Abstract
Epilepsy is common in patients with brain tumors. Patients presenting seizures as the first sign of a malignant glioma are at increased risk of recurrent seizures despite treatment with antiepileptic drugs. However, little is known about the incidence of epilepsy in the last stage of disease and in the end–of-life phase of brain tumor patients. We retrospectively analyzed the incidence of seizures in the last months of life in a series of patients affected by high-grade gliomas who were assisted at home during the whole course of the disease until death. A total of 157 patients were available for analysis. Of these patients, 58 (36.9 %) presented seizures in the last month before death. The risk of seizures in the end-of-life phase is higher in patients presenting previous history of epilepsy, particularly in patients with late-onset epilepsy. Out of the 58 patients presenting seizures in the last month of life, 86.2 % had previously had seizures and 13.8 % were seizure free. Most patients may encounter swallowing difficulties in taking anticonvulsants orally due to dysphagia and disturbances of consciousness, thus anticonvulsant treatment needs to be modified in advance. Loss of seizure control in the end-of-life phase may influence the quality of life of patients and their caregivers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Epilepsy is common in patients with brain tumors (BT), with more than one-third of cases with primary brain tumors presenting epileptic seizures during the course of disease [1–3]. Seizures may represent the symptom leading to diagnosis of glioma, but they may also appear at glioma recurrence or during disease progression [4–7]. The frequency of epilepsy in patients with BT is 30 % or more depending on tumor type [1, 2]. For 30–50 % of patients with BT, an epileptic seizure is the presenting clinical sign of a tumor; 10–30 % will develop seizures later on in the course of disease [4, 8]. Several factors affect epileptogenesis in patients with BT, including tumor histology, tumor location, changes in peritumoral environment, and genetic factors [5, 6, 8–11]. Low-grade gliomas (LGG) are the most epileptogenic, and seizure occurrence is reported in 60–88 % of patients. The frequency of seizures in high-grade glioma is lower (30–50 % in glioblastoma). Epilepsy may occur at the onset of disease or in the follow-up phase (late-onset seizures) [4]. In patients without seizures at the onset of disease, the probability of developing epilepsy is reported to be relatively low [6, 12]. Patients with malignant glioma, who commonly present with seizures as the first sign, are at increased risk of recurrent seizures [4]. Recurrent seizures are frequent (50–75 %) in patients presenting seizures in spite of treatment with antiepileptic drugs (AEDs) [4, 13]. Seizure control is an important issue in clinical management and supportive care in neuro-oncology. Quality of life of BT patients is strongly influenced by the severity of epilepsy and intensity of anticonvulsant treatment. Moreover, patients presenting uncontrolled seizures have been reported to suffer from major neurological deficits including a number of neuropsychological and psychological problems [13–15]. Several papers have reported the incidence of seizures at the onset or in the course of disease, but little is known about the frequency of epilepsy in the last stage of disease and in the end-of-life phase of BT patients [12, 16–18]. Recent papers have reported a surprising high incidence of epilepsy (37–50 %) in the last week of life of BT patients [16–18]. Epilepsy seems to be one of the more frequent symptoms in the last stage of disease. Even patients not presenting epilepsy in their previous history of disease may present seizures in the last period of life [4].
In a small series of BT patients dying in hospital, almost 50 % of patients presented seizures in the last 2 weeks before death [17]. In a previous study by our group on “End of Life issues in BT patients,” we reported that epilepsy represents a major issue in the management of dying patients, particularly in those assisted at home [18]. Seizure occurrence in the last period of life may influence the quality of life of patients and families. It further requires adequate supportive care and treatment modifications, considering that most patients in their end-of-life phase present symptoms, for instance, disturbances of consciousness and dysphagia, that may affect oral intake of drugs [17].
In the terminal phase of the disease, as a result of social, economic, individual, and cultural reasons, some patients are admitted to hospital, while others die in hospices or at home. The different settings of care in the end-of-life phase of BT patients may explain the lack of data in the neuro-oncology literature providing the real incidence of symptoms and supportive care needs. The aim of this study is to evaluate the incidence of seizures in the last months of life in a series of patients affected by high-grade gliomas assisted at home during the whole course of the disease until death.
Materials and methods
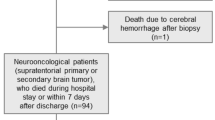
At the Regina Elena National Cancer Institute, Rome, a pilot project called “Palliative home-care for neuro-oncological patients,” including a comprehensive program of home care supported by the Regione Lazio Health System, has been carried out since 2000. The home staff included one neurologist, two physiotherapists, two psychologists, one social worker, and four specialist nurses. Home assistance for patients discharged by our institution included neurologic surveys, nurse assistance, neurorehabilitation, psychological support, and social worker support for patients and families. In the late stages of the disease, patients received daily home visits for palliative and supportive care, nursing, and psychological support. With the aim to collect data on symptoms experienced in the last stage of the disease, particularly regarding incidence of seizures, in 2005 an electronic record system was established to collect history data on seizures (seizure incidence before the last month of life), seizure frequency during the last month of life, and related anticonvulsant treatment. We defined seizures according to the International League Against Epilepsy (ILAE) classification system [19]. Previous seizures were defined as seizure at onset in case of epilepsy as the presenting symptom of the tumor or late-onset epilepsy in case of seizures occurring during the course of the disease but not present previously. Incidence of symptoms affecting oral intake of drugs (disturbances of consciousness and dysphagia) was also collected.
Characteristics of patients, and incidence of neurological symptoms and complications in the last stage of disease, were retrospectively collected from home care clinical records. One hundred fifty-seven records of patients dying between 2005 and 2009 were available for analysis.
Statistical analysis
SPSS software 15.0 was used for statistical analysis. Baseline characteristics and incidence were analyzed by means of descriptive statistics. Chi-square tests and T tests were used to test differences in baseline characteristics between the studied patients and other patients in the cohort.
Results
One hundred fifty-seven records of consecutive patients who died at home between 2005 and 2009 were available for the analysis. Patients who died in other settings (hospitals or hospices) were not included in this study. All patients were affected by high-grade gliomas (grade 3 and grade 4).
Overall, 58 (36.9 %) patients presented one or more seizures in the last month before death. All patients except eight were administered antiepileptic therapy. Seizure type was focal in 79 % of cases and secondarily generalized in 18 %, and 2.5 % of patients had epileptic status. There was no significant difference of gender between patients with or without seizures in the last month of life (chi-square 0,330; p = 0.566).
Concerning previous seizure history (epilepsy before last month of life), 85 (54.1 %) of patients reported at least one seizure during disease and 72 (45.8 %) were seizure free.
Among 85 patients presenting seizures during the course of disease, 61.1 % of patients (52/85) had seizures at onset and 38.8 % (33/85) presented late-onset epilepsy.
The risk of seizures in the end-of-life phase was found to be higher in patients presenting previous history of epilepsy, particularly in patients with late-onset epilepsy: out of 52 patients presenting epilepsy at onset, 25 (48.1 %) presented seizures in the last month of life; out of 33 patients presenting late-onset epilepsy, 25 (75.8 %) presented seizures in the last month of life (p < 0.001) (Table 1). Among the 99 patients not presenting seizures in the last month of life, 41.2 % experienced seizures during the course of the disease and 64.7 % were seizure free [p < 0.0001; odds ratio (OR) 11.429, confidence interval (CI): 4.872–26.806].
Eight patients (5.0 %) not experiencing seizures in the previous history of disease presented seizures in the last month of life.
There was no significant correlation between seizure occurrence and tumor histology (chi-square 1,735; p = 0.42). Furthermore, we did not observe any significant differences between tumor location in the brain and incidence of epilepsy in the end-of-life phase (chi-square 1,735; p = 0.52).
Anticonvulsant treatment
The majority of patients (n = 138) were treated with AEDs. Among the group of 99 patients not presenting seizures during the course of disease, only 19 patients (12.1 %) were not treated with prophylactic AED therapy; none of them experienced seizures.
No correlations were observed between AED treatment and probability of presenting seizures in the end-of–life phase. Among patients presenting seizures in the last month of life, 86.2 % were taking AEDs.
Neurological deterioration in the end-of-life phase, particularly difficulty in swallowing, disturbances of consciousness, and palliative sedation, may influence oral intake of AEDs. In our population of BT patients followed at home in the last month of life, 110 patients (70 %) presented mild to severe dysphagia, and 88 required parenteral hydration. Ninety-nine patients (63 %) presented disturbances of consciousness from lethargy to coma lasting from 1 to 31 days before death. In another eight cases, pharmacological palliative sedation was initiated in response to delirium. Only 29 (18.4 %) patients were able to swallow oral drugs until the last days of life.
Considering the difficulty in ability to swallow due to progressive neurological deterioration, we modified antiepileptic therapy in 130 patients in advance, independently of seizure occurrence, introducing parenteral AEDs (mainly intramuscular phenobarbital).
Discussion
Little is known about the symptoms and needs of BT patients in the end-of-life phase, with too many patients not receiving adequate supportive care [17]. However, increased attention is being paid to palliative care and end-of-life issues in neuro-oncology. There is a large consensus regarding the need to improve knowledge regarding patients in end-of-life care and enhancing the quality of palliative care for patients dying from BTs. Patients and their caregivers should be assisted in an adequate setting by a well-trained neuro-oncology multidisciplinary palliative team dedicated to managing frequent symptoms. Recently, some studies have focused on supportive care needs of BT patients in the last stage of disease [16–18]. A surprisingly high incidence of epilepsy in patients with BT has been reported in these studies, but still few data are available on epilepsy in the last stage of disease. This is the first study reporting the incidence of epilepsy in the end-of-life phase in a large population of patients with high-grade gliomas assisted at home until death. Our results show that epilepsy is one of the most frequent symptoms in the last stage of disease of BT patients (36.9 %).
The risk of presenting seizures in the last month of disease is significantly higher in patients with previous history of epilepsy (86.2 % in patients with previous seizures versus 13.8 % in seizure-free patients). Seizures may occur in the last days of life also in patients not experiencing seizures previously.
Given the high incidence of seizures in the last period of life, anticonvulsant treatment in this stage of disease needs to be optimized. Recommendations for use of AEDs in neuro-oncology are available, but not specifically focused on the terminal phase of the disease [18, 20–22]. The majority of patients in the last month of life of our series had difficulty in taking drugs orally due to dysphagia, disturbances of consciousness, or both, thus showing that use of more commonly utilized oral AEDs in the end-of-life phase may be problematic. In the last stage of the disease, neuro-oncologists should modify the prescription of AEDs in advance [17]. Oral treatment needs to be adapted according to the various ways of administering the drugs (intramuscular, rectal, transdermal, or subcutaneous). The issues concerning AED prophylaxis in high-risk patients in the end-of-life phase and regarding the route of antiepileptic administration need to be better evaluated by carrying out larger studies. At present, there are no data regarding the preferred drug [16]. The availability of AEDs for parenteral use may be different in various countries; however, in our experience we preferred use of intramuscular phenobarbital in patients assisted at home or intravenous levetiracetam in hospitalized patients.
This study presents several limits due to possibly underestimating seizure incidence in this population of patients. Moreover, in the home care setting and in the end-of-life phase, it does not allow us to obtain neurophysiologic data and serum concentration of AEDs that may influence seizure incidence.
The occurrence of seizures in the end-of-life phase may influence the quality of life of patients and their caregivers. Moreover, lack of control of symptoms often leads to rehospitalization, increasing healthcare system costs and more importantly worsening patients’ quality of life. Correct management and information given to families may avoid inappropriate hospital readmission in case of uncontrolled seizures. BT patients’ symptoms in the end-of-life phase are particularly complex, requiring a multidisciplinary approach by a well-trained neuro-oncology team.
However, currently there is a lack of palliative care provision for patients affected by advanced brain tumor. Nevertheless, there is a great need for education in palliative and end-of-life care in neuro-oncology. Wider availability of palliative programs and home care models of assistance may represent an alternative to in-hospital care for managing patients dying of brain tumors and may improve the quality of end-of-life care [23].
Further clinical research is needed to develop specific palliative care guidelines for appropriate management of patients with BTs.
References
Liigant A, Haldre S, Oun A et al (2001) Seizure disorders in patients with brain tumours. Eur Neurol 45:46–51
Lynam LM, Lyons MK, Drazkowski JF et al (2007) Frequency of seizures in patients with newly diagnosed brain tumors: a retrospective review. Clin Neurol Neurosurg 109:634–638
Van breemen MS, Brogna C, Gil Robles S, Duffau H (2008) Brain tumors and epilepsy. Expert Rev Neurother 8(6):941–955
Hildebrand J, Lecaille C, Perennes J et al (2005) Epileptic seizures during follow-up of patients treated for primary brain tumors. Neurology 65:212–215
Scott GM, Gibberd FB (1980) Epilepsy and other factors in the prognosis of gliomas. Acta Neurol Scand 61(4):227–239
Wrensch M, Minn Y, Chew T, Bondy M, Berger MS (2002) Epidemiology of primary brain tumors: current concepts and review of the literature. Neuro Oncol 4(4):278–299
Sizoo EM, Braam L, Postma TJ, Pasman HR, Heimans JJ, Klein M, Reijneveld JC, Taphoorn MJ (2010) Symptoms and problems in the end-of-life phase of high-grade glioma patients. Neuro Oncol 12(11):1162–1166
Rudà R, Trevisan E, Soffietti R (2010) Epilepsy and brain tumors. Curr Opin Oncol 22(6):611–620
Beaumont A, Whittle IR (2000) The pathogenesis of tumour associated epilepsy. Acta Neurochir 142(1):1–15
Irlbacher K, Brandt SA, Meyer BU (2002) In vivo study indicating loss of intracortical inhibition in tumor-associated epilepsy. Ann Neurol 52(1):119–122
Lee JW, Wen PY, Hurwitz S, Black P, Kesari S, Drappatz J, Golby AJ, Wells WM 3rd, Warfield SK, Kikinis R, Bromfield EB (2010) Morphological characteristics of brain tumors causing seizures. Arch Neurol 67(3):336–342
Moots PL, Maciunas RJ, Eisert DR, Parker RA, Laporte K, Abou-Khalil B (1995) The course of seizure disorders in patients with malignant gliomas. Arch Neurol 52(7):717–724
Glantz MJ, Cole BF, Forsyth PA, Recht LD, Wen PY, Chamberlain MC, Grossman SA, Cairncross JG (2000) Practice parameter: anticonvulsant prophylaxis in patients with newly diagnosed brain tumors. Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 54(10):1886–1893
Glantz MJ, Cole BF, Friedberg MH, Lathi E, Choy H, Furie K, Akerley W, Wahlberg L, Lekos A, Louis S (1996) A randomized, blinded, placebo-controlled trial of divalproex sodium prophylaxis in adults with newly diagnosed brain tumors. Neurology 46(4):985–991
Van Breemen MS, Wilms EB, Vecht CJ (2007) Epilepsy in patients with brain tumours: epidemiology, mechanisms, and management. Lancet Neurol 6(5):421–430
Krouwer HG, Pallagi JL, Graves NM (2000) Management of seizures in brain tumor patients at the end of life. J Palliat Med 3(4):465–475
Oberndorfer S, Lindeck-Pozza E, Lahrmann H, Struhal W, Hitzenberger P, Grisold W (2008) The end of life hospital setting in patients with glioblastoma. J Palliat Med 11:26–30
Pace A, Di Lorenzo C, Guariglia L, Jandolo B, Carapella CM, Pompili A (2009) End of life issues in brain tumor patients. J Neurooncol 91(1):39–43
Panayiotopoulos CP (2012) The new ILAE report on terminology and concepts for the organization of epilepsies: critical review and contribution. Epilepsia 53(3):399–404
Tremont-Lukats IW, Ratilal BO, Armstrong T, Gilbert MR (2008) Antiepileptic drugs for preventing seizures in people with brain tumors. Cochrane Database Syst Rev 2:CD004424
Wick W, Menn O, Meisner C, Steinbach J, Hermisson M, Tatagiba M (2005) Pharmacotherapy of epileptic seizures in glioma patients: who, when, why and how long? Onkologie 28(8-9):391–396
Sirven JI, Wingerchuk DM, Drazkowski JF, Lyons MK, Zimmerman RS (2004) Seizure prophylaxis in patients with brain tumors: a meta-analysis. Mayo Clin Proc 79(12):1489–1494
Pace A, Di Lorenzo C, Capon A, Villani V, Benincasa D, Guariglia L, Salvati M, Brogna C, Mantini V, Mastromattei A, Pompili A (2012) Quality of care and rehospitalization rate in the last stage of disease in brain tumor patients assisted at home: a cost effectiveness study. J Palliat Med 15(2):225–227
Conflict of interest
All authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pace, A., Villani, V., Di Lorenzo, C. et al. Epilepsy in the end-of-life phase in patients with high-grade gliomas. J Neurooncol 111, 83–86 (2013). https://doi.org/10.1007/s11060-012-0993-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-012-0993-2