Abstract
To examine the impact of glutamate on post-operative seizures and survival in a cohort of patients with grade II to IV supratentorial glioma. A retrospective analysis was performed on 216 patients who underwent surgery for supratentorial gliomas. Primary explanatory variables were peritumoural and/or tumoural glutamate concentrations, glutamate transporter expression (EAAT2 and SXC). Univariate and multivariate survival analysis was performed with primary outcomes of time to first post-operative seizure and overall survival. Subgroup analysis was performed in patients with de novo glioblastomas who received adjuvant chemoradiotherapy. 47 (21.8 %), 34 (15.8 %) and 135 (62.5 %) WHO grade II, III and IV gliomas respectively were followed for a median of 15.8 months. Following multivariate analysis, there was a non-significant association between higher peritumoural glutamate concentrations and time to first post-operative seizure (HR 2.07, CI 0.98–4.37, p = 0.06). In subgroup analysis of 81 glioblastoma patients who received adjunct chemoradiotherapy, peritumoural glutamate concentration was significantly associated with time to first post-operative seizure (HR 3.10, CI 1.20–7.97, p = 0.02). In both the overall cohort and subgroup analysis no glutamate cycle biomarkers were predictive of overall survival. Increased concentrations of peritumoural glutamate were significantly associated with shorter periods of post-operative seizure freedom in patients with de novo glioblastomas treated with adjuvant chemoradiotherapy. No glutamate cycle biomarkers were predictive of overall survival. These results suggest that therapies targeting glutamate may be beneficial in tumour associated epilepsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Seizures commonly occur in patients with supratentorial gliomas. Such tumour associated epilepsy (TAE) is not controlled by antiepileptic drug therapy in approximately a third of patients [1–4]. Poor seizure control is associated with a worsening of quality of life and cognitive function within this population [5]. The precise neurobiological mechanisms underpinning the development of epilepsy and pharmacoresistance in patients with gliomas are uncertain.
Alterations within glutamate homeostasis however, appear to play a pivotal role in epileptogenesis in patients with gliomas, particularly in the peritumoural region [6–9]. Under physiological conditions, to prevent aberrant signalling, glutamate is cleared rapidly from the extracellular space by excitatory amino acid transporters (EAAT), predominantly EAAT2, in astrocytes [10]. Glutamate is also shuttled back into the extracellular space in exchange for cystine by system xC (SXC) transporter in order to participate in metabolism of the potent anti-oxidant glutathione [11].
Glioma cells have been found to upregulate SXC expression [9, 12] leading to generation of greater amounts of protective glutathione, which may confer a survival advantage to tumour cells in hypoxic microenvironments. The resultant increase in extra-cellular glutamate excessively activates glutamate receptors causing excitotoxicity to peri-tumoural structures and promoting tumour growth and invasion [9, 13–16]. Tumours also mediate the down regulation of EAAT2, which impairs the region’s ability to re-uptake glutamate, creating an environment favouring tumour growth [17]. These changes to the glutamate cycle enhance the survival, growth and invasive abilities of gliomas in cell based and murine models.
Increased peritumoural glutamate concentrations were shown to induce epileptiform activity in glioma implanted mice [6] under the influence of glutamate release from the SXC transporter [7]. Our research group recently examined glutamate homeostasis in 288 patients with supratentorial gliomas [8], finding an association between higher tumoural and peri-tumoural glutamate concentrations and pre-operative seizures. It is unknown whether glutamate may also play a role in post-operative seizures, or overall survival. However, such a role would provide a therapeutic target in glioma and TAE treatment.
In the present analysis, we examined the association between glutamate cycle changes, post-operative seizures and survival in a cohort of patients with grade II to IV supratentorial glioma followed up post-operatively. We hypothesized that these changes in the glutamate cycle might also be associated with post-operative seizures and shorter overall survival in patients with gliomas.
Materials and methods
Patient selection
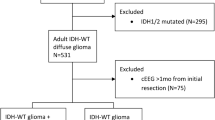
Subjects were selected from a database of 221 patients who underwent craniotomy at the Royal Melbourne Hospital (RMH) or Melbourne Private Hospital (MPH) between 2003 and 2011 for supratentorial glioma, and had peritumoural and/or tumoural tissue sampled for glutamate cycle biomarker analysis (defined below). 175 patients from this database had already been included in an early analysis by our research group examining glutamate and pre-operative seizures [8]. Demographic, glutamate molecular analysis and pre-operative seizure information were the only data points utilized from this previous study.
Inclusion criteria were (a) histopathological diagnosis of WHO grade II, III or IV glioma (as determined by an anatomical neuropathologist), and (b) available follow-up to determine at least one month of post-operative seizure history.
Clinico-pathological data collection
Clinical data were collected from medical records and the Australian Cancer Grid database as part of the BioGrid Australia™ clinical informatics system [18]. The author collecting data was blinded to molecular results. The clinicopathological variables collected were gender, age and histopathological diagnosis at the time of glutamate cycle biomarker analysis, date of first histological diagnosis, side and lobe of lesion. Collected oncological treatment data included the extent of surgery, post-operative chemotherapy and radiotherapy use. Surgery was classified as gross macroscopic resection, subtotal resection (50–95 %), partial resection (less than 50 %) or biopsy. Extent of resection was most commonly determined by post-operative MRI, and was obtained from the multi-disciplinary meeting record or neurosurgical correspondence.
The peritumoural biopsy was within 1 cm of the tumour margin, judged intra-operatively by the surgeon, determined by macroscopic appearance and MRI-guided surgical navigation. Radiologically it was defined as the region outside the FLAIR signal for low grade gliomas and the region outside contrast enhancement for high grade gliomas. The location of peritumoural tissue was determined on an individual basis. The majority of peritumoural samples were taken from white matter.
Seizures and epilepsy were defined in accordance with international classification [19]. TAE was defined as one or more seizures occurring in the presence of a supratentorial glioma. Pre-operative seizures were defined as seizures, attributable to the glioma, occurring before the patient’s first surgery. Time to first post-operative seizure in the first 12 months following glutamate biomarker analysis was collected. When an exact time was not documented in the medical record, it was estimated by the mid time point over the interval that the seizure occurred. Estimation of time to first seizure occurred in 16.7 %.
Patients were followed up until July 2014 or until death or referral to a palliative care service and discharge from specialist follow-up. Overall survival was defined as time from initial histological diagnosis until last follow-up.
Epilepsy treatment
An anti-epileptic drug was commenced following first seizure attributable to a glioma. Pre-operatively, most patients without a seizure were also prescribed a prophylactic AED by the treating neurosurgeon. Post-operatively, all patients were followed by either a neurosurgeon and/or medical oncologist who undertook initial seizure management. Patients with seizures difficult to control were referred to an epileptologist. In general, patients were initially treated with single anti-epileptic drug. Dose adjustment and drug changes were made based on clinical response in terms of seizure control and adverse effects. Serum AED levels were monitored as clinically indicated. Prophylactic AED was generally ceased after a period of 3–6 months of seizure freedom.
Molecular analysis
The primary independent variables were tumoural and peri-tumoural glutamate cycle biomarkers. Biopsy of brain adjacent to tumour provided the peri-tumoural tissue sample. Biopsy location was judged by the neurosurgeon with the aid of stereotactic MRI-guided navigation. Tumour and peritumoural tissue samples were analysed for glutamate cycle biomarkers including protein concentration of glutamate, EAAT2 transporter and SXC transporter, as previously described [8, 20]. High-performance chromatography was utilized to determine tissue concentration of glutamate. Western blotting was used to quantify the expression of EAAT2 and SXC transporters using integrated optical density (IOD) for protein bands normalized against IOD values for actin [8].
Outcomes
The primary endpoints were time to first post-operative seizure up to 12 months following resection, and overall survival. The 12 month seizure outcome was chosen to minimize the confounding factor of survival on seizure incidence, given the high proportion of glioblastoma patients in the cohort and small number alive after 12 months.
Subgroup analysis
Patients with de novo glioblastomas who received subsequent chemo-radiotherapy were selected for a subgroup analysis. This group represented a relatively more homogenous population which is commonly enrolled in clinical trials.
Statistical analysis
Univariate survival analysis was performed with cox regression. A log transformation was used to convert glutamate cycle biomarkers (glutamate, EAAT2 and SXC) to a normal distribution. A p value <0.2 was chosen to select variables to be included in multivariate analysis using cox regression. A backwards stepwise regression was performed to remove the most non-significant variables from the model. A p value of <0.05 was considered to indicate statistical significance on multivariate analysis. Hazard ratios are presented with 95 % confidence intervals (CIs). Kaplan–Meier curves were utilized to display overall survival with a log-rank test employed to compare survival curves. Given there is no normal range for glutamate concentrations, a level greater or equal to the median was deemed ‘high’ for Kaplan–Meier analysis. Given the high drop out of patients (30 % by 6 months and 31 % by 12 months) due to death, the ‘time to event’ approach was deemed more statistically appropriate than an actuarial method for analysis of seizure freedom. All analyses were performed with SPSS-version 22 (SPSS Inc., Chicago, IL).
Ethics
This study protocol was approved by the Melbourne Health Human Research and Ethics Committee (HREC 2006.199). All patients in this study (or their families) gave written informed consent to participate. The authors confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Results
Patient cohort
Of the 221 subjects in the database, 216 were included for analysis (Table 1). Five patients were excluded; one had cerebellar glioma, one had ependymoma, and three had less than one month of follow-up. One hundred and seventy patients from this cohort were included in a previous published analysis [8].
Patients were followed up for a median of 15.8 months. Grade II gliomas had a follow-up of 63.7 months; Grade III gliomas 32.1 months; Grade IV gliomas 10.1 respectively. 81 patients with de novo glioblastomas treated with chemoradiotherapy were examined in a subgroup analysis (Supplementary Table 1). 68 (83.9 %) within this subgroup received Stupp protocol adjuvant therapy, and those who didn’t were treated before this regimen became standard of care in 2005 [21].
Anti-epileptic drug use
Post-operative AED data was available in 205 (94.9 %) of patients. 28 (12.9 %) patients had their AED withdrawn for at least 6 months due to seizure control. 93 patients from the entire cohort had post-operative seizures and 94.6 % patients were receiving AED at the time of post-operative seizures. In the 205 subjects with AED data, phenytoin was utilized in 77.6 %, levetiracetam in 31.2 %, valproate in 19.0 % and carbamazepine in 19.0 %. Clonazepam, lamotrigine, topiramate, oxcarbazepine, clobazam, phenobarbitone, primidone, pregabalin, zonisamide and perampanel were all each used in less than 5 % of subjects. 60.5 % of subjects (124/205) were only prescribed a single AED.
Post-operative seizures
At the 12 month post-operative point, 81 patients (37.5 %) had had at least one post-operative seizure. On univariate analysis, temporal lobe location (HR 1.68), pre-operative seizures (HR 2.14), extent of surgical resection, higher peritumoural EAAT2 (HR 1.82) and higher peritumoural glutamate concentration (HR 1.36) were all associated with shorter time to first seizure (Table 2) and included in multivariate analysis. No other glutamate cycle biomarkers in tumoural or peritumoural tissue were predictive of time to first seizure, including tumoural glutamate concentration (HR 1.0). Following multivariate analysis, only extent of surgical resection was associated with time to first post-operative seizure (p = 0.04). Although it approached significance, there was no association between peritumoural glutamate concentrations and time to first post-operative seizure (HR 2.07, CI 0.98–4.37, p = 0.06). No other variables remained in the final backward regression model.
In the de novo glioblastoma with chemoradiotherapy subgroup analysis, pre-operative seizure (HR 1.83, CI 0.96–3.50, p = 0.08) and higher peritumoural glutamate concentration (HR 3.10, CI 1.20–7.97, p = 0.02, n = 56) were associated with shorter time to first post-operative seizure (Table 3). In a multivariate model (n = 56), higher peritumoural glutamate concentration remained (HR 3.10, CI 1.20–7.97, p = 0.02) the only variable significantly associated with the occurrence of post-operative seizures (Fig. 1).
Probability of seizure freedom according to glutamate concentrations Time to first post-operative seizure Kaplan–Meier survival curves. a According to peritumoural glutamate concentration n = 131, p = 0.16. b According to tumoural glutamate concentration n = 200, p = 0.98. c According to peritumoural glutamate concentration in de novo glioblastoma with adjuvant therapy subgroup, n = 56, p = 0.007. d According to tumoural glutamate concentration in de novo glioblastoma with adjuvant therapy subgroup, n = 78, p = 0.73
Survival
Overall median survival was 62.5 months (interquartile range, IQR 39.2–83.5), 32.1 months (IQR 15.7–104.3) and 10.1 months (IQR 4.6–18.0) for WHO grade II, III and IV gliomas respectively. When examining the entire glioma cohort, no tumour or peritumoural glutamate biomarkers predicted overall survival (Supplementary Table 2) (Fig. 2).
Predictors of survival were analysed in the more homogenous de novo glioblastoma with adjuvant therapy population. Overall median survival for this cohort was 14.5 months (IQR 9.7–21.7). Age at diagnosis (HR 1.0, CI 1.00–1.04, p = 0.06), lobe of lesion (p = 0.004), extent of resection (p = 0.05), tumour SXC transporter expression (HR 0.632, CI 0.32–1.26, p = 0.19, n = 44) and peritumoural glutamate concentration (HR 0.745, CI 0.52–1.08, p = 0.12, p n = 56) were associated with overall survival on univariate analysis. No glutamate cycle biomarkers were significantly prognostic in a multivariate model (Supplementary Table 3).
Discussion
This study is novel in investigating the association between tumoural and peritumoural glutamate cycle biomarkers and post-operative seizures and survival in patients with supratentorial gliomas. The major findings were that while glutamate cycle biomarkers were not associated with post-operative seizures or survival in the overall patient population, a higher peritumoural glutamate level was associated with seizure recurrence in those with de novo glioblastomas treated with chemoradiotherapy.
In gliomas, glutamate homeostasis is altered both within tumour and in the peri-tumoural region. Higher extra-cellular concentrations of glutamate have been reported in tumour and peritumoural tissue using microdialysis [22–24] and high performance liquid chromatography [6, 8]. In our previous study, the peritumoural region had significantly higher glutamate concentrations than the tumour itself, suggesting a degree of peritumoural independence [8].
Peritumoural tissue is increasingly regarded as the key structure responsible for epileptogenesis with studies suggesting ictal onset zone is in the region 1–2 mm from the tumour edge [25]. This tissue surrounding brain tumours harbours an altered microenvironment compared with normal brain [24]. An imbalance in glutamate neurotransmission has long been proposed as a key mechanism in network hyperexcitability [26, 27]. However, only recently, has upregulated glutamatergic neurotransmission been linked to seizures in rodents and pre-operative humans with gliomas [6–9]. One possible mechanism of epileptogenesis is the over excitation of peritumoural extra-synaptic NMDA receptors by excess glutamate [28].
We have shown in subgroup analysis that peritumoural glutamate concentration at time of resection predicts seizures over the subsequent 12 months. This subgroup was chosen as they represented a homogenous group with similar tumour type and adequate performance status to all receive adjuvant chemoradiotherapy. Although the subgroup size was small, the significant signal in this well controlled cohort supports the epileptogenic nature of peritumoural glutamate. One potential mechanism explaining this association is that peritumoural glutamate levels stay elevated over the course of post-operative period and directly maintain a hyperexcitable local network. Alternatively, initial peaks in peritumoural glutamate concentration may help prime a local network for seizures, potentially via priming of glutamate receptors [28].
The failure of the analysis of the whole tumour cohort to reach statistical significance may be related to the heterogeneous nature of the population. The role of glutamate cycle adaptations in lower grade gliomas have not been well studied and likely only contribute in part to the pathogenesis of TAE, with other molecular factors such as isocitrate dehydrogenase mutations [29] and impaired GABAergic inhibition [30, 31] also likely playing an important role. In addition, chemotherapy and radiotherapy have been described to have a positive impact on seizure control [32–34] and these therapies differed widely across the cohort and may have clouded the influence of glutamate.
In contrast to our work on pre-operative tumour related seizures [8], EAAT2 and SXC expression did not correlate with seizures post-operatively. Within gliomas, SXC is responsible for the majority of extra-cellular glutamate [11] and the small sample of peritumoural cases analysed for transporter expression may have been insufficient to detect a correlation.
In our analysis, ‘time to first post-operative seizure’ was selected as a primary outcome measure. This was in favour of the examining seizure frequency or freedom, as is commonly assessed in epilepsy drug trials. This ‘time to event survival analysis’ was chosen as the most appropriate method given the variability in follow-up, owing largely to the short survival of patients with grade IV gliomas.
There is a large amount of cell line and animal data suggesting that glutamate homeostasis promotes survival and tissue invasion for the glioma cells. Upregulation of SXC leads to the highly protective glutathione, an important anti-oxidant. Increased glutathione confers resistance against chemoradiotherapy [35], AMPA receptor stimulation induces tumour cell migration [13] while glutamate secretion triggers neurotoxic cell death and gives a growth advantage to gliomas [15]. Importantly, blockade of SXC, AMPA and NMDA and upregulation of EAAT2 suppress glioma growth and improves tumour survival [12–17]. Reduced expression of SXC has also been associated with prolonged overall survival in a small human cohort with grade IV gliomas [9].
Despite these preclinical findings, we did not find any of our measured glutamate cycle biomarkers to be prognostic, both when examining our cohort as a whole and within the de novo glioblastoma with adjuvant therapy subgroup. Our results are in line with clinical studies that reported lack of benefit from anti-glutamate therapy for gliomas. These included two early phase clinical trials that examined the role of sulfasalazine, a SXC antagonist as adjuvant therapy for patients with recurrent [36] and newly diagnosed high grade glioma [37]. A lack of survival benefit and significant adverse effects in both studies have limited future studies of this well studied SXC antagonist in high grade glioma patients. In addition, two studies analysed the impact of talampanel, an AMPA receptor antagonist, in glioblastoma patients and found no survival benefit [38, 39]. Our findings add doubt to the role of glutamate in determining glioblastoma survival in humans.
The main limitation of this study is its retrospective nature and small sample size. Tumour progression and subsequent therapy, both important influences on seizures, were not documented owing to the inherent inaccuracy in collecting this variable retrospectively. During the follow-up period of our study, molecular markers such as IDH1, 1p19q and ATRX were not routinely assessed. Given their now recognized prognostic implications, the absence of these markers weakens our survival analysis. Anti-epileptic treatments and the approach to drug adjustments varied across the cohort; yet importantly, only a minority of post-operative seizures occurred off AED (5.4 %). Characterization of seizure semiology (e.g. focal, generalized, status epilepticus) were not consistently available, but would have be a clinically useful addition to our analysis. Finally, the study spanned a long time period, during which neuro-oncological practices had inevitably changed, creating heterogeneity within the cohort. The examination of a larger sample would allow confirmation of our subgroup findings.
Our analysis adds to a growing body of evidence supporting glutamate in the pathogenesis of tumour associated seizures. If glutamate is indeed a useful biomarker to direct therapy against, choose patients for treatment and measure response, a non-invasive alternative to brain sampling is required [40]. Prospective imaging studies that examine post-operative seizures, tumour progression and glutamate over the course of disease will be important in further characterizing the link between glutamate adaptations and seizures. Such prospective studies will be necessary to define populations that may benefit from targeted epilepsy treatments. One exciting target is the AMPA receptor given the antagonist, perampanel, has recently been approved for use in Australia after showing efficacy as adjunctive therapy in refractory focal epilepsy.
Conclusion
Glutamate cycle biomarkers in tumoural and peritumoural tissue did not predict overall survival and adds further doubt to the role of glutamate in determining glioma survival in humans. In contrast, increased concentrations of peritumoural glutamate were associated with shorter periods of post-operative seizure freedom in patients de novo glioblastomas treated with adjuvant chemoradiotherapy. These findings suggest a hyperexcitable peritumoural network due to elevated glutamate and support this region as a target for future therapies against TAE.
References
Kerkhof M, Dielemans JC, van Breemen MS, Zwinkels H, Walchenbach R, Taphoorn MJ, Vecht CJ (2013) Effect of valproic acid on seizure control and on survival in patients with glioblastoma multiforme. Neurooncology 15(7):961–967. doi:10.1093/neuonc/not057
Pallud J, Audureau E, Blonski M, Sanai N, Bauchet L, Fontaine D, Mandonnet E, Dezamis E, Psimaras D, Guyotat J, Peruzzi P, Page P, Gal B, Parraga E, Baron MH, Vlaicu M, Guillevin R, Devaux B, Duffau H, Taillandier L, Capelle L, Huberfeld G (2014) Epileptic seizures in diffuse low-grade gliomas in adults. Brain J Neuro 137(Pt 2):449–462. doi:10.1093/brain/awt345
Chaichana KL, Parker SL, Olivi A, Quinones-Hinojosa A (2009) Long-term seizure outcomes in adult patients undergoing primary resection of malignant brain astrocytomas. Clinical article. J Neurosurg 111(2):282–292. doi:10.3171/2009.2.JNS081132
You G, Sha ZY, Yan W, Zhang W, Wang YZ, Li SW, Sang L, Wang Z, Li GL, Li SW, Song YJ, Kang CS, Jiang T (2012) Seizure characteristics and outcomes in 508 Chinese adult patients undergoing primary resection of low-grade gliomas: a clinicopathological study. Neurooncology 14(2):230–241. doi:10.1093/neuonc/nor205
Klein M, Engelberts NH, van der Ploeg HM, Kasteleijn-Nolst Trenite DG, Aaronson NK, Taphoorn MJ, Baaijen H, Vandertop WP, Muller M, Postma TJ, Heimans JJ (2003) Epilepsy in low-grade gliomas: the impact on cognitive function and quality of life. Ann Neurol 54(4):514–520. doi:10.1002/ana.10712
Buckingham SC, Campbell SL, Haas BR, Montana V, Robel S, Ogunrinu T, Sontheimer H (2011) Glutamate release by primary brain tumors induces epileptic activity. Nat Med 17(10):1269–1274. doi:10.1038/nm.2453
Campbell SL, Buckingham SC, Sontheimer H (2012) Human glioma cells induce hyperexcitability in cortical networks. Epilepsia 53(8):1360–1370. doi:10.1111/j.1528-1167.2012.03557.x
Yuen TI, Morokoff AP, Bjorksten A, D’Abaco G, Paradiso L, Finch S, Wong D, Reid CA, Powell KL, Drummond KJ, Rosenthal MA, Kaye AH, O’Brien TJ (2012) Glutamate is associated with a higher risk of seizures in patients with gliomas. Neurology 79(9):883–889. doi:10.1212/WNL.0b013e318266fa89
Robert SM, Buckingham SC, Campbell SL, Robel S, Holt KT, Ogunrinu-Babarinde T, Warren PP, White DM, Reid MA, Eschbacher JM, Berens ME, Lahti AC, Nabors LB, Sontheimer H (2015) SLC7A11 expression is associated with seizures and predicts poor survival in patients with malignant glioma. Sci Transl Med 7(289):289ra286. doi:10.1126/scitranslmed.aaa8103
Danbolt NC (2001) Glutamate uptake. Prog Neurobiol 65(1):1–105
Ye ZC, Rothstein JD, Sontheimer H (1999) Compromised glutamate transport in human glioma cells: reduction-mislocalization of sodium-dependent glutamate transporters and enhanced activity of cystine-glutamate exchange. J Neurosci 19(24):10767–10777
Savaskan NE, Heckel A, Hahnen E, Engelhorn T, Doerfler A, Ganslandt O, Nimsky C, Buchfelder M, Eyupoglu IY (2008) Small interfering RNA-mediated xCT silencing in gliomas inhibits neurodegeneration and alleviates brain edema. Nat Med 14(6):629–632. doi:10.1038/nm1772
Lyons SA, Chung WJ, Weaver AK, Ogunrinu T, Sontheimer H (2007) Autocrine glutamate signaling promotes glioma cell invasion. Cancer Res 67(19):9463–9471. doi:10.1158/0008-5472.CAN-07-2034
Ye ZC, Sontheimer H (1999) Glioma cells release excitotoxic concentrations of glutamate. Cancer Res 59(17):4383–4391
Takano T, Lin JH, Arcuino G, Gao Q, Yang J, Nedergaard M (2001) Glutamate release promotes growth of malignant gliomas. Nat Med 7(9):1010–1015. doi:10.1038/nm0901-1010
Ramaswamy P, Aditi Devi N, Hurmath Fathima K, Dalavaikodihalli Nanjaiah N (2014) Activation of NMDA receptor of glutamate influences MMP-2 activity and proliferation of glioma cells. Neurol Sci 35(6):823–829. doi:10.1007/s10072-013-1604-5
de Groot JF, Liu TJ, Fuller G, Yung WK (2005) The excitatory amino acid transporter-2 induces apoptosis and decreases glioma growth in vitro and in vivo. Cancer Res 65(5):1934–1940. doi:10.1158/0008-5472.CAN-04-3626
Merriel RB, Gibbs P, O’Brien TJ, Hibbert M (2011) BioGrid Australia facilitates collaborative medical and bioinformatics research across hospitals and medical research institutes by linking data from diverse disease and data types. Hum Mutat 32(5):517–525. doi:10.1002/humu.21437
Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, Engel J Jr, Forsgren L, French JA, Glynn M, Hesdorffer DC, Lee BI, Mathern GW, Moshe SL, Perucca E, Scheffer IE, Tomson T, Watanabe M, Wiebe S (2014) ILAE official report: a practical clinical definition of epilepsy. Epilepsia 55(4):475–482. doi:10.1111/epi.12550
Clarke G, O’Mahony S, Malone G, Dinan TG (2007) An isocratic high performance liquid chromatography method for the determination of GABA and glutamate in discrete regions of the rodent brain. J Neurosci Methods 160(2):223–230. doi:10.1016/j.jneumeth.2006.09.006
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups, The National Cancer Institute of Canada Clinical Trials Group (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352 (10):987–996. doi:10.1056/NEJMoa043330
Roslin M, Henriksson R, Bergstrom P, Ungerstedt U, Bergenheim AT (2003) Baseline levels of glucose metabolites, glutamate and glycerol in malignant glioma assessed by stereotactic microdialysis. J Neurooncol 61(2):151–160
Behrens PF, Langemann H, Strohschein R, Draeger J, Hennig J (2000) Extracellular glutamate and other metabolites in and around RG2 rat glioma: an intracerebral microdialysis study. J Neurooncol 47(1):11–22
Marcus HJ, Carpenter KL, Price SJ, Hutchinson PJ (2010) In vivo assessment of high-grade glioma biochemistry using microdialysis: a study of energy-related molecules, growth factors and cytokines. J Neurooncol 97(1):11–23. doi:10.1007/s11060-009-9990-5
Kohling R, Senner V, Paulus W, Speckmann EJ (2006) Epileptiform activity preferentially arises outside tumor invasion zone in glioma xenotransplants. Neurobiol Dis 22(1):64–75. doi:10.1016/j.nbd.2005.10.001
Stephens ML, Williamson A, Deel ME, Bensalem-Owen M, Davis VA, Slevin J, Pomerleau F, Huettl P, Gerhardt GA (2014) Tonic glutamate in CA1 of aging rats correlates with phasic glutamate dysregulation during seizure. Epilepsia 55(11):1817–1825. doi:10.1111/epi.12797
During MJ, Spencer DD (1993) Extracellular hippocampal glutamate and spontaneous seizure in the conscious human brain. Lancet 341(8861):1607–1610
Gao X, Wang H, Cai S, Saadatzadeh MR, Hanenberg H, Pollok KE, Cohen-Gadol AA, Chen J (2014) Phosphorylation of NMDA 2B at S1303 in human glioma peritumoral tissue: implications for glioma epileptogenesis. Neurosurg Focus 37(6):E17. doi:10.3171/2014.9.FOCUS14485
Liubinas SV, D’Abaco GM, Moffat BM, Gonzales M, Feleppa F, Nowell CJ, Gorelik A, Drummond KJ, O’Brien TJ, Kaye AH, Morokoff AP (2014) IDH1 mutation is associated with seizures and protoplasmic subtype in patients with low-grade gliomas. Epilepsia. doi:10.1111/epi.12662
Pallud J, Le Van Quyen M, Bielle F, Pellegrino C, Varlet P, Labussiere M, Cresto N, Dieme MJ, Baulac M, Duyckaerts C, Kourdougli N, Chazal G, Devaux B, Rivera C, Miles R, Capelle L, Huberfeld G (2014) Cortical GABAergic excitation contributes to epileptic activities around human glioma. Sci Transl Med 6(244):244ra89. doi:10.1126/scitranslmed.3008065
Campbell SL, Robel S, Cuddapah VA, Robert S, Buckingham SC, Kahle KT, Sontheimer H (2015) GABAergic disinhibition and impaired KCC2 cotransporter activity underlie tumor-associated epilepsy. Glia 63(1):23–36. doi:10.1002/glia.22730
van den Bent MJ, Afra D, de Witte O, Ben Hassel M, Schraub S, Hoang-Xuan K, Malmstrom PO, Collette L, Pierart M, Mirimanoff R, Karim AB, EORTC Radiotherapy and Brain Tumor Groups, The UKMRC (2005) Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: the EORTC 22845 randomised trial. Lancet 366 (9490):985–990. doi:10.1016/S0140-6736(05)67070-5
Koekkoek JA, Dirven L, Heimans JJ, Postma TJ, Vos MJ, Reijneveld JC, Taphoorn MJ (2014) Seizure reduction in a low-grade glioma: more than a beneficial side effect of temozolomide. J Neurol Neurosurg Psychiatry. doi:10.1136/jnnp-2014-308136
Koekkoek JA, Dirven L, Heimans JJ, Postma TJ, Vos MJ, Reijneveld JC, Taphoorn MJ (2016) Seizure reduction is a prognostic marker in low-grade glioma patients treated with temozolomide. J Neuro Oncol 126(2):347–354. doi:10.1007/s11060-015-1975-y
Robert SM, Ogunrinu-Babarinde T, Holt KT, Sontheimer H (2014) Role of glutamate transporters in redox homeostasis of the brain. Neuro Chem Int. doi:10.1016/j.neuint.2014.01.001
Robe PA, Martin DH, Nguyen-Khac MT, Artesi M, Deprez M, Albert A, Vanbelle S, Califice S, Bredel M, Bours V (2009) Early termination of ISRCTN45828668, a phase 1/2 prospective, randomized study of sulfasalazine for the treatment of progressing malignant gliomas in adults. BMC Cancer 9:372. doi:10.1186/1471-2407-9-372
Takeuchi S, Wada K, Nagatani K, Otani N, Osada H, Nawashiro H (2014) Sulfasalazine and temozolomide with radiation therapy for newly diagnosed glioblastoma. Neurol India 62(1):42–47. doi:10.4103/0028-3886.128280
Grossman SA, Ye X, Chamberlain M, Mikkelsen T, Batchelor T, Desideri S, Piantadosi S, Fisher J, Fine HA (2009) Talampanel with standard radiation and temozolomide in patients with newly diagnosed glioblastoma: a multicenter phase II trial. J Clin Oncol 27(25):4155–4161. doi:10.1200/JCO.2008.21.6895
Iwamoto FM, Kreisl TN, Kim L, Duic JP, Butman JA, Albert PS, Fine HA (2010) Phase 2 trial of talampanel, a glutamate receptor inhibitor, for adults with recurrent malignant gliomas. Cancer 116(7):1776–1782. doi:10.1002/cncr.24957
Liubinas SV, Drummond KJ, Desmond PM, Bjorksten A, Morokoff AP, Kaye AH, O’Brien TJ, Moffat BA (2014) Glutamate quantification in patients with supratentorial gliomas using chemical shift imaging. NMR Biomed 27(5):570–577. doi:10.1002/nbm.3095
Acknowledgments
Dr. Andrew Neal conducted statistical analysis with the assistance of Mark Tacey from Centre for Clinical Epidemiology, Biostatistics and Health Services Research, Royal Melbourne Hospital, University of Melbourne, VIC 3050.
Funding
Dr. Andrew Neal was supported by an Australian Postgraduate Award Scholarship (University of Melbourne), The UCB Pharma Clinical Scholarship and by the Royal Melbourne Hospital Neuroscience Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Neal, A., Yuen, T., Bjorksten, A.R. et al. Peritumoural glutamate correlates with post-operative seizures in supratentorial gliomas. J Neurooncol 129, 259–267 (2016). https://doi.org/10.1007/s11060-016-2169-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-016-2169-y