Abstract
Glucagon-like peptide 1 (GLP-1) analogues have been commercialized for the management of type 2 diabetes. Recent studies have underscored GLP-1’s role as a modulator of alcohol-related behavior. However, the role of the GLP-1 analogue liraglutide on alcohol-withdrawal responses have not been fully elucidated. Liraglutide binds to the G-protein-coupled receptor and activates an adenylyl cyclase and the associated classic growth factor signaling pathway, which acts growth factor-like and neuroprotective properties. The underlying neurobiological mechanisms of liraglutide on alcohol withdrawal remains unknown. This study endeavored to explore the effects of liraglutide on the emotion and memory ability of alcohol-withdrawal mice, and synaptic morphology in the medial prefrontal cortex (mPFC) and the hippocampus (HP), and thus affects the relapse-like drinking of alcohol-withdrawal mice. The alcohol-withdrawal group was reintroduced to a 20% v/v alcohol and water through the two-bottle choice for four consecutive days, a period referred to as alcohol re-drinking. Male C57BL/6J mice were exposed to a regimen of 20% alcohol and water for a duration of 6 weeks. This regimen established the two-bottle choice model of alcohol exposure. Learning capabilities, memory proficiency, and anxiety-like behavior were evaluated using the Morris water maze, open field, and elevated plus maze paradigms. Furthermore, synaptic morphology and the levels of synaptic transport-related proteins were assessed via Golgi staining and Western Blot analysis after a two-week alcohol deprivation period. Alcohol re-drinking of alcohol-withdrawal mice was also evaluated using a two-bottle choice paradigm. Our findings indicate that liraglutide can substantially decrease alcohol consumption and preference (p < 0.05) in the alcohol group and enhance learning and memory performance (p < 0.01), as well as alleviate anxiety-like behavior (p < 0.01) of alcohol-withdrawal mice. Alcohol consumption led to a reduction in dendritic spine density in the mPFC and HP, which was restored to normal levels by liraglutide (p < 0.001). Furthermore, liraglutide was found to augment the levels of synaptic transport-related proteins in mice subjected to alcohol withdrawal (p < 0.01). The study findings corroborate that liraglutide has the potential to mitigate alcohol consumption and ameliorate the memory impairments and anxiety induced by alcohol withdrawal. The therapeutic efficacy of liraglutide might be attributed to its role in counteracting synapse loss in the mPFC and HP regions and thus prevented relapse-like drinking in alcohol-withdrawal mice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol use disorder (AUD) is a chronic and relapsing cerebral disorder characterized by compulsive alcohol usage, pervasive negative emotional states, and recurrent episodes of relapse following withdrawal [1]. The World Health Organization (WHO) reports that excessive alcohol consumption accounts for over three million deaths globally per annum [2]. Alcohol consumption has been linked to more than 200 diseases and injuries, including mental disorders, liver and cardiovascular diseases, as well as accidental injuries [3]. Anxiety, a characteristic symptom associated with alcohol withdrawal, often precipitates relapses [4, 5]. Frequently, patients self-medicate for anxiety and depression with alcohol, thereby escalating the risk of AUD, while withdrawal from alcohol can also precipitate anxiety and depression [6].
AUD significantly impacts the structural, functional, and neurochemical aspects of the brain, particularly the reward circuit regions such as the ventral tegmental area (VTA), nucleus accumbens (NAc), medial prefrontal cortex (mPFC), and the hippocampus (HP) [7,8,9,10]. These regions are instrumental in the development and perpetuation of addiction [11, 12]. Chronic alcohol exposure can engender neurotoxic effects, impair synaptic plasticity, and lead to neuronal death by necrosis and apoptosis [13]. Thus, improving synaptic plasticity to protect neuronal circuits and connectivity may be a potential treatment strategy for AUD. The potential effects of alcohol withdrawal on synaptic morphology and transmission in the HP and mPFC and their subsequent impact on the learning and memory abilities in alcohol mice warrant further investigation.
In view of patients’ differential response to treatments, a universal treatment consensus for AUD is yet to be established. Interestingly, recent studies have spotlighted the modulatory role of glucagon-like peptide-1 (GLP-1) in alcohol reinforcement, thereby presenting it as a novel approach to AUD treatment [14, 15]. The GLP-1 receptor is expressed on neurons and found in most areas of the brain in mice, indicating that GLP‐1 plays a key signalling role [16, 17]. The GLP-1 receptor agonist Exendin-4 has demonstrated a reduction in alcohol intake in both mice [13, 18, 19] and several rat models [20,21,22] and it has been shown to affect the propensity for alcohol relapse in mice [23]. Findings from a randomized controlled trial on GLP-1 receptor agonists in AUD patients have provided invaluable insights into their potential as a novel treatment target for addiction [24].Liraglutide, a commercially available GLP-1 analogue, is used for the treatment of type II diabetes mellitus [25]. Our prior research has revealed liraglutide’s neuroprotective effects in mouse models of Alzheimer’s disease, by way of preserving memory formation and synaptic plasticity, safeguarding mitochondrial activity, and mitigating chronic inflammation in the brain [26,27,28]. A phase II clinical trial featuring liraglutide for Alzheimer’s disease patients (NCT01843075) manifested neuroprotective effects and enhancements in cognition and brain volume, as detected by MRI scans [29,30,31]. Moreover, a phase II clinical trial exhibited clear neuroprotection in patients with Parkinson’s disease (NCT02953665) [32], and a pilot study reported improvements in patients with mood disorders [33, 34]. While GLP-1 analogues have been found to reduce alcohol consumption in mice and rats [18, 22, 35], the effects of liraglutide on alcohol-withdrawal responses remain to be defined. Liraglutide binds to the G‐protein‐coupled GLP‐1 receptor and activates the associated classic growth factor signaling pathway, which acts growth factor-like and neuroprotective properties [36]. Additionally, the underlying neurobiological mechanisms of liraglutide on alcohol withdrawal in the HP and mPFC remains unknown.
In the current study, we employed a two-bottle choice paradigm to evaluate the effects of liraglutide on alcohol consumption and preference. The locomotive, emotional, learning, and memory capabilities of alcohol-withdrawal mice were assessed using the open field, elevated plus maze and water maze paradigms to determine the impact of liraglutide on alcohol-mediated behavior. Subsequently, synaptic loss and the levels of synaptic transport-related proteins were examined by Golgi staining and Western Blot analysis in the HP and mPFC of alcohol-withdrawal mice to evaluate the effects of liraglutide on synaptic morphological plasticity. We hypothesize that liraglutide would reduce anxiety-like behavior, augment learning and memory capabilities of alcohol-withdrawal mice, and normalize synaptic loss, which thus prevented relapse-like drinking in alcohol-withdrawal mice.
Materials and Methods
Animals
Male C57BL/6J mice, aged between 8 and 10 weeks, were procured from the Henan Laboratory Animal Center. All mice were kept under standardized conditions of temperature (22 ± 3°), relative humidity (40–60%), and a 12-hour light/dark cycle, with unrestricted access to purified tap water and food. All experimental protocols and procedures involving animals adhered to the guidelines set by the Henan Animal Research Ethics Committee. Prior to the commencement of experiments, mice were acclimated to the two-bottle choice paradigm in the animal facility for at least one week, during which time all mice had constant access to two water bottles without treatment.
Alcohol Drinking Paradigm
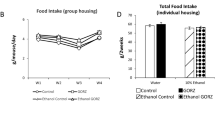
A two-bottle choice alcohol-drinking paradigm was utilized to induce voluntary consumption of considerable volumes of alcohol, as previously described [37, 38]. As depicted in Fig. 1, all mice were acclimated for one week in the animal facility, during which time they had constant access to two water bottles. Subsequently, mice were provided unrestricted access to one water bottle and one 20% alcohol bottle over three 24-hour sessions per week (on Mondays, Wednesdays, and Fridays) for a duration of 6 weeks. For the drinking experiments, alcohol was diluted in purified tap water to a final concentration of 20%. To negate any positional bias, the location of the two bottles was alternated daily. At all other times, two water bottles were provided. After a withdrawal period of two weeks, mice were given access to one water bottle and one 20% alcohol bottle again for four days. See Fig. 1.
Experimental Designs
Experiment 1: The C57BL/6 male mice (n = 12 mice/group) were randomly assigned to four groups: Control group (n = 12), Liraglutide group (Lira, n = 12), Alcohol group (n = 12), and Alcohol + Lira group (n = 12). In the control and Lira groups, both bottles were consistently filled with purified tap water for 6 weeks. In the Alcohol and Alcohol + Lira groups, one bottle contained water and the other 20% v/v alcohol, accessible on an intermittent schedule over the 6 weeks. Liquid intake and body weight of the mice were recorded following each 24-hour alcohol access period. Liraglutide was dissolved in sterile isotonic saline (0.9% NaCl) and injected intraperitoneally once daily (50 nmol/kg). This dose was selected from pilot testing in our lab as well as previously published reports [39, 40]. Saline or liraglutide were administered during the 5th to 6th week of alcohol exposure. See Fig. 2A.
Liraglutide reduced alcohol consumption and preference. A Scheme of the experimental procedure; BTotal fluid consumption of mice in each group(Two-way RM ANOVA, interaction: F(51;748) = 0.6728, P = 0.8283, Group: F(3,44) = 0.02591, P = 0.8744); C Body weight of mice in each group(Two-way RM ANOVA, interaction: F(51,748) = 1.731, P = 0.0043, Group: F(3,44) = 1.630, P = 0.1961); D Alcohol solution consumption of the alcohol group and alcohol + Lira group(Two-way RM ANOVA, interaction: F(17,374) = 2.282, P = 0.0027, Group: F(1,22) = 6.570, P = 0.0177,); E Alcohol preference of alcohol group and alcohol + Lira group(Two-way RM ANOVA, interaction: F(17,374) = 1.465, P = 0.1060, Group: F(1,22) = 7.409, P = 0.0140); F Alcohol solution consumption of the alcohol group and alcohol + Lira group on Friday of the 5th and 6th week; G Alcohol preference of alcohol group and alcohol + Lira group on Friday of the 5th and 6th week. Data are presented as the Mean ± S.E.M. n = 12 for each group. *P < 0.05 compared with the Alcohol group
Experiment 2: The C57BL/6 male mice (n = 12 mice/group) were randomly assigned to four groups: Control group (n = 12), Liraglutide group (n = 12), Alcohol group (n = 24), and Alcohol + Lira group (n = 24). In the control and Lira groups, both bottles were consistently filled with purified tap water for 6 weeks. In the Alcohol and Alcohol + Lira groups, one bottle contained water and the other 20% v/v alcohol, accessible on an intermittent schedule over the 6 weeks. After 6 weeks of intermittent access to alcohol, all alcohol mice (Alcohol group and Alcohol + Lira group mice, n = 24) underwent a two-week alcohol deprivation period. Subsequently, half of the alcohol mice (Alcohol group and Alcohol + Lira group mice, n = 12)were reintroduced to a 20% v/v alcohol or water through the two-bottle choice for four consecutive days, a period referred to as alcohol re-drinking (see Fig. 3A), and all the remaining mice were subjected to behavioral test and then histological test. Saline or Liraglutide were administered from alcohol withdrawal until sacrifice.
Liraglutide prevented relapse-like drinking in mice. A Scheme of the experimental procedure; B Total fluid consumption of mice in each group (Two-way RM ANOVA, interaction: F(15,110) = 0.2937, P = 0.8813, Group: F(3,44) = 0.07828, P = 0.7823); C Body weight of mice in each group (Two-way RM ANOVA, interaction: F(15,110) = 3.053, P = 0.0538, Group: F(3,44) = 10.75, P = 0.0034); D Alcohol consumption of mice in re-drinking(Two-way RM ANOVA, interaction: F(4;88) = 0.3951, P = 0.8116, Group: F(1;22) = 4.039, P = 0.0375); E Alcohol preference of mice in re-drinking (Two-way RM ANOVA, interaction: F(4;88) = 0.4985, P = 0.7689, Group: F(1;22) = 5.1283, P = 0.0156). Data are presented as the Mean ± S.E.M. n = 12 for each group. *P < 0.05, **P < 0.01 compared with the Alcohol group
Liquid intake and body weight of the mice were recorded following each 24-hour alcohol access period. A Morris water maze test was conducted to evaluate learning and long-term memory following a two-week alcohol deprivation period. On the last day of the water maze test, the mice were also subjected to open-field and elevated plus maze tests to assess anxiety-like behavior. At the conclusion of the behavioral protocol, mice were anesthetized deeply with isoflurane, and the brain structures implicated in memory and emotion (HP and mPFC regions) were evenly excised post-decapitation for Golgi staining and Western Blot analysis.
Behavioral Tests
Open-Field Test (OFT)
The open-field test was conducted in alignment with previously established methods [41]. The testing apparatus consisted of a polyvinyl chloride enclosure measuring 42 × 42 × 42 cm. During the test, each mouse was gently introduced into the enclosure. A software-based system (SMART3.0.05) initiated tracking and recorded the mouse’s movement for a span of 10 min. Following each trial, the apparatus was sanitized with a 75% ethanol solution to eliminate any residual scent from the previous subject.
Elevated Plus Maze (EPM)
The elevated plus maze test implemented as per earlier descriptions [42]. The maze, composed of polyvinyl chloride, consisted of a central area (10 × 10 cm), two open arms (50 × 10 cm each), and two closed arms (50 × 10 cm each). Mice were gently placed in the central area of the maze, facing a closed arm. The software system (SMART3.0.05) initiated recording of the mouse’s movements over a duration of 5 min. Similar to the open-field test, the maze was cleaned with a 75% ethanol solution after each mouse to prevent scent-based bias.
Morris Water Maze (MWM)
The Morris Water Maze was conducted according to a previously established method [43]. The Morris Water Maze apparatus comprises a circular pool, 150 cm in diameter and 60 cm high, filled with water maintained at a temperature of 25 ± 2°. Within the pool is a small escape platform with a diameter of 10 cm. The testing protocol included an initial spatial training phase (acquisition phase) and a probe trial (recall phase). From day 1 to 5, each mouse was trained from the same quadrant of 4 possible directions. If a mouse failed to locate the escape platform within 60 s, it was guided to the platform and allowed to remain there for 30 s. A video tracking system and software system (SMART3.0.05) recorded escape latency and total swimming distance within the 60-second timeframe. On the sixth day, with the escape platform removed, mice were placed into the quadrant opposite to where the platform had previously been concealed. Their duration in the target quadrant and the number of times they crossed the previous platform location within 60 s were recorded.
Methods of Tissue Sampling and Euthanasia in Mice
Following the completion of behavioral tests, mice were anesthetized via an intraperitoneal injection of urethane (1.5 g/kg). Post-anesthesia, mice were rapidly immobilized on an operating table, and their chests were surgically opened. A 0.9% saline solution (40 ml) was administered via the left ventricle. Subsequently, the hippocampus (HP) and medial prefrontal cortex (mPFC) regions were swiftly excised post-decapitation for subsequent experimental analysis.
Golgi Staining and Spine Morphology Analysis
Golgi staining was conducted following the prescribed steps outlined by the manufacturer (FD Rapid GolgiStain™ Kit, USA). Brain tissue samples were submerged in the impregnation solution provided in the Rapid GolgiStain kit. The samples were sectioned into 100 μm slices and placed on glass slides for microscopic examination as per the manufacturer’s directions. The prepared slices underwent a dehydration process via a series of ethanol baths at concentrations of 50%, 75%, 95%, and 100% for 4 min at each concentration. Post-dehydration, the tissue samples were clarified in xylene before image acquisition using an Olympus Eclipse microscope.
Synapse densities were quantified utilizing the Golgi staining method. The total count of dendritic spines on a specified segment of dendrites was performed under 100x magnification. The resulting value was then divided by the length of the dendrite segment to derive the dendritic spine density. Three brain slices of tissue were assessed per animal and the average value of the three slices was taken for statistical analysis. The investigator conducting the counting was blinded to the treatment conditions of the mice.
Western Blot
Tissue samples were pulverized using an ultrasonic cell disrupter in ice-cold radioimmunoprecipitation assay (RIPA) buffer supplemented with a protease inhibitor mixture. Subsequently, samples were homogenized and centrifuged at 12,000×g for 10 min at 4 °C. The resulting supernatants were collected, and protein concentrations were determined using a BCA protein assay kit. Denatured protein (30 µg loading) was subjected to SDS-PAGE, and transferred onto PVDF membranes. The membranes were then blocked with 5% BSA in TBST and then cropped according to the MW marker to remove irrelevant sections of the membrane. The cropped membranes then were incubated with different primary antibodies (p-GluA1, 1:1000, Abcam, ab109464; GluA1, 1:1000, Abcam, ab109450; vGluT1,1:1000, Abcam, ab227805, Synaptophysin, 1:500, ABclonal, A6344; PSD95, 1:500, ABclonal, A0131; β-actin, 1:10000, ABclonal, AC026) overnight at 4 °C. After incubation with Goat anti-Rabbit HRP-conjugated secondary antibodies (goat anti-rabbit, 1:5000, Abcam, ab6721; goat anti-mouse, 1:5000, Abcam, ab6789), the membranes were developed using the ECL-Plus detection kit (GE Healthcare Bio-Sciences, USA). The exposure time was set automatically by iBright CL750 (Thermo Scientific). Brain tissue proteins extracted from each mouse were determined with each antibody three times and the averages were taken for statistical analysis.
Statistics
All statistical analysis was conducted using GraphPad Prism 8.0 software. Anderson-Darling normality test and Levene’s Test for Homogeneity of Variances was used to validate the data prior to performing analysis of variance (ANOVA). All statistical data were tested for normality and homogeneity of variance. Data of alcohol consumption had one main treatment condition (Drug) and one repeated factor (Time), thus two-way ANOVA tests (Drug× Time) and independent sample t-test (drug) were conducted respectively. MWM data in experiment 2 had one main treatment condition (Alcohol or Drug) and one repeated factor (Training days), thus two-way RM ANOVAs and Tukey’s post-hoc test were conducted when appropriate. The remaining data had one main treatment condition (Alcohol or Drug), which were analyzed by one-way ANOVA followed by the recommended post-hoc test (Tukey’s). Data results were reported as Mean ± SEM, and a p-value less than 0.05 was considered to indicate a statistically significant difference.
Results
Liraglutide Reduced Alcohol Consumption and Preference in Mice
We utilized a two-bottle choice paradigm to assess the impact of liraglutide on alcohol consumption and preference in mice. Figure 2 depicts the alcohol consumption and preference in the alcohol and Alcohol + Lira groups. There was no significant difference in total fluid consumption and body weight between the groups (Fig. 2BC). After 6 weeks of exposure, the mice showed a significant increase in alcohol consumption and alcohol preference after 6 weeks of alcohol exposure (Fig. 2DE). Alcohol consumption on Friday of the 5th and 6th week in alcoholic mice was also analyzed. The liraglutide-treated mice exhibited a decrease in alcohol consumption and preference on Friday of the 6th week compared to the alcohol-only group (Fig. 2FG).
Liraglutide Prevented Relapse-Like Drinking in Mice
After 6 weeks of intermittent access to alcohol, mice were deprived of alcohol for 2 weeks. The alcohol withdrawal model could be used to reflect relapse-like drinking. Following a two-week withdrawal period, the mice were reintroduced to a 20% v/v alcohol or tap water through the two-bottle choice for four consecutive days, a period referred to as alcohol re-drinking. No significant interaction was evident in total liquid intake (Fig. 3B), body weight (Fig. 3C), alcohol consumption (Fig. 3D) and alcohol preference (Fig. 3E). However, mice receiving liraglutide treatment demonstrated reduced body weight, alcohol consumption, and preference compared to the alcohol group.
Liraglutide Improves Anxiety and Memory Impairments Induced by Alcohol Withdrawal
Open-Field Test
The open-field test result showed that there were significant differences among groups in the percent of distance in central areas after alcohol withdrawal. Compared to the control group, the percentage of distance covered in central areas in the alcohol group diminished after withdrawal. Notably, liraglutide treatment significantly increased this percentage relative to vehicle injection in the alcohol group (Fig. 4C), indicating an increase in exploratory activity. There was no significant difference among groups in the total distance travelled in the open field after withdrawal (Fig. 4B).
Liraglutide improved anxiety-like behavior in alcohol withdrawal mice. A Movement trajectory plots of mice in each group after withdrawal. B Total distance statistics in each group after withdrawal (One-way ANOVA, F(3,36) = 2.506, P = 0.0745). C Central distance statistics in each group after withdrawal (One-way ANOVA, F(3,36) = 5.252, P = 0.0041; Control vs. Alcohol, P = 0.029; Alcohol vs. Alcohol + Lira, P = 0.031); Data are presented as the Mean ± S.E.M. n = 10 for each group. *P < 0.05 compared with control group; #P < 0.05 compared with Alcohol group
Elevated Plus Maze
Figure 5 illustrates the findings from the EPM. Significant variations among groups were noted in the percentage of distance and time spent in open arms after alcohol withdrawal. Compared to the control group, both the percentage of distance and time spent in open arms by the alcohol group was reduced. Conversely, liraglutide treatment significantly augmented the percentage of distance and time in open arms compared to the alcohol group (Fig. 5CD). There was no significant difference among groups in the total distance travelled in the open arm and closed arm after withdrawal (Fig. 5B). a finding that aligns with results from the open-field test.
Liraglutide alleviated anxiety-like behavior in alcohol withdrawal mice. A Movement trajectory plots of mice in each group after withdrawal; B Total distance travelled in each group after withdrawal (One-way ANOVA, F(3,36) = 0.3340, P = 0.8008); C Percentage of distance travelled in open arms after withdrawal (One-way ANOVA, F(3, 36) = 3.282, P = 0.0318; Control vs. Alcohol, P = 0.0043; Alcohol vs. Alcohol + Lira, P = 0.0089).; D Percentage of time spent in open arms after withdrawal(One-way ANOVA, F(3,36) = 5.162, P = 0.0045; Control vs. Alcohol, P = 0.0015; Alcohol vs. Alcohol + Lira, P = 0.0383). Data are presented as the Mean ± S.E.M. n = 10 for each group. **P < 0.01 compared with control group; #P < 0.05, ##P < 0.01 compared with alcohol group
Morris Water Maze (MWM)
In the location-based navigation test, the escape latency in each group showed a decreasing trend after alcohol withdrawal (Fig. 6B). Compared to the control group, the alcohol group demonstrated a significant increase in escape latency in the alcohol group increased significantly. However, liraglutide treatment markedly reduced the escape latency compared to the alcohol group. The spatial exploration track diagram for each group on the sixth day revealed that there were significant differences among groups in the number of target crossings and the time in target quadrant after alcohol withdrawal (Fig. 6ACD). Compared to the control group, the number of target crossings and the time in target quadrant in the alcohol group was significantly decreased, In contrast, liraglutide treatment substantially increased the number of target crossings and the time in target quadrant compared to the alcohol group (Fig. 6CD).
Liraglutide improved spatial learning and memory abilities in alcohol withdrawal mice. A Movement trajectory plots of mice in each group after withdrawal; B Escape latency in each groups after withdrawal (Two-way RM ANOVA, interaction: F(57,684) = 3.521, P < 0.001, Group: F(3;36) = 18.89, P < 0.001); C Target crossing in each groups after withdrawal (One-way ANOVA, F(3,36) = 10.45, P < 0.001; Control vs. Alcohol, P = 0.0042; Alcohol vs. Alcohol + Lira, P = 0.0172); D Time in target quadrant in each groups after withdrawal(One-way ANOVA, F(3,36) = 9.55, P < 0.001; Control vs. Alcohol, P = 0.0014; Alcohol vs. Alcohol + Lira, P = 0.0242). Data are presented as the Mean ± S.E.M. n = 10 for each group. *P < 0.05 compared with control group; #P < 0.05 compared with alcohol group
Liraglutide Modulates Synaptic Density in Alcohol-Withdrawal Mice
Synaptic plasticity encompasses modifications to synaptic morphology, reflected by dendritic spine density, and alterations to synaptic transmission. To identify changes in spine morphology in the mPFC and HP following a two-week withdrawal period, we utilized Golgi staining. A significant difference was observed between the groups. Dendritic spine density in the alcohol group declined in comparison to the control group in both the mPFC (Fig. 7AB) and HP (Fig. 7CD). Furthermore, liraglutide treatment markedly elevated the dendritic spine density relative to the alcohol group (Fig. 7BD).
Liraglutide increased the spine densities of neurons in alcohol-withdrawal mice. A Examples of Golgi-stained neurons in mPFC of each group mice after withdrawal; B Liraglutide increased dendritic spine density in the mPFC neurons of alcohol-withdrawal mice(One-way ANOVA, F(3, 20) = 7.96, P = 0.0049; Control vs. Alcohol, P = 0.0273; Alcohol vs. Alcohol + Lira, P = 0.0411); C Examples of Golgi-stained neurons in HP of each group mice after withdrawal; D Liraglutide increased dendritic spine density in the HP neurons of alcohol- exposure mice(One-way ANOVA, F(3, 20) = 10.08, P = 0.0013; Control vs. Alcohol, P < 0.001; Alcohol vs. Alcohol + Lira, P = 0.0091). Data are presented as the Mean ± S.E.M. n = 6 for each group. *P < 0.05, ***P < 0.001 compared with control group; #P < 0.05, ##P < 0.01 compared with the alcohol group
Liraglutide Modulates Synaptic Protein Expression Levels in Alcohol-Withdrawal Mice
To probe the influence of liraglutide on proteins associated with synaptic transport in alcohol-withdrawal mice, we assessed the expression of synapse-related proteins p-GluA1, GluA1, vGluT1, SYN and PSD95 in the mPFC (Fig. 8A) and HP (Fig. 9A) regions of mice after alcohol withdrawal. Total GluA1 protein expression in the alcohol group in did not significantly deviate from the control group, but the expression of p-GluA1 decreased. Liraglutide treatment increased the expression of p-GluA1 compared to the alcohol group (Fig. 8B).
Liraglutide modulates protein expression levels involved in synaptic transmission in mPFC in alcohol-withdrawal mice. A Western blot showing the protein levels of p-GluA1, GluA1, vGluT1, SYN, PSD-95 in mPFC of mice in all groups after withdrawal; B Statistical results of p-GluA1 protein expression in mPFC after withdrawal(One-way ANOVA, F(3,20) = 11.26, P < 0.001; Control vs. Alcohol, P = 0.0068; Alcohol vs. Alcohol + Lira, P = 0.0323); C Statistical results of vGluT1 protein expression in mPFC after withdrawal(One-way ANOVA, F(3,20) = 8.328, P = 0.0011; Control vs. Alcohol, P = 0.0245; Alcohol vs. Alcohol + Lira, P = 0.0197); D Statistical results of SYN protein expression in mPFC after withdrawal(One-way ANOVA, F(3,20) = 10.63, P < 0.001; Control vs. Alcohol, P = 0.0002; Alcohol vs. Alcohol + Lira, P = 0.0152); E Statistical results of PSD-95 protein expression in mPFC after withdrawal(One-way ANOVA, F(3,20) = 13,62, P < 0.0001; Control vs. Alcohol, P = 0.0311; Alcohol vs. Alcohol + Lira, P = 0.0267). Data are presented as the Mean ± S.E.M. n = 6 for each group. *P < 0.05, **P < 0.01, compared with control group; #P < 0.05 compared with the alcohol only group
Liraglutide modulates proteins involved in synaptic transmission in HP in alcohol-withdrawal mice. A Western blot showing the protein levels of p-GluA1, GluA1, SYN, PSD-95 in HP of mice in all groups after withdrawal. B Statistical results of p-GluA1 protein expression in HP after withdrawal(One-way ANOVA, F(3.20) = 11.08, P < 0.001; Control vs. Alcohol, P < 0.0001; Alcohol vs. Alcohol + Lira, P = 0.0414); C Statistical results of vGluT1 protein expression in HP after withdrawal(One-way ANOVA, F(3,20) = 10.87, P < 0.001; Control vs. Alcohol, P < 0.001; Alcohol vs. Alcohol + Lira, P = 0.0301); D Statistical results of SYN protein expression in HP after withdrawal(One-way ANOVA, F(3,20) = 12.82, P < 0.0001; Control vs. Alcohol, P < 0.001; Alcohol vs. Alcohol + Lira, P = 0.0056); E Statistical results of PSD-95 protein expression in HP after withdrawal(One-way ANOVA, F(3.20) = 11.73, P < 0.001; Control vs. Alcohol, P < 0.001; Alcohol vs. Alcohol + Lira, P = 0.0347). Data are presented as the Mean ± S.E.M. n = 6 for each group. ***P < 0.001, ****P < 0.0001 compared with control group; #P < 0.05 compared with alcohol group
Significant differences were observed among groups in the expression of VGluT1, SYN and PSD-95. The alcohol-only group post-withdrawal demonstrated lower expression of VGluT1, SYN and PSD-95 compared to the control group. Conversely, liraglutide treatment in the alcohol group led to elevated the expression of VGluT1, SYN and PSD-95 compared to the alcohol only group (Fig. 8C–E).
To further scrutinize the impact of liraglutide on synaptic protein expression in the HP regions of mice post-alcohol withdrawal, Western blotting was employed to determine the expression levels of p-GluA1, vGluT1, GluA1, SYN, and PSD-95. Significant differences were found among groups in the expression of p-GluA1, vGluT1, SYN, and PSD-95. The expression levels of p-GluA1, vGluT1, SYN, and PSD-95 in the alcohol group were substantially reduced compared to the control mice. On the other hand, liraglutide treatment led to significant elevations in the expression levels of p-GluA1, vGluT1, SYN, and PSD-95 compared to the alcohol group (Fig. 9B–E).
Discussion
This investigation illuminates a pivotal function of GLP-1 signalling in a murine model of alcohol consumption and subsequent resumption of alcohol intake following alcohol withdrawal. Specifically, we showed that systemic liraglutide administration mitigates the return to alcohol drinking and anxiety-like behavior, memory impairments, and synapse loss in male mice following alcohol withdrawal. Our rodent findings are consistent with experimental and clinical studies that showed GLP-1 analogue liraglutide could reduce alcohol consumption [14, 44]. These studies indicate that clinically available GLP-1 receptor agonists deserve to be tested as potential treatments of AUD. Our study extended to the significant role of GLP-1 receptors in an animal model of alcohol withdrawal and relapse drinking.
The free-choice bottle model represents a non-invasive, straightforward experimental design for self-administration, mimicking human alcohol consumption patterns [45]. We observed that liraglutide attenuated both alcohol consumption and preference in mice, without influencing overall fluid intake during the experimental period. A notable finding of this study is the enduring reduction in alcohol consumption and preference by liraglutide following a two-week withdrawal period, implying a potentially sustained regulatory process. Previous research has noted a reduction in alcohol intake following acute pharmacological activation of the GLP-1 receptor using Exendin-4 in a two-bottle selection experiment [38]. Exendin-4 and liraglutide have also been found to decrease alcohol intake in vervet monkeys [46], further suggesting that GLP-1 receptor activation in the brain inhibits alcohol consumption in rodents and non-human primates.
Consistent alcohol intoxication invariably impairs learning and memory processes, mediated by specific neural circuits [47]. Evidence indicates that initial exposure to alcohol may augment hippocampal function, thereby contributing to addiction development. In accordance with the self-administration hypothesis, withdrawal from alcohol results in deficits in learning and memory [48, 49]. Our study discovered that liraglutide ameliorated learning and memory impairments caused by alcohol withdrawal in mice exposed to alcohol. Observations from human adolescent studies indicate that heavy alcohol consumption correlates with poorer cognitive function across a wide range of neuropsychological assessments, encompassing learning, memory, attention, executive functioning, and impulsivity [50]. We also examined the anxiety-like behavior in mice exposed to alcohol. Alcohol dependence often leads to anxiety and depression-like behaviors, particularly in newborns and adolescents [51]. Our findings clearly demonstrate the ameliorative effect of liraglutide on alcohol-induced anxiety. Our findings clearly demonstrate the ameliorative effect of liraglutide on alcohol-induced anxiety., thus suggesting that GLP-1 receptor activation may modulate alcohol-related behaviors by influencing reward circuits. To this point, the engagement of the amygdala, hypothalamus, medial prefrontal cortex, and hippocampus in reward behavior has been documented [52, 53]. Our findings reveal a significant diminution in the expression levels of synaptic proteins in the mPFC and HP regions during withdrawal in mice exposed to alcohol.
In the central nervous system, AMPA receptors comprise functional tetramers formed from diverse combinations of four subunits (GluA1-4), with GluA1 being the predominant subunit in neuronal synaptic and extra-synaptic AMPA receptors [54, 55]. The amplification of GluA1 expression and its phosphorylation are commonly proposed mechanisms for drug action in the study of Alzheimer’s disease, depression, and addiction. An increase in the phosphorylation of the GluA1 receptor appears to be a counteractive mechanism against the pathophysiological features of Alzheimer’s disease and depression [56]. Our study found that, while the total protein expression of GluA1 in the alcohol group remained unchanged compared to the control group, the expression of p-GluA1 diminished. Liraglutide treatment elevated p-GluA1 levels compared to those in the alcohol-only group, suggesting normalization of synaptic transmission.
Synaptophysin, which is expressed extensively in all nerve terminals, especially at the presynaptic membrane, is widely recognized as a crucial marker of synaptogenesis and synaptic plasticity. PSD-95, a synaptic protein, serves to stabilize dendritic spines at the postsynaptic membrane [57]. We noted significant disparities in the expression of SYN and PSD-95 among groups; however, liraglutide treatment led to increased expression of SYN and PSD-95 compared to the alcohol group. Furthermore, we quantified the relative expression level of VGluT1 in the mPFC and HP regions post alcohol withdrawal and found that liraglutide treatment heightened VGluT1 expression compared to the alcohol group. VGluT1 plays a crucial role in central nervous system learning and memory, primarily by influencing synaptic Glu transport and long-term potentiation. Reduction of VGluT1 expression in the hippocampus can instigate changes in dendritic structure, thereby reducing synaptic connectivity, leading to neurofibrillary lesions and impairments in learning and memory [58]. To corroborate these findings, we assessed dendritic spine density using Golgi staining. We observed a reduction in dendritic spine density in mice exposed to alcohol, which was ameliorated by liraglutide treatment. These findings further substantiate the deleterious impact of alcohol on synaptic numbers and function in mice and the therapeutic potential of liraglutide in treating AUD. Previous studies have highlighted the protective effect of chronic treatment with GLP-1 receptor agonists on synapses in various disease models [59]. Our study augments this body of research by demonstrating that alcohol-induced synaptic damage can be mitigated by liraglutide.
Sex differences may play a critical role in modulating how chronic alcohol use impacts the brain and thus causes the development of AUD [60]. Male animals show a more pronounced display of negative behaviors and neuroactivity after alcohol withdrawal compared to female animals [61, 62]. However, Women with AUD experience higher risks of developing cancers, alcohol-related liver injury, and cardiovascular disease compared to men with AUD despite comparable levels of drinking [63,64,65]. The role of gonadal steroid hormones in regulating multiple functions in the brain may partly explain the sex differences in the development of AUD [66,67,68]. This topic is worthy of further assessment in the future, as our study only included male mice. Additionally, animal models have advanced from only modeling self-administration of alcohol, which on its own does not necessarily model AUD characteristics, to more sophisticated behavioral models that capture addiction-related aspects, such as alcohol seeking, compulsive intake, dependence, and relapse [69]. The chronic intermittent access to ethanol vapor (CIE) model, which has predictive and construct validity to induce ethanol dependence in animals is available, too. Further studies in these models are warranted to enhance our knowledge of how liraglutide affects alcoholism.
In conclusion, our findings suggest that liraglutide can mitigate alcohol consumption and ameliorate learning and anxiety in mice exposed to alcohol. The therapeutic effect of liraglutide may be achieved by safeguarding synapses and enhancing synaptic transmission in the mPFC and HP regions. These results provide a foundation and an innovative research avenue for future investigations into the effects and mechanisms of AUD, as well as potential novel pharmaceutical interventions for this disorder.
Data Availability
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Merikangas KR et al (1998) Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict Behav 23(6):893–907
Peacock A et al (2018) Global statistics on alcohol, Tobacco and illicit drug use: 2017 status report. Addiction 113(10):1905–1926
Azevedo CA, Mammis A (2018) Neuromodulation therapies for Alcohol Addiction: A literature review. Neuromodulation 21(2):144–148
Gajbhiye SV et al (2018) Minocycline in Alcohol Withdrawal Induced anxiety and alcohol relapse in rats. Curr Clin Pharmacol 13(1):65–72
Ribadier A, Varescon I (2019) Anxiety and depression in Alcohol Use Disorder individuals: the role of personality and coping strategies. Subst Use Misuse 54(9):1475–1484
Conway KP et al (2016) Association of Lifetime Mental Disorders and subsequent alcohol and Illicit Drug Use: results from the National Comorbidity Survey-Adolescent supplement. J Am Acad Child Adolesc Psychiatry 55(4):280–288
Peris J et al (2022) Conditioned social preference and reward value of activating oxytocin-receptor-expressing ventral tegmental area neurons following repeated daily binge ethanol intake. Alcohol Clin Exp Res 46(2):194–206
Ho AL et al (2018) The nucleus accumbens and Alcoholism: a target for deep brain stimulation. Neurosurg Focus 45(2):E12
Shang P et al (2020) Chronic Alcohol exposure induces aberrant mitochondrial morphology and inhibits respiratory capacity in the Medial Prefrontal cortex of mice. Front Neurosci 14:561173
King JA et al (2020) Chronic alcohol-induced liver injury correlates with memory deficits: role for neuroinflammation. Alcohol 83:75–81
Russo SJ, Nestler EJ (2013) The brain reward circuitry in mood disorders. Nat Rev Neurosci 14(9):609–625
Lodge DJ, Grace AA (2006) The laterodorsal tegmentum is essential for burst firing of ventral tegmental area dopamine neurons. Proc Natl Acad Sci U S A 103(13):5167–5172
Sirohi S et al (2016) Central & peripheral glucagon-like peptide-1 receptor signaling differentially regulate addictive behaviors. Physiol Behav 161:140–144
Jerlhag E (2018) GLP-1 signaling and alcohol-mediated behaviors; preclinical and clinical evidence. Neuropharmacology 136(Pt B):343–349
Marty VN et al (2020) Long-Acting Glucagon-Like Peptide-1 receptor agonists suppress Voluntary Alcohol Intake in male Wistar rats. Front Neurosci 14:599646
Graham DL et al (2020) A novel mouse model of glucagon-like peptide-1 receptor expression: a look at the brain. J Comp Neurol 528(14):2445–2470
Reich N, Hölscher C (2022) The neuroprotective effects of glucagon-like peptide 1 in Alzheimer’s and Parkinson’s Disease: an in-depth review. Front Neurosci 16:970925
Suchankova P et al (2015) The glucagon-like peptide-1 receptor as a potential treatment target in Alcohol Use Disorder: evidence from human genetic association studies and a mouse model of alcohol dependence. Transl Psychiatry 5(6):e583
Sørensen G, Caine SB, Thomsen M (2016) Effects of the GLP-1 agonist Exendin-4 on intravenous ethanol self-administration in mice. Alcohol Clin Exp Res 40(10):2247–2252
Shirazi RH, Dickson SL, Skibicka KP (2013) Gut peptide GLP-1 and its analogue, Exendin-4, decrease alcohol intake and reward. PLoS ONE 8(4):e61965
Vallof D, Kalafateli AL, Jerlhag E (2019) Brain region specific glucagon-like peptide-1 receptors regulate alcohol-induced behaviors in rodents. Psychoneuroendocrinology 103:284–295
Colvin KJ et al (2020) Brain site-specific inhibitory effects of the GLP-1 Analogue Exendin-4 on alcohol intake and operant responding for palatable food. Int J Mol Sci 21(24):9710
Thomsen M et al (2017) The glucagon-like peptide 1 receptor agonist Exendin-4 decreases relapse-like drinking in socially housed mice. Pharmacol Biochem Behav 160:14–20
Klausen MK et al (2022) Exenatide once weekly for alcohol use disorder investigated in a randomized, placebo-controlled clinical trial. JCI Insight 7(19):e159863
Vilsboll T (2009) Liraglutide: a new treatment for type 2 Diabetes. Drugs Today (Barc) 45(2):101–113
McClean P et al (2011) The Diabetes drug Liraglutide prevents degenerative processes in a mouse model of Alzheimer’s Disease. J Neurosci 31:6587–6594
McClean PL, Holscher C (2014) Liraglutide can reverse memory impairment, synaptic loss and reduce plaque load in aged APP/PS1 mice, a model of Alzheimer’s disease. Neuropharmacology 76:57–67
Parthsarathy V, Holscher C (2013) The type 2 Diabetes drug liraglutide reduces chronic inflammation induced by irradiation in the mouse brain. Eur J Pharmacol 700(1–3):42–50
Hölscher C (2022) Protective properties of GLP-1 and associated peptide hormones in neurodegenerative disorders. Br J Pharmacol 179(4):695–714
Femminella GD et al (2019) Evaluating the effects of the novel GLP-1 analogue liraglutide in Alzheimer’s Disease: study protocol for a randomised controlled trial (ELAD study). Trials 20(1):191
Edison P et al (2023) MRI CHANGES FOLLOWING TREATMENT OF GLP‐1 ANALOGUE, LIRAGLUTIDE IN ALZHEIMER’S DISEASE. Alzheimer’s Dementia 19:e080538
Hogg E et al (2023) A Phase II, Randomized, Double-Blinded, Placebo-Controlled Trial of Liraglutide in Parkinson’s Disease. Available at SSRN. https://ssrn.com/abstract=4212371
Mansur RB et al (2017) Liraglutide promotes improvements in objective measures of cognitive dysfunction in individuals with mood disorders: a pilot, open-label study. J Affect Disord 207:114–120
Mansur RB et al (2017) Treatment with a GLP-1R agonist over four weeks promotes weight loss-moderated changes in frontal-striatal brain structures in individuals with mood disorders. Eur Neuropsychopharmacol 27(11):1153–1162
Chuong V et al (2023) The glucagon-like peptide-1 (GLP-1) analogue semaglutide reduces alcohol drinking and modulates central GABA neurotransmission. JCI Insight 8(12):e170671
Sharma M, Jalewa J, Holscher C (2013) Neuroprotective and anti-apoptotic effects of Liraglutide on SH-SY5Y cells exposed to methylglyoxal stress. J Neurochem 128:459–471
Simms JA et al (2008) Intermittent access to 20% ethanol induces high ethanol consumption in Long-Evans and Wistar rats. Alcohol Clin Exp Res 32(10):1816–1823
Egecioglu E et al (2013) The glucagon-like peptide 1 analogue Exendin-4 attenuates alcohol mediated behaviors in rodents. Psychoneuroendocrinology 38(8):1259–1270
Hunter K, Holscher C (2012) Drugs developed to treat Diabetes, liraglutide and lixisenatide, cross the blood brain barrier and enhance neurogenesis. BMC Neurosci 13(1):33–38
Liu W et al (2015) Neuroprotective effects of lixisenatide and liraglutide in the MPTP mouse model of Parkinson’s Disease. Neuroscience 303:42–50
Kraeuter AK, Guest PC, Sarnyai Z (2019) The open field test for measuring locomotor activity and anxiety-like behavior methods. Method Mol Biol 1916:99–103
Abreu-Villaça Y et al (2013) Combined exposure to Tobacco smoke and ethanol during adolescence leads to short- and long-term modulation of anxiety-like behavior. Drug Alcohol Depend 133(1):52–60
Bromley-Brits K, Deng Y, Song W (2011) Morris water maze test for learning and memory deficits in Alzheimer’s disease model mice. J Vis Exp 53:e2920
Vallof D et al (2016) The glucagon-like peptide 1 receptor agonist liraglutide attenuates the reinforcing properties of alcohol in rodents. Addict Biol 21(2):422–437
Sanchis-Segura C, Spanagel R (2006) Behavioural assessment of drug reinforcement and addictive features in rodents: an overview. Addict Biol 11(1):2–38
Thomsen M et al (2019) Effects of glucagon-like peptide 1 analogs on alcohol intake in alcohol-preferring vervet monkeys. Psychopharmacology 236(2):603–611
Van Skike CE, Goodlett C, Matthews DB (2019) Acute alcohol and cognition: remembering what it causes us to forget. Alcohol 79:105–125
Kutlu MG, Gould TJ (2016) Effects of Drugs of abuse on hippocampal plasticity and hippocampus-dependent learning and memory: contributions to development and maintenance of addiction. Learn Mem 23(10):515–533
Stavro K, Pelletier J, Potvin S (2013) Widespread and sustained cognitive deficits in Alcoholism: a meta-analysis. Addict Biol 18(2):203–213
Lees B et al (2020) Effect of alcohol use on the adolescent brain and behavior. Pharmacol Biochem Behav 192:172906
Bosse KE et al (2019) Neonatal alcohol exposure augments voluntary ethanol intake in the absence of potentiated anxiety-like behavior induced by chronic intermittent ethanol vapor exposure. Alcohol 79:17–24
Robbins T, Everitt B (1996) Neurobehavioural mechanisms of reward and motivation. Curr Opin Neurobiol 6:228–236
Stankiewicz AM et al (2015) Novel candidate genes for Alcoholism–transcriptomic analysis of prefrontal medial cortex, hippocampus and nucleus accumbens of Warsaw alcohol-preferring and non-preferring rats. Pharmacol Biochem Behav 139(Pt A):27–38
Cai WT et al (2021) Immunohistochemical detection of GluA1 subunit of AMPA receptor in the rat nucleus accumbens following cocaine exposure. Korean J Physiol Pharmacol 25(1):79–85
Henley JM, Wilkinson KA (2016) Synaptic AMPA receptor composition in development, plasticity and Disease. Nat Rev Neurosci 17(6):337–350
Zhang J, Abdullah JM (2013) The role of GluA1 in central nervous system disorders. Rev Neurosci 24(5):499–505
Liu B et al (2020) Lemon essential oil ameliorates age-associated cognitive dysfunction via modulating hippocampal synaptic density and inhibiting acetylcholinesterase. Aging 12(9):8622–8639
He H et al (2012) Neurodevelopmental role for VGLUT2 in pyramidal neuron plasticity, dendritic refinement, and in spatial learning. J Neurosci 32(45):15886–15901
Hölscher C (2022) GLP-1 and GIP peptide hormones and novel receptor agonists protect synapses in Alzheimer and Parkinson’s Disease. Front Synaptic Neurosci 14:955258
Flores-Bonilla A, Richardson HN (2020) Sex differences in the Neurobiology of Alcohol Use Disorder. Alcohol Res 40(2):04
Morales M et al (2018) Chronic intermittent ethanol exposure modulation of glutamatergic neurotransmission in rat Lateral/Basolateral Amygdala is Duration-, Input-, and sex-dependent. Neuroscience 371:277–287
Crowley NA et al (2019) Ketamine normalizes binge drinking-induced defects in glutamatergic synaptic transmission and ethanol drinking behavior in female but not male mice. Neuropharmacology 149:35–44
White AJ et al (2017) Lifetime Alcohol Intake, binge drinking behaviors, and Breast Cancer risk. Am J Epidemiol 186(5):541–549
Aberg F et al (2017) Binge drinking and the risk of liver events: a population-based cohort study. Liver Int 37(9):1373–1381
Wilsnack RW et al (2018) Gender differences in binge drinking. Alcohol Res 39(1):57–76
Vandegrift BJ et al (2017) Estradiol increases the sensitivity of ventral tegmental area dopamine neurons to dopamine and ethanol. PLoS ONE 12(11):e0187698
Hamson DK, Roes MM, Galea LA (2016) Sex hormones and cognition: neuroendocrine influences on memory and learning. Compr Physiol 6(3):1295–1337
Hyer MM, Phillips LL, Neigh GN (2018) Sex differences in synaptic plasticity: hormones and Beyond. Front Mol Neurosci 11:266
Goltseker K, Hopf FW, Barak S (2019) Advances in behavioral animal models of Alcohol Use Disorder. Alcohol 74:73–82
Funding
This work was supported by National Natural Science Foundation of China (81771193, 81974169, 82171226), National Key R&D Program of China (2019YFC1712104), and Postgraduate independent Innovation Project of Academy of Medical Sciences of Zhengzhou University.
Author information
Authors and Affiliations
Contributions
WL, ZW designed the experiments and analyzed the data. WL prepared the manuscript. Authors WW, ZW, YX, CH provided comments and revised the manuscript, and authors YX, CH were the supervisors. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This study protocol was reviewed and approved by the Ethics committee of Zhengzhou university, approval number ZZUIRBGZR2017-459.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, W., Wang, Z., Wang, W. et al. Liraglutide Reduces Alcohol Consumption, Anxiety, Memory Impairment, and Synapse Loss in Alcohol Dependent Mice. Neurochem Res 49, 1061–1075 (2024). https://doi.org/10.1007/s11064-023-04093-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-023-04093-6