Abstract
The aim of this study was designed to investigate the possible beneficial effects of Nigella sativa (NS) and thymoquinone (TQ) on histopathological changes of sciatic nerves in streptozotocin-induced diabetic rats. The rats were randomly allotted into one of four experimental groups: A (control), B (diabetic untreated), C (diabetic treated with NS) and D (diabetic treated with TQ); each group contain ten animals. B, C and D groups received streptozotocin (STZ) to induce diabetes. The rats in NS and TQ treated groups were given NS (in a dose of 400 mg/kg body weight) and TQ (50 mg/kg body weight) once a day orally by using intra-gastric intubation for 12 weeks starting 2 days after STZ injection, respectively. Blood and tissue samples were obtained for biochemical and histopathological investigation. The treatment of both NS and TQ caused a sharp decrease in the elevated serum glucose (P < 0.01, 0.05, respectively), and an increase in the lowered serum insulin concentrations (P < 0.01, 0.05, respectively), in STZ-induced diabetic rats. STZ induced a significant decrease in the area of insulin immunoreactive β-cells (P < 0.0001). NS (P < 0.001) and TQ (P < 0.01) treatment resulted in increased area of insulin immunoreactive β-cells significantly. To date, no histopathological changes of sciatic nerves in STZ induced diabetic rats by NS and TQ treatment have been reported. In this study, histologic evaluation of the tissues in diabetic animals treated with TQ and especially NS showed fewer morphologic alterations. Myelin breakdown decreased significantly after treatment with NS and TQ. The ultrastructural features of axons also showed remarkable improvement. We believe that further preclinical research into the utility of NS and TQ may indicate its usefulness as a potential treatment on peripheral neuropathy (PN) in STZ induced diabetic rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus results in severe metabolic imbalances and pathological changes in many tissues. Oxidative stress plays an important role in the etiology of diabetes and diabetic complications [1]. Diabetics and experimental animal models exhibit high-oxidative stress due to persistent and chronic hyperglycemia, thereby deplete the activity of the antioxidative defense system and thus promote free radicals generation [2]. Such models include alloxan or streptozotocin (STZ) induced diabetic rats and mice [3].
The STZ, an antibiotic produced by Streptomyces achromogenes, is the most commonly used agent in experimental diabetes [4]. The mechanism by which STZ destroys β-cells of the pancreas and induces hyperglycaemia is still unclear. Many actions have been attributed to STZ that are similar to what has been described for the diabetogenic action of alloxan that include damage to pancreatic β-cell membranes [5] and to depletion of intra-cellular nicotinamide adenine dinucleotide in islet cells [6]. In addition, STZ has been shown to induce DNA strand breaks and methylation in pancreatic islet cells [7].
It is well known that neuropathy occurs in spontaneous and experimental diabetes being the STZ model widely used to investigate the experimental diabetic peripheral neuropathies [8–11]. Despite the failure to reproduce the widespread structural abnormalities in peripheral nerve observed in cases of established neuropathy in man, animal studies may be informative as to the changes that develop in the early stages of human diabetes [11].
Several interactive pathogenetic mechanisms of diabetic peripheral neuropathy (DPN) have been identified in both human and murine models and persistent hyperglycaemia has been regarded as a primary risk factor for neuropathy [12]. Long-term hyperglycaemia would lead to subsequent enhanced oxidative stress, increased aldose reductase (AR) activity [13], accumulation of advanced glycation end-products (AGE) [14, 15] and decreased Na+/K+-ATPase activity [16]. As a result, it could induce progressive damage to the peripheral sensory and autonomic nervous systems [17]. To date, except for rigorous glycaemic control, there are few means to affect or slow the natural progression of DPN owing to limitations of the current inadequate drug therapy [18]. Despite the challenges ahead, the future holds promise for more effective treatments for diabetes mellitus and its complications.
The black seed, Nigella sativa (NS), family Ranunculaceae has been shown to contain >30% of fixed oil and 0.4–0.45% wt./wt. of volatile oil. The volatile oil has been shown to contain 18.4–24% thymoquinone (TQ = 2-isopropyl-5-methyl-1,4-benzoquinone) and 46% monoterpenes such as p-cymene and α-piene [19]. Recently, clinical and animal studies have shown that the extracts of the black seeds have many therapeutic effects such as bronchodilatation, immunomodilative [20], antibacterial [21], hypotensive [22], antidiabetic [23, 24], hepatoprotective [23, 25], gastroprotective [26], antihistaminic and antioxidative [27] and neuroprotective [28]. TQ was isolated as the principal active ingredient from the volatile oil of NS [29]. TQ has been shown to attenuate eicosanoid generation [30], cisplatin nephrotoxicity [31], tetrachloride hepatotoxicity [32], rheumatoid arthritis [33] and gastric mucosal damage [27].
In spite of these studies, there is no available information on the effect of NS and TQ on DPN. Hence, in the present study, we compared the possible beneficial effects of NS and TQ on histopathological changes of sciatic nerves in STZ induced diabetic rats.
Experimental procedure
Plant material and extraction procedure
The NS seeds were purchased from a local herb store in Van, Turkey. Sample specimens have been kept at the Department of Histology and Embryology, Yuzuncu Yil University, Van, Turkey for future reference. The seeds of NS were powdered in a mixer. About 20 g of the powdered seeds were added to 400 ml of distilled water and extraction was carried out by steam distillation. The distillation process was continued until about 200 ml of distillate was collected. The distillate was extracted three times with chloroform. Moisture was removed by anhydrous sodium sulphate and the resultant extract was evaporated using a 40°C water bath leading to the appearance of the volatile oil. About 500 mg of the volatile oil were dissolved in 1 ml of dimethyl sulphoxide (DMSO) then 9 ml of normal saline was added to yield a concentration of 50 mg volatile oil per 1 ml solution. The oil was given once daily orally in a dose of 400 mg/kg body weight by using intra-gastric intubation for up to 12 weeks [34]. TQ was obtained from Sigma Chemical Co., St. Louis, MO, USA. It was dissolved by the initial addition of DMSO, followed by the addition of normal saline (the final concentration of DMSO was <0.5%). The solution was administered at a dose of 50 mg/kg body weight once daily by using intra-gastric intubation for up to 12 weeks [35].
Animals
Forty healthy male Wistar albino rats, weighing 220–250 g and averaging 16 weeks old were utilized in this study. They were housed in macrolon cages under standard laboratory conditions (light period 7.00 a.m. to 7.00 p.m., 21 ± 2°C, relative humidity 55%). The animals were given standard rat pellets (Murat animal food product Co., Ankara, Turkey) and tap water ad libitum.
Experimental design
The rats were randomly allotted into one of four experimental groups: A (control), B (diabetic untreated), C (diabetic treated with NS) and D (diabetic treated with TQ); each group contain ten animals. B, C and D groups received STZ (Sigma). Diabetes was induced in three groups by a single intra-peritoneal (i.p) injection of STZ (50 mg/kg, freshly dissolved in 5 mmol/l citrate buffer, pH 4.5) [23, 24]. Two days after STZ treatment, development of diabetes in three experimental groups was confirmed by measuring blood glucose levels in a tail vein blood samples. Rats with blood glucose levels of 250 mg/dl or higher were considered to be diabetic. Serum glucose levels in control animals remained normal for the duration of the study. Diabetes mellitus was confirmed by Ames One Touch Glucometer (LifeScan, Johnson and Johnson, New Brunswick, NJ, USA). Control rats were injected with the same volume of isotonic NaCl as the diabetic animals that received STZ. The rats in NS and TQ treated groups were given NS (in a dose of 400 mg/kg body weight) and TQ (50 mg/kg body weight) once a day orally by using intra-gastric intubation for 12 weeks starting 2 days after STZ injection, respectively. Control and diabetic untreated rats were injected with the same volume of isotonic NaCl as the diabetic treated animals that received NS and TQ. The initial and final body weight changes of the various groups were recorded. All animals received humane care according to the criteria outlined in the “Guide for the Care and Use of Laboratory Animals” prepared by the National Academy of Sciences and published by the National Institutes of Health.
Biochemical analysis
At the end of the experiment, rats were fasted overnight for 12 h, and sacrificed under chloralhydrate (6 ml of 7% chloralhydrate kg, Sigma) anaesthesia. Blood samples were collected by cardiac puncture using a heparinized syringe. Serum glucose was determined by the hexokinase method with reagents from Boehringer, Mannheim, Germany [36]. Insulin was determined using a double-antibody radioimmunoassay kit (Amersham Radiochemical Centre, Bucks, UK) [37].
Histopathological procedures
Biopsies from the pancreatic and sciatic nerves tissues of the rats were harvested and tissue fragments were fixed in 10% neutral buffered formalin solution, embedded in paraffin and then stained with hematoxylin and eosin (H&E). The preparations were evaluated by means of a bright-field microscope and photographed (Optiphot 2; Nikon, Tokyo, Japan).
Immunohistochemical procedures
Biopsies from the pancreatic and sciatic nerves tissues of the rats were harvested and tissue fragments were fixed in 10% neutral buffered formalin solution, embedded in paraffin and sectioned at 5 μm thickness. Immunocytochemical reactions were performed according to the ABC technique described by Hsu et al. [38]. The procedure involved the following steps: (1) endogenous peroxidase activity was inhibited by 3% H2O2 in distilled water for 30 min; (2) the sections were washed in distilled water for 10 min; (3) nonspecific binding of antibodies was blocked by incubation with normal goat serum (DAKO X 0907, Carpinteria, CA, USA) with PBS, diluted 1:4; (4) the sections were incubated with specific monoclonal mouse antisera against human insulin protein (18-0066; Zymed, San Francisco, CA, USA), diluted 1:50 for 1 h and then kept at room temperature; (5) the sections were washed in PBS for 3 × 3 min; (6) the sections were incubated with ABC complex (DAKO LSAB 2 Kit); (7) the sections were washed in PBS for 3 × 3 min; (8) peroxidase was detected with an aminoethylcarbazole substrate kit (AEC kit; Zymed Laboratories); (9) the sections were washed in tap water for 10 min and then dehydrated; (10) nuclei were stained with hematoxylin; and (11) the sections were mounted in DAKO paramount.
Electron microscopy
For electron microscopy, sciatic nerves specimens were fixed with 2.5% glutaraldehyde in 0.1 M sodium phosphate buffer (pH 7.2) for 3 h at 4°C, washed in the same buffer for 1 h at 4°C and post-fixed with 1% osmium tetraoxide in sodium phosphate buffer for 1 h at 4°C. The tissues were then dehydrated in graded series of ethanol starting at 50% each step for 10 min and, after two changes in propylene oxide. The tissue specimens were embedded in araldite. Ultrathin sections were prepared with Mg-uranyl acetate and lead citrate for the electron microscopic (Jeol JEM 1010) evaluation. Some specimens were sliced into semithin (1 μm) cross-sections and stained with toluidine blue. Six different images from each specimen were taken to calculate myelinated fibre area and density using an image analysis system (Image-Pro Plus 5.0, Media Cybernetics, Silver Spring, MD, USA). The investigator was blind to group identity during the morphometry process.
Image analysis
The system used consisted of a PC with hardware and software for image acquisition and analysis, a Spot Insight QE (Diagnostic Instruments, Silver Spring, MD, USA) camera, and an optical microscope. The method requires preliminary software procedures involving spatial calibration (on a micron scale) and setting of colour segmentation for quantitative colour analysis. Ten Langerhans islets from each rat (100 islets for each group) were chosen randomly. The intensity of staining with antiinsulin antibodies of β-cells in pancreatic islets of control, diabetic untreated, diabetic treated with NS and diabetic treated with TQ groups were scored as 0 (absent), 1 (weak), 2 (moderate), 3 (strong), or 4 (very strong) in image analysis system. Then the percentage of the insulin immunoreactive β-cell area in the Langerhans islets (100 islets for each group) was estimated. The percentage of the insulin immunoreactive β-cells was calculated according to these results. The investigator who obtained these measurements was unaware of the experiment being performed.
Statistical analysis
The data were expressed as the mean ± standard deviation (SD), and analysed by repeated measures of variance. A Tukey test was used to test for differences among means when an analysis of variance (ANOVA) indicated a significant (P < 0.05) F ratio. For the analysis of the immunohistochemical data, a nonparametric test (Kruskal–Wallis) was used. Differences were considered statistically significant when the P < 0.05.
Results
Biochemical findings
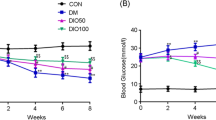
Blood glucose and serum insulin levels of experimental animals are shown in Table 1. The diabetic animals exhibited consistently hyperglycaemia (P < 0.01) and insulin deficiency (P < 0.001). The treatment of both NS and TQ caused a sharp decrease in the elevated serum glucose (P < 0.01, 0.05, respectively), and an increase in the lowered serum insulin concentrations (P < 0.01, 0.05, respectively) (Table 1) in STZ induced diabetic rats.
The baseline weights of the rats at the beginning of the study were similar in all groups. At the end of the treatment, diabetic animals presented weight loss. The initial and final body weights were not different in control rats and NS and TQ-treated diabetic rats (Table 1).
Immunohistochemical findings
Immunohistochemical labelling of the pancreatic tissues of control rats revealed strong insulin antigen positivity in the β-cells of the islets (Fig. 1a). In diabetic untreated rats, the cells were essentially negative for insulin-immunoreactivity and only a few β-cells in some islets displayed slight insulin-immunopositivity in small granules (P < 0.0001) (Fig. 1b). In diabetic rats with NS treatment, both the number of insulin-immunoreactive β-cells and the immunopositivity of their granules increased in comparison to that seen in diabetic untreated rats (P < 0.001) (Fig. 1c) and diabetic treated with TQ (P < 0.01) (Fig. 1d) (Table 2). The percentage of the insulin immunoreactive β-cells area was calculated and results are shown in Table 3. STZ induced a significant decrease in the area of insulin immunoreactive β-cells (P < 0.0001). NS (P < 0.001) and TQ (P < 0.01) treatment resulted in increased area of insulin immunoreactive β-cells significantly.
(a) Control group showing β-cells in the islet of Langerhans that are strongly stain with the antiinsulin antibody. (b) In the islets of Langerhans of diabetic rats, β-cells are almost negative for insulin-immunoreactivity. (c) and (d) The numbers of insulin-immunoreactive granules in β-cells of diabetic rats with NS treatment increased in comparison to that seen in diabetic rats treated with TQ (Immunoperoxidase, haematoxylin counterstain, scale bar 50 μm)
Histopathologic changes
The mean myelinated fibre area was decreased in diabetic rats (34.6 ± 4.8) compared with nondiabetic rats (55.4 ± 6.2) and these changes were alleviated by NS (48.3 ± .1) and TQ (41.7 ± .7). In contrast, the mean fibre density was increased in diabetic rats (19.8 ± .25) compared with nondiabetic rats (10.3 ± .9), but the increase was inhibited by NS (13.2 ± .1) and TQ (16.3 ± .7) administration (P < 0.05 or 0.01; Table 4).
In control rats, histology of sciatic nerves was normal (Fig. 2a). An increase of the connective tissue was seen around the epineurium (Fig. 2b) in diabetic rats, whereas the mass of connective tissue of sciatic nerves was markedly reduced in TQ (Fig. 2d) and especially NS treated groups (Fig. 2c).
Representative light microphotographs showing the sciatic nerve. (a) Control rats: normal connective tissue without fibrosis around the epineurium is seen. (b) Diabetic neuropathy rats: an increase of the connective tissue with fibrosis is seen around the epineurium (arrow head). (c) Diabetic neuropathy rats treated NS: light fibrosis are seen around the epineurium (arrow head). (d) Diabetic neuropathy rats treated TQ: mild fibrosis (arrow head) is seen around the epineurium. H&E, scale bar 100 μm
Electron microscopic findings
Ultrastructural examination of the sciatic nerves in control group showed normal structure (Fig. 3a). Sciatic nerve electronmicrograph of diabetic rats shows myelin destructions with onion-bulb and bubble form protrusion on the myelin sheath and axolemma border of myelinated axons. The most striking morphologic changes of the axonal myelins were vacuolization and lamellar seperation. Shrunken and swollen axons were common. Total damage and deformation of the axons was evident in some nerve fibres. Degenerative changes were also observed in Schwann cells. There were vacuolization in the cytoplasm of these cells. In the endoneural areas among the myelinated and unmyelinated axons there were seen abundant collagen fibres. Fibre degeneration was associated with endoneurial edema. Collagen fibres among the myelinated fibres were less than surrounding unmyelinated axons. Unmyelinated fibres were relatively normal (Fig. 3b). Histologic evaluation of the tissues in animals pretreated with TQ and especially NS showed fewer morphologic alterations. Myelin breakdown decreased markedly after treatment with TQ (Fig. 3d), but to lesser extent than NS (Fig. 3c). Likewise, ultrastructural features of myelin and axons showed remarkable improvement. Vacuolization and lamellar seperation of the axonal myelin was less obvious. The fine structure of Schwann cells was seemingly normal. Collagen fibres and endoneurial edema were also less in NS and TQ groups as compared with the diabetic rats (Fig. 3c, d).
Representative transmission electron micrographs showing the ultrastructure of sciatic nerves. (a) Control rats: intact myelinated axon. (b) Diabetic neuropathy rats: serious demyelination (arrow head) is seen, with entire axon separation from sheaths (asterisk). In the endoneural edema areas among the myelinated and unmyelinated axons there were seen abundant collagen fibres. (c) Diabetic neuropathy rats treated with NS: tiny segmental demyelination and local axon separation from sheaths (asterisk) is seen. Collagen fibres and endoneurial edema were also less obvious. (d) Diabetic neuropathy rats treated with TQ: mild axon separation from the sheaths (asterisk) is seen. Collagen fibres and endoneurial edema were relatively less (m myelin, a axon, e endoneural edema, c collagen fibres). Scale bar 1 μm
Discussion
In the current study, we compared the possible beneficial effects of NS and TQ on PN in STZ induced diabetic rats. DPN is a multifactorial disorder, attributable to the reversible metabolic consequences of hyperglycaemia, insulin deficiency, or both [12] that are thought to induce further neurochemical, neurotrophic, or neurovascular defects in the peripheral nervous system. Accumulating evidence implicates increased oxidative stress [39–42] and alterations in glucose-sensitive signal transduction pathways [43] in the pathogenesis of experimental diabetic neuropathy. Hyperglycaemia is proposed to promote oxidative stress and generate reactive oxygen species (ROS). In turn, increased ROS are directly neurotoxic, promoting neuronal apoptosis [44, 45], and may inhibit mitochondrial respiratory enzymes, leading to deficits of nerve energy production and nerve functional deficits. Insulin deficiency can also promote alterations in fatty acid metabolism [46], limiting the formation of arachidonate [46], and thereby perturbing the production of vasodilating eicosanoids including prostacyclin [47] and prostaglandin (PG) E1 [48]. In the nerve, increased oxidative stress [49, 50], and nerve hypoxia [51].
Peripheral neuropathy, associated with diabetes, neurotoxic chemotherapy, human immunodeficiency virus (HIV)/antiretroviral drugs, alcoholism, nutrient deficiencies, heavy metal toxicity and other etiologies, results in significant morbidity. Diabetes results in increased products of oxidation. In hyperglycaemia, glucose combines with protein, yielding glycosylated proteins, which can become damaged by free radicals and combine with fats, yielding AGEs that damage sensitive tissues. In addition, glycosylation of antioxidant enzymes can render the defense system less efficient. Significant evidence points to increased oxidative stress in DPN, either because of enhanced production of ROS or defective scavenging of free radicals. Conventional pain medications primarily mask symptoms and have significant side effects and addiction profiles. However, a widening body of research indicates alternative medicine may offer significant benefit to this patient population. Alpha-lipoic acid, acetyl-l-carnitine, benfotiamine, methylcobalamin and topical capsaicin are among the most well researched alternative options for the treatment of PN [52]. The pathology of diabetic neuropathy also involves polyol pathway flux, oxidative stress, AGE and microvascular injuries. Polyol pathway flux activated by hyperglycaemia plays an important role in diabetic neuropathy and other tissues prone to diabetic complications [53].
It has been reported that at week 12, rats with STZ induced diabetes exhibited symptoms of diabetes and diabetic complications, including peripheral sensory nerve injury. Moreover, clinical data have shown that up to 100% of diabetic patients suffering PN manifest electrophysiological conduction abnormalities [54]. In an experiments, diabetic rats treated with bendazac lysine (BDL) and epalrestat exhibited amelioration of the changes in pathological morphology of myelinated nerve fibres. Therapy with an AR inhibitor has been reported to correct peripheral nerve defects, such as improving slowed motor nerve conduction velocity, increasing nerve blood flow and preventing structural nerve fibre damage [55]. In diabetic models, BDL exhibited dose-dependent inhibitory effects on AR [56]. Animal studies also confirm the benefit of benfotiamine for neuropathy in a rat model of DPN [57, 58]. One study comparing the effect of water-soluble thiamine with lipid-soluble benfotiamine found benfotiamine superior in preventing functional nerve damage and preventing formation of AGEs—a cause of DPN [58]. In STZ induced diabetic rats, methylcobalamin resulted in decreased demyelination and protection of nerve fibre density and size. The rats were administered intra-muscular methylcobalamin at a very high-daily dose of 500 mcg/kg body weight for 16 weeks [59]. An in vitro study helps to illuminate a possible mechanism for pyridoxine in the prevention of DPN. Both pyridoxine and its intermediate metabolite pyridoxamine were found to inhibit free radical formation, lipid peroxidation, and protein glycosylation, and protect (Na+/K+)-ATPase activity—all mechanisms involved in DPN—in red blood cells exposed to high-glucose concentrations [60].
Among pathogenetic factors associated with diabetic neuropathy, hyperglycaemia may be the trigger for biochemical dysfunction leading to the development of DPN. Persistent hyperglycaemia also brings about an abatement of insulin secretion and insulin resistance of peripheral tissues, which further worsens the control of blood glucose levels in diabetes [61, 62]. TQ and especially NS ameliorated blood glucose and insulin levels in the present study, in accordance with data reported previously [34, 35]. This indicates that NS and TQ affects blood glucose levels, and insulin. We deduced that the antioxidant activity of NS may alleviate damage to β-cells in the pancreas caused by STZ, so that the condition in NS-treated diabetic rats in the present study, including the secretion of insulin and hyperglycaemia levels in the serum, was better than that of the TQ group.
In our previous study [28], we found that NS has some neuroprotective and restorative effects on secondary pathochemical events after spinal cord injury in rats. These restorative effects mainly observed on oxidative stress and neuronal numbers and neuronal morphology. But to date, no biochemical and histopathological changes of sciatic nerves in STZ induced diabetic rats by NS and TQ treatment have been reported. In this study, histologic evaluation of the tissues in diabetic animals treated with TQ and especially NS showed fewer morphologic alterations. Myelin breakdown decreased significantly after treatment with TQ, but to lesser extent than NS. Vacuolization and lamellar seperation of the axonal myelin was less obvious in NS group. Collagen fibres and endoneurial edema were also less in NS group as compared with the TQ treated diabetic rats.
As in previous studies [63, 64], the weight gain of the diabetic rats was significantly decreased as compared with that of the control animals. This is caused by a decreased availability of glucose and amino acids to cells, creating a shortage of substrates for cellular biosynthesis and affecting related cellular metabolism [64]. Dietary supplementation with 10 and 20% xylitol in the diabetic rats led to increased body weight as compared with the diabetic rats without xylitol. This is most likely a consequence of the ability of diabetic animals to use xylitol as a substrate in energy metabolism [65]. Likewise, in our previous study [24], NS and TQ treated rats had normal weight comparable to that of normal rats.
In summary, we conclude that TQ and especially NS therapy causes biochemical and morphologic improvement on sciatic nerves which have been subjected to STZ exposure. We postulate that the neuroprotective effects of TQ and especially NS are attributed to its direct and indirect antioxidant actions. We believe that further preclinical research into the utility of NS and TQ may indicate its usefulness as a potential treatment on PN in STZ induced diabetic rats.
References
Thorpe SR, Baynes JW (1996) Role of the Maillard reaction in diabetes mellitus and diseases of aging. Drugs Aging 9(2):69–77
Baynes JW (1991) Role of oxidative stress in development of complications in diabetes. Diabetes 40:405–412
Gillery P, Monboisse JC, Maquart FX, Borel JP (1989) Does oxygen free radical increased formation explain long term complications of diabetes mellitus? Med Hypotheses 29(1):47–50
Rakieten N, Rakieten ML, Nadkarni MV (1963) Studies on the diabetogenic action of streptozotocin. Cancer Chemother Rep 29:91–98
Bhattacharya G (1954) On the protection against alloxan diabetes by hexoses. Science 120:841–843
Schein PS, Cooney DA, McMenamin MG, Anderson T (1973) Streptozotocin diabetes—further studies on the mechanism of depression of nicotinamide adenine dinucleotide concentrations in mouse pancreatic islets and liver. Biochem Pharmacol 15:2625–2631
Matkovics B, Kotorman M, Varga IS, Hai DQ, Varga C (1997–1998) Oxidative stress in experimental diabetes induced by streptozotocin. Acta Physiol Hung 85:29–38
Jakobsen J, Lundbaek K (1976) Neuropathy in experimental diabetes: an animal model. Br Med J 2:278–279
Jakobsen J (1979) Early and preventable changes of peripheral nerve structure and function in insulin-deficient diabetic rats. J Neurol Neurosurg Psychiatry 42:509–518
Sharma AK, Thomas PK, De Molina AF (1977) Peripheral nerve fiber size in experimental diabetes. Diabetes 26:689–692
Sharma AK, Duguid IG, Blanchard DS, Thomas PK (1985) The effect of insulin treatment on myelinated nerve fiber maturation and integrity and on body growth in streptozotocin diabetic rats. J Neurol Sci 67:285–297
The Diabetes Control, Complications Trial Research Group (1995) The effect of intensive diabetes therapy on thedevelopment and progression of neuropathy in the Diabetes Control and Complications Trial. Ann Int Med 122:561–568
Cameron NE, Cotter MA, Basso M, Hohman TC (1997) Comparison of theeffects of inhibitors of aldose reductase and sorbitol dehydrogenase on neurovascular function, nerve conduction and tissue polyol pathway metabolites in streptozotocin-diabetic rats. Diabetologia 40:271–281
Karachalias N, Babaei-Jadidi R, Ahmed N, Thornalley PJ (2003) Accumulation of fructosyl-lysine and advanced glycation end products in the kidney, retina and peripheral nerve of streptozotocin-induced diabetic rats. Biochem Soc Trans 31:1423–425
Gries AF (1995) Alternative therapeutic principles in the prevention of microvascular and neuropathic complications. Diabetes Res Clin Pract 28(Suppl):S201–S207
Vague P, Coste TC, Jannot MF, Raccah D, Tsimaratos M (2004) C-Peptide Na+,K+-ATPase and diabetes. Exp Diabesity Res 5:37–50
Babaei-Jadidi R, Karachalias N, Ahmed N, Battah S, Thornalley PJ (2003) Prevention of incipient diabetic nephropathy by high-dose thiamine and benfotiamine. Diabetes 52:2110–2120
The St Thomas’ Diabetic Study Group (1986) Failure of improved glycaemic control to reverse diabetic autonomic neuropathy. Diabet Med 3:330–4
El-Tahir KE, Ashour MM, Al-Harbi MM (1993) The respiratory effects of the volatile oil of the black seed (Nigella sativa) in guinea-pigs: elucidation of the mechanism(s) of action. Gen Pharmacol 24:1115–1122
El-Kadi A, Kandil O (1987) The black seed (Nigella sativa) and immunity: its effect on human T cell subset. Fed Proc 46:1222
Hanafy MSM, Hatem ME (1991) Studies on the antimicrobial activity of Nigella sativa seed (black cumin). J Ethnopharmacol 34:275–278
Zaoui A, Cherrah Y, Lacaille-Dubois MA, Settaf A, Amarouch H, Hassar M (2000) Diuretic and hypotensive effects of Nigella sativa in the spontaneously hypertensive rat. Therapy 55:379–382
Kanter M, Meral I, Yener Z, Ozbek H, Demir H (2003) Partial regeneration/proliferation of the ß-cells in the islets of Langerhans by Nigella sativa L. in streptozocin-induced diabetic rats. Tohoku J Exp Med 20:213–219
Kanter M, Coskun O, Korkmaz A, Oter S (2004) Effects of Nigella sativa on oxidative stress and ß-Cell damage in streptozocin-induced diabetic rats. Anat Rec 279:685–691
Kanter M, Coskun O, Budancamanak M (2005) Hepatoprotective effects of Nigella sativa L and Urtica dioica L on lipid peroxidation, antioxidant enzyme systems and liver enzymes in carbon tetrachloride-treated rats. World J Gastroenterol 11(42):6684–6688
Kanter M, Demir H, Karakaya C, Ozbek H (2005) Gastroprotective activity of Nigella sativa L oil and its constituent, thymoquinone against acute alcohol-induced gastric mucosal injury in rats. World J Gastroenterol 11(42):6662–6666
Kanter M, Coskun O, Uysal H (2006) The antioxidative and antihistaminic effect of Nigella sativa and its major constituent, thymoquinone on ethanol-induced gastric mucosal damage. Arch Toxicol 80(4):217–224
Kanter M, Coskun O, Kalayci M, Buyukbas S, Cagavi F (2006) Neuroprotective effects of Nigella sativa on experimental spinal cord injury in rats. Hum Exp Toxicol 25(3):127–133
Mahfouz M, El-Dakhakhny M (1960) The isolation of a crystalline active principle from Nigella sativa L. seeds. J Pharm Sci UAR 1:1–19
Houghton PJ, Zarka R, Heras B, Hoult RS (1995) Fixed oil of Nigella sativa and derived thymoquinone inhibit eicosanoid generation in leucocytes and membrane lipid peroxidation. Planta Med 61:33–36
Badary OA, Nagi MN, Al-Shabanah OA, Al-Sawaf HA, Al-Sohaibani MO, Al-Bekairi AM (1997) Thymoquinone ameliorates the nephrotoxicity induced by cisplatin in rodents and potentiates its antitumor activity. Can J Physiol Pharmacol 75:1356–1361
Al-Gharably M, Badary OA, Nagi MN et al (1997) Protective effect of thymoquinone against carbon tetrachloride-induced hepatotoxicity in mice. Res Commun Pharmacol Toxicol 2:41–50
Budancamanak M, Kanter M, Demirel A, Ocakci A, Uysal H, Karakaya C (2006) Protective effects of thymoquinone and methotrexate on the renal injury in collagen-induced arthritis. Arch Toxicol 80(11):768–776
Fararh KM, Atoji Y, Shimizu Y, Takewaki T (2002) Isulinotropic properties of Nigella sativa oil in Streptozotocin plus Nicotinamide diabetic hamster. Res Vet Sci 73:279–282
Fararh KM, Shimizu Y, Shiina T, Nikami H, Ghanem MM, Takewaki T (2005) Thymoquinone reduces hepatic glucose production in diabetic hamsters. Res Vet Sci 79:219–223
Passey RB, Gillum RF, Fuller JB, Urry FM, Giles ML (1974) Evaluation and comparison of 10 glucose methods and the reference method recommended in the proposed product class standard. Clin Chem 1977 23:131–139
Hales CN, Randle PJ (1963) Immunoassay of insulin with insulin-antibody precipitate. Biochem J 88:137–146
Hsu SM, Raine L, Fanger H (1981) Use of avidin-biotin-peroxidase complex (ABC) in immunperoxidase techniques: a comparison between ABC and unlabeled antibody (PAP) procedures. J Histochem Cytochem 29:577–580
Cameron NE, Cotter MA, Archibald V, Dines KC, Maxfield EK (1994) Anti-oxidant and pro-oxidant effects on nerve conduction velocity, endoneurial blood flow and oxygen tension in non-diabetic and streptozotocin-diabetic rats. Diabetologia 37:449–459
Tuck RR, Schmelzer JD, Low PA (1984) Endoneurial blood flow and oxygen tension in the sciatic nerves of rats with experimental diabetic neuropathy. Brain 107:935–950
Cameron NE, Cotter MA, Maxfield EK (1993) Anti-oxidant treatment prevents the development of peripheral nerve dysfunction in streptozotocin-diabetic rats. Diabetologia 36:299–304
Cameron NE, Cotter MA, Horrobin DH, Tritschler HJ (1998) Effects of alphalipoic acid on neurovascular function in diabetic rats: interaction with essential fatty acids. Diabetologia 41:390–399
Stevens MJ, Feldman EL, Thomas TP, Greene DA (1997) The pathogenesis of diabetic neuropathy. In: Veves A, Conn PMC (eds) Clinical management of diabetic neuropathy. Totowa, NJ, Humana, pp 13–47
Luo Y, Umegaki H, Wang X, Abe R, Roth GS (1998) Dopamine induces apoptosis through an oxidation-involved SAPK/JNK activation pathway. J Biol Chem 273:3756–3764
Park DS, Morris EJ, Stefanis L, Troy CM, Shelanski ML, Geller HM, Greene LA (1998) Multiple pathways of neuronal death induced by DNA-damaging agents, NGF deprivation, and oxidative stress. J Neurosci 18:830–840
Horrobin DF (1988) The roles of essential fatty acids in the development of diabetic neuropathy and other complications of diabetes mellitus. Prostaglandins Leukot Essent Fatty Acids 31:181–197
Ward KK, Low PA, Schmelzer JD, Zochodne DW (1989) Prostacyclin and noradrenaline in peripheral nerve of chronic experimental diabetes in rats. Brain 112:197–208
Subbiah MTR, Deitemeyer D (1980) Altered synthesis of prostaglandins in platelet and aorta from spontaneously diabetic Wistar rats. Biochem Med 23:231–235
Faux SP, Howden PJ (1997) Possible role of lipid peroxidation in the induction of NF-kappaB and AP-1 in RFL-6 cells by crocidolite asbestos: evidence following protection by vitamin E. Environ Health Perspect 105(Suppl 5):1127–1130
Adderley SR, Fitzgerald DJ (1999) Oxidative damage of cardiomyocytes is limited by extracellular regulated kinases 1/2-mediated induction of cyclooxygenase-2. J Biol Chem 274:5038–5046
Schmedtje JF Jr, Ji YS, Liu WL, DuBois RN, Runge MS (1997) Hypoxia induces cyclooxygenase-2 via the NF-kappaB p65 transcription factor in human vascular endothelial cells. J Biol Chem 272:601–608
Kathleen AH (2006) Peripheral neuropathy: pathogenic mechanisms and alternative therapies. Altern Med Rev 11(4):294–329
Tomlinson DR, Stevens EJ, Diemel LT (1994) Aldose reductase inhibitors and their potential for the treatment of diabetic complications. Trends Pharmacol Sci 15:293–297
Hong C (2000) Electrophysiology detection for EMG, SCV, MCV and SEP on diabetic patients suffering peripheral neuropathy. Acta Acad Med Xuzhou 20:427–428
Cameron NE, Cotter MA, Hohman TC (1996) Interactions between essential fatty acid, prostanoid, polyol pathway and nitric oxide metabolism in the neurovascular deficit of diabetic rats. Diabetologia 39:172–182
Yu JX, Yin XX, Shen JP, Qiu J, Yin HL, Jiang SJ (2006) Protective effects of bendazac lysine on diabetic peripheral neuropathy in streptozotocin-induced diabetic rats. Clin Exp Pharmacol Physiol 33:1231–1238
Sanchez-Ramirez GM, Caram-Salas NL, Rocha-Gonzalex HI, Vidal-Cantu GC, Medina-Santillan R, Reyes-Garcia G, Granados-Soto V (2006) Benfotiamine relieves inflammatory and neuropathic pain in rats. Eur J Pharmacol 530:48–53
Stracke H, Hammes HP, Werkmann D, Mavrakis K, Bitsch I, Netzel M, Geyer J, Kopcke W, Sauerland C, Bretzel RG, Federlin KF (2001) Efficacy of benfotiamine versus thiamine on function and glycation products of peripheral nerves in diabetic rats. Exp Clin Endocrinol Diabetes 109:330–336
Yagihashi S, Tokui A, Kashiwamura H, Takagi S, Imamura K (1982) In vivo effect of methylcobalamin on the peripheral nerve structure in streptozotocin diabetic rats. Horm Metab Res 14:10–13
Jain SK, Lim G (2001) Pyridoxine and pyridoxamine inhibits superoxide radicals and prevents lipid peroxidation, protein glycosylation, and (Na+ + K+)-ATPase activity reduction in high glucosetreated human erythrocytes. Free Radic Biol Med 30:232–237
Leahy J, Bonner-Weir S, Weir G (1992) Beta-cell dysfunction induced by chronic hyperglycemia: current ideas on mechanism of impairedglucose-induced insulin secretion. Diabetes Care 15:442–455
Rossetti L, Giaccari A, Defronzo R (1990) Glucose toxicity. Diabetes Care 13:610–630
Ar‘Rajab A, Ahrtn B (1993) Long-term diabetogenic effect of streptozotocin in rats. Pancreas 8:50–57
Wong KK, Tzeng ESF (1993) Appearance of different diabetic symptoms after streptotozocin administration: a comparison study. Biochem Mol Biol Int 30:1035–1041
Mattila PT, Knuuttila ML, Svanberg MJ (1998) Dietary xylitol supplementation prevents osteoporotic changes in streptozotocin-diabetic rats. Metabolism 47:578–583
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kanter, M. Effects of Nigella sativa and its Major Constituent, Thymoquinone on Sciatic Nerves in Experimental Diabetic Neuropathy. Neurochem Res 33, 87–96 (2008). https://doi.org/10.1007/s11064-007-9419-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-007-9419-5