Abstract
Despite moderate improvements in outcome of glioblastoma after first-line treatment with chemoradiation recent clinical trials failed to improve the prognosis of recurrent glioblastoma. In the absence of a standard of care we aimed to investigate institutional treatment strategies to identify similarities and differences in the pattern of care for recurrent glioblastoma. We investigated re-treatment criteria and therapeutic pathways for recurrent glioblastoma of eight neuro-oncology centres in Switzerland having an established multidisciplinary tumour-board conference. Decision algorithms, differences and consensus were analysed using the objective consensus methodology. A total of 16 different treatment recommendations were identified based on combinations of eight different decision criteria. The set of criteria implemented as well as the set of treatments offered was different in each centre. For specific situations, up to 6 different treatment recommendations were provided by the eight centres. The only wide-range consensus identified was to offer best supportive care to unfit patients. A majority recommendation was identified for non-operable large early recurrence with unmethylated MGMT promoter status in the fit patients: here bevacizumab was offered. In fit patients with late recurrent non-operable MGMT promoter methylated glioblastoma temozolomide was recommended by most. No other majority recommendations were present. In the absence of strong evidence we identified few consensus recommendations in the treatment of recurrent glioblastoma. This contrasts the limited availability of single drugs and treatment modalities. Clinical situations of greatest heterogeneity may be suitable to be addressed in clinical trials and second opinion referrals are likely to yield diverging recommendations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma is the most common and devasting primary brain tumour with an annual incidence of about three per 100,000 [1] persons. It is associated with great morbidity and early mortality. Even after multimodal treatment with temozolomide chemoradiation (RT/TMZ → TMZ) progression-free survival (PFS) and overall survival (OS) remain poor with 6.9 and 14.2 months, respectively [2]. Recently, four large phase III trials failed to improve outcome after first-line therapy in terms of OS [3–6]. Hence, effective salvage treatment of recurrent glioblastoma remains a demanding problem in neuro-oncology.
The oral alkylating agent TMZ is widely used for the treatment of recurrent glioblastoma (TMZ re-challenge) [7–11]. However, the optimal dosing schedule and the minimal time interval from first line TMZ are unknown. This topic was investigated in a single prospective phase II trial using a metronomic TMZ schedule [9]. Patients with a tumour recurrence at least 3 months after RT/TMZ or 2 months after completion of RT/TMZ and six maintenance cycles of TMZ reached modest PFS rates after 6 months (PFS-6) of 27.3 and 35.7 %, respectively. Recently, two dose-intensified TMZ schedules have been prospectively investigated at first relapse after at least two cycles of maintenance TMZ after RT/TMZ to avoid interference with pseudoprogression [11]. None of the regimes were superior with a median time to treatment failure of 1.8 months [Arm A: one week on (120 mg/m2 per day)/one week off] and 2.0 months [Arm B: three weeks on (80 mg/m2 per day)/one week off], respectively. However, methylation of the MGMT promoter was a strong positive prognostic factor of PFS-6 (methylated 39.7 % vs. unmethylated 6.9 %) [11]. Small targeted drugs like enzastaurin or cediranib failed to show benefit in recent phase III trials when compared to lomustine in recurrent glioblastoma [12, 13]. Therefore, lomustine has advanced to a widely used alkylating drug either alone or in combination whenever TMZ is not considered to be appropriate for the treatment of recurrent glioblastoma [14, 15]. In contrast to the European Union, bevacizumab, an anti-angiogenic agent targeting VEGF-A, has been approved in selected countries (i.e. North America, Switzerland) for the treatment of recurrent glioblastoma based on uncontrolled phase II studies [16, 17].
Due to the limited efficacy of second-line systemic treatment, focal strategies with re-operation and re-irradiation have also been introduced as salvage treatments. However, little evidence for these therapies is available as most studies investigated only small or retrospective patient cohorts [18–25]. Furthermore, availability of stereotactic radiotherapy or radiosurgery and financial resources of health care systems account for significant differences in use between countries and even national regions.
As effective treatment options are scarce and controlled trials are rare for recurrent glioblastoma, therapeutic decisions are mostly based on low level evidence [26]. Beyond evidence, experience (eminence-based medicine) may provide additional guidance. Possibly, further information can be extracted from the community, for example as patterns of care studies [27]. Patterns of care studies often rely on specific scenarios which are presented to participants, these are then analysed; the limitation being that the answers are restricted to only these specific scenarios. When the collected information is appropriately formatted [28], e.g. decision trees are collected, patterns of practice can be analysed for multiple combinations of parameters [29]. In the setting of low evidence for salvage treatment we aimed to collect treatment algorithms from Swiss neuro-oncological centres which derive their treatment recommendations from multidisciplinary tumour boards. The collected information was used to perform a comprehensive patterns care and patterns of algorithms analysis for the treatment of recurrent glioblastoma.
Materials and methods
Based on specific parameters (characteristics of the patient and the disease) recommendations can be defined. The concept of diagnostic nodes (Dodes) has been developed [28, 29] to allow for a cross-comparison of recommendations in decision-tree format and has been applied in a clinical setting [30, 31]. Dodes are organized into decision trees using pre-defined categories. Standardized nomenclature of parameters and recommendations is a prerequisite for automated comparisons and an unbiased evaluation. Based on Dodes and the objective consensus methodology [29], consensus and heterogeneity were analysed (Fig. 1).
Analysis by the objective consensus method. Example of an early recurrent, small and resectable glioblastoma harbouring a methylated MGMT (mMGMT) promoter. For fit patients heterogeneous treatment options were recommended among the centres (A–H), whereas in unfit patients 6 out of 8 centres (A, B, E, G, H, F) suggested BSC and only two centres (C, D) recommended alternative treatments. Bev bevacizumab; Lom lomustine; OP operation; TMZ temozolomide; BSC best supportive care; SRS stereotactic radiosurgery; & combined treatment; + sequential treatment
Hospitals with an interdisciplinary neuro-oncology unit including at least full-time service of neuro-surgery, radiotherapy and medical neuro-oncology with a dedicated neuro-oncology tumour board being represented in the Swiss Group for clinical cancer research (SAKK) were asked to participate in the study. Treatment recommendations for recurrent glioblastoma were collected without specifications in formatting. Free-text, Microsoft PowerPoint slides and hand-drawn diagrams were converted without changing content into treatment algorithms and after several bilateral exchanges defined as final by 1st of January 2015. These were again discussed among the participating centres. Two centres took patient preference explicitly into account; these were related to the decision for active treatment versus best supportive care (BSC). Despite these criteria being important for daily practice, they were eliminated for the analysis as they do not rely on a tumour board decision and of course should apply to every clinical decision. Similar criteria were fused into new comprehensive categories to simplify their usage and enable cross-comparability (i.e. the criteria fitness based upon performance status, co-morbidities and age). The resulting data were presented to the participants and minor corrections were applied. The interpretation by all participants resulted in the final discussion.
Results
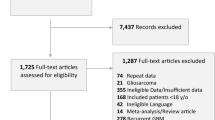
In total, 8 Swiss centres (Aarau, Basel, Bellinzona, Bern, Geneva, Lausanne, St. Gallen, Zurich) participated and provided written or schematic information of their interdisciplinary local treatment strategy for recurrent glioblastoma. The original treatment algorithms included a total of 23 re-treatment criteria and a list of 16 treatment options (Table 1; Fig. 2).
Processing and simplification
As the considerable variability of the re-treatment criteria lead to an exponential rise in possible combinations, we simplified and integrated similar criteria with minor differences (Table 1). For example, the various thresholds of Karnofsky performance scale (KPS), age, Eastern cooperative oncology group performance status (ECOG) and the presence of co-morbidities were summarized as “fit” or “unfit”. Additionally, tumours were summarized as “resectable” or “non-resectable” according to their occurrence in eloquent areas and non-diffuse/localized distribution. Need for steroid use and symptomatic recurrent glioblastoma were merged to only one category. After simplification the trees were analysed with the so defined 8 essential criteria. All centres used resectability, fitness and time of recurrence as re-treatment criteria. Five centres (A, C-E, H) used the MGMT promoter status. However, we gathered no information which method and threshold for MGMT promoter methylation status was used in clinical practise. Four centres used tumour size (B, C, G, H) and unifocality (C, E, F, H). Only three and two centres, respectively, took symptoms (F, G, H) and complete resection of enhancing tumour (CRET) (A, B) into account.
Re-treatment criteria
All centres dichotomised their decision to actively treat recurrent glioblastoma with anti-tumour strategies by using the performance status (PS). Generally, “unfit” patients with a low PS were referred to BSC without offering active oncological treatment. The KPS and the ECOG were both reported. However, the lowest threshold for active anti-tumour re-treatment varied considerably (KPS from 50 to 90; ECOG 0–1) (Table 1). The same was true for age (between 50 and 75 years). However, age was only reported as a re-treatment criterion in 2 out of 8 centres.
Re-treatment options
Five treatments were offered against recurrent glioblastoma in at least 4 centres (Fig. 2). These were the combination of re-operation with either TMZ or bevacizumab, monotherapy with either TMZ or bevacizumab and BSC. Interestingly, the time required to consider TMZ re-challenge ranged from 2 to 6 months. Four centres additionally relied on the MGMT promoter methylation status to indicate an alkylator-based systemic treatment (TMZ or lomustine). Various re-treatment modalities and schemes were reported among the centres (Fig. 2). These included re-operation, re-irradiation, chemotherapy or immunotherapy, either as a monotherapy or as a multimodal treatment. For example, therapy varied by the combination of anti-neoplastic agents (bevacizumab, lomustine, temozolomide, bevacizumab/lomustine given in standard dosing), the schedule of re- irradiation (40 Gy in 1.66 fractions, 42 Gy in 2.66 factions, 35 Gy in 3.5 fractions, 20 Gy in 2.0 fractions), re-irradiation with and without TMZ or bevacizumab and the method of re-irradiation (stereotactic radiotherapy (SRT), 3D-conformal or intensity modulated radiotherapy). Furthermore, criteria like the localisation and distribution of the tumour (local/distant recurrence; single/multiple/diffuse recurrence; operable/not-operable) were also taken into account (Table 1).
Consensus treatment strategies
Figure 3 displays a comprehensive and condensed view of the re-treatment recommendations for recurrent glioblastoma where a majority recommendation was present (5 out of 8 centres; 63 %). Seven out of 8 re-treatment criteria are implemented (time of recurrence, operability, size of the tumour, symptoms, fitness, MGMT promoter methylation and unifocality). The CRET criterion, which was only used in 2 centres (A, B), was not relevant to reach a majority treatment recommendation. Strong consensus was generally achieved in unfit patients. In all but one scenario 6 out of 8 centres recommended BSC instead of an anti-tumour treatment (fit = no). In contrast, in fit patients majority consensus was rare (fit = yes). Five out of 8 centres would treat fit patients with bevacizumab when a large non-operable early recurrent glioblastoma with an unmethylated MGMT promoter is present (asterisk in Fig. 3). Additionally, TMZ would be the preferred recommendation (hash in Fig. 3) in fit patients with a late recurrent, non-unifocal, non-operable and large glioblastoma with a methylated MGMT promoter with (5 out of 8 centres, 63 %) or without clinical symptoms (6 out of 8 centres, 75 %).
The most common recommendations tree reveals areas of consensus (at least 5 out of 8 centres, >63 %) for patients who are unfit (A–F). The most common recommendation is best supportive care (BSC). Only on 3 clinical scenarios either bevacizumab (BEV, asterisk) or temozolomide (TMZ, hash) (B,E,F) is recommended by the majority of centres depending on the presence of symptoms. Only 7 out of 8 re-treatment criteria (all but the CRET criterion, see Fig. 3) were relevant for achieving a majority recommendation
Discussion
In the absence of a standard of care for recurrent glioblastoma the aim of the present study was to investigate applied treatment strategies in 8 neuro-oncology centres in Switzerland. As we anticipated great heterogeneity we further aimed to identify clinical criteria which lead to individualized treatment decisions and to check if these criteria overlap between different centres. Our expectations in this regard were met as we identified various treatment modalities and multiple schedules as well as a plethora of various criteria for the treatment of recurrent glioblastoma. Based on these results, it is very unlikely that patients with recurrent glioblastoma obtain the same treatment recommendation twice if they seek a second opinion in Switzerland. On the one hand this is due to individualized treatments for a given patient and takes patient- and centre-specific factors into account (i.e. availability of certain treatment options). On the other hand different recommendation can cause a decision dilemma for the patient.
Original parameters could be processed and reformatted with the help of a standardized procedure (Dodes). This method enables the identification of the most common treatment recommendations for any specific parameter combination [29]. The process was feasible and produced the most commonly agreed upon treatment recommendation derived from heterogeneous references. The data presented here might therefore serve as one basis to develop a nationwide treatment guideline. Moreover, areas of controversy or low overlap can be used to address clinically important questions for future clinical trials.
All centres used the PS to decide about the indication of a tumour specific therapy. PS was measured with the KPS and ECOG which are well known instruments of daily oncological practice [14]. Additionally, age was a relevant criterion to guide treatment in some centres. PS and age are established prognostic factors for first-line as well as for second-line treatments [14, 32–36]. Recent studies set a threshold of KPS 60 % (corresponding to ECOG 2) as a prerequisite for tumour specific treatment interventions [4, 5, 37, 38] as inferior PS is associated with increased side effects from any intervention and lowers the chance of clinical benefit [14, 36, 39]. The greatest consensus in our analysis was identified in unfit patients corresponding to a low PS. These patients would be mostly referred to BSC as the strategy of choice independent of operability, MGMT promoter methylation or time of recurrence, among other criteria (Fig. 3). Accordingly, this approach represents a robust consensus recommendation. This result is not trivial, as three out of eight centres did not actively claimed BSC as a primary re-treatment modality even after several feed-back rounds (Fig. 2). However, we are confident that a low PS would lead to the implementation of BSC without additional tumour specific treatment in daily practise in all centres. This issue might reflect a limitation of the study that not all applied treatment strategies are specifically enumerated by the participants.
Despite the negative prognostic impact of mental and cognitive decline [39] none of the centres reported mental status or a formal cognitive testing (i.e. MiniMental Status Exam) as an aid to decide about treatment for recurrent glioblastoma. It is tempting to speculate that the physicians felt they integrate all dimensions of neurological function in clinical decision making and do not need these scales for whatever reason (i.e. time consuming procedure). Co-morbidities and their formal investigation were also rarely taken into account (i.e. Charlson co-morbidity score) and none of the centres reported usage of a structured geriatric assessment [40–43]. Hence, the issue of fitness for re-treatment in recurrent glioblastoma mostly relies on a subjective perspective of the physician.
Various strategies of re-operation, re-irradiation, systemic therapy and multimodal treatments were reported [14]. Major level of consensus was reached for TMZ re-challenge in lesions with a methylated MGMT promoter even in the absence of a controlled trial at the time of investigation. Only recently, the DIRECTOR and the BELOB trial demonstrated the prognostic value of the MGMT-promoter methylation for PFS-6 and PFS-9, respectively, with significantly better outcome in recurrent glioblastoma with a methylated MGMT promoter [11, 15]. However, the optimal time span between first-line and second-line TMZ at recurrence still remains elusive.
The anti-angiogenic agent bevacizumab is approved for the treatment of recurrent glioblastoma in selected countries including Switzerland. Somewhat surprisingly, only in fit, non-operable patients with a large lesion and an unmethylated MGMT promoter a majority of centres (63 %) would offer bevacizumab. No consensus was obvious in all other occasions, despite approval and its steroid-sparing properties. The reason for this low overlap might be related to the absence of a controlled clinical trial for the use of bevacizumab in recurrent glioblastoma or the recently reported failure in the first-line treatment setting [4, 38]. Moreover, conflicting results about a negative impact on neuro-cognition may also hamper widespread use of this compound [44, 45].
Re-irradiation alone or in combination with systemic treatment did not reach any consensus. In addition to the paucity of controlled clinical trials this might reflect heterogeneity of radiation dose and technique. Despite the low efficacy of re-irradiation as a monotherapy observed in a controlled phase II trial with PFS-6 rates of 3.8 % [24] a second radiation either alone or in combination with systemic therapy still remained a salvage treatment in five out of eight centres. However, this applies only in a selected patient population with good prognostic criteria. Of note, the same is true for re-operation which is mostly recommended in combination with other treatments in 7 out of 8 centres. Additionally, a controlled clinical trial demonstrating efficacy of this approach is also lacking. However, positive prognostic criteria (KPS > 80, tumour size ≤ 50 ml, non-eloquent region) for the estimation of prolonged postoperative survival after re-operation have been reported [46]. In this regard it has to be mentioned that local treatment strategies are driven by the experience of the local physicians, the availability to diverse radiation techniques and the attitude of neuro-surgeons to offer glioblastoma resection at recurrence.
Conclusion
The neuro-oncologist may be equally soothed or unsettled by these results. For certain clinical scenarios, 8 centres provided 6 different treatment recommendations. This sheds an interesting light on the value and risk of obtaining a second opinion in this context. Despite experience and access to published literature, the interpretation and clinical implementation of this was very different among Swiss neuro-oncology centres.
The application of a decision tree analysis (objective consensus) was able to identify decision criteria relevant in clinical practice across centres. Future trials and guidelines should take these criteria into account to ease the transition of trial results and recommendations into clinical neuro-oncology.
References
Ostrom QT, Bauchet L, Davis FG, Deltour I, Fisher JL, Langer CE, Pekmezci M, Schwartzbaum JA, Turner MC, Walsh KM (2014) The epidemiology of glioma in adults: a “state of the science” review. Neuro-oncology 16:896–913
Stupp R, Mason WP, Van Den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, Colman H, Chakravarti A, Pugh S, Won M (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370:699–708
Gilbert MR, Wang M, Aldape KD, Stupp R, Hegi ME, Jaeckle KA, Armstrong TS, Wefel JS, Won M, Blumenthal DT, Mahajan A, Schultz CJ, Erridge S, Baumert B, Hopkins KI, Tzuk-Shina T, Brown PD, Chakravarti A, Curran WJ Jr, Mehta MP (2013) Dose-dense temozolomide for newly diagnosed glioblastoma: a randomized phase III clinical trial. Journal of Clinical Oncology 31:4085–4091. doi:10.1200/JCO.2013.49.6968
Stupp R, Hegi ME, Gorlia T, Erridge SC, Perry J, Hong Y-K, Aldape KD, Lhermitte B, Pietsch T, Grujicic D (2014) Cilengitide combined with standard treatment for patients with newly diagnosed glioblastoma with methylated MGMT promoter (CENTRIC EORTC 26071-22072 study): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol 15:1100–1108
Chinot OL, Wick W, Mason W, Henriksson R, Saran F, Nishikawa R, Carpentier AF, Hoang-Xuan K, Kavan P, Cernea D (2014) Bevacizumab plus radiotherapy—temozolomide for newly diagnosed glioblastoma. N Engl J Med 370:709–722
Wick W, Steinbach JP, Kuker WM, Dichgans J, Bamberg M, Weller M (2004) One week on/one week off: a novel active regimen of temozolomide for recurrent glioblastoma. Neurology 62:2113–2115
Brandes AA, Tosoni A, Cavallo G, Bertorelle R, Gioia V, Franceschi E, Biscuola M, Blatt V, Crino L, Ermani M, Gicno (2006) Temozolomide 3 weeks on and 1 week off as first-line therapy for recurrent glioblastoma: phase II study from gruppo italiano cooperativo di neuro-oncologia (GICNO). Br J Cancer 95:1155–1160. doi:10.1038/sj.bjc.6603376
Perry JR, Belanger K, Mason WP, Fulton D, Kavan P, Easaw J, Shields C, Kirby S, Macdonald DR, Eisenstat DD, Thiessen B, Forsyth P, Pouliot JF (2010) Phase II trial of continuous dose-intense temozolomide in recurrent malignant glioma: RESCUE study. Journal of Clinical Oncology 28:2051–2057. doi:10.1200/JCO.2009.26.5520
Norden AD, Lesser GJ, Drappatz J, Ligon KL, Hammond SN, Lee EQ, Reardon DR, Fadul CE, Plotkin SR, Batchelor TT, Zhu JJ, Beroukhim R, Muzikansky A, Doherty L, Lafrankie D, Smith K, Tafoya V, Lis R, Stack EC, Rosenfeld MR, Wen PY (2013) Phase 2 study of dose-intense temozolomide in recurrent glioblastoma. Neuro-oncology 15:930–935. doi:10.1093/neuonc/not040
Weller M, Tabatabai G, Kastner B, Felsberg J, Steinbach JP, Wick A, Schnell O, Hau P, Herrlinger U, Sabel MC, Wirsching HG, Ketter R, Bahr O, Platten M, Tonn JC, Schlegel U, Marosi C, Goldbrunner R, Stupp R, Homicsko K, Pichler J, Nikkhah G, Meixensberger J, Vajkoczy P, Kollias S, Husing J, Reifenberger G, Wick W, Group DS (2015) MGMT promoter methylation is a strong prognostic biomarker for benefit from dose-intensified temozolomide rechallenge in progressive glioblastoma: the DIRECTOR Trial. Clin Cancer Res 21:2057–2064. doi:10.1158/1078-0432.CCR-14-2737
Wick W, Puduvalli VK, Chamberlain MC, van den Bent MJ, Carpentier AF, Cher LM, Mason W, Weller M, Hong S, Musib L (2010) Phase III study of enzastaurin compared with lomustine in the treatment of recurrent intracranial glioblastoma. J Clin Oncol 28:1168–1174
Batchelor TT, Mulholland P, Neyns B, Nabors LB, Campone M, Wick A, Mason W, Mikkelsen T, Phuphanich S, Ashby LS (2013) Phase III randomized trial comparing the efficacy of cediranib as monotherapy, and in combination with lomustine, versus lomustine alone in patients with recurrent glioblastoma. J Clin Oncol 31:3212–3218
Weller M, van den Bent M, Hopkins K, Tonn JC, Stupp R, Falini A, Cohen-Jonathan-Moyal E, Frappaz D, Henriksson R, Balana C, Chinot O, Ram Z, Reifenberger G, Soffietti R, Wick W, European Association for Neuro-Oncology Task Force on Malignant G (2014) EANO guideline for the diagnosis and treatment of anaplastic gliomas and glioblastoma. Lancet Oncol 15:e395–e403. doi:10.1016/S1470-2045(14)70011-7
Taal W, Oosterkamp HM, Walenkamp AM, Dubbink HJ, Beerepoot LV, Hanse MC, Buter J, Honkoop AH, Boerman D, de Vos FY, Dinjens WN, Enting RH, Taphoorn MJ, van den Berkmortel FW, Jansen RL, Brandsma D, Bromberg JE, van Heuvel I, Vernhout RM, van der Holt B, van den Bent MJ (2014) Single-agent bevacizumab or lomustine versus a combination of bevacizumab plus lomustine in patients with recurrent glioblastoma (BELOB trial): a randomised controlled phase 2 trial. Lancet Oncol 15:943–953. doi:10.1016/S1470-2045(14)70314-6
Kreisl TN, Zhang W, Odia Y, Shih JH, Butman JA, Hammoud D, Iwamoto FM, Sul J, Fine HA (2011) A phase II trial of single-agent bevacizumab in patients with recurrent anaplastic glioma. Neuro-oncology 13:1143–1150
Vredenburgh JJ, Desjardins A, Herndon JE 2nd, Dowell JM, Reardon DA, Quinn JA, Rich JN, Sathornsumetee S, Gururangan S, Wagner M, Bigner DD, Friedman AH, Friedman HS (2007) Phase II trial of bevacizumab and irinotecan in recurrent malignant glioma. Clin Cancer Res 13:1253–1259. doi:10.1158/1078-0432.CCR-06-2309
Woernle CM, Peus D, Hofer S, Rushing EJ, Held U, Bozinov O, Krayenbuhl N, Weller M, Regli L (2015) Efficacy of surgery and further treatment of progressive glioblastoma. World Neurosurg. doi:10.1016/j.wneu.2015.03.018
Franceschi E, Bartolotti M, Tosoni A, Bartolini S, Sturiale C, Fioravanti A, Pozzati E, Galzio R, Talacchi A, Volpin L, Morandi L, Danieli D, Ermani M, Brandes AA (2015) The effect of re-operation on survival in patients with recurrent glioblastoma. Anticancer Res 35:1743–1748
Vuorinen V, Hinkka S, Farkkila M, Jaaskelainen J (2003) Debulking or biopsy of malignant glioma in elderly people—a randomised study. Acta Neurochir (Wien) 145:5–10. doi:10.1007/s00701-002-1030-6
Fogh SE, Andrews DW, Glass J, Curran W, Glass C, Champ C, Evans JJ, Hyslop T, Pequignot E, Downes B, Comber E, Maltenfort M, Dicker AP, Werner-Wasik M (2010) Hypofractionated stereotactic radiation therapy: an effective therapy for recurrent high-grade gliomas. J Clin Oncol 28:3048–3053. doi:10.1200/JCO.2009.25.6941
Mizumoto M, Okumura T, Ishikawa E, Yamamoto T, Takano S, Matsumura A, Oshiro Y, Ishikawa H, Sakurai H, Tsuboi K (2013) Reirradiation for recurrent malignant brain tumor with radiotherapy or proton beam therapy. Technical considerations based on experience at a single institution. Strahlenther Onkol 189:656–663. doi:10.1007/s00066-013-0390-6
Gutin PH, Iwamoto FM, Beal K, Mohile NA, Karimi S, Hou BL, Lymberis S, Yamada Y, Chang J, Abrey LE (2009) Safety and efficacy of bevacizumab with hypofractionated stereotactic irradiation for recurrent malignant gliomas. Int J Radiat Oncol Biol Phys 75:156–163. doi:10.1016/j.ijrobp.2008.10.043
Wick W, Fricke H, Junge K, Kobyakov G, Martens T, Heese O, Wiestler B, Schliesser MG, von Deimling A, Pichler J, Vetlova E, Harting I, Debus J, Hartmann C, Kunz C, Platten M, Bendszus M, Combs SE (2014) A phase II, randomized, study of weekly APG101 + reirradiation versus reirradiation in progressive glioblastoma. Clin Cancer Res 20:6304–6313. doi:10.1158/1078-0432.CCR-14-0951-T
Hundsberger T, Brügge D, Putora PM, Weder P, Weber J, Plasswilm L (2013) Re-irradiation with and without bevacizumab as salvage therapy for recurrent or progressive high-grade gliomas. J Neurooncol 112:133–139
Weller M, Cloughesy T, Perry JR, Wick W (2013) Standards of care for treatment of recurrent glioblastoma—are we there yet? Neuro-oncology 15:4–27
Putora PM, Oldenburg J (2013) Swarm-based medicine. J Med Internet Res 15:e207. doi:10.2196/jmir.2452
Putora PMBM, Papachristofilou A, Mariotti F, Paoli B, Plasswilm L (2010) Dodes (diagnostic nodes) for guideline manipulation. J Radiat Oncol Inf 2:1–8
Putora PM, Panje CM, Papachristofilou A, Dal Pra A, Hundsberger T, Plasswilm L (2014) Objective consensus from decision trees. Radiat Oncol 9:270
Rothermundt C, Bailey A, Cerbone L, Eisen T, Escudier B, Gillessen S, Grunwald V, Larkin J, McDermott D, Oldenburg J, Porta C, Rini B, Schmidinger M, Sternberg C, Putora PM (2015) Algorithms in the first-line treatment of metastatic clear cell renal cell carcinoma-analysis using diagnostic nodes. Oncologist 20:1028–1035. doi:10.1634/theoncologist.2015-0145
Panje CM, Dal Pra A, Zilli T, Daniel RZ, Papachristofilou A, Herrera FG, Matzinger O, Plasswilm L, Putora PM (2015) Consensus and differences in primary radiotherapy for localized and locally advanced prostate cancer in Switzerland: a survey on patterns of practice. Strahlenther Onkol. doi:10.1007/s00066-015-0849-8
Batchelor TT, Mulholland P, Neyns B, Nabors LB, Campone M, Wick A, Mason W, Mikkelsen T, Phuphanich S, Ashby LS, Degroot J, Gattamaneni R, Cher L, Rosenthal M, Payer F, Jurgensmeier JM, Jain RK, Sorensen AG, Xu J, Liu Q, van den Bent M (2013) Phase III randomized trial comparing the efficacy of cediranib as monotherapy, and in combination with lomustine, versus lomustine alone in patients with recurrent glioblastoma. J Clin Oncol 31:3212–3218. doi:10.1200/JCO.2012.47.2464
Wick W, Puduvalli VK, Chamberlain MC, van den Bent MJ, Carpentier AF, Cher LM, Mason W, Weller M, Hong S, Musib L, Liepa AM, Thornton DE, Fine HA (2010) Phase III study of enzastaurin compared with lomustine in the treatment of recurrent intracranial glioblastoma. J Clin Oncol 28:1168–1174. doi:10.1200/JCO.2009.23.2595
Weller M, Cloughesy T, Perry JR, Wick W (2013) Standards of care for treatment of recurrent glioblastoma–are we there yet? Neuro-oncology 15:4–27. doi:10.1093/neuonc/nos273
Mariniello G, Peca C, De Caro Mdel B, Giamundo A, Donzelli R, Maiuri F (2014) Glioblastoma in the elderly: the impact of advanced age on treatment and survival. J Neurol Surg A Cent Eur Neurosurg 75:276–281. doi:10.1055/s-0033-1349713
Kirkpatrick JP, Sampson JH (2014) Recurrent malignant gliomas. Semin Radiat Oncol 24:289–298. doi:10.1016/j.semradonc.2014.06.006
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for R, Treatment of Cancer Brain T, Radiotherapy G, National Cancer Institute of Canada Clinical Trials G (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. The New England journal of medicine 352:987–996. doi:10.1056/NEJMoa043330
Chinot OL, de La Motte Rouge T, Moore N, Zeaiter A, Das A, Phillips H, Modrusan Z, Cloughesy T (2011) AVAglio: phase 3 trial of bevacizumab plus temozolomide and radiotherapy in newly diagnosed glioblastoma multiforme. Adv Ther 28:334–340. doi:10.1007/s12325-011-0007-3
Gorlia T, van den Bent MJ, Hegi ME, Mirimanoff RO, Weller M, Cairncross JG, Eisenhauer E, Belanger K, Brandes AA, Allgeier A, Lacombe D, Stupp R (2008) Nomograms for predicting survival of patients with newly diagnosed glioblastoma: prognostic factor analysis of EORTC and NCIC trial 26981-22981/CE.3. Lancet Oncol 9:29–38. doi:10.1016/S1470-2045(07)70384-4
Fiorentino A, Caivano R, Chiumento C, Cozzolino M, Clemente S, Pedicini P, Fusco V (2012) Comorbidity assessment and adjuvant radiochemotherapy in elderly affected by glioblastoma. Med Oncol 29:3467–3471. doi:10.1007/s12032-012-0246-4
Balducci M, Fiorentino A, De Bonis P, Chiesa S, Manfrida S, D’Agostino GR, Mantini G, Frascino V, Mattiucci GC, De Bari B, Mangiola A, Micciche F, Gambacorta MA, Colicchio G, Morganti AG, Anile C, Valentini V (2012) Impact of age and co-morbidities in patients with newly diagnosed glioblastoma: a pooled data analysis of three prospective mono-institutional phase II studies. Med Oncol 29:3478–3483. doi:10.1007/s12032-012-0263-3
Ackerl M, Flechl B, Dieckmann K, Preusser M, Widhalm G, Sax C, Marosi C (2014) Outcome evaluation in glioblastoma patients older than 65 years: importance of individual assessment of treatment tolerance. Clin Neuropathol 33:399–406. doi:10.5414/NP300761
Bauchet L, Zouaoui S, Darlix A, Menjot de Champfleur N, Ferreira E, Fabbro M, Kerr C, Taillandier L (2014) Assessment and treatment relevance in elderly glioblastoma patients. Neuro-oncology 16:1459–1468. doi:10.1093/neuonc/nou063
Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, Colman H, Chakravarti A, Pugh S, Won M, Jeraj R, Brown PD, Jaeckle KA, Schiff D, Stieber VW, Brachman DG, Werner-Wasik M, Tremont-Lukats IW, Sulman EP, Aldape KD, Curran WJ Jr, Mehta MP (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370:699–708. doi:10.1056/NEJMoa1308573
Chinot OL, Wick W, Mason W, Henriksson R, Saran F, Nishikawa R, Carpentier AF, Hoang-Xuan K, Kavan P, Cernea D, Brandes AA, Hilton M, Abrey L, Cloughesy T (2014) Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med 370:709–722. doi:10.1056/NEJMoa1308345
Park JK, Hodges T, Arko L, Shen M, Dello Iacono D, McNabb A, Olsen Bailey N, Kreisl TN, Iwamoto FM, Sul J, Auh S, Park GE, Fine HA, Black PM (2010) Scale to predict survival after surgery for recurrent glioblastoma multiforme. J Clin Oncol 28:3838–3843. doi:10.1200/JCO.2010.30.0582
Acknowledgments
TH, LP received honaria for advisory board lecture and travel grants from Roche and MSD. PR received honoraria for advisory board activities or lectures from MSD, Roche, Novartis and Molecular Partners. MW has received research grants from Acceleron, Actelion, Alpinia Institute, Bayer, Isarna, MSD, Merck & Co, Novocure, PIQUR and Roche and honoraria for lectures or advisory board participation or consulting from Celldex, Immunocellular, Isarna, Magforce, MSD, Merck & Co, Northwest Biotherapeutics, Novocure, Pfizer, Roche and Teva.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AFH, UR, DM, PYD, KC, EH, AP, MWG, DB disclosed no conflict of interest.
Ethical standards
No specific patient data was used in this project.
Funding
The Department of Radiation Oncology (PMP) at the Cantonal hospital St. Gallen received a grant from Roche, Switzerland to perform this analysis.
Additional information
On behalf of the Swiss Group for Clinical Cancer Research (SAKK) Central Nervous System working group.
Rights and permissions
About this article
Cite this article
Hundsberger, T., Hottinger, A.F., Roelcke, U. et al. Patterns of care in recurrent glioblastoma in Switzerland: a multicentre national approach based on diagnostic nodes. J Neurooncol 126, 175–183 (2016). https://doi.org/10.1007/s11060-015-1957-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1957-0