Abstract
Background
Re-Irradiation (Re-RT) is an established treatment option for young patients with recurrent glioblastoma (GBM). Multiple reports show a low risk of side-effects as well as a good efficacy resulting in median survival times ranging from 5 to 18 months. Elderly patients, however, are underrepresented in reports about Re-RT. Even in the elderly, with concomitant radiochemotherapy and adjuvant chemotherapy, progression-free survival times now are approaching 6 months or even longer.
Methods
We report on 25 consecutive patients with at least 65 years of age treated with Re-RT for recurrent GBM. We analyzed the patient’s files for the treatment regimens, side-effects and survival times. Survival times, as well as hazards, were calculated by the Kaplan Meier method as well as Cox-regression method, respectively.
Results
The median overall survival was 6.9 months, treatment was well tolerated with only minor side effects. Use of systemic treatments as well as the length of the interval between 1st -line radiotherapy and re-irradiation were associated with a favorable prognosis. The latter remained significant after multivariate analysis.
Conclusion
Re-RT of elderly GBM patients should not be withheld based purely on age since the treatment is safe and results in comparable survival times to younger patients. When counseling elderly patients with recurrent GBM, especially the length of the interval since 1st line radiotherapy should be considered as a prognostic factor and an additional systemic treatment option should be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Almost all patients with glioblastoma (GBM) relapse at some time point of their disease. Therefore, there is an urgent need for efficient salvage treatments. Although prospective trials comparing different treatment modalities in recurrent GBM are sparse, there are currently mainly three modalities available in this clinical situation. These modalities are a 2nd surgery, systemic treatments, and re-irradiation (Re-RT) [1]. Furthermore, many centers use a combination of two or all of these modalities.
Re-RT is generally initiated in patients with inoperable recurrent disease in cases where the interval from the end of 1st line radiotherapy (RT) to Re-RT is longer than 6 months. A plethora of different fractionation schemes and target volume concepts have been published so far, with currently no preference for any of them over another. As heterogeneous as these concepts are, as large is the spectrum of re-irradiation results, which ranges in median survival times between 5 and 18 months [2]. The heterogeneity of these results is—at least partly—due to the heterogeneity of risk factors between the investigated cohorts. Several risk scores do exist, which allow a prognostication in individual cases: Most of them use the clinical factors age, the grading at the primary site as well as the length of the interval between the 1st and the 2nd course of RT—among others—for prognostication of the survival after Re-RT [3, 4].
As in younger patients, RT is a cornerstone of the 1st line treatment of elderly GBM patients, too. It provides better results than best supportive care alone [5]. Furthermore, it is effective in all patients, independent from the MGMT methylation status [6]. After hypofractionated RT schemes have proven to be non-inferior to normofractionated regimens as stand-alone treatments [7,8,9], the superiority of a temozolomide-based radiochemotherapy (RCHT) has been shown by Perry et al., only recently [10]. Noteworthy, the progression-free survival (PFS) was significantly increased in the RCHT-arm, with approximately one-third of the patients with an interval of more than 6 months since the end of 1st-line treatment as compared to around 10% in the arm treated with RT only [10]. These patients qualify for Re-RT—at least based on a time-interval-criterion between first and second RT. Despite that, only very few patients underwent Re-RT after participating in the Perry-Trial [10]. This might be due to missing data on Re-RT in elderly patients, or other medical reasons since the clinical decline in the aged population may be more substantial than in younger patients with recurrent GBM.
To our knowledge, there is no evidence for the feasibility of Re-RT in elderly patients, as the median ages in the published Re-RT are around 51.5 years [2]. However, the ageing population is growing, and thus treatment decisions in cases of GBM-recurrence with patients having excellent overall performance status are increasing. Therefore, we analyzed the data of elderly patients treated between 2010 and 2016 with a second course of RT at our department.
Methods
Eligibility
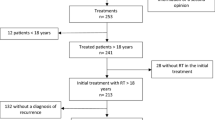
Patients with initially histologically proven and treated GBM, who underwent Re-RT for recurrent GBM were eligible for this analysis. At the time point of Re-RT, all patients were at least 65 years old. We included cases of Re-RT between 2010 and 2016, performed at the Department for Radiation Oncology at the Klinikum rechts der Isar of the Technical University of Munich. This retrospective analysis was approved by the local ethical committee of the Technical University of Munich (Project Number 408/14).
25 patients met all inclusion criteria. Details on the patients’ characteristics can be found in Table 1. Briefly, the median age of the predominantly male cohort (16 males vs. 9 females) was 69.6 years (range 65–79 years). The patients were in a generally good condition (median ECOG 1, range 0–2) and were initially diagnosed for GBM; in two cases, an oligodendroglial component was present, too. IDH1 mutations were assessed in 10 patients at primary diagnosis, and mutations were found in 2 cases. MGMT promoter methylation of the primary GBM was investigated in 14 cases and was found to be hypermethylated in 5 of these patients.
A majority of the included cases underwent 2nd surgery before Re-RT, with 7 subtotal resections (STR), 1 near total resection (NTR) and 4 gross total resections (GTR). Additionally, 2 patients received Gliadel wafers during 2nd surgery. Besides, 5 patients underwent 2nd line chemotherapy (ChT) before Re-RT. Diagnosis of recurrent GBM was confirmed either by MRI, amino acid-PET (9 cases) and/or histology (7 cases).
Re-RT was performed 13.5 months after the 1st course of RT (median; range 5.9 to 228.9 months).
Radiotherapy
We performed Re-RT under stereotactic guidance in different dosing and target volume regimens. The target volume definition was performed with iPlan RT (v 4.1.1, BrainLab AG, Munich, Germany). The gross tumor volume (GTV) was defined as the enhancing masses on 1 mm sliced, isometric, T1 weighted MRIs and on 1 mm sliced contrast-enhanced computed tomography (CT) scans. In 9 cases, additional FET-PET images were available, too. In these cases, the hot-spots were defined visually and included in the GTV. Dependent on the dosing regimen described below as well as in Table 2, a margin from 0 to 15 mm, corrected for anatomic barriers, was added to generate the clinical target volume (CTV). Generally, the higher the dose per fraction was, the smaller we chose the CTV-margin. Daily stereotactic guidance was used in all cases and performed with the frameless ExacTrac system (BrainLab AG, Munich, Germany). All patients were treated with 6 MV photons of a medical linear accelerator (LINAC) equipped with a micro-multi-leaf collimator (micro-MLC; Trilogy, Varian Medical Systems, Palo Alto, USA). Treatment planning was performed either with the iPlan System (v 4.1.1 BrainLab AG, Munich, Germany) or with Eclipse (version 13, Varian Medical Systems, Palo Alto, USA). Dependent on the location of the recurrent GBM, either 3D conformal treatment plans with coplanar and non-coplanar beams or intensity modulated radiotherapy (IMRT) plans, partially as volumetric intensity modulated arc therapy-plans (VMAT) were generated. The dose was prescribed to an individual reference point, mostly within the isocenter, and to surround the PTV with the 95% isodose curve. For the IMRT and VMAT plans, the dose was prescribed to D50% with a Dmin not lower than 95% of the prescribed dose. Lower than prescribed doses were accepted in individual cases in the direct vicinity of organs at risk (OAR), such as the chiasm, the brainstem or the optic nerves to reduce the risk of side-effects. Concomitant chemotherapy was accepted only in patients treated with lower doses per fraction and given in 4 cases.
Follow up
All patients underwent a tight follow up (FU) after Re-RT with including clinical workup, physical examination as well as imaging series. Patients had their first follow up visit 4–6 weeks after Re-RT and were seen in 3-months intervals after that. Usually, follow-up imaging included T1 weighted MRIs as well as T2 FLAIR-Images. Experienced neuroradiologists determined the imaging-based progression-free survival according to the RANO HGG criteria [11]. When progression or necrosis was suspected, a FET-PET was obtained. Noteworthy, neither use perfusion-imaging, nor dynamic PET-imaging was used as a standard protocol.
Endpoints and statistics
We retrospectively surveyed the clinical files as well as all available imaging data sets of all selected patients. The primary objective of this analysis was overall survival (OS); secondary objectives were Progression-free survival (PFS) and safety.
Furthermore, we surveyed the files for the treatments that were used before and after Re-RT, to allow a more precise description of our cohort.
We performed all statistical analyses in IBM SPSS v. 14. We analyzed all survival endpoints by the Kaplan Meyer-Method. The median overall survival (mOS) was calculated from the first day of re-treatment to the date of death or, if censored, to the last follow up of the patients. PFS was calculated from the first day of Re-RT to the first occurrence of recurrent disease, suspected clinical progression or death, whatever occurred first.
Subgroup analysis included comparisons between patients with good versus poor performance status, standard- versus hypofractionated regimens, younger versus older than the median age of the cohort and longer versus shorter interval between 1st and 2nd course of RT. COX regression was used for univariate as well as multivariate analysis. Factors with significance in univariate analysis were included into a multivariate analysis.
Results
Survival
The median OS of the entire cohort was 6.9 months; 6 patients survived more than 10 months and 2 patients more than 2 years (Fig. 1). The median progression-free survival was 4.3 months (Fig. 2). On univariate analysis, patients with an interval of more than 12 months from 1st to the 2nd course of RT (mOS 8.8 vs. 4.1 months, hazard ratio (HR) 3.313, 95% confidence interval (CI) 1.273–8.622, p = 0.014, Fig. 3a) had a significantly better OS. There was a trend towards improved OS in patients receiving CHT during or after Re-RT (mOS 4.3 vs. 10.6 months, HR 2.333, CI 0.993–5.482, p = 0.052, Fig. 3b). Neither the ECOG nor the age or the fractionation regimen had a significant influence on OS (Fig. 3c, d). In multivariate analysis, only the length of the interval from 1st to the 2nd course of RT remained significant (p = 0.014).
Cox regression analysis. Results from the univariate Cox-regression analysis. a The interval from 1st RT to Re-RT. The published cut-off of 12 months was used. HR 3.313 (p = 0.014). b Chemotherapy. A monotherapy was defined as a reference. The HR for ChT adjuvant or at progression was 2.333 (p = 0.052). c Age. The median age of 69.5 years was used to dichotomize the cohort. HR from being older than 69.5 years: 0.62 (p = 0.268). d ECOG. The HR for ECOG 1 and 2 to ECOG 0 was 0.43 and 0.799, respectively (p = 0.208 and 0.623). e Dosing regimen. Standard fractionation was defined as a reference. HR for mild and strong hypofractionation 1.457 and 1.180 (p = 0.437 and 0.784)
Response
The response to RT at 6 weeks after RT was evaluable in 17 from 25 patients. For the remaining 8 patients, no imaging data were available for the relevant time point. Assuming that all patients who died until 10 weeks after Re-RT died from progressive disease, 4 additional patients can be included in the analysis. In conclusion, the rates for stable disease (SD), progressive disease (PD) and PD versus pseudoprogression than were 48%, 33%, and 19%, respectively.
At 4.5 months, 1 patient with pseudoprogression was in partial remission (PR), 1 was lost of follow up, and two patients had PD. In total, 12 patients were available for response assessment by imaging criteria, and 10 patients were dead or died within 4 weeks of the scheduled re-staging; 3 Patients were lost of follow up. Thus, at 4.5 months 9% were in PR, 5% in SD and 9 patients in 86% in PD or dead.
Systemic treatments
Four patients were treated with concomitant systemic treatment during RT. Two patients participated in the APG-101 trial and were also treated adjuvantly [12]. Of note, we do not know whether these patients received the APG-101 or placebo. Further two patients received concomitant Temozolomide (TMZ) which was continued to adjuvant Temozolomide by one patient. One further patient decided to receive adjuvant temozolomide after mono-Re-RT.
Most of the patients with PD did not receive further treatments. However, 8 patients underwent salvage treatments. In the half of the cases (4/8), a TMZ re-challenge was prescribed. One of these patients also did receive Bevacizumab upon further progression. 2 patients received CCNU, one of them together with Bevacizumab. One patient received Bevacizumab as last line treatment. Notably, all patients that received Bevacizumab were treated with hypofractionated regimens.
Toxicity
The treatment was generally well tolerated. We did not see any radiation necrosis, and consequently, no surgery for the treatment of side effects was necessary. There was one patient with a stroke after RT, yet this was not deemed to be related to the Re-RT.
Discussion
The present work represents the first report on Re-RT in a purely elderly cohort [2, 13]. With a median age of 69.6 years, our cohort is about 10 years older than all formerly reported cohorts on Re-RT. We included all patients with a recurrent GBM who were older than 65 years at the time of the treated recurrence, as several trials on elderly GBM patients chose this age as an inclusion criterion [6, 7, 10]. The treatment of elderly patients with recurrent GBM with Re-RT resulted in an mOS of 6.9 months with an acceptable safety profile. Importantly, the survival with Re-RT is within the range of previously reported series [2, 14]. The response to the treatment has mainly to be deemed as a deceleration of a further progression. Only very few patients had a partial remission. However, also a slowed down progression can be an important treatment effect for this poor-prognosis group [13]. Concerning the survival endpoint, the comparable efficacy is an important novelty, as efficient salvage treatments are frequently withheld from elderly patients. Especially patients who relapse with a longer interval from 1st line RT, as well as patients who undergo additional systemic treatments do benefit from Re-RT. Interestingly and consistent with some other reports, we found a sex-difference favoring males of females (ratio 1.77 : 1) for the re-treatment [15, 16]. The reason, as well as the robustness for this preference, is unknown, as there is no known sex-difference in the 1st diagnosis of GBM and as prospective data from RTOG 0525 did not report a significant sex-difference [15, 17].
The elderly cohort, as defined as patients older than 65 years, is underrepresented in Re-RT-series due to several factors. First of all, the likelihood of being able to undergo Re-RT is decreased in older patients [15]. The lower chance for undergoing Re-RT is due to a generally lower performance status with increasing age as well as a higher likelihood to suffer from concomitant diseases. Secondly, a higher rate of less aggressive first-line treatments with either best supportive care or mono-therapies is used in elderly patients, even in the primary treatment setting [15]. As single modality regimens result in shorter progression-free survivals as compared to multi-modality regimens [10] and as mono-therapies have been a standard of care for elderly GBM patients in the past decade [18], we consequently saw less aged patients that progress as late as at least six months after the end of 1st line RT [6, 8, 9]. Therefore, the median age in former reports about Re-RT was within a range between 20 and 60 years [13]. As already stated in the introduction, this might change after a broad adoption of the RChT regimen published by Perry et al., which showed a PFS that was approaching the 6-months interval [10, 19, 20].
Patients treated with Re-RT had an mOS of 6.9 months, calculated from the onset of Re-RT. The survival-time is within the range of formerly published reports on Re-RT [2, 13]. There are only very few prospective reports on the efficacy of Re-RT in GBM [2]. Shi and colleagues recently published an article on the late results from RTOG 0525 [17]. In this cohort, patients who were treated with BSC only had an mOS of 4.8 months; this was significantly lower than the mOS of patients who were treated with RT only, ChT only or RChT after progression (8.2, 10.5, 11.3 months) [17]. Also in our cohort, the use of a 2nd line chemotherapy, either as an adjuvant or as a further salvage strategy, was associated with a strong trend (p 0.052) towards improved survival. It is important to note, however, that there is an essential difference in the way how OS was defined in this report, as it was determined from progression after 1st line treatment and not from the beginning of Re-RT. Furthermore, the patients in RTOG 0525 were less pre-treated than our cohort. The median age of the cohort was 50.3 years for patients with RChT, 54.6 years for patients with ChT only, 55.6 years for patients with RT only and 58.0 years for patients who were treated with BSC only. When these difference in the pre-treatment, as well as the differences in OS calculation, are considered, our results are very comparable to the results from RTOG 0525.
Besides the use of systemic treatments after Re-RT, which was a significant predictor for a longer survival after Re-RT, the interval from 1st line treatment to Re-RT was the most significant factor for the prognosis of our patients. This interval was a significant factor within a univariate as well as a multivariate analysis. The weight of the interval-factor is in line with former reports of Re-RT and was included in several risk scores for Re-RT, too [3, 4, 21]. Biological factors, such as MGMT promotor hypermethylation or IDH-mutation were only partially available for the patients who underwent surgery at our hospital. Due to legal aspects, a post-hoc-analysis of specimens which were drawn in other hospitals was not possible. We therefore decided against including a statistical analysis of these factors. When molecular factors are not available, however, the interval from 1st to 2nd RT might serve as a surrogate for the underlying biology. Noteworthy, we believe that the effect of other clinical factors, such as the performance score or the age might also have an influence, yet the limited number of cases in this series precludes further conclusions.
We also analyzed the impact of different treatment regimens on the survival times of our patients. There was no difference in the prognosis of our patients between the used regimens, which is in line with the results from a recent meta-analysis from Kazmi et al., which reported regimens with less or more than f fractions to be equal-efficient regarding 6- and 12 months OS [22]. In our study, a comparison of different treatment regimens was possible as the Re-RT policies at our department changed within the investigated period. Initially, a hypofractionated regimen was preferred. Since 2014, we prefer a regimen with standard fractionation as this allows us to treat patients with concomitant temozolomide during Re-RT. Additionally, we believe a standard fractionation regimen to have a superior toxicity profile [13]. As one could argue that there was no radiation necrosis in our cohort—independent from the fractionation scheme—it should be mentioned, that only patients with hypofractionated Re-RT received Bevacizumab during their disease. As Bevacizumab is known to have an excellent efficacy against radiation necrosis, this potentially veiled toxicity of the hypofractionation regimen [23, 24]. Nonetheless, it seems that regimens with higher doses to smaller volumes versus lower doses to larger volumes are interchangeable regarding the efficacy as well as the safety. This conclusion was also drawn by the first meta-analysis on re-irradiation published by Kazmi et al. [22]. As a consequence, physicians should choose the target volume and dosing regimens dependent on other factors, such as the possibility to undergo concomitant chemotherapy, the volume of the recurrent GBM, the technical capabilities or the vicinity to OARs. Concerning the safety of re-irradiation, several single institutional reports, reviews as well as the meta-analysis do concisely show that re-irradiation is a safe treatment option for rGBM and our data show that this also seems to hold true for an aged cohort [2, 13, 16, 22].
The report is limited by the retrospective non-comparative methodology which could result in a selection bias as well as an underreporting of low-grade toxicities [22]. We aimed to avoid a selection bias by defining clear inclusion criteria and by focusing on a homogenous cohort of patients. Consequently, we decided to focus on patients, who presented with a histological proven GBM before 1st line treatment in order to limit a selection-bias which could be introduced by including patients with a malignant transformation from low-grade gliomas. Nonetheless, comparison to BSC-series remains to be difficult, and conclusions about survival benefits due to intervention should be drawn with caution. Furthermore, the decision for a more homogenous cohort limited the number of patients feasible for this analysis. Lastly, due to the still short survival after re-irradiation, objective responses at 4.5 months after Re-RT was not available for all patients. To give a rough assumption of the response, we assumed that all patients who died did so with a progressive disease. As this not necessarily is true, the response rate might be an underestimation.
Conclusion
This report is the first report of Re-RT of elderly GBM patients. We could show that Re-RT is feasible with acceptable safety. Re-RT for elderly patients with recurrence results in survival times that are comparable to younger patients with recurrent GBM who are treated with Re-RT. Nonetheless, prospective comparative trials are needed to clarify the role of Re-RT in recurrent GBM. In line with previous data, patients with longer intervals from 1st line treatment and patients who received systemic treatments additionally to Re-RT did have a better prognosis; this should be considered when patients are counseled. Generally, the decision in favor of or against Re-RT should not be based on age only.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Weller M, van den Bent M, Tonn J, Stupp R, Preusser M, Cohen-Jonathan-Moyal E, Henriksson R, Le Rhun E, Balana C, Chinot O, Bendszus M, Reijneveld J, Dhermain F, French P, Marosi M, Watts C, Oberg I, Pilkington G, Baumert B, Taphoorn M, Hegi M, Westphal M, Reifenberger R, Soffietti S, Wick W (2017) For the European Association for Neuro-Oncology (EANO) Task Force on Gliomas. EANO guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol. https://doi.org/10.1016/S1470-2045(17)30194-8
Straube C, Elpula G, Gempt J, Gerhardt J, Bette S, Zimmer C, Schmidt-Graf F, Meyer B, Combs SE (2017) Re-irradiation after gross total resection of recurrent glioblastoma. Strahlenther Onkol. https://doi.org/10.1007/s00066-017-1161-6
Combs SE, Edler L, Rausch R, Welzel T, Wick W, Debus J (2013) Generation and validation of a prognostic score to predict outcome after re-irradiation of recurrent glioma. Acta Oncol 52:147–152. https://doi.org/10.3109/0284186X.2012.692882
Kessel KA, Hesse J, Straube C, Zimmer C, Schmidt-Graf F, Schlegel J, Meyer B, Combs SE (2017) Modification and optimization of an established prognostic score after re-irradiation of recurrent glioma. PLoS ONE 12:e0180457. https://doi.org/10.1371/journal.pone.0180457
Keime-Guibert F, Chinot O, Taillandier L, Cartalat-Carel S, Frenay M, Kantor G, Guillamo J-S, Jadaud E, Colin P, Bondiau P-Y, Meneï P, Loiseau H, Bernier V, Honnorat J, Barrié M, Mokhtari K, Mazeron J-J, Bissery A, Delattre J-Y (2007) Radiotherapy for glioblastoma in the elderly. N Engl J Med 356:1527–1535. https://doi.org/10.1056/NEJMoa065901
Wick W, Platten M, Meisner C, Felsberg J, Tabatabai G, Simon M, Nikkhah G, Papsdorf K, Steinbach JP, Sabel M, Combs SE, Vesper J, Braun C, Meixensberger J, Ketter R, Mayer-Steinacker R, Reifenberger G, Weller M (2012) Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase 3 trial. Lancet Oncol 13:707–715. https://doi.org/10.1016/S1470-2045(12)70164-X
Roa W, Kepka L, Kumar N, Sinaika V, Matiello J, Lomidze D, Hentati D, Guedes de Castro D, Dyttus-Cebulok K, Drodge S, Ghosh S, Jeremi B, Rosenblatt E, Fidarova E (2015) International atomic energy agency randomized phase III study of radiation therapy in elderly and/or frail patients with newly diagnosed glioblastoma multiforme. J Clin Oncol. https://doi.org/10.1200/JCO.2015.62.6606
Malmström A, Grønberg BH, Marosi C, Stupp R, Frappaz D, Schultz H, Abacioglu U, Tavelin B, Lhermitte B, Hegi ME, Rosell J, Henriksson R (2012) Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial. Lancet Oncol 13:916–926. https://doi.org/10.1016/S1470-2045(12)70265-6
Roa W, Brasher PM, Bauman G, Anthes M, Bruera E, Chan A, Fisher B, Fulton D, Gulavita S, Hao C, Husain S, Murtha A, Petruk K, Stewart D, Tai P, Urtasun R, Cairncross JG, Forsyth P (2004) Abbreviated course of radiation therapy in older patients with glioblastoma multiforme: a prospective randomized clinical trial. J Clin Oncol 22:1583–1588. https://doi.org/10.1200/JCO.2004.06.082
Perry JR, Laperriere N, O’Callaghan CJ, Brandes AA, Menten J, Phillips C, Fay M, Nishikawa R, Cairncross JG, Roa W, Osoba D, Rossiter JP, Sahgal A, Hirte H, Laigle-Donadey F, Franceschi E, Chinot O, Golfinopoulos V, Fariselli L, Wick A, Feuvret L, Back M, Tills M, Winch C, Baumert BG, Wick W, Ding K, Mason WP (2017) Short-course radiation plus temozolomide in elderly patients with glioblastoma. N Engl J Med 376:1027–1037. https://doi.org/10.1056/NEJMoa1611977
Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E, DeGroot J, Wick W, Gilbert MR, Lassman AB, Tsien C, Mikkelsen T, Wong ET, Chamberlain MC, Stupp R, Lamborn KR, Vogelbaum MA, Van Den Bent MJ, Chang SM (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28:1963–1972. https://doi.org/10.1200/JCO.2009.26.3541
Wick W, Fricke H, Junge K, Kobyakov G, Martens T, Heese O, Wiestler B, Schliesser MG, Von Deimling A, Pichler J, Vetlova E, Harting I, Debus J, Hartmann C, Kunz C, Platten M, Bendszus M, Combs SE (2014) A phase II, randomized, study of weekly APG101 + reirradiation versus reirradiation in progressive glioblastoma. Clin Cancer Res 20:6304–6313. https://doi.org/10.1158/1078-0432.CCR-14-0951-T
Amichetti M, Amelio D (2011) A review of the role of re-irradiation in recurrent high-grade Glioma (HGG). Cancers (Basel) 3:4061–4089. https://doi.org/10.3390/cancers3044061
Combs SE, Thilmann C, Edler L, Debus J, Schulz-Ertner D (2005) Efficacy of fractionated stereotactic reirradiation in recurrent gliomas: long-term results in 172 patients treated in a single institution. J Clin Oncol 23:8863–8869. https://doi.org/10.1200/JCO.2005.03.4157
Steffens R, Semrau S, Lahmer G, Putz F, Lettmaier S, Eyüpoglu I, Buchfelder M, Fietkau R (2016) Recurrent glioblastoma: who receives tumor specific treatment and how often? J Neurooncol 1–8. https://doi.org/10.1007/s11060-016-2079-z
Fokas E, Wacker U, Gross MW, Henzel M, Encheva E, Engenhart-Cabillic R (2009) Hypofractionated stereotactic reirradiation of recurrent glioblastomas. Strahlenther Onkol 185:235–240. https://doi.org/10.1007/s00066-009-1753-x
Shi W, Scannell Bryan M, Gilbert MR, Mehta MP, Blumenthal DT, Brown PD, Valeinis E, Hopkins K, Souhami L, Andrews DW, Tzuk-Shina T, Howard SP, Youssef EF, Lessard N, Dignam JJ, Werner-Wasik M (2017) Investigating the effect of reirradiation or systemic therapy in patients with glioblastoma after tumor progression: a secondary analysis of NRG oncology/radiation therapy oncology group trial 0525. Int J Radiat Oncol Biol Phys 100:38–44. https://doi.org/10.1016/j.ijrobp.2017.08.038
Weller M, van den Bent M, Hopkins K, Tonn JC, Stupp R, Falini A, Cohen-Jonathan-Moyal E, Frappaz D, Henriksson R, Balana C, Chinot O, Ram Z, Reifenberger G, Soffietti R, Wick W (2014) EANO guideline for the diagnosis and treatment of anaplastic gliomas and glioblastoma. Lancet Oncol 15:e395–e403. https://doi.org/10.1016/S1470-2045(14)70011-7
Straube C, Scherb H, Gempt J, Bette S, Zimmer C, Schmidt-Graf F, Schlegel J, Meyer B, Combs SE (2017) Does age really matter? Radiotherapy in elderly patients with glioblastoma, the Munich experience. Radiat Oncol 12:77. https://doi.org/10.1186/s13014-017-0809-9
Straube C, Combs SE (2017) Kombination von Strahlentherapie mit Temozolomid bei über 65-jährigen Glioblastompatienten. Strahlentherapie Onkol 193:510–512. https://doi.org/10.1007/s00066-017-1134-9
Kessel KA, Hesse J, Straube C, Zimmer C, Schmidt-Graf F, Schlegel J, Meyer B, Combs SE (2017) Validation of an established prognostic score after re-irradiation of recurrent glioma. Acta Oncol (Madr) 56:422–426. https://doi.org/10.1080/0284186X.2016.1276621
Kazmi F, Yu ·, Soon Y, Yiat ·, Leong H, Wee ·, Koh Y, Vellayappan B (2018) Re-irradiation for recurrent glioblastoma (GBM): a systematic review and meta-analysis. J Neurooncol. https://doi.org/10.1007/s11060-018-03064-0
Xu Y, Rong X, Hu W, Huang X, Li Y, Zheng D, Cai Z, Zuo Z, Tang Y (2018) Bevacizumab monotherapy reduces radiation-induced brain necrosis in nasopharyngeal carcinoma patients: a randomized controlled trial. Int J Radiat Oncol 101:1087–1095. https://doi.org/10.1016/j.ijrobp.2018.04.068
Levin VA, Bidaut L, Hou P, Kumar AJ, Wefel JS, Bekele BN, Prabhu S, Loghin M, Gilbert MR, Jackson EF (2011) Randomized double-blind placebo-controlled trial of bevacizumab therapy for radiation necrosis of the central nervous system. Int J Radiat Oncol Biol Phys 79:1487–1495. https://doi.org/10.1016/j.ijrobp.2009.12.061
Acknowledgements
To our patients.
Author information
Authors and Affiliations
Contributions
CS designed the study, collected and analyzed the data and prepared the manuscript. SA collected some data and revised the manuscript. FSG, JG, CZ, JS, and BM gave important intellectual input and carefully revised the manuscript. SC supervised the work and revised the manuscript. All authors approved the final version for submission.
Corresponding author
Ethics declarations
Conflict of interest
Christoph Straube: received a scholarship from Medac GmbH; received a travel grant from NovoCure Ltd.; contributed to a brochure for patients about GBM which was partially sponsored by NovoCure Ltd. Received Speakers Honoria from Teva Pharmaceutical Industries Ltd. Jens Gempt and Bernhard Meyer: work as consultants for BrainLab. Friederike Schmidt-Graf: served as an author for Medac GmbH. Claus Zimmer: has served on scientific advisory boards for Philips and Bayer Schering; serves as co-editor on the Advisory Board of Clinical Neuroradiology; has received speaker honoraria from Bayer-Schering and Philips and has received research support and investigator fees for clinical studies from Biogen Idec, Quintiles, MSD Sharp & Dome, Boehringer Ingelheim, Inventive Health Clinical UK Ltd., Advance Cor, Brainsgate, Pfizer, Bayer-Schering, Novartis, Roche, Servier, Penumbra, WCT GmbH, Syngis, SSS International Clinical Research, PPD Germany GmbH, Worldwide Clinical Trials Ltd., Phenox, Covidien, Actelion, Medivation, Medtronic, Harrison Clinical Research, Concentric, Penumbra, Pharmtrace, Reverse Medical Corp., Premier Research Germany Ltd., Surpass Medical Ltd. and GlaxoSmithKline. Stephanie E. Combs: has served on Advisory Board of Bristol-Myers-Squibb (BMS), Roche, Novocure, Daiichi Synkio, Astra Zeneca, Icotec; Advisory board and Speaker’s Bureau for BrainLab; Advisory Board of Roche, Daiichi Sankyo and Varian Medial Systems. Has received Speakers Honoraria from BrainLab, Accuray, Dr. Sennewald, BMS, Astra Zeneca, Roche, Varian Medical Systems, Icotec, Elekta, Novocure and Medac GmbH. Stefanie Antoni has nothing to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required. We obtained a positive ethical vote of the ethical committee at Klinikum rechts der Isar, Technical University of Munich (Project Number 408/14).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Straube, C., Antoni, S., Gempt, J. et al. Re-irradiation in elderly patients with glioblastoma: a single institution experience. J Neurooncol 142, 327–335 (2019). https://doi.org/10.1007/s11060-019-03101-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-019-03101-6