Abstract
In this retrospective evaluation, we correlated radiation dose parameters with occurrence of optical radiation-induced toxicities. 213 meningioma patients received radiation between 2000 and 2013. Radiation dose and clinical data were extracted from planning systems and patients’ files. The range of follow-up period was 2–159 months (median 75 months). Median age of patients was 60 years (range 23–86). There were 163 female and 50 male patients. In 140 cases, at least one of the neuro-optic structures (optic nerves and chiasm) was inside the irradiated target volumes. We found 15 dry eye (7 %) and 24 cataract (11.2 %) cases. Median dose to affected lachrymal glands was 1.47 Gy and median dose to affected lenses was 1.05 Gy. Age and blood cholesterol level in patients with cataract were significantly higher. Patients with dry eye were significantly older. Only two patients with visual problems attributable to radiation treatment were seen. They did not have any risk factors. Maximum and median delivered doses to neuro-optic structures were not higher than 57.30 and 54.60 Gy respectively. Low percentages of cases with radiation induced high grade optic toxicities show that modern treatment techniques and doses are safe. In very few patients with optic side effects, doses to organs at risk were higher than the defined constraint doses. This observation leads to the problem of additional risk factors coming into play. The role of risk factors and safety of higher radiation doses in high grade meningiomas should be investigated in more comprehensive studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Loss of vision is a deleterious, albeit rare side effect in patients treated with radiotherapy for brain and skull base tumors. Causes can be radiation-induced optic neuropathy (RION), cataract, dry eye or retinopathy [1, 2].
In patients with brain tumors and head and neck malignancies, RION is a late complication of radiotherapy to the anterior visual pathway resulting in acute, painless and irreversible visual loss. RION presents with monocular visual loss, although second eye involvement may rapidly follow or within months [3]. RION occurs commonly between 10 and 20 months, with an average of 18 months after treatment, but the onset may range from three months to 9 years [3]. Dose is the most important cause for RION. Cumulative doses of radiation that exceed 50 Gy or single doses to the anterior visual pathway or greater than 10 Gy are usually required for RION to develop. The risk of toxicity increases markedly at doses >60 Gy at 1.8 Gy/fraction and at >12 Gy for single-fraction radiosurgery [3, 4]. A relation between the dose of radiation and the latency to the onset of symptoms has been suggested too [3, 4]. Several factors are associated with a higher risk for developing RION or for the occurrence of RION with lower total doses of radiation. An increased risk of RION has been reported with increasing age, pre-existing compression of the optic nerve and chiasm by tumor and previous external beam radiation [5, 6]. Data on other clinical factors such as chemotherapy, diabetes mellitus, hypertension and smoking have been inconsistent [4]. Treatment of RION with systemic corticosteroids, anticoagulation and hyperbaric oxygen has been generally unsuccessful and disappointing [6, 7].
The diagnosis of RION is suggested in ophthalmologic exam, by an impaired visual function with loss of visual acuity and visual field defect in the absence of other causes. If the visual loss is unilateral or asymmetric, a relative afferent pupillary defect (RAPD or Marcus Gunn pupil) will be present. The visual field may show any pattern of optic nerve or chiasmal defects. Another sign of RION may be decreased color vision or dyschromatopsia. In ophthalmoscopy, optic nerve will appear normal or swollen. The CT scan is typically normal, as are the unenhanced T1- and T2-weighted MRI images. However, MRI with contrast demonstrates marked enhancement of the optic nerve and chiasm on T1-weighted images. The key clinical differential diagnosis of RION is tumor recurrence. In contrast to RION, tumor recurrence generally shows a slower course of visual loss [4, 8].
In this retrospective evaluation, a detailed survey has been performed in patients treated with radiotherapy for meningioma. We correlated radiation dose parameters with the occurrence of optical radiation-induced toxicities including RION, cataract and dry eye. Compared to data in the literature, the present manuscript adds valuable information. This analysed series is one of the largest and homogeneous treatment group of patients with data on optic toxicity; therefore it is an important information for the radiation oncology community.
Materials and methods
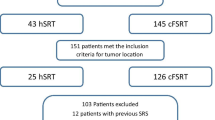
We selected all the meningioma patients who received radiation treatment in our centre from 2000 until 2013. Out of 247 patients, those with previous radiation therapy for head malignancies and those with incomplete planning data or missing clinical data were excluded. Finally 213 patients entered the study.
Treatment planning was done with the following planning systems: eclipse 10 planning system (Varian Medical Systems, Palo Alto, CA, USA), TomoTherapy’s planning station (Accuray Inc., Madison, WI, USA), Brainscan and iPlan (BrainLab AG, Feldkirchen, Germany). Radiotherapy techniques included Intensity Modulated Radiation Therapy (IMRT), Tomotherapy or three dimensional (3D) treatment and radio-surgery. The majority of patients (n = 205), received “Fractionated Stereotactic Radiation Treatment” (FSRT) or “Stereotactic Radio-Surgery” (SRS) (Suppl. 1). Suppl. 2 shows an example of a planning CT scan with contoured target volumes and organs at risk (OARs).
Dose parameters including maximum, mean and median doses to the target volumes and OARs (optic nerves, chiasm, lenses, eyeballs and lachrymal glands) were extracted from the planning systems. In most patients treated between 2000 and 2006 (n = 120), only one target volume was delineated planning target volume (PTV). In these patients gross tumor volume (GTV) was not contoured. Due to technical limitations, the mean total dose (Dmean) was not extractable in patients treated based on Brainscan system (n = 157). So in this study, we used the median total dose (Dmedian) which was extractable for all the patients, instead of Dmean. Considering the different radiation treatment techniques, total prescribed doses and doses per fraction, we also calculated EQD2 (equivalent total doses in 2-Gy fractions) in order to report the doses in a consistent way. Calculations were based on an α/β of 2 for meningioma and on an α/β of 3 for OARs (for long term side effects) [9, 10]. We also evaluated dose distributions in neuro-optic structures that are shown by the volume percentages of optic nerves and chiasm which received 45, 50, 54 and 60 Gy, as these doses represent relevant tolerance doses for neuro-optic structures reported in the literature [11].
Out of 213 patients, 187 patients were treated with one treatment plan, 26 patients were treated with at least two plans (23 patients had two and three patients had three plans). Analysis of total radiation doses delivered to target volumes and OARs in these 26 patients was not as straightforward as for the other patients. Some of these patients were treated with Brainscan planning system, in which summation of different plans is not possible. Even if the summation was possible—as in the patients treated with iPlan and eclipse—this summation would not be absolutely reliable, as new planning CT-scans were done for the new phases of treatment. As a rigid registration was used to align all CT-scans, the summation plan made by the system does not necessarily show exactly the summation of the delivered dose to the same anatomical voxel and areas. Nevertheless, we accepted this inexactness; for all the patients with more than one treatment plan, a summation of relevant doses (Dmax1 + Dmax2,…) was made, allowing a rough evaluation of doses delivered to the target volumes and OARs in all the patients.
Clinical data, concomitant as well as former diseases, and the clinical path of all patients were extracted from the patients’ files. For patients who had missed their routine follow up protocol, we called the patients (or their family doctors when necessary) and asked them to come for a new visit or to send us their latest documents regarding their follow ups in other centers or cities. Patients lost from follow up were censored according to the date of their last visit. Of note, hypercholesterolemia and hypertension was supposed as risk factors, if patients reported about a history of hypertension or hypercholesterolemia and were under specific medication. Neither blood pressure nor cholesterol-Levels were collected routinely. The range of follow-up period was 2–159 months (median 75 months). Evaluation of the side effects was done according to CTCAE-4.03. We took only those side effects into consideration that began after radiation treatment. Ophthalmologic exams were initiated at baseline, if visual signs or symptoms were present on clinical evaluation or in patient’s history. After end of radiotherapy, all the patients were asked about the visual problems in their periodic follow-up visits. Patients with new visual signs or symptoms or patients with changes in previous visual signs or symptoms were referred for a new ophthalmologic exam.
We used Microsoft Excel 2013 for collecting the data. Statistical analysis was done with IBM SPSS v. 18. Actuarial analysis has been used for reporting about median time to progression. If the data fulfilled criteria for a normal distribution, significance levels were calculated using two sided student T test.
Results
General characteristics of the patients and detailed information about the primary tumor side are shown in Tables 1 and 2, respectively. The age range of the patients was 23–86 years old (median 60 and mean 59). In 72 cases no surgical intervention was performed before radiation treatment. These patients had only a radiographic diagnosis of meningioma.
The most prevalent signs and symptoms were visual acuity defect (25.8 %), headache (22 %), visual field defect (16.9 %), dizziness (13.1 %), diplopia (12.2 %), sensory disorder due to trigeminal nerve dysfunction (10.8 %), exophthalmus (8.4 %) and ptosis (7 %). In total, 100 patients (46.9 %) had signs or symptoms related to eyes and visual system (most of them had more than one sign or symptom) (Suppl. 3). These patients had also a baseline ophthalmologic exam result in their files.
In 38 cases at least one of the neuro-optic structures including optic nerves and chiasm, were involved by the tumor directly, which meant an infiltration that was seen and reported by radiologist in the MRI (Suppl. 4). Yet not all MRI reports stated about the status of the neuro-optic structures.
An important point is, that the neuro-optic structures might have been inside the target volumes of radiation treatment not only because of being involved by the tumor, but also because of their vicinity to the tumor. Out of 213 patients, only in 73 cases, none of the neuro-optic structures was inside the target volumes. In the other 140 patients, at least one of the neuro-optic structures was totally or partially inside one of the planning target volume of the radiation treatment (Table 2).
Median total prescribed dose in all patients were 54 Gy (15–60 Gy). Doses per fraction ranged from 1.75 to 17 Gy and the number of fractions ranged between 1 and 31. The details about delivered doses to PTV and OARs in Suppl. 5. Dose distributions in neuro-optic structures (V45, V50, V54 and V60) are shown in Suppl. 6. These parameters could be calculated only for those patients treated with one plan (n = 187). Dmax values were >54 Gy in 147 OARs, Dmed values exceeded 54 Gy in 7 OARs (Table 3). In order to reduce uncertainties growing from largely different dose/fraction, patients with less than 5 fractions were excluded from further analysis. We subsequently analyzed the remaining 190 patients, whether specific tumor locations were related to higher Dmax values (Table 4). Briefly, meningiomas located within the cavernous sinus, at the skull base, the sphenoid wing, the optic nerve sheath, the sella and at the middle cranial fossa were significantly associated with higher Dmax values, at least in one of the neuro-optic OARs. As an internal control, involvement of neuro-optic OARs into the PTV was also significantly associated with higher Dmax values.
We subsequently investigated, whether treatment techniques had an influence on Dmed- and Dmax-value within neuro-optic OARs. Also for this analysis, RS-cases were excluded. Intriguingly, 3D-planning was associated with significantly lower Dmed within the left optic nerve (p = 0.038), while Dmax did not significantly differ. Dmax values of more than 54 Gy (EQD2) were more likely when 3D planning was used (Fig. 1).
Out of 213 patients, recurrence after radiation treatment occurred in 24 cases (11.2 %). The median interval between treatment and recurrence was 34.5 (3–78 months) (Suppl. 7 and 8). Five cases presented with new tumors after the first radiation therapy (second primary tumors). Details about these patients are shown in Suppl. 9.
There were two patients with visual problems after radiation therapy that could be attributed to RION. Both of them were referred for fractionated stereotactic radiotherapy for a radiologically diagnosed meningioma. The planning for both patients was done using the Brainscan system, so Dmean was not extractable. In both patients 3D-conformal treatment planning was used. In both patients only one target volume was defined (PTV). During the follow up period, the primary tumors were stable, without any progression in both patients. Table 5 shows the characteristics of the tumor and the treatment in these two patients. During follow-up of the first patient, there was a progressive problem with right side visual acuity that began 2 months after end of radiotherapy. The left sided vision was unimpaired. In an MRI, done 43 months after end of radiation, right para-optical nerve sheath edema was reported. Since no further ophthalmological exams and MRIs were available, we could not judge the severity of his acuity problem on right side. Therefore, this case should be supposed as a suspicious case of RION on right side. In the second case, the defect in right side visual field improved after treatment. However, 11 months after end of radiotherapy, defects in visual acuity and visual field in both eyes, especially right eye, occurred. In addition, edema in both optic nerves was reported in an MRI done 1 year after end of radiation treatment. In the right eye, visual acuity and visual field problem, dyschromatopsia, RAPD and optic nerve atrophy were reported in ophthalmologic exams. On the left side, atrophy of optic nerve was detected. Neither treatment with corticosteroids nor with hyperbaric oxygen therapy was effective, as the right eye remained nearly amaurotic, the acuity of left eye was 0.4 two years after treatment (grade 4 and 3 respectively). Suppl. 10 and 11 show the contoured volumes and the dose distribution in these two cases.
Fifteen cases of newly diagnosed dry eye after radiotherapy were observed (7 %). 12 cases had grade 1 dry eye. Eight of them were treated by artificial tears and the other 4 did not need any treatment. Three patients had grade 2 dry eye. All of them received artificial tears and lubricants for treatment. The median of interval between treatment and beginning of dry eye was 17 months (1–139 months). Dry eye occurred mostly ipsilateral, except one case that developed bilateral dry eyes. Of note, detection of dry eye was based on subjective data collected via interviews by patients and only rarely based on ophthalmologic exams. Details of radiation dose to lachrymal glands are shown in Table 6 and Suppl. 12. None of these patients had a history of dry eye before radiation treatment. One of them had tumor recurrence during follow up period, but the salvage treatment was surgery, not radiation treatment. Regarding tumor location, most of these patients had tumors in direct vicinity to the optic pathway (11 patients), most of them were treated with 3D-conformal technique (10 patients).
Twenty four patients developed cataract after radiotherapy (11.2 %). 11 of these cases needed surgical removing of the lens (grade 3). The other patients were in grade 1 and 2. The median of interval between treatment and cataract was 47.5 months (6–141 months). Cataract occurred ipsilateral, except six cases with bilateral cataract. Details of radiation dose to lenses are available in Table 6 and Suppl. 13. None of these patients had cataract before radiation treatment. Three cases had local recurrence and 1 case had second primary lesions. In all of these cases no salvage treatment was done except in one patient who received salvage surgery, not radiation treatment. Regarding tumor location, most of these patients had tumors in vicinity of optic pathway (18 patients), most of them were treated with 3D-conformal technique (18 patients).
Discussion
In the present manuscript, we show that optic toxicity after stereotactic radiotherapy of meningiomas is a very rare side effect, and that the development of any optic toxicity depends tightly on dose-volume effects. This analysis focused on factors influencing the development of visual impairment by RION, cataract and dry eye after fractionated stereotactic radiotherapy.
The probably most severe optic toxicity is RION—which can results in complete blindness of patients. The two most important treatment-related risk factors for optic nerve/chiasm injury are the total dose and the fraction size. Toxicity increases significantly at doses >54–60 Gy (1.8–2 Gy/fraction) and at >12 Gy for single-fraction radio-surgery [3, 12]. For those patients with deficit in visual acuity and visual field, it was observed that the median and max dose in the optic nerves and chiasm was higher than in the group without the complications [13]. For whole organ tolerance, Emami et al. [11] listed the doses corresponding to 5 % probability of blindness within 5 years after treatment and the 50 % probability within 5 years as 50 and 65 Gy, respectively. In our cohort, Dmed Dmax values for OAR involved into the PTV were >50 Gy but only two sever complications were reported (2 cases in 125 cases, 1.6 %, RS-cases excluded). Similar RION-rates were reported also from other groups [14, 15]. A probabilistic component clearly exists, because some patients receiving greater doses did not develop complications [4, 9]. Also in our cases, maximum doses to neuro-optical structures were >50 and >54 Gy in case 1 and 2, respectively (Table 5). 3D-planning was used in both cases, no case of RION occurred within the patients treated with IMRT plans. No statistical significant dosimetric advantage of IMRT over 3D-planning neither in our cohort nor in the cohort of others [15, 16] was reported. However, also in our experience, IMRT allows a more sufficient limitation of Dmax values in OARs (Fig. 1), even when on expense of higher Dmed values [16].
Especially in older ages dry eye is not uncommon in the general population [17]. However, in our study, symptoms linked with dry eye were not present before radiotherapy. It is known that “dry eye” is related to the high dose of radiation delivered to the lachrymal glands. Although the tolerance dose of lachrymal glands is about 34–40 Gy [18–20], it is quite probable that lower doses of radiation also lead to dry eye, but with mild symptoms and longer intervals after radiotherapy [8, 18]. In most cases, delivered dose to the lachrymal glands were lower than the mentioned constraint dose, while the interval between treatment and dry eye in some of them was only 1 month (suppl. 12). The median delivered dose to affected lachrymal glands in these 15 patients was not much different with the delivered dose to lachrymal glands in all the patients (Tables 6 and suppl. 12). So we could not define a dose–effect relationship. However, these results may be explained to a certain extent by other predisposing factors. Table 7 shows that there is a trend that older age, hypercholesterolemia and arterial hypertension may play a role in developing of dry eye. This role is significant regarding patients’ age, regarding the other two items no significant difference was found.
Numerous reports are available on the development of cataract related to radiotherapy: in adults, after 2.5–6.5 Gy the latent period of cataract is 8 years with a 33 % risk of progressive cataract, while after 6.5–11.5 Gy, the latent period is 4 years, with a 66 % risk [21], but again it is expected that lower doses of radiation may lead to cataract with less severity and longer intervals after end of radiation treatment [22]. Another point is patients’ age and senile cataract; it is not always easy to differentiate radiation induced cataract and senile cataract [23]. In our study the median dose to most affected lenses in patients with cataract was less than the mentioned constraint dose (suppl. 13). Also the median dose to the affected lenses was equal or just minimally higher than the median dose to lenses in all the patients (Table 6 and suppl. 13). Nevertheless, when the cataract occurs after the radiation treatment, and ipsilaterally or bilaterally but first or more severe at the side of tumor (the side that received more radiation dose), the role of radiation can’t be ruled out. However in our study, patients with cataract are significantly older (Table 7). In six cases we had bilateral cataract. In all of these cases, cataracts occurred simultaneously, or first occurred at the side of tumor. In two cases with radio-surgery (the last two cases in Suppl. 13), the radiation doses to the lenses were very low, but cataract in these cases occurred after radiation treatment, in one eye, at the side of tumor with relatively long intervals. Table 7 also shows that there is a trend that all the four risk factors may have a role in developing of cataract but only the difference regarding hypercholesterolemia is significant.
A point about dry eye and cataract patients is that in both groups, majority of tumors were located in vicinity of optic pathway and most of these patients were treated with 3D-conformal technique, rather than novel techniques (IMRT or SRS). This point shows that when we irradiate tumors around optic pathway, lachrymal glands and lenses are more vulnerable to radiation side-effects, especially if we do not apply novel techniques of radiation.
In our cohort, the local control rate was 88.8 % within a median follow up of 75 month. This correlates with the efficacy of radiotherapy for the treatment of meningiomas that was reported in several studies [14, 15] (Suppl. 8).
Conclusion
The low percentages of patients with radiation induced high grade optic toxicities including RION, dry eye and cataract, show that current treatment techniques and doses, including more sophisticated ones like stereotactic treatments are safe. However, delivered doses to the OARs in most of patients with optical side effects were less than the established constraint doses. Hence, the role of the risk factors and co-morbidities including age, arterial hypertension, hypercholesterolemia, diabetes and smoking in increasing the radiation induced side effects should be investigated in more comprehensive studies, especially with regard to brain tumors with good prognosis like meningioma. In addition, it seems necessary to evaluate the safety of higher radiation doses that seem to be more effective in high grade meningiomas.
References
Lessell S (2004) Friendly fire: neurogenic visual loss from radiation therapy. J Neuroophthalmol 24:243–250
Gordon KB, Char DH, Sagerman RH (1995) Late effects of radiation on the eye and ocular adnexa. Int J Radiat Oncol Biol Phys 31:1123–1139
Danesh-Meyer HV (2008) Review: radiation-induced optic neuropathy. J Clin Neurosci 15:95–100
Mayo C, Martel MK, Marks LB et al (2010) Radiation dose-volume effects of optic nerves and chiasm. Int J Radiat Oncol Biol Phys 76:S28–S35
Parsons JT, Bova FJ, Fitzgerald CR et al (1994) Radiation optic neuropathy after megavoltage external-beam irradiation: analysis of time–dose factors. Int J Radiat Oncol Biol Phys 30:755–763
Guy J, Mancuso A, Quisling RG, Beck R, Moster M (1990) Gadolinium-DTPAenhanced magnetic resonance imaging in optic neuropathies. Ophthalmology 97:592–600
Bhandare N, Monroe AT, Morris CG et al (2005) Does altered fractionation influence the risk of radiation-induced optic neuropathy? Int J Radiat Oncol Biol Phys 62:1070–1077
Behbehani R (2007) Clinical approach to optic neuropathies. Clin Ophthalmol 1(3):233–246
Onodera S, Aoyama H, Katoh N et al (2011) Long-term outcomes of fractionated stereotactic radiotherapy for intracranial skull base benign meningiomas in single institution. Jpn J Clin Oncol 41(4):462–468
Fowler JF (1989) Fractionation and therapeutic gain. In: Steel GG, Adams GE, Horwich A (eds) The biological basis of radiotherapy, 2nd edn. Elsevier, Amsterdam, pp S181–S207
Emami B, Lyman J, Brown A et al (1991) Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 21:109–122
Leavitt JA, Stafford SL, Link MJ, Pollock BE (2013) Long-term evaluation of radiation-induced optic neuropathy after single-fraction stereotactic radiosurgery. IJROBP 87(3):524–527
Martel MK, Sandler HM, Cornblath WT et al (1997) Dose–volume complication analysis for visual pathway structures of patients with advanced paranasal sinus tumors. Int J Radiat Oncol Biol Phys 38:273–284
Hamm K, Henzel M, Groß MW, Surber G, Kleinert G, Engenhart-Cabillic R (2008) Radiosurgery/stereotactic radiotherapy in the therapeutical concept for skull base meningiomas. Zentralbl Neurochir 69:14–21
Milker-Zabel S, Zabel-du Bois A, Huber P, Schlegel W, Debus J (2007) Intensity-modulated radiotherapy for complex-shaped meningioma of the skull base: long-term experience of a single institution. Int J Radiat Oncol Biol Phys 68:858–863
Khoo VS, Oldham M, Adams EJ, Bedford JL, Webb S, Brada M (1999) Comparison of intensity-modulated tomotherapy with stereotactically guided conformal radiotherapy for brain tumors. Int J Radiat Oncol 45:415–425
The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye Workshop (2007) Ocul Surf 5(2):93–107. http://www.ncbi.nlm.nih.gov/pubmed/17508117
Parsons JT, Bova FJ, Mendenhall WM, Million RR, Fitzgerald CR (1996) Response of the normal eye to high dose radiotherapy. Oncology 10(6):837–852
Parsons JT, Bova FJ, Fitzgerald CR et al (1994) Severe dry-eye syndrome following external beam irradiation. Int J Radiat Oncol Biol Phys 30(4):775–780
Bhandare N, Moiseenko V, Song WY et al (2012) Severe dry eye syndrome after radiotherapy for head-and-neck tumors. Int J Radiat Oncol Biol Phys 82(4):1501–1508
Brady LW, Perez CA (2013) Head and neck: eye and orbit. In: Halperin EC, Brady LW, Perez CA, DE Wazer (eds) Principles and practice of radiation oncology, 6th edn. Lippincott Williams & Wilkins, Philadelphia
Turner JE (2008) Chemical and biological effects of radiation: delayed somatic effects. In: Turner JE (ed) Atoms, radiation and radiation protection, 3rd edn. Wiley VCH, Oak Ridge
Rehani MM Radiation protection—cataract and protection. ESR @ Work November 2013. https://www.myesr.org/cms/website.php?id=/en/publications_media/esr_work/esr_work_november_2013/radiation_protection_-_cataract_and_protection.htm
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with Ethics Guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975 (in its most recently amended version).
Conflict of interest
None of the authors has any conflict of interest related to this work.
Additional information
We dedicate this publication to our dear colleague, Karin Roth, who passed away during the period she was working with us on this scientific project.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Farzin, M., Molls, M., Kampfer, S. et al. Optic toxicity in radiation treatment of meningioma: a retrospective study in 213 patients. J Neurooncol 127, 597–606 (2016). https://doi.org/10.1007/s11060-016-2071-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-016-2071-7