Abstract
The effect of hydrogen peroxide (H2O2) on cytosolic free calcium concentration ([Ca2+]c) as well as its effect on glutamate secretion in rat hippocampal astrocytes have been the aim of the present research. Our results show that 100 μM H2O2 induces an increase in [Ca2+]c, that remains at an elevated level while the oxidant is present in the perfusion medium, due to its release from intracellular stores as it was observed in the absence of extracellular Ca2+, followed by a significant increase in glutamate secretion. Ca2+-mobilization in response to the oxidant could only be reduced by thapsigargin plus FCCP, indicating that the Ca2+-mobilizable pool by H2O2 includes both endoplasmic reticulum and mitochondria. We conclude that ROS in hippocampal astrocytes might contribute to an elevation of resting [Ca2+]c which, in turn, could lead to a maintained secretion of the excitatory neurotransmitter glutamate, which has been considered a situation potentially leading to neurotoxicity in the hippocampus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Astrocytes form the largest population of non-excitable cells in mammalian central nervous system (CNS) and are intimately associated with neurons. This cell type was initially considered to form a substrate with supportive and metabolic roles in the CNS. However, nowadays it is known that astrocytes provide more than a merely structural and trophic support for the neurons and, in addition, are able to regulate neuronal activity and synaptic neurotransmission [1–3]. They respond with an increase in intracellular free Ca2+ concentration ([Ca2+]c) after stimulation with a variety of neurotransmitters, neuromodulators and hormones. Many of these stimuli mediate their effect through the activation of membrane metabotropic receptors which, coupled via G-proteins to phospholipase C, lead to the generation of the intracellular messenger inositol 1,4,5-trisphosphate (IP3) that, in turn, releases Ca2+ from the endoplasmic reticulum (ER). Astrocytes can as well increase [Ca2+]c via ionotropic receptors, which are ligand-gated cation channels which mediate Ca2+ entry into the cell [4]. Rise in [Ca2+]c regulates intracellular events such as metabolic responses, ion transport systems, secretion of neuroactive substances, differentiation and gene expression.
Due to its critical importance for the cellular functions, resting [Ca2+]c and the recovery from increases in [Ca2+]c produced by receptor/channel activation is provided by the plasma membrane Ca2+-ATPase (PMCA), the electrochemically driven Na+/Ca2+ exchanger and the sarcoendoplasmic reticulum Ca2+-ATPase (SERCA) [5]. Astrocytes contain an elaborate ER that serves as a major source for rapid release of Ca2+ into the cytosol. Together with the ER another capacious Ca2+ pool is represented by mitochondria, and it has been proposed that they play an active role in Ca2+ signaling both in physiological and in pathological conditions [6]. Additionally, Ca2+ release from intracellular stores is typically accompanied by a substantial Ca2+ influx from the extracellular space both by capacitative and non-capacitative mechanisms [7].
Reactive oxygen species (ROS) is a term that describes chemical compounds derived from molecular oxygen [8]. ROS can be produced in the course of different physiological processes and react with a large variety of oxidizable cellular components. Overproduction of ROS can cause morphological and functional alterations of the cell, including alteration of intracellular Ca2+ homeostasis, and has been considered the basis of excitotoxicity injury mechanisms [9].
The secretion of neuroactive agents by astrocytes serves to communicate with other surrounding astrocytes and neurons [10]. Glutamate is the principal excitatory neurotransmitter and its interaction with specific membrane receptors is responsible for many neurological functions, including cognition, memory and sensation. It has been postulated that excessive activation of glutamate receptors may mediate neuronal injury or death due to Ca2+ overload [11]. Given that many pathological conditions in brain have the ROS formation as a potential underlying cause [12], it was of interest to investigate the effect of ROS on [Ca2+]c and glutamate secretion in rat hippocampal astrocytes, in order to gain more insights onto the basis of neurodegenerative disorders.
Experimental procedure
Chemicals
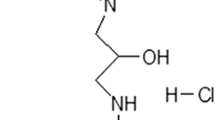
Cell culture reagents, Dulbecco’s modified Eagle’s medium (DMEM), Hank’s Balanced Salts (HBSS) and Trypsin-EDTA were obtained from Gibco BRL (Invitrogen S.A., Spain). MITO+ (concentrated serum extender) and rat-tail collagen were obtained from BD Biosciences (Bedford, MA, USA). Penicillin/Streptomycin was obtained from PAA Laboratories GmbH (Austria). Papain was obtained from Worthington Biochemical Corp. (Lakewood, NJ, USA). Fura-2/AM, dimethyl bis-(o-aminophenoxy)-ethane-N,N,N′,N′-tetra acetic (BAPTA-AM) and thapsigargin (Tps) were obtained from Molecular Probes Inc. (Europe). LDH-assay kit (TOX-7), bovine serum albumine (BSA), β-nicotinamide adenine dinucleotide phosphate (NADP+), carbonyl cyanide p-trifluoromethoxy-phenylhydrazone (FCCP), ethylene glycol-bis(2-aminoethylether)-N,N,N′,N′-tetraacetic acid (EGTA), glutamate dehydrogenase, hydrogen peroxide (H2O2), primary monoclonal mouse anti-GFAP and anti-MAP2 clone HM-2 antibodies, FITC-conjugated secondary antibody (IgG goat anti-mouse), (S)-3,5-dihydroxyphenilglycine (DHPG), trypsin inhibitor and all other chemicals used were obtained from Sigma Chemicals Co. (Spain).
Subjects
Newborn (24 h) Wistar rats were used for this study. Animal procedures were approved by the institutional Bioethical Committee.
Preparation of cell cultures
Three to five brains of 1 day-old-rat pups were employed in each cell culture preparation. Following decapitation and extraction of the brain, hemispheres were separated and the hippocampi were dissected. After careful removal of meninges the tissue was subject to digestion with papain during 1 h at 37°C. After enzymatic digestion the tissue was washed and resuspended in DMEM supplemented with fetal bovine serum (10%), penicillin (20000 IU), streptomycin (0.1 mg ml−1) and MITO+ (0.1%). Thereafter, the cells were mechanically disgregated by gently pipetting the tissue through tips of small diameter. Cells were then plated in 75 cm2 flasks and cultured for 10–14 days at 37°C in a humidified incubator (5% CO2). Twenty-four hours after isolation cells were washed twice with standard phosphate-buffered saline (PBS: 137 mM NaCl, 2.7 mM KCl, 10 mM Na2HPO4, 2 mM KH2PO4; pH adjusted to 7.4) to remove death cells and fresh culture medium was added to the flask. After the cells had reached confluence the medium was removed and replaced by HBSS medium containing trypsin-EDTA. Cells were detached by 5 min incubation in this medium. Trypsinization step was stopped by adding culture medium supplemented with 0.25% bovine serum albumin and 0.25% trypsin inhibitor. Cells were centrifuged (50–60g, 5 min) and resuspended in culture medium.
Finally, the cells were reseeded onto collagen plus poli-d-lysin-coated glass cover slips (250,000 to 750,000 cells) placed in independent dishes (35 mm diameter) and incubated in culture medium in a humidified incubator at 37°C and 5% CO2. The experiments were carried out after 7–9 days after plating of the astrocytes, once the cells had reached confluence.
Dye loading
For dye loading of the cells the culture medium was replaced by a Na-Hepes buffer containing (in mM): 140 NaCl, 4.7 KCl, 1.3 CaCl2, 1 MgCl2, 10 Hepes, 10 glucose, 0.2% bovine serum albumin (pH adjusted to 7.4). Cells were incubated with fura-2 acetoxymethyl ester (4 μM) at room temperature (23–25°C) for 45 min. Changes in fluorescence emitted by this fluorophore reflect changes in [Ca2+]c [13].
Fluorescence measurements
For monitorization of Ca2+-dependent fluorescence signals the coverslip with cultured astrocytes was mounted on an experimental perfusion chamber and placed on the stage of an epifluorescence inverted microscope (Nikon Diaphot T200). The cells were continuously superfused with a control Na-Hepes buffer containing (in mM): 140 NaCl, 4.7 KCl, 2 CaCl2, 2 MgCl2, 10 Hepes, 10 glucose (pH adjusted to 7.4). Two media containing different concentrations of KCl were employed to distinguish astrocytes from other cell types in culture. The media contained 0.2 and 50 mM KCl. In these media, the NaCl concentration was changed in order to maintain the osmolarity.
When Ca2+ free conditions were applied, the Na-Hepes buffer contained no added Ca2+ and was supplemented with 0.5 mM EGTA. In a set of glutamate secretion studies cells were loaded with the intracellular Ca2+ chelator dimethyl-BAPTA-AM (10 μM) for 30 min at room temperature (23–25°C). In these experiments, Ca2+ was additionally omitted from the extracellular solution and 0.5 mM EGTA was added.
For fluorescence changes determination an image acquisition and analysis system for video microscopy was employed (Hamamatsu Photonics). Cells were alternatively excited with light from a xenon arc lamp passed through a high-speed monochromator (Polychrome IV, Photonics) at 340/380 nm. Fluorescence emission at 505 nm was detected using a cooled digital CCD camera (Hisca CCD C-6790, Hamamatsu) and recorded using dedicated software (Aquacosmos 2.5, Hamamatsu Photonics). All fluorescence measurements were made from areas considered individual astrocytes. Some control experiments were performed and prior to the addition of stimuli cells were perfused with solutions containing 0.2 mM KCl or 50 mM KCl to distinguish astrocytes from putative growing neurons. It has been shown that astrocytes respond to low extracellular KCl by mobilizing Ca2+, and this has not been observed in neurons [14, 15].
We can discard an effect of the oxidant on fura-2-emission fluorescence that could induce artifacts in the determination of [Ca2+]c. In our experimental conditions, the concentration of H2O2 employed did not influence fura-2-derived fluorescence. Furthermore, no apparent morphological changes of astrocytes were observed that could introduce errors in Ca2+ measurements in our experimental conditions (data not shown). All stimuli were dissolved in the extracellular Na-Hepes buffer and applied directly to the cells in the perfusion chamber. Experiments were performed at room temperature (23–25°C) and results are expressed as the ratio of fluorescence emitted at both excitation wavelengths, previously normalized to the basal (resting) fluorescence.
Immunocytochemistry
GFAP is a specific intermediate filament protein in astrocytes, and is the most common characteristic used to identify this growing cell type in culture. Briefly, the cells, attached to the coverslip, were fixed with 4% paraformaldehyde, permeabilized with 0.1% Triton X 100 and incubated with a primary antibody (mouse anti-GFAP or mouse anti-MAP2). Following washing out of the first antibody cells were incubated with a FITC-labeled secondary antibody (goat anti-mouse). Monitorization of FITC-derived fluorescence signals was performed employing confocal laser-scanning microscopy (Bio-Rad, MRC 1024). Samples were excited at 488 nm from a 100-mW Argon ion laser and emitted fluorescence was recorded at >515 nm.
Glutamate release assay
To detect the release of glutamate from cultured astrocytes, we have employed an enzyme-linked system by which, in the presence of glutamate, glutamate dehydrogenase reduces NAD+ to NADH in the presence of CaCl2. NADH fluoresces when excited with UV light, therefore the enzymatic reaction can be used as an indirect indicator of glutamate secretion. To stimulate glutamate release from astrocytes, cells were incubated with agonists during 20 min in Na-Hepes buffer. Afterwards the incubation medium was removed and centrifuged (1200 rpm) to remove detached cells. Supernatant (2 ml) was then transferred to a cuvette placed in a spectrofluorimeter (RFPC5001-Shimadzu). Released glutamate was monitored following previously described methods [16] by measuring fluorescence at excitation and emission wavelengths of 340 and 460 nm, respectively. A standard curve of glutamate was performed and employed to calculate the released glutamate into the medium. Release values quoted in the text are levels attained after 20 min of incubation (nmol (mg protein)−1 (20 min)−1).
Cell viability assay
Cell viability was not significantly changed by the experimental treatments as assayed by trypan blue exclusion test and was greater than 95%. Additional tests were performed to further evaluate viability, in which cells were incubated with calcein, an acetoximethyl-ester dye, that accumulates into cells and leakage through the plasma membrane is related to cell viability loss. Calcein fluorescence was determined by exciting the cells at 490 nm and monitorization of emitted fluorescence at 520 nm. In our conditions, treatments of cells did not induce loss of calcein-derived fluorescence in the time range in which our determinations were performed, a sign of cell membrane integrity (data not shown). Cellular membrane integrity after H2O2 treatment was also determined by release of lactate dehydrogenase (LDH) into incubation medium. The assay is based on the reduction of NAD by the action of LDH. The resulting reduced NAD (NADH) is utilized in the stoichiometric conversion of a tetrazolium dye. The resulting colored compound is measured spectrophotometrically at 490 nm [17]. LDH activity in the supernatant is expressed as percent of the total content of LDH at the beginning of the incubation period. A commercially prepared kit and controls (Sigma TOX-7) were employed in this assay.
Statistical analysis
Statistical analysis was performed by Student’s t-test and only P-values < 0.05 were considered statistically significant.
Results
Identification of astrocytes in culture
We employed immunocytochemical staining for glial fibrillary acidic protein (GFAP) and MAP2 to, respectively, identify astrocytes and exclude putative neurons growing in cultures. In our hands, the cultures showed a rich content of fluorescence-stained cells with anti-GFAP and none with anti-MAP2 antibodies. A confocal fluorescence image of GFAP-positive cells can be seen in Fig. 1.
On the other hand, additional tests were performed to identify astrocytes in culture. Cell type specific calcium responses in hippocampal cells have been shown [14, 15], which can be employed to distinguish astrocytes growing in culture. Astrocytes have the property to respond to low external KCl concentrations (0.2 mM) by mobilizing Ca2+. This cell type occasionally shows Ca2+ mobilization in response to higher KCl concentrations (50 and 100 mM). Conversely, neurons will only show a Ca2+ response when challenged with the higher KCl concentrations. Cells can be identified as well by their morphology, however, at the beginning of our experiments we employed a short pulse of a low (0.2 mM) KCl concentration as a tool to eventually discriminate between the observed responses due to astrocytes stimulation and possible neurons in the same culture, and to ensure whether there is a major population of growing astrocytes.
Under these experimental conditions, perfusion of cells with a solution containing 0.2 mM KCl led to a transient increase in [Ca2+]c, which returned towards the resting level when the cells were perfused with the control Na-Hepes buffer (Fig. 2; n = 4 experiments, 43 of 46 total cells studied). When 50 mM KCl was present in the perfusion medium only a 17% of cells showed a short and transient increase in [Ca2+]c, whereas the rest of cells studied remained unresponsive to the stimulus. Following a 2–3 min washing out period of the 50 mM KCl solution, a second challenge of cells with the 0.2 mM KCl solution again led to a transient increase in [Ca2+]c, confirming a major population of astrocytes in the culture.
Changes in [Ca2+]c of astrocytes in response to low external KCl. Astrocytes are non-excitable cells that respond with Ca2+-mobilizing signals when challenged with low KCl concentration solutions. The graphic shows two typical traces of changes in [Ca2+]c of astrocytes in culture. Experiments were carried out in the presence of extracellular Ca2+ (2 mM)
In the present study, over 95% of the cells in culture responded to 0.2 mM KCl solution, an index of high population of astrocytes and low presence of growing neurons in the cultures.
LDH assay
In order to rule out the possibility that the concentration of H2O2 employed in the present study could cause cell damage, therefore leading to changes in membrane permeability that could interfere with our determinations, we performed a series of experiments in which astrocytes were incubated in the presence of the oxidant during 30 min and the LDH released into the incubation medium was assayed. Under these experimental conditions the values of absorbance at 490 nm, which are related to the content of LDH in the supernatant, were 0.061 ± 0.006 (n = 5), 0.051 ± 0.002 (n = 5) and 1.604 ± 0.006 (n = 4) for unstimulated cells, cells stimulated with 100 μM H2O2 and cell lysates, respectively. When data are expressed as the percentage of the total content of LDH, treatment of astrocytes with the oxidant did not induce any significant increase in LDH activity in the supernatant compared to that found at the beginning of the experiments (0.77 ± 0.15% vs. 0.76 ± 0.02%, n = 5). Since these values were obtained after incubation of cells for 30 min, a period of time longer than that employed for the determination of other parameters in the present study, we can exclude an effect of H2O2 due to loss of cell viability.
Effect of H2O2 on [Ca2+]c
Perfusion of astrocytes with 100 μM H2O2 led to an increase in [Ca2+]c, which reached a constant level over the basal and remained elevated. In the presence of the oxidant, application of the stimuli used to distinguish astrocytes in culture, 0.2 and 50 mM KCl, failed to induce any increases in [Ca2+]c (Fig. 3A; n = 6 experiments, 85.5% of 131 total cells studied).
Effect of H2O2 on [Ca2+]c. Time-course of changes in [Ca2+]c in response to 100 μM H2O2 both in the presence (A) and in absence (B, C and D) of extracellular Ca2+ (medium containing 0.5 mM EGTA). Control short pulses of 0.2 mM as well as 50 mM KCl were applied to the cells at the beginning of the experiments. In C and D pulses of KCl were applied to the cells in the presence of Ca2+ in the perfusion medium (2 mM). Afterwards, cells were perfused with a Ca2+ free medium and stimulated with H2O2 (C and D). A horizontal bar shows when Ca2+ free medium was applied to the cells
To avoid contribution of extracellular Ca2+ to H2O2-evoked signals we carried out experiments in the absence of Ca2+ in the perfusion medium (containing 0.5 mM EGTA). In the Ca2+-free medium, perfusion of astrocytes with 100 μM H2O2 led to an increase in [Ca2+]c, that reached a constant level over the basal similarly to what had happened in the presence of extracellular Ca2+ (Fig. 3B; n = 9 experiments, 68% of 163 total cells studied). This indicates that the oxidant releases Ca2+ from intracellular stores. However, in this situation, the level of [Ca2+]c achieved was clearly lower compared to that observed in the presence of Ca2+ in the extracellular medium. Again, in the presence of the oxidant, perfusion of cells with 0.2 and 50 mM KCl failed to evoke further increases in [Ca2+]c in all cells studied. On some occasions, an initial spike of [Ca2+]c followed by a sustained increase to a plateau (Fig. 3C; n = 6, 11% of 143 total cells studied), as well as an oscillatory pattern of [Ca2+]c over the basal, was observed in the presence of the oxidant (Fig. 3D; n = 6, 20% of 143 cells studied).
Effect of H2O2 on agonist-sensitive Ca2+ pools
Quisqualic acid is a naturally occurring compound activating ionotropic glutamate non-N-methyl-d-aspartic acid (NMDA) receptors and metabotropic glutamate receptors [18]. To evaluate contribution of agonist-sensitive intracellular Ca2+ pools to H2O2-evoked Ca2+ signals, astrocytes were stimulated with quisqualic acid (50 μM). Perfusion of cells with the agonist in the presence of extracellular Ca2+ led to an increase in [Ca2+]c, which returned towards the basal value following removal of the stimulus (Fig. 4A; n = 4 experiments, 100% of 45 total cells studied).
Effect of agonist-induced Ca2+ stores depletion on H2O2-evoked responses. (A) Time-course of changes in [Ca2+]c in response to quisqualic acid (50 μM) in the presence of extracellular Ca2+. (B) Changes in [Ca2+]c in response to quisqualic acid and subsequent addition of H2O2 (100 μM) in a Ca2+-free medium (containing 0.5 mM EGTA). (C) Time-course of changes in [Ca2+]c in response to 100 μM H2O2 in the absence of extracellular Ca2+ and subsequent stimulation of cells with quisqualic acid (50 μM). (D) Changes in [Ca2+]c after stimulation of cells with DHPG (100 μM) in the absence of extracellular Ca2+ and subsequent addition of H2O2 (100 μM). (E) Time-course of changes in [Ca2+]c in response to 100 μM H2O2 in the absence of extracellular Ca2+ and subsequent stimulation of cells with DHPG (100 μM)
We analyzed if both quisqualic acid and H2O2 release Ca2+ from the same intracellular Ca2+ store. Stimulation of astrocytes with quisqualic acid (50 μM) in the absence of extracellular Ca2+ (medium containing 0.5 mM EGTA) led to an increase in [Ca2+]c. Release of Ca2+ from the agonist sensitive Ca2+ stores was not sufficient to block a further increase in [Ca2+]c in response to 100 μM H2O2 application, since after stimulation of cells with the glutamate receptor-agonist the oxidant still increased [Ca2+]c, which reached an elevated level over the basal value (Fig. 4B; n = 5 experiments, 72% of 78 total cells studied). Conversely, previous application of the oxidant blocked the responses to stimulation of cells with quisqualic acid (Fig. 4C; n = 5 experiments, 90% of 67 total cells studied).
A more specific agonist for metabotropic glutamate receptors, (S)-3,5-dihydroxyphenilglycine (DHPG), was employed in another set of experiments since quisqualic acid has effect on non-NMDA ionotropic in addition to metabotropic receptors [19]. Stimulation of cells with 100 μM DHPG in a Ca2+ free medium led to a transient increase in [Ca2+]c that did not block H2O2-evoked increase in [Ca2+]c (Fig. 4D; n = 5 experiments, 62% of 111 total cells studied). As it had been observed for quisqualic acid, previous application of the oxidant led to an increase in [Ca2+]c that completely blocked DHPG effect on [Ca2+]c (Fig. 4E; n = 4 experiments, 71% of 69 total cells studied).
Effect of SERCA inhibition on H2O2-evoked Ca2+ signals
Thapsigargin (Tps), the most potent selective SERCA inhibitor, is often used to estimate Ca2+ pool content. It has been recently shown that the functional Ca2+ stores of astrocytes can be depleted by inhibitors of the SERCA. In a Ca2+ free medium, Tps only induces an increase in [Ca2+]c due to Ca2+ release from intracellular stores [14, 20].
In order to further investigate the source for Ca2+ release in the presence of H2O2, cells were incubated in the presence of 1 μM Tps in a Ca2+ free medium (containing 0.5 mM EGTA). In the presence of the SERCA-inhibitor, a transient increase in [Ca2+]c was observed, which later decreased and returned towards the prestimulation level. Following Tps application cells were perfused with 100 μM H2O2, which induced an additional release of Ca2+ from intracellular stores (Fig. 5A; n = 4 experiments, 93% of 55 total cells studied). In this set of experiments the rate of decay of [Ca2+]c to resting levels was significantly slower after treatment of cells with the oxidant in comparison to Tps (−0.00132 ± 0.00002 vs. −0.00273 ± 0.0001, P < 0.001).
Effect of H2O2 on Tps-sensitive Ca2+ stores. (A) Time-course of changes in [Ca2+]c evoked by Tps (1 μM) and subsequent addition of 100 μM H2O2. (B) Effect of H2O2 (100 μM) on [Ca2+]c and subsequent perfusion of cells with 1 μM Tps. All tests were performed in the absence of extracellular Ca2+ (medium containing 0.5 mM EGTA)
When the order of application of the agents was inverted, and H2O2 was applied prior to Tps, the oxidant evoked an increase in [Ca2+]c that remained elevated and blocked any additional release of Ca2+ following Tps introduction in the perfusion medium. Moreover, even after inhibition of SERCA by Tps, removal of the oxidant from the extracellular medium caused a decrease in [Ca2+]c that returned towards the basal level (Fig. 5B; n = 5 experiments, 97% of 90 total cells studied).
Effect of mitochondrial Ca2+ pool depletion on H2O2-evoked Ca2+ signals
Because Tps alone was not able to inhibit the effect of H2O2 we decided to analyze the involvement of mitochondrial Ca2+ content in H2O2-evoked responses. It has been reported that the mitochondrial uncoupler FCCP (100 nM) leads to depolarization of mitochondria and therefore it releases accumulated Ca2+ [21]. Perfusion of astrocytes with 1 μM Tps plus 100 nM FCCP in the absence of extracellular Ca2+ to deplete ER and mitochondrial Ca2+ pools evoked a transient increase in [Ca2+]c that later decreased and returned towards a plateau over the prestimulation level. Further stimulation of cells with 100 μM H2O2 failed to evoke additional increases in [Ca2+]c (Fig. 6A; n = 3 experiments, 61% of 68 total cells studied). On the other hand, stimulation of cells with H2O2 evoked an increase in [Ca2+]c and blocked any additional release of Ca2+ following introduction of Tps plus FCCP in the perfusion medium, indicating that the oxidant mobilizes Ca2+ from both ER and mitochondria (Fig. 6B; n = 4 experiments, 69% of 68 total cells studied).
Effect of mitochondrial and non-mitochondrial Ca2+ pools depletion on H2O2-evoked responses. (A) Time-course of changes in [Ca2+]c evoked by Tps (1 μM) plus FCCP (100 nM) and subsequent addition of 100 μM H2O2. (B) Effect of H2O2 (100 μM) on [Ca2+]c and subsequent perfusion of cells with 1 μM Tps plus FCCP (100 nM). All tests were performed in the absence of extracellular Ca2+ (medium containing 0.5 mM EGTA)
Effect of H2O2 on glutamate secretion
It is known that astrocytes can release glutamate through a Ca2+-dependent mechanism and consequently signal to adjacent neurons. Therefore, we performed a series of experiments to test whether the increase in [Ca2+]c evoked by H2O2 could lead to a secretion of this intercellular messenger. Stimulation of astrocytes with 100 μM H2O2 led to a significant increase in glutamate secretion as compared to unstimulated cells (13.40 ± 1.99 nmol (mg protein)−1 (20 min)−1, n = 13, vs. 1.55 ± 0.23 nmol (mg protein)−1 (20 min)−1, n = 14; P < 0.001). Tps (1 μM), that increases [Ca2+]c by inhibition of SERCA, induced as well a statistically significant increase in glutamate secretion (13.18 ± 3.05 nmol (mg protein)−1 (20 min)−1, n = 5 vs. 1.55 ± 0.23 nmol (mg protein)−1 (20 min)−1, n = 14; P < 0.001).
To further assay the dependence of H2O2-evoked glutamate secretion on Ca2+ mobilization, we performed a series of experiments in the presence of the intracellular Ca2+ chelator BAPTA (10 μM) and in the absence of extracellular Ca2+ (medium containing 0.5 mM EGTA). Under these conditions glutamate secretion in response to stimulation of cells with 100 μM H2O2 was significantly reduced compared to the effect observed in the presence of extracellular Ca2+ (7.03 ± 0.85 nmol (mg protein)−1 (20 min)−1, n = 13 vs. 13.40 ± 1.99 nmol (mg protein)−1 (20 min)−1, n = 13; P < 0.01).
Discussion
Ca2+ plays important roles in regulating several different functions of astrocytes including mitogenic responses to growth factors and neurotransmitters. It also regulates gene expression and release of signaling molecules that can modulate the activity of surrounding astrocytes and neurons [22]. On the other hand, oxidative stress is recognized as accountable for red-ox regulation involving ROS. Its role is pivotal for the modulation of critical cellular functions, notably for neurons, astrocytes and microglia such as apoptosis, ion transport and Ca2+ mobilization involved in excitotoxicity, and therefore represents a leading cause of neuronal injury [23].
Here we show that H2O2 increases [Ca2+]c in astrocytes, which results from its release from agonist- and thapsigargin-sensitive, as well as mitochondrial, Ca2+ pools. The increase in [Ca2+]c was smaller in the absence of extracellular Ca2+, which can be interpreted either as a consequence of depletion of cytosolic Ca2+ stores under these conditions, or a stimulation of Ca2+ influx into the cytosol in response to H2O2 when the ion is present in the extracellular space. The results further support an inhibition of Ca2+ extrusion mechanisms and a stimulation of glutamate secretion due to the elevated [Ca2+]c achieved in the presence of the oxidant.
Our results show that quisqualic acid and DHPG evoked changes in [Ca2+]c that did not block H2O2-induced Ca2+ responses. However, the oxidant was able to abolish Ca2+ responses to both glutamate receptor-agonists. H2O2 inhibited as well the responses of astrocytes to pulses of low KCl concentration that normally lead to transient elevations in [Ca2+]c. This can be interpreted as an effect of the ROS to release Ca2+ from the agonist-sensitive Ca2+ stores.
On the other hand, intracellular Ca2+ stores can be depleted by Tps, the most potent selective SERCA inhibitor. In a Ca2+ free medium, Tps only induces an increase in [Ca2+]c due to Ca2+ release from intracellular stores [14, 20]. Our results show that H2O2 released Ca2+ from Tps-releasable Ca2+ pool, since following perfusion of astrocytes with the oxidant Tps failed to evoke further changes in [Ca2+]c.
The stimulatory effect of H2O2 on resting [Ca2+]c and its inhibitory effect on both agonist- and Tps-induced Ca2+ mobilization could be due to a direct effect on the Ca2+ release process. Mitochondria represent the major source of intracellular ROS production. It is known that accumulated mitochondrial H2O2 can be released to the cytoplasm leading to damage of different transport mechanisms, ion channel modification, lipid peroxidation and DNA damage [24]. SERCA is the transport system responsible for refilling the intracellular Ca2+ store. Therefore, the potential damage of strong oxidants on SERCA would be expected to produce cytoplasmic Ca2+ overload [25]. SERCA is inactivated by ROS in HEK293 cells, synaptosomes, vascular tissue, or skeletal muscle [26–29]. Our data could be explained by an action of H2O2 to inhibit SERCA in this cell type, which leads to depletion of agonist- and Tps-sensitive pools and releases Ca2+ into the cytosol.
Our results also show that following agonist- and Tps-treatment inclusion of H2O2 in the perfusion medium induced an additional increase in [Ca2+]c, which suggests that the oxidant releases Ca2+ from agonist- and Tps-insensitive Ca2+ stores. The responses could only be blocked by additional inhibition of mitochondria with FCCP treatment which leads to the release of Ca2+ accumulated in the organelle. Our data therefore show that the H2O2-releasable Ca2+ pool includes both endoplasmic reticulum and mitochondria.
In addition to SERCA, PMCA and the Na+/Ca2+ exchanger play a critical role in the recovery of resting [Ca2+]c [5]. The PMCA appears to be very sensitive to inhibition by ROS and hence may be a target of oxidative stress [27, 30, 31]. Its inhibition by ROS will therefore decrease Ca2+ extrusion from the cell leading to its accumulation within the cytosol. This is in accordance with our results, which show that, in the absence of extracellular Ca2+, H2O2 evoked a sustained increase in [Ca2+]c that remained at an elevated level, and only returned towards the basal value following removal of the oxidant from the perfusion medium. This was observed even after inhibition of SERCA with a previous treatment of cells with Tps, which avoids a decrease in [Ca2+]c due to Ca2+ transport into the ER. The results presented here can be also explained on the basis of a reversible action of ROS to inhibit Ca2+ extrusion by PMCA and/or Na+/Ca2+ exchanger in astrocytes [32], which hence lead to an elevated level of [Ca2+]c.
Glutamate is the major excitatory neurotransmitter in mammalian brain and is involved in several mechanisms of brain plasticity such as learning and memory, development and aging. It is the candidate intercellular messenger used in the cellular cross-talk between astrocytes and neurons in the CNS [33]. This neurotransmitter can be released by astrocytes in response to physiological Ca2+ levels to modulate adjacent neurons [34]. However, overstimulation of glutamatergic transmission may be toxic by affecting normal function of neural cells. In the brain, a low extracellular concentration of glutamate is normally maintained between times of exocytotic transmission in order to prevent continual activation or desensitization of receptors and to avoid excitotoxicity [35].
In the present study, we show that H2O2 stimulates glutamate secretion via Ca2+-dependent mechanisms. An excessive and maintained secretion of glutamate, probably caused by the constant increase in [Ca2+]c achieved in the presence of H2O2, can therefore represent a major mechanism responsible for both neuronal and glial damage and death. The concentration of H2O2 we have employed falls in the range described in other studies of the effect of oxidative stress on cellular physiology. Ouyang et al. [36] have demonstrated that the antiapoptotic protein Bcl-XL has a protective role against ROS-induced cell death in astrocytes in culture, even though the concentration employed in their study was four times higher (400 μM) than the one employed by us in the present study.
In summary, our results show that H2O2 releases Ca2+ from intracellular stores leading to a complete depletion of Ca2+ pools. The H2O2-sensitive Ca2+ pool includes that released by glutamate-receptor agonists and Tps, as well as mitochondria. Altogether this might contribute to a maintained elevated [Ca2+]c in the presence of ROS which, in turn, would stimulate glutamate secretion by astrocytes, a situation potentially leading to neurotoxicity in the hippocampus. The mechanisms underlying glutamate secretion in response to the oxidant will be subject of further study.
References
Araque A, Carmignoto G, Haydon PG (2001) Dynamic signalling between astrocytes and neurons. Annu Rev Physiol 63:795–813
Haydon PG (2001) GLIA: listening and talking to the synapse. Nat Rev Neurosci 2:185–193
Koizumi S, Fujishita K, Tsuda M et al. (2003) Dynamic inhibition of excitatory synaptic transmission by astrocytes-derived ATP in hippocampal cultures. P Natl Acad Sci USA 100:11023–11028
Braet K, Cabooter L, Paemeleire K et al. (2004) Calcium signal communication in the central nervous system. Biol Cell 96:79–91
Verkhratsky A, Orkand RK, Kettenmann H (1998) Glial calcium: homeostasis and signalling function. Physiol Rev 78:99–141
Duchen MR (2000) Mitochondria and Ca2+ in cell physiology and pathophysiology. Cell Calcium 28:339–348
Jung S, Pfeiffer F, Deitmer JW (2000) Histamine-induced calcium entry in rat cerebellar astrocytes: evidence for capacitative and non-capacitative mechanisms. J Physiol London 527:549–561
Turrens JF (2003) Mitochondrial formation of reactive oxygen species. J Physiol London 522:335–344
Rosado JA, Redondo PC, Salido GM et al. (2006) Calcium signaling and reactive oxygen species in non-excitable cells. Mini-Revs Med Chem 6:409–415
Verkhratsky A, Kettenmann H (1996) Calcium signalling in glial cells. Trends Neurosci 19:346–352
Emerit J, Edeas M, Bricaire F (2004) Neurodegenerative diseases and oxidative stress. Biomed Pharmacother 58:39–46
Metodiewa D, Koska C (2002) Reactive oxygen species and reactive nitrogen species: relevance to cyto(neuro)toxic events and neurologic disorders. An overview. Neurotox Res 1:197–233
Grynkiewicz G, Poenie M, Tsien RY (1985) A new generation of Ca2+ indicators with greatly improved fluorescence properties. J Biol Chem 260:3440–3450
Dallwig R, Deitmer JW (2002) Cell-type specific calcium responses in acute rat hippocampal slices. J Neurosci Meth 116:77–87
Beck A, Nieden RZ, Schneider HP et al. (2004) Calcium release from intracellular stores in rodent astrocytes and neurons in situ. Cell Calcium 35:47–58
Rodríguez-Moreno A, Sihra TS (2004) Presynaptic kainate receptor facilitation of glutamate release involves protein kinase A in the rat hippocampus. J Physiol London 557:733–745
Decker T, Lohmann-Matthes ML (1998) A quick and simple method for the quantitation of lactate dehydrogenase release in measurements of cellular cytotoxicity and tumor necrosis factor (TNF) activity. J Immunol Methods 15:61–69
Vestergaard HT, Vogensen SB, Madsen U et al. (2004) Analogues of homoibotenic acid show potent and selective activity following sensitization by quisqualic acid. Eur J Pharmacol 488:101–109
Ireland DR, Guevremont D, Williams JM et al. (2004) Metabotropic glutamate receptor-mediated depression of the slow after hyperpolarization is gated by tyrosine phosphatases in hippocampal CA1 pyramidal neurons. J Neurophysiol 92:2811–2819
Humez S, Legrand G, Vanden-Abeele F et al. (2004). Role of endoplasmic reticulum calcium content in prostate cancer cell growth regulation by IGF and TNFalpha. J Cell Physiol 201:201–213
González A, Schulz I, Schmid A (2000) Agonist-evoked mitochondrial Ca2+ signals in mouse pancreatic acinar cells. J Biol Chem 275:38680–38686
Mattson MP, Chan SL (2003) Neuronal and glial calcium signalling in Alzheimer’s disease. Cell Calcium 34:385–397
Xu J, Yu S, Sun AY et al. (2003) Oxidant-mediated AA release from astrocytes involves cPLA(2) and iPLA(2). Free Radical Bio Med 34:1531–1543
Jacobson J, Duchen MR (2002) Mitochondrial oxidative stress and cell death in astrocytes-requirement for stored Ca2+ and sustained opening of the permeability transition pore. J Cell Sci 115:1175–1188
Sánchez S, Fernández-Belda F, Soler F (2004) Functional effect of hydrogen peroxide on the sarcoplasmic reticulum membrane: uncoupling and irreversible inhibition of the Ca2+-ATPase protein. Arch Biochem Biophys 431:245–251
Henschke PN, Elliott SJ (1995) Oxidized glutathione decreases luminal Ca2+ content of the endothelial cell Ins(1,4,5)P3-sensitive Ca2+ store. Biochem J 312:485–489
Pereira C, Ferreira C, Carvalho C et al. (1996) Contribution of plasma membrane and endoplasmic reticulum Ca2+-ATPases to the synaptosomal [Ca2+]i increase during oxidative stress. Brain Res 713:269–277
Viner RI, Krainev AG, Williams TD et al. (1997) Identification of oxidation-sensitive peptides within the cytoplasmic domain of the sarcoplasmic reticulum Ca2+-ATPase. Biochemistry 36:7706–7716
Barnes KA, Samson SE, Grover AK (2000) Sarco/endoplasmic reticulum Ca2+-pump isoform SERCA3a is more resistant to superoxide damage than SERCA2b. Mol Cell Biochem 203:17–21
Zaidi A, Michaelis M (1999) Effects of reactive oxygen species on brain synaptic plasma membrane Ca2+-ATPase. Free Radical Bio Med 27:810–821
Pariente JA, Camello C, Camello PJ et al. (2001) Release of calcium from mitochondrial and nonmitochondrial intracellular stores in mouse pancreatic acinar cells by hydrogen peroxide. J Membr Biol 179:27–35
Kourie JI (1998) Interaction of reactive oxygen species with ion transport mechanisms. Am J Physiol Cell Ph 275:1–24
Innocenti B, Parpura V, Haydon PG (2000) Imaging extracellular waves of glutamate during calcium signalling in cultured astrocytes. J Neurosci 20:1800–1808
Parpura V, Haydon PG (2000) Physiological astrocytic calcium levels stimulate glutamate release to modulate adjacent neurons. P Natl Acad Sci USA 97:8629–8634
Cavelier P, Attwell D (2005) Tonic release of glutamate by a DIDS-sensitive mechanism in rat hippocampal slices. J Physiol London 564:397–410
Ouyang YB, Carriedo SG, Giffard RG (2002) Effect of Bcl-XL overexpression on reactive oxygen species, intracellular calcium, and mitochondrial membrane potential following injury of astrocytes. Free Radical Bio Med 33:544–551
Acknowledgements
This work was supported by Junta de Extremadura-Consejería de Educación, Ciencia y Tecnología (2PR04A009). María P. Granados is supported by a grant from Consejería de Educación, Ciencia y Tecnología-Junta de Extremadura y Fondo Social Europeo (FIC02A022). The authors would like to thank Dr. Rafael Fernández Chacón and Mr. Pablo García-Junco Clemente from the Faculty of Medicine of the University of Sevilla for their valuable criticisms and help in preparing the cell cultures, and Mrs. Mercedes Gómez Blázquez, from the Department of Physiology of the University of Extremadura, for her technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
González, A., Granados, M.P., Pariente, J.A. et al. H2O2 Mobilizes Ca2+ from Agonist- and Thapsigargin-sensitive and Insensitive Intracellular Stores and Stimulates Glutamate Secretion in Rat Hippocampal Astrocytes. Neurochem Res 31, 741–750 (2006). https://doi.org/10.1007/s11064-006-9078-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-006-9078-y