Abstract
The diagnosis of glioblastoma (GBM) often carries a dismal prognosis, with a median survival of 14.6 months. A particular challenge is the diagnosis of GBM in the elderly population (age > 75 years), who have significant comorbidities, present with worse functional status, and are at higher risk with surgical treatments. We sought to evaluate the impact of current GBM treatment, specifically in the elderly population. The authors undertook a retrospective review of all patients aged 75 or older who underwent treatment for GBM from 1997 to 2016. Patient outcomes were evaluated with regards to demographics, surgical variables, postoperative treatment, and complications. A total of 82 patients (mean age 80.5 ± 3.8 years) were seen. Most patients presented with confusion (57.3%) and associated comorbidities, and prior anticoagulation use was common in this age group. Extent of resection (EOR) included no surgery (9.8%), biopsy (22.0%), subtotal resection (40.2%), and gross-total resection (23.2%). Postoperative adjuvant therapy included temozolomide (36.1%), radiation (52.5%), and bevacizumab (11.9%). A mean overall survival of 6.3 ± 1.2 months was observed. There were 34 complications in 23 patients. Improved survival was seen with increased EOR only for patients without postoperative complications. A multivariate Cox proportional hazards model showed that complications (HR = 5.43, 95% CI 1.73, 17.04, p = 0.004) predicted poor outcome. Long-term survivors (> 12 months survival) and short-term survivors had similar median preoperative Karnofsky Performance Scale (KPS) score (80 vs. 80, p = 0.43), but long-term survivors had unchanged postoperative KPS (80 vs. 60, p = 0.02) and no complications (0/9 vs. 23/72, p = 0.04). The benefit of glioblastoma treatment in our series was limited by the postoperative complications and KPS. Presence of a complication served as an independent risk factor for worsened overall survival in this age group. It is likely that decreased patient function limits postoperative adjuvant therapy and predisposes to higher morbidity especially in this age group.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
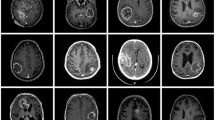
Glioblastoma (GBM) is the most aggressive primary brain tumor in adults and delivers an especially poor prognosis in elderly patients [13]. It is well established that extent of resection (EOR) is associated with better prognosis in the general population [20]. Maximal safe resection, with a goal of gross-total resection (GTR), has been associated with improved overall survival (OS) [4, 9]. Previous studies have reported significantly improved survival with resection thresholds of ≥ 98%, [7, 12] > 95%, [4] and > 78%, [21] while other studies have endorsed supratotal resection [3, 23]. Because of the infiltrative nature of GBM, it has recently been suggested that extended resection (> 53%) of tissue beyond the region that enhances with contrast on T2/FLAIR (fluid-attenuated inversion recovery) magnetic resonance imaging (MRI) may confer additional significant survival [14].
Whereas the benefits of maximal safe resection are irrefutable in younger patients, the management of elderly patients with GBM remains controversial. Elderly patients may present with diminished functional status at the time of diagnosis, be subject to additional comorbidities compared with younger patients, and show a slower recovery. The landmark study by Stupp et al., in which patients received maximal safe resection with radiotherapy and temozolomide, excluded patients aged > 70 years [24]. Because of the paucity of clinical evidence directed specifically at the elderly patient population, neither maximal resection nor cautious management has been thoroughly substantiated in improving the mortality in this age group. Because of the limited evidence regarding treatment in the elderly, we evaluated the current standard of care in the treatment of glioblastoma to determine whether this patient population differs with respect to complications and outcome after surgical resection.
Methods
Patient sample
After institutional board review approval, a retrospective review of all consecutive patients seen from November 1995 through December 2016 was performed. All patients aged > 75 years with GBM (World Health Organization grade IV astrocytoma) were included. Patients either underwent pathological diagnosis or were strongly suspected to demonstrate GBM on imaging based on T1 contrast-enhanced sequences. Demographic, surgical, and pathological variables were collected. Karnofsky Performance Score (KPS) was identified retrospectively by chart review. Patients with missing or incomplete data were excluded. For surgical resection, subtotal resection defined lesions with postoperative residual tumor while gross-total resection included lesions without postoperative residual. Residual tumor was identified by the presence of postcontrast enhancement on T1 imaging not seen on non-contrast T1 imaging.
Statistical analysis
All continuous data were summarized as means ± standard deviation. Continuous variables were analyzed by t-test and discrete variables were analyzed by Mann–Whitney U test or Chi-squared test. Kaplan–Meier survival analysis was performed, and a Cox proportional hazards model was created. All variables with a p < 0.05 on a univariate analysis were entered into a multivariate model. Statistical analysis was performed with SPSS (V20.0, IBM, Armonk, NY), with a p < 0.05 considered statistically significant.
Results
Patient characteristics
A total of 82 patients with a mean age of 80.5 ± 3.8 years were identified in this study (Table 1). The most common presenting symptom was confusion (57.3%), but patients presented with a wide array of symptoms, including weakness (19.5%), language deficits (15.9%), headaches (12.2%), seizure (8.5%), gait imbalance (8.5%), falls (6.1%), memory deficits (4.9%), and visual deficits (3.7%). Comorbidities included hypertension (43.9%), cardiac disease (25.6%; e.g., atrial fibrillation, coronary artery disease, stents, coronary artery bypass graft), cancer (15.9%), diabetes (13.4%), and venous thromboembolism (8.5%; e.g., deep vein thrombosis, pulmonary embolism). Prior anticoagulation use included aspirin (23.2%), warfarin (8.5%), and other drugs (2.4%).
Tumors were most often located in the temporal lobe (25.6%), but lesions were also found in the parietal (20.7%), frontal (17.1%), combined supratentorial lobes (13.4%), and occipital (9.8%) areas (Table 2). Evaluation of preoperative imaging studies suggested that GBM was highly suspected in 54/82 (66%) of patients by the attending neuroradiologist based on radiology imaging reports, but present on the differential diagnosis of all patients in this age group. Most patients underwent a subtotal resection (STR, 40.2%); smaller numbers of patients had GTR (23.2%), biopsy (22.0%), or no surgery (9.8%). Surgical adjuncts included stealth neuronavigation (89.6%) and intraoperative MRI (IMRIS, 9.0%). The median preoperative and postoperative KPS scores were 80 and 70, respectively. Tumor isocitrate dehydrogenase (IDH) status was wild-type in 26.8% and mutant in 1.2%, but unknown in 71.2%; similarly, O-6-methylguanine-DNA methyltransferase (MGMT) status was unknown in most patients (74.3%) but was methylated in 14.6% and unmethylated in 11.0%. Patients underwent postoperative temozolomide (36.1%), radiation (52.5%), bevacizumab (11.9%), or other (4.9%) treatment; however, a sizeable portion did not undergo postoperative therapy (20.7%). The mean length of stay was 7 ± 6 days. A mean OS of 6.5 ± 1.2 months was observed along with a median (50%) survival of 3.0 ± 1.0 months.
Complications
Postoperative complications included 34 events in 23 patients (31.9%) (Table 3). Major complications, requiring medical or surgical treatment, accounted for 76.4% of the complications while minor complications accounted for 23.5% of all complications. Postoperative neurological deficits (29.4%) were most common; other complications were postoperative hemorrhage (11.8%) and readmission within 30 days for uncontrolled pain or headache (8.8%), cardiac dysfunction (5.8%), altered mental status (5.8%), stroke (5.8%), transfusion (2.9%), coagulopathy (2.9%), conversion to craniotomy from biopsy due to hemorrhage (2.9%), cerebrospinal fluid leak (2.9%), urinary tract infection (2.9%), status epilepticus (2.9%), unexpected postoperative seizure (2.9%), tracheostomy (2.9%), respiratory distress (2.9%), pneumonia (2.9%), and venous thromboembolism (2.9%). A breakdown of major and minor complications showed a higher tendency for complications to occur with greater EOR. Univariable and multivariable logistic regression analysis of complication was performed (Table 4). Univariable analysis showed that age (OR [odds ratio] = 1.16, 95% confidence interval [CI] 1.01–1.34), postoperative KPS (OR = 0.9, 95% CI 0.85–0.95), and length of stay (OR = 1.11, 95% CI 1.01–1.23) predicted poor outcome; however, on multivariable analysis only postoperative KPS (OR = 0.89, 95% CI 0.96–1.49) predicted a complication after controlling for age and length of stay. Thus, patients with a lower postoperative KPS were more likely to have a complication.
The distribution of change in median KPS is shown in Fig. 1a for patients with complications, in Fig. 1b based on IDH-1 status, and in Fig. 1c based on MGMT methylation status. Overall, 41.5% of patients (n = 34) showed a decline in postoperative KPS, 2.4% (n = 2) showed an improved postoperative KPS, 37.8% (n = 31) had an unchanged KPS, and 18.3% (n = 15) had insufficient information to determine a KPS change. The median preoperative KPS did not differ between patients with and without complications (80 and 80, p = 0.83, Mann–Whitney U test), respectively, but the median postoperative KPS was significantly lower for patients with complications (75 and 55, p = 0.003, Mann–Whitney U test). The median change in KPS (postoperative minus preoperative) was − 20 and 0 for patients with and without complications, respectively. Similarly, while median preoperative KPS did not differ between patients with no, minor, or major complications (80 vs. 80 vs. 80, p = 0.86, Kruskal–Wallis test), there was a significant decrease in median postoperative KPS with either minor or major complications (75 vs. 55 vs. 55, p = 0.0001, Kruskal–Wallis test). There was a significant decrease in median change in KPS for patients with either minor or major complication (0 vs. − 20 vs. − 20, p = 0.0001, Kruskal–Wallis). These results suggest a similar decrease in KPS for elderly patients with either minor or major complications.
Change in Karnofsky Performance Status score in patients with and without complication, isocitrate dehydrogenase 1 mutation, and O-6-methylguanine-DNA methyltransferase methylation. a Change in KPS (postoperative minus preoperative) in patients with and without complication are shown. Although a similar median preoperative KPS (80 vs. 80, p = 0.83) was seen in the two groups, postoperative KPS (75 vs. 55, p = 0.003) was significantly lower in patients who experienced complications. Rate of change in KPS by patient IDH-1 b and MGMT methylation c status
Overall survival prediction
Kaplan–Meier survival analysis was used to evaluate the effect of EOR, surgical adjuvants, and complications on OS. When survival was assessed based on the volume of resection (Fig. 2a), a greater resection volume was significantly associated with a longer mean OS: no surgical treatment (0.8 ± 0.3 months), biopsy (3.7 ± 1.1 months), STR (5.0 ± 1.4 months), and GTR (12.1 ± 3.0 months) (p < 0.0001, Log-rank test). Similarly, evaluation of OS associated with postoperative adjuvant therapies—no treatment (1.7 ± 0.4 months), radiation only (4.9 ± 1.1 months), temozolomide (11.4 ± 6.1 months), and radiation plus temozolomide (16.8 ± 2.7 months)—indicated significantly better survival with greater therapy (p < 0.0001, Log-rank test) (Fig. 2b). Survival was also evaluated separately in patients with or without a complication (Fig. 2c, d). Significantly longer survival was seen with greater resection margins in patients who did not have a complication (p = 0.003), but no improvement in survival was seen with greater resection volume if the patient had an identified complication (p = 0.87); in fact, survival was significantly shorter than expected (OS 1.7 ± 0.4 months) for patients with complications.
Kaplan–Meier survival curves for elderly patients with GBM. Mean ± SE of the mean (SEM) overall survival (OS) of 6.5 ± 1.2 months was seen. a OS for patients who had no surgical treatment (0.8 ± 0.3 months) and those who had biopsy (3.7 ± 1.1 months), STR (5.0 ± 1.4), and GTR (12.1 ± 3.0) were significantly different (p < 0.0001). b Survival was significantly longer in patients who had more aggressive adjuvant treatment: no treatment (1.7 ± 0.4), radiation only (4.9 ± 1.1), temozolomide (11.3 ± 6.1), and radiation plus temozolomide (16.8 ± 2.7) (p < 0.0001). c, d Complications affected the length of OS. In patients who had no complications (c), survival improved with greater extent of resection (EOR): no surgical treatment (1.0 ± 0.7), biopsy (4.1 ± 1.2), STR (7.8 ± 2.3), and GTR (16.0 ± 3.6) (p < 0.003). Survival with no adjuvant therapy (4.4 ± 1.1), radiation only (12.3 ± 2.8), TMZ (29.7 ± 18.8 months) and combined radiation and TMZ (40.9 ± 7.3) were significantly different (p < 0.0001). d On the other hand, in patients who experienced complications, there was no difference in length of OS with greater EOR: biopsy (1.1 ± 0.2), STR (1.7 ± 0.5), GTR (1.8 ± 0.6) (p = 0.87). A log-rank test was used for all comparisons. GTR gross total resection, STR subtotal resection, RT radiotherapy, TMZ temozolomide
Univariate and multivariate Cox proportional hazards models were used to identify variables affecting OS (Table 5). Univariate analysis suggested that preoperative KPS (Hazard ratio [HR] = 0.97, 95% CI 0.95–0.99), postoperative KPS (HR = 0.96, 95% CI 0.94–0.98), adjuvant radiotherapy (HR = 0.28, 95% CI 0.15–0.51), adjuvant temozolomide (HR = 0.17, 95% CI 0.09–0.34), adjuvant bevacizumab (HR = 0.02, 95% CI 0.06–0.68), complications (HR = 3.12, 95% CI 1.71–5.68), and length of stay (HR = 1.04, 95% CI 1.001–1.083) were most predictive of poorer OS. In addition, a greater EOR predicted a reduced HR: no surgery (reference), biopsy (HR = 0.22, 0.08–0.66), STR (HR = 0.22, 0.08–0.59), GTR (HR = 0.093, 0.03–0.285). On multivariate analysis, only the presence of a complication (HR = 5.43, 95% CI 1.73–17.04) significantly affected OS after controlling for other factors.
Long-term survivors
Patients living < 12 months were similar to those living ≥ 12 months (long-term survivors) in age (80.8 ± 3.8 vs. 78.7 ± 3.4, p = 0.12) and EOR (p = 0.06) (Table 6), but there was a significant difference in preoperative KPS (75 ± 12 vs. 84 ± 5, p = 0.04), postoperative KPS (65 ± 16 vs. 80 ± 7, p = 0.007), and use of adjuvant therapy (p = 0.003). Long-term survivors were also less likely to have complications (23 vs. 0, p = 0.04).
Discussion
Although the results of this study support several well-known aspects of glioblastoma treatment, they also demonstrate the nuances of treatment in the elderly. Our results supported the benefits of greater EOR and postoperative adjuvant therapy in the elderly. However, our results also support that postoperative complications and lower KPS resulted in significantly shorter survival. Patients with long-term survival showed sustained postoperative KPS and were less likely to have postoperative complications.
Our study suggests the potential for reduced survival in the elderly treated with GBM. A number of factors may contribute to the less robust survival benefit seen in the elderly. Patients ≥ 75 years generally undergo less extensive surgeries, or no surgery at all, compared with younger patients [15]. Although more aggressive resection may improve survival, such an approach also increases the risk of neurological deficits and diminished postoperative performance status and may be attempted less often in elderly patients. While several studies indicate improved survival with greater EOR, these studies have involved a younger subset of elderly patients (median 61 to 75 years across studies) [2, 17, 22, 26]. Poor KPS and cognitive deficits have been associated with worse outcomes in adult patients [1, 5, 20], and an increased combination of unfavorable symptoms as seen in elderly patients may further diminish survival [5]. Polypharmacy and comorbid conditions frequently observed in the elderly may also contraindicate the overall benefits of surgery [25]. Our study showed many of these features including significant rates of comorbidity, lower overall function (e.g., KPS) both before and after surgery, common presentation with confusion, and significant anticoagulation use in this patient population. Postoperative KPS was the only factor that predicted complications, although it is unclear whether this was immediately postoperative or at the end of the hospitalization. Finally, postoperative complications may prohibit patients from receiving potentially beneficial adjuvant therapies, and elderly patients may be excluded from clinical trials because of their comorbidities, making it more difficult to extend survival even following a gross-total tumor resection.
Neurosurgery in the elderly
There are special considerations during neurosurgical care of elderly patients. Chibbaro et al. [6] found a longer LOS in elderly patients compared with the general population, suggesting longer times for recovery. The effect of traditional radiotherapy and/or chemotherapy for the treatment of GBM in the elderly has been less than robust [8, 18, 19]. Other studies have also shown that the elderly show worse outcomes simply as a function of age during the treatment of aneurysms, [16] spinal deformity, [11] and meningiomas [10], among other diseases. Another interesting element to consider is that there was a suspicion of GBM based on reports from preoperative imaging in 54/82 (66%) patients in our study, as well as a strong suspicion as the leading diagnosis in all cases. This raises the question of whether “confirming” the diagnosis via surgical removal of tumor is necessary in cases where the patient may experience multiple medical comorbidities. Certainly misdiagnosis and subsequently incorrect treatment would be considerations without tissue diagnosis. The results of our study support the potential for reduced survival in the elderly especially those experiencing complications. A surgical strategy aiming to obtain tissue diagnosis while minimizing complications may be warranted in this age group.
We did include 8 patients in this study who were presumed to have GBM based on MRI imaging but did not undergo surgery to confirm pathologic diagnosis. Two of these patient elected to go to hospice and did not receive any adjuvant therapies. One patient elected to try radiation alone acknowledging that this was not standard of care. He passed away 51 days after diagnosis. One patient had recently undergone a renal transplant and was deemed to sick for surgical intervention. The remaining patients underwent a combination of adjuvant chemotherapy/radiation based on imaging results, oncology input, and patient/family preference. The authors acknowledge that treating without a tissue diagnosis is not current standard of care.
Limitations
One limitation to our study involves its single-center retrospective nature and the incomplete information regarding mutational status of tumors. The effect of tumor mutation on glioblastoma is well known. Many of the patients in this series underwent treatment prior to the availability of widespread testing for specific gene mutations, but it is likely these patients had primary glioblastoma with a low number of IDH-1 mutations. In addition, the duration of completed postoperative chemotherapy and radiotherapy was not available in this patient group. The patients in our study also did not benefit from newer treatments that have shown survival benefit in glioblastoma patients, such as laser interstitial thermal ablation and the Optune device [19].
Conclusions
This study supports the role of maximal safe resection and postoperative adjuvant therapy in the treatment of glioblastoma of the elderly. However, it emphasizes that patient complications and KPS status play important roles in prognosis as well. These data may be helpful in the guidance of patients and in surgical decision-making.
References
Alvarez de Eulate-Beramendi S, Alvarez-Vega MA, Balbin M, Sanchez-Pitiot A, Vallina-Alvarez A, Martino-Gonzalez J (2016) Prognostic factors and survival study in high-grade glioma in the elderly. Br J Neurosurg 30:330–336
Babu R, Komisarow JM, Agarwal VJ, Rahimpour S, Iyer A, Britt D et al (2016) Glioblastoma in the elderly: the effect of aggressive and modern therapies on survival. J Neurosurg 124:998–1007
Bauchet L, Mathieu-Daude H, Fabbro-Peray P, Rigau V, Fabbro M, Chinot O et al (2010) Oncological patterns of care and outcome for 952 patients with newly diagnosed glioblastoma in 2004. Neuro Oncol 12:725–735
Bloch O, Han SJ, Cha S, Sun MZ, Aghi MK, McDermott MW et al (2012) Impact of extent of resection for recurrent glioblastoma on overall survival: clinical article. J Neurosurg 117:1032–1038
Chaichana KL, Chaichana KK, Olivi A, Weingart JD, Bennett R, Brem H et al (2011) Surgical outcomes for older patients with glioblastoma multiforme: preoperative factors associated with decreased survival. Clinical article. J Neurosurg 114:587–594
Chibbaro S, Di Rocco F, Makiese O, Mirone G, Marsella M, Lukaszewicz AC et al (2010) Neurosurgery and elderly: analysis through the years. Neurosurg Rev 34:229–234
Grabowski MM, Recinos PF, Nowacki AS, Schroeder JL, Angelov L, Barnett GH et al (2014) Residual tumor volume versus extent of resection: predictors of survival after surgery for glioblastoma. J Neurosurg 121:1115–1123
Guedes de Castro D, Matiello J, Roa W, Ghosh S, Kepka L, Kumar N et al (2017) Survival outcomes with short-course radiation therapy in elderly patients with glioblastoma: data from a randomized phase 3 trial. Int J Radiat Oncol Biol Phys 98:931–938
Hardesty DA, Sanai N (2012) The value of glioma extent of resection in the modern neurosurgical era. Front Neurol 3:140
Ikawa F, Kinoshita Y, Takeda M, Saito T, Yamaguchi S, Yamasaki F et al (2017) Review of current evidence regarding surgery in elderly patients with meningioma. Neurol Med Chir 57: 521–533
Jain A, Hassanzadeh H, Puvanesarajah V, Klineberg EO, Sciubba DM, Kelly MP et al (2017) Incidence of perioperative medical complications and mortality among elderly patients undergoing surgery for spinal deformity: analysis of 3519 patients. J Neurosurg Spine 27: 534–539
Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F et al (2001) A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg 95:190–198
Laperriere N, Weller M, Stupp R, Perry JR, Brandes AA, Wick W et al (2013) Optimal management of elderly patients with glioblastoma. Cancer Treat Rev 39:350–357
Li YM, Suki D, Hess K, Sawaya R (2016) The influence of maximum safe resection of glioblastoma on survival in 1229 patients: Can we do better than gross-total resection? J Neurosurg 124:977–988
Noorbakhsh A, Tang JA, Marcus LP, McCutcheon B, Gonda DD, Schallhorn CS et al (2014) Gross-total resection outcomes in an elderly population with glioblastoma: a SEER-based analysis. J Neurosurg 120:31–39
Ohkuma H, Shimamura N, Naraoka M, Katagai T (2017) Aneurysmal subarachnoid hemorrhage in the elderly over age 75: a systematic review. Neurol Med Chir 57: 575–583
Oszvald A, Guresir E, Setzer M, Vatter H, Senft C, Seifert V et al (2012) Glioblastoma therapy in the elderly and the importance of the extent of resection regardless of age. J Neurosurg 116:357–364
Park M, Lee SK, Chang JH, Kang SG, Kim EH, Kim SH et al (2017) Elderly patients with newly diagnosed glioblastoma: can preoperative imaging descriptors improve the predictive power of a survival model? J Neurooncol 134:423–431
Perry JR, Laperriere N, O’Callaghan CJ, Brandes AA, Menten J, Phillips C et al (2017) Short-course radiation plus temozolomide in elderly patients with glioblastoma. N Engl J Med 376:1027–1037
Sanai N, Berger MS (2008) Glioma extent of resection and its impact on patient outcome. Neurosurgery 62:753–764
Sanai N, Polley MY, McDermott MW, Parsa AT, Berger MS (2011) An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg 115:3–8
Scott JG, Suh JH, Elson P, Barnett GH, Vogelbaum MA, Peereboom DM et al (2011) Aggressive treatment is appropriate for glioblastoma multiforme patients 70 years old or older: a retrospective review of 206 cases. Neuro Oncol 13:428–436
Stummer W, Reulen HJ, Meinel T, Pichlmeier U, Schumacher W, Tonn JC et al (2008) Extent of resection and survival in glioblastoma multiforme: identification of and adjustment for bias. Neurosurgery 62:564–576
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Torrance AD, Powell SL, Griffiths EA (2015) Emergency surgery in the elderly: challenges and solutions. Open Access Emerg Med 7:55–68
Zhang C, Wang X, Hao S, Su Z, Zhang P, Li Y et al (2016) Analysis of treatment tolerance and factors associated with overall survival in elderly patients with glioblastoma. World Neurosurg 95:77–84
Acknowledgements
We thank Kristin Kraus, M.Sc., for her editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karsy, M., Yoon, N., Boettcher, L. et al. Surgical treatment of glioblastoma in the elderly: the impact of complications. J Neurooncol 138, 123–132 (2018). https://doi.org/10.1007/s11060-018-2777-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-2777-9