Abstract
Lithium and valproate (VPA) are the most commonly prescribed mood-stabilizing drugs. Recently, several studies have reported their neuroprotective properties in several models of neural toxicity and, in some pathological conditions, large amounts of intracellular ATP can be released from damaged cells. In the present study, we investigate the potential neuroprotective effect of lithium and VPA against ATP-induced cell death in hippocampal slices of adult rats. Acute (in vitro) and chronic (in vivo) treatment at therapeutic doses with lithium or VPA significantly prevent the ATP-induced cell death. Lithium and VPA also exerted a synergic effect in the prevention of ATP-induced cell death. Moreover, hippocampal slices prepared from rats chronically treated with lithium or VPA presented a significant reduction in cell death in the presence of cytotoxic extracellular ATP. Although further investigations are necessary, our results show the neuroprotective effect of lithium and VPA against neuronal death induced by extracellular ATP, probably through a different pathway, and suggest novel uses of these drugs in neurogenerative diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lithium ion and valproate (VPA), a short-chain fatty acid, are commonly used mood-stabilizing drugs for bipolar disorder [1–3]. In addition, several studies have reported neuroprotective properties of mood stabilizers in several models of neural toxicity [4]; however, the biochemical basis of their therapeutic effect is poorly understood. A large number of studies, encompassing in vitro, in vivo, and clinical analyses have concluded that lithium is neuroprotective. Given the vastly different methodologies and parameters employed by these studies, the basic finding that lithium is neuroprotective is strongly supported [5]. In vitro studies have shown that lithium has neuroprotective effects in multiple cell lines, including cerebellar granule cells, cerebral cortical cells, hippocampal neurons [6], PC 12 cells [7], and neuroblastoma cells [8] from both humans and rodents. Furthermore, in vitro lithium treatment has successfully provided neuroprotection against a wide variety of insults, such as oubain [4, 9], anticonvulsants [6], potassium deprivation [10, 11], α-amino-3-hydroxy-5-methylisoxazole-4-propionate (AMPA) and kainate [12], β-amyloid peptide [13, 14], β-bungarotoxin [15], and ischemia [16].
Sodium VPA has also been reported to have neuroprotective properties, including cerebral ischemia [2, 17, 18]. VPA may have a role in the treatment of excitotoxic states in the hippocampus. Chronic treatment with VPA led to a dose-dependent increase in hippocampal glutamate uptake capacity [19]. In addition, a close similarity exists between the molecular effects of lithium compared with VPA, both showing benefits in manic-depressive illness [19].
Adenine nucleotides and nucleosides represent an important class of extracellular molecules involved in the modulation of signaling pathways that are crucial for normal functioning of the nervous system [20]. Besides the well established effects of ATP in the cell metabolism, there is evidence to show that extracellular ATP can stimulate mitogenesis and cellular proliferation or cause cytotoxic effects, depending on the cell type and the ATP concentration [21]. In some pathological conditions, large amounts of intracellular ATP can be released from damaged cells [22, 23], forming part of an important response mechanism to cell lysis, as is the case for astrocyte responses to injury in CNS. High concentrations of extracellular ATP can induce cell death in different cell types, including thymocytes, hepatocytes, microglial, and myeloid cells [24, 25].
Recently, Neary and Kang [26] reported that ATP, released upon traumatic injury, hypoxia and cell death contributes to the gliotic response by binding to specific cell surface astrocytic P2 nucleotide receptors. These authors showed that the ability of ATP to kill cells involves both necrosis and apoptosis by activation of P2X1 and P2X7 receptors. There is some evidence to indicate that the P2X7 receptor can mediate cell death by lytic pore formation in cells (independently of Ca+2) or by stimulating excessive Ca+2 influx after prolonged activation of the receptor [22].
The events induced by extracellular adenine nucleotides are controlled by the action of ecto-enzymes, which play a central role in modulating the extracellular levels of these important signaling molecules [27]. We have recently shown that chronic treatment with lithium promoted an enhancement of ATP and AMP hydrolysis in synaptossomes from the hippocampus of rats, suggesting that the purinergic system may be involved in the potential neuroprotective lithium action in hippocampal lesions [28].
Since ATP is known to be released in the extracellular milieu of the CNS, both in physiological and pathological conditions and lithium and VPA have also been reported to have neuroprotective properties, the objective of present study was to investigate the potential neuroprotective effect of treatment lithium and VPA in a model of ATP-induced cell death in hippocampal slices of adult rats.
Experimental procedures
Preparation and incubation of slices
Male Wistar rats (2 months; weighing 220–260 g) were maintained under standard conditions (12 h light/dark, 22 ± 2°C). The rats had free access to food (standard lab rat chow) and water. Procedures for the care and use of animals were adopted according to the guide for the care and use of laboratory animals (National Research Council). Rats were killed by decapitation and the brain was isolated in a modified Krebs–Henseleit solution containing (in mM): 120.0 NaCl, 2.0 KCl, 3.0 CaCl2, 25.0 Hepes, 1.2 MgSO4, 1.18 KH2PO4, 11.0 glucose (pH 7.4). The hippocampi were quickly dissected out and transverse sections (400 μm) were prepared using a Mcllwain tissue chopper. Hippocampal slices were placed into separate 24-well plates and maintained for 30 min in the same modified Krebs–Henseleit solution (incubation medium). In all experiments, the slices were incubated in a humidified atmosphere at 37°C.
Acute in vitro treatment of slices with lithium or VPA
After 30 min of pre-incubation, as described above, the medium was replaced by incubation medium containing 1.0 mM lithium or 0.5 mM VPA (these concentrations represent therapeutic blood levels in patients treated with these drugs [29]) and then maintained for 30 min at 37°C. The control group was maintained in the same conditions (without lithium or VPA). After 30 min, the medium was replaced by an incubation medium containing 5.0 mM ATP (final concentration) and the slices were maintained at 37°C for 18 h. After this time, an aliquot of the incubation medium was withdrawn and the activity of lactate dehydrogenase (LDH) was determined.
Chronic treatment of rats with lithium or VPA
Lithium
The rats were divided into two groups: one group received standard rat chow and the other group had lithium chloride (2.5 mg/g of chow) and NaCl (17 mg/g of chow) added to the food. This previously described treatment lasted for 4 weeks [30], the animals remained healthy and the serum lithium levels at the end of the period were determined by atomic absorption spectrometry. The serum lithium concentration was 1.18 ± 0.05 mEq/l (mean ± SEM, n = 18), which is in the range observed in lithium treated patients.
Valproate
A dose of 300 mg/kg of VPA [31] or saline, as a vehicle control, was injected intraperitoneally (i.p.) daily, or every 12 h for 14 days.
After chronic treatments with lithium or VPA the animals were killed by decapitation and hippocampal slices were prepared and incubated with ATP as described above.
Cell viability
The degree of cellular damage was evaluated by measuring the activity of LDH (EC 1.1.1.27) [32]. Briefly, after different times of incubation with ATP, the incubation medium was collected and LDH activity was evaluated by a colorimetric method, according to the procedure of Whitaker [33]. The results were expressed as the ratio of released activity to total activity obtained after freeze-thawing the slices (100% of cell death).
Statistical analysis
All experiments were carried out at least 6—9 times in triplicate and data are expressed as mean ± SEM Data were analyzed by unpaired ANOVA followed by post hoc comparisons (Student–Newman–Keuls test) using an Instat software package (GraphPad Software, San Diego, CA, USA).
Results
Cytolytic effect of extracellular ATP
To establish the experimental conditions of ATP-induced cell death, the slices were treated with different concentrations of ATP (0.1, 0.5, 3.0, 5.0 mM) for 24 h. The presence of 0.1 or 0.5 mM of ATP did not cause a significant increase in the LDH released when compared with control slices, while a significant increase in LDH release was observed with 3.0 or 5.0 mM of ATP (data not shown). Since extensive cell death was also observed in control slices after this long period of incubation, the subsequent experiments were performed with 5.0 mM of ATP for 18 h of treatment.
Since the ATP added to the incubation medium may be degraded by slices to its metabolites [34], we evaluated the effect of 3.0 mM of ADP, AMP or Adenosine (Ado) on cell lysis by evaluating LDH release. Figure 1 shows that ADP, AMP, and Ado did not cause a significant increase in the LDH release when compared with control slices, confirming that the cell death observed in our experiments is the consequence of ATP and not its metabolites.
Effect of ATP metabolites on cell death. The slices were prepared as described in Materials and methods and treated with 5.0 mM of ATP, 3.0 mM of ADP, 3.0 mM of AMP or 3.0 mM of Adenosine (ADO). After 18 h, the incubation medium was collected and LDH activity was measured. Leakage of LDH is represented as a percentage of the total releasable enzyme. The data are the mean ± SEM of at least six experiments run in triplicate. **Significantly different from the control group for P < 0.01 (Student–Newman–Keuls test)
Lithium and VPA prevent ATP-induced cell death
Initially, the abilities of lithium or VPA (acute in vitro treatment) to protect hippocampal slices against ATP-induced cell death were evaluated. As shown in Fig. 2a, slices pre-treated with 1.0 mM of lithium before the exposure to ATP demonstrated a significant reduction in LDH release (11 ± 5%), compared with slices treated only with 5.0 mM of ATP (57 ± 12%). Similarly, pre-treatment with 0.5 mM of VPA significantly reduced cell death to 36 ± 7% when compared with the respective control (67 ± 7%) (Fig. 2b).
Effect of pre-treatment of hippocampal slices with lithium or valproate on the ATP-induced cell death. The slices were prepared as described in Materials and methods and pre-treated: (a) with 1.0 mM of lithium (Li) or (b) 0.5 mM of valproate (VPA) for 30 min before the treatment with 5.0 mM of ATP. After 18 h, the incubation medium was collected and LDH activity was measured. Leakage of LDH is represented as a percentage of the total releasable enzyme. The data are the mean ± SEM of at least six experiments run in triplicate. ***Significantly different from the respective ATP group for P < 0.001 (Student–Newman–Keuls test)
Since the in vitro treatment with lithium or VPA significantly prevented ATP-induced cell death, we evaluated whether chronic treatment of hippocampal slices of rats with lithium or VPA (in vivo treatment) demonstrated the same protection against the cell death induced by extracellular ATP. Figure 3 shows that hippocampal slices prepared from rats chronically treated with lithium presented a significant reduction in cell death in the presence of cytotoxic extracellular ATP. This protective effect was similar after 18 and 24 h of treatment with ATP. It is important to note that slices from rats chronically treated with lithium, but not exposed to ATP, demonstrated a significant reduction in LDH release when compared with the respective controls, suggesting that lithium is also able to prevent the basal cell death that occurs during slice preparation (Fig. 3).
Effect of chronic treatment with lithium on ATP-induced cell death. Rats received standard rat chow (control group) or lithium chloride (2.5 mg/g of chow) plus NaCl (17 mg/g of chow) added to the food for 4 weeks (lithium group). Slices prepared as described in Materials and methods and, following 1, 4, 12, 18 or 24 h of treatment with 5.0 mM of ATP, the incubation medium was collected and the LDH activity was measured. Leakage of LDH is represented as a percentage of the total releasable enzyme. The data are the mean ± SEM of at least six experiments run in triplicate. The effect was statistically determined by Student–Newman–Keuls test. aSignificantly different from the control group (P < 0.001); bSignificantly different from the ATP group (P < 0.05); cSignificantly different from the control group (P < 0.05)
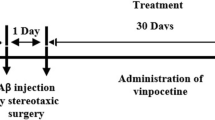
To investigate the effects of chronic treatment with VPA on ATP-induced cell death, rats received a dose of 300 mg/kg of VPA or saline (vehicle control) i.p. daily [31] (Fig. 4a) or every 12 h (Fig. 4b) for 14 days. Results show that chronic treatment with 300 mg/kg of VPA every 12 h was able to prevent, significantly, ATP-induced cell death (Fig. 4b), reducing LDH release from 65 ± 10 to 26 ± 7%. Conversely, this effect was not observed when rats were injected with just one dose of VPA per day (Fig. 4a) for the same period of treatment (14 days).
Effect of chronic treatment with valproate on ATP-induced cell death. Rats were treated with 300 mg/kg of valproate (VPA) or saline (vehicle control) every 24 h (a) or 12 h (b) for 14 days. The slices were prepared as described in Materials and methods and treated with 5.0 mM of ATP. After 18 h, the incubation medium was collected and the LDH activity was measured. Leakage of LDH is represented as a percentage of the total releasable enzyme. The data are the mean ± SEM of at least six experiments run in triplicate. ***Significantly different from the slices treated with ATP in the control group and saline group, for P < 0.001 (Student–Newman–Keuls test)
In vitro lithium and VPA treatment prevents BzATP-induced cell death
In order to investigate the involvement of the P2X7 receptor in ATP-induced cell death, hippocampal slices were treated with BzATP, a specific agonist of P2X7 for 1, 4, 12, 18 or 24 h (Fig. 5a). The treatment of slices with 0.1 mM BzATP caused a significant increase in the percentage of the LDH released after 4, 12, 18, and 24 h, when compared to the respective controls. This effect is significantly reduced by the simultaneous presence of 500 nM Brilliant Blue G, a specific P2X7 antagonist [35] (Fig 5b). Subsequently, the possible neuroprotective effect of lithium and VPA on BzATP-induced cell death was investigated. As observed in Fig. 5c, slices pre-treated with 1.0 mM of lithium or 0.5 mM of VPA for 30 min showed a significant reduction in LDH release (22 ± 13 and 26 ± 14%, respectively) when compared with slices treated with 0.1 mM BzATP (60 ± 11%).
Effect of pre-treatment with lithium or valproate on BzATP-induced cell death. (a) The slices were prepared as described in Materials and methods and treated with 0.1 mM of BzATP for different times (1, 4, 12, 18 or 24 h) before determining LDH activity. (b) The slices were pre-treated with 500 nM of Brilliant Blue G (BBG) for 30 min before the treatment with 5.0 mM of ATP or 0.1 mM of BzATP. (c) The slices were pre-treated with 1.0 mM of lithium (Li) or 0.5 mM of valproate (VPA) for 30 min before the treatment with 0.1 mM of BzATP. In (b) and (c), after 18 h, the incubation medium was collected and the LDH activity was measured. Leakage of LDH is represented as a percentage of the total releasable enzyme. The data are the mean ± SEM of at least nine experiments run in triplicate. The effect was statistically determined by Student–Newman–Keuls test. *Significantly different from the respective control group (P < 0.05); **Significantly different from the respective control group (P < 0.01); ***Significantly different from the respective control group (P < 0.001); #Significantly different from the ATP group (P < 0.001). ##Significantly different from the BzATP group (P < 0.01). aSignificantly different from the control group (P < 0.001); bSignificantly different from the BzATP group (P < 0.01)
Synergic effect of lithium and VPA
Since the exact mechanism of lithium and VPA action remains unknown, we evaluated the effect of simultaneous in vitro pre-treatment with lithium and VPA on ATP-induced cell death. As shown in Fig. 6, when the slices were pre-treated with lithium and VPA simultaneously, a significant reduction in LDH release (20 ± 6%) was observed when compared with slices pre-treated with lithium (48 ± 10%) or VPA (45 ± 8%), separately.
Synergic effect of pre-treatment with lithium and valproate on ATP-induced cell death. The slices were prepared as described in Materials and methods and pre-treated with: 1.0 mM lithium (Li), 0.5 mM valproate (VPA), 1.0 mM lithium and 0.5 mM valproate simultaneously (Li + VPA) for 30 min before the treatment with 5.0 mM ATP. After 18 h, the incubation medium was collected and the LDH activity was measured. Leakage of LDH is represented as a percentage of the total releasable enzyme. The data are the mean ± SEM of at least six experiments run in triplicate. The effect was statistically determined by Student–Newman–Keuls test. aSignificantly different from the control group (P < 0.001); bSignificantly different from the ATP group (P < 0.01); cSignificantly different from the ATP group (P < 0.001); dSignificantly different from the ATP group (P < 0.001); eSignificantly different from the Li + ATP group (P < 0.05); fSignificantly different from the VPA + ATP group (P < 0.05)
Discussion
Initially, we established a model to study ATP-induced cell death in hippocampal slices by measuring the release of the cytosolic enzyme LDH, a well established marker of cell injury and death. Our results confirmed the cytolytic activity of extracellular ATP in hippocampal slices, a preparation that maintains the interactions among neural cells and preserves the integrity of neural tissue. Hydrolysis of extracellular ATP cannot explain the results reported here since ADP, AMP, and Ado did not have cytolytic effects (Fig. 1). Since cell death potentially elevates the extracellular concentration of ATP to millimolar levels [24], the data obtained here, allow us to use this in vitro model to study neuronal injury in which an increase of extracellular ATP is involved [36] and to investigate the neuroprotective effect of lithium and VPA.
The treatment of acute disorders such as ischemia/hypoxia and brain trauma requires a rapid clinical intervention. To test the effects of acute treatment, we treated the slices with lithium or VPA at therapeutic concentrations, for 30 min (in vitro treatment) before submitting them to cytotoxic ATP concentration. Significant reductions in LDH release were observed when compared with respective controls (Fig. 2), indicating that it is possible to prevent the cytolytic effect of extracellular ATP acutely; however, the relevance of this observation in a therapeutic approach requires further study.
Additionally, we treated adult rats with lithium and VPA to evaluate the effects of chronic treatment (in vivo treatment) on the neural protection against cell death induced by extracellular ATP. As shown in Figs. 3 and 4, a significant reduction in LDH release was also observed in slices prepared from rats chronically treated with therapeutic doses of lithium or VPA. These results may be compared with another study from our group, in which the neuroprotective effect of chronic treatment with lithium was shown in a model of neuronal death using organotypic slice cultures exposed to oxygen and glucose deprivation [16].
Since the cytotoxicity of ATP may be induced by the activation of P2X7 receptors [24, 37], we submitted hippocampal slices to BzATP, a specific agonist of P2X7, to evaluate the participation of this receptor in the effect of lithium and VPA. As observed in Fig. 5c, the pre-treatment of slices with 1.0 mM of lithium or 0.5 mM of VPA for 30 min caused a significant reduction in the LDH release after incubation with BzATP, suggesting the involvement of this receptor in the cell death induced by ATP. The application of BBG, known specific P2X7 receptor antagonist, caused a significant but partial blockage on cell death induced by ATP and BzATP. Although the inhibition of BBG on P2X7 receptors is very slowly reversible [35] it is possible that the partial blockage observed could be due to the long period of incubation (18 h). However, the potential involvement of other P2 receptors than P2X7 in the cell death evoked by ATP, as it was proposed by Amadio et al. [38], cannot be excluded.
According to Rowe and Chuang [5], lithium produces its neuroprotective effects not only via multiple pathways, but possibly though a direct influence at several levels of the same pathway. The effects of lithium on neuronal transduction systems have been extensively studied in animal models and many hypotheses have been proposed to explain its therapeutic action. Studies indicate that lithium has both direct and indirect actions that contribute to inhibit GSK3β. Since GSK3β has recently been identified as an important proapoptotic enzyme [8, 39, 40], it has been suggested that the inhibition of GSK3β by lithium and VPA may account, in part, for the neuroprotective actions of these agents, as well as contributing to their therapeutic effects in bipolar disorder [8, 41, 42].
Lithium and VPA are the two most prevalently used therapeutic agents in the treatment of bipolar mood disorder. Therefore, many investigators have an interest in determining whether these two agents share common sites of action [43]. Here, we showed that when slices were pre-treated with lithium and VPA simultaneously, a significant reduction in LDH release was observed when compared with slices pre-treated with lithium or VPA separately (Fig. 6). These results demonstrate that therapeutic doses of lithium and VPA, in vitro, exert a synergic effect in the prevention of ATP-induced cell death, suggesting the involvement of different signaling pathways; these findings are in agreement with data from the literature indicating different mechanisms for the neuroprotective actions of lithium and VPA [9, 44–47]. Many reports have shown the neuroprotective effects of these drugs in chronic treatment [4, 17, 18]. An important finding of the present study was the demonstration of the protective effects of lithium and VPA during acute treatment. Although more studies are necessary, these findings could have clinical relevance.
The mechanisms involved in neuronal death are complex and some hypotheses may be raised to explain the neuroprotective effects observed in the present study. As reviewed by Le Feuvre et al. [36], ATP and P2X7 receptors can potentially regulate interleukin-1-mediated neuropathologies and, thus, may act as mediators of cell death following pathological insults, such as inflammation, trauma, and stress. We suggest that the effects observed, at least for the chronic treatment with lithium, may be explained by the fact that lithium treatment increases the physiological antagonist of the interleukin-1 receptors [48], therefore antagonizing the stimulatory effect of the cytotoxic ATP inflammatory process.
Another possible explanation for the neuroprotection induced by lithium against ATP signalization is the potential stimulation exerted by ATP and ADP via P2 receptors coupled to PLC, which produces diacylglycerol, in turn activating PKC [49] and resulting in the closure of K+ channels. A classical explanation for the neuroprotective effects of lithium involves the hypothesis of the damping of the signal transduction via PIP2 with a consequent decrease in PKC activity. Finally, although the role of PKC in regulating the P2X7 receptor remains elusive, it is possible that the neuroprotective effect of lithium and/or VPA could be the consequence of a decrease in PKC activity that, in turn, decreases the P2X7-mediated Ca2+ signaling [50].
Our in vitro results may also be an important tool for the understanding of the mechanisms involved in the cellular death induced by ATP, considering that the pathways involved with P2X7 receptors functions may be modulated by lithium and VPA.
Our knowledge of the molecular mechanisms involved in the neuroprotective action of lithium and VPA are incomplete, but our results support the hypothesis that these drugs could be used in the prophylaxis and/or treatment of neurodegenerative diseases that involve increases in ATP levels.
References
Bauer M, Alda M, Priller J, Young LT (2003) Implications of the neuroprotective effects of lithium for the treatment of bipolar and neurodegenerative disorders. Pharmacopsychiatry 36:250–254
Chuang DM, Chen RW, Franaszek EC, Ren M, Hashimoto R, Seratov V, Kanai H, Hough C, Hiroi T, Leeds P (2002) Neuroprotective effects of lithium in cultured cells and animal models of diseases. Bipolar Disor 4:129–136
Harwood AJ, Agam G (2003) Search for a common mechanism of mood stabilizers. Biochem Pharmacol 15:179–189
Henion JP, El-Marsi MA, Huff MO, El-Mallakh RS (2002) Evaluation of neuroprotection by lithium and valproic acid against oubain-induced cell damage. Bipolar Disor 4:201–206
Rowe MK, Chuang DM (2004) Lithium neuroprotection: molecular mechanisms and clinical implications. Expert Rev Mol Med 6:1–8
Nonaka S, Katsube N, Chuang DM (1998) Lithium protects rat cerebellar granule cells against apoptosis induced by anticonvulsivants, phenytoin and carbamazepine. J Pharmacol Exp Ther 286:539–547
Bournat JC, Brown AM, Soler AP (2000) Wnt-1 dependent activation of the survival factor NF-kappaB in PC12 cells. J Neurosci Res 61:21–32
Bijur GN, Sarno P, Jope RS (2000) Glycogen synthase kinase-3beta facilitates staurosporine and heat shock-induced apoptosis: protection by lithium. J Biol Chem 275:7583–7590
Li R, Shen Y, El-Mallakh RS (1994) Lithium protects agains oubain-induced cell death. Lithium 5:211–216
D’Mello SR, Anelli R, Calissano P (1994) Lithium induces apoptosis in immature cerebellar granule cells but promotes survival of mature neurons. Exp Cell Res 211:332–338
Mora A, Sabio G, Gonzalez-Polo RA, Cuenda A, Lessi dr, Alonso JC, Fuentes JM, Soler G, Centeno F (2001) Lithium inhibits caspase-3 activation and dephosphorylation of PKB and GSK3 induced by K+ deprivation in cerebellar granule cells. J Neurochem 78:199–206
Hashimoto R (2002) Lithium protection against glutamate excitotoxicity in rat cerebral cortical neurons; involvement of NMDA receptor inhibition possibly by decreasing NR2B tyrosine phosphprylation. J Neurochem 80:589–597
Alvarez G, Monoz-Montano JR, Satrustegui J, Avila J, Bogonez E, Diaz-Nido J (1999) Lithium protects cultured neurons against beta-amyloid-induced neurodegeneration. FEBS Lett 453:260–264
Wei H, Leeds PR, Quian Y, Wei W, Chen R, Chuanh D (2000) Beta-amyloid peptide-induced death of PC12 cells and cerebellar granulle cell neurons is inhibited by long-term lithium treatment. Eur J Pharmacol 392:117–123
Tseng WP, Lin-Shiau SY (2002) Long-term lithium treatment prevents neurotoxic effects of beta-bungarotixin in primary cultured neurons. J Neurosci Res 69:633–641
Cimarosti H, Rodnight R, Tavares A, Paiva R, Valentim L, Rocha E, Salbego C (2001) An investigation of the neuroprotective effect of lithium in organotypic slice cultures of rat hippocampus exposed to oxygen and glucose deprivation. Neuro Lett 315:33–36
Li R, El-Mallakh RS (2000) A noval evidence of different mechanisms of lithium and valproate neuroprotective actino on human SY5Y neuroblastoma cells: caspase-3 dependency. Neuro Lett 294:147–150
Ren M, Leng Y, Jeong M, Leeds PR, Chuang DM (2004) Valproic acid reduces brain damage induced by transient focal cerebral ischemia in rats: potential roles of histone deacetylase inhibition and heat shock protein induction. J Neurochem 89:1358–1367
Vajda FJE (2002) Valproate and neuroprotection. J Clin Neuro 5:508–514
Ralevic V, Burnstock G (1998) Receptors for purines and pyrimidines. Pharmacol Rev 50:413–492
Lemmens R, Vanduffel L, Teuchy H, Culic O (1996) Regulation of proliferation of LLC-MK2 cells by nucleosides and nucleotides: the role of ecto-enzymes. J Biochem 316:551–557
Chow SC, Kass GEN, Orrenius S (1997) Purines and their roles in apoptosis. Neuropharmacology 36:1149–1156
Agteresch HJ, Dagnelie PC, Van Den Berg JW, Wilson JH (1999) Adenosine triphosphate: established and potential clinical applications. Drugs 58:211–232
Di Virgilio F (2000). The dual role of extracellular ATP. J Auton Nerv Syst 81:59–63
Ferrari D, Los M, Bauer MKA, Vandenabeele P, Wesselborg S, Schulze-Osthoff K (1999) P2Z purinoceptors ligation induces activation of caspases with distinct roles in apoptotic and necrotic alterations of cell death. FEBS Lett 447:71–75
Neary JT, Kang Y (2005) Signaling from P2 nucleotide receptors to protein kinase cascades induced by CNS injury: implications for reative gliosis and neurodegeneration. Mol Neurobiol 31:95–103
Zimmermann H (2001) Ectonucleotidases: Some recent developments and a note on nomenclature. Drug Dev Res 52:44–56
Wilot LC, Da Silva RS, Ferreira OJ, Bonam CD, Sarkis JJF, Rocha E, Battastini AMO (2004) Chronic treatment with lithium increases the ecto-nucleotidase activities in rat hippocampal synatosomes. Neurosci Lett 368:167–170
Young LT and Woods CM (1996) Mood stabilizers have differential effects on endogenous ADP ribosylation in C6 glioma cells. Euro J Pharmacol 309:215–218
Rocha E, Rodnight R (1994) Chronic administration of lithium chloride increases immunodetectable glial fibrillary acidic protein in the rat hippocampus. J Neurochem 63:1582–1584
Hassel B, Iversen EG, Gjerstad L, Tauboll E (2001) Up-regulation of hippocampal glutamate transport during chronic treatment with sodium valproate. J Neurochem 77:1285–1292
Legrand C, Bour JM, Jacob C, Capiaumont J, Martial A, Marc A, Wudtke M, Kretzmer G, Demangel C, Duval D, Hache J (1992) Lactate dehydrogenase (LDH) activity of the number of dead cells in the medium of cultured eukaryotic cells as marker. J Biotech 25:231–243
Whitaker JF (1969) A general colorimetric procedure for the estimation of enzymes witch are linked to the NADH-NAD+ system. Clin Chim Acta 24:23–27
Bruno AN, Bonan CD, Wofchuk ST, Sarkis JJ, Battastini AMO (2002) ATP diphosphohydrolase (NTPDase1) in rat hippocampal slices and effect of glutamate on the enzyme activity in different phases of development. Life Sci 71:215–225
Jiang LH, Mackenzie AB, North RA, Surprenant A (2000). Brilliant Blue G selectively blocks ATP-gated rat P2X7 receptors. Mol Pharmacol 58:82–88
Le Feuvre R, Brough D, Rothwell N (2002) Extracellular ATP and P2X7 receptors in neurodegeneration. Euro J Pharmacol 447:261–269
Dubyak GR, El-Moatassim C (1993) Signal transduction via P2 purinergic receptors for extracellular ATP and nucleotides. Am J Physiol 265:C577–C606
Amadio S, D’Ambrosi N, Cavaliere F, Murra B, Sancesario G, Bernardi G, Burnstock G, Volonté C (2002) P2 receptor modulation and cytotoxicity function in cultured CNS neurons. Neuropharmacology 42:489–501
Pap M, Cooper GM (1998) Role of glycogen synthase kimase-3 in the phosphatidylinositol 3-kinase/Akt cell survival pathway. J Biol Chem 273:19929–19932
Crowder RJ, Freemann RS (2000) Glycogen synthase kinase-3 beta activity is critical for neuronal death caused by inhibiting phosphatidylinositol 3-kinase or Akt but not for death caused by nerve growth factor withdrawal. J Biol Chem 44:34266–34271
Grimes CA, Jope RS (2001) CREB DNA binding activity is inhibited by glycogen synthase kinase-3 beta and facilitated by lithium. J Neurochem 78:1219–1232
Li X, Bijur GN, Jope RS (2002) Glycogen synthase kinase 3β, mood stabilizers, and neuroprotection. Bipolar Disor 4:137–144
Jope RS (1999) Anti-bipolar therapy: mechanism of action of lithium. Mol Psychiatry 4:117–128
Chen B, Wang JF, Hill BC, Young LT (1999) Lithium and valproate differentially regulate brain regional expression of phosphorylated CREB and c-Fos. Mol Brain Res 70:45–53
De Sarno P, Li X, Jope RS (2002) Regulation of Akt and glycogen synthase kinase-3β phosphorylation by sodium valproate and lithium. Neuropharmacology 43:1158–1164
Mora A, Sabio G, Alonso JC, Soler G, Centeno F (2002) Different dependence of lithium and valproate on PI3K/PKB pathway. Bipolar Disor 4:195–200
Lai SL, Zhao C, Warsh JJ, Li PP (2006) Cytoprotection by lithium and valproate varies between cell types and cellular stresses. Euro J Pharmacol 539:18–26
Maes M, Song C, Lin AH, Pioli R, Kenis G, Kubera M, Bosmans E (1999) In vitro immunoregulatory effects of lithium in healthy volunteers. Psychopharmacology 4:401–407
Somei K, Sasaki K, Nara K, Ooe M, Yokota M, Miura H, Somei H (1996) Intracellular mechanisms of ATP-induced depolarizing response in the bullfrog sympathetic ganglion cells. Methods Find Exp Clin Pharmacol 7:443–448
Hung AC, Chu YJ, Lin YH, Weng JY, Hammer BC, Au YC, Sun SH (2005) Roles of protein kinase C in regulation of P2X7 receptor-mediated calcium signaling of cultured type-2 astrocyte cell line, RBA-2. Cell Signal 17:1384–1396
Author information
Authors and Affiliations
Corresponding author
Additional information
L. C. Wilot and A. Bernardi equally contributed by this work.
Rights and permissions
About this article
Cite this article
Wilot, L.C., Bernardi, A., Frozza, R.L. et al. Lithium and Valproate Protect Hippocampal Slices Against ATP-induced Cell Death. Neurochem Res 32, 1539–1546 (2007). https://doi.org/10.1007/s11064-007-9348-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-007-9348-3