Abstract
Stereotactic biopsies are procedures performed to obtain tumor tissue for diagnostic examinations. Cerebral lesions of unknown entities can safely be accessed and tissue can be examined, resulting in correct diagnosis and according treatment. Stereotactic procedures of lesions in highly eloquent regions such as the brainstem have been performed for more than two decades in our department. In this retrospective study we focus on results, approaches, modalities of anesthesia, and complications. We performed a retrospective analysis of our prospective database, including 26 patients who underwent stereotactic biopsy of the brainstem between April 1994 and June 2015. All of the patients underwent preoperative MRI. Riechert–Mundinger-frame was used before 2000, thereafter the Leksell stereotactic frame was used. After 2000 entry and target points were calculated by using BrainLab stereotactic system. We evaluated histopathological results as well as further treatment; additionally we compared complications of local versus general anesthesia and complications of a frontal versus a trans-cerebellar approach. Median age of all patients was 33 years, and median number of tissue samples taken was 12. In all patients a final histopathological diagnosis could be established. 5 patients underwent the procedure under local anesthesia, 21 patients in general anesthesia. In 19 patients a frontal approach was performed, while in 7 patients a trans-cerebellar approach was used. Complications occurred in five patients. Thereby no significant difference was found with regard to approach (frontal versus trans-cerebellar) or anesthesia (local versus general). Stereotactic biopsies even of lesions in the brainstem are a save way to obtain tumor tissue for final diagnosis, resulting in adequate treatment. Approach can be trans-cerebellar or frontal and procedure can be performed either under local or general anesthesia without significant differences concerning complication rate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the past stereotactic biopsies were performed in many neurosurgical departments as a standard procedure to obtain tumor tissue. In doing so, different localizations of brain lesions are relatively easy to access using stereotactic guidance. Frame based stereotactic biopsy (STX) provides a save and efficient way to obtain tissue of cerebral lesions of unknown entities. To initiate further treatment, exact histopathological diagnosis is needed, since radiological diagnosis alone can sometimes be misleading. Eloquent localizations such as the brainstem have of course always played an important role. Since frame guided STX is a very well established procedure with high accuracy and low complication rates it is especially useful for deep seated, small lesions [13, 21].
In the pertaining literature stereotactic biopsies of brainstem lesions are described to be carried out under local or general anesthesia and different approaches for brainstem lesions are used. In general, biopsies can be performed frame based or neuro-navigation based. Mortality and morbidity rates of stereotactic procedures are known to be very low, but only few studies have hitherto focused on biopsy of such eloquent areas as the brainstem. Since quality of the pre- and intraoperative scans (CT, MRI, PET) have improved over the last years, stereotactic procedures have gained in safety resulting in an improved contrast between tumor tissue and brain [17, 19, 30]. Postoperative neurological deficits are therefore observed seldom.
The rationale for this study was to increase knowledge about benefit and complications of stereotactic biopsies of unknown brainstem lesions. We evaluate complication rates of stereotactic brainstem biopsies under local versus general anesthesia and we compare frontal versus trans-cerebellar approaches. Authors of former studies were of the opinion that adequate imaging could replace biopsy [2]. They concluded that in many cases further treatment is not altered after biopsy and therefore imaging can replace biopsy. This conclusion, however, only referred to infiltrative tumors of the pontine tegmentum that were almost always DIPGs. DIPGs with a typical appearance on MR are very unlikely to be non-astrocytic tumors.
It was our aim to show, that nowadays stereotactic procedures also in eloquent areas like the brainstem are of low risk and result in reliable diagnosis and imaging techniques are additional tools to be used for guiding biopsies.
Methods
We performed a retrospective analysis of our prospective database and included 26 patients who underwent STX between April 1994 and June 2015. All patients suffered from brainstem lesions of unknown entity and all patients underwent the procedure according to interdisciplinary tumorboard decision.
Lesions defined as brainstem lesions were involving the mesencephalon (with tectum or tegmentum), crus cerebri, pons or medulla oblongata.
All patients underwent thin sliced MRI prior to surgery.
After the stereotactic frame was mounted to the head with two pins frontal and two pins occipital, the patient underwent CT scan.
Before 2000, the Riechert–Mundinger-frame was used and the stereotactic trajectory was then calculated on basis of a phantom.
After 2000 CT and MRI imaging were fused, using the BrainLab iplan software (iPlanCranial 1.0 software; BrainLab system, Feldkirchen/Munich). Target and entry points were also calculated by BrainLab iplan software. Approaches were either frontal or trans-cerebellar, depending on the operating surgeon. Surgery was performed under local or general anesthesia.
The decision whether to use a frontal or a trans-cerebellar approach was based on the exact localization of the lesion. Lesions accessible by a frontal approach (e.g. tectum, tegmentum) were accessed via a frontal approach. Lesions of the caudal brainstem (e.g. medulla oblongata) were accessed trans-cerebellar.
In general patients who underwent biopsy in the earlier years underwent the procedure in local anesthesia. In doing so the surgeons wanted to observe closely the neurological status of the patient also intraoperatively.
During the last years the procedure was performed under general anesthesia due to the previously gained good results with low rates of complications.
Results
Eighteen patients were male and 8 were female, median age of all patients was 33 years.
Anesthesia
Five patients (19 %) underwent the procedure under local anesthesia, 21 patients (81 %) under general anesthesia.
Imaging
All patients underwent thin slice preoperative MRI and in all patients CT, with the stereotactic frame attached was performed on the day of the surgery. Imaging data of both were then fused to calculate entry and targetpoint (Leksell stereotactic system, BrainLab iplan software). In 17 patients a postoperative CT was performed and in nine cases not. At the beginning of stereotactic procedures being performed at our department, postoperative CT scans were assessed on a routine basis. During the last years postoperative CT scans were only performed if a new neurological deficit occurred.
We compared neuroradiological diagnosis with histological proven diagnosis. In 20 patients (76 %) the neuroradiological diagnosis was correct; in 6 patients (23 %) it was incorrect.
Among the incorrect diagnoses from neuroradiologists was a suspected ependymoma which was a PNET, a metastasis which was a B-cell lymphoma, a suspected high grade glioma was a lymphoma, a suspected lymphoma was a glioblastoma, a gliomatosis was a B-cell lymphoma histologically, and a suspected high grade glioma was a germinoma after histological examination.
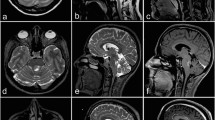
Figure 1 gives an overview of the different lesions which were performed.
Overview of variety of lesions which were biopsated. a–c Upper row T2w hyperintense lesion of the pontomedullary junction with slight contrast enhancement (asterisk). Histopathological diagnosis was medulloblastoma. d–f Middle row T2w hyperintense, non-enhancing lesion of the tectal plate (arrow) highly suggestive for tectal glioma, which was also the histopathological diagnosis after STX. g–i Lower row T2w inhomogenous mass with multiple enhancing foci of the thalamomesencephal junction (ellipse). STX revealed glioblastoma multiforme.
Approach
In 19 patients (73 %) a frontal approach was used and in 7 patients (27 %) the approach was trans-cerebellar.
Histopathological diagnosis
In all patients a final histopathological diagnosis was made. Median number of tissue samples taken was 12 (range 6–20). Samples were taken in 1 mm steps using a biopsy forceps. In all patients multiple biopsies were taken to ensure a definite histopathological diagnosis.
Astrocytoma WHO II was diagnosed in nine (34.6 %) patients, astrocytoma WHO III in two (7.7 %) and glioblastoma in five (19.2 %) patients. Medulloblastoma was diagnosed in three patients (11.5 %), diffuse intrinsic brainstem glioma in two patients (7.7 %) and three patients suffered from lymphoma (11.5 %). Primitive neuroectodermal tumor (PNET) and germinoma were diagnosed in one patient each (3.8 %). An overview of histopathological analyses is given in Table 1.
Treatment
A majority of 13 (50 %) patients underwent radiation postoperatively; seven patients received radiochemotherapy (26.8 %), while two patients underwent chemotherapy alone (7.7 %). In two patients control imaging after 3 months was recommended (7.7 %). One patient was lost for follow up (3.9 %). One patient died due to multiple organ dysfunction before receiving further therapy (3.9).
Table 2 provides all demographic, clinical, and imaging details of all patients.
Complications
In 17 patients a postoperative CT scan was performed. Surgery related complications occurred in five patients (19.2 %) (one with facial palsy, one with hydrocephalus, three with small local bleedings in the biopsied area).
Among these patients we consider hydrocephalus as a severe complication (3.9 %), since only this patient required further surgical treatment (see below).
All other complications, listed below, were mild and symptoms decreased during the postoperative stay at our department. The small bleedings were asymptomatic (two patients had received local anesthesia, one general anesthesia, all three had frontal approaches).
The patient (8 years) who developed a facial palsy postoperatively underwent surgery under general anesthesia and the surgeon chose a trans-cerebellar approach for a pons lesion. A CT scan was performed postoperatively to exclude hemorrhage. The CT showed only mild postoperative swelling. Cortisone (20 mg) was administered and the grade of the palsy decreased during the following days.
In three patients a small hemorrhage was found in the biopsied area after CT scan was performed on a routine basis. All of the hemorrhages were clinically silent and since these patients did not show any neurological deficits no further treatment was needed.
One patient showed a postoperative prolonged awakening phase (after general anesthesia and frontal approach), therefore a CT scan was performed. The scan showed a hydrocephalus due to swelling in the biopsied area (mesencephalon). The patient received an external ventricular drain. Unfortunately this patient was already in a bad condition prior to surgery (cirrhosis of the liver with low thrombocytes and reduced KPS of 50). He developed pneumonia during the further course on our intensive care unit. With beginning liver and lung failure his family decided not to force any more medical therapy after they received the histopathological diagnosis of his tumor, which was glioblastoma WHO IV. The patient died a few days after surgery due to multi-organ-dysfunction. In our series mortality is therefore 3.8 %.
Statistical analysis
Using Chi-squared test, we compared the two different approaches (frontal versus trans-cerebellar) and the modality of anesthesia used (general versus local). We correlated approach and anesthesia to the complications mentioned above. P values of 0.05 and below were considered statistically significant.
P was 1.0 for approach trans-cerebellar versus frontal and 0.6 for local anesthesia versus general anesthesia (fisher’s exact test).
Illustrative case for frontal approach
A 52 year old patient presented with a left sided weakness and gait instability at the neurological department. CT and MRI scans were performed, imaging revealed a contrast enhancing tumor mass of the mesencephalon. We discussed the case in our interdisciplinary tumor board where a STX was finally suggested. Surgery was performed by a frontal approach (due to the mesencephalic tumor, Fig. 2a–c) and general anesthesia. The histopathological examination revealed a glioblastoma.
Illustrative case for transcerebellar approach
This 3 year old patient presented with an incipient hemiparesis and ataxia. He also showed abnormal hypersalivation. The MRI scan showed a pons tumor of unknown dignity. The tumor showed no contrast enhancement. The pediatric tumorboard recommended STX, which was then performed. A transcerebellar approach was used, due to the pontine localization of the tumor (Fig. 3a–c). The child underwent the procedure under general anesthesia. Histopathological examination established the diagnosis of diffuse intrinsic brainstem glioma.
Discussion
Stereotactic biopsy of brain lesions of unknown entity is a standard procedure in numerous neurosurgical departments nowadays. Also eloquent areas such as the brainstem have been accessed since the 1980s [6–8], but decision-making whether to biopsy a lesion in this eloquent area is not easy. Today most cases are discussed in an interdisciplinary tumorboard, evaluating the indication and consequence of STX.
Although most brainstem tumors are found in children, the diversity of pathologies is higher in adults [11, 29]. In contrast to biopsies in other areas of the brain, the brainstem is mostly accessed stereotactically, due to the high precision reached by the stereotactic systems [13]. Mostly frame based systems such as the Leksell system, the Cosman–Robert–Wells or the Brown–Robert–Wells system are used [18, 25]. Nevertheless also frameless, navigation based systems are reported to be a safe alternative [14]. Frame-based procedures can be performed under local or general anesthesia, while procedures with frame-less systems usually have to be carried out under general anesthesia [27]. Local anesthesia can be of advantage for patients with cardio-pulmonary diseases since they do not need sedation and mechanic ventilation during local anesthesia. In children stereotactic biopsies are usually performed under general anesthesia.
In general STX is a safe procedure with low mortality and morbidity rates, nevertheless some authors reported higher complication rates for lesions in the brainstem [4, 5]. In contrast the reviews of Samadani et al. and Kickingereder et al. stated no higher complication rates for STX of lesions in the brainstem [10, 23]. In his review from 2012 Kickingereder et al. showed diagnostic success of the procedure between 94.5 and 97.6 %, morbidity was between 5.6 and 10.2 %, mortality was 0.5−1.4 % [10]. Our results meet the results of his work, finding diagnostic success in 100 % of the patients who underwent biopsy. In our study morbidity was 19.2 % (including hemorrhages without clinical symptoms in 11.5 % and neurological deficits in 7.7 %) mortality was 3.9 %. Morbidity and mortality rates of the patients in our study are somewhat higher than presented by Kickingereder et al. [10]. However, the patient who deceased in the further course died due to multi organ dysfunction not related directly to surgery.
From the late 1980s on different approaches (frontal versus trans cerebellar) are reported [6, 7]. It is still unclear and depends on the exact localization and configuration of the lesion which approach is chosen by the surgeon.
Also in our study, brainstem lesions have been accessed in both ways. In our series, a frontal approach was used for all patients who underwent surgery before 2010. After 2010 a trans-cerebellar approach was used for patients with lesions in the pons and in the medulla oblongata (Fig. 2a–c). If the lesion had to be accessed from lateral trans-cerebellar, the Leksell frame was fixed to the head oblique in order to keep the pins beyond the planned trajectory [20]. A frontal approach was used for patients who had lesions of the tegmentum and tectum. Frontal approaches were planned by using a pre-coronary burrhole with a trajectory not penetrating the ventricle (examples of trajectory planning see illustrative case Fig. 1a–c). Our observation concerning the two different approaches meet the statement of Goncalves-Ferreira et al., who also suggest that lesions involving the medulla oblongata should be accessed trans-cerebellar, lesions in the mesencephalon should be accessed through a frontal approach [8].
A literature research by Samadani et al. evaluated 469 stereotactic biopsies of brainstem tumors in adults [23]. They analyzed whether a patient should undergo biopsy or empiric therapy by relying on the certainty of the diagnosis reported by the radiologist, neurosurgeon and consulting physician. In our opinion this underlines the dilemma of treating brain stem lesions. Even if the radiologist is 100 % certain about the diagnosis, there is still a number of patients who might receive inadequate therapy if he is mistaken. Furthermore we want to point out that for future therapies molecular markers such as O6-Methylguanin-DNS-Methyltransferase (MGMT) and Isocitratedehydrogenase-1 (IDH-1) and alpha-thalassemia/mental retardation syndrome X-linked (ATRX) might play an important role. These markers can only be estimated by obtaining tissue samples, for example through biopsy [28].
The study of Massager et al. evaluated MRI and PET Data in 30 patients, finding correct diagnosis, after comparison with histopathological data from STX in only 63 % of the patients [15]. Accordingly we compared neuroradiological diagnosis with histologically proven diagnosis. We found the radiological diagnosis to be correct in only 73 % of the patients (n = 20) supporting strongly our perception that biopsy of brainstem lesions is indispensible before commencement of potentially hazardous therapies. It is important to point out that three of the six (50 %) incorrect diagnosed patients were biopsied before 2000.
However, even though modern imaging has improved over the last years enormously, still it has not matched the accuracy of histological analysis yet. This might be true especially in case of brain stem masses due to artifacts, limiting imaging of the skull base and below [3, 24, 26].
Blasel et al. found that peritumoral elevated relative cerebral blood volume (rCBV) has a high diagnostic accuracy in differentiating GBM from metastases. Peritumoral rCBV was significantly lower in patients with metastases than in glioblastoma patients [3]. Lescher et al. recently concentrated in grading pediatric brain tumors according to their signal intensity in T2. They found that there is a cut of value which can be calculated by T2 measurement to discriminate low grade tumor from high-grade tumors [12].
Abdelaziz et al. recently compared the value of MR-spectroscopy (MRS) with the results of STX. The authors found MRS to be a reliable tool in grading gliomas, but they agree that also MRS is a tool used to guide stereotactic surgery rather than to replace it [1]. Hattingen et al. give a good overview of quantitative MRI measurements, which are also used to monitor tumor tissue reactions to therapy [9].
Here discussed techniques as proposed by Lescher et al. and Abdelaziz might help to guide stereotactic biopsies in the future [1, 12]. But imaging alone stays indicative and there still is not evidence enough to base further therapies on.
We strongly agree with Vedantam Rajshekhar, who states that therapy of brain stem lesions should not be based on imaging alone, since therapies can cause side-effects and can therefore be potentially harmful. Since the histological grading can only be performed using tumor tissue, the authors clearly state that biopsy is needed in contrast to children with suspected diffuse pontine glioma. Here the histological grading does not predict the outcome as it does in adults. We also agree with the author who suggests that the shortest route for biopsy should be taken (for pontine and medullary lesions-transcerebellar and for midbrain biopsies transfrontal) [22].
Our data underline, that there is no significant difference concerning complication rates in procedures performed in general or local anesthesia and approaches frontal versus cerebellar (general versus local anesthesia p = 0.6, frontal versus trans cerebellar approach p = 1.0). Both modalities of anesthesia and different approaches of brainstem lesions do not inherit a higher complication risk and can therefore safely be performed.
Conclusion
Stereotactic biopsy is a save procedure to obtain tumor tissue for further treatment even in eloquent areas such as the brainstem. Approaches can be frontal or trans cerebellar and surgeries can be performed under local or general anesthesia without significant difference concerning complication rates.
References
Abdelaziz O, Eshra M, Belal A, Elshafei M (2016) Diagnostic value of magnetic resonance spectroscopy compared with stereotactic biopsy of intra-axial brain lesions. J Neurol Surg A Cent Eur Neurosurg 77(4):283–290 (Epub ahead of print)
Albright AL, Packer RJ, Zimmerman R et al (1993) Magnetic resonance scans should replace biopsies for the diagnosis of diffuse brain stem gliomas: a report from the Children’s Cancer Group. Neurosurgery 33:1026–1029
Blasel S, Jurcoane A, Franz K, Morawe G, Pellikan S, Hattingen E (2010) Elevated peritumoural rCBV values as a mean to differentiate metastases from high-grade gliomas. Acta Neurochir (Wien) 152(11):1893–1899
Cartmill M, Punt J (1999) Diffuse brain stem glioma. A review of stereotactic biopsies. Childs Nerv Syst 15:235–237 (discussion 238)
Dellaretti M, Reyns N, Touzet G, Dubois F, Gusmao S, Pereira JL, Blond S (2012) Stereotactic biopsy for brainstem tumors: comparison of transcerebellar with transfrontal approach. Stereotact Funct Neurosurg 90:79–83
Frank F, Fabrizi AP, Frank-Ricci R, Gaist G, Sedan R, Peragut JC (1988) Stereotactic biopsy and treatment of brain stem lesions: combined study of 33 cases (Bologna-Marseille). Acta Neurochir Suppl (Wien) 42:177–181
Giunta F, Grasso G, Marini G, Zorzi F (1989) Brain stem expanding lesions: stereotactic diagnosis and therapeutical approach. Acta Neurochir Suppl (Wien) 46:86–89
Goncalves-Ferreira AJ, Herculano-Carvalho M, Pimentel J (2003) Stereotactic biopsies of focal brainstem lesions. Surg Neurol 60:311–320 (discussion 320)
Hattingen E, Jurcoane A, Nelles M, Müller A, Nöth U, Mädler B, Mürtz P, Deichmann R, Schild HH (2015) Quantitative MR imaging of brain tissue and brain pathologies. Clin Neuroradiol 25 (Suppl 2):219–24
Kickingereder P, Willeit P, Simon T, Ruge MI (2013) Diagnostic value and safety of stereotactic biopsy for brainstem tumors: a systematic review and meta-analysis of 1480 cases. Neurosurgery 72:873–881 (discussion 882; quiz 882)
Landolfi JC, Thaler HT, DeAngelis LM (1998) Adult brainstem gliomas. Neurology 51(4):1136–1139
Lescher S, Whora K, Schwabe D, Kieslich M, Porto L (2016) Analysis of T2 signal intensity helps in the differentiation between high and low-grade brain tumours in paediatric patients. Eur J Paediatr Neurol 20(1):108–113
Lunsford LD, Niranjan A, Khan AA, Kondziolka D (2008) Establishing a benchmark for complications using frame-based stereotactic surgery. Stereotact Funct Neurosurg 86:278–287
Lu Y, Yeung C, Radmanesh A, Wiemann R, Black PM, Golby AJ (2015) Comparative effectiveness of frame-based, frameless, and intraoperative magnetic resonance imaging-guided brain biopsy techniques. World Neurosurg 83(3):261–268. doi:10.1016/j.wneu.2014.07.043 (Epub 2014 Aug 1)
Massager N (2002) Usefulness of PET scan guidance in stereotaxic radioneurosurgery using a gamma knife. Bull Mem Acad R Med Belg 157:355–362 (discussion 363–359)
Mathisen JR, Giunta F, Marini G, Backlund EO (1987) Transcerebellar biopsy in the posterior fossa: 12 years experience. Surg Neurol 28:100–104
Nöth U, Hattingen E, Bähr O, Tichy J, Deichmann R (2015) Improved visibility of brain tumors in synthetic MP-RAGE anatomies with pure T1 weighting. NMR Biomed 28(7):818–830
Pell MF, Thomas DG, Krateminos GP (1993) Stereotactic management of intrinsic brain stem lesions. Ann Acad Med Singapore 22:447–451
Preuss M, Werner P, Barthel H, Nestler U, Christiansen H, Hirsch FW, Fritzsch D, Hoffmann KT, Bernhard MK, Sabri O (2014) Integrated PET/MRI for planning navigated biopsies in pediatric brain tumors. Childs Nerv Syst 30(8):1399–403. doi:10.1007/s00381-014-2412-9 (Epub 2014 Apr 8)
Quick-Weller J, Duetzmann S, Behmanesh B, Seifert V, Weise LM, Marquardt G. (2015) Oblique positioning of the stereotactic frame for biopsies of cerebellar and brainstem lesions. World Neurosurg 86:466-469
Raabe A, Krishnan R, Zimmermann M, Seifert V (2003) Frame-less and frame-based stereotaxy? How to choose the appropriate procedure. Zentralbl Neurochir 64(1):1–5
Rajshekhar V, Moorthy RK (2010) Status of stereotactic biopsy in children with brain stem masses: insights from a series of 106 patients. Stereotact Funct Neurosurg 88(6):360–366
Samadani U, Stein S, Moonis G, Sonnad SS, Bonura P, Judy KD (2006) Stereotactic biopsy of brain stem masses: Decision analysis and literature review. Surg Neurol 66:484–490 (discussion 491)
Schmalfuss IM, Camp M (2008) Skull base: pseudolesion or true lesion? Eur Radiol 18(6):1232–1243
Spiegelmann R, Friedman WA (1991) Rapid determination of thalamic CT-stereotactic coordinates: a method. Acta Neurochir (Wien) 110:77–81
Tanaka N, Abe T, Kojima K, Nishimura H, Hayabuchi N (2000) Applicability and advantages of flow artifact-insensitive fluid-attenuated inversion-recovery MR sequences for imaging the posterior fossa. Am J Neuroradiol 21(6):1095–1098
Weise LM, Bruder M, Eibach S, Seifert V, Byhahn C, Marquardt G, Setzer M (2013) Efficacy and safety of local versus general anesthesia in stereotactic biopsies: a matched-pairs cohort study. J Neurosurg Anesthesiol 25:148–153
Weise LM, Harter PN, Eibach S, Braczynski AK, Dunst M, Rieger J, Bahr O, Hattingen E, Steinbach JP, Plate KH, Seifert V, Mittelbronn M (2014) Confounding factors in diagnostics of MGMT promoter methylation status in glioblastomas in stereotactic biopsies. Stereotact Funct Neurosurg 92:129–139
White HH (1963) Brain stem tumors occurring in adults. Neurology 13:292–300
Wagner M, Nafe R, Jurcoane A, Pilatus U, Franz K, Rieger J, Steinbach JP, Hattingen E (2011) Heterogeneity in malignant gliomas: a magnetic resonance analysis of spatial distribution of metabolite changes and regional blood volume. J Neurooncol 103(3):663–672
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare not to have any conflict of interest concerning this study. This retrospective study was approved by the local ethics committee.
Rights and permissions
About this article
Cite this article
Quick-Weller, J., Lescher, S., Bruder, M. et al. Stereotactic biopsy of brainstem lesions: 21 years experiences of a single center. J Neurooncol 129, 243–250 (2016). https://doi.org/10.1007/s11060-016-2166-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-016-2166-1