug Intelligence Center 2005). In contrast, cannabis seized in New Zealand showed no significant changes in THC content between 1976 and 1996 (Poulsen and Sutherland 2000), suggesting that these trends may not be international.
The psychoactive effects of marijuana are experienced almost immediately after smoking, peak levels of intoxication are reported to occur in about 30 min, and effects diminish in approximately 4 h (Grotenhermen 2003). After oral consumption, subjective “highs” have a later onset and longer duration—peak effects are felt by 90 min and abate in up to 6 h (Grotenhermen 2003). The mind-altering effects experienced by cannabis users are varied, but some effects are more commonly reported than others. Green et al. (2003) conducted a detailed semiquantitative review of studies reporting subjective effects of smoking cannabis, including only those studies with sample sizes of more than 30 participants and that provided sufficient information regarding the manner in which data were gathered and analyzed. Across naturalistic investigations that asked open-ended questions about subjective effects of smoking cannabis among experienced users, the most common response was “relaxation.” Other common responses included happiness, increased sensory perception, deep thought, and laughter. Negative effects were reported less often, but included dizziness, becoming withdrawn, and hunger. Aggregating information from naturalistic studies using closed-ended questionnaires revealed similar reports, which included the perception of slowing of time, increased appetite, and also relaxation. Other less common but unpleasant symptoms reported included paranoia, anxiety, depression, drowsiness, and dizziness. Studies examining acute administration of cannabis in laboratory settings produced variable results. In such settings, others have reported that subjective effects do not differ substantially whether cannabis is smoked or consumed orally (Wachtel et al. 2002). Overall, subjective responses to intoxication from cannabis appear to have some common features, but vary widely based on the individual, their prior experience, expectations, and setting.
Neuroimaging Acute Effects of Cannabis
Numerous investigations have been conducted to examine how smoking cannabis or administering THC intravenously affects brain functioning, as visualized through various neuroimaging techniques. These studies yield insights into in vivo functioning of the human brain acutely under the effects of cannabis. Several consistent findings have emerged despite use of different neuroimaging tools, differences in methods of exposing subjects to THC, and subject groups across studies that differed on important substance use parameters such as severity of cannabis use and prior experience with cannabis. Several excellent reviews examining this topic have been written by others over the years (Crippa et al. 2005; Loeber and Yurgelun-Todd 1999; Quickfall and Crockford 2006; Rojas et al. 2005; Solowij 1999).
The most recent and comprehensive of these (Quickfall and Crockford 2006) provided a review on human structural and functional neuroimaging studies of individuals exposed to cannabis that were published in peer-reviewed journals from 1966–2005. Included were 12 investigations specifically examining brain functioning during acute intoxication (Mathew et al. 1989, 1992, 1997, 1998, 1999, 2002; Mathew and Wilson 1993; O’Leary et al. 2000, 2002, 2003; Volkow et al. 1991, 1996). Most studies examined regional cerebral blood flow (rCBF) or brain metabolism at rest using radio-labeled molecules in subject groups who were administered cannabis compared to controls, although a few examined brain metabolism as participants were engaged in various cognitive tasks. With few exceptions, findings have been fairly consistent across studies despite heterogeneity in subject characteristics, revealing increases in CBF and brain metabolism throughout the cortex during acute intoxication. In regional analyses, increased rCBF is most often seen in frontal, limbic, paralimbic, and cerebellar regions. These changes have been observed 30 min after a low-dose intravenous infusion of THC and are found to persist for more than 120 min (Mathew et al. 2002).
Correlations between rCBF and subjective feelings of intoxication have been reported in most studies. For example, subjective ratings of intoxication have been shown inversely correlated with rCBF in hippocampi and right parietal regions (Mathew et al. 1997), but positively correlated with global cortical CBF (Mathew et al. 1992) and rCBF in frontal cortex and the left anterior cingulate (Mathew et al. 1997). Similarly, feelings of depersonalization were shown to be positively correlated with rCBF in right frontal cortex (Mathew and Wilson 1993; Mathew et al. 1999) and the anterior cingulate. In contrast, others only report positive correlations between cerebellar metabolism and ratings of intoxication (Volkow et al. 1991, 1996).
Studies examining brain functioning among individuals acutely intoxicated with THC while engaged in specific neurocognitive tasks are still few. When asked to perform a dichotic listening task during intoxication with cannabis, subjects showed typical patterns of increased rCBF in frontal, limbic, paralimbic, and cerebellar regions; however, decreased rCBF was observed in temporal lobe regions thought important for auditory attention (O’Leary et al. 2000), despite no differences on task performance compared to those that received a placebo (O’Leary et al. 2002). Intoxicated individuals have also been shown to perform more rapidly on a self-timed tapping task, suggesting altered time sense, which has been correlated with rCBF in the cerebellum (O’Leary et al. 2003). Studies employing fMRI with acutely intoxicated cannabis users may provide new and interesting findings in this area. Clearly, there remains much to be learned about the neural systems underlying the subjective effects and neuropsychological difficulties associated with acute cannabis intoxication.
Acute Effects of Cannabis on Neuropsychological Performance
Acute intoxication with cannabis produces changes in brain functioning and obvious subjective effects. Thus, it is not surprising that individuals acutely intoxicated with cannabis (or THC infusions) tend to demonstrate deficits on neuropsychological measures. Throughout the 1970s, several investigations had begun to characterize the neuropsychological deficits evident during acute intoxication with cannabis. A thorough review of studies published prior to 1980 on this topic suggested that results were somewhat equivocal on several measures of attention and executive functions, but a clear pattern of disruption in memory was present among intoxicated individuals (Ferraro 1980). Specifically, when subjects are presented with new information while acutely intoxicated, they show fairly consistent deficits in their ability to spontaneously recall the information. In contrast, no impairments are typically observed when intoxicated subjects are asked to recall information that was presented prior to cannabis administration (i.e., when sober). Similarly, no deficits are observed in recalling remote events and semantic knowledge. More recently, Ranganathan and D’Souza (2006) reviewed the extant literature on acute effects of marijuana (or THC) on neuropsychological functioning with a specific analysis of memory functions and arrived at similar conclusions based on the 35 studies they examined. They reported that the most consistent deficits are found on measures of immediate and delayed recall (but usually not recognition) of word-lists, prose, and nonverbal stimuli when information is presented to acutely intoxicated individuals—with no differences in recall for information learned prior to intoxication. Nonetheless, across all paradigms, individuals under the influence of THC were found to have a tendency to produce more intrusion and false positive errors when recalling information.
During recent years, measures of decision making, inhibitory control, and impulsivity have emerged as promising probes sensitive to neurobehavioral disturbances observed among individuals with substance dependence. For example, recent studies find that drug users perform more poorly than control participants on measures of impulsive decision-making (Bechara et al. 2001; Gonzalez et al. 2007; Grant et al. 2000), motor inhibition (Fillmore and Rush 2002), rate of discounting delayed rewards (Bechara et al. 2001; Kirby et al. 1999; Madden et al. 1997; Petry et al. 1998), and risk taking (Bornovalova et al. 2005; Crowley et al. 2006). At this time, however, only a few investigations have examined how decision making and inhibitory control are affected by acute administration of THC. McDonald et al. (2003) examined the performance of 37 adults with a prior history of cannabis use who were drug free on the day of testing on several measures of impulsivity (i.e., stop-signal, go/no-go, and delay discounting tasks) and found that higher doses of THC (15 mg oral dose), but not lower doses (7.5 mg) produced poorer performance on stop reaction times; however, neither dose produced effects on go/no-go and delay discounting tasks. Similarly, Ramaekers et al. (2006) found evidence of impairments on a stop-signal task, but not the Iowa Gambling Task (a measure of decision making) among 20 individuals with a history of cannabis use with standardized doses of THC via smoked cigarettes. In contrast, evidence for increased risky decision making was observed in a sample of 10 cannabis users administered standardized doses of cannabis cigarettes ranging from 0 to 3.58% THC, but only when given the highest dose (Lane et al. 2005).
In summary, individuals intoxicated with cannabis generally report pleasant subjective effects but demonstrate altered brain functioning and difficulties on specific measures of neuropsychological functioning. The most commonly observed changes in brain functioning are increased CBF and metabolism in various parts of the cortex, most notably in frontal regions, limbic and paralimbic structures, and the cerebellum. These changes often correlate with a subjective experience of intoxication. As it pertains to neuropsychological functions, acute intoxication with cannabis has most consistently demonstrated retrieval-based memory problems, but only for material presented when participants are intoxicated. Effects of THC on other neurocognitive functions, including measures of decision-making and inhibition, remain somewhat mixed at this time.
Non-Acute Effects of Cannabis Use
Methodological Considerations Important for Studies on Non-Acute Effects of Cannabis
It is a seemingly obvious assertion to note that individuals with a history of cannabis use are not always acutely intoxicated. As previously noted, 40.1% of individuals in the U.S. reported ever having used cannabis during 2005, but only 6% reported use during the prior month (SAMHSA 2005). As such, it can be argued that the non-acute effects of cannabis on brain functioning may present a greater public health issue. For apparent ethical reasons, healthy individuals with no history of substance use cannot be randomly assigned into groups that are administered varying amounts of cannabis in a supervised setting for a long period of time and later tested after different lengths of abstinence. Therefore, we rely on retrospective studies of individuals with a history of cannabis use and examine their performance relative to nonusers, often with cross-sectional designs. This retrospective approach yields valuable information, but is beset with various methodological challenges that limit causal inferences (Gonzalez et al. 2002; Pope 2002; Pope et al. 1995).
Studies examining the non-acute effects of cannabis use often employ participant samples that differ substantially on a variety of factors that may affect neuropsychological performance, such as varying length of abstinence, severity of substance use (e.g., amount, frequency, duration, degree of addiction), and presence of comorbid conditions (including other substance use and psychiatric disorders). Results might vary, for example, depending at what time point after abstinence participants are tested, since non-acute effects may be ascribed to different post-abstinence stages; that is, immediately after abstinence while withdrawal symptoms may be experienced (withdrawal effects), after withdrawal symptoms subside but with cannabinoids present to some extent in their bodies (residual effects), or after much time has elapsed since last use (long term or permanent effects) (e.g., Pope et al. 1995). Furthermore, studies may differ on whether cannabis users have a history of diagnosed substance-use disorders. Use and abuse of multiple illicit drugs over a lifetime is common among individuals with substance dependence. Therefore, it is difficult to find subject samples that have used only cannabis, and when such samples are successfully recruited, the ability to generalize from their findings is questionable. Finally, in all but a few of the studies on the non-acute effects of cannabis presented below, it remains unknown whether the observed neuropsychological deficits among cannabis users are the direct results of cannabis or may have predated cannabis use. There is ample literature showing genetic and neurobehavioral antecedent risk factors for substance dependence, which suggests that some neuropsychological problems may predate drug use (e.g., Vanyukov et al. 2003). Without the use of twin studies or longitudinal research designs that follow participants through various stages of drug use (before use, during use, and during multiple time points after abstinence), these important questions remain difficult to answer. As studies on the non-acute effects of cannabis use are presented below, it is important to keep these methodological issues in mind.
Neuroimaging Non-Acute Effects of Cannabis Use
As previously noted, several investigators have reviewed studies using brain imaging techniques to examine the effects of cannabis on human subjects (Crippa et al. 2005; Loeber and Yurgenlun-Todd 1999; Quickfall and Crockford 2006; Rojas et al. 2005; Solowij 1999). Quickfall and Crockford (2006) reported on ten investigations examining structural brain changes among abstinent cannabis users (Aasly et al. 1993; Block et al. 2000a; Campbell et al. 1971; Co et al. 1977; Hannerz and Hindmarsh 1983; Kuehnle et al. 1977; Matochik et al. 2005; Tzilos et al. 2005; Wiesbeck and Taeschner 1991; Wilson et al. 2000) and 12 investigations employing functional neuroimaging techniques (Amen and Waugh 1998; Block et al. 2000b, 2002; Eldreth et al. 2004; Kanayama et al. 2004; Lundqvist et al. 2001; Mathew et al. 1986, 1989; Pillay et al. 2004; Tunving et al. 1986; Volkow et al. 1996; Wilson et al. 2000).
Most studies of structural brain changes (the majority of which were older studies using CT) were deemed to suffer from significant methodological limitations, particularly from using cannabis users with significantly high comorbid use of other substances. Despite that, few investigations reported significant differences on CT scans of cannabis users compared to nonusers, which may not be surprising given the limited utility of CT to detect the subtle structural changes that may occur with cannabis use. The most methodologically sound studies all employed volumetric MRI techniques, but found disparate results—two showed no significant differences between cannabis users and controls (Block et al. 2000a; Tzilos et al. 2005), but another (Matochik et al. 2005) reported less brain volume than controls in some regions (R parahippocampal gyrus, L parietal lobe), but greater brain volumes in others (precentral gyrus, R thalamus). Interestingly, MRI was used to compare hippocampal volumes among adolescents with history of cannabis and alcohol use, alcohol use alone, and normal controls, but significantly smaller hippocampal volumes were found only among the group that only used alcohol (Medina et al. 2007). Of note, a recent study employing MR spectroscopy examined various regions of interest (putamen, globus pallidus, thalamus, dorsolateral prefrontal cortex, frontal white matter, hippocampus, ventral tegmental area, anterior cingulate, and posterior cingulate) among 13 current, frequent cannabis users compared to 13 controls, and found lower NAA/Cr ratios suggestive of neuronal injury only in the dorsolateral prefrontal cortex (Hermann et al. 2007). When taken together, most studies at this time do not provide evidence for structural brain abnormalities among abstinent cannabis users; however, more investigations using high resolution MRI and MRS with strong research designs are needed to better address this research question. Overall, findings of structural brain abnormalities among cannabis users remain equivocal, with disparate findings that may in part reflect the possibility that cannabis may affect brain tissue in distinct ways under different conditions.
As with studies on the acute effects of cannabis on brain functioning, most studies to date examining brain functioning among abstinent cannabis users have employed PET to examine rCBF at rest or during performance of a task. In contrast to increased brain metabolism usually observed during acute intoxication, the most consistent finding is lower brain metabolism among abstinent cannabis users compared to controls. Brain hypometabolism has been noted globally (Mathew et al. 1986, 1989; Tunving et al. 1986), and specifically in frontal lobes (Lundqvist et al. 2001) and cerebellum (Block et al. 2000b; Volkow et al. 1996). One investigation found evidence for decreased metabolism in temporal lobes (Amen and Waugh 1998). More recently, cerebral blood volume was found to be decreased in the right frontal, left temporal, and cerebellar regions of cannabis users after 6–36 h of abstinence compared to controls (Sneider et al. 2006). Thus, evidence is consistent for decreased CBF among abstinent cannabis users, but the specific brain regions where most affected differ somewhat across studies.
Several studies have examined changes in cerebral metabolism among abstinent cannabis users in response to a cognitive challenge. Block et al. (2002) found that recently abstinent, frequent users of cannabis showed decreased metabolism in prefrontal cortical regions, increased metabolism in cerebellum, and a different lateralization pattern of hippocampal metabolism relative to controls during one of several conditions of a list-learning task. Bolla and colleagues (2005) examined brain metabolism with PET during performance of the Iowa Gambling Task among a group of control participants and cannabis users with 25 days of supervised abstinence. They reported poorer overall performance among the abstinent cannabis users, as well as evidence of dose-related effects, with altered patterns of brain activation that included orbitofrontal and dorsolateral prefrontal cortex. Compared to matched controls, decreased activation on fMRI during an associative learning task was reported in prefrontal and hippocampal regions of frequent cannabis users who were abstinent, despite no structural differences (Jager et al. 2007). Another study reported decreased metabolism in left prefrontal regions and increased metabolism in hippocampus among 11 frequent cannabis users after 25 days of abstinence compared to matched controls while performing a modified version of the Stroop Color Word Task (Eldreth et al. 2004). Similarly, Gruber and Yurgelun-Todd (2005) found altered patterns of brain activation on fMRI in prefrontal cortex and anterior cingulate among nine heavy cannabis users (with recent use) compared to controls, while performing a Stroop Task. Using tasks of spatial working memory during fMRI, several investigators have reported altered patterns of brain activation among abstinent cannabis users that involve parietal cortex (Jager et al. 2006) as well as widespread patterns of increased and decreased activation involving prefrontal, striatal, and temporal brain regions (Chang et al. 2006; Kanayama et al. 2004). Among adolescents undergoing fMRI, Schweinsburg et al. (2005) found that those with alcohol use disorders and concomitant marijuana use showed different patterns of brain activation during a spatial working memory task in prefrontal and temporal regions compared to healthy controls and those who used alcohol alone. Decreased activation in supplementary motor cortex and anterior cingulate was observed on fMRI among nine recently abstinent (4–36 h) heavy cannabis users during a finger tapping task relative to 16 controls despite no differences between groups on task performance (Pillay et al. 2004). It is evident from these investigations that recently abstinent cannabis users show altered patterns of brain activation during various cognitive tasks, often despite no differences in task performance. Additional studies are still needed to understand the permanence of these changes despite continued abstinence. Furthermore, as new methodologies emerge, it will be interesting to understand the types of structural and neurochemical changes that account for altered patterns of brain activation in the absence of discernable functional impairments and their clinical significance.
Non-Acute Effects of Cannabis Use on Neuropsychological Functioning
Studies employing functional neuroimaging provide valuable information on differences in brain functioning that may be attributable to cannabis use. However, changes in brain functioning and metabolism are not synonymous with functional impairments. Arguably, studies examining performance on neuropsychological instruments shed more light on this subject. Further, such studies often employ large batteries of tests that provide information on significant deficits, as well as areas of spared performances, within the same subject sample. Investigations using this approach are plentiful, but methodological problems in such studies also abound. This may, in part, contribute to the disparity in conclusions across the many reviews conducted on the topic of non-acute effects of cannabis (e.g., Iversen 2000; Pope et al. 1995; Solowij 1998, 1999; Wert and Raulin 1986). For example, some conclude “...no evidence that marijuana...leads to functional impairment” (Wert and Raulin 1986). Others note “...the data support a ‘drug residue’ effect...but evidence is as yet insufficient to support or refute a...toxic effect on the CNS” (Pope et al. 1995). Yet others purport that “...long-term use of cannabis leads to a more subtle and selective impairment of cognitive function” (Solowij et al. 2002).
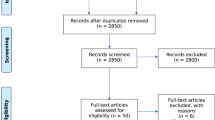
A recent systematic review by Gonzalez et al. (2002) summarized 40 investigations on the non-acute effects of cannabis on neuropsychological functioning, which dated from 1973 to 2002. The authors established a set of criteria pertinent to study design deemed essential to yield interpretable results regarding non-acute effects of cannabis use. Criteria were: (1) a study sample of subjects whose predominant or exclusive drug of abuse was cannabis; (2) an appropriate control group with limited or no cannabis use history; (3) use of valid and standardized neuropsychological tests; (4) abstinence from all substances of abuse at testing; (5) reported length of abstinence from cannabis; (6) adequate controls for effects of other substance use among cannabis users; and (7) obtained and controlled for neurological and mental health history. It is worth noting that these criteria represented minimal standards—optimal cross-sectional designs should contain a control and cannabis group that are well matched on as many potential confounds and premorbid factors as possible. Further, urine toxicology testing should be employed to ensure abstinence at the time of testing. In the absence of such standards, a variety of possible confounds could account for any significant differences obtained between groups. Surprisingly, only 13 of the 40 studies reviewed met all criteria. Thus, some caution was warranted when interpreting the totality of findings from existing studies at the time.
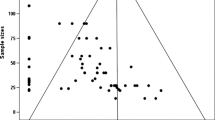
Qualitative reviews are also prone to several constraints that can be addressed through the use of meta-analytic techniques. For example, bias may be present across reviewers who may find different features of a study’s findings salient. Additionally, individual studies are often underpowered to detect subtle effects. Such studies would be interpreted by a reviewer as yielding a null finding. Meta-analysis addresses these issues by arriving at quantitative estimates that provide information on both magnitude and statistical significance of effects that are pooled and appropriately weighted (i.e., sample size and variance) across investigations. However, meta-analysis relies on the quality of the studies included.
In order to improve interpretability of published findings and arrive at quantitative estimates of a possible residual effect of cannabis use, a meta-analysis was conducted by Grant et al. (2003) using the same pool of investigations identified by Gonzalez et al. (2002). An additional criterion was added that required investigations to provide sufficient statistical information to allow calculations of effect sizes for meta-analysis, resulting in the exclusion of some studies (e.g., Fletcher et al. 1996). In total, all criteria were met by 11 investigations (Block and Ghoneim 1993; Carlin and Trupin 1977; Croft et al. 2001; Ehrenreich et al. 1999; Gouzoulis-Mayfrank et al. 2000; Hamil 1996; Pope and Yurgelun-Todd 1996; Pope et al. 2001; Rodgers 2000; Solowij 1995; Solowij et al. 2002). An additional four studies were added (Deif et al. 1993; Grant et al. 1973; Rochford et al. 1977; Wig and Varma 1977) after slightly relaxing the criteria, yielding a total of 15, providing data on 1,188 subjects (704 cannabis users and 484 nonusers). Across studies, participants’ history of cannabis use tended to involve smoking cannabis multiple times a week, with an average duration of use across studies that ranged from a couple of years to several decades. When recorded, average length of abstinence from cannabis across studies was fairly recent, but ranged from approximately 24 h to several months. Data were aggregated across studies to obtain effect sizes indicative of performance differences between cannabis-using groups and non-using groups on eight separate domains of neuropsychological functioning (simple reaction time, attention, verbal/language, abstraction/executive, perceptual motor, motor, learning, and forgetting) and on an overall index of neuropsychological performance. Findings were comparable when considering the 11 studies that met all criteria and the larger set of 15 studies. Overall, evidence emerged for a “residual cannabis effect” that was statistically significant but of small magnitude (d = −0.15, 99% CI [−0.29, −0.2]), suggesting that cannabis users’ neuropsychological performance was about one-fifth of a standard deviation worse than controls. A confidence interval containing “zero” would suggest no significant effect. When examining effect sizes obtained for individual neuropsychological domains, the only statistically significant effects were observed for learning (d = −0.21, 99% CI [−0.39, −0.02]) and forgetting (d = −0.27, 99% CI [−0.49, −0.4]). Thus, results from the meta-analysis suggested residual effects of cannabis use on memory, but of small magnitude. It is worth noting that these results are consistent with the types of deficits most commonly observed among individuals acutely intoxicated with cannabis (i.e., memory deficits), suggesting that such deficits may persist after intoxication subsides. However, longitudinal investigations are required to better characterize the duration of possible residual deficits.
Several studies have been published after the meta-analysis, indicating the presence of neuropsychological deficits among abstinent heavy cannabis users compared to controls in various neurocognitive abilities, including measures of decision making. For example, Bolla et al. (2002) examined a sample of 22 nontreatment-seeking heavy cannabis users who reported smoking a median of 35 joints per week and underwent 28 days of supervised abstinence prior to neuropsychological assessment. They found that higher frequency of cannabis-use correlated with poorer performance across most neuropsychological measures, including tests of memory, executive functions, inhibitory control, and psychomotor speed. Others have recently reported poorer performance among both short- and long-term cannabis users on measures of verbal memory, language functions, and processing speed compared to controls after 24 h of abstinence (Messinis et al. 2006). Paradoxically, deficits on measures of information-processing speed, compared to 22 controls, were also reported among 22 heavy cannabis users while abstinent, but not while acutely intoxicated (Kelleher et al. 2004). Deficits on the Iowa Gambling Task have also been demonstrated among abstinent heavy cannabis users compared to controls (Bolla et al. 2005; Verdejo-Garcia et al. 2007; Whitlow et al. 2004), even after 25 days of supervised abstinence (Bolla et al. 2005; Verdejo-Garcia et al. 2007). These recent investigations provide valuable evidence, but most have employed small samples of cannabis users (between 10 and 22) and are also subject to some of the methodological problems previously discussed. Furthermore, it has yet to be determined if these deficits are specific to cannabis (or drug use in general) or if they were present prior to initiation of cannabis use. Like the results from the cannabis meta-analysis, these studies cannot establish a causal link between cannabis use and its neuropsychological effects nor can they confidently determine the course of changes in neuropsychological functioning that may occur after abstinence.
A few investigations have employed longitudinal, within-subjects designs with neuropsychological tests administered at different time points after verified abstinence in order to strengthen causal inferences between cannabis use and its effects on neuropsychological functioning. Pope and colleagues (2001) examined groups of former heavy cannabis users (n = 45), current heavy cannabis users (n = 63), and non-using controls (n = 72) that completed thorough neuropsychological assessments at days 0, 1, 7, and 28 of supervised abstinence. Only current heavy users performed more poorly than controls (on measures of verbal memory); however, these differences were only observed on days 0, 1, and 7, with no significant differences detected by day 28. Thus, recently abstinent heavy cannabis users evidenced impairments only on measures of memory, which dissipated after approximately one month, suggesting that impairments observed soon after abstinence likely reflect a withdrawal or residual effect.
Two studies by another research group (Fried and Smith 2001; Fried et al. 2005) examined the neuropsychological performance of a large cohort (n = 74 and n = 113) of longitudinally followed individuals at ages 9–12 years old and again at 17–20 years of age. At follow-up, all subjects were classified into subgroups according to severity of current and previous cannabis use: (1) current regular heavy cannabis smokers (>5 joints/week); (2) current regular light smokers (<5 joints/week); 3) former regular smokers (no regular use for at least 3 months and no more than two joints in the last two months); and (4) a control group who reported not using cannabis regularly. This longitudinal design allowed consideration of an individual’s actual (rather than estimated) neuropsychological functioning before and after initiation of regular cannabis use. Groups were fairly well-matched, with adequate control of pertinent confounds and current cannabis users reported abstinence for at least one day prior to testing. Relative to their baselines, only current heavy cannabis users demonstrated a statistically significant decrease in IQ scores (four point difference), immediate and delayed memory, and information-processing speed. However, effect sizes were fairly small for each of these comparisons with no control for Type-I error despite numerous statistical tests. Current light users and former heavy users were not found to differ significantly from controls, suggesting that deficits in neuropsychological functioning (when present) are most likely to been seen only among current heavy users. However, unlike the study by Pope et al. 2001, these authors were unable to retest the group of current heavy users after a longer period of abstinence to determine the persistence of their deficits.
Another unique investigation that overcomes the issue of possible premorbid differences between cannabis users and nonusers employed a comprehensive battery of neuropsychological tests to examine 54 monozygotic male twin pairs discordant for history of cannabis use (Lyons et al. 2004). Twin pairs were genetically identical, raised in the same home and did not differ on history of alcohol, other drug use, or indices of achievement (e.g., employment, educational attainment, school grades, and academic difficulties). On average, those with history of cannabis use first began regular use of cannabis at about 21 years of age (range = 19–43) for an average duration of about 6 years (range 1–22 years). No participants reported using cannabis at least one year prior to testing, with last regular use occurring about 27 years prior on average. Of over 50 different indices of neuropsychological performance examined, statistically significant differences of very small magnitude were only observed on one measure of visuoconstructional abilities (Block Design).
When taken together, investigations on non-acute effects of cannabis use indicate that abstinent cannabis users experience poorer neuropsychological performance than noncannabis-using controls. These deficits appear to be of small magnitude, generally circumscribed to memory, and appear to resolve within weeks. Furthermore, the totality of evidence suggests that any deficits observed are most likely to be seen only among heavy, frequent users of cannabis, notwithstanding acute cannabis intoxication. Some evidence suggests that heavy cannabis use may produce deficits on measures of decision-making and inhibitory control that persist for longer. At this time, however, it has not been determined if such deficits are a result of cannabis use or if they represent premorbid problems that may have contributed to the development of a cannabis use disorder.
Cannabis Abuse, Dependence, and Addiction
All drugs of abuse appear to exert similar effects on the brain’s reward pathways that may lead to development of drug addiction among a subset of individuals–cannabis is no exception. Indeed, the endocannabinoid signaling system has been implicated in the neuropathophysiology of drug addiction (Maldonado et al. 2006). Addiction has been described as a chronic brain disease that involves compulsive use of a substance in the face of negative consequences (Leshner 1997). Such problematic use can have dire consequences on social and vocational functioning, since the addicted individual may engage in use of the drug at the expense of other important daily activities at home and at work. The DSM-IV-TR provides diagnostic criteria for cannabis dependence and abuse which requires individuals to exhibit various behaviors suggestive of addiction to obtain a diagnosis. For example, diagnostic criteria for cannabis dependence requires a maladaptive pattern of use that leads to significant impairment and may include such features as tolerance to the drug, withdrawal, unsuccessful attempts to quit, and disruptions in social, occupational, or recreational activities. As noted earlier, 1.7% of the U.S. population over 12 years old met criteria for a cannabis substance use disorder during 2005 (Substance Abuse and Mental Health Services Administration 2005). Furthermore, of people who have undergone substance use treatment, 27% reported cannabis as the drug for which treatment was sought (Substance Abuse and Mental Health Services Administration 2005). Although most individuals that have ever used cannabis will not meet criteria for a substance use disorder, the use of cannabis presents a significant impediment for the 4,090,000 in the U.S. that did meet criteria during 2005 (Substance Abuse and Mental Health Services Administration 2005).
The ability of prolonged cannabis administration to produce tolerance and withdrawal symptoms in animals has been the topic of several recent reviews (Gonzalez et al. 2005; Maldonado 2002; Tanda and Goldberg 2003). Based on current evidence, consensus exists for development of tolerance in animals receiving long-term administration of THC and that after administering a potent CB1 antagonist (SR 141716A), withdrawal symptoms emerge. However, evidence for a withdrawal syndrome (or abstinence phenomena) is inconsistent when animals undergo natural discontinuation. In humans, mounting evidence supports a withdrawal syndrome among long-term frequent cannabis users undergoing abstinence. Budney et al. (2004) report that findings from several well-controlled inpatient laboratory and outpatient studies demonstrate that chronic daily cannabis smokers reliably display unfavorable symptoms upon abstinence that emerge by 48 h after cessation of use, peak between two and six days, and remit within one to two weeks. Based on evidence from 20 studies, they proposed criteria for a cannabis withdrawal syndrome that is characterized by “significant distress or dysfunction” from at least four of the following symptoms: anger and aggression, decreased appetite or weight loss, irritability, nervousness/anxiety, restlessness, sleep difficulties, chills, depressed mood, stomach pain, shakiness, and sweating. The authors report that the criteria were formulated on the basis of investigations in which the samples were comprised of chronic daily cannabis smokers. They emphasize the need for more research to determine the quantity, frequency, and duration of cannabis use that is necessary to elicit a withdrawal syndrome.
Summary and Concluding Remarks
The past two decades have experienced remarkable breakthroughs in understanding the mechanisms by which cannabis produces its psychoactive effects. An endocannabinoid signaling system that includes cannabinoid receptors to which THC binds has been discovered and characterized in the human brain. This system has been implicated in regulation of various brain functions and shows great promise for therapeutic applications (Grant and Cahn 2005).
Scientific advances have also been made in understanding the neurobehavioral consequences of cannabis use through the use of neuroimaging. Current evidence clearly demonstrates changes in brain functioning among acutely intoxicated and abstinent cannabis users. The most consistent findings are of increased blood blow or hypermetabolism during acute intoxication and decreased blood flow or hypometabolism during recent abstinence, when participants are at rest. The duration of these changes after abstinence is less clear but may persist for weeks. Subtle differences in brain functioning have also been reported among abstinent cannabis users involved in various neurocognitive tasks; as expected, however, the specific brain regions affected vary according to task and across studies. These changes in brain functioning do not necessarily translate to functional impairments, since abstinent cannabis users in such studies often reveal no differences on task performance. Neither do differences in brain functioning translate to evidence for structural damage. Indeed, evidence for structural brain damage in humans as a result of cannabis use remains equivocal, and it may be that various yet unknown circumstances may affect whether cannabis will exert neurotoxic or neuroprotective effects.
Poorer performances on measures of neuropsychological functioning are also observed among cannabis users. Those who are acutely intoxicated show deficits in memory that appear specific to material presented during acute intoxication and usually only during free recall paradigms when recognition cues are not provided. Such deficits can be best characterized as “retrieval-based,” which would suggest disruptions of prefrontal brain circuits rather than frank damage to hippocampal structures. Consistent with this interpretation is evidence for intrusion and false positive errors during memory testing and functional neuroimaging studies that more often reveal disturbances in prefrontal structures than in the temporal lobes. It may be that disruptions in brain structures outside the mid-temporal lobes more likely mediate cannabis-related memory problems, which may be “executive” in nature. Poorer memory is also the most reliably detected deficit among abstinent cannabis users, which suggests that memory disturbances experienced during acute use persist after intoxication subsides. However, these deficits appear to be mild and transient.
At this time, the preponderance of evidence suggests circumscribed deficits of small magnitude that are most commonly seen with frequent and heavy use of cannabis. Individuals with such patterns of use may also be those most likely to be addicted to cannabis and meet criteria for a cannabis-related substance-use disorder. Although they represent only a small percentage of those that have ever tried cannabis, in the United States alone they numbered more than 4 million during 2005. Thus, cannabis use disorders are of significant concern for public health. Given the significant negative impact that drug addiction can have on an individual’s life, it can be argued that one of the greatest neurobehavioral liabilities from cannabis use is its potential for addiction. These potential risks must be weighed in tandem with the developing therapeutic applications of cannabis and specific cannabinoids, since the risk for development of dependence and limited risk for neuropsychological deficits may not be sufficient to contraindicate use under many circumstances.
The progress made in understanding the effects of cannabis use on brain functioning and resulting neurobehavioral consequences has been exciting. Equally provocative are the many important questions that are yet unanswered. What differences exist between those that develop a cannabis addiction and those that do not? Under what conditions will cannabis be neuroprotective or neurotoxic? What changes in brain structure and function occur with different patterns of cannabis use, what is their clinical significance, and how long do they last? Is smoking cannabis sufficiently harmful to brain functioning to undermine its therapeutic use? At this time, it remains as important as ever that scientific evidence continue to inform the complex social, political, and legal debates that often surround this complicated drug.
References
Aasly, J., Storsaeter, O., Nilsen, G., Smevik, O., & Rinck, P. (1993). Minor structural brain changes in young drug abusers. A magnetic resonance study. Acta Neurologica Scandanivica, 87, 210–214.
Agurell, S., Halldin, M., Lindgren, J. E., Ohlsson, A., Widman, M., Gillespie, H., et al. (1986). Pharmacokinetics and metabolism of delta 1-tetrahydrocannabinol and other cannabinoids with emphasis on man. Pharmacology Review, 38, 21–43.
Amen, D. G., & Waugh, M. (1998). High resolution brain SPECT imaging of marijuana smokers with AD/HD. Journal of Psychoactive Drugs, 30, 209–214.
Anthony, J. C., Warner, L. A., & Kessler, R. C. (1994). Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: Basic findings from the National Comorbidity Survey. Experimental and Clinical Psychopharmacology, 2, 244–268.
Bechara, A., Dolan, S., Denburg, N., Hindes, A., Anderson, S. W., & Nathan, P. E. (2001). Decision-making deficits, linked to a dysfunctional ventromedial prefrontal cortex, revealed in alcohol and stimulant abusers. Neuropsychologia, 39, 376–389.
Block, R. I., Erwin, W. J., Farinpour, R., & Braverman, K. (1998). Sedative, stimulant, and other subjective effects of marijuana: relationships to smoking techniques. Pharmacology Biochemistry and Behavior, 59, 405–412.
Block, R. I., & Ghoneim, M. M. (1993). Effects of chronic marijuana use on human cognition. Psychopharmacology, 110, 219–228.
Block, R. I., O’Leary, D. S., Ehrhardt, J. C., Augustinack, J. C., Ghoneim, M. M., Arndt, S., et al. (2000a). Effects of frequent marijuana use on brain tissue volume and composition. Neuroreport, 11, 491–496.
Block, R. I., O’Leary, D. S., Hichwa, R. D., Augustinack, J. C., Boles Ponto, L. L., Ghoneim, M. M., et al. (2002). Effects of frequent marijuana use on memory-related regional cerebral blood flow. Pharmacology Biochemistry and Behavior, 72, 237–250.
Block, R. I., O’Leary, D. S., Hichwa, R. D., Augustinack, J. C., Ponto, L. L. B., Ghoneim, M. M., et al. (2000b). Cerebellar hypoactivity in frequent marijuana users. Neuroreport, 11, 749–753.
Bolla, K. I., Brown, K., Eldreth, D., Tate, K., & Cadet, J. L. (2002). Dose-related neurocognitive effects of marijuana use. Neurology, 59, 1337–1343.
Bolla, K. I., Eldreth, D. A., Matochik, J. A., & Cadet, J. L. (2005). Neural substrates of faulty decision-making in abstinent marijuana users. Neuroimage, 26, 480–492.
Bornovalova, M. A., Daughters, S. B., Hernandez, G. D., Richards, J. B., & Lejuez, C. W. (2005). Differences in impulsivity and risk-taking propensity between primary users of crack cocaine and primary users of heroin in a residential substance-use program. Experimental and Clinical Psychopharmacology, 13, 311–318.
Breivogel, C. S., Griffin, G., Di Marzo, V., & Martin, B. R. (2001). Evidence for a new G protein-coupled cannabinoid receptor in mouse brain. Molecular Pharmacology, 60, 155–163.
Budney, A. J., Hughes, J. R., Moore, B. A., & Vandrey, R. (2004). Review of the validity and significance of cannabis withdrawal syndrome. American Journal of Psychiatry, 161, 1967–1977.
Campbell, A. M., Evans, M., Thomson, J. L., & Williams, M. J. (1971). Cerebral atrophy in young cannabis smokers. Lancet, 2, 1219–1224.
Carlin, A. S., & Trupin, E. W. (1977). The effect of long-term chronic marijuana use on neuropsychological functioning. International Journal of the Addictions, 12, 617–624.
Chang, L., Yakupov, R., Cloak, C., & Ernst, T. (2006). Marijuana use is associated with a reorganized visual-attention network and cerebellar hypoactivation. Brain, 129, 1096–1112.
Chevaleyre, V., & Castillo, P. E. (2004). Endocannabinoid-mediated metaplasticity in the hippocampus. Neuron, 43, 871–881.
Childers, S. R., Pacheco, M. A., Bennett, B. A., Edwards, T. A., Hampson, R. E., Mu, J., et al. (1993). Cannabinoid receptors: G-protein-mediated signal transduction mechanisms. Biochemical Society Symposia, 59, 27–50.
Co, B. T., Goodwin, D. W., Gado, M., Mikhael, M., & Hill, S. Y. (1977). Absence of cerebral atrophy in chronic cannabis users. Evaluation by computerized transaxial tomography. Journal of the American Medical Association, 237, 1229–1230.
Compton, W. M., Grant, B. F., Colliver, J. D., Glantz, M. D., & Stinson, F. S. (2004). Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. Journal of the American Medical Association, 291, 2114–2121.
Crippa, J. A., Lacerda, A. L., Amaro, E., Busatto, F. G., Zuardi, A. W., & Bressan, R. A. (2005). Brain effects of cannabis-neuroimaging findings. Revista Brasileira de Psiquiatria, 27, 70–78.
Croft, R. J., Mackay, A. J., Mills, A. T. D., & Gruzelier, J. G. H. (2001). The relative contributions of ecstasy and cannabis to cognitive impairment. Psychopharmacology, 153, 373–379.
Crowley, T. J., Raymond, K. M., Mikulich-Gilbertson, S. K., Thompson, L. L., & Lejuez, C. W. (2006). A risk-taking “set” in a novel task among adolescents with serious conduct and substance problems. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 175–183.
Davies, S. N., Pertwee, R. G., & Riedel, G. (2002). Functions of cannabinoid receptors in the hippocampus. Neuropharmacology, 42, 993–1007.
Deif, A., El, S. A., & Fawzy, R. K. (1993). Neurological, psychiatric and C.T. evaluation of chronic cannabis smokers. Journal of the Medical Research Institute, 14, 151–160.
De Petrocellis, L., Cascio, M. G., & Di Marzo, V. (2004). The endocannabinoid system: a general view and latest additions. British Journal of Pharmacology, 141, 765–774.
Devane, W. A., Dysarz, F. A., III, Johnson, M. R., Melvin, L. S., & Howlett, A. C. (1988). Determination and characterization of a cannabinoid receptor in rat brain. Molecular Pharmacology, 34, 605–613.
Devane, W. A., Hanus, L., Breuer, A., Pertwee, R. G., Stevenson, L. A., Griffin, G., et al. (1992). Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science, 258, 1946–1949.
Di Marzo, V., Breivogel, C. S., Tao, Q., Bridgen, D. T., Razdan, R. K., Zimmer, A. M., et al. (2000). Levels, metabolism, and pharmacological activity of anandamide in CB1 cannabinoid receptor knockout mice: Evidence for non-CB1, non-CB2 receptor-mediated actions of anandamide in mouse brain. Journal of Neurochemistry, 75, 2434–2444.
Ehrenreich, H., Rinn, T., Kunert, H. J., Moeller, M. R., Poser, W., Schilling, L., et al. (1999). Specific attentional dysfunction in adults following early start of cannabis use. Psychopharmacology, 142, 295–301.
Eldreth, D. A., Matochik, J. A., Cadet, J. L., & Bolla, K. I. (2004). Abnormal brain activity in prefrontal brain regions in abstinent marijuana users. Neuroimage, 23, 914–920.
Ellis, G. M., Jr., Mann, M. A., Judson, B. A., Schramm, N. T., & Tashchian, A. (1985). Excretion patterns of cannabinoid metabolites after last use in a group of chronic users. Clinical Pharmacology and Therapeutics, 38, 572–578.
ElSohly, M. A., Ross, S. A., Mehmedic, Z., Arafat, R., Yi, B., & Banahan, B. F. (2000). Potency trends of Delta(9)-THC and other cannabinoids in confiscated marijuana from 1980–1997. Journal of Forensic Sciences, 45, 24–30.
ElSohly, M. A., & Slade, D. (2005). Chemical constituents of marijuana: the complex mixture of natural cannabinoids. Life Sciences, 78, 539–548.
Eubanks, L. M., Rogers, C. J., Beuscher, A. E., Koob, G. F., Olson, A. J., Dickerson, T. J., et al. (2006). A molecular link between the active component of marijuana and Alzheimer’s disease pathology. Molecular Pharmacology, 3, 773–777.
European Monitoring Centre for Drugs and Drug Addiction. (2004). Annual Report 2004: The state of the drugs problem in the European Union and Norway Luxembourg: Office for Official Publications of the European Communities.
Ferraro, D. P. (1980). Acute effects of marijuana on human memory and cognition. In R. C.Petersen (Ed.), Marijuana research findings: 1980. Washington D.C.: Department of Health and Human Services.
Fillmore, M. T., & Rush, C. R. (2002). Impaired inhibitory control of behavior in chronic cocaine users. Drug and Alcohol Dependence, 66, 265–273.
Fisk, J. E., Montgomery, C., Wareing, M., & Murphy, P. N. (2006). The effects of concurrent cannabis use among ecstasy users: neuroprotective or neurotoxic? Human Psychopharmacology, 21, 355–366.
Fletcher, J. M., Page, J. B., Francis, D. J., Copeland, K., Naus, M. J., Davis, C. M., et al. (1996). Cognitive correlates of long-term cannabis use in Costa Rican men. Archives of General Psychiatry, 53, 1051–1057.
Fride, E., Foox, A., Rosenberg, E., Faigenboim, M., Cohen, V., Barda, L., et al. (2003). Milk intake and survival in newborn cannabinoid CB1 receptor knockout mice: evidence for a “CB3” receptor. European Journal of Pharmacology, 461, 27–34.
Fried, P. A., & Smith, A. M. (2001). A literature review of the consequences of prenatal marihuana exposure. An emerging theme of a deficiency in aspects of executive function. Neurotoxicology and Teratology, 23, 1–11.
Fried, P. A., Watkinson, B., & Gray, R. (2005). Neurocognitive consequences of marihuana—a comparison with pre-drug performance. Neurotoxicology and Teratology, 27, 231–239.
Galiegue, S., Mary, S., Marchand, J., Dussossoy, D., Carriere, D., Carayon, P., et al. (1995). Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. European Journal of Biochemistry, 232, 54–61.
Glass, M., Brotchie, J. M., & Maneuf, Y. P. (1997a). Modulation of neurotransmission by cannabinoids in the basal ganglia. Eureopean Journal of Neuroscience, 9, 199–203.
Glass, M., Dragunow, M., & Faull, R. L. (1997b). Cannabinoid receptors in the human brain: A detailed anatomical and quantitative autoradiographic study in the fetal, neonatal and adult human brain. Neuroscience, 77, 299–318.
Gonzalez, R., Bechara, A., & Martin, E. M. (2007). Executive functions among individuals with methamphetamine or alcohol as drugs of choice: Preliminary observations. Journal of Clininical and Experimental Neuropsychology, 29, 155–159.
Gonzalez, R., Carey, C., & Grant, I. (2002). Nonacute (Residual) neuropsychological effects of cannabis use: A qualitative analysis and systematic review. Journal of Clinical Pharmacology, 42, 48S–57S.
Gonzalez, S., Cebeira, M., & Fernandez-Ruiz, J. (2005). Cannabinoid tolerance and dependence: a review of studies in laboratory animals. Pharmacology Biochemistry and Behavior, 81, 300–318.
Gonzalez, R., Rippeth, J. D., Carey, C. L., Heaton, R. K., Moore, D. J., Schweinsburg, B. C., et al. (2004). Neurocognitive performance of methamphetamine users discordant for history of marijuana exposure. Drug and Alcohol Dependence, 76, 181–190.
Gouzoulis-Mayfrank, E., Daumann, J., Tuchtenhagen, F., Pelz, S., Becker, S., Kunert, H. J., et al. (2000). Impaired cognitive performance in drug free users of recreational ecstasy (MDMA). Journal of Neurology, Neurosurgery and Psychiatry, 68, 719–725.
Grant, I. & Cahn, B. R. (2005). Cannabis and endocannabinoid modulators: Therapeutic promises and challenges. Clinical Neuroscience Research, 5(2–4), 185–199.
Grant, S., Contoreggi, C., & London, E. D. (2000). Drug abusers show impaired performance in a laboratory test of decision making. Neuropsychologia, 38, 1180–1187.
Grant, I., Gonzalez, R., Carey, C. L., Natarajan, L., & Wolfson, T. (2003). Non-acute (residual) neurocognitive effects of cannabis use: A meta-analytic study. Journal of the International Neuropsychological Society, 9, 679–689.
Grant, I., Rochford, J., Fleming, T., & Stunkard, A. (1973). A neuropsychological assessment of the effects of moderate marihuana use. Journal of Nervous & Mental Disease, 156, 278–280.
Green, B., Kavanagh, D., & Young, R. (2003). Being stoned: a review of self-reported cannabis effects. Drug and Alcohol Review, 22, 453–460.
Grotenhermen, F. (2003). Pharmacokinetics and pharmacodynamics of cannabinoids. Clinical Pharmacokinetics, 42, 327–360.
Gruber, S. A., & Yurgelun-Todd, D. A. (2005). Neuroimaging of marijuana smokers during inhibitory processing: A pilot investigation. Brain Research, 23, 107–118.
Grundy, R. I. (2002). The therapeutic potential of the cannabinoids in neuroprotection. Expert Opinions on Investigational Drugs, 11, 1365–1374.
Guzman, M., Sanchez, C., & Galve-Roperh, I. (2001). Control of the cell survival/death decision by cannabinoids. Journal of Molecular Medicine, 78, 613–625.
Hamil, W. L. (1996). Auditory learning and memory performance among veterans with a history of stimulant abuse. Dissertation Abstracts International: Section B: The Sciences & Engineering, 56, 5806.
Hampson, A. J., Grimaldi, M., Lolic, M., Wink, D., Rosenthal, R., & Axelrod, J. (2000). Neuroprotective antioxidants from marijuana. Annals of the New York Academy of Sciences, 899, 274–282.
Hannerz, J., & Hindmarsh, T. (1983). Neurological and neuroradiological examination of chronic cannabis smokers. Annals of Neurology, 13, 207–210.
Hanus, L., Abu-Lafi, S., Fride, E., Breuer, A., Vogel, Z., Shalev, D. E., et al. (2001). 2-Arachidonyl glyceryl ether, an endogenous agonist of the cannabinoid CB1 receptor. Proceedings of the National Academy of Sciences of the United States of America, 98, 3662–3665.
Heishman, S. J., Stitzer, M. L., & Yingling, J. E. (1989). Effects of tetrahydrocannabinol content on marijuana smoking behavior, subjective reports, and performance. Pharmacology Biochemistry and Behavior, 34, 173–179.
Herkenham, M., Lynn, A. B., Little, M. D., Johnson, M. R., Melvin, L. S., de Costa, B. R., et al. (1990). Cannabinoid receptor localization in brain. Proceedings of the National Academy of Sciences, 87, 1932–1936.
Hermann, D., Sartorius, A., Welzel, H., Walter, S., Skopp, G., Ende, G., et al. (2007). Dorsolateral prefrontal cortex n-acetylaspartate/total creatine (NAA/tCr) loss in male recreational cannabis users. Biolgical Psychiatry, 61, 1281–1289.
Herning, R. I., Hooker, W. D., & Jones, R. T. (1986). Tetrahydrocannabinol content and differences in marijuana smoking behavior. Psychopharmacology, 90, 160–162.
Huestis, M. A., Mitchell, J. M., & Cone, E. J. (1996). Urinary excretion profiles of 11-nor-9-carboxy-delta 9-tetrahydrocannabinol in humans after single smoked doses of marijuana. Journal of Analytical Toxicology, 20, 441–452.
Iversen, L. L. (2000). The science of marijuana. New York: Oxford University Press.
Jager, G., Kahn, R. S., Van Den, B. W., Van Ree, J. M., & Ramsey, N. F. (2006). Long-term effects of frequent cannabis use on working memory and attention: an fMRI study. Psychopharmacology, 185, 358–368.
Jager, G., Van Hell, H. H., De Win, M. M., Kahn, R. S., Van Den, B. W., Van Ree, J. M., et al. (2007). Effects of frequent cannabis use on hippocampal activity during an associative memory task. European Neuropsychopharmacology, 17, 289–297.
Jiang, H. E., Li, X., Zhao, Y. X., Ferguson, D. K., Hueber, F., Bera, S., et al. (2006). A new insight into Cannabis sativa (Cannabaceae) utilization from 2500-year-old Yanghai Tombs, Xinjiang, China. Journal of Ethnopharmacology, 108, 414–422.
Johnston, L. D., O’Malley, P. M., Bachman, J. G., & Schulenberg, J. E. (2006). Monitoring the future study. Washington, DC: NIDA.
Kanayama, G., Rogowska, J., Pope, H. G., Gruber, S. A., & Yurgelun-Todd, D. A. (2004). Spatial working memory in heavy cannabis users: A functional magnetic resonance imaging study. Psychopharmacology, 176, 239–247.
Kelleher, L. M., Stough, C., Sergejew, A. A., & Rolfe, T. (2004). The effects of cannabis on information-processing speed. Addictive Behaviors, 29, 1213–1219.
Kirby, K. N., Petry, N. M., & Bickel, W. K. (1999). Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology-General, 128, 78–87.
Kuehnle, J., Mendelson, J. H., Davis, K. R., & New, P. F. (1977). Computed tomographic examination of heavy marijuana smokers. Journal of the American Medical Association, 237, 1231–1232.
Landfield, P. W., Cadwallader, L. B., & Vinsant, S. (1988). Quantitative changes in hippocampal structure following long-term exposure to delta 9-tetrahydrocannabinol: Possible mediation by glucocorticoid systems. Brain Research, 443, 47–62.
Lane, S. D., Cherek, D. R., Tcheremissine, O. V., Lieving, L. M., & Pietras, C. J. (2005). Acute marijuana effects on human risk taking. Neuropsychopharmacology, 30, 800–809.
Lawston, J., Borella, A., Robinson, J. K., & Whitaker-Azmitia, P. M. (2000). Changes in hippocampal morphology following chronic treatment with the synthetic cannabinoid WIN 55,212-2. Brain Research, 877, 407–410.
Leshner, A. I. (1997). Addiction is a brain disease, and it matters. Science, 278, 45–47
Loeber, R. T. & Yurgelun-Todd, D. A. (1999). Human neuroimaging of acute and chronic marijuana use: Implications for frontocerebellar dysfunction. Human Psychopharmacology-Clinical and Experimental, 14, 291–304.
Lundqvist, T., Jonsson, S., & Warkentin, S. (2001). Frontal lobe dysfunction in long-term cannabis users. Neurotoxicology and Teratology, 23, 437–443.
Lyons, M. J., Bar, J. L., Panizzon, M. S., Toomey, R., Eisen, S., Xian, H., et al. (2004). Neuropsychological consequences of regular marijuana use: A twin study. Psychological Medicine, 34, 1239–1250.
Madden, G. J., Petry, N. M., Badger, G. J., & Bickel, W. K. (1997). Impulsive and self-control choices in opioid-dependent patients and non-drug-using control participants: Drug and monetary rewards. Experimental and Clinical Psychopharmacology, 5, 256–262.
Maejima, T., Ohno-Shosaku, T., & Kano, M. (2001). Endogenous cannabinoid as a retrograde messenger from depolarized postsynaptic neurons to presynaptic terminals. Neuroscience Research, 40, 205–210.
Maldonado, R. (2002). Study of cannabinoid dependence in animals. Pharmacology & Therapeutics, 95, 153–164.
Maldonado, R., Valverde, O., & Berrendero, F. (2006). Involvement of the endocannabinoid system in drug addiction. Trends in Neuroscience, 29, 225–232.
Marsicano, G., Moosmann, B., Hermann, H., Lutz, B., & Behl, C. (2002). Neuroprotective properties of cannabinoids against oxidative stress: Role of the cannabinoid receptor CB1. Journal of Neurochemistry, 80, 448–456.
Mathew, R. J., Tant, S., & Burger, C. (1986). Regional cerebral blood flow in marijuana smokers. British Journal of Addictions, 81, 567–571.
Mathew, R. J., & Wilson, W. H. (1993). Acute changes in cerebral blood-flow after smoking marijuana. Life Sciences, 52, 757–767.
Mathew, R. J., Wilson, W. H., Chiu, N. Y., Turkington, T. G., Degrado, T. R., & Coleman, R. E. (1999). Regional cerebral blood flow and depersonalization after tetrahydrocannabinol administration. Acta Psychiatrica Scandinavica, 100, 67–75.
Mathew, R. J., Wilson, W. H., Coleman, R. E., Turkington, T. G., & Degrado, T. R. (1997). Marijuana intoxication and brain activation in marijuana smokers. Life Sciences, 60, 2075–2089.
Mathew, R. J., Wilson, W. H., Humphreys, D. F., Lowe, J. V., & Wiethe, K. E. (1992). Regional cerebral blood flow after marijuana smoking. Journal of Cerebral Blood Flow and Metabolism, 12, 750–758.
Mathew, R. J., Wilson, W. H., & Tant, S. R. (1989). Acute changes in cerebral blood-flow associated with marijuana smoking. Acta Psychiatrica Scandinavica, 79, 118–128.
Mathew, R. J., Wilson, W. H., Turkington, T. G., & Coleman, R. E. (1998). Cerebellar activity and disturbed time sense after THC. Brain Research, 797, 183–189.
Mathew, R. J., Wilson, W. H., Turkington, T. G., Hawk, T. C., Coleman, R. E., DeGrado, T. R., et al. (2002). Time course of tetrahydrocannabinol-induced changes in regional cerebral blood flow measured with positron emission tomography. Psychiatry Research: Neuroimaging, 116, 173–185.
Matochik, J. A., Eldreth, D. A., Cadet, J. L., & Bolla, K. I. (2005). Altered brain tissue composition in heavy marijuana users. Drug and Alcohol Dependence, 77, 23–30.
Matsuda, L. A., Lolait, S. J., Brownstein, M. J., Young, A. C., & Bonner, T. I. (1990). Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature, 346, 561–564.
McAllister, S. D., & Glass, M. (2002). CB1 and CB2 receptor-mediated signalling: a focus on endocannabinoids. Prostaglandins, Leukotrienes and Essential Fatty Acids, 66, 161–171.
McDonald, J., Schleifer, L., Richards, J. B., & de Wit, H. (2003). Effects of THC on behavioral measures of impulsivity in humans. Neuropsychopharmacology, 28, 1356–1365.
Mechoulam, R. (2002). Discovery of endocannabinoids and some random thoughts on their possible roles in neuroprotection and aggression. Prostaglandins Leukotrienes and Essential Fatty Acids, 66, 93–99.
Mechoulam, R., Benshabat, S., Hanus, L., Ligumsky, M., Kaminski, N. E., Schatz, A. R., et al. (1995). Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochemical Pharmacology, 50, 83–90.
Mechoulam, R., & Gaoni, Y. (1967). The absolute configuration of delta-1-tetrahydrocannabinol, the major active constituent of hashish. Tetrahedron Letters, 12, 1109–1111.
Mechoulam, R., & Hanus, L. (2000). A historical overview of chemical research on cannabinoids. Chemistry and Physics of Lipids, 108, 1–13.
Mechoulam, R., Panikashvili, D., & Shohami, E. (2002). Cannabinoids and brain injury: therapeutic implications. Trends in Molecular Medicine, 8, 58–61.
Medina, K. L., Schweinsburg, A. D., Cohen-Zion, M., Nagel, B. J., & Tapert, S. F. (2007). Effects of alcohol and combined marijuana and alcohol use during adolescence on hippocampal volume and asymmetry. Neurotoxicology and Teratology, 29, 141–152.
Merlin, M. D. (2003). Archaeological evidence for the tradition of psychoactive plant use in the Old World. Economic Botany, 57, 295–323.
Messinis, L., Kyprianidou, A., Malefaki, S., & Papathanasopoulos, P. (2006). Neuropsychological deficits in long-term frequent cannabis users. Neurology, 66, 737–739.
Milton, N. G. (2002). Anandamide and noladin ether prevent neurotoxicity of the human amyloid-beta peptide. Neuroscience Letters, 332, 127–130.
Munro, S., Thomas, K. L., & Abu-Shaar, M. (1993). Molecular characterization of a peripheral receptor for cannabinoids. Nature, 365, 61–65.
National Drug Intelligence Center (2005). National Drug Threat Assessment 2005 U.S. Department of Justice.
O’Leary, D. S., Block, R. I., Flaum, M., Schultz, S. K., Boles Ponto, L. L., Watkins, G. L., et al. (2000). Acute marijuana effects on rCBF and cognition: A PET study. Neuroreport, 11, 3835–3841.
O’Leary, D. S., Block, R. I., Koeppel, J. A., Flaum, M., Schultz, S. K., Andreasen, N. C., et al. (2002). Effects of smoking marijuana on brain perfusion and cognition. Neuropsychopharmacology, 26, 802–816.
O’Leary, D. S., Block, R. I., Turner, B. M., Koeppel, J., Magnotta, V. A., Ponto, L. B., et al. (2003). Marijuana alters the human cerebellar clock. Neuroreport, 14, 1145–1151.
Onaivi, E. S., Ishiguro, H., Gong, J. P., Patel, S., Perchuk, A., Meozzi, P. A., et al. (2006). Discovery of the presence and functional expression of cannabinoid CB2 receptors in brain. Annals of the New York Academy of Sciences, 1074, 514–536.
Pertwee, R. G. (1997). Pharmacology of cannabinoid CB1 and CB2 receptors. Pharmacology and Therapeutics, 74, 129–180.
Petry, N. M., Bickel, W. K., & Arnett, M. (1998). Shortened time horizons and insensitivity to future consequences in heroin addicts. Addiction, 93, 729–738.
Pillay, S. S., Rogowska, J., Kanayama, G., Jon, D. I., Gruber, S., Simpson, N., et al. (2004). Neurophysiology of motor function following cannabis discontinuation in chronic cannabis smokers: An fMRI study. Drug and Alcohol Dependence, 76, 261–271.
Pope, H. G. (2002). Cannabis, cognition, and residual confounding. Journal of the American Medical Association, 287, 1172–1174.
Pope, H. G., Gruber, A. J., Hudson, J. I., Huestis, M. A., & Yurgelun-Todd, D. (2001). Neuropsychological performance in long-term cannabis users. Archives of General Psychiatry, 58, 909–915.
Pope, H. G., Jr., Gruber, A. J., & Yurgelun-Todd, D. (1995). The residual neuropsychological effects of cannabis: the current status of research. Drug and Alcohol Dependence, 38, 25–34.
Pope, H. G. Jr., & Yurgelun-Todd, D. (1996). The residual cognitive effects of heavy marijuana use in college students. Journal of the American Medical Association, 275, 521–527.
Porter, A. C., Sauer, J. M., Knierman, M. D., Becker, G. W., Berna, M. J., Bao, J. Q., et al. (2002). Characterization of a novel endocannabinoid, virodhamine, with antagonist activity at the CB1 receptor. Journal of Pharmacology and Experimental Therapeutics, 301, 1020–1024.
Poulsen, H. A., & Sutherland, G. J. (2000). The potency of cannabis in New Zealand from 1976 to 1996. Science & Justice, 40, 171–176.
Quickfall, J., & Crockford, D. (2006). Brain neuroimaging in cannabis use: A review. Journal of Neuropsychiatry and Clinical Neurosciences, 18, 318–332.
Ramaekers, J. G., Kauert, G., van Ruitenbeek, P., Theunissen, E. L., Schneider, E., & Moeller, M. R. (2006). High-potency marijuana impairs executive function and inhibitory motor control. Neuropsychopharmacology, 31, 2296–2303.
Ramirez, B. G., Blazquez, C., Gomez del, P. T., Guzman, M., & de Ceballos, M. L. (2005). Prevention of Alzheimer’s disease pathology by cannabinoids: Neuroprotection mediated by blockade of microglial activation. Journal of Neuroscience, 25, 1904–1913.
Ranganathan, M., & D’Souza, D. C. (2006). The acute effects of cannabinoids on memory in humans: A review. Psychopharmacology, 188, 425–444.
Rochford, J., Grant, I., & LaVigne, G. (1977). Medical students and drugs: Further neuropsychological and use pattern considerations. International Journal of the Addictions, 12, 1057–1065.
Rodgers, J. (2000). Cognitive performance amongst recreational users of “ecstasy”. Psychopharmacology, 151, 19–24.
Rojas, R., Riascos, R., Vargas, D., Cuellar, H., & Borne, J. (2005). Neuroimaging in drug and substance abuse part I: Cocaine, cannabis, and ecstasy. Topics in Magnetic Resonance Imaging, 16, 231–238.
SAMHSA. (2005). Summary of Findings from the 2005 National Household Survey on Drug Abuse. Rockville, MD, Office of Applied Studies. Ref Type: Generic.
Sarne, Y., & Keren, O. (2004). Are cannabinoid drugs neurotoxic or neuroprotective? Medical Hypotheses, 63, 187–192.
Sarne, Y., & Mechoulam, R. (2005). Cannabinoids: Between neuroprotection and neurotoxicity. Current Drug Targets CNS and Neurological Disorders, 4, 677–684.
Scallet, A. C., Uemura, E., Andrews, A., Ali, S. F., McMillan, D. E., Paule, M. G., et al. (1987). Morphometric studies of the rat hippocampus following chronic delta-9-tetrahydrocannabinol (THC). Brain Research, 436, 193–198.
Schweinsburg, A. D., Schweinsburg, B. C., Cheung, E. H., Brown, G. G., Brown, S. A., & Tapert, S. F. (2005). fMRI response to spatial working memory in adolescents with comorbid marijuana and alcohol use disorders. Drug and Alcohol Dependence, 79, 201–210.
Sneider, J. T., Pope, H. G., Jr., Silveri, M. M., Simpson, N. S., Gruber, S. A., & Yurgelun-Todd, D. A. (2006). Altered regional blood volume in chronic cannabis smokers. Experimental and Clinical Psychopharmacology, 14, 422–428.
Solowij, N. (1995). Do cognitive impairments recover following cessation of cannabis use? Life Sciences, 56, 2119–2126.
Solowij, N. (1998). Cannabis and cognitive functioning. New York: Cambridge University Press.
Solowij, N. (1999). Long-term effects of cannabis on the central nervous system. In H. Kalant, W. Corrigall, W. Hall, & R. Smart (Eds.), The health effects of cannabis (pp. 195–265). Toronto: Addiction Research Foundation.
Solowij, N., Stephens, R. S., Roffman, R. A., Babor, T., Kadden, R., Miller, M., et al. (2002). Cognitive functioning of long-term heavy cannabis users seeking treatment. Journal of the American Medical Association, 287, 1123–1131.
Sugiura, T., Kondo, S., Sukagawa, A., Nakane, S., Shinoda, A., Itoh, K., et al. (1995). 2-Arachidonoylgylcerol—A possible endogenous cannabinoid receptor-ligand in brain. Biochemical and Biophysical Research Communications, 215, 89–97.
Tanda, G., & Goldberg, S. R. (2003). Cannabinoids: Reward, dependence, and underlying neurochemical mechanisms—A review of recent preclinical data. Psychopharmacology, 169, 115–134.
Tunving, K., Thulin, S. O., Risberg, J., & Warkentin, S. (1986). Regional cerebral blood-flow in long-term heavy cannabis use. Psychiatry Research, 17, 15–21.
Tzilos, G. K., Cintron, C. B., Wood, J. B., Simpson, N. S., Young, A. D., Pope, H. G. Jr., et al. (2005). Lack of hippocampal volume change in long-term heavy cannabis users. American Journal of Addictions, 14, 64–72.
United Nations Office on Drugs and Crimes. (2004). World Drug Report United Nations Publications.
Vanyukov, M. M., Tarter, R. E., Kirisci, L., Kirillova, G. P., Maher, B. S., & Clark, D. B. (2003). Liability to substance use disorders: 1. Common mechanisms and manifestations. Neuroscience and Biobehavioral Review, 27, 507–515.
Verdejo-Garcia, A., Benbrook, A., Funderburk, F., David, P., Cadet, J. L., & Bolla, K. I. (2007). The differential relationship between cocaine use and marijuana use on decision-making performance over repeat testing with the Iowa Gambling Task. Drug and Alcohol Dependence, 90, 2–11.
Volkow, N. D., Gillespie, H., Mullani, N., Tancredi, L., Grant, C., Ivanovic, M., et al. (1991). Cerebellar metabolic-activation by delta-9-tetrahydro-cannabinol in human brain—A study with positron emission tomography and F-18 2-fluoro-2-deoxyglucose. Psychiatry Research-Neuroimaging, 40, 69–78.
Volkow, N. D., Gillespie, H., Mullani, N., Tancredi, L., Grant, C., Valentine, A., et al. (1996). Brain glucose metabolism in chronic marijuana users at baseline and during marijuana intoxication. Psychiatry Research-Neuroimaging, 67, 29–38.
Wachtel, S. R., ElSohly, M. A., Ross, S. A., Ambre, J., & de, W. H. (2002). Comparison of the subjective effects of Delta(9)-tetrahydrocannabinol and marijuana in humans. Psychopharmacology, 161, 331–339.
Wert, R. C., & Raulin, M. L. (1986). The chronic cerebral effects of cannabis use. II. Psychological findings and conclusions. International Journal of Addictions, 21, 629–642.
Whitlow, C. T., Liguori, A., Livengood, L. B., Hart, S. L., Mussat-Whitlow, B. J., Lamborn, C. M., et al. (2004). Long-term heavy marijuana users make costly decisions on a gambling task. Drug and Alcohol Dependence, 76, 107–111.
Wiesbeck, G. A., & Taeschner, K. L. (1991). A cerebral computed tomography study of patients with drug-induced psychoses. European Archives of Psychiatry and Clininical Neuroscience, 241, 88–90.
Wig, N. N., & Varma, V. K. (1977). Patterns of long-term heavy cannabis use in North India and its effects on cognitive functions: A preliminary report. Drug & Alcohol Dependence, 2, 211–219.
Wilson, W., Mathew, R., Turkington, T., Hawk, T., Coleman, R. E., & Provenzale, J. (2000). Brain morphological changes and early marijuana use: A magnetic resonance and positron emission tomography study. Journal of Addictive Disease, 19, 1–22.
Zuardi, A. W. (2006). History of cannabis as a medicine: A review. Revista Brasileira de Psiquiatria, 28, 153–157.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gonzalez, R. Acute and Non-acute Effects of Cannabis on Brain Functioning and Neuropsychological Performance. Neuropsychol Rev 17, 347–361 (2007). https://doi.org/10.1007/s11065-007-9036-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-007-9036-8