Abstract
Diabetic neuropathy represents one of the most prevalent complications of diabetes mellitus. The aim of this study was to investigate the effect of diabetes-induced disturbances in neurons on the Ca2+-triggered membrane fusion process in cell-free system in relation to plasmalemma cholesterol level. The gabapentin therapy on the exocytosis process was also studied. The diabetes in rats was induced by streptozotocin (60 mg/kg of body weight, i.p.). After 4 weeks of diabetes induction the one group of diabetic rats was treated with gabapentin (50 mg/kg, i.p.) during 1 month. Fusion experiments were performed in the cell-free model system using fluorescent dye octadecylrhodamine B. The [2-14C]serotonin preloaded synaptosomes were used for assay of stimulated neurotransmitter release. The synaptosomal plasma membrane cholesterol level in diabetic rats was on 12 % higher than in control and was decreased on 5 % after gabapentin therapy. The rate of synaptic vesicles fusion with plasma membranes in the presence of Ca2+ and synaptosomal cytosolic proteins was decreased to 14.5 % in diabetic rats as compared to control (23 %) and after gabapentin administration to diabetic rats was raised to 18 %. At diabetes the stimulated synaptosomal serotonin release was increased in 1.7–2 folds and was partially normalized by gabapentin therapy. Together, these findings suggest that elevated cholesterol content in neuronal plasma membranes at diabetes impairs the membrane fusion process in neurons that can induce the development of neuropathy. Diabetes-evoked impairments of the exocytotic process can be attenuated by gabapentin therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The variety of complications associated with diabetes extend to the central nervous system (CNS) and induce the dysregulation of multiple extracellular and intracellular signalling cascades, which in turn could lead to alteration in neuronal and synaptic functions [1, 2]. However, the mechanisms leading to complex morphological, metabolic and functional changes in the central and peripheral nervous system in diabetes mellitus are multiple and incompletely understood.
The Ca2+-triggered fusion of synaptic vesicles (SVs) with the presynaptic plasma membranes (PM) is regarded as a final step of exocytosis. Recent genetic and biochemical studies have revealed that this highly regulated fusion process involves a cascade of protein–protein and protein–lipid interactions [3, 4]. According to the SNARE hypothesis, protein complex known as the soluble N-ethylmaleimide-sensitive factor attachment protein receptors (SNAREs) plays a fundamental role in synaptic vesicle fusion process [5]. We consider that disturbances of calcium-dependent SVs fusion in neurons may be one of pathophysiological mechanism at diabetes.
Moreover among the lipids that compose neuronal membranes cholesterol has often been reviewed as compound involved in regulated exocytosis [6–8]. Cholesterol and its derivatives are implicated in processes such as the modulation of membrane protein function, membrane trafficking, transmembrane signaling and steroid hormone’s synthesis [9]. The importance of cholesterol for brain functions is attested by the fact that the brain contains >2 % cholesterol by weight. Most (80–90 %) cellular cholesterol is located in the PM [10, 11], it is also enriched in exocytic vesicles, comprising up to 40 mol % of total lipids [12].
The cholesterol-enriched microdomains of neuronal plasmalemma and SVs have important role in synaptic function [13, 14].
We have demonstrated that isolated membrane structures of synaptosomes retain the capacity for Ca2+-triggered fusion [15]. Our cell-free system serves as the model of final step of exocytosis and was used for the studying of alterations of this process at diabetes and for monitoring of drugs which affect on membrane fusion process.
It is known that the action of antiepileptic drugs (AEDs) is directed toward protection of the brain against the development of abnormally massive hypersynchronous impulse activity of cerebral neurons. Most anticonvulsive AEDs can act simultaneously via several cellular mechanisms. Gabapentin, a lipophilic compound, was initially synthesized to mimic the chemical structure of GABA by addition of a cyclohexyl to its backbone [16]. The gabapentin is a blocker of voltage-gated calcium channels that produces multiple pharmacological effects and it is used not only as an anticonvulsant but also in the treatment of chronic pain related to diabetic peripheral neuropathy [17].
The aim of this study was the investigation of diabetes-induced disturbances in neurons and effect of gabapentin therapy on the Ca2+-triggered membrane fusion in cell-free system and serotonin release from synaptosomes.
Materials and Methods
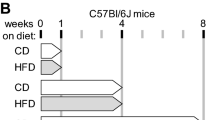
Unless otherwise stated, all chemicals were reagent-grade quality and streptozotocin was purchased from Sigma Chemical Co., St. Louis, Mo., USA. The experiments were performed on male Wistar rats with approximately body weight 250–270 g, fed a standard rat laboratory diet and had free access to food and water. Following 1–2 weeks of acclimation, animals were randomly assigned to treatment groups. Diabetes was induced in the male rats by a single intraperitoneal injection of freshly prepared solution of streptozotocin (60 mg/kg of body weight) dissolved in citrate buffer (pH 4.5) while the control group was injected with the buffer only. Body weights of all the animals were recorded weekly, prior to the treatments and sacrifice. Animals were maintained on 12-h light/dark cycle and randomly divided into the following groups: (1) control group; (2) diabetic group with 8-weeks duration of diabetes; (3) diabetic group treated with gabapentin in a dose of 50 mg/kg body weight−1 day−1, intraperitoneally, for 4 weeks. The rats with blood glucose level over 21.3 ± 1.9 mmol/l were taken into experiments. All procedures were carried out in accordance with the national and international guidelines and laws concerning animal welfare and are ethically acceptable. After 8 weeks rats of experimental and control groups were sacrificed via cervical dislocation under mild diethyl ether narcosis. Plasma glucose level was determined by Glukometr Precision Xtra Plus (MediSense UK Ltd., Oxon, UK).
Isolation of Synaptosomes
The Wistar rats (150–200 g body weight) were killed by decapitation; the brains were rapidly removed and kept on ice. Rat brains were weighted, cut into pieces, transferred to ice-cold 0.32 M sucrose, 10 mM Tris-HCl, pH 7.5 (9 ml/g of brain tissue) and gently homogenized using a glass homogenizer with a Teflon plunger (0.25 mm clearance). All manipulations were performed at 0 °C. Synaptosomes were prepared by differential centrifugation of rat brain homogenate. The homogenate was centrifuged at 1,500g for 10 min and the supernatant was removed and centrifuged at 12,000g for 20 min. The resultant pellet was the fraction of crude synaptosomes. For serotonin release assay the crude synaptosomal fraction was resuspended and subjected to centrifugation in discontinuous sucrose gradient (0.8, 1.0 and 1.2 M layers) at 83,000g for 1 h. Synaptosomes collected at the interface between 0.8 and 1.2 M sucrose layers were diluted with 3 volumes of Tris-HCl buffer (pH 7.4) and centrifugated at 105,000g for 30 min. The final pellet was slowly resuspended in ice-cold medium. Preloading and release of [2-14C]serotonin were conducted in oxygenated ice-cold standard 0.1 M sodium phosphate-buffered salt solution containing the following (in mM): NaCl–125; KCl–5; MgCl2–1.42; CaCl2–0.87; glucose–11; pH 7.4. Each assay tube contained freshly isolated synaptosomes (0.1 mg of protein per sample in a total volume of 0.2 ml) and 10 μM monoamine oxidase inhibitor iproniazide. After preincubation for 5 min (37 °C), assays were initiated by addition of [2-14C]serotonin to final concentration of 20 nM. Samples were incubated at 37 °C for 5 min and then filtered through Whatman GF/C filters soaked previously in 0.1 M sodium phosphate-buffer. Filters were rapidly washed twice with 8 ml of ice-cold standard salt solution. The [2-14C]serotonin release from preloaded synaptosomes in medium was initiated with addition of 4-aminopyridine (0.1 mM) or KCI (15 mM) to estimate the level of stimulated exocytosis or without for study of basal release. Aliquots were collected in 5 min after serotonin release and were counted for released radioactivity from synaptosomes in dioxane scintillator in a liquid scintillation counter.
Isolation of Synaptic Vesicles and Cytosolic Fraction of Synaptosomes
Crude synaptosomes were lysed by rapid resuspension in 1 mM EGTA, 10 mM Tris-HCl pH 8.1 (3 ml/g of brain tissue) and incubated at 4 °C for 60 min. The preparation was centrifuged at 20,000g for 30 min. The pellet (M1) was used to separate the PM of synaptosomes [18]. The supernatant was centrifuged at 55,000g for 60 min. Then obtained supernatant was centrifuged at 130,000g, 4 °C for 60 min to obtain the synaptic vesicle fraction (pellet) and the cytosolic fraction of synaptosomes. The synaptic vesicle pellet was suspended in 10 mM Tris-HCl, pH 7.5. The composition of the vesicle fraction was controlled by PM marker (Na+/K+-ATPase). No PM contamination was present in the purified synaptic vesicle preparation since Na+/K+-ATPase could not be detected after purification.
Isolation of Plasma Membranes
The M1 fraction was resuspended in 0.32 M sucrose, 10 mM Tris-HCl pH 7.5 and layered on a discontinuous (0.8–1.1 M) sucrose gradient. Centrifugation was carried out in the bucket-rotor at 50,000g for 120 min. Membrane fraction was collected at the interphase between 0.8 and 1.1 M sucrose and 4 volume of 10 mM Tris-HCl pH 7.5 was added. This suspension was centrifugated at 130,000g for 10 min. Finally, the pellet was resuspended in 0.32 M sucrose, 10 mM Tris-HCl pH 7.5. Purified PM were taken for the membrane fusion studies.
Detection of Membrane Fusion by Technique with Octadecyl Rhodamine Probe (R18)
The R18 assay was proposed by Keller and Hoekstra for membrane fusion monitoring and based on the relief of self-quenching of probe fluorescence [19]. The probe dilution into the target membrane as a result of its transfer and/or membrane fusion increases the fluorescence emission signal. Measurement of the fluorescence of R18 can provide a continuous and a quantitative assessment of membrane fusion. The membrane fusion was initiated by 10−5 M CaCl2 addition. Free Ca2+ concentrations medium were set by Ca2+/EGTA buffers as described by Portzehl [20].
Incorporation of R18 into Synaptic Vesicles
The solution of R18 in ethanol was added to 0.2 ml of synaptic vesicle suspension (1 mg/ml of protein) in 10 mM Tris-HCl, pH 7.5 and incubated for 5 min at 37 °C in the dark. The final concentrations of the probe and ethanol were 20 μM and 0.5 % (v/v), respectively. Unbound R18 was removed by passing through column with Sephadex G-75. The fluorescence of labeled SVs was about 80–90 % quenched. Quenching (Q) was calculated according to Q = 1 − F/Fmax, where F is the fluorescence and Fmax is the fluorescence measured after addition of detergent C12E8 (octaethyleneglycol-dodecyl ether) at final concentration of 0.1 %. R18-loaded SVs were kept on ice in dark until using. This labelled preparation was designated as R18-SVs.
Determination of Cholesterol Level
Extraction of lipids from PM was carried out by the method of Dyer [21]. Free cholesterol fraction was isolated by one-dimensional thin layer chromatography by using of benzene:ethyl acetate:ice acetic acid (85:15:1). Quantitative determination of cholesterol was performed by the method of Boyle [22] or by gas–liquid chromatography with instrument HGRC 5,300 Carlo Erba Instruments (Italy). We used 0.5 m length column with internal diameter 3 mm that was filled by shymalit with phase OV-1 1.5 %, at a constant temperature of 250 °C.
Liposomes Preparation
Liposomes were prepared from phosphatidylcholine, phosphatidylethanolamine and cardiolipine (molar ratio, 2:3:5), final lipid concentration 3 mg/ml. Lipids were dried under argon to a thin film in a glass tube followed by hydration in the medium containing 150 mM NaCl, 10 mM Tris-HCl, pH 7.5 and ultrasonication of lipid suspension. Liposomes were sized by extrusion using the Avanti Mini—extruder with 100-nm pore size filters.
All data are expressed as the mean ± SEM. Differences in means between groups were tested using the Mann–Whitney U test and considered to be statistically significant at p < 0.05.
Results
Diabetes-Induced Increase of Cholesterol Concentration in Plasma Membrane of Synaptosomes
Three groups of rats were used in experiments: the control; the diabetes-induced rats; the diabetic rats treated by gabapentin. In diabetic rats hyperglycemia was maintained throughout the study period and by the end of the 8 weeks blood glucose was four times higher compared to its initial concentration (p < 0.05, Table 1). Initial body weights of control and diabetic rats were similar (p < 0.05, Table 1). After 8 weeks of diabetes duration the body weight was 1.32 times lower than those of the age-matched diabetic rats at the beginning of experiments (p < 0.05, Table 1). Diabetic rats treated by gabapentin had no changes in body weight as compared to untreated and the blood glucose concentration was not changed too.
In diabetic rats the cholesterol level in synaptosomal PM was 12 % higher than in control (p < 0.05). After gabapentin treatment of diabetic rats the cholesterol content in PM of synaptosomes was slightly decreased.
The Fusion of SVs with Target Membranes with Different Cholesterol Content in vitro
Further, it was investigated how different content of cholesterol in artificial target membranes affects their fusion with SVs. In these experiments we used liposomes instead of synaptosomal PM. It should be noted that the negatively charged liposomes were able to fuse with SVs in buffered medium in the absence of calcium ions (Fig. 1a, column 1). When the 2 % cholesterol was added to phospholipid composition of liposomes (phosphatidylcholine: phosphatidylethanolamine: cardiolipin: cholesterol = 2: 3: 5: 0.2), a decrease in the rate of their fusion with SVs was detected (Fig. 1a, column 2). The increasing of cholesterol content in liposomes to 10 % exerts the reduction of the membrane fusion rate by approximately 50–60 % as compared to control. These results suggest that the addition of cholesterol into the phospholipid membrane of liposomes evoked rigidity which affects their ability to fuse with biological membranes.
The fusion of SVs with cholesterol enriched target membranes: a liposomes, the fluorescence intensity was measured after 1 min of experiment; b synaptosomal PM. The concentration of cholesterol in synaptosomal PM: 1. 0.67 ± 0.07 mmol/mg protein (control); 2. 0.88 ± 0.07 mmol/mg protein (after saturation by cholesterol)
To determine whether changes in cholesterol content are important for the synapse function at diabetes the cell-free system of membranes fusion was used. The synaptosomal PM were loaded with cholesterol by using the mixture of MCD-cholesterol in a molar ratio of 8:1. After the incubation of 30 min at 25 °C it was found the increase of cholesterol level by 30 %. Such cholesterol concentration had significant effect on calcium-triggered fusion of SVs with PM (Fig. 1b). The level of membrane fusion of R18 labelled SVs with cholesterol-enriched PM after 4 min of experiment was about 12 % (curve 2) while the rate of membrane fusion in the control was at 20 % (curve 1). Thus, it is noteworthy that in diabetic rats the alteration in cholesterol content of PM can affects the membrane fusion process in neurons.
The Kinetic of Fusion of Synaptosomal Membrane Structures Isolated from Diabetic Rat Brains
Synaptosomal PM of diabetic rats with enhanced level of cholesterol were used for examination of calcium-stimulated process of membrane fusion. The fusion between synaptosomal PM and SVs was monitored by R18 assay as described in section of experimental procedures. The R18 fluorescence assay validity in examination of membranes fusion in cell-free system was previously described [23].
After addition of calcium to the suspension of SVs and PM isolated from synaptosomes of control rats the rate of membrane fusion was about 25 % at 4 min (Fig. 2, curve 1). For the same time the rate of synaptic vesicle fusion with PM isolated from brain of diabetic rats was less than control and reached 15 % (Fig. 2, curve 3). Whereas, in group of rats with diabetes treated by gabapentin the rate of synaptosomal membrane structures fusion was raised to 18 % (curve 2).
These results indicate that diabetes in rats leads to weakening of membrane fusion process that is a slightly restored after gabapentin therapy.
The results of Table 1 and obtained in cell-free system (Fig. 2) allowed us to suppose the existence of correlation between the cholesterol content in PM and the rate of membrane fusion.
The Effect of Gabapentin Therapy of Diabetic Rats on Fusion Activity of Synaptosomal Cytosolic Proteins in vitro
When in the cell-free system the cytosolic proteins of synaptosomes obtained from diabetic rats after gabapentin therapy replaced on synaptosomal cytosolic proteins isolated from diabetic rat brain neurons the rate of membrane fusion was decreased (Fig. 3, curve 3).
The effect of gabapentin therapy of diabetic rats on fusion activity of synaptosomal cytosolic proteins in vitro. The time course of R18 dequenching upon fusion reaction of synaptic vesicles (SVs), plasma membrane (PM) and synaptosomal cytosolic proteins (Cyt): 1—control (SVscont + PMcont + Cytcont); 2—after gabapentin therapy (SVs gab + PM gab + Cyt gab ); 3—membrane structures after gabapentin therapy with cytosolic proteins isolated from diabetic rat brains (SVs gab + PM gab + Cyt dia ); 4—all components of cell-free system were isolated from diabetic rat brains (SVs dia + PM dia + Cyt dia ). Membrane fusion was induced by 10−5 M Ca2+
Thus, the gabapentin therapy of diabetic rats leads to restoration the function of cytosolic proteins of synaptosomes promoting the membrane fusion.
The Effect of Gabapentin on the Process of Ca2+-Stimulated Fusion of Synaptosomal Membrane Structures
To establish the direct effects of gabapentin on the membrane fusion process the cell-free system consisting of SVs and PM isolated from brain synaptosomes of control rats was utilized.
Figure 4, curve 1 presents the level of calcium-induced fusion of synaptosomal membrane structures after addition of 3 mg/ml of gabapentin and was equal to 16 %, whereas in the absence of gabapentin the fusion level was only 10 % (curve 2). Thus, in cell-free system as the model of the last step of exocytosis, the calcium-stimulated SVs fusion with synaptosomal PM was enhanced by antiepileptic drug gabapentin.
Effect of gabapentin on the Ca2+-triggered rate of synaptic vesicle fusion with synaptosomal PM. 1—after addition of 3.0 mg gabapentin to the medium; 2—control. To 1 ml of solution that contained 1 mg synaptosomal cytosolic proteins and the suspension of R18-labelled SVs (5 μg protein) were added PM (40 μg protein). The membrane fusion reaction was induced by 10−5 M calcium
Gabapentin Therapy Modulates the Serotonin Release from Synaptosomes at Diabetes
In this set of experiments, we evaluated the release of [2-14C]serotonin from isolated preloaded synaptosomes of rat brains. In according to data of Fig. 5, in diabetic rats the basal level of serotonin release from nerve terminals was elevated by 45 % as compared to those in control (bars 1).
The levels of [2-14C]serotonin release (for 5 min) from synaptosomes isolated from brains of rats from groups: control; with diabetes; with diabetes treated by gabapentin in dose 50 mg/kg b.w. every day, intraperitonealy during 4 weeks. The [2-14C]serotonin release: basal—(1), stimulated by 0.1 mM 4-aminopyridine—(2) or 15 mM KCl—(3). Iproniazide (monoamine oxidase inhibitor, 10 μM) was presented in standard assay solution to minimize serotonin catabolism. Data represent mean ± SEM. for three independent experiments which performed fourfold
In control group the serotonin release stimulated by 4-aminopirydine and KCl increased by 60 and 75 % in comparison with the basal release, respectively (bars 2 and 3). In diabetic rats the release of neurotransmitter provoked by these agents was raised by 80 and 125 %, respectively, after the subtraction of basal level of neurotransmitter release. Thus, the significant difference in serotonin release from synaptosomes between control and diabetic rats was induced by this pathology.
After gabapentin monotherapy of diabetic rats the basal level of serotonin release was less than that at diabetes and was equaled to ~116 %, in addition, the release of serotonin induced by 4-aminopyridine and KCl was also partially normalized. Our findings suggest that the chronic gabapentin treatment of diabetic rats has modulating effect on exocytosis process.
Discussion
Poorly controlled type 1 diabetes leads to severe complications, including angiopathy, nephropathy, neuropathy, especially painful diabetic neuropathy etc. [24–26]. There is strong evidence that diabetes impairs the CNS and metabolic imbalance resulting from insulin deficiency elicits measurable deficits in cognition, somatosensory, and motor-function [27]. It has been reported that animals with streptozotocin-induced diabetes have also impaired memory [28].
The potential association with diabetes has hypercholesterolemia that can be considered as the major risk factor of atherosclerosis [29]. It is well known that cholesterol is crucial for synaptic structure, function, and genesis [30]. In fact, hypercholesterolemia is present in 70 % of patients diagnosed with diabetes and 77 % who are undiagnosed [31]. Insulin-resistant patients have increased cholesterol synthesis [32]. The all brain cholesterol is synthesized in the brain and little or none of the peripheral cholesterol crosses the blood–brain barrier [33].
Our studies demonstrated that in experimental animals with streptozotocin-induced diabetes, the cholesterol content in synaptosomal PM was elevated by 12 % as compared to control (Table 1). In line with this, there are data that in STZ-treated rats, glucose, low density lipoproteins, triglycerides and total cholesterol levels in blood increased to 1.43–3.0-fold, high density lipoprotein, HbA1c and insulin sensitivity index increased to 1.1–1.23-fold compared to control [34]. Therefore this study was undertaken to find the connection between the exocytosis process at diabetes and cholesterol level in neuronal PM. However, our results are inconsistent with recently reported findings that in diabetic mice there is a reduction of gene expression of transcriptional regulator of cholesterol metabolism SREBP-2 that leads to inhibition of cholesterol synthesis in the brain and decrease cholesterol content in synaptosomal membranes [35].
It is known that the increase of cholesterol in the membranes leads to an augmentation of microviscosity and limited mobility that impair their fusion. In agreement with this, our results showed that increase of cholesterol content in the phospholipid bilayer of negatively charged liposomes as target membranes impairs their ability to fuse with SVs (Fig. 1a). Moreover, the fusion ability of cholesterol-saturated synaptosomal PM with SVs was also reduced (Fig. 1b). It should be noted, that in contrast to artificial increasing of the plasma membrane cholesterol content by MCD: cholesterol mixture, in case of liposomes it was added to their lipid composition. On the basis of these findings we convinced that in cell-free system the alteration of cholesterol content affects membrane fusion process. Earlier we investigated a specific role of cholesterol in processes of SVs fusion with various target membranes such as SVs or synaptosomal plasma membrane [36]. Methyl-β-cyclodextrin was used as a cholesterol binding agent to modulate the cholesterol content in membrane. Methyl-β-cyclodextrin depleted the cholesterol of synaptosomal plasma membrane in manner that depends on time, mediums temperature and MCD concentration. The treatment of synaptosomal PM with methyl-β-cyclodextrin (2.5 mM) decreased the level of total cholesterol by 8 % that suppressed the rate of Ca2+-dependent membrane fusion in model system. Moreover, at the partial extraction of cholesterol (−20 % of total cholesterol) from the SV membranes the intensity of calcium-induced SV fusion was decreased as compared with control.
Thus, cholesterol removal from PM by low dose of methyl-β-cyclodextrin alters the ability of membrane proteins to promote the lipid bilayer mixing [36]. Our results are consistent with the crucial and quantitatively established role of cholesterol in the mechanism of Ca2+-triggered exocytosis [6, 7, 37–39].
It should be noted that in diabetic rats the cholesterol level in synaptosomal PM was 12 % higher than in control (Table 1) and the rate of synaptic vesicle fusion with these membranes was inhibited (Fig. 2, curve 3). We suggest that the cholesterol quantity in synaptosomal PM or SVs is the crucial determinant for synaptic transmission efficiency in nerve terminals. The findings suggest that diabetes may cause physiologically drastic failure in realization of last exocytosis step—membrane fusion that can provoke the disturbances in motor activity and sensory-motor function. Hence, the patients with this disease have an increased risk of cognitive decline compared with healthy individuals.
An important question which this study does not discussed is how therapy with statins (cholesterol biosynthesis inhibitors) might alter brain function in patients with diabetes. Some studies have reported relatively acute cognitive decline and memory loss in individuals after treatment by statins, which improve after discontinuation of the drug [40].
The treatment of painful diabetic peripheral neuropathy is difficult and limited by the range of its efficiency. The drug gabapentin significantly reduced hyperalgesia in rats with streptozotocin-induced diabetes [41]. Gabapentin-treated patients had substantially lower mean daily pain scores and essential improvement of all secondary efficacy parameters, which included mean sleep interference [42]. Preliminary studies have shown that the anticonvulsant gabapentin is beneficial in the management of these states, but it remains an unlicensed indication.
After gabapentin therapy of diabetic rats the cholesterol content in PM of synaptosomes was slightly decreased (Table 1). In this case, the rate of fusion of synaptosomal membrane structures approaches to control (Fig. 2, curve 2). It is not excluded, that increasing of kinetic of membrane fusion may be a consequence of the decreasing of cholesterol level in neuronal PM. Well known that SNAREs proteins, responsible for realization and regulation of the process of membrane fusion are localized in cholesterol-enriched lipid microdomains of the membrane bilayers [7]. The current study may be in line with another important assumption that diabetes induces significant changes in content of the some synaptic membrane proteins which participate in forming of fusion-driving protein complex SNARE. In hippocampal cultures were detected the changes of content such proteins as SNAP-25, synaptotagmin-1 and VGluT-1 induces by long-term exposure to high glucose [43]. Moreover, it was found that synaptophysin/synaptobrevin interaction critically depends on the cholesterol content [44]. Based on presented data we suppose that the disturbances of cholesterol concentration in synaptosomal membrane structures lead to a change in conformation and functioning of membrane proteins, including SNARE. Thus, the gabapentin therapy of diabetic rats may be realized through the changes in cholesterol level in membrane structures of synaptosomes which in turn affects on fusion ability of proteins.
We have found that the Ca2+-triggered fusion of SVs with neuronal PM in vitro requires the presence of elements of synaptosomal cytosolic fraction [45]. It is known that the cytosolic protein Munc13-1 is essential for secretory vesicle priming and has a crucial role for both neurotransmitters and insulin exocytosis [46]. Thus, the impairments of function of synaptosomal cytosolic proteins may be an important factor contributing to the development of diabetic neuropathy.
Experimental data presented in Fig. 3, curve 3 indicate that gabapentin therapy of diabetic rats leads to partial restoration of the fusogenic function of cytosolic proteins of synaptosomes as compared to those of diabetic rats. Consequently, the changes of the last step of exocytosis induced by diabetes may be associated not only with increased cholesterol content of synaptosomal PM that modifies the function of membrane-bounded proteins but also with diabetes-induced impairments of synaptosomal cytosolic proteins (Fig. 3, curve 4).
Previously we have shown the modulatory action of anticonvulsive agent gabapentin on calcium-induced fusion between SVs. Despite the fact, that gabapentin has hydrophobic nature, this drug did not change the intensity of calcium dependent fusion between proteolytically treated SVs or the same SVs with liposomes. Our data shown, that gabapentin addition also did not increase the calcium-dependent fusion of negatively charged liposomes [47]. The direct addition of antiepileptic drug gabapentin into model system, consisting SVs and synaptosomal PM, enhanced the rate of membrane fusion (Fig. 4). Therefore, the action of this antiepileptic drug may be realized via its interaction with membrane fusion proteins but not with a lipid bilayer.
The possible mechanism of anticonvulsant gabapentin action is binding to α2δ calcium channel subunits [48] on the presynaptic neurones that induce the inhibition of neuronal calcium influx [49] and activation of glutamate dehydrogenase [50]. Although gabapentin is rapidly absorbed, readily crosses the blood–brain barrier and is orally active in several animal models of epilepsy, it neither binds to GABAA or GABAB receptors nor metabolized to GABA [51].
As can be seen in Fig. 5, the basal release of serotonin from synaptosomes rises at diabetes that may provoke the depletion of pool of SVs. Moreover, serotonin release induced by plasma membrane depolarization is more profound elevated at diabetes. Thus, the diabetes-induced increase of serotonin release may reflect the complex set of changes in protein functions of nervous endings [52].
Recently, it was found that diabetes alters the content of exocytotic proteins in hippocampal nerve terminals and changes the neurotransmitter release [43]. Taken together, these data provide a relationship between STZ-induced diabetes, altered synapse function in brain and chronic neurodegenerative disorders. Moreover, all these findings are in line with our previous studies demonstrating that development of brain cells nuclea dysfunction in STZ-induced diabetic rats, renal hypertrophy and multiple manifestations of peripheral neuropathy in diabetic Akita mice are associated with overactivation of the poly(ADP-ribose)polymerase-1 (PARP-1), main enzyme of the poly-ADP-ribosylation processes [53, 54]. It is known that the main role of these processes is to detect and signal single-strand DNA breaks to the enzymatic machinery involved in their repair. However PARP-1 overactivation leads to ATP depletion in cells that can induce lysis and cells death.
It should be noted, that gabapentin treatment of diabetic rats leads to normalization of serotonin release (both basal and stimulated, Fig. 5) and also to restoring of membrane fusion of SVs with PM of synaptosomes (Fig. 2, curve 2). Our data imply that gabapentin acts at last step of exocytosis, i.e., membrane fusion that was confirmed by the decrease of depolarisation-evoked release of serotonin from nerve terminals at diabetes. Thus, diabetes-induced impairments of the exocytotic process, which have the pathological significance, can be attenuated by gabapentin therapy.
It was shown that gabapentin administration was associated with an average increase of prominent inhibitory neurotransmitter γ-aminobutyric acid (GABA) concentration in brain by 55.7 % [55]. In addition, gabapentin increases GABA turnover in various brain regions [56] and influences on GABA which also is present in high concentrations in β-cells of islets of Langerhans and co-released with insulin [57, 58]. It was suggested that autocrine GABA, via activation of GABA(A)Rs, depolarizes the pancreatic β-cells and enhances insulin secretion.
An opposite view was presented by Sorensen with co-authors, who demonstrate the presence of GABAergic nerve cell bodies at the periphery of islets with numerous GABA-containing processes extending into the islet mantle [59]. Their observations provide new insight into the complex nature of GABAergic neurons and GABA of β-cells in regulation of islet function. In addition, GABA through GABA receptors in brain stem has a regulatory role during active regeneration of pancreas of pancreatectomised rats which could have immense clinical significance in the treatment of diabetes [60].
It can be assumed that gabapentin therapy of diabetic rats leads to the increased GABA not only in the brain but also in GABAergic nerve cell bodies of islets. Thereby, the increased GABA concentration in islet may improve insulin secretion. Moreover, in diabetic brain, insulin is responsible for the expression of genes of SREBP-2 leading to altered content of the cholesterol [35].
In the context of our reflection we suppose that in the islets of Langerhans the gabapentin-induced elevation of GABA stimulates the insulin secretion, which in turn, regulates the level of cholesterol in brain neurons. These results can be important for understanding of mechanisms of gabapentin action, which may be useful in the treatment of diabetic neuropathies or to slow their progression.
The study was involved for participation in Cedars Sinai Medical Center’s International Research and Innovation Management Program, the Association for Regional Cooperation in the Fields of Health, Science and Technology (RECOOP HST Association) and Cedars—Sinai Medical Center–RECOOP Research Centers (CRRC).
References
Biessels GJ, Deary IJ, Ryan CM (2008) Cognition and diabetes: a lifespan perspective. Lancet Neurol 7:184–190
Cukierman T, Gerstein HC, Williamson JD (2005) Cognitive decline and dementia in diabetes—systematic overview of prospective observational studies. Diabetologia 48:2460–2469
Südhof TC (1995) The synaptic vesicle cycle: a cascade of protein–protein interactions. Nature 375:645–653
Lin RC, Scheller RH (2000) Mechanisms of synaptic vesicle exocytosis. Annu Rev Cell Dev Biol 16:19–49
Söllner T, Whiteheart SW, Brunner M (1993) SNAP receptors implicated in vesicle targeting and fusion. Nature 362:318–324
Churchward MA, Coorssen JR (2009) Cholesterol, regulated exocytosis and the physiological fusion machine. Biochem J 423:1–14
Rituper B, Flašker A, Guček A, Chowdhury H, Zorec R (2012) Cholesterol and regulated exocytosis: a requirement for unitary exocytotic events. Cell Calcium 52:250–258
Borisova T, Sivko R, Borysov A, Krisanova N (2010) Diverse presynaptic mechanisms underlying methyl-beta-cyclodextrin-mediated changes in glutamate transport. Cell Mol Neurobiol 30:1013–1023
Ikonen E (2008) Cellular cholesterol trafficking and compartmentalization. Nat Rev Mol Cell Biol 9:125–138
Lange Y (1991) Disposition of intracellular cholesterol in human fibroblasts. J Lipid Res 32:329–339
Takamori S, Holt M, Stenius K, Lemke EA, Gronborg M, Riedel D et al (2006) Molecular anatomy of a trafficking organelle. Cell 127:831–846
Taverna E, Saba E, Rowe J, Francolini M, Clementi F, Rosa P (2004) Role of lipid microdomains in P/Q type calcium channel (Cav2.1) clustering and function in presynaptic membranes. J Biol Chem 279:5127–5134
Chamberlain LH, Burgoyne RD, Gould GW (2001) SNARE proteins are highly enriched in lipid rafts in PC12 cells: implications for the spatial control of exocytosis. Proc Natl Acad Sci 98:5619–5624
Lang T, Bruns D, Wenzel D, Riedel D, Holroyd P, Thiele C et al (2001) SNAREs are concentrated in cholesterol-dependent clusters that define docking and fusion sites for exocytosis. EMBO J 20:2202–2213
Ya Terletskaya, Trikash I (1998) Calcium-triggered fusion of synaptic vesicles and synaptosomal plasma membranes in vitro. Neurophysiology 30:291–293
Honarmand A, Safavi M, Zare M (2011) Gabapentin: an update of its pharmacological properties and therapeutic use in epilepsy. J Res Med Sci 16:1062–1069
Kong VKF, Irwin MG (2007) Gabapentin: a multimodal perioperative drug? Br J Anaesth 99:775–786
De Lores Arnaiz GR, Alverci M, de Robertis E (1967) Ultrastructural and enzymic studies of cholinergic and noncholinergic synaptic membranes isolated from brain cortex. J Neurochem 14:215–225
Hoekstra D, De Boer T, Klappe K, Wilschut J (1984) Fluorescence method for measuring the kinetics of fusion between biological membranes. Biochemistry 23:5675–5681
Portzehl H, Caldwell PC, Rueegg JC (1964) The dependence of contraction and relaxation of muscle fibres from the crab Maia squinado on the internal concentration of free calcium ions. Biochim Biophys Acta 79:581–591
Bligh EG, Dyer WJ (1959) A rapid method of total lipid extraction and purification. Can J Biochem Physiol 37:911–917
Zlatkis A, Zak B, Boyle AJ (1953) A new method for the direct determination of serum cholesterol. J Lab Clin Med 41:486–492
Trikash I, Gumenyuk V, Lishko V (2010) The fusion of synaptic vesicle membranes studied by lipid mixing: the R18 fluorescence assay validity. Chem Phys Lipids 163:778–786
Backonja M, Glanzman RL (2003) Gabapentin dosing for neuropathic pain: evidence from randomized, placebo-controlled clinical trials. Clin Ther 25:81–104
Jensen PG, Larson JR (2001) Management of painful diabetic neuropathy. Drugs Aging 18:737–749
Sima AA (2006) Pathological mechanisms involved in diabetic neuropathy: can we slow the process? Curr Opin Investig Drugs 7:324–337
Emerick AJ, Richards MP, Kartje GL, Neafsey EJ, Stubbs EB Jr (2005) Experimental diabetes attenuates cerebral cortical-evoked forelimb motor responses. Diabetes 54:2764–2771
Biessels GJ, Cristino NA, Rutten GJ, Hamers FP, Erkelens DW, Gispen WH (1999) Neurophysiological changes in the central and peripheral nervous system of streptozotocin-diabetic rats. Course of development and effects of insulin treatment. Brain 122:757–768
Homma Y (2004) Predictors of atherosclerosis. J Atheroscler Thromb 11:265–270
Mauch DH, Nagler K, Schumacher S, Goritz C, Muller EC, Otto A, Pfrieger FW (2001) CNS synaptogenesis promoted by glia-derived cholesterol. Science 294:1354–1357
Yaffe K (2007) Metabolic syndrome and cognitive decline. Curr Alzheimer Res 4:123–126
Pihiajamaki J, Gylling H, Miettinen TA, Laakso M (2004) Insulin resistance is associated with increased cholesterol synthesis and decreased cholesterol absorption in normoglycemic men. J Lipid Res 45:507–512
Dehouck B, Fenart L, Dehouck MP, Pierce A, Torpier G, Cecchelli R (1997) A new function for the LDL receptor: transcytosis of LDL across the blood–brain barrier. J Cell Biol 138:877–889
Yang H, Fan S, Song D, Wang Z, Ma S, Li S et al (2013) Long-term streptozotocin-induced diabetes in rats leads to severe damage of brain blood vessels and neurons via enhanced oxidative stress. Mol Med Rep 7:431–440
Suzuki R, Lee K, Jing E, Biddinger SB, McDonald JG, Montine TJ et al (2010) Diabetes and insulin in regulation of brain cholesterol metabolism. Cell Metab 12:567–579
Humeniuk VP, Trykash IO (2011) Exocytotic steps in cell-free system after cholesterol deprivation in synaptosomal plasma membranes and synaptic vesicles. Ukr Biokhim Zh 83:53–64
Ormerod KG, Rogasevskaia TP, Coorssen JR, Mercier AJ (2012) Cholesterol-independent effects of methyl-beta-cyclodextrin on chemical synapses. PLoS One 7:e36395
Krisanova N, Sivko R, Kasatkina L, Borisova T (2012) Neuroprotection by lowering cholesterol: a decrease in membrane cholesterol content reduces transporter-mediated glutamate release from brain nerve terminals. Biochim Biophys Acta 1822:1553–1561
Borisova T, Krisanova N, Sivko R, Borysov A (2010) Cholesterol depletion attenuates tonic release but increases the ambient level of glutamate in rat brain synaptosomes. Neurochem Int 56:466–478
Evans MA, Golomb BA (2009) Statin-associated adverse cognitive effects: survey results from 171 patients. Pharmacotherapy 29:800–811
Backonja M, Beydoun A, Edwards KR, Schwartz SL, Fonseca V, Hes M et al (1998) Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: a randomized controlled trial. JAMA 280:1831–1836
Vinik A (2005) Clinical review: use of antiepileptic drugs in the treatment of chronic painful diabetic neuropathy. J Clin Endocrinol Metab 90:4936–4945
Gaspar JM, Castilho Á, Baptista FI, Liberal J, Ambrósio AF (2010) Long-term exposure to high glucose induces changes in the content and distribution of some exocytotic proteins in cultured hippocampal neurons. Neuroscience 171:981–992
Mitter D, Reisinger C, Hinz B, Hollmann S, Yelamanchili SV, Treiber-Held S, Ohm TG, Herrmann A, Ahnert-Hilger G (2003) The synaptophysin/synaptobrevin interaction critically depends on the cholesterol content. J Neurochem 84:35–42
Trikash IO, Kolchinskaya LI (2006) Fusion of synaptic vesicles and plasma membrane in the presense of synaptosomal soluble proteins. Neurochem Int 49:270–275
Juranek JK, Geddis MS, Kothary P, Hays A, Schmidt AM, Brannagan TH 3rd (2014) Reduced expression of Munc13-1 in human and porcine diabetic peripheral nerve. Acta Histochem 116:106–111
Gumenyuk VP, Volinets GP, Kuchmerovskaya TM, Trikash IO (2009) Effects of antiepileptic agents on homotypic fusion of synaptic vesicles. Neurophysiology 41:395–403
Gee NS, Brown JP, Dissanayake VUK, Offord J, Thurlow R, Woodruff GN (1996) The novel anticonvulsant drug, gabapentin (neurontin), binds to the α2δ subunit of a calcium channel. J Biol Chem 271:5768–5776
Fink K, Meder W, Dooley DJ, Gothert M (2000) Inhibition of neuronal Ca2+ influx by gabapentin and subsequent reduction of neurotransmitter release from rat neocortical slices. Br J Pharmacol 130:900–906
Cho SW, Cho EH, Choi SY (1998) Activation of two types of brain glutamate dehydrogenase isoproteins by gabapentin. FEBS Lett 426:196–200
Kammerer M, Rassner MP, Freiman TM, Feuerstein TJ (2011) Effects of antiepileptic drugs on GABA release from rat and human neocortical synaptosomes. Naunyn Schmiedebergs Arch Pharmacol 384:47–57
Kuchmerovska T, Shymanskyy I, Chlopicki S, Klimenko A (2010) 1-Methylnicotinamide (MNA) in prevention of diabetes-associated brain disorders. Neurochem Int 56:221–228
Kuchmerovska T, Shymanskyy I, Donchenko G, Pakirbaieva L, Klimenko A (2004) Poly-ADP-ribosylation enhancement in brain cells nuclei is associated with diabetic neuropathy. J Diabetes Complicat 18:198–204
Drel VR, Pacher P, Stavniichuk R, Xu W, Zhang J, Kuchmerovska TM, Slusher B, Obrosova IG (2011) Poly(ADP-ribose)polymerase inhibition counteracts renal hypertrophy and multiple manifestations of peripheral neuropathy in diabetic Akita mice. Int J Mol Med 28:629–635
Cai K, Nanga RP, Lamprou L, Schinstine C, Elliott M, Hariharan H et al (2012) The impact of gabapentin administration on brain GABA and glutamate concentrations: a 7T 1H-MRS study. Neuropsychopharmacology 37:2764–2771
Loscher W, Honack D, Taylor CP (1991) Gabapentin increases aminooxyacetic acid-induced GABA accumulation in several regions of rat brain. Neurosci Lett 128:150–154
Bansal P, Wang S, Liu S, Xiang YY, Lu WY, Wang Q (2011) GABA coordinates with insulin in regulating secretory function in pancreatic INS-1 β-cells. PLoS One 6:e26225
Braun M, Ramracheya R, Bengtsson M, Clark A, Walker JN et al (2010) Gamma-aminobutyric acid (GABA) is an autocrine excitatory transmitter in human pancreatic beta-cells. Diabetes 59:1694–1701
Sorenson RL, Garry DG, Brelje TC (1991) Structural and functional considerations of GABA in islets of Langerhans. Beta-cells and nerves. Diabetes 40:1365–1374
Balarama Kaimal S, Gireesh G, Paulose CS (2007) Decreased GABAA receptor function in the brain stem during pancreatic regeneration in rats. Neurochem Res 32:1813–1822
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trikash, I., Gumenyuk, V. & Kuchmerovska, T. Diabetes-Induced Impairments of the Exocytosis Process and the Effect of Gabapentin: The Link with Cholesterol Level in Neuronal Plasma Membranes. Neurochem Res 40, 723–732 (2015). https://doi.org/10.1007/s11064-015-1520-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-015-1520-6