Abstract
Microglia, rapidly activated following peripheral nerve injury (PNI), accumulate within the spinal cord and adopt inflammation that contributes to development and maintenance of neuropathic pain. Microglia express functional Toll-like receptors (TLRs), which play pivotal roles in regulating inflammatory processes. However, little is known about the role of TLR3 in regulating neuropathic pain after PNI. Here TLR3 expression and autophagy activation was assayed in dorsal root ganglions and in microglia following PNI by using realtime PCR, western blot and immunohistochemistry. The role of TLR3/autophagy signaling in regulating tactile allodynia was evaluated by assaying paw mechanical withdrawal threshold and cold allodynia after intrathecal administration of Poly (I:C) and 3-methyladenine (3-MA). We found that L5 spinal nerve ligation (SNL) induces the expression of TLR3 in dorsal root ganglions and in primary rat microglia at the mRNA and protein level. Meanwhile, L5 SNL results in an increased activation of autophagy, which contributes to microglial activation and subsequent inflammatory response. Intrathecal administration of Poly (I:C), a TLR3 agonist, significantly increases the activation of microglial autophagy, whereas TLR3 knockdown markedly inhibits L5 SNL-induced microglial autophagy. Poly (I:C) treatment promotes the expression of proinflammatory mediators, whereas 3-MA (a specific inhibitor of autophagy) suppresses Poly (I:C)-induced secretion of proinflammatory cytokines. Autophagy inhibition further inhibits TLR3-mediated mechanical and cold hypersensitivity following SNL. These results suggest that inhibition of TLR3/autophagy signaling contributes to alleviate neurophathic pain triggered by SNL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuropathic pain following peripheral nerve injury (PNI), correlated with local neuroinflammation in the spinal cord, is a severe incapacitating condition with which clinical treatment remains a major challenge [1, 2]. PNI results in microglial activation that induces excessive inflammation, which contributes to neuropathic pain and secondary tissue damage [3]. The advances in suitable therapy for the purpose of alleviating neuropathic pain hypersensitivity have been limited because the pathophysiological mechanisms causing this remain unclear. Revealing underlying mechanisms for the development of neuroinflammation and neuropathic pain is indispensable for developing effective pharmacotherapy.
Toll-like receptors (TLRs) have been shown to play an important role in inducing innate immunity by recognizing exogenous structures in microorganisms or produced from tissue injury [4, 5]. TLRs signaling have been implicated in the activation of spinal cord microglia during the development of nerve injury-induced neuropathic pain [6, 7]. Several studies showed that microglia express functional TLR2, TLR3, TLR4 and TLR9 [8]. TLR4 is a key microglial receptor in the initiation of behavioral hypersensitivity following PNI. TLR4 expression in spinal microglia is upregulated after L5 SNL in rats [6]. TLR4-knockout mice show a reduced microglial activation and strongly decreased expression of pain related cytokines, and these animals develop less neuropathic pain [9]. Likewise, several studies observed that TLR2 triggers the proinflammatory activation of spinal cord microglia during peripheral nerve injury [10, 11]. Kim et al. demonstrated that TLR2 is necessary for the development of neuropathic pain [10]. TLR2/4 promotes microglial activation and inflammatory injury partly by activating autophagy [12, 13]. Emerging studies showed that TLR3 is also crucial to the development and maintenance of neuropathic pain [14]. Obata et al. reported that TLR3 could induce p38 mitogen-activated protein kinase (MAPK) activation in spinal microglia and result in the development of SNL-induced neuropathic pain [15]. Ketamine can significantly attenuate SNL-induced mechanical allodynia by depressing TLR3 signaling in spinal microglia in a rat model of neuropathic pain [14]. However, the underlying mechanisms of TLR3 in regulating neuropathic pain are not clarified.
Autophagy is a lysosome-mediated intracellular catabolic process by which cells remove their damaged organelles for the maintenance of cellular homeostasis [16]. Several researches showed that autophagy involves in the regulation of inflammatory response [17, 18]. Shi et al. demonstrated that miR-195 increases neuroinflammation and aggravates neuropathic pain by inhibiting autophagy following PNI [18]. Interestingly, mRNA is an endogenous ligand for TLR3. Therefore traumatic injury that accumulates RNA in pathologic lesions has the potential to activate this receptor [8].
Based on above findings, we hypothesized that TLR3 might be involved in nerve injury-induced activation of spinal cord microglia, and autophagy might play important roles in TLR3-mediated neuroinflammation and neuropathic pain.
Materials and Methods
Neuropathic Pain Model
All animal experiments were carried out according to the guidelines of the International Association for the Study of Pain and were approved by the Animal Care and Use Committee of Ruijin Hospital Luwan Branch. Male Sprague–Dawley rats (180–200 g) were purchased from the Animal Center of the Chinese Academy of Sciences (Shanghai, China) and maintained in a specific pathogen-free environment under conditions of 22–25 °C ambient with food and water available. Every effort was made to alleviate pain and suffering during the experimental procedures, and the number of rats used was the least required to obtain significant statistical power.
The L5 SNL model was produced as previously described [19, 20]. Briefly, rats were anesthetized with isoflurane (2.5%, Baxter, Deerfield, IL), and an approximately 2-cm long skin incision was made along the rat’s back. After removal of L6 transverse spinal process, the L5 spinal nerve was identified and ligated tightly with a 3 − 0 silk thread without damage to the dorsal root ganglions or other nerves. In sham-operated rats, the left L5 spinal nerve was isolated, without ligation. In each group, the ipsilateral L4 spinal nerve remained untouched, and the right side was not subjected to any surgery.
Real-time PCR
Total RNA was isolated from ipsilateral spinal cord or cultured microglia by using Trizol Reagent (Life Technologies, CA, USA) and was reverse-transcribed to cDNA using the Oligo (dT) 18 primer. Quantitative real-time PCR (qPCR) was performed using a standard protocol from the SYBR Premix Ex Taq (TaKaRa) on Applied Biosystems 7300 real-time PCR system (Applied Biosystems, Foster City, CA). The qPCR primers for TLR3 are as follows: forward (TCTTTCCTACAACAGCCTCCG) and reverse (TAAATGCTCGCTTCAAACTCAG). β-actin was used as references for mRNAs. Each sample was analyzed in triplicate. PCR was carried out as previously described [21] at the following conditions: denaturing at 94 °C for 10 min, followed by 40 cycles of 94 °C for 10 s, 55 °C for 10 s and 72 °C for 10 s. Data were analyzed using the comparative threshold cycle (Ct) method, and results were expressed as fold difference.
Western Blot Analysis
After quantifications of the protein samples using BCA Protein Assay Kit (Pierce Biotechonology, Rockford, IL). A total of 120 µg protein of ipsilateral L5 spinal sample or cultured microglia was electrophoresed through a 12% SDS-polyacrylamide gel, and then wet electro-transferred to 0.2 µm PVDF membranes (Bio-Rad). The blots were incubated overnight at 4 °C with antibodies (TLR3: 1 µg/mL, ab62566, Abcam, CA, USA; Microtubule-associated protein 1 light chain 3 beta (LC3B): 1 µg/mL, ab63817, Abcam; Sequestosome 1 (SQSTM1/ p62): 2 µg/mL, ab56416, Abcam), then incubated with a goat anti-rabbit HRP-conjugated secondary antibody (1:5000, Jackson, USA). Protein signals were assayed using an enhanced chemiluminescence detection system (Pierce Biotechonology, Rockford, IL). An anti-β-actin antibody with 1:1000 dilution (Cell Signaling Technology, USA) was used as an internal control. The intensity of the selected bands was analyzed using Image J software (National Institutes of Health [NIH], Bethesda, MD, USA).
Primary Microglial Cell Cultures
The spinal microglial cells were isolated by Percoll density gradient centrifugation as described previously [8, 10, 18, 22]. Briefly, rats were sacrificed and the portions of the ipsilateral L4–L5 spinal cord were isolated. Spinal cords were ground in ice-cold Hanks’ balanced salt solution. Suspensions were passed through a 70-μm cell strainer (Falcon, Becton Dickinson and Company, Heidelberg, Germany) and cells were centrifuged at 1000 rpm for 10 min. A density gradient consisting of 4 mL cells in 75% Percoll, 3 mL 50% Percoll, 3 mL 35% Percoll and 2 mL PBS was centrifuged (1000 g for 20 min). Cells at the 50/75% interface were collected, washed in ice-cold PBS, and maintained in DMEM, supplemented with heat-inactivated 10% fetal bovine serum (Gibco, USA), 100 U/mL penicillin, and 0.1 mg/mL streptomycin (Gibco, USA). Microglia were harvested from the underlying astrocytic monolayer by gentle agitated. Purity of microglia was determined by CD11b staining and was greater than 98% (Supplementary Fig. S1). The following experiments were carried out after culturing for 2–4 days.
ELISA Assay
Primary microglial cells were plated on 96-well plates at a density of 2 × 104/well. After stimulation with indicated reagents, IL-1β and TNF-α released into the culture medium were assessed using ELISA kits. Rat IL-1β and TNF-α ELISA kits were purchased from R&D Systems (R&D, MN, USA). Plates were read using a microplate reader (Model 550, Bio-Rad, USA) at a 450 nm wavelength. Each sample was analyzed in triplicate.
Immunofluorescence
Rats were anesthetized with sodium pentobarbital (50 mg/kg, i.p.) and transcardially perfused with 4% paraformaldehyde in 0.1 M PBS (pH 7.4). The L5 spinal cord was removed, postfixed in 4% paraformaldehyde for 1 h at room temperature. Spinal cord transverse Sections (14-μm-thick) were prepared on a gelatin-coated slide glass using a cryomicrotome (Leica). The sections were briefly rinsed in PBS and blocked in a solution containing 5% BSA (Sigma) and 0.1% Triton X-100 (Sigma) for 1 h at room temperature. The sections were then incubated overnight at 4 °C with the indicated primary antibody (TLR3: 5 µg/mL, ab62566, Abcam). After rinsing in 0.1 M PBS, the sections were incubated for 1 h at room temperature with a mixture of FITC-conjugated or Cy3-conjugated secondary antibodies (1:200, Jackson ImmunoResearch Laboratories). Fluorescent images were obtained with the FluoView™ FV1000 confocal microscope (Olympus, Tokyo, Japan).
Additionally, microglial cells were fixed with 4% paraformaldehyde, and subjected to immunocytochemistry using TLR3 antibody (5 µg/mL, ab62566, Abcam). Microglia were identify using Iba1 antibody (1:1000, WAKO). Samples were examined with the FluoView™ FV1000 confocal microscope (Olympus).
Autophagy level was assayed using an autophagy detection kit according to the manufacturers’ instructions (ENZ-51031-K200, Enzo life science). In brief, 2 × 104 microglial cells were seeded on poly-l-lysine-coated coverslips sitting on the bottom of 12-well plates. After 24 h, cells were washed once in PBS and re-suspended in 1 × Cyto-ID Green autophagy detection reagent and incubated at room temperature for 30 min. Analysis of the stained cells was performed with the FluoView™ FV1000 confocal microscope (Olympus). Green puncta was calculated to show the activation of autophagy.
Intrathecal Injections
Intrathecal administration was performed by lumbar puncture as described by Calvo et al. [23]. Under anaesthesia a 26G-gauge needle was inserted between the L5 and L6 vertebrae. About 10 μL of working solution containing poly (I:C) (5 mg/mL), 3-MA (1.5 mg/kg/day) or siRNA mixtures against TLR3 (0.2 μg/μl, Santa Cruz Biotechnology, CA, USA), which was referred to as Khoroosh’s study [24] and according to our preliminary results, was given once a day for 2 weeks. The knockdown effects of the mixtures of three siRNAs were verified in vivo and in vitro. Saline was used for control injections. The quality of each injection was ensured by the observation of an injection-induced tail-flick.
Behavioral Assessment
Tests were performed as described previously [18]. Mechanical sensitivity were tested using calibrated von Frey filaments (Stoelting, Wood Dale, IL) applied to the plantar surface of the hind paw ipsilateral to surgery. A servo-controlled mechanical stimulus was applied to the plantar surface at 10-min intervals. The withdrawal threshold of each paw was tested three times for each time point and mean values were used in the analysis. To test the cold allodynia, a drop (50 µl) of acetone was applied to the centre of the plantar face of a hindpaw. Acetone was applied alternately twice to each hindpaw, with 5 min between each successive application. Responses were monitored during 2 min after acetone application. All behavioral tests were assessed by the same author (Weijia Chen) who is not aware of the group assignment.
Statistical Analysis
Data are presented as mean ± standard deviation (SD) from at least three separate experiments. The unpaired Student t test was used to assess statistical differences between two experimental conditions. Differences among more than two experimental conditions were tested by the one-way ANOVA, followed by the Scheffé test to analyze differences between groups. Behavioural data was analyzed using RM two-way ANOVA. Differences were deemed statistically significant at p < 0.05.
Results
L5 SNL Results in an Increased Expression of TLR3
Emerging studies showed that TLRs play pivotal roles in PNI-induced inflammatory processes, and individual TLRs have been investigated in nociception [25]. However, the role of TLR3 in the regulation of neuropathic pain following SNL remains unclear. Here we first assayed whether L5 SNL changes the expression level of TLR3. As shown in Fig. 1a, TLR3 mRNA level is promptly increased in the L5 spinal cord tissues after L5 SNL and maintained at higher values throughout a period of 14 d compared to that for the sham-operated group. Then we carried out immunofluorescence analysis costaining with antibodies against TLR3 and Iba1 in the ipsilateral L5 spinal cord dorsal horn. Figure 1b showed that TLR3 expression is increased following injury, and the TLR3-immunoreactivity usually co-localized to microglial markers Iba1. Western blot analysis also verified that the expression of TLR3 is enhanced after L5 SNL compared to sham-operated group (Fig. 1c).
We further analyzed the expression level of TLR3 in primary microglial cells because microglial cells are key cellular mediators of neuroinflammatory processes. Figure 1d showed that the mRNA level of TLR3, which is low in sham-operated rats, is upregulated in spinal microglia after L5 SNL, starting from postoperative 2 days, and persisting a period of 14 days. Western blot analysis verified that the protein level of TLR3 is increased following L5 SNL (Fig. 1e). We next performed double-immunolabeling with cell type specific markers and found that most TLR3 + cells are positive for the microglial markers Iba1, and spinal microglia with the high levels of TLR3 also indicates an activated morphology (Fig. 1f).
TLR3 expression is increased after SNL. a The mRNA level of TLR3 is increased in the L5 spinal cord tissues after L5 SNL. Total RNA was extracted from the L5 spinal cord tissues of sham-operated and SNL-injured rats and was subjected to real-time PCR to analyze the relative expression level of TLR3 in each sample. n = 9. *p < 0.05 vs. sham. b TLR3 and microglial marker (Iba-1) protein levels were assayed using in situ immunofluorescence in the ipsilateral L5 spinal cord dorsal horn. Representative spinal cord sections are shown. Scale bar 50 µm. c Western blot analysis of TLR3 protein expression in the L5 spinal cord tissues in each sample. n = 9. *p < 0.05 vs. sham. d Primary spinal microglial cells were isolated from sham-operated and SNL-injured rats at the indicated time, and relative TLR3 mRNA levels were analyzed by real-time PCR. n = 9. *p < 0.05 vs. sham. e Primary spinal microglial cells were isolated from sham-operated and SNL-injured rats at the indicated time, and relative TLR3 protein levels were analyzed using western blot. n = 9. *p < 0.05. f Double immunofluorescence labeling for TLR3 (red) and cell-type markers (Iba-1, microglia marker, green) in spinal microglial cells isolated from sham-operated and SNL-injured rats. Scale bar 50 µm. (Color figure online)
L5 SNL Increases the Activation of Microglial Autophagy
Much evidence demonstrated that TLRs-mediated autophagy contributes to microglial activation and inflammatory injury in mouse models of intracerebral haemorrhage [13] or in rat models of PNI [25]. Autophagy activation involves in the regulation of inflammatory response [17, 18]. For example, autophagy inhibition suppresses miR-195-induced neuroinflammation and neuropathic pain after PNI [18]. To verify this speculation, we carried out in situ IHC costaining with antibodies against LC3 and Iba1 in the ipsilateral L5 spinal cord dorsal horn. Figure 2a showed that LC3 expression is increased following injury, and the LC3-immunoreactivity usually co-localized to microglial markers Iba1. Then primary microglia cells were isolated from sham- and SNL-treated rats, and respective activation of autophagy was analyzed. Figure 2b showed that following SNL, there is an increase of green puncta representing autophagic vacuoles and an accumulation of LC3-II in spinal microgial cells, indicating that autophagy is activated. The ratio of LC3-II to LC3-I has been shown to be a reliable indicator of autophagy [26]. Figure 2c showed that L5 SNL results in an increase in the ratio of LC3-II/LC3-I. The ubiquitin-binding protein p62 is an autophagy substrate, which upon direct binding to LC3 incorporates into autophagosomes and is efficiently degraded by autophagy [27]. The autophagy flux is further determined by assaying the decrease of p62/SQSTM1 protein level, a well-established autophagy substrate (Fig. 2d).
L5 SNL increases the activation of microglial autophagy. a Autophagy marker (LC3) and microglial marker (Iba-1) protein levels were assayed using in situ IHC in the ipsilateral L5 spinal cord dorsal horn. Representative spinal cord sections are shown. n = 3, Scale bar 100 µm. b Primary spinal microglial cells were isolated from sham-operated and SNL-injured rats (n = 3) at day 10, and the autophagosome formation was visualized by assaying activated green puncta. Punctate staining is indicative for the redistribution of LC3 to autophagosomes. The average number of green puncta per cell with standard deviation for each group is presented. Scale bar 50 µm. *p < 0.05. c Primary spinal microglial cells were isolated from sham-operated and SNL-injured rats (n = 3) at day 10, and LC3B protein levels were assayed using western blot analysis. p < 0.05. d Primary spinal microglial cells were isolated from sham-operated and SNL-injured rats (n = 3) at day 10, and the protein levels of p62 were assayed using western blot analysis. p < 0.05. (Color figure online)
TLR3 Positively Regulates Autophagy Activation
L5 SNL upregulates TLR3 expression and increases the activation of autophagy. Then we will investigate whether TLR3 mediates autophagy activation. Primary microglial cells were isolated from sham rats and were treated with Poly (I:C), a TLR3 agonist. Figure 3a showed that Poly (I:C) treatment results in an increase of green puncta, indicating that autophagy is activated. Western blot analysis showed that Poly (I:C) treatment increases the ratio of LC3-II/LC3-I (Fig. 3b). The autophagy flux is further verified by assaying the decrease of p62/SQSTM1 protein level (Fig. 3c). We next investigated whether TLR3 knockdown inhibits microglial autophagy after L5 SNL. Figure 3d, e showed that the activation of microglial autophagy following SNL, measured by immunofluorescence and western blot analysis, is decreased after TLR3 knockdown in vivo. The inhibition of autophagy flux is further verified by assaying the p62/SQSTM1 protein level (Fig. 3f). These data suggest that TLR3 positively regulates autophagy activation following L5 SNL.
TLR3 positively regulates autophagy activation. a Primary spinal microglial cultures isolated from sham rats (n = 3) were treated with poly (I:C) (0.5 μg/mL), and the autophagosome formation was evaluated by assaying green puncta. The average number of green puncta per cell with standard deviation for each group is presented. Scale bar 50 µm. *p < 0.05. Primary spinal microglial cultures isolated from sham rats (n = 3) were treated with poly (I:C), and LC3B protein levels (b) or p62 protein levels (c) were assayed using western blot analysis. *p < 0.05. Primary spinal microglial cultures were isolated from SNL-rats (n = 3) treated with TLR3 specific siRNAs, and the autophagosome formation was evaluated by assaying green puncta (d), LC3B protein levels (e) or p62 protein levels (f). Scale bar 50 µm. *p < 0.05. (Color figure online)
TLR3/Autophagy Signaling Regulates Neuroinflammation, and Mechanical and Cold Hypersensitivity After L5 SNL
To investigate the role of TLR3/autophagy signaling on regulating neuroinflammation and neuropathic pain following SNL, microglial cells were treated with Rapa (an autophagy agonist) and proinflammatory cytokines were assessed after treatment with Poly (I:C). Rapa significantly increases Poly (I:C)-induced expression of IL-1β and TNF-α in spinal microglia, whereas knockdown of TLR3 suppresses Poly (I:C) and Rapa-induced release of pro-inflammatory cytokines (Fig. 4a, b). Expectedly, 3-MA (a specific autophagy inhibitor) treatment inhibits Poly (I:C)-induced secretion of pro-inflammatory cytokines (Fig. 4c, d).
TLR3/autophagy signaling regulates neuroinflammation. Primary spinal microglial cultures isolated from sham-operated rats (n = 3) were treated with siTLR3 (30nM), poly (I:C) (0.5 μg/mL) and Rapa (500 nM). ELISA analysis of IL-1β (a) or TNF-α (b) of protein levels were carried out using Elisa kit. Primary spinal microglial cultures isolated from sham-operated rats (n = 3) were treated with poly (I:C) (0.5 μg/mL) and 3-MA (1 μM). ELISA analysis of IL-1β (c) or TNF-α (d) of protein levels were carried out using Elisa kit. Data are expressed as mean ± SD. *p < 0.05
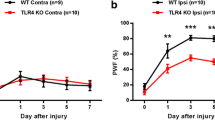
To examine the role of TLR3/autophagy signaling in regulating tactile allodynia, we measured paw mechanical withdrawal threshold and cold allodynia after intrathecal administration of Poly (I:C) and 3-MA. Intrathecal administration of Poly (I:C) results in a significant increase in cold sensitivity, whereas 3-MA effectively inhibits Poly (I:C)-induced acute cold hypersensitivity (Fig. 5a). Poly (I:C) treatment displays a marked decrease in the paw mechanical withdrawal threshold in rat model of L5 SNL, whereas intrathecal administration of 3-MA reduces the effect of Poly (I:C) on enhancing mechanical sensitivity (Fig. 5b). These results confirmed that inhibition of TLR3/autophagy signaling might effectively suppress SNL-induced neuroinflammation and alleviate neuropathic pain.
TLR3/autophagy regulates mechanical and cold hypersensitivity after L5 SNL. Cold (a) and mechanical (b) pain-related hypersensitivity developed after treatment with poly (I:C) (5 mg/mL, 10 μL, once a day) and 3-MA (1.5 mg/kg/day) at the indicated time after surgery. n = 9. Data are expressed as mean ± SD. *p < 0.05, # p < 0.05
Discussion
Several studies have demonstrated the expression of TLRs on spinal glia and the ability of TLR agonists to evoke secretion of cytokines, and have emphasized the role of spinal TLRs in spinally mediated facilitated pain states [25, 28–30]. In models of persistent inflammation, mice with defects in TLRs expression show a prominent attenuation of behaviorally defined hyperpathia [25, 31].
In the current study, our results clearly show the induction of TLR3 in the spinal microglia and that TLR3 expression is crucial to the production of pro-inflammatory cytokines, including TNF-a and IL-1β. Meanwhile, L5 SNL induces the activation of autophagy, which contributes to microglial activation and subsequent pro-inflammatory response. More important, we revealed that TLR3 directly regulates autophagy activation in spinal microglia. Intrathecal administration of Poly (I:C) contributes to the activation of microglial autophagy, whereas TLR3 inhibition by its specific siRNAs suppresses L5 SNL-induced microglial autophagy. Functionally, autophagy activation by Rapa treatment increases the production of pro-inflammatory cytokines, whereas knockdown of TLR3 inhibits Rapa-induced neuroinflammation. Finally we demonstrated that autophagy inhibition by specific inhibitor alleviates TLR3-mediated mechanical and cold hypersensitivity following L5 SNL.
Autophagy, an intracellular degradation and energy recycling mechanism, is emerging as a crucial regulator of immune responses, and defects in autophagy have been linked to several inflammation-related diseases [16, 32], including steroid-resistant airway inflammation [33], inflammatory bowel disease [34] and neuroinflammation [35]. The relationship between autophagy and inflammation are complex. On one hand, previous studies showed that autophagy negatively regulates inflammation to prevent the harmful amplification of inflammatory factors [36]. For example, autophagy inhibition results in an activation of inflammasomes which control the proteolytic processing and secretion of IL-1β and IL-18 under inflammatory stress [37, 38]. In an addition, inhibition of autophagy related 16-like 1 promotes the releases of IL-1β and IL-18 in the mouse model of Crohn’s disease [39]. On another hand, several reports demonstrated that autophagy contributes to microglial activation and inflammatory injury. For example, erythrocyte lysis induces TLR4-mediated microglial autophagy [13]. The autophagy inhibition decreases microglial activation and inflammatory injury, and improves the neurological function after intracerebral haemorrhage [13]. Also, cocaine-induced upregulation of autophagy contributes to cocaine-mediated activation of microglia. Inhibition of autophagy results in a decreased expression and release of inflammatory factors in microglial cells [40]. In our study, we found that L5 SNL activates microglial autophagy. Autophagy activation contributes to the releases of pro-inflammatory cytokines and increases mechanical and cold hypersensitivity after L5 SNL.
Emerging studies revealed that TLR-mediated autophagy regulates microglial activation and inflammatory injury. TLR 4 is a sensor for autophagy associated with innate immunity [41]. Yang et al. reported that lysed erythrocyte-treated microglia (TLR4−/−) have reduced autophagy activation and inflammation compared with microglia (wildtype) in vitro [13]. The autophagy inhibitor (3-MA) could markedly inhibit microglial activation and inflammatory injury due to lysed erythrocyte treatment, and improve the neurological function of intracerebral haemorrhage mice. Additionally, TLR2 ligands could also induce autophagy and regulate microglial cell death [12]. However, the roles of TLR3 in regulating autophagy activation and the effects of TLR3/autophagy signaling on regulating neuroinflammation and subsequent neuropathic pain following PNI remain unclear. Here our results demonstrated that upregulated expression of TLR3 following L5 SNL promotes the activation of microglial autophagy, and that inhibition of TLR3/autophagy signaling contributes to alleviate neurophathic pain triggered by SNL.
References
Ellis A, Bennett DL (2013) Neuroinflammation and the generation of neuropathic pain. Br J Anaesth 111:26–37
Masuda T, Iwamoto S, Yoshinaga R, Tozaki-Saitoh H, Nishiyama A, Mak TW, Tamura T, Tsuda M, Inoue K (2014) Transcription factor IRF5 drives P2 × 4R+-reactive microglia gating neuropathic pain. Nat Commun 5:3771
Myers RR, Campana WM, Shubayev VI (2006) The role of neuroinflammation in neuropathic pain: mechanisms and therapeutic targets. Drug Discov Today 11:8–20
Takeuchi O, Akira S (2010) Pattern recognition receptors and inflammation. Cell 140:805–820
Nguyen MD, Julien JP, Rivest S (2002) Innate immunity: the missing link in neuroprotection and neurodegeneration? Nat Rev Neurosci 3:216–227
Tanga FY, Nutile-McMenemy N, DeLeo JA (2005) The CNS role of Toll-like receptor 4 in innate neuroimmunity and painful neuropathy. Proc Natl Acad Sci USA 102:5856–5861
Mei XP, Zhou Y, Wang W, Tang J, Zhang H, Xu LX, Li YQ (2011) Ketamine depresses toll-like receptor 3 signaling in spinal microglia in a rat model of neuropathic pain. Neurosignals 19:44–53
Li X, Cudaback E, Keene CD, Breyer RM, Montine TJ (2011) Suppressed microglial E prostanoid receptor 1 signaling selectively reduces tumor necrosis factor alpha and interleukin 6 secretion from toll-like receptor 3 activation. Glia 59:569–576
Bettoni I, Comelli F, Rossini C, Granucci F, Giagnoni G, Peri F, Costa B (2008) Glial TLR4 receptor as new target to treat neuropathic pain: efficacy of a new receptor antagonist in a model of peripheral nerve injury in mice. Glia 56:1312–1319
Kim D, Kim MA, Cho IH, Kim MS, Lee S, Jo EK, Choi SY, Park K, Kim JS, Akira S, Na HS, Oh SB, Lee SJ (2007) A critical role of toll-like receptor 2 in nerve injury-induced spinal cord glial cell activation and pain hypersensitivity. J Biol Chem 282:14975–14983
Lim H, Kim D, Lee SJ (2013) Toll-like receptor 2 mediates peripheral nerve injury-induced NADPH oxidase 2 expression in spinal cord microglia. J Biol Chem 288:7572–7579
Arroyo DS, Soria JA, Gaviglio EA, Garcia-Keller C, Cancela LM, Rodriguez-Galan MC, Wang JM, Iribarren P (2013) Toll-like receptor 2 ligands promote microglial cell death by inducing autophagy. FASEB J 27:299–312
Yang Z, Liu B, Zhong L, Shen H, Lin C, Lin L, Zhang N, Yuan B (2015) Toll-like receptor-4-mediated autophagy contributes to microglial activation and inflammatory injury in mouse models of intracerebral haemorrhage. Neuropathol Appl Neurobiol 41:e95–e106
Mei XP, Zhou Y, Wang W, Tang J, Wang W, Zhang H, Xu LX, Li YQ (2011) Ketamine depresses toll-like receptor 3 signaling in spinal microglia in a rat model of neuropathic pain. Neurosignals 19:44–53
Obata K, Katsura H, Miyoshi K, Kondo T, Yamanaka H, Kobayashi K, Dai Y, Fukuoka T, Akira S, Noguchi K (2008) Toll-like receptor 3 contributes to spinal glial activation and tactile allodynia after nerve injury. J Neurochem 105:2249–2259
Klionsky DJ, Emr SD (2000) Autophagy as a regulated pathway of cellular degradation. Science 290:1717–1721
Srivastava IN, Shperdheja J, Baybis M, Ferguson T, Crino PB (2015) mTOR pathway inhibition prevents neuroinflammation and neuronal death in a mouse model of cerebral palsy. Neurobiol Dis 85:144–154
Shi G, Shi J, Liu K, Liu N, Wang Y, Fu Z, Ding J, Jia L, Yuan W (2013) Increased miR-195 aggravates neuropathic pain by inhibiting autophagy following peripheral nerve injury. Glia 61:504–512
Kim SH, Chung JM (1992) An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain 50:355–363
Ge Y, Wu F, Sun X, Xiang Z, Yang L, Huang S, Lu Z, Sun Y, Yu WF (2014) Intrathecal infusion of hydrogen-rich normal saline attenuates neuropathic pain via inhibition of activation of spinal astrocytes and microglia in rats. PLoS One 9:e97436
Ueno S, Yamada H, Moriyama T, Honda K, Takano Y, Kamiya HO, Katsuragi T (2002) Measurement of dorsal root ganglion P2X mRNA by SYBR Green fluorescence. Brain Res Brain Res Protoc 10:95–101
Dominguez E, Rivat C, Pommier B, Mauborgne A, Pohl M (2008) JAK/STAT3 pathway is activated in spinal cord microglia after peripheral nerve injury and contributes to neuropathic pain development in rat. J Neurochem 107:50–60
Calvo M, Zhu N, Grist J, Ma Z, Loeb JA, Bennett DL (2011) Following nerve injury neuregulin-1 drives microglial proliferation and neuropathic pain via the MEK/ERK pathway. Glia 59:554–568
Khorooshi R, Morch MT, Holm TH, Berg CT, Dieu RT, Draeby D, Issazadeh-Navikas S, Weiss S, Lienenklaus S, Owens T (2015) Induction of endogenous Type I interferon within the central nervous system plays a protective role in experimental autoimmune encephalomyelitis. Acta Neuropathol (Berl) 130:107–118
Stokes JA, Corr M, Yaksh TL (2013) Spinal toll-like receptor signaling and nociceptive processing: regulatory balance between TIRAP and TRIF cascades mediated by TNF and IFNbeta. Pain 154:733–742
Klionsky DJ, Abeliovich H, Agostinis P, Agrawal DK, Aliev G, Askew DS et al (2008) Guidelines for the use and interpretation of assays for monitoring autophagy in higher eukaryotes. Autophagy 4:151–175
Berliocchi L, Russo R, Maiaru M, Levato A, Bagetta G, Corasaniti MT (2011) Autophagy impairment in a mouse model of neuropathic pain. Mol Pain 7:83
Bowman CC, Rasley A, Tranguch SL, Marriott I (2003) Cultured astrocytes express toll-like receptors for bacterial products. Glia 43:281–291
Jack CS, Arbour N, Manusow J, Montgrain V, Blain M, McCrea E, Shapiro A, Antel JP (2005) TLR signaling tailors innate immune responses in human microglia and astrocytes. J Immunol 175:4320–4330
Qi J, Buzas K, Fan H, Cohen JI, Wang K, Mont E, Klinman D, Oppenheim JJ, Howard OM (2011) Painful pathways induced by TLR stimulation of dorsal root ganglion neurons. J Immunol 186:6417–6426
Bsibsi M, Ravid R, Gveric D, van Noort JM (2002) Broad expression of Toll-like receptors in the human central nervous system. J Neuropathol Exp Neurol 61:1013–1021
Levine B, Klionsky DJ (2004) Development by self-digestion: molecular mechanisms and biological functions of autophagy. Dev Cell 6:463–477
Suzuki Y, Maazi H, Sankaranarayanan I, Lam J, Khoo B, Soroosh P, Barbers RG, James Ou JH, Jung JU, Akbari O (2015) Lack of autophagy induces steroid-resistant airway inflammation. J Allergy Clin Immunol 137(5):1382–1389
Rufini S, Ciccacci C, Di Fusco D, Ruffa A, Pallone F, Novelli G, Biancone L, Borgiani P (2015) Autophagy and inflammatory bowel disease: Association between variants of the autophagy-related IRGM gene and susceptibility to Crohn’s disease. Dig Liver Dis 47:744–750
Motori E, Puyal J, Toni N, Ghanem A, Angeloni C, Malaguti M, Cantelli-Forti G, Berninger B, Conzelmann KK, Gotz M, Winklhofer KF, Hrelia S, Bergami M (2013) Inflammation-induced alteration of astrocyte mitochondrial dynamics requires autophagy for mitochondrial network maintenance. Cell Metab 18:844–859
Liang P, Le W (2015) Role of autophagy in the pathogenesis of multiple sclerosis. Neurosci Bull 31:435–444
Shi CS, Shenderov K, Huang NN, Kabat J, Abu-Asab M, Fitzgerald KA, Sher A, Kehrl JH (2012) Activation of autophagy by inflammatory signals limits IL-1beta production by targeting ubiquitinated inflammasomes for destruction. Nat Immunol 13:255–263
Deretic V, Saitoh T, Akira S (2013) Autophagy in infection, inflammation and immunity. Nat Rev Immunol 13:722–737
Saitoh T, Fujita N, Jang MH, Uematsu S, Yang BG, Satoh T, Omori H, Noda T, Yamamoto N, Komatsu M, Tanaka K, Kawai T, Tsujimura T, Takeuchi O, Yoshimori T, Akira S (2008) Loss of the autophagy protein Atg16L1 enhances endotoxin-induced IL-1beta production. Nature 456:264–268
Guo ML, Liao K, Periyasamy P, Yang L, Cai Y, Callen SE, Buch S (2015) Cocaine-mediated microglial activation involves the ER stress-autophagy axis. Autophagy 11:995–1009
Xu Y, Jagannath C, Liu XD, Sharafkhaneh A, Kolodziejska KE, Eissa NT (2007) Toll-like receptor 4 is a sensor for autophagy associated with innate immunity. Immunity 27:135–144
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest exist.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, W., Lu, Z. Upregulated TLR3 Promotes Neuropathic Pain by Regulating Autophagy in Rat With L5 Spinal Nerve Ligation Model. Neurochem Res 42, 634–643 (2017). https://doi.org/10.1007/s11064-016-2119-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-016-2119-2