Abstract
The pathogenesis of sepsis associated encephalopathy (SAE) is not yet clear: the blood–brain barrier (BBB) disruption has been indicated among the possible causative mechanisms. S100B, a calcium binding protein, originates in the central nervous system but it can be also produced by extra-cerebral sources; it is passively released from damaged glial cells and neurons; it has limited passage through the BBB. We aimed to demonstrate BBB damage as part of the pathogenesis of SAE by cerebral spinal fluid (CSF) and serum S100B measurements and by magnetic resonance imaging (MRI). This paper describes four septic patients in whom SAE was clinically evident, who underwent MRI and S100B measurement. We have not found any evidence of CSF-S100B increase. Serum S100B increase was found in three out of four patients. MRI did not identify images attributable to BBB disruption but vasogenic edema, probably caused by an alteration of autoregulation, was diagnosed. S100B does not increase in CSF of septic patients; S100B increase in serum may be due to extracerebral sources and does not prove any injury of BBB. MRI can exclude other cerebral pathologies causing brain dysfunction but is not specific of SAE. BBB damage may be numbered among the contributors of SAE, which aetiology is certainly multifactorial: an interplay between the toxic mediators involved in sepsis and the indirect effects of hyperthermia, hypossia and hypoperfusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Sepsis associated encephalopathy (SAE) is a neurological complication of sepsis characterized by clinical features ranging from inattention and agitation to coma. Deterioration of neurological functions often follows multiple organ failure in sepsis patients; neverthless, even patients who have sepsis but have an acceptable hemodynamic stability and oxygenation could manifest neurological dysfunction as first organ failure.
The pathophysiology of SAE is poorly understood: increased permeability and disruption of the brain–blood barrier (BBB) and the associated brain edema may be involved in the pathogenesis [1, 2].
The blood–CSF barrier, the vascular–endothelial barrier and the arachnoid barrier constitute the functional brain barrier.
Blood–CSF barrier is constituted by epithelial cells of the plexus, joined by tight junctions, which form a continuous layer. Vascular-endothelial barrier is achieved by tight junctions between endothelial cells. In addition to the endothelial cells, pericytes, perivascular microglia, and astrocytes contribute to the barrier. Arachnoid barrier is guaranteed by the outermost layer of cells of the arachnoid [3].
S100B [4], a calcium binding protein produced in the central nervous system mainly—but not exclusively—by astroglial cells has been proposed as diagnostic marker of blood–brain barrier disruption [5]: for this peculiarity S100B monitoring could be relevant in patients affected by SAE.
CT head scan and cerebrospinal fluid analysis do not give definitive information in case of SAE; MRI may aid in diagnosis of brain abnormalities and eventually in prognostication, but its cost and the complicated transport of patients have been a limitation to the widespread use of this investigation in the clinical management of sepsis [6].
We report four cases of critical patients who developed SAE: S100B measurement in liquor and serum, MRI and EEGs recordings were performed.
Methods
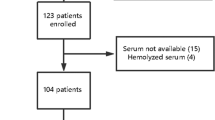
Two comatose patients affected by severe sepsis and two patients with septic shock were admitted in our ICU. Pre-existing CNS diseases and any known condition associated with a S100B increase in serum or liquor [7] were excluded. Both patients underwent total body CT scan at admission.
The patients underwent standard treatment and diagnostic protocol for sepsis [8]. The patients were followed up for 90 days: neurological recovery was evaluated by Glasgow Outcome Scale (GOS), measured at ICU discharge and at 90 days.
At ICU admission, S100B concentrations were measured by Liaison® Sangtec 100 (Sangtec Medical, Sweden), using an automated immunoluminometric assay for the quantification of protein. The assay was performed according to the manufacturer’s instructions. A serum S100B level >0.15 μg/l was defined as increased; the sensitivity of the S100B assay was <0.02 μg/l [9].
When appropriate, (in two cases, to exclude cerebral infections) cerebral spinal fluid (CSF) was withdrawn (lumbar puncture) for chemical and microbiological examination. In controls lumbar CSF S100B ranged from 0.16 to 0.52 μg/l [10]; S100B serum/CSF ratio is about 1/18 when the BBB is intact [10].
Brain MRI was performed on a 1.5 T-magnet system (T1–T2 weighted and FLAIR and DWI imaging) as soon as possible after the clinical diagnosis of SAE.
On the first day, EEG was recorded and scored according the classification of Young [12], to allow the comparison of results.
Alteration of consciousness was evaluated by Glasgow Coma Scale (GCS) daily.
Patients
1. 33 years old, male, affected by chronic renal failure (CRF). Admitted in ICU because of catheter related sepsis and coma: Glasgow Coma Scale (GCS) was 7 (best eye response (BER) = 1, best motor response (BMR) = 5, best verbal response (BVR) = 1).
On day 7, septic shock was reported; on day 20, the patient was apyretic with stable hemodynamics, GCS was 10 (BER = 4, BMR = 5, BVR = 1). On day 38, the patient developed VAP and on day 44 the patient died without recovering consciousness.
2. 51 years old, male, affected by severe descending necrotizing mediastinitis, requiring surgical treatment. Admitted in ICU on the 5th post-operative day, because of septic shock; GCS was 12 (BER = 4; BMR = 6; BVR = 2). On the 26th post-operative day, he underwent MRI (Fig. 1) since the transport was finally considered safe, thanks to the improved hemodynamics.
On the 47th day he was transferred to surgery, well oriented and cooperative; on day 90 he recovered consciousness completely.
3. 49 year old, female, affected by CRF, treated by peritoneal dialysis, underwent hemicolectomy for bowel perforation. On the third post-operative day, because of deterioration of consciousness (GCS = 9; BER = 2; BMR = 5; BVR = 2) the patient was intubated and mechanically ventilated. No signs of shock were evident; S100B levels were assessed, MRI and EEG were performed. She completely recovered and the patient was fully conscious since day 27. On day 90, she presented complete functional recovery.
4. 61 year old, male, underwent gastrectomy because of cancer. On the 7th post-operative day the patient was intubated and mechanically ventilated because of deterioration of consciousness (GCS = 4; BER = 2; BMR = 1; BVR = 1) and hemodynamic instability. The EEG and the MRI were performed. S100B levels were measured; the same day the patient developed septic shock and, after 4 days, died without recovering consciuosness.
Results
Results are described in Table 1.
Patients were intensively studied for excluding every possible differential diagnosis of SAE. Acute ischemic stroke and central nervous infection were waived by clinical examination and CT scan at admission in both cases. As concern patient 1 and 3, we rapidly ruled out prolonged hypotension, hypoglycaemia, electrolyte abnormalities as causes of coma but some metabolic derangements as elevation of BUN and hyperammoniemia, (evidences of renal and hepatic dysfunction), could not be dismissed definitively. At ICU admission, ammoniemia value (75 μm/l and 78, respectively) was elevated but not unequivocal causes of coma; the patients underwent dialysis treatment three times a week during their ICU stay.
The EEG showed diffuse cerebral involvement and was indicative of metabolic encephalopathy in patient 1, 3 and 4 while it was almost normal in patient 2, who scored a GCS of 12.
S100B serum levels were increased in patient 1 and 3 who were in coma (GCS 7 and 9) but normal (below 0.15 μg/l, commonly used as cut-off value) in patient 2 who suffered a less degree of cerebral dysfunction (GCS 12) and slightly increased in patient 4 who was in severe coma (GCS 4) and died without recovering consciousness.
Cereberal spinal fluid analysis was negative and S100B CSF levels were normal in both cases.
Magnetic resonance imaging was normal at admission in patients 1 and 3 while patient 2 (on day 20) presented in the frontal region, cortical and sub-cortical, more evident on the right side, small hyper intense areas (T2 weighted and FLAIR imaging). Similar results were present in patient 4 MRI (small hyper intense areas localized in periventricular regions) which could suggest vasogenic edema, more easily related to the loss of cerebral auto-regulation than to BBB disruption. Cytotoxic edema was excluded by diffusion images.
Patient 1 repeated MRI and EEG on day 20, after he had suffered and recovered from septic shock: results were unchanged, compared to those of admission.
Discussion
S100B did not increase in CSF in our two SAE patients. At the moment, due to the small number of patients described in this observational paper, it is impossible to draw any definitive conclusion.
The exact physiopathology of SAE is not known but direct CNS injury have been included in the list of contributors to the alteration of consciousness. Since S100B has a poor ability to escape the tight junctions of the blood-brain barrier, its increase in the serum has been attributed to an increased permeability of the BBB. The BBB disruption and opening are leading to vasogenic brain edema, which can contribute to the pathogenesis of SAE. In porcine endotoxemic shock, Larsson et al. [13] found increased serum levels of S100B which were attributed to minor blood–brain barrier damage caused by the endotoxin effect on glial cell integrity even if the authors cannot exclude the contribution of other cells.
If the serum levels of S100B depended exclusively on the entity of brain damage and BBB disruption, we should find a very large increase in S100B CSF values, as conditio sine qua non for achieving the serum increase. As previously reported [7] the increase of S100B in septic patients does not correlate with the severity of the neurological impairment or with the outcome. The release of S100B from extracerebral tissue (S100B found in chondrocytes and adipocytes is up to 1/4 of S100B brain content [9]) is a well known topic and in absence of a very relevant CSF levels increase, the concentrations of the blood circulating protein cannot be attributed to alteration of BBB or direct brain damage. Moreover, S100B may have a role in delayed reparative processes and may be of potential therapeutic value in patients who sustain various forms of acute brain damage [14].
Nevertheless, the possibility that BBB damage is an important contributor of SAE deserves high regard: an increased BBB permeability has been demonstrated in numerous experimental models of sepsis or SIRS [15].
In a MRI study of septic shock patients, Sharshar et al. [6] described injuries of the white matter in the “border” regions, where the terminal vessels may be easily jeopardized, independently of specific BBB lesions.
Bartisnsky [16] reported 26 cases of PRES associate with isolated infection or sepsis: the term PRES (posterior reversible encephalopathy syndrome) [17] is used to indicate vasogenic edema in the parietal/occipital regions in many different inflammatory diseases, postchemotherapy and in eclampsia patients.
The acronym CABS (cerebral autoregulation breakdown syndrome) has been proposed by A. Rossi (personal data not published) to indicate all the brain MRI findings that are somehow related to systemic inflammation, which are potentially reversible and often located in the posterior regions, where autoregulation is more delicate and easily lost. MRI images of edema in SAE may be related to the loss of autoregulation even if the initial vasogenic edema may evolve into cytotoxic edema.
In our opinion, SAE is surely multifactorial and it’s arduous to exclude interplay between the toxic mediators involved in sepsis and the indirect effects of hyperthermia, hypossia and hypoperfusion. The role of S100B in SAE is not clear but is increase in serum is very probably of extracerebral origin and does not prove an injury of BBB.
References
Sharshar T, Hopkinson NS, Orlikowski D, Annane D (2005) Science review: the brain in sepsis–culprit and victim. Crit Care 9:37–44. doi:10.1186/cc2951
Esen F, Erdem T, Aktan D, Orhan M, Kaya M, Eraksoy H, Cakar N, Telci L (2005) Effect of magnesium sulfate administration on blood–brain barrier in a rat model of intraperitoneal sepsis: a randomized controlled experimental study. Crit Care 9:R18–R23. doi:10.1186/cc3004
Baumann N, Pham-dinh D (2002) Astrocytes. In: Ramachandran VS (ed) Encyclopedia of the Human Brain. Academic Press, New York, pp 251–268
Donato R (2003) Intracellular and extracellular roles of S100 proteins. Microsc Res Tech 60:540–551. doi:10.1002/jemt.10296
Unden J, Christensson B, Bellner J, Alling C, Romner B (2004) Serum S100B levels in patients with cerebral and extracerebral infectious disease. Scand J Infect Dis 36:10–13. doi:10.1080/00365540310017294
Sharshar T, Carlier R, Bernard F, Guidoux C, Brouland JP, Nardi O, De la Grandmaison GL, Aboab J, Gray F, Menon D, Annane D (2007) Brain lesions in septic shock: a magnetic resonance imaging study. Intensive Care Med 33:798–806. doi:10.1007/s00134-007-0598-y
Piazza O, Russo E, Cotena S, Esposito G, Tufano R (2007) Elevated S100B levels do not correlate with the severity of encephalopathy during sepsis. Br J Anaesth 99:518–521. doi:10.1093/bja/aem201
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL (2008) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med 34(1):17–60. doi:10.1007/s00134-007-0934-2
Heizmann CW (2004) S100B protein in clinical diagnostics: assay specificity. Clin Chem 50:249–251. doi:10.1373/clinchem.2003.027367
Kleine TO, Benes L, Zofel P (2003) Studies of the brain specificity of S100B and neuron-specific enolase (NSE) in blood serum of acute care patients. Brain Res Bull 61:265–279. doi:10.1016/S0361-9230(03)00090-X
Reiber H (2001) Dynamics of brain-derived proteins in cerebrospinal fluid. Clin Chim Acta 310:173–186. doi:10.1016/S0009-8981(01)00573-3
Young GB, Bolton CF, Archibald YM, Austin TW, Wells GA (1992) The electroencephalogram in sepsis-associated encephalopathy. J Clin Neurophysiol 9:145–152. doi:10.1097/00004691-199201000-00016
Larsson A, Lipcsey M, Sjolin J, Hansson LO, Eriksson MB (2005) Slight increase of serum S-100B during porcine endotoxemic shock may indicate blood–brain barrier damage. Anesth Analg 101:1465–1469. doi:10.1213/01.ANE.0000180193.29655.6A
Kleindienst A, Hesse F, Bullock MR, Buchfelder M (2007) The neurotrophic protein S100B: value as a marker of brain damage and possible therapeutic implications. Prog Brain Res 161:317–325. doi:10.1016/S0079-6123(06)61022-4
Tsao N, Hsu HP, Wu CM, Liu CC, Lei HY (2001) Tumour necrosis factor-alpha causes an increase in blood–brain barrier permeability during sepsis. J Med Microbiol 50:812–821
Bartynski WS, Boardman JF, Zeigler ZR, Shadduck RK, Lister J (2006) Posterior reversible encephalopathy syndrome in infection, sepsis, and shock. AJNR Am J Neuroradiol 27:2179–2190
Servillo G, Bifulco F, De Robertis E, Piazza O, Striano P, Tortora F, Striano S, Tufano R (2007) Posterior reversible encephalopathy syndrome in intensive care medicine. Intensive Care Med 33:230–236. doi:10.1007/s00134-006-0459-0
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Piazza, O., Cotena, S., De Robertis, E. et al. Sepsis Associated Encephalopathy Studied by MRI and Cerebral Spinal Fluid S100B Measurement. Neurochem Res 34, 1289–1292 (2009). https://doi.org/10.1007/s11064-008-9907-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-008-9907-2