Abstract
Hyperbaric oxygen (HBO) is known to cause oxidative stress in several organs and tissues. Due to its high rate of blood flow and oxygen consumption, the brain is one of the most sensitive organs to this effect. The present study was performed to elucidate the relation of HBO exposure time to its oxidative effects in rats’ brain cortex tissue. For this purpose, 49 rats were randomly divided into five groups. Except the control group, study groups were subjected to three atmospheres HBO for 30, 60, 90, and 120 min. Their cerebral cortex layer was taken immediately after exposure and used for analysis. Thiobarbituric acid reactive substances (TBARS), superoxide dismutase (SOD), glutathione peroxidase (GSH-Px), and nitrate–nitrite (NOX) levels were determined. TBARS and SOD levels were found to increase in a time-dependent manner. GSH-Px activity reflected an inconsistent course. NOX levels were found to be increased only in the 120 min exposed group. The results of this study suggests that HBO induced oxidative effects are strongly related with exposure time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperbaric oxygen (HBO), exposure to oxygen at a pressure greater than one atmosphere absolute (ATA), has been successfully used as an adjunctive therapy for many clinical disorders related to both ischemia and/or hypoxia [1]. Given the general association of high partial oxygen pressures with formation of reactive oxygen species (ROS), the use of HBO in treating conditions which present increased ROS production themselves, such as ischemia/reperfusion injury, appears counterintuitive [2]. Thus, HBO seems to interact with molecular components of the cell, e.g., a wide range of cytokines, which are still not defined in detail [3–5].
The fact that pure oxygen exposure can be toxic has a long history beginning with the report of Antoine L. Lavoisier in 1789, only several years after the discovery of oxygen by Joseph Priestley [6]. Approximately one century later Paul Bert observed toxic effects during pure oxygen administration under pressure [7], summarized as muscle twitching and spasm, nausea and vomiting, dizziness, vision (tunnel vision) and hearing difficulties (tinnitus), twitching of facial muscles, irritability, confusion and a sense of impending doom, trouble breathing, anxiety, unusual fatigue, and finally seizures, called together as the ‘Paul Bert effect.’ Thus, investigators attracted attention to the possible detrimental effects of oxygen exposure under pressure whereby the brain was defined as on of the most important target tissues to be affected. Nevertheless, due to the vital nature of oxygen, HBO therapy has achieved more and more utilizing areas during the last decades [1]. Taken together, with or without pressure, oxygen therapy is widely accepted as a double-edged sword; therefore, nearby the reports to the beneficial effects of HBO, a considerable number of studies on the subject ‘oxygen toxicity’ have been published over the last four decades [8–12].
Today we clearly know that HBO treatment results with increased ROS production [13–16] and that ROS have the ability to act as important signaling molecules [17]. Moreover, it has been hypothesized that some of HBO’s beneficial effects may occur via the action of the stimulated reactive molecules, especially superoxide ( \( {\text{O}}^{{ \cdot - }}_{{\text{2}}} \)) and hydrogen peroxide (H2O2) [18]. HBO is a very interesting therapeutic modality which is known to produce oxidative stress itself, but reduces oxidative stress when used in pathologic conditions [19]. Edema reduction, impairment of leukocyte adhesion, enhancement of antibacterial mechanisms, stimulation of fibroblast proliferation, and neovascularization constitutes the majority of HBO’s beneficial pharmacological effects [20], but neither the basic mechanisms of these benefits nor those of its adverse effects have been established adequately.
One main goal of our research team is to elucidate the oxidative effects of HBO and to provide more information about its ‘pharmacodynamics’; i.e., relation to exposure pressure, relation to exposure time, and persistence of those effects. To achieve this aim, recently, we showed in rats that the oxidative effect of HBO is related to exposure pressure [21]. In that study, rats were exposed to a single-session of HBO fixed at 2 h exposure time but with varying pressures starting from normobaric level up to three ATA; thiobarbituric acid reactive substances (TBARS) as a measure of lipid peroxidation and the antioxidant enzyme superoxide dismutase (SOD) were found to increase proportional with incremental pressure in all investigated tissues. The present study was established as a complementary issue to the previous one, differing with the fixed pressure and the variable exposure period. This time, glutathione peroxidase (GSH-Px) activity, another antioxidant enzyme, was measured along with SOD and TBARS levels. Nitric oxide (NO), known to play role in central nervous system (CNS) oxygen toxicity [22, 23], is also included in the measured parameter list via the indirect detection of its end products nitrate and nitrite (NOX) levels. Especially, the potential of NO as a signaling molecule [24] makes it to an important molecule which may interact with the effects of HBO [25].
Experimental procedure
Animals and study groups
The Experimentation Ethics Committee of our institution approved the experimental procedures of the study. A total of 49 adult, male Sprague-Dawley rats bred in our laboratory were used for the experiment. The rats were 12 weeks old and weighed 200–250 g. Housing was at 22–24°C with light from 08.00 a.m. to 08.00 p.m. with free access to water. All animals were fed a commercial diet during the experiment. They were randomly distributed into five groups as follows: (A) control group without HBO exposure (n = 9); (B) 30 min HBO exposed group (n = 10); (C) 60 min HBO exposed group (n = 10); (D) 90 min HBO exposed group (n = 10); (E) 120 min HBO exposed group (n = 10).
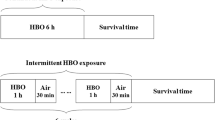
HBO exposure
A special animal hyperbaric chamber (made in Etimesgut Military Equipment Factory; Ankara, Turkey) was used for HBO exposure. The exposure pressure was set 3 ATA for all study groups, except the control group which is not exposed to HBO to determine basal (physiologic) levels of measured parameters. Ventilation rate was provided as 3–4 l/min. Compression and decompression of the chamber was completed gradually in 5–10 min. All administrations were started at the same hour in the morning (08.00 p.m.) to prevent biologic rhythm changes.
Chemicals
All chemicals were obtained from Sigma-Aldrich Chemie GmbH (Taufkirchen, Germany) and all organic solvents from Merck KGaA (Darmstadt, Germany). All reagents were of analytical grade, were prepared each day (except the phosphate buffer) and stored in a refrigerator at +4°C. The reagents were equilibrated at room temperature for 0.5 h before use when the analysis was initiated or reagent containers were refilled. Phosphate buffers were stable at +4°C for 1 month.
Tissue preparation
Right after the exposure period, the animals were anesthetized with a ketamine (85 mg/kg) plus xylasine (12.5 mg/kg) combination. The brain was removed immediately and the entire cerebral cortex from each animal was collected into separate tubes and frozen in liquid nitrogen. The frozen tissues were then homogenized in phosphate buffer (0.1 mmol/l, pH 3) by means of a homogenizator (Heidolph Diax 900; Heidolph Elektro GmbH, Kelhaim, Germany). Finally, the supernatants were divided into 2–3 parts, put in separate tubes, and stored at −80°C.
Biochemical analysis
First of all, the protein content of brain cortex tissue was measured by the method of Lowry et al. with bovine serum albumin as the standard [26]. Lipid peroxidation levels were measured with the thiobarbituric acid (TBA) reaction using the method of Ohkawa et al. [27]. This method was used to obtain a spectrophotometric measurement of the color produced during the reaction to TBA with MDA at 535 nm. For this purpose, 2.5 ml of 100 g/l trichloroacetic acid solution was added to 0.5 ml homogenate in each centrifuge tube and placed in a boiling water bath for 15 min. The mixture was cooled and centrifuged at 1,000g for 10 min. Next, 2 ml of the supernatant was added to 1 ml of 6.7 g/l TBA solution in a test tube, and placed in a boiling water bath for 15 min. The solution was then cooled and its absorbance was measured with a spectrophotometer (Shimadzu UV-1601; Kyoto, Japan). TBARS levels were presented as nmol/g-protein. SOD activity was assayed using the nitroblue tetrazolium (NBT) method of Sun et al. [28]. The stock solution contained 10 mg of Cu/Zn-SOD from bovine liver dissolved in 10 ml of isotonic saline; before being used in the assay, it was diluted to 600 μg/l with distilled water. The SOD assay reagent consisted of the combination of following reagents: 80 ml of 0.3 mmol/l xanthine solution, 40 ml of 0.6 mmol/l ethylenediaminetetraacetic acid (EDTA) solution, 40 ml of 150 μmol/l NBT solution, 24 ml of 400 mmol/l Na2CO3 solution and 12 ml of bovine serum albumin. The samples were subjected to ethanol-chloroform (62.5/37.5%) extraction prior to the assay of enzyme activity. Briefly, 400 μl of ice-cold ethanol/chloroform mixture was mixed thoroughly with 250 μl of sample. After vortexing for 30 s and centrifugation at 3,000g at +4°C for 5 min, the upper aqueous layer was collected. The collected supernatant was diluted by a factor of 100, and 0.5 ml of the diluted solution was used for the assay by addition to 2.5 ml of SOD assay reagent. NBT was reduced to formazan by \( {\text{O}}^{{ \cdot - }}_{{\text{2}}} \), which has a strong absorbance at 560 nm. One unit (U) of SOD is defined as the amount of protein that inhibits the rate of NBT reduction by 50%. The calculated SOD activity was expressed as U/g-protein. GSH-Px activity was measured using the method described by Paglia and Valentine coupling the GSH-Px activity with the oxidation of NADPH by glutathione reductase [29]. The oxidation of NADPH was spectrophotometrically followed up at 340 nm at 37°C. The reaction mixture consisted of 50 mmol potassium phosphate buffer (pH 7), 1 mmol EDTA, 1 mmol NaN3, 0.2 mmol NADPH, 1 mmol glutathione and 1 U/ml of glutathione reductase. The absorbance at 340 nm was recorded for 5 min. The activity was the slope of the lines as mmol of NADPH oxidized per minute. GSH-Px activity was expressed as U/g-protein. NOX levels of brain cortex homogenates were measured in triplicate after conversion of nitrate to nitrite by nitrate reductase, and nitrite was measured by using the Griess reaction as described by Moshage et al. [30]. The intraessay and interassay coefficients of variation were 3 and 7%, respectively. Recoveries of both nitrites and nitrates in our samples were greater than 95%. The final calculated levels were presented as ng/g-protein.
Statistical analyses
All results were expressed as median and range. Variance analyses were performed with the Kruskal–Wallis test followed with post hoc Mann–Whitney U test. Additionally, Pearson correlation analyses of the TBARS, SOD, GSH-Px, and NOX changes were conducted. Estimated ‘P’ values of less than 0.05 were regarded as statistically significant.
Results
All numeric outcome is collected in Fig. 1 in detail.
Outcome of antioxidant enzymes activities, lipid peroxidation and nitrite-nitrate measurement in rat’s brain cortex tissue: values are presented as ‘median and range’; statistically significant # versus control group, and § versus 30 min, ¥ versus 60 min and $ versus 90 min exposed groups. SOD activity presented clearly an increasing course depending to exposure time, whereas GSH-Px activities resulted changeable. The increases of SOD activity were estimated to be in correlation with time increment (P < 0.01), whereas GSH-Px activity presented no correlation to exposure time (P > 0.05). HBO induced a significant increase of TBARS levels with proportion to exposure time; the increase rate was found to be correlated with exposure time (P < 0.01). NOx values, indicating NO production in brain cortex tissue, first continued at a relative constant level until 90 min HBO exposure. Then, with 2 h of exposure a significant increasing effect was to see
Lipid peroxidation
Thiobarbituric acid reactive substances values presented a significant raise which began just with 30 min exposure and continued to increase proportional to exposure time (P = 0.041 for group B, P < 0.001 for groups C, D, and E versus control). Furthermore, when comparisons were performed step-to-step with incremental exposure time, all steps were found to present significant increases (P < 0.001 for comparisons as follows: group B versus C, group C versus D and group D versus E).
Antioxidant enzymes activity
Superoxide dismutase activity tended to follow the course of TBARS levels, except with 30 min of exposure (P > 0.05 for group B, P < 0.001 for groups C, D, and E versus control). Albeit significantly increased at all time points of exposure, the outcome of GSH-Px differed from both, TBARS and SOD, reflecting the highest activity at 30 min and tended then to decline to relatively lower levels (P = 0.001 for groups B and C, P = 0.018 for group D, and P = 0.027 for group E versus control).
Step-to-step comparisons indicated significance for SOD at all steps (P = 0.002 for group B versus C and C versus D, P < 0.001 for group D versus E), whereas GSH-Px activity presented no significant change among steps of exposure time (P > 0.05 for all).
Nitrites-Nitrates
Nitrate–nitrite values were found to be unchanged until 90 min of exposure and showed first a significant increase with 120 min of HBO exposure (P > 0.05 for groups B, C, and D, P = 0.003 for group E versus control). The rise of NOX values was only significant at the step from 90 to 120 min (P = 0.003 for group D versus E, P > 0.05 for else).
Correlation analysis
The increasing rates of TBARS, SOD, and NOX were estimated to be in correlation with each other (r = 0.905, P < 0.001 for TBARS versus SOD; r = 0.559, P < 0.001 for TBARS versus NOX; and r = 0.400, P = 0.004 for SOD versus NOX). However, changes of GSH-Px were found not to be correlated with other parameters (P > 0.05 for all).
Discussion
During it’s clinically use since 1960s there is no serious toxicity report depending on the HBO treatments; e.g., a retrospective clinical study established on over 80,000 patients treated with HBO reported only two seizure cases [31]. Nevertheless, the potential risk of toxicity belong to breathed 100% oxygen during treatment sessions restricts further widening of its indication area. The majority of experimental work established on this topic have been tended to direct toxic effects of HBO with relatively higher pressure/duration ranges than clinically used, such as 4–5 ATA and/or longer periods over 2 h [11, 13, 32–35]. It is impossible to adapt these works to approved therapeutic limits, i.e., a maximum exposure pressure of 3 ATA and 2 h duration [1]. Thus, in our previous studies [21, 36–40] as well as in the present one we investigated around HBO-induced oxidative action within this approved limits.
Using HBO as a source of oxidative stress to investigate the effectiveness of several antioxidant molecules is a widely accepted method [41]. Recent work of our laboratory presented successful effects of melatonin, a strong antioxidant molecule, against HBO-induced oxidative stress [36–38]. Our most recent studies, clearly demonstrated that molecules of the oxidant and antioxidant systems, i.e., TBARS, SOD, GSH-Px, and NOX, did not persist at increased levels more than 60–90 min in several tissues after HBO exposure [39, 40]. Nevertheless, a pressure- and/or time-response relationship of HBO’s oxidative action has not been systematically investigated in well-designed studies. Investigating the pressure-response effect we previously defined an incremental oxidative effect of HBO with relation to exposure pressure; in that study significant oxidative effect of hyperoxia began just with normobaric 100% oxygen exposure but the oxidative level increased significantly with incremental pressure [21]. The results of the present study demonstrated that HBO-induced oxidative effects are not only depending on pressure but also to exposure duration.
Almost all of the studies investigating the relation of HBO to oxidative parameters are agreeing with the declaration that HBO causes oxidative stress which is demonstrated with various oxidation products in several tissues. In this study we tried to provide information on the time-response relationship of HBO exposure and several oxidant/antioxidant parameters. TBARS and SOD-values presented clearly a time-related incremental course in the present study, whereas GSH-Px activity reacted variable. A statistical significant raise of GSH-Px activity was seen which is not correlated with the increase rate of SOD and TBARS; interestingly, the enzyme’s activity tended to present an earlier peak and decreased to lower levels with prolonged sessions. Recently, it was demonstrated that hyperoxia stimulates SOD mRNA expression in the rat brain [42, 43]. In agreement with this statement, a newly finished work in our laboratory provided evidence that HBO can directly induce transcription and translation of SOD in rats’ brain cortex tissue (not published yet). This may be a possible reason for the increasing rates of SOD with HBO exposure.
The variable outcome of GSH-Px activity is also concordant with literature since having the most conflicting reports above all antioxidant enzymes [32, 33, 44, 45]. In our previous work, we determined GSH-Px activity two times, once with a single session [37] and second with a multiple HBO exposure procedure [38], which resulted both with statistically insignificant levels in brain and lung tissue of rats. Although not significant, the previous one-session study resulted with a slightly high GSH-Px value in brain tissue after a 3 ATA/2 h exposure [37]. Differently, the present study resulted with statistically high GSH-Px levels at the same point reflecting again a conflicting outcome of this enzyme. Nevertheless, its course tended to decrease (see in Fig. 1) and a considerable number of the studies performed with longer HBO exposures than 2 h reported a fall in GSH-Px activity [32, 34, 35]. Without doubt, measurement of additional parameters of the glutathione cycle, namely glutathione reductase and oxidized-reduced glutathione, and on the other hand the antioxidant enzyme catalase, fighting against the same reactive molecule, H2O2, would provide helpful data to understand this conflict. However, due to technical problems we couldn’t widen our assay spectrum.
In our study, NOX levels of brain cortex homogenates first increased with 120 min of HBO exposure. Nevertheless the courses of TBARS, SOD and NOX were found to be in correlation with each other, whereas GSH-Px appeared uncorrelated. This estimated relation seems to designate an interesting point: HBO exposure first causes an overproduction of \( {\text{O}}^{{ \cdot - }}_{{\text{2}}} \) which have to be scavenged via SOD [22]. The second-step reaction with SOD results with H2O2 formation and GSH-Px and catalase (not detected in our study) are the antioxidant enzymes responsible to fight against this reactive molecule. Insufficient amounts or function of these enzymes will result with hydroxyl radical production leading to oxidative stress. From the other point of view, NO is another molecule known and reported to play role in HBO-triggered oxidative action. Interestingly, NO competes with SOD to react with \( {\text{O}}^{{ \cdot - }}_{{\text{2}}} \); this reaction leads to peroxynitrite formation, a highly reactive molecule with the ability to damage almost all organic macromolecules resulting with enhanced oxidative stress. The correlation between NOX, SOD, and TBARS outcome of our study reflects the idea that at the level of 30 min HBO exposure SOD was sufficiently able to scavenge \( {\text{O}}^{{ \cdot - }}_{{\text{2}}} \) produced, and therefore GSH-Px production also increased for its H2O2-degrading function. Then, GSH-Px activity trended to decline, which may indicate increasing production of NO and so peroxynitrite; however, the pressure-related increase of TBARS levels support this guess, whereas NO measurement only found to be increased at the 2 h exposure level.
Indeed, NO response to HBO exposure presents conflicting results in literature. Thom et al. reported an increase of NO production in the rat brain with all partial oxygen pressures above that of ambient air [46, 47]. They defined that this result was more dependent to neuronal nitric oxide synthase (nNOS) which was activated via different ways: the altered redox status or intracellular calcium entry [47]. On the contrary, studies of Demchenko et al. reported NO and cerebral blood flow (CBF) first to decrease (up to 75 min at 3 ATA, 60 min at 4 ATA and 30 min at 5 ATA) which is then switched to an increased state leading to hyperoxic convulsions [48–50]. In those studies, they stated that the early vasoconstrictive phase is endothelial NOS (eNOS) dependent, whereas the late vasodilatative and toxic stage depends on both eNOS and nNOS [49, 50]. Another study, performed with 3 ATA HBO for 2 h, reported increased l-Arginine levels indicating decreased NO production in the rat brain [51]. Our newly published study agrees with this statement [52], however, another study of our team [39] and the present one resulted on the opposite side with increased NO levels. From this point of view, the HBO exposure procedure of 3 ATA for 2 h seems to be a critic level for the switching point of vasoconstrictive to vasodilatative state reported by Demchenko et al. [48–50]. We suggest that the exact level of this shift may vary from study to study due do several unpredictable factors. Additionally, the sensitivity of the Griess reaction may also be a reason for this puzzling outcome. Of course, direct measurement of \( {\text{O}}^{{ \cdot - }}_{{\text{2}}} \), NO and peroxynitrite would be able to lighten this matter, but as mentioned above, technical problems of our laboratory have limited the study.
As result, in our study, TBARS and SOD levels presented a linear graphic tending to increase continuously with incremental exposure time which is almost found to be mutually correlated. Additionally, the step from 90 to 120 min reflected a special importance for all measured parameters, except GSH-Px. Similarly, our previous work reporting the pressure-related effects of HBO demonstrated that increasing the exposure pressure from 2.5 to 3 ATA produced the most pronounced rise of TBARS in several rat tissues [21]. Taken together, the upper limits of the clinically approved maximal pressure/duration range, namely 3 ATA pressure and 2 h duration [1], presented the highest oxidative effects reflected with TBARS, SOD, and NOx measurement in brain cortex tissue of rats. Both the duration step from 90 to 120 min and raising the pressure from 2.5 to 3 ATA resulted with pronounced action. Since the common used ranges are varying from 1.5 to 2.5 ATA pressure for 60–90 min duration [1], the outcome of this study supports the safety of the therapeutic use of HBO. Further molecular studies, focused on the possible transcriptional/translational properties of HBO which will be compared with several antioxidant treatments are planned to elucidate the basics of HBO’s effects.
References
Feldmeier JJ (2003) Hyperbaric oxygen: indications and results; the hyperbaric oxygen therapy committee report. Undersea & Hyperbaric Medical Society, Kensington, MD
Buras JA, Stahl GL, Svoboda KK et al (2003) Hyperbaric oxygen downregulates ICAM-1 expression induced by hypoxia and hypoglycemia: the role of NOS. Am J Physiol Cell Physiol 278:C292–C302
Bonomo SR, Davidson JD, Yu Y et al (1998) Hyperbaric oxygen as a signal transducer: upregulation of platelet derived growth factor-beta receptor in the presence of HBO2 and PDGF. Undersea Hyperb Med 25:211–216
Kang TS, Gorti GK, Quan SY et al (2004) Effect of hyperbaric oxygen on the growth factor profile of fibroblasts. Arch Facial Plast Surg 6:31–35
Sakoda M, Ueno S, Kihara K et al (2004) A potential role of hyperbaric oxygen exposure through intestinal nuclear factor-kappaB. Crit Care Med 32:1722–1729
Partington JR (1957) A short history of chemistry, 3rd edn. Macmillan, London
Bert P (1978) La pression barométrique, recherches e physiologie expérimentale. Masson, Paris
Jamieson D, Vandenbrenk HA (1964) The effects of antioxidants on high pressure oxygen toxicity. Biochem Pharmacol 13:159–164
Saltzman HA, Fridovich I (1973) Oxygen toxicity. Introduction to a protective enzyme: superoxide dismutase. Circulation 48:921–923
Freeman B, Crapo JD (1981) Hyperoxia increases oxygen radical production in rat lungs and lung mitochondria. J Biol Chem 256:10986–10992
Jamieson D (1991) Lipid peroxidation in brain and lungs from mice exposed to hyperoxia. Biochem Pharmacol 41:749–756
Chavko M, Auker CR, McCarron RM (2003) Relationship between protein nitration and oxidation and development of hyperoxic seizures. Nitric Oxide 9:18–23
Yusa T, Beckman JS, Crapo JD et al (1987) Hyperoxia increases H2O2 production by brain in vivo. J Appl Physiol 63:353–358
Torbati D, Church DF, Keller JM et al (1992) Free radical generation in the brain precedes hyperbaric oxygen-induced convulsions. Free Radic Biol Med 13:101–106
Narkowicz CK, Vial JH, McCartney PW (1993) Hyperbaric oxygen therapy increases free radical levels in the blood of humans. Free Radic Res Commun 19:71–80
Elayan IM, Axley MJ, Prasad PV et al (2000) Effect of hyperbaric oxygen treatment on nitric oxide and oxygen free radicals in rat brain. J Neurophysiol 83:2022–2029
Droge W (2002) Free radicals in the physiological control of cell function. Physiol Rev 82:47–95
Hink J, Jansen E (2001) Are superoxide and/or hydrogen peroxide responsible for some of the beneficial effects of hyperbaric oxygen therapy? Med Hypotheses 57:764–769
Thom SR, Elbuken ME (1991) Oxygen-dependent antagonism of lipid peroxidation. Free Radic Biol Med 10:413–426
Kindwall EP, Gottlieb LJ, Larson DL (1991) Hyperbaric oxygen therapy in plastic surgery: a review article. Plast Reconstr Surg 88:898–908
Oter S, Korkmaz A, Topal T et al (2005) Correlation between hyperbaric oxygen exposure pressures and oxidative parameters in rat lung, brain, and erythrocytes. Clin Biochem 38:706–711
Oury TD, Ho YS, Piantadosi CA et al (1992) Extracellular superoxide dismutase, nitric oxide and central nervous system O2 toxicity. Proc Natl Acad Sci USA 89:9715–9717
Bitterman N, Bitterman H (1998) L-Arginine-NO pathway and CNS oxygen toxicity. J Appl Physiol 84:1633–1638
Torreilles J (2001) Nitric oxide: one of the more conserved and widespread signaling molecules. Front Biosci 6:D1161–D1172
Zhilyaev SY, Moskvin AN, Platonova TF et al (2003) Hyperoxic vasoconstriction in the brain is mediated by inactivation of nitric oxide by superoxide anions. Neurosci Behav Physiol 33:783–787
Lowry OH, Rosebrough NJ, Farr AL et al (1951) Protein measurement with the folin-phenol reagent. J Biol Chem 193:265–275
Ohkawa H, Ohshi N, Yagi K (1979) Assay or lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Sun Y, Oberley LW, Ying L (1988) A simple method for clinical assay of superoxide dismutase. Clin Chem 34:497–500
Paglia DE, Valentine WN (1967) Studies on the quantitative and qualitative characterisation of erythrocyte glutathione peroxidase. J Lab Clin Med 70:158–169
Moshage H, Kok B, Huizenga JR et al (1995) Nitrite and nitrate determinations in plasma: a critical evaluation. Clin Chem 41:892–896
Yildiz S, Aktas S, Cimsit M et al (2004) Seizure incidence in 80,000 patient treatments with hyperbaric oxygen. Aviat Space Environ Med 75:992–994
Jenkinson SG, Jordan JM, Lawrence RA (1988) BCNU-induced protection from hyperbaric hyperoxia: role of glutathione metabolism. J Appl Physiol 65:2531–2536
Jenkinson SG, Jordan JM, Duncan CA (1989) Effectes of selenium deficiency on glutathione-induced protection from hyperbaric hyperoxia in rat. Am J Physiol 257:L393–L398
Harabin AL, Braisted JC, Flynn ET (1990) Response of antioxidant enzymes to intermittent and continuous hyperbaric oxygen. J Appl Physiol 69:328–335
Boadi WY, Kerem D, Yannai S (1991) Effect of dietary factors on antioxidant enzymes in rats exposed to hyperbaric oxygen. Vet Hum Toxicol 33:105–109
Topal T, Oter S, Korkmaz A et al (2004) Exogenously administered and endogenously produced melatonin reduce hyperbaric oxygen-induced oxidative stress in rat lung. Life Sci 75:461–467
Dundar K, Topal T, Ay H et al (2005) Protective effects of exogenously administered or endogenously produced melatonin on hyperbaric oxygen-induced oxidative stress in the rat brain. Clin Exp Pharmacol Physiol 32:926–930
Mollaoglu H, Topal T, Ozler M et al (2007) Antioxidant effects of melatonin in rats during chronic exposure to hyperbaric oxygen. J Pineal Res 42:50–54
Ay H, Topal T, Ozler M et al (2007) Persistence of hyperbaric oxygen-induced oxidative effects 3 after exposure in rat brain cortex tissue. Life Sci 80:2025–2029
Ay H, Topal T, Uysal B et al (2007) Time-dependent course of hyperbaric oxygen-induced oxidative effects in rat lung and erythrocytes. Clin Exp Pharmacol Physiol 34:787–791
Muth CM, Glenz Y, Klaus M et al (2004) Influence of an orally effective SOD on hyperbaric oxygen-related cell damage. Free Radic Res 38:927–932
Freiberger J, Coulombe K, Suliman H et al (2004) Superoxide dismutase responds to hyperoxia in rat hippocampus. Undersea Hyperb Med 31:227–232
Freiberger JJ, Suliman HB, Sheng H et al (2006) A comparison of hyperbaric oxygen versus hypoxic cerebral preconditioning in neonatal rats. Brain Res 1075:213–222
Puglia CD, Loeb GA (1984) Influence of rat brain superoxide dismutase inhibition by diethyldithiocarbamate upon the rate of development of central nervous system oxygen toxicity. Toxicol Appl Pharmacol 75:258–264
Pablos MI, Reiter RJ, Chuang JI et al (1997) Acutely administred melatonin reduces oxidative damage in lung and brain induced by hyperbaric oxygen. J Appl Physiol 83:354–358
Thom SR, Fisher D, Zhang J et al (2003) Stimulation of perivascular nitric oxide synthesis by oxygen. Am J Physiol Heart Circ Physiol 284:H1230–H1239
Thom SR, Bhopale V, Fisher D et al (2002) Stimulation of nitric oxide synthase in cerebral cortex due to elevated partial pressures of oxygen: an oxidative stress response. J Neurobiol 51:85–100
Demchenko IT, Boso AE, O’Neill TJ et al (2000) Nitric oxide and cerebral blood flow responses to hyperbaric oxygen. J Appl Physiol 88:1381–1389
Demchenko IT, Boso AE, Whorton AR et al (2001) Nitric oxide production is enhanced in rat brain before oxygen-induced convulsions. Brain Res 917:253–261
Demchenko IT, Atochin DN, Boso AE et al (2003) Oxygen seizure latency and peroxynitrite formation in mice lacking neuronal or endothelial nitric oxide synthases. Neurosci Lett 344:53–56
Ito T, Yufu K, Mori A et al (1996) Oxidative stress alters arginine metabolism in rat brain: effect of sub-convulsive hyperbaric oxygen exposure. Neurochem Int 29:187–195
Akgul EO, Cakir E, Ozcan O et al (2007) Pressure-related increase of asymmetric dimethylarginine caused by hyperbaric oxygen in the rat brain: a possible neuroprotective mechanism. Neurochem Res DOI: 10.1007/s11064-007-9363-4
Acknowledgments
This work was supported by the ‘Gulhane Military Medical Academy Research and Progress Center’ with the grant AR–2005/25. The preliminary outcome of the study was previously presented at the ‘32nd National Congress on Physiological Sciences’ (18–22 September, Denizli, Turkey; in Turkish), and at the ‘1st Ion Channels and Oxidative Stress Congress’ (14–16 September, Isparta, Turkey).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Korkmaz, A., Öter, S., Sadir, S. et al. Exposure Time Related Oxidative Action of Hyperbaric Oxygen in Rat Brain. Neurochem Res 33, 160–166 (2008). https://doi.org/10.1007/s11064-007-9428-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-007-9428-4