Abstract
Introduction
Primary central nervous system lymphoma (PCNSL) is a rare disease with a dismal prognosis compared to its systemic large B-cell lymphoma counterpart. Real world data are limited, when considering a uniform backbone treatment.
Methods
A retrospective study of all adult patients treated sequentially with a high-dose methotrexate (HD MTX)-based regimen in a single tertiary medical center between 2003 and 2019.
Results
The 2015–2019 period differed from its predecessor in that most patients were treated with an HD MTX-based polychemotherapy regimen as opposed to HD MTX monotherapy (81% vs. 13%, P < .001), rituximab was given as standard of care (100% vs. 56%, P < .01), and most induction-responsive patients received consolidation treatment (70% vs. 18%, P = .01). The median progression-free and overall survival (OS) for the entire cohort (n = 73, mean age 64 years) was 9.9 and 29.8 months, respectively. Patients diagnosed between 2015 and 2019 had superior OS (P = .03) compared to those treated earlier. An interim partial response (PR) state, documented after two cycles of chemotherapy, was associated with increased incidence of progression, with only 33% of those patients achieving end-of-induction complete response. Twenty-three percent of patients developed thrombotic events and 44% developed grade 3–4 infections. HD MTX-based polychemotherapy induction was associated with both increase in thrombotic and infection incidence.
Conclusions
Contemporary HD MTX-based combination therapies suggestively improved the outcomes for PCNSL, but at a cost of increased incidence of toxicity. Patients who achieve an interim PR status are at a high risk for treatment failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system lymphoma (PCNSL) is an aggressive malignancy arising exclusively within the brain, spinal cord, leptomeninges, or eye, with a histology of diffuse large B-cell lymphoma (DLBCL) in 95% of the cases [1]. PCNSL is a rare disease that accounts for only < 1% of all non-Hodgkin’s lymphomas and 2.4–3% of all brain tumors, with a prognosis inferior to patients with systemic DLBCL [2,3,4]. This poorer outcome may result in part from the uniform expression of an activated B-cell-like immunophenotype and the challenge of efficiently delivering systemic chemotherapy to the CNS through the blood-brain barrier (BBB) [5, 6].
The current treatment of PCNSL is administered in two phases: induction and consolidation. Most modern induction regimens combine high-dose methotrexate (HD MTX) as the backbone of treatment with the addition of other chemotherapeutic agents that cross the BBB, including procarbazine, temozolomide, cytarabine, and thiotepa [7,8,9,10]. The chemotherapy regimen is usually combined with rituximab, although the data to support this approach are less robust than those for systemic DLBCL [11, 12]. Most current PCNSL protocols include a consolidation phase employing one of the following approaches with the aim of improving long-term progression-free survival (PFS): whole-brain irradiation (WBRT), myeloablative chemotherapy with autologous hematopoietic cell transplantation (HCT), or non-myeloablative chemotherapy. Data on both the overall benefit of consolidation and the superiority of the individual options are limited [10, 13].
The aim of the current study was to analyze the outcomes of patients with PCNSL treated outside clinical trials with HD MTX-based regimens between 2003 and 2019 in a single tertiary medical center dedicated for CNS tumors, with a focus on the efficacy of the shifting therapeutic trends and the investigation of factors predicting long-term PFS.
Methods
Patients
The electronic charts of sequential adult patients with PCNSL between October 2003 and December 2019 in the Tel Aviv Sourasky Medical Center (TASMC) database were systematically reviewed. TASMC is a tertiary center whose neuro-oncology and hematology services are referral centers for patients throughout Israel as well as for medical tourists from the Palestinian authority as well as Eastern Europe. Eligibility criteria for this analysis were adult patients (> 18 years) with PCNSL who received HD MTX-based induction chemotherapy. Patients were excluded if they were diagnosed as having systemic DLBCL with secondary CNS involvement or if they were primarily referred to palliative care or to non-HD MTX-based treatment. Baseline characteristics of the disease and patient demographics were collected at diagnosis. The disease status was defined according to the International Extranodal Lymphoma Study Group (IELSG) classification including age, the Eastern Cooperative Oncology Group (ECOG) performance score, elevated serum lactic acid dehydrogenase (LDH) levels, high cerebrospinal fluid (CSF) protein levels, and involvement of deep regions of brain (periventricular, basal ganglia, brainstem, and/or cerebellum) [14]. In cases for which a CSF evaluation was not available, we used a modified IELSG score (IELSG/4), which included the four remaining criteria of the original IELSG scoring system [15]. In addition, patients were risk-stratified according to the Memorial Sloan-Kettering Cancer Center (MSKCC) prognostic model, which includes three classes: class 1 (patients < 50 years), class 2 (patients ≥ 50; Karnofsky performance score [KPS] ≥ 70) and class 3 (patients ≥ 50; KPS < 70) [16]. Since 2015, patients were routinely examined for ocular involvement and, if feasible, underwent lumbar puncture for CSF evaluation.
The protocol of this study was approved by the Institutional Review Board in accordance with the Declaration of Helsinki. Informed consent was waived for this retrospective analysis.
Treatment schedules and supportive care
HD MTX was given at a dose of 1.5–8 gr/m2 with intravenous hydration and alkalization of urine to a target pH of 7.5 and a standard rescue regimen with folinic acid. We defined HD MTX monotherapy as either solely HD MTX or with the addition of rituximab. A single MTX infusion defined a single cycle. Polychemotherapy induction was defined as HD MTX plus any other conventional chemotherapy with or without rituximab.
HD MTX plus cytarabine protocols were given every 3 weeks, while HD MTX with either procarbazine or temozolomide were given every other week. Due to reimbursement issues, some patients received rituximab only after they had been discharged to the outpatient clinic after the first dose of MTX.
Deep venous thromboembolism (VTE) prophylaxis, as well as anti-bacterial prophylaxis, were not been given systematically. Trimethoprim/sulfamethoxazole (TMP/SMX) prophylaxis for pneumocystis jiroveci pneumonia (PJP) was given to all patients. Granulocyte colony-stimulating factor (G-CSF) was routinely given after HD MTX plus cytarabine-containing protocols. Starting in 2014, patients < 70 years of age who achieved a complete response (CR) state post-induction therapy were referred to an autologous HCT. The preparative regimen included carmustine 400 mg/m2 on day 5, etoposide 150 mg/m2 on days 5- to -3, and thiotepa 5 mg/kg twice daily on days − 4 to − 3 (3.5 mg/kg in patients > 65 years of age). Hospitalization was required for all courses of chemotherapy. Blood counts, electrolytes, and renal function were assessed daily.
Toxicity assessment and venous thromboembolism
Patients were evaluated for the incidence of hematologic, renal, and neurological toxicity, as well as clinical and microbiology-documented infections. The toxicity profile was graded according to CTCAE v4.3. Due to the retrospective nature of this analysis, we were able to retrieve the data on toxicity only for patients treated after 2015. The VTE incidence was evaluated for all patients from 2003 to 2019.
Efficacy assessment
The primary endpoint of this study was overall survival (OS), defined as the time from initiation of induction to last follow-up or death. Response was assessed according to the International PCNSL Collaborative Group criteria [17]. From 2003 to 2006, therapeutic response was assessed by a computerized tomographic scan or a brain magnetic resonance imaging (MRI) study. After 2006, response assessment with MRI was preferably performed after two cycles of HD MTX, at the end of induction, and after consolidation. Subsequently, patients who achieved CR were followed with a brain MRI every 3–6 months. Patients were also evaluated with brain MRIs before and after each line of therapy for determination of the extent of disease.
Statistical analysis
Data were analyzed up to April 2020. Continuous variables were described as the mean, median, standard deviation, and range of “n” observations. Categorical data were described with contingency tables, including frequency and percent. Individual subject listings were generated and analyzed. Confidence intervals (CIs) were calculated at the (two-sided) 95% level of confidence. Differences between the two groups of patients were examined by the Mann–Whitney test for continuous variables and the two-tailed Fisher’s exact test for categorical variables. All P values were derived from likelihood ratio statistics and were two-sided. OS was estimated by applying the Kaplan-Meier method. Death was treated as a competing risk in the analyses of relapse/progression. To test the impact of autologous HCT we case-control analysis by matching patients in CR prior to autologous HCT to patients in CR who got other consolidations. Matching criteria were according to age (± 5 years) and IELSG-4 score.
Cox regression was employed for multivariate analyses of risk factors for all time-to-event endpoints. Hazard ratios (HR) and 95% CIs are provided together with P values for each analysis for comparison with the reference category. Data were analyzed with the SPSS version 25.0.
Results
Characteristics of patients and disease
Between October 2003 and December 2019, 73 patients were treated for PCNSL with an HD MTX-based regimen. Five patients (age > 80 years, n = 2; severe chronic pulmonary or coronary disease n = 2, and death prior to starting therapy, n = 1) diagnosed in the period of 2010–2019 were not eligible for HD MTX-based regimen (9% of the 55 patients that were diagnosed with PCNSL in this period of time). The median follow-up of the entire cohort was 22 months (range, 4-165). Table 1 lists patient characteristics for the entire HD MTX-based cohort. The mean age of the entire cohort was 64 years (range 35.6–83.3, standard deviation [SD] ± 10.6). There was no difference in either the patients’ mean age or ECOG score throughout the two time periods (P = .217 and P = .559, respectively). At diagnosis, 30 (41.1%) patients had an ECOG score of 0–1, 33 (45.2%) had elevated LDH, and 49 (67.1%) were diagnosed with involvement of deep brain structures. All patients were HIV-negative, but six (8.2%) had iatrogenic immunodeficiency status. Sixty patients (82.1%) had a high IESLG/4 score (i.e., 2–4). Nine (12.3%), 25 (34.2%) and 39 (53.4%) patients were stratified to class 1 (low risk), 2, and 3 (high risk), respectively, according to the MSKCC prognostic model. A brain biopsy was obtained in 72 cases (98.6%) and from vitrectomy in only one case. All of the biopsies confirmed the diagnosis of large B-cell lymphoma. Twelve and eight percent of patients had documented ocular and CSF involvement, respectively. Fifteen patients (20.5%) received steroids before the diagnostic biopsy had been performed.
Induction chemotherapy: regimen, response, and factors associated with response
The induction chemotherapy characteristics are listed in Table 2. The mean number of days from diagnostic biopsy to the first HD MTX-based regimen was 16 ± 8 days. The mean number of days from diagnostic biopsy to first rituximab was 22 ± 19 days. Forty-eight (65.8%) of the patients were treated with a monotherapy regimen of HD MTX, and the remainder received a combination of HD MTX with either procarbazine or temozolomide (n = 17, 23.3%), or cytarabine (n = 8, 10.9%). The switch from monotherapy to multiagent chemotherapy throughout the study period was highly significant (P < .001). The mean number of HD MTX courses was 5.4 ± 2.26. Overall, the doses of MTX decreased throughout the years, while rituximab became standard of care (Table 2).
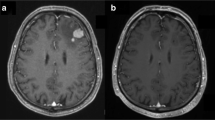
Figure 1 depicts the course of treatment for the entire cohort. Data on the interim imaging response (performed after two courses of therapy) were available for 66 patients, whose overall response rate was 85%. Twenty-six (39%) had complete response (CR) and 30 (46%) had partial response (PR), while 10 (15%) had progressive disease (PD) (Fig. 1).
Imaging response assessment at the end of HD MTX-based induction was available for 60 patients and it revealed that 37 (62%) patients had CR, 6 (10%) had PR, and 17 (28%) had PD (Fig. 1). Patients with CR of disease at interim imaging had an 88% chance of maintaining response at the end of the induction, while patients with PR status of disease had an only 33% chance of improving their response to a CR status by the end of induction therapy. We were not able to identify prognostic factors (e.g., sex, year of diagnosis, IELSG/4 prognostic score, or treatment with rituximab) that were associated with improved response to CR status at completion of induction therapy for the patients who achieved a PR status at interim imaging.
The two factors that were identified in the multivariate analysis to be associated with a greater chance of achieving a post-induction CR status were multiagent chemotherapy (OR 2.5, 95% CI 1.2–4.7, P = .048) and time of diagnosis between 2015 and 2019 (OR 6.186, 95% CI 1.006–38.058, P = .049). Sex, IESLG/4 prognostic score, previous steroid treatment, and rituximab treatment (analyzed as both a dichotomous and continuous variable) were not significantly associated with a better response.
Consolidation
Among the 40 patients with imaging studies at the end of induction who achieved a response to HD MTX-based induction chemotherapy, 19 (48%) patients had received consolidation (autologous HCT, n = 10; cytarabine-based chemotherapy, n = 6; WBRT, n = 3). Of note, all 10 autologous HCTs were conducted between 2015 and 2019, while all radiation treatments were administered between 2003 and 2009. The median age of the patients who received consolidation was 62.5 years. Seventy percent of the patients who were treated between 2015 and 2019 and had achieved a response had received consolidation treatment (88% of them were ≤ 70 years of age), compared to only 18% before that period (P = .01).
There were six patients that had a PR state prior to consolidation. Three received consolidation (chemotherapy, n = 2; autologous HCT, n = 1) and eventually achieved a CR state post consolidation. All these patients are still progression-free (7, 13 and 17 months post induction treatment). Three patients did not get consolidation and all progressed within 6 months. Two patients progressed during consolidation. Among all cohort, the overall response to induction ± consolidation was 56% (CR; n = 38, 52% and PR; n = 3, 4%).
Second-line treatment
Among 38 who achieved CR, 26 patients relapsed. Twenty-four patients who had initially achieved a CR after HD MTX-containing induction received second-line treatment for relapse (chemotherapy, n = 19 [79%] and WBRT, n = 5 [21%]). Seven patients were treated with an ifosfamide-etoposide-based regimen; six patients were given a combination of HD MTX and cytarabine; five were treated with HD MTX monotherapy; one patient was treated with temozolomide monotherapy. Three of the 24 patients, that received second-line with either chemotherapy or WBRT, were given consolidation treatment with autologous HCT.
Venous thromboembolism and regimen-related toxicity
Seventeen patients (23.3%) developed thrombotic events (prior to commencing therapy n = 4; during induction, n = 8; at relapse, n = 5). Fifteen had deep vein thrombosis (DVT), two had superficial vein thrombosis, and seven patients developed pulmonary emboli in addition to DVT. Four thrombotic events were catheter-related. None of the cases was fatal. We found that both higher IELSG-4 score and induction with polychemotherapy regimen were associated with increased VTE incidence (OR 1.3, p = .06 and OR 1.7, p = .008, respectively), while gender, year of diagnosis, did not have an impact on the incidence of VTE.
Of the patients diagnosed between 2015 and 2019, 11 (44%) developed grade 3–4 hematologic toxicity. Of note, all eight patients who were treated with combination of HD MTX and cytarabine experienced grade 3–4 hematologic toxicity. None of the patients developed a bleeding episode. Eight patients (32%) developed renal toxicity, the majority grade 1–2; one patient, who was treated with combination HD-MTX and cytarabine, had grade 3 renal toxicity. All eight cases resolved with supportive therapy.
Eleven patients (44%) developed grade 3–4 documented infections (gram-negative bacteremia, n = 8; gram negative urinary tract infection, n = 1; enterococcal meningitis, n = 1; cytomegalovirus disease, n = 1). One patient, although instructed to take TMP/SMX prophylaxis, contracted PJP after recovering from a gram-negative bacteremia. Among all tested variables both higher ECOG score and induction with polychemotherapy regimen were associated with increased incidence of infections (OR 2.1, p = .041 OR 1.5, p = .027, respectively), while gender, age, and IELSG-4 did not have an impact on the rate of infections. Of note, majority (n = 7, 88%) of the patients given combination HD-MTX and cytarabine developed grade 3–4 infection.
Two patients (8%) developed neurotoxicity during induction treatment: one was a 46-year-old woman who developed transient ataxia after four courses of HD MTX, cytarabine and rituximab. The other patient, a 64-year-old man, developed confusion and agitation followed by seizures after two courses of HD MTX, procarbazine, and rituximab. His treatment was switched to ifosfamide, etoposide, and cytarabine, which was followed by slow but eventually complete resolution of the neurologic sequelae.
Non-relapse mortality
None of the patients died during induction chemotherapy. Overall, four patients died in CR (9% of all CR patients): three sustained septic shock and one patient who had severe cognitive impairment following WBRT sustained a rapid deterioration due to an unidentified cause. There were no cases of HCT-related mortality. The low number of patients with non-relapse mortality precluded us from analyzing factors associated with mortality.
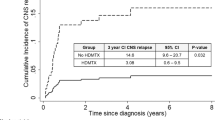
Progression-free survival
The median PFS for the responding patients (43 patients that had a long-term follow-up and achieved at least a PR state) was 9.6 (95% CI 4.4–14.8) months. The median PFS for patients who achieved any response at the end of HD MTX-containing induction was 27.8 (95% CI 12.97–42.62) months, with a 2-year PFS rate of 63%. There was no difference in PFS when we compared younger and older patients (p = .27), (Fig. 2a). There was no difference in PFS between patients with post induction-PR state and those with post induction-CR state who received consolidation (p = .518), although this analysis is limited by the small number of patients in PR state (n = 6). For patients treated with a second line for recurrence or progression, there was no difference in median PFS between those given chemotherapy-based salvage therapy or WBRT (10.7 [95% CI 5.55–15.78] vs. 9.5 [95% CI 6.23–12.76] months, respectively, P = .65). Of note, following second progression, none of the patients who previously got WBRT for the first progression, received additional therapy while 8 of the 17 patients who got chemotherapy-based salvage therapy for the first progression received additional therapy (chemotherapy, n = 5 and radiation, n = 3). Multivariate analysis identified both low IESLG/4 prognostic score (HR 0.3, 95% CI 0.02–1.02, P = .05) and rituximab treatment (HR 0.87, 95% CI 0.25–1.01, P = .05) to be associated with a better PFS, while sex, year of diagnosis, combination induction chemotherapy (vs. monotherapy), consolidation, and previous steroid use did not impact PFS (Table 3).
To further test the impact of autologous HCT on PFS, we analyzed the effect of HCT compared to other consolidation modalities. While using log rank test, HCT was associated with only a trend (P = .08); using the Breslow test autologous HCT was associated with improved PFS compared to other consolidation options (P = .014).
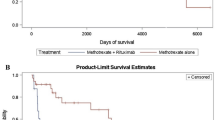
Overall survival
In total, 27 patients were alive at the time of data extraction (27/73, 37%), of whom 23 were in CR. The OS at 2 years for the entire cohort was 58% (95% CI 43–71). The median survival for the entire cohort and for the responding patients was 29.8 (95% CI 23.09–36.44) months and 39.4 (95% CI 10.54–68.26) months, respectively (Fig. 2b). The median OS for patients with primary refractory disease was only 7.7 (95% CI 4.9–10.56) months. Median OS was higher in patients with post-induction CR state compared to patients with post-induction PR state who received consolidation (60 vs. 21 months, p < .01, respectively).
The median OS for patients given a second-line treatment was prolonged in patients given chemotherapy compared to those given WBRT (35.3 [95% CI 20.3–50.3] months vs. 16 [95% CI 4.7–27.5] months, respectively, P = .01). Multivariate analysis identified advanced age as being associated with poorer OS (HR 1.12, 95% CI 1.02–9.98, P = .04), while both the year of diagnosis (latter period of 5 years) and a low IELSG/4 score were associated with a better OS (HR 0.45, 95% CI 0.23–0.95, P = .03 and HR 0.39, 95% CI 0.09–0.82, P < .01, respectively) (Table 3). All other analyzed factors (sex, rituximab treatment, induction combination treatment, and receiving consolidation) did not impact OS.
Analysis of the various consolidations regimens revealed that the median OS was improved in patients given autologous HCT compared to patients who received other consolidation regimens or no consolidation treatment (35.3, 31.4, and 21.1 months, respectively, P = .051). In addition, analyzing OS in matched patients who underwent autologous HCT vs. those who received other consolidations showed that median OS was 35.2 (95% CI not applicable) months and 25.9 (95% CI 23.5–28.3) months, respectively, p = .087), Fig. 2c.
Discussion
This is a single-center retrospective analysis of the changing dogmas in the treatment of PCNSL over time. In the period between 2015 and 2019, most of the patients were treated with of HD MTX-based polychemotherapy (as opposed to HD MTX monotherapy); rituximab was incorporated in the induction chemotherapy for all patients; and most of the patients who responded to induction received a consolidation treatment. Diagnosis between 2015 and 2019 was associated with a better OS (P = .03). considering age of the patients and performance status have not changed over time, it is suggested that the superior outcomes seen in recent years may be attributed to the use of more modern therapeutic strategies, however sample size is too small to produce conclusive results.
The median PFS and OS for the entire cohort were 9.9 and 29.8 months, respectively. These results are in line with a recent publication from the French oculo-cerebral lymphoma network, which reported data for 1002 patients with PCNSL diagnosed between 2011 and 2016, and who had a median PFS and OS of 10.5 and 25.3 months, respectively [2].
Similar to other publications, we showed that HD MTX-based polychemotherapy was suggestively more effective than HD MTX alone (P = .048), although sample size was relatively small. A randomized trial that compared HD-MTX induction monotherapy to HD MTX plus cytarabine demonstrated that the latter regimen resulted in superior rates of CR (18% vs. 46%, P = .006), as well as improved 3-year failure-free survival (21% vs. 38%, P = .01) [9]. Of note, that study had been criticized because of under-treatment in the monotherapy arm, since HD MTX was given every 3 weeks (as opposed to every 2 weeks) and for only four cycles, thus resulting in an exceptionally low CR rate. A meta-analysis of first-line PCNSL therapy in patients ≥ 60 years also demonstrated significantly improved PFS when HD MTX was combined with other chemotherapies compared to HD MTX monotherapy (adjusted HR 0.39, 95% CI 0.27–0.58, P < .001) [18].
MTX in contemporary PCNSL protocols is usually delivered at a dose of 3.5 g/m2, since current data do not suggest any benefit from doses > 4 g/m2 [19]. In line with that finding, we observed a shift in the HD MTX dose in our cohort from 8 gr/m2 before 2015 to 3–3.5 gr/m2 in recent years.
The addition of rituximab to induction therapy resulted in a prolonged PFS (P = .05), but it did not influence OS. That finding is contrary to a randomized trial that did not find any benefit in adding rituximab to an HD MTX, carmustine, teniposide, and prednisone chemotherapy regimen [11]. Other trial has shown that the addition of rituximab and thiotepa to HD MTX and cytarabine was associated with improved response and survival rates [8]. However, since the latter trial had no treatment arm that contained thiotepa without rituximab, it is unclear whether the benefit was driven by the addition of rituximab, thiotepa, or both agents.
WBRT has long been considered a cornerstone of consolidation treatment, but it is fraught with associated severe neurotoxicity [20]. In recent years, reduced-dose WBRT [21], non-myeloablative chemotherapy [10], and high-dose chemotherapy with HCT [13] have emerged as alternative consolidation modalities with less neurotoxicity. In our current study, HCT was associated with improvement in both PFS and OS compared to other consolidation options, however, HCT did not have a significant impact on either PFS or OS in the regression analysis, suggesting a selection bias in allocating patients to HCT.
The IELSG32 trial [13] included a second randomization of HCT vs. WBRT as consolidation after HD MTX-based induction chemoimmunotherapy. Both strategies were equally effective, with no significant differences in 2-year PFS. However, there was a significant impairment in attention and executive functions in patients treated with WBRT after a median duration of 28 months, which contrasted with a significant improvement in these functions in patients allocated to the HCT arm. A multicenter French trial [22] showed that the 2-year PFS was actually superior after HCT when compared to WBRT (87% vs. 63%, respectively).
We demonstrated a high rate of early failure among those patients in PR at interim assessment; with only 33% of them upgrading their response to a CR status at the end of induction. We did not observe any difference in the outcomes of patients with CR at the end of treatment based on their interim imaging responses. This suggests that major goal of therapy should be achieving a CR at the end of induction, perhaps by intensifying therapy. Conversely, Pels et al. [23] demonstrated that patients with PCNSL who achieved CR after two courses of chemotherapy had significantly improved PFS and OS than patients with CR after termination of treatment, but with only a PR after the second cycle.
While there was no difference in PFS between patients with post induction-PR state who received consolidation compared to those who achieved a post-induction CR state, median OS was better in the former group. Although the sample size is small, the difference in OS is significance (60 vs. 21 months, p < .01), suggesting that patients with post induction CR state can tolerate further therapy as oppose to those who achieve only a PR state.
Our study also showed that patients who received chemotherapy as a second-line treatment had a significantly longer OS compared to those who received WBRT (35.3 vs. 16, respectively, P = .01), however these results are subject to selection bias. Indeed, patients who got WBRT did not get additional therapy after a second progression, while half of the patients who were given chemotherapy, got additional therapy when experiencing a second relapse.
There are no randomized trials in the setting of refractory or relapsed PCNSL. Similar to our results, Hottinger et al. reported a median OS of 16 months from the initiation of WBRT given as salvage therapy after HD MTX-based induction [24]. Two ifosfamide-etoposide-based PCNSL salvage regimens produced a 1-year and 2-year OS of 41% and 25%, respectively [25, 26]. Patients with PCNSL who responded to HD MTX at initial diagnosis can be re-challenged with MTX, since chemosensitivity to this agent is typically maintained- Pentsova et al. reported a median OS of 41 months with this approach [27]. Finally, autologous HCT was associated with favorable outcomes in selected patients with recurrent PCNSL [28, 29].
Seventeen of our patients (23.3%) developed thrombotic events. Four of them were diagnosed with VTE even before starting induction, and eight others were diagnosed with VTE during induction treatment. This finding correlates with previous series that reported a relatively high VTE incidence in PCNSL patients [30, 31], and further emphasizes the importance of VTE prophylaxis. The increased risk of developing VTE that was recorded with polychemotherapy-induction regimen may be explained in part by the more frequent use of central lines. Patients given induction with polychemotherapy regimen should be kept on VTE prophylaxis. Since no case of VTE was documented during consolidation, i.e. when almost all patients were in CR status, VTE in this stage may be considered but is not mandatory.
Between 2015 and 2019, Eleven patients (44%) developed grade 3–4 documented infections. Seven (88%) of the patients treated with combination HD-MTX and cytarabine had grade 3–4 infection (mostly gram-negative bacteria). 88% of the patients given combination HD-MTX and cytarabine developed 3–4 infection. Ferreri et al. [9] recorded infective complication in only 32% of patients treated with HD MTX plus cytarabine (after implementing prophylactic G-CSF and antimicrobial prophylaxis this rate dropped to 15%). This difference in the rate of infection may be partially explained by the fact that we did not administer routine antimicrobial prophylaxis, but may also reflect a higher incidence of infections in “real-life” data.
Our study is limited by the small sample size, its retrospective design, and by the fact that the study patients were treated according to different protocols with different doses of MTX. Furthermore, we were not able to reliably report adverse events in patients treated before 2015. Nonetheless, ours is one of the largest reports of this uncommon disease, and all patients were treated uniformly with first-line therapy based on HD MTX in a national CNS lymphoma center.
In conclusion, the results of this single center large retrospective study demonstrated that therapy with HD MTX-based multi-agent induction, incorporating rituximab and followed by consolidation, has improved outcomes in PCNSL. Future studies should investigate the augmentation of therapy in patients achieving a PR-only state in their mid-term MRI scans.
References
Swerdlow SH, Campo E, Pileri SA et al (2016) The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 127:2375–2390
Houillier C, Soussain C, Ghesquieres H et al (2020) Management and outcome of primary CNS lymphoma in the modern era: an LOC network study. Neurology 94:e1027–e1039
Pfreundschuh M, Schubert J, Ziepert M et al (2008) Six versus eight cycles of bi-weekly CHOP-14 with or without rituximab in elderly patients with aggressive CD20 + B-cell lymphomas: a randomised controlled trial (RICOVER-60). Lancet Oncol 9:105–116
Villano JL, Koshy M, Shaikh H et al (2011) Age, gender, and racial differences in incidence and survival in primary CNS lymphoma. Br J Cancer 105:1414–1418
Camilleri-Broet S, Criniere E, Broet P et al (2006) A uniform activated B-cell-like immunophenotype might explain the poor prognosis of primary central nervous system lymphomas: analysis of 83 cases. Blood 107:190–196
Deeken JF, Loscher W (2007) The blood-brain barrier and cancer: transporters, treatment, and Trojan horses. Clin Cancer Res 13:1663–1674
Abrey LE, Yahalom J, DeAngelis LM (2000) Treatment for primary CNS lymphoma: the next step. J Clin Oncol 18:3144–3150
Ferreri AJ, Cwynarski K, Pulczynski E et al (2016) Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and rituximab (MATRix regimen) in patients with primary CNS lymphoma: results of the first randomisation of the International Extranodal Lymphoma Study Group-32 (IELSG32) phase 2 trial. Lancet Haematol 3:e217–e227
Ferreri AJ, Reni M, Foppoli M et al (2009) High-dose cytarabine plus high-dose methotrexate versus high-dose methotrexate alone in patients with primary CNS lymphoma: a randomised phase 2 trial. Lancet 374:1512–1520
Rubenstein JL, Hsi ED, Johnson JL et al (2013) Intensive chemotherapy and immunotherapy in patients with newly diagnosed primary CNS lymphoma: CALGB 50202 (Alliance 50202). J Clin Oncol 31:3061–3068
Bromberg JEC, Issa S, Bakunina K et al (2019) Rituximab in patients with primary CNS lymphoma (HOVON 105/ALLG NHL 24): a randomised, open-label, phase 3 intergroup study. Lancet Oncol 20:216–228
Schmitt AM, Herbrand AK, Fox CP et al (2019) Rituximab in primary central nervous system lymphoma—a systematic review and meta-analysis. Hematol Oncol 37:548–557
Ferreri AJM, Cwynarski K, Pulczynski E et al (2017) Whole-brain radiotherapy or autologous stem-cell transplantation as consolidation strategies after high-dose methotrexate-based chemoimmunotherapy in patients with primary CNS lymphoma: results of the second randomisation of the International Extranodal Lymphoma Study Group-32 phase 2 trial. Lancet Haematol 4:e510–e523
Ferreri AJ, Blay JY, Reni M et al (2003) Prognostic scoring system for primary CNS lymphomas: the International Extranodal Lymphoma Study Group experience. J Clin Oncol 21:266–272
D’Haene N, Catteau X, Maris C et al (2008) Endothelial hyperplasia and endothelial galectin-3 expression are prognostic factors in primary central nervous system lymphomas. Br J Haematol 140:402–410
Abrey LE, Ben-Porat L, Panageas KS et al (2006) Primary central nervous system lymphoma: the Memorial Sloan-Kettering Cancer Center prognostic model. J Clin Oncol 24:5711–5715
Abrey LE, Batchelor TT, Ferreri AJ et al (2005) Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol 23:5034–5043
Kasenda B, Ferreri AJ, Marturano E et al (2015) First-line treatment and outcome of elderly patients with primary central nervous system lymphoma (PCNSL)—a systematic review and individual patient data meta-analysis. Ann Oncol 26:1305–1313
Joerger M, Huitema AD, Illerhaus G, Ferreri AJ (2012) Rational administration schedule for high-dose methotrexate in patients with primary central nervous system lymphoma. Leuk Lymphoma 53:1867–1875
Abrey LE, DeAngelis LM, Yahalom J (1998) Long-term survival in primary CNS lymphoma. J Clin Oncol 16:859–863
Morris PG, Correa DD, Yahalom J et al (2013) Rituximab, methotrexate, procarbazine, and vincristine followed by consolidation reduced-dose whole-brain radiotherapy and cytarabine in newly diagnosed primary CNS lymphoma: final results and long-term outcome. J Clin Oncol 31:3971–3979
Houillier C, Taillandier L, Dureau S et al (2019) Radiotherapy or autologous stem-cell transplantation for primary cns lymphoma in patients 60 years of age and younger: results of the Intergroup ANOCEF-GOELAMS Randomized Phase II PRECIS Study. J Clin Oncol 37:823–833
Pels H, Juergens A, Schirgens I et al (2010) Early complete response during chemotherapy predicts favorable outcome in patients with primary CNS lymphoma. Neuro Oncol 12:720–724
Hottinger AF, DeAngelis LM, Yahalom J, Abrey LE (2007) Salvage whole brain radiotherapy for recurrent or refractory primary CNS lymphoma. Neurology 69:1178–1182
Arellano-Rodrigo E, Lopez-Guillermo A, Bessell EM et al (2003) Salvage treatment with etoposide (VP-16), ifosfamide and cytarabine (Ara-C) for patients with recurrent primary central nervous system lymphoma. Eur J Haematol 70:219–224
Mappa S, Marturano E, Licata G et al (2013) Salvage chemoimmunotherapy with rituximab, ifosfamide and etoposide (R-IE regimen) in patients with primary CNS lymphoma relapsed or refractory to high-dose methotrexate-based chemotherapy. Hematol Oncol 31:143–150
Pentsova E, Deangelis LM, Omuro A (2014) Methotrexate re-challenge for recurrent primary central nervous system lymphoma. J Neurooncol 117:161–165
Choi MK, Kang ES, Kim DW et al (2013) Treatment outcome of relapsed/refractory primary central nervous system diffuse large B-cell lymphoma: a single-center experience of autologous stem cell transplantation. Int J Hematol 98:346–354
Welch MR, Sauter CS, Matasar MJ et al (2015) Autologous stem cell transplant in recurrent or refractory primary or secondary central nervous system lymphoma using thiotepa, busulfan and cyclophosphamide. Leuk Lymphoma 56:361–367
Goldschmidt N, Linetsky E, Shalom E et al (2003) High incidence of thromboembolism in patients with central nervous system lymphoma. Cancer 98:1239–1242
Hohaus S, Tisi MC, Bartolomei F et al (2018) Risk factors for venous thromboembolism in patients with lymphoma requiring hospitalization. Blood Cancer J 8:54
Funding
The authors received no funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sarid, N., Bokstein, F., Blumenthal, D.T. et al. Impact of contemporary regimens on the outcomes and toxicity of primary CNS lymphoma: a single-center retrospective analysis of 73 patients. J Neurooncol 151, 211–220 (2021). https://doi.org/10.1007/s11060-020-03654-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03654-x