Abstract
The hypoxia-inducible factor (HIF)-mediated signaling pathway is an adaptive and protective mechanism that is triggered by hypoxia, ischemia, and other pathophysiological conditions. The expression of HIF-1α and downstream genes, some of which are pro-apoptotic whereas others are pro-survival, is up-regulated in ischemic stroke. Interestingly, however, the effects of HIF-1α activation are different in the early and late stages of acute cerebral ischemia, and these differences may depend on the duration and severity of hypoxia. Therefore, in the present study, we investigated the effect of HIF-1α activation in chronic cerebral hypoperfusion, which plays an important role in the development of dementia. Permanent bilateral common carotid artery occlusion (2VO) was used to induce chronic global cerebral hypoperfusion in rats. The expression of HIF-1α protein and the transcription of downstream genes were measured at different time points, including 0 h, 12 h, 24 h, 3 days, 7 days, 14 days, 28 days, 42 days, and 56 days after 2VO. HIF-1α increased as early as 12 h after the occlusion and remained high for at least 56 days. Interestingly, mRNA levels of both pro-apoptotic (Bcl-2/adenovirus EIB 19 kDa-interacting protein 3, NADPH oxidase activator 1, and NIP3-like protein X) and pro-survival (vascular endothelial growth factor, glucose transporter-1) genes were up-regulated at the early stage after 2VO, followed by a gradual decline to baseline/control levels. Thus, HIF-1α increased consistently during chronic cerebral hypoperfusion, whereas both pro-apoptotic and pro-survival downstream genes were up-regulated only early after 2VO. This mismatch in gene expression may contribute to the lack of a protective effect of highly expressed HIF-1α during the chronic stage of cerebral hypoperfusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypoxia-inducible factor 1 (HIF-1) is a pivotal regulator of gene expression in response to hypoxia. HIF-1 target genes include pro-survival genes involved in angiogenesis, energy metabolism, erythropoiesis, vasomotor control, and cell proliferation, such as vascular endothelial growth factor (VEGF), glucose transporter-1 (GLUT-1), and erythropoietin (EPO) [1, 2]. Paradoxically, HIF-1α is also involved in hypoxia-dependent inflammation, apoptosis, and cellular stress. Some of the pro-death genes that are involved include Bcl-2/adenovirus EIB 19 kDa-interacting protein 3 (BNIP-3), NADPH oxidase activator 1 (Noxa), NIP3-like protein X (NIX), and others [3–5]. Consequently, despite the undisputed role of HIF-1 in regulating oxygen homeostasis, both neuroprotective and detrimental effects of HIF-1 have been observed in various acute ischemia models [6]. Some research has indicated a role for HIF-1α in mediating both pro-death and pro-survival responses that may depend on the duration of the ischemia [7] and the types of pathological stimuli [8]. Nevertheless, whether elevated HIF levels are detrimental or protective in the setting of cerebral ischemia and what role the time course of HIF activation and downstream gene effects play are unclear.
Chronic cerebral hypoperfusion (CCH), a preclinical condition of mild cognitive impairment and the prevalent pathophysiological state in patients with dementia [9], is a less severe form of ischemia that develops more slowly than an acute ischemic stroke [10, 11]. A number of studies have identified cerebral hypoperfusion in brain regions associated with cognitive functions both in Alzheimer’s disease and in vascular dementia patients, and have supported the notion of a reduced blood supply to brain as a decisive factor in the pathogenesis of cognitive impairment [12, 13]. Therefore, HIF-induced long-term effects may be important factors in the development of CCH, which may provide a potential target for dementia therapy.
In this study, we examined HIF-induced effects during CCH. Permanent bilateral common carotid artery occlusion (2VO) was used to induce the rat model of chronic global cerebral hypoperfusion. The expression of HIF-1α and the effects on transcription of downstream pro-survival and pro-apoptotic genes were measured for 8 weeks after the vessels were ligated.
Materials and Methods
Animals
120 Male Wistar rats (weight 220–250 g, 7 weeks old, obtained from Vital River Laboratory Animal Technology Co. Ltd., Beijing, China) were group-housed in polypropylene cages at 22 ± 2 °C with 55 ± 5 % humidity and maintained on a 12-h dark/light artificial cycle (lights on at 7:00 a.m.) with ad libitum access to water and food. All animal procedures were performed according to protocols approved by the National Institutes of Health Guide for the Care and Use of Laboratory Animals, and the Animal Ethics Committee of the Medical School of Wuhan University approved their use.
Model Establishment and Experimental Design
Chronic cerebral hypoperfusion was induced with 2VO [14]. Food and water were withheld for 1 day prior to surgery. Rats were anesthetized with 10 % chloral hydrate (300 mg/kg, i.p.). The bilateral common carotid arteries of rats were exposed via a midline ventral incision, carefully separated from the vagal nerves, and permanently ligated with silk suture. Rats that underwent a sham operation were treated in a similar manner, except that the common carotid arteries were not ligated. During the operation, body temperature was maintained at 37.5 ± 0.5 °C. After surgery, the wounds were sutured, and rats were allowed to recover from anesthesia before being returned to their cages.
The levels of various hypoxia-induced mediators were detected with quantitative real-time PCR (qPCR) and Western blotting at different time points, including 0 h (before 2VO, without occlusion), 12 h, 24 h, 3 days, 7 days, 14 days, 28 days, 42 days, and 56 days after 2VO. Samples for detection were obtained from the hippocampus of rats after they had been anesthetized with chloral hydrate. The tissue was frozen immediately in liquid nitrogen and stored at −80 °C until Western blotting and qPCR.
qPCR
Total RNA was extracted from individual hippocampi using the Trizol method (Invitrogen). RNA (4 μg) was reverse transcribed into cDNA using a First Strand cDNA Synthesis kit (TOYOBO, Japan). cDNA (0.2 μg) was amplified with a qPCR kit using the gene-specific primers listed in Table 1. The reaction was performed using THUNDERBIRD SYBR qPCR Mix (TOYOBO, Japan). The PCR cycles were as follows: initial denaturation (50 °C, 2 min; 95 °C, 2 min), 40 cycles (95 °C, 15 s; annealing at 58 °C, 15 s; extension at 72 °C, 45 s), and a final extension (72 °C, 10 min). Specific amplification was confirmed with melting curve analysis. All reactions were performed in triplicate using β-actin as an endogenous control. The changes in mRNAs were expressed as fold-change using the formula (\(2^{{ - \Updelta \Updelta C_{\text{t}} }}\)).
Western Blotting
Nuclear proteins were extracted from the hippocampus of rats for immunoblotting analysis using a kit from the Keygen Institute of Biotechnology (Keygen, Nanjing, China). Protein samples (40 μg) were fractionated with 10 % SDS-PAGE, transferred to 0.45-μm PVDF membranes at 200 mA for 1 h, and stained with Ponceau red to confirm equal loading. The blots were blocked with 5 % nonfat milk in Tris-buffered saline containing 0.1 % Tween 20 (TBST) at room temperature for 1 h. Membranes were then incubated with primary antibodies (anti-HIF-1α: 1:1,000 in TBST, BD Transduction Laboratories, San Diego, CA, USA; anti-β-actin: 1:2,000 in TBST, Santa Cruz, Dallas, TX, USA) at 4 °C overnight, washed three times with TBST, and incubated with peroxidase-conjugated secondary antibodies (anti-mouse: 1:3,000 in TBST, KPL, MD, USA) for 30 min. Membranes were washed three times with TBST, and labeled proteins were visualized with chemiluminescence (SuperSignal West Pico, Pierce, Rockford, IL, USA). Semiquantification of immunoreactive bands on X-ray film was performed with optical density analysis (HPIAS 2000, Tongji Qianping Company, Wuhan, China). Densities were normalized to β-actin.
Statistical Analysis
Statistical analysis was performed with GraphPad Prism 5.0 software. Data are the mean ± SEM. The Western blot results were analyzed with one-way ANOVA with Dunnett’s test. PCR results were analyzed with two-way ANOVA followed by Bonferroni post-tests. p < 0.05 was considered statistically significant.
Results
Accumulation of HIF-1α During CCH
To determine whether HIF-1α accumulated in response to chronic global hypoperfusion, the expression of HIF-1α in the hippocampus at different time points after 2VO was examined with Western blotting. Chronic cerebral hypoperfusion induced by 2VO triggered a steady increase in HIF-1α levels in the hippocampus (Fig. 1). Protein levels began to increase as early as 12 h after the operation (p > 0.05; Fig. 1b), were increased by more than 10-fold by 28 days, and remained high for at least 56 days (p < 0.01; Fig. 1b).
Western blot analysis of HIF-1α expression in rat hippocampus at different times (0 h–56 days) after 2VO operation. a Representative Western blotting result from hippocampal nucleoprotein extracts probed with the indicated antibodies. b Quantitation of HIF-1α protein expression. Each bar represents the mean relative optical density ± SEM (n = 6). **p < 0.01 as compared with 0 h
Transcription of HIF-1–Mediated Pro-Survival Genes During CCH
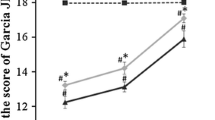
Vascular endothelial growth factor, GLUT-1, and EPO are genes with established roles in neuronal survival and/or vascular biology, and their expression is regulated by HIF-1. qPCR analysis showed that mRNA levels of VEGF and GLUT-1, but not EPO, were significantly increased in the hippocampus in the early stage after 2VO (Fig. 2). VEGF mRNA peaked at ~ 24 h–3 days (p < 0.01; Fig. 2a) and then declined slowly to normal levels. Similarly, the expression of GLUT-1 increased significantly as early as 12–24 h after 2VO (p < 0.01) and remained higher in the first 7 days as compared with sham-operated rats (p < 0.01, p < 0.05; Fig. 2b). In contrast, the expression of EPO was a little higher than that in sham rats, but the differences were not statistically significant over the entire time period that we examined (p > 0.05; Fig. 2c).
HIF-1–dependent expression of pro-survival genes in rat hippocampus during CCH. qPCR analysis of the indicated genes (a VEGF; b GLUT-1; c EPO) at different times after 2VO or sham operation. Values represent the mean relative expression ± SEM (n = 5). *p < 0.05, **p < 0.01 as compared with sham-operated rats
The Transcription of HIF-1–Mediated Pro-Apoptotic Genes During CCH
Similar to pro-survival genes, the expression of HIF-1–regulated pro-death genes (BNIP-3, NIX, Noxa) tended to increase in the early stage after 2VO (Fig. 3). The induction of NIX and Noxa at the mRNA level peaked at 3 days after the vascular ligation (p < 0.05, p < 0.01; Fig. 3b, c) and then decreased to non-hypoperfused levels. The expression of BNIP showed similar increasing trend in the first three days, but without statistical significance (p > 0.05, Fig. 3a).
HIF-1–dependent expression of pro-apoptotic genes in rat hippocampus during CCH. qPCR analysis of the indicated genes (a BNIP-3; b NIX; c Noxa) at different times after 2VO or sham operation. Values represent the mean relative expression ± SEM (n = 5). *p < 0.05, **p < 0.01 as compared with sham-operated rats
Discussion
Increasing number of studies indicate that cerebral hypoperfusion is one of the initial conditions that are critical to the development of cognitive dysfunction[15]. Cerebral hypoperfusion can cause disorders in neuronal electrical activity, inhibition of protein synthesis, apoptosis, and oxidative stress, which may be pathophysiological mechanisms that contribute to cognitive impairment [16]. Despite the detrimental effects of hypoperfusion, the decline in cellular oxygen levels does, however, induce compensatory or endogenous adaptive and regenerative mechanisms to defend against hypoperfusion injury and to allow recovery of brain function [16, 17]. Regulation of the endogenous adaptive processes involves the concerted activation of various transcription factors, including HIF. As our data show, chronic global cerebral hypoperfusion triggered long-lasting accumulation of HIF-1α protein in rat hippocampus, which is a brain region that is susceptible to ischemia and is involved in cognition.
HIF-1 is a dimeric transcriptional complex consisting of HIF-1a and HIF-1b subunits. HIF-1 activity is controlled by the availability and activity of the HIF-1a subunit. Under normoxic conditions, HIF-1a is hydroxylated by oxygen-dependent proline hydroxylases (PHDs) and is rapidly degraded. Under hypoxic-ischemic conditions in which oxygen is limited, PHDs are less active, and, thus, the HIF-1 complex becomes stabilized and accumulates in the cytosol. The HIF-1 complex then translocates to the nucleus, resulting in transcription of HIF-1 target genes such as VEGF, EPO, GLUT-1, etc., which promote neuronal adaptation for survival under hypoxic conditions [2]. These downstream genes are responsible for protection from cerebral ischemia/hypoxic injury [1]. The expression of VEGF and EPO activates VEGF receptors and EPO receptors, respectively, which promote vasodilation and angiogenesis, inhibit excitotoxicity, and protect neural cells from apoptosis [18, 19]. GLUT-1 is highly expressed in brain endothelial cells and is critical for glucose entry into the CNS. GLUT-1 enhances the concentration of glucose and thereby also promotes neuroprotection [20].
HIF-1a protein accumulates and there is a consequent up-regulation of HIF-1 target genes (VEGF, EPO) after cerebral ischemia [21, 22]. Chavez and LaManna showed that HIF-1a accumulation starts as early as 1 h after restoration of blood flow and persists up to 7 days after transient global ischemia [23]. Neuron-specific knockdown of HIF-1 aggravates brain damage after a 30-min middle cerebral artery occlusion (MCAO) and reduces the survival rate of MCAO mice [24]. Inhibiting HIF-1 PHDs to trigger the accumulation of HIF-1a protects the brain from cerebral stroke damage [25, 26]. Thus, studying HIF-1 appears to be important for the development of novel therapeutic interventions in ischemia-related neurological disease.
As CCH is less severe and more slowly developing global ischemia, HIF-1A may play a more important role in the pathological process. Unfortunately, how it works is still poorly understood. In the present study, we revealed that similar to acute ischemia, after 2VO, HIF-1α levels increased initially and remained elevated during hypoperfusion for at least 8 weeks. The expression of the HIF-regulated genes VEGF and GLUT-1 was higher in the first 7 days as compared with expression in sham-operated rats. The expression of EPO was slightly higher than in the sham group.
Previous researchers have noted an increased capillary diameter, neovascularization, and enhanced VEGF immunohistochemistry in the cortex and hippocampus in models of CCH, as well as enlargement of the arteries at the base of the brain, and these events coincide with the upregulation of HIF-mediated genes [27, 28]. In addition, cerebral blood flow values gradually begin to recover at 1 week and normalize over a period of months in the 2VO model, even though the occlusion is permanent [17, 29]. Under these conditions, compensatory or adaptive mechanisms are turned on. Thus, we hypothesize that the HIF transcription complex may be involved in endogenous protective mechanisms during CCH by activating the genetic program of hypoxic adaptation.
HIF-1 has also been shown to mediate pro-death responses, although its probable role in triggering adaptive responses has been detected. HIF governs the expression of several pro-apoptotic genes including BNIP-3, NIX, and Noxa [30], which cause mitochondrial dysfunction leading to cell injury and death [3–5]. The expression of HIF-1–regulated pro-death BH3-only family members such as BNIP-3 is increased after cerebral ischemia [31, 32]. Brain-specific knockout of HIF-1α may be neuroprotective after acute global ischemic injury for 75 min [33]. Likewise, our data revealed significant increases in NIX and Noxa transcription on the third day after 2VO. Consequently, HIF-1α appears to mediate both pro-death and pro-survival responses during CCH.
Which of the HIF-1a–related functions is most dominant may depend on the severity or duration of the ischemic or hypoxic insult [7, 8] as well as the cell type in which it is induced [34]. In a rat model of focal ischemia, selective inhibition of HIF-1a during early, but not late, time points was neuroprotective [35]. In addition, the different effects of transient focal ischemia for 30 min [24] and acute global ischemia for 75 min as described above [32] support the dual characteristics of HIF.
Considering the increase in expression of both pro-survival and pro-apoptosis genes during early stages of CCH, whether HIF-mediated pro-survival responses are dominant over deleterious effects or vice versa remains unknown. Our results suggest that HIF-regulated pro-survival genes changed more than pro-death genes. The tendency of an increase in pro-survival genes was sustained for at least 1 week, whereas the increase in pro-apoptosis genes was relatively temporary. We will next perform research in which the accumulation of HIF-1 is blocked or promoted to explore its exact function.
It is worth mentioning that, mismatching with the expression of HIF-1α, the level of downstream genes display no significant difference between 2VO and sham operation rats at the late stage of hypoperfusion, which might attribute to the lack of sufficient protective effect of highly expressed HIF-1α level at the chronic stage.
References
Correia SC, Moreira PI (2010) Hypoxia-inducible factor 1: a new hope to counteract neurodegeneration? J Neurochem 112:1–12
Benarroch EE (2009) Hypoxia-induced mediators and neurologic disease. Neurology 73:560–565
Althaus J, Bernaudin M, Petit E, Toutain J, Touzani O, Rami A (2006) Expression of the gene encoding the pro-apoptotic BNIP3 protein and stimulation of hypoxia-inducible factor-1alpha (HIF-1alpha) protein following focal cerebral ischemia in rats. Neurochem Int 48:687–695
Sowter HM, Ratcliffe PJ, Watson P, Greenberg AH, Harris A (2001) HIF-1-dependent regulation of hypoxic induction of the cell death factors BNIP3 and NIX in human tumors. Cancer Res 61:6669–6673
Kim JY, Ahn HJ, Ryu JH, Suk K, Park JH (2004) BH3-only protein Noxa is a mediator of hypoxic cell death induced by hypoxia-inducible factor 1alpha. J Exp Med 199:113–124
Karuppagounder SS, Ratan RR (2012) Hypoxia-inducible factor prolyl hydroxylase inhibition: robust new target or another big bust for stroke therapeutics? J Cereb Blood Flow Metab 32:1347–1361
Halterman MW, Miller CC, Federoff HJ (1999) Hypoxia-inducible factor-1alpha mediates hypoxia-induced delayed neuronal death that involves p53. J Neurosci 19:6818–6824
Aminova LR, Chavez JC, Lee J, Ryu H, Kung A, LaManna JC, Ratan RR (2005) Prosurvival and prodeath effects of hypoxia-inducible factor-1alpha stabilization in a murine hippocampal cell line. J Biol Chem 280:3996–4003
Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, Launer LJ, Laurent S, Lopez OL, Nyenhuis D, Petersen RC, Schneider JA, Tzourio C, Arnett DK, Bennett DA, Chui HC, Higashida RT, Lindquist R, Nilsson PM, Roman GC et al (2011) Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42:2672–2713
Ruitenberg A, den Heijer T, Bakker SL, van Swieten JC, Koudstaal PJ, Hofman A (2005) Cerebral hypoperfusion and clinical onset of dementia: the Rotterdam Study. Ann Neurol 57:789–794
Marshall RS, Lazar RM (2011) Pumps, aqueducts, and drought management: vascular physiology in vascular cognitive impairment. Stroke 42:221–226
Pluta R, Kocki J, Maciejewski R, Ułamek-Kozioł M, Jabłoński M, Bogucka-Kocka A, Czuczwar SJ (2012) Ischemia signalling to Alzheimer-related genes. Folia Neuropathol 50:322–329
Pluta R, Ułamek M, Jabłoński M (2009) Alzheimer’s mechanisms in ischemic brain degeneration. Anat Rec (Hoboken) 292:1863–1881
Kumaran D, Udayabanu M, Kumar M, Aneja R, Katyal A (2008) Involvement of angiotensin converting enzyme in cerebral hypoperfusion induced anterograde memory impairment and cholinergic dysfunction in rats. Neuroscience 155:626–639
Pluta R, Januszewski S, Jabłoński M, Ułamek M (2010) Factors in creepy delayed neuronal death in hippocampus following brain ischemia-reperfusion injury with long-term survival. Acta Neurochir Suppl 106:37–41
Farkas E, Luiten PG, Bari F (2007) Permanent, bilateral common carotid artery occlusion in the rat: a model for chronic cerebral hypoperfusion-related diseases. Brain Res Rev 54:162–180
Choy M, Ganesan V, Thomas DL, Thornton JS, Proctor E, King MD, van derWeerd L, Gadian DG, Lythgoe MF (2006) The chronic vascular and haemodynamic response after permanent bilateral common carotid occlusion in newborn and adult rats. J Cereb Blood Flow Metab 26:1066–1075
Brines M, Cerami A (2005) Emerging biological roles for erythropoietin in the nervous system. Nat Rev Neurosci 6:484–494
Ruiz de Almodovar C, Lambrechts D, Mazzone M, Carmeliet P (2009) Role and therapeutic potential of VEGF in the nervous system. Physiol Rev 89:607–648
Lawrence MS, Sun GH, Kunis DM, Saydam TC, Dash R, Ho DY, Sapolsky RM, Steinberg GK (1996) Overexpression of the glucose transporter gene with a herpes simplex viral vector protects striatal neurons against stroke. J Cereb Blood Flow Metab 16:181–185
Semenza GL (2000) Surviving ischemia: adaptive responses mediated by hypoxia-inducible factor 1. J Clin Invest 106:809–812
Sharp FR, Bernaudin M (2004) HIF1 and oxygen sensing in the brain. Nat Rev Neurosci 5:437–448
Chavez JC, LaManna JC (2002) Activation of hypoxia-inducible factor-1 in the rat cerebral cortex after transient global ischemia:potential role of insulin-like growth factor-1. J Neurosci 22:8922–8931
Baranova O, Miranda LF, Pichiule P, Dragatsis I, Johnson RS et al (2007) Neuron-specific inactivation of the hypoxia inducible factor 1alpha increases brain injury in a mouse model of transient focal cerebral ischemia. J Neurosci 27:6320–6332
Giusti S, Plazas SFD (2011) Neuroprotection by hypoxic preconditioning involves upregulation of hypoxia-inducible factor-1 in a prenatal model of acute hypoxia. J Neurosci Res 22766:468–478
Valsecchi V, Pignataro G, PreteA D, Sirabella R, Matrone C, Boscia F, Scorziello A, Sisalli MJ, Esposito E, Zambrano N, Renzo GD, Annunziato L (2011) NCX1 Is a novel target gene for hypoxia-inducible factor-1 in ischemic brain preconditioning. Stroke 42:754–763
Ohtaki H, Fujimoto T, Sato T, Kishimoto K, Fujimoto M, Moriya M, Shioda S (2006) Progressive expression of vascular endothelial growth factor (VEGF) and angiogenesis after chronic ischemic hypoperfusion in rat. Acta Neurochir Suppl 96:283–287
Busch HJ, Buschmann IR, Mies G, Bode C, Hossmann KA (2003) Arteriogenesis in hypoperfused rat brain. J Cereb Blood Flow Metab 23:621–628
Otori T, Katsumata T, Muramatsu H, Kashiwag F, Katayama Y, Terashi A (2003) Long-term measurements of cerebral blood flow and metabolism in a rat chronic hypoperfusion model. Clin Exp Pharmacol Physiol 30:266–272
Chen W, Ostrowski RP, Obenaus A, Zhang JH (2009) Prodeath or prosurvival: two facets of hypoxia inducible factor-1 in perinatal brain injury. Exp Neurol 216:7–15
Shibata M, Hattori H, Sasaki T, Gotoh J, Hamada J, Fukuuchi Y (2002) Temporal profiles of the scbcellular localization of BIM, a BH3-only protein, during middle cerebral artery occlusion in mice. J Cereb Blood Flow Metab 22:810–820
Schmidt-Kastner R, Aguirre-Chen C, Kietzmann T, Saul I, Busto R, Ginsberg MD (2004) Nuclear localization of the hypoxia-regulated pro-apoptotic protein BNIP3 after global brain ischemia in the rat hippocampus. Brain Res 1001:133–142
Helton R, Cui J, Scheel JR, Ellison JA, Ames C, Gibson C, Blouw B, Ouyang L, Dragatsis I, Zeitlin S, Johnson RS, Lipton SA, Barlow C (2005) Brain-specific knock-out of hypoxia-inducible factor-1alpha reduces rather than increases hypoxic–ischemic damage. J Neurosci 25:4099–4107
Yan J, Zhou B, Taheri S, Shi H (2011) Differential effects of HIF-1 Inhibition by YC-1 on the overall outcome and blood-brain barrier damage in a rat model of ischemic stroke. PLoS ONE 6:27798
Yeh SH, Ou LC, Gean PW, Hung JJ, Chang WC (2011) Selective inhibition of early-but not late-expressed HIF-1a is neuropro- tective in rats after focal ischemic brain damage. Brain Pathol 21:249–262
Acknowledgments
This work was supported by the National Natural Science Foundation of China (81171029).
Conflict of interest
The authors declare no competing financial interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, Y., Zhang, J., Liu, H. et al. Changes in Levels of Hypoxia-Induced Mediators in Rat Hippocampus During Chronic Cerebral Hypoperfusion. Neurochem Res 38, 2433–2439 (2013). https://doi.org/10.1007/s11064-013-1158-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-013-1158-1