Abstract
The retina captures and converts light between 400–760 nm into electrical signals that are sent to the brain by way of the optic nerve and in the process helps to translate these electrical signals into what is known as vision. The same light that allows vision to occur is nevertheless also potentially toxic to retinal cells in certain situations. The shorter wavelengths of light are known to interact with chromophores in photoreceptors and pigment epithelial cells to cause oxidative stress and severe damage. Indeed it is generally accepted that short wavelength light effects is one cause for loss of photoreceptor function in age-related macular degeneration. Recent studies have demonstrated that light may be a contributing factor for the death of retinal ganglion cells in certain situations. Light as impinging on the retina, especially the short wavelength form, affect mitochondrial chromophores and can result in neurone death. Importantly ganglion cell axons within the eye are laden with mitochondria and unlike the outer retina are not protected from short wavelength light by macular pigments. It has therefore been proposed that when ganglion cell function is already compromised, as in glaucoma, then light impinging on their mitochondria might be a contributor to their eventual demise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The region of the electromagnetic spectrum termed “visible light” is between 400 and 760 nm. Light with wavelengths below this region are generally harmful to humans (ultraviolet, X-rays) and are filtered out by the earth’s atmosphere. Wavelengths above this region are the infrared (heat) forms and those wavelengths used in various communication and detection technologies (radio, radar, TV and microwave).
Historically, the detrimental influences of light to the eye beyond the lens have been associated with photoreceptors and retinal pigment epithelial (RPE) cells in the outer retina. The wavelengths of light reaching the retina is between 400–760 nm. The more reactive shorter wavelengths are prevented from reaching the retina by the cornea and lens [1]. The cornea absorbs wavelengths below 295 nm while the lens strongly absorbs wavelengths of light between 300–400 nm [2]. Both cornea and the lens also absorb part of infrared radiation (980–1,430 nm) and the vitreous absorbs light above 1,400 nm [3]. Absorption of the shorter wavelengths of visible radiation by the lens rises exponentially with age, due to yellowing caused by a gradual elevation of chromophores in the lens [4]. The greatest exposure of the retina to blue light therefore probably occurs in the first two decades of life [5] with individuals above 60 years of age being exposed to significantly lower fluxes of short-wavelength visible radiation than younger individuals. Blue light has been shown in numerous studies to be particularly toxic to the retina and significantly its intensity impinging on the retina is substantially reduced during the ageing process because of the yellowing of the lens. It has been suggested that the gradual yellowing of the lens is a protective physiological process for the ageing retina from blue light toxicity. This has been recognised clinically and as a consequence modern intraocular lens inserted after cataract removal filter out most of the blue wavelength light.
Photosensitizers in the Retina
Retinal photoreceptors are uniquely adapted to function over a wide range of ambient conditions. However, in most species prolonged intense visible light exposure can lead to photoreceptor damage and a generation of reactive oxygen species (ROS). In nocturnal animals, the light intensity to cause visual cell damage needs only to be two or three times above room lighting for this to occur [6–8]. Such findings have historically been related to the aetiology of debilitating ocular conditions where photoreceptor dysfunction takes place as occurs in age-related macular degeneration (AMD). It is generally acknowledged that oxidative damage that results from ROS is involved in the development of AMD [9, 10] and that ROS is generated by light interaction with photosensitizers or chromophores associated with the outer retina.
Light damage to the retina is probably multi-factorial with several different mechanisms being involved depending on the chromophore being activated for the initiation of photodamage. The retina contains a large number of chromophores of which the most obvious are the visual pigments. These are 11-cis-retinal-protein complexes, which collectively absorbs light across the whole of the visible spectrum. Selectivity is achieved by the different light absorption characteristics of rods and the three different types of cones in the human retina. Individual cone pigments vary and are maximally sensitive to long (red light), medium (green light) and short (blue light) wavelengths of light. Rods in contrast are all sensitive to blue-green light.
Rhodopsin is undoubtedly the chromophore responsible for photoreceptor damage in nocturnal rodents but this might not be entirely the case in primates [11]. It seems probable that in some species photo-bleaching of rhodopsin and/or other visual pigments is more the cause for the formation of phototoxic products to cause photodamage to the retina. The chromophore all-trans-retinal (vitamin A aldehyde), is one of the products of photo-bleached rhodopsin and is abundantly present in the retina and shown to be particularly sensitive to blue-light absorbance to cause cell toxicity [12].
A number of retinal chromophores exist in addition to rhodopsin and all-trans-retinal that when activated could lead to visual cell damage. These include the broad band absorbers of melanin complexes and lipofuscin that are present in RPE cells [13] and increase in content with age [14]. It has been demonstrated that white light irradiation of melanin or lipofuscin results in increased production of various types of ROS [15–17] to cause RPE death.
Haemoglobin and other proteins that contain porphyrin, such as mitochondrial enzymes like cytochrome oxidase (COX), have absorption maxima around 400 nm [18]. The porphyrin triplets formed by absorption of photons of suitable wavelengths can result in the formation of singlet oxygen and ROS [19] which may damage various cellular constituents. It is known that COX absorbs in the blue part of the spectrum in both its oxidised and reduced forms [20]. Another mitochondrial enzyme, cytochrome P450 is also known to absorb light of wavelengths near 450 nm when bound to carbon monoxide [21].
Flavins such as riboflavin (vitamin B2) and flavoprotein nucleotides are essential components of numerous cytosolic and mitochondrial enzyme systems. Absorption spectra of flavins are around 450–520 nm and when activated induce oxidation of several substances as well as generation of hydrogen peroxide [22, 23].
Mitochondrial Homeostasis Related to Ageing and Neurone Susceptibility
Neurones in particular have a heavy dependence on their mitochondria [24] and good evidence suggests that optimum mitochondrial homeostasis decreases with age [25, 26]. A decline in neuronal mitochondrial function is now recognised to occur in various neurodegenerative diseases and in ageing generally [27–29]. Indeed, the incidence of glaucoma in which loss of vision is caused by ganglion cells dying increases exponentially with age [30]. Unfortunately, the precise molecular basis underlying this detrimental loss in mitochondrial function in ageing remains a mystery. Despite the presence of uncoupling proteins within mitochondria to buffer the production of excessive ROS [31] optimum mitochondrial function still decreases with ageing. Altered regulation of mitochondrial fission and fusion might play a part as such processes control mitochondrial numbers, morphology, and functions [32, 33]. A decline in the efficiency of the electron transport chain function of mitochondria clearly appears to occur during ageing. For example, mitochondrial ATP production decreases and ROS increases in mitochondria from aged rodents [34, 35]. Moreover, good evidence exists to show that an increase in cellular ROS affects mtDNA function as well as induce a number of other biochemical processes, loosely termed as oxidative stress [25, 36, 37]. It is of interest to note that Tezel et al. [38] found ganglion cells from aged (24 months old) rats to be more susceptible to an insult of elevated intraocular pressure than younger (3 months old) animals showing that the functional state of neurones in situ decreases as age progresses.
Retinal Ganglion Cell Mitochondria
Retinal ganglion cells are unusual because they have quite long unmylinated axons in the eye and only become mylinated when in the optic nerve [39, 40]. The unmylinated parts of ganglion cell axons are laden with mitochondria [24, 41]. In contrast mitochondria are few in number in the mylinated parts of ganglion cell axons being restricted to areas of the Nodes of Ranvier [40, 42]. It is generally assumed that the large amount of mitochondria in the unmylinated parts of ganglion cell axons is to provide the necessary energy to propagate the action potential out of the eye globe which does not occur in the optic nerve where propagation is relayed from one Node Ranvier to another.
It is well known that the redox balance within mitochondria is critical for cellular homeostasis since the mitochondria house the energy producing systems of a cell and mitochondria plays a key role in ageing and age-related disorders [24, 37]. Production of ROS such as hydroxyl radical, singlet oxygen, hydrogen peroxide and peroxynitrite is finely balanced with sophisticated antioxidant and repair systems located in this complex organelle. Loss of these systems leads to protein oxidations that are the hall marks of many ocular diseases including retinal degenerations associated with ganglion cell loss as in glaucoma.
Significantly, the mitochondria associated with ganglion cell axons lacking myelin are unique in that they are directly exposed to light impinging on the retina. Other neurones in the retina have relatively short unmylinated axons and therefore less heavily dependent on mitochondria for normal functions in which transference of information is clearly of importance. Photoreceptor inner segments have significant numbers of mitochondria required primarily for protein synthesis as the photoreceptor outer segments are being continuously phagocytosed and renewed. Significantly, photoreceptor mitochondria are shielded from light by the macular pigments but this is not the case for ganglion cell axonal mitochondria [43, 44].
Light Affects on Mitochondrial Photosynthesizers
As already discussed light of defined wavelengths has the potential to be absorbed by mitochondrial constituents such as COX, cytochrome P45 isoenzymes, and flavin protein nucleotides. Indeed a variety of studies have suggested that photosynthesizers located to mitochondria generate ROS as a result of interaction with light [44–51]. Good evidence for this being the case was obtained by studies where freshly isolated mitochondria from the rat liver was exposed to light (400–760 nm) as impinging on the retina. Fig. 1 shows data where freshly isolated mitochondria or disrupted mitochondria caused by sonication were maintained in the dark or exposed to light at two different intensities (800 lux or 4,000 lux) for 12 h. Thereafter, the mitochondrial dehydrogenase (WST-1 assay) and redox potential (MTT assay) of the samples were assessed. WST-1 (4-[3-(4-iodophenyl)-2-(4-nitrophenyl)-2H-5-tetrazolio]-1,3-benzene disulfonate) is a tetrazolium dye containing an electron-coupling agent that is cleaved by mitochondrial dehydrogenase enzyme to a formazan dye with an absorbance at 490 nm. MTT is reduced to an insoluble, blue formazan product because of acceptance of electrons from cellular reducing equivalents such as NADH, NADPH or succinate thus providing an assay for the redox state of a sample. The results show that light (4,000 lux) decreases mitochondrial dehydrogenase and the redox state of mitochondria as compared with the dark state. Moreover, where mitochondrial function was disrupted by sonication light had no affect on mitochondrial dehydrogenase or redox state. These studies demonstrate proof of principle for the idea that light (400–760 nm) can decrease the metabolic state of mitochondria by reducing mitochondrial dehydrogenase and altering the redox state which implies a production of ROS. Moreover, this process only occurs in functional mitochondria which suggest that the cause of the light affect is by an action on the electron transport system [44].
The influence of light on isolated mitochondria from rat liver. Mitochondria in physiological medium were placed in dark or exposed to white light (800 or 4,000 lux) for 12 h. In some cases mitochondria were first sonicated and then placed in the dark. Redox potential (MTT assay) and mitochondrial dehydrogenase (WST-1 assay) associated with the samples were then determined. Sonication disrupts mitochondrial function indicated by a reduction in mitochondrial dehydrogenase and the redox state. Moreover, mitochondrial function is less efficient in the light than dark. (From Osborne et al. [44])
Figure 2 and 3 show studies that have been conducted both on a transformed retinal ganglion cell line (RGC-5 cells) and primary cultures of rat neurones [52, 53]. Here it was demonstrated that exposure of such cultures to white light (400–760 nm) for defined periods resulted in a generation of ROS accompanied by cell death. Cell death was measured in a variety of ways which included assessing the numbers of GABAergic neurones in primary culture, counting the number of TUNEL positive cells and in viability assays where the WST-1 and MTT assays were employed. The negative effect of light on cell survival in these cell culture studies is blunted by a variety of agents that include α-lipoic acid, trolox and the flavonoid epigalicatechin gallate (ECCG) (Fig. 4). Immunohistochemical evidence to suggest that light-induced RGC-5 cell death is elicited by an effect on their mitochondria is shown in Fig. 5. The protein OPA-1 is exclusively associated with mitochondria identified by use of a mitochondrial stain (mitotracker) in RGC-5 cells kept in the dark but when exposed to light OPA-1 now does not co-localise with mitotracker in all instances. More persuasive evidence for light inducing cell death by affecting their mitochondria was demonstrated in cultures of fibroblasts [54]. In these studies fibroblasts were exposed to ethedium bromide for 50 days so impairing mitochondrial DNA and affecting their respiratory chain activity. These fibroblasts with impaired mitochondria were unaffected by a defined light insult. In contrast the same light insult caused a generation of ROS and cell death to fibrobalsts with functional mitochondria [54].
This figure shows dissociates of rat retinal cells maintained in culture (dark) for 7 days. The cultures in the upper panels were “stained” for GABA and are twice the magnification of the cultures shown in the lower panels, processed for reactive oxygen species (ROS). It can be seen in b that the processes of GABA neurones are shorter following a white light insult (1,000 lux for the last 2 days) when compared with cells maintained in the dark for all seven days. Moreover, such a light insult d causes a stimulation of ROS (appears as white dots) which is virtually absent from cultures kept in the dark c. (From Lascaratos et al. [52])
This figure shows cultured RGC-5 cells stained for phosphatidylserine to indicate apoptosis (a–c) and ROS (d–f). a and d are dark maintained cultures. Cultures exposed to white light (1,000 lux, 48 h) show some cells to exhibit apoptosis (arrow heads, Fig. b) and the presence of ROS (small arrows, Fig. e). When 10μM epigallocatechin gallate (EGCG) was present in the culture medium (c and f) during the light insult little sign of apoptosis or ROS production were apparent. (From Zhang et al. [65])
This figure shows that exposure of RGC-5 cell cultures to white light (1,000 lux for 48 h) reduced cell viability by approximately 25% measured by the MTTassay. This effect is attenuated in a concentration-dependent manner by antioxidants such as α-lipoic acid (LA), trolox and EGCG. (From Osborne et al. [54])
This figure shows RGC-5 cell cultures stained for the localisation of mitochondrial OPA-1 immunoreactivity (a, d) and for mitochondria by use ofmitotracker (b, e). The upper panels are cultures maintained in the dark. The lower panels show cultures that have been exposed to white light (1,000 lux for 48 h). In the dark state OPA-1 immunoreactivity and mitotracker co-localise as shown in C. However, light (f) appears to cause a disruption of mitochondria because OPA-1 and mitotracker do not co-localise in many instances (f). The RGC-5 cell nuclei in c and f were stained blue by use of DAPI
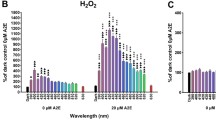
Expose of RGC-5 cells in culture to white (400–760 nm), blue (400–450 nm) or red (600–700 nm) light show that blue light affects cell survival significantly more than white light (Fig. 6). In contrast red light had no affect on RGC-5 cell survival which is consistent with studies conducted by others. For example near-infrared light via light-emitting diode treatment is known to promote wound healing in humans and animals [55] and to up-regulate cytochrome oxidase activity and ATP content in primary cultures of rat visual cortical neurons functionally inactivated by tetrodotoxin, potassium cyanide, sodium azide or rotenone [56–58].
This figure compares the effect of blue (465–470nm, 400 lux), white (400–600nm, 1,000 lux) and red (625–635nm, 1,000 lux) light on the survival of RGC-5 cells in culture over a period of 24 and 48 h. It can be seen that blue light is much more effective than white light at killing cells and that red light is practically ineffective. Results are means of two experiments
The hazards of blue light to the retina has been recognised particular by its action on RPE/photoreceptors involving chromophores formed by rhodopsin intermediates such as protein A2E a major component of lipofuscin [59, 60]. However, relatively recently it has been shown that blue light still affect RPE cells where the lipofucsin has been removed so suggesting a direct influence on mitochondrial function [51, 61]. Studies on RGC-5 cells show that this is indeed the case because such cells are free from chromophores normally associated with RPE/photoreceptors.
Light Affects on Retinal Ganglion cell Mitochondrial Homeostasis
The only central nervous neurones directly exposed to visible light are associated with the retina. The outer retinal neurones are to some extent protected from light by the macular pigments but this is not the case for retinal ganglion cells. Moreover, ganglion cell axons within the retina are laden with mitochondria. Since laboratory studies show that light can affect mitochondrial function the potential for this occurring to ganglion cells in situ cannot be ignored. We have therefore proposed that light entering the eye will directly affect ganglion cell mitochondria resulting in a generation of ROS but this is kept in a balanced state by normal scavenging mechanisms associated with the neurones. As a consequence in the normal healthy ganglion cell light does not have a detrimental influence on the neurone’s mitochondria or function. However, should ganglion cell homeostasis be compromised for one reason or another then light, particularly the blue component, might become a hazard [44]. For example, Leber optic atrophy is a maternally transmitted disorder, affecting males more frequently than females, due to mutations in mitochondrial genes encoding complex I sub-unit proteins [42, 62]. Clinically, there is an acute onset of visual loss caused by ganglion cell dysfunction, first in one eye, and then a few weeks to months later in the other. Since all mitochondria are affected by mutations it remains a mystery why ganglion cells show loss of function before other central nervous system neurones. One possibility is that it is because of light having a secondary negative affect on ganglion cell mitochondria.
It is also known from experimental studies that mitochondrial function becomes less efficient as aging progresses suggesting that optimum neuronal homeostasis decreases with age [24, 62, 63]. Moreover, the numbers of retinal ganglion cells in retinas from young individuals are known to be significantly greater than in old individuals [64]. It is therefore tempting to speculate that light might be a risk factor to ganglion cells as aging proceeds.
Finally in a disease like glaucoma ganglion cell homeostasis might be initially affected by, for example raised intraocular pressure so causing a decrease blood flow and ischemia to the optic nerve axons. Light might now become one cause for the ganglion cells to subsequently die as the disease progresses [24, 44].
Conclusions
Historically light, particularly blue light has been considered to be a hazard to the retina by affecting RPE/photoreceptors and to be a major factor for the cause for age-related macular degeneration. Our recent studies have focussed on how light affects mitochondrial function and related to the fact that ganglion cell axons within the retina are laden with mitochondria. We therefore suggest that light is a risk factor for the survival of retinal ganglion cells in certain situations where the neurones homeostasis is compromised for one reason or another. This might be the case in glaucoma; certain diseases associated with mitochondrial mutations, ageing and even diabetes. In such cases a longer preservation of vision might be obtained by simply use of appropriate spectacles aimed at filtering out blue light.
References
Sliney DH (2002) How light reaches the eye and its components. Int J Toxicol 21:501–509
Said FS, Weale RA (1959) The variation with age of the spectral transmissivity of the living human crystalline lens. Gerontologia 3:213–231
Boettner EA, Wolter JR (1962) Transmission of the ocular media. Invest Ophthalmol Vis Sci 1:776–783
Weale RA (1988) Age and the transmittance of the human crystalline lens. J Physiol 395:577–587
Lerman S (1983) An experimental and clinical evaluation of lens transparency and aging. J Gerontol 38:293–301
Noell WK (1965) Aspects of experimental and hereditary degeneration. In: Graymore C (ed) Biochemistry of the Retina. Academic Press, London, pp 51–72
Noell WK, Walker VS, Kang BS et al (1966) Retinal damage by light in rats. Invest Ophthalmol 5:450–473
Organisciak DT, Vaughan DK (2010) Retinal light damage: mechanisms and protection. Prog Retin Eye Res 29:113–134
Beatty S, Koh H, Phil M et al (2000) The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol 45:115–134
Feigl B (2009) Age-related maculopathy—linking aetiology and pathophysiological changes to the ischaemia hypothesis. Prog Retin Eye Res 28:63–86
Rózanowska M, Sarna T (2005) Light-induced damage to the retina: role of rhodopsin chromophore revisited. Photochem Photobiol 81:1305–1330
Grimm C, Wenzel A, Williams T et al (2001) Rhodopsin-mediated blue-light damage to the rat retina: effect of photoreversal of bleaching. Invest Ophthalmol Vis Sci 42:497–505
Boulton M, Docchio F, Dayhaw-Barker P et al (1990) Age-related changes in the morphology, absorption and fluorescence of melanosomes and lipofuscin granules of the retinal pigment epithelium. Vision Res 30:1291–1303
Feeney-Burns L, Hilderbrand ES, Eldridge S (1984) Aging human RPE: morphometric analysis of macular, equatorial, and peripheral cells. Invest Ophthalmol Vis Sci 25:195–200
Boulton M, Rózanowska M, Rózanowski B (2001) Retinal photodamage. J Photochem Photobiol B 64:144–161
Margrain TH, Boulton M, Marshall J et al (2004) Do blue light filters confer protection against age-related macular degeneration. Prog Retin Eye Res 23:523–531
Sarna T (1992) Properties and function of the ocular melanin—a photobiophysical view. J Photochem Photobiol B 12:215–258
Mellerio J (1994) Light effects on the retina. In: Albert DM, Jakobiec FA (eds) Principles and Practice of Ophthalmology: Basic Sciences. Saunders, Philadelphia, pp 1326–1345
Bonnett RAA, Charalamhides EJ, Land RS et al (1980) Triplet states of porphyrin esters. J Chem Soc Faraday Trans 1 76:852–859
Bell JE, Hall C (1981) Hemoproteins. In: Bell JE (ed) Spectroscopy in biochemistry. CRC Press, Boca Raton, FL, pp 42–46
Ortiz de Montellano PR (1995) The 1994 Bernard B. Brodie Award Lecture. Structure, mechanism, and inhibition of cytochrome P450. Drug Metab Dispos 23:1181–1187
Hockberger PE, Skimina TA, Centonze VE et al (1999) Activation of flavin-containing oxidases underlies light-induced production of H2O2 in mammalian cells. Proc Natl Acad Sci 96:6255–6260
Garcia J, Silva E (1997) Flavin-sensitive photooxidation of amino acids present in a parenteral nutrition infusate: protection by ascorbic acid. J Nutr Biocem 8:341–345
Osborne NN (2010) Mitochondria: their role in ganglion cell death and survival in primary open angle glaucoma. Exp Eye Res 90:750–757
Boveris A, Navarro A (2008) Brain mitochondrial dysfunction in aging. IUBMB Life 60:308–314
Dietrich MO, Horvath TL (2009) GABA keeps up an appetite for life. Cell 137:1177–1179
Chan DC (2006) Mitochondria: dynamic organelles in disease, aging, and development. Cell 125:1241–1252
Lin MT, Beal MF (2006) Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature 443:787–795
Beal MF (2005) Mitochondria take center stage in aging and neurodegeneration. Ann Neurol 58:495–505
Kong GY, Van Bergen NJ, Trounce IA et al (2009) Mitochondrial dysfunction and glaucoma. J Glauco 18:93–100
Dietrich MO, Horvath TL (2010) The role of mitochondrial uncoupling proteins in lifespan. Pflugers Arch 459:269–275
Bossy-Wetzel E, Barsoum MJ, Godzik A et al (2003) Mitochondrial fission in apoptosis, neurodegeneration and aging. Curr Opin Cell Biol 15:706–716
Knott AB, Bossy-Wetzel E (2008) Impairing the mitochondrial fission and fusion balance: a new mechanism of neurodegeneration. Ann NY Acad Sci 1147:283–292
Navarro A, Boveris A (2007) Brain mitochondrial dysfunction in aging: conditions that improve survival, neurological performance and mitochondrial function. Front Biosci 201:1154–1163
Boveris A, Navarro A (2008) Systemic and mitochondrial adaptive responses to moderate exercise in rodents. Free Radic Biol Med 44:224–229
Ott M, Gogvadze V, Orrenius S et al (2007) Mitochondria, oxidative stress and cell death. Apop 12:913–922
Jarrett SG, Lin H, Godley BF et al (2008) Mitochondrial DNA damage and its potential role in retinal degeneration. Prog Retin Eye Res 27:596–607
Tezel G, Luo C, Yang X (2007) Accelerated aging in glaucoma: immunohistochemical assessment of advanced glycation end products in the human retina and optic nerve head. Invest Ophthalmol Vis Sci 48:1201–1211
Wang L, Dong J, Cull G et al (2003) Varicosities of intraretinal ganglion cell axons in human and nonhuman primates. Invest Ophthalmol Vis Sci 44:2–9
Bristow EA, Griffiths PG, Andrews RM et al (2002) The distribution of mitochondrial activity in relation to optic nerve structure. Arch Ophtalmol 120:791–796
Carelli V, Ross-Cisneros FN, Sadun AA (2004) Mitochondrial dysfunction as a cause of optic neuropathies. Prog Retin Eye Res 23:53–89
Carelli V, Ross-Cisneros FN, Sadun AA (2002) Optic nerve degeneration and mitochondrial dysfunction: genetic and acquired optic neuropathies. Neurochem Int 40:573–584
Krinsky NI, Landrum JT, Bone RA (2003) Biologic mechanisms of the protective role of lutein and zeoxanthin in the eye. Annu Rev Nutr 23:213–231
Osborne NN, Lascaratos G, Bron AJ et al (2006) A hypothesis to suggest that light is a risk factor in glaucoma and the mitochondrial optic neuropathies. Br J Ophthalmol 90:237–241
Jung JS, Kim HJ, Cho M (1990) Action spectra for the generation of singlet oxygen from mitochondrial membranes from soybean (glycine max) hypocotyls. Photochem Photobiol 51:561–566
Chen E, Söderberg PG, Qian W (1992) Inhibition of cytochrome oxidase by blue light (404 nm). A factor that causes retinal injury? Invest. Ophthalmol. Vis. Sci. 33:919
Chen E, Söderberg PG, Lindström B (2002) Cytochrome oxidase activity in rat retina after exposure to 404 nm blue light. Curr Eye Res 11:825–831
Chen Q, Vazques EJ, Moghaddas S et al (2003) Production of reactive oxygen species by mitochondria: central role of complex III. J Biol Chem 278:36027–36031
Egorov SY, Krasnovsky AA Jr, Bashtanov MY et al (1999) Photosensitization of singlet oxygen formation by pterins and flavins. Time-resolved studies of oxygen phosphorescence under laser excitation. Biochemistry (Mosc) 64:1117–1121
King A, Gottlieb E, Brooks DG et al (2004) Mitochondria-derived reactive oxygen species mediate blue light-induced death of retinal pigment epithelial cells. Photochem Photobiol 79:470–475
Godley BF, Shamsi FA, Liang F et al (2005) Blue light induces mitochondrial DNA damage and free radical production in epithelial cells. J Biol Chem 280:21061–21066
Wood JP, Lascaratos G, Bron AJ et al (2007) The influence of visible light exposure on cultured RGC-5 cells. Mol Vis 14:334–344
Lascaratos G, Ji D, Wood JP et al (2007) Visible light affects mitochondrial function and induces neuronal death in retinal cell cultures. Vis Res 47:1191–1201
Osborne NN, Li GY, Ji D et al (2008) Light affects mitochondria to cause apoptosis to cultured cells: possible relevance to ganglion cell death in certain optic neuropathies. J Neurochem 105:2013–2028
Whelan HT, Smits RL Jr, Buchman EV et al (2001) Effect of NASA light-emitting diode irradiation on wound healing. J Clin Laser Med Surg 19:305–314
Wong-Riley MT, Bai X, Buchmann E et al (2001) Light-emitting diode treatment reverses the effect of TTX on cytochrome oxidase in neurons. Neuroreport 12:3033–3037
Wong-Riley MT, Liang HL, Eells JT et al (2005) Photobiomodulation directly benefits primary neurons functionally inactivated by toxins: role of cytochrome c oxidase. J Biol Chem 280:4761–4771
Liang HL, Whelan HT, Eells JT et al (2008) Near-infrared light via light-emitting diode treatment is therapeutic against rotenone- and 1-methyl-4-phenylpyridinium ion-induced neurotoxicity. Neuroscience 153:963–974
Wenzel A, Grimm C, Samardzija M et al (2005) Molecular mechanisms of light-induced photoreceptor apoptosis and neuroprotection for retinal degeneration. Prog Retin Eye Res 24:275–306
Sparrow JR, Cai B (2001) Blue light-induced apoptosis of A2E-containing RPE: involvement of caspase-3 and protection by Bcl-2. Invest Ophthalmol Vis Sci 42:1356–1362
Rezai KA, Gasyna E, Seagle BL, Norris JR Jr, Rezaei KA (2008) AcrySof Natural filter decreases blue light-induced apoptosis in human retinal pigment epithelium. Graefes Arch Clin Exp Ophthalmol 246:671–676
Carelli V, Rugolo M, Sgarbi G et al (2004) Bioenergetics shapes cellular death pathways in Leber’s hereditary optic neuropathy: a model of mitochondrial neurodegeneration. Biochim Biophys Acta 1658:172–179
Navarro A, Boveris A (2007) The mitochondrial energy transduction system and the aging process. Am J Physiol Cell Physiol 292:C670–C686
Curcio CA, Drucker DN (1993) Retinal ganglion cells in Alzheimer’s disease and aging. Ann Neurol 33:248–257
Zhang B, Rusciano D, Osborne NN (2008) Orally administered epigallocatechin gallate attenuates retinal neuronal death in vivo and light-induced apoptosis in vitro. Brain Res 10:141–152
Acknowledgment
This article is dedicated to Professor Abel Lajtha who has been chief editor of Neurochemistry Research for the past 35 years. Abel is very much one of the fathers of modern neurochemistry and has been an inspiration to many of us because of his scientific achievements and many contributions to the neurochemistry/neuroscience communities. Thank you Abel and wish you well in your “retirement”.
Author information
Authors and Affiliations
Corresponding author
Additional information
Special issue in honour of Professor Abel Lajtha.
Cátedra de Biomedicina (Chair of Biomedicine) supported by the Fundación BBVA, Spain.
Rights and permissions
About this article
Cite this article
Osborne, N.N., Kamalden, T.A., Majid, A.S.A. et al. Light Effects on Mitochondrial Photosensitizers in Relation to Retinal Degeneration. Neurochem Res 35, 2027–2034 (2010). https://doi.org/10.1007/s11064-010-0273-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-010-0273-5