Abstract
The mechanism of tumorigenesis associated with nicotinamide adenine dinucleotide phosphate (NADP+)-dependent isocitrate dehydrogenase 1 (IDH1) mutations in gliomas is not fully understood. Loss of catalytic activity leading to a decrease in α-ketoglutarate (αKG) and gain of novel catalytic activity leading to production of d-2-hydroxylglutarate (d-2-HG) are both found in IDH1-mutated glioma cells. Both the decrease of αKG and accumulation of d-2-HG inhibit the activity of multiple dioxygenases including prolyl hydroxylase domain-2 (PHD2), collagen prolyl-4-hydroxylase, histone demethylases, and the ten–eleven translocation (TET) family of 5-methylcytosine hydroxylases. Here we correlated the products of these dioxygenases after IDH1 gene mutations with tumorigenesis in human astroglioma samples. DNA sequencing was carried out for 253 astroglioma samples to identify IDH1 mutations. Immunohistochemistry analysis was employed to verify the levels of endostatin, dimethylated H3k79 (H3k79me2), and 5-hydroxymethylcytosine (5hmC) in these astroglioma samples. IDH1 mutations occurred frequently in low grades of astrocytoma. One case bearing both IDH1 and IDH2 mutations was identified. IDH1-mutated cases displayed more frontal lobe location and p53-positive immunostaining than wild-type cases. IDH1 mutations were associated with increased histone methylation and decreased 5hmC. By inhibiting endostatin expression, IDH1 mutations indirectly promoted angiogenesis in gliomas. All these changes were same in astroglioma at different malignancy grade. IDH1 mutations showed wide regulation of angiogenesis and genome-wide change of histone and DNA methylation, which were not suppressed as the malignancy level progressed, suggesting an early role of IDH1 mutations in astrocytoma tumorigenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Somatic mutations of NADP+-dependent isocitrate dehydrogenase 1 (IDH1) are frequently observed in grade II-III gliomas, secondary glioblastomas, and acute myeloid leukemia (AML) [1–3]. IDH1 mutations have also been reported in colon and prostate cancers, though with much lower frequency [4]. All reported IDH1 mutations are heterozygous and result in amino acid substitutions at a single arginine residue (R132). Cytosolic IDH1 exists as a homodimer and catalyzes oxidative decarboxylation of isocitrate (ICT) to αKG [5]. Mutant IDH1 dominantly inhibits wild-type IDH1 and causes a nearly 50 % decrease in αKG concentration in cells expressing the IDH1R132H mutant [6]. Dang et al. [7] reported that IDH1R132 mutations observed in gliomas cause a gain of function, namely reduction of αKG to d-2-HG in an NADPH-dependent manner. This finding was later confirmed by Ward et al. [3], who reported that d-2-HG also accumulates in AML samples bearing IDH1R132 mutations. Accumulation of a different enantiomer, l-2-HG, in a rare metabolic disorder caused by a defect in l-2-HG dehydrogenase in mitochondria that results in psychomotor retardation, progressive ataxia, and leukodystrophy [8, 9] has been shown to have increased risk of developing brain tumors [10]. However, accumulation of d-2-HG, which is linked to d-2-hydroxyglutaric aciduria, has not been reported as associated with tumorigenesis [10]. Therefore, whether d-2-HG acts as an oncometabolite and how it exerts tumorigenicity have yet to be elucidated.
2-HG and αKG are two structurally similar molecules with the exception that the oxygen atom linked to C2 in αKG is replaced by a hydroxyl group in 2-HG. This similarity suggests the possibility that 2-HG may bind to and function as a competitive inhibitor of αKG-dependent dioxygenases. There are more than 60 dioxygenases whose activities are dependent on or affected by αKG [11–14]. Many of these enzymes have a K m for αKG, at near-physiological αKG concentrations, estimated at around 50 μM [6], making their activities particularly susceptible to αKG level fluctuation and αKG analog inhibition. Xu et al. [15] reported that 2-HG is a competitive inhibitor of multiple αKG dioxygenases, including the α-subunit collagen prolyl-4-hydroxylases (CP4H), histone demethylases, and the TET family 5-methylcytosine (5mC) hydroxylases.
The activity of collagen prolyl-4-hydroxylases (CP4H) is dependent on αKG [16]. Prolyl hydroxylation is required for biosynthesis of collagens, including production of endostatin, a 20-kDa secreted peptide derived from proteolytic cleavage of type XVIII collagen that has been implicated in inhibition of angiogenesis and tumor growth [17, 18]. JmjC domain-containing histone demethylases are another group of dioxygenases that require αKG, the demethylation being coupled to conversion of αKG to succinate [17]. A decrease in the activity of demethylases is expected to increase histone methylation. Mammalian genomes encode more than 30 JmjC domain-containing demethylases that fall into seven subfamilies [19], each of which recognize and remove methyl groups on distinct residues on different histones, including several that target specific methylation sites on histone H3. Increased H3K79 dimethylation (H3K79me2) was found in MLL-rearranged mouse leukemia and human AML patients, making it an interesting target for analysis since IDH1 mutations occur at high frequency in AML [3, 20].
Cytosine methylation near gene transcription start sites (TSSs) is critical for transcription silencing [21]. TET hydroxylases, a group of αKG-dependent dioxygenases, catalyze conversion of 5-methylcytosine (5mC) to 5-hydroxymethylcytosine (5hmC) [22], and their activity promotes the silencing effect of cytosine methylation.
To gain further insight into how IDH1 mutations promote tumorigenesis, we analyzed the IDH1 mutation ratio and the expression of the products of multiple dioxygenases, including CP4H, histone demethylases, and the TET family of 5mC hydroxylases, in a large number of Chinese astroglioma samples at different malignancy grades.
Materials and methods
Tumor specimens
Paraffin-embedded glioma samples collected from the Department of Neuropathology, Institute of Neurology, Affiliated Huashan Hospital of Fudan University were obtained with informed consent from patients. All tumor sections were reviewed by two independent neuropathologists and diagnosed according to World Health Organization (WHO) criteria. Tumors were generally classified into three subtypes: diffuse astrocytoma WHO grade II (A II, 61 cases), anaplastic astrocytoma WHO grade III (A III, 42 cases), and glioblastoma WHO grade IV (GBM, 150 cases). No oligodendrogliomas were included in our samples.
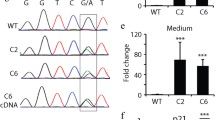
Direct DNA sequencing for IDH1 mutations
For DNA extraction, consecutive sections of paraffin-embedded samples were directly collected. Tissue samples were then deparaffinized using dimethylbenzene and washed with ethanol. Genomic DNA was isolated as previously described [26]. IDH1 and IDH2 mutations at R132 and R172, respectively, were assessed by bidirectional cycle sequencing of polymerase chain reaction (PCR)-amplified fragments. Primers used were IDH1-forward 5′-TGAGCTCTATATGCCATCACTGC-3′ and IDH1-reverse 5′-CAATTTCATACCTTGCTTAATGGG-3′, and IDH2-forward 5′-GTCTGGCTGTGTTGTTGCTTG-3′ and IDH2-reverse 5′-CAGAGACAAGAGGATGGCTAGG-3′, respectively. PCR reactions were performed in volume of 15 μl, containing 1× PCR buffer, 0.2 mM deoxynucleotide triphosphates (dNTPs), 1 mM of each primer, 6 % dimethyl sulfoxide (DMSO), 0.05 unit/ml platinum Taq (Invitrogen), and 3–10 ng DNA. A touchdown PCR program was used for PCR amplification. PCR conditions were as follows: 94 °C for 2 min; three cycles of 94 °C for 20 s, 64 °C for 15 s, 70 °C for 10 s; three cycles of 94 °C for 20 s, 61 °C for 15 s, 70 °C for 10 s; three cycles of 94 °C for 20 s, 58 °C for 15 s, 70 °C for 10 s; and 35 cycles of 94 °C for 20 s, 57 °C for 15 s, and 70 °C for 10 s, followed by 70 °C for 5 min. Sequencing was performed using the direct sequencing method (Invitrogen). Each sample was analyzed in both sense and antisense directions.
Immunohistochemistry (IHC)
IHC was performed on 5-μm-thick sections using a standard avidin–biotin–peroxidase technique with the labeled streptavidin biotin (LSAB) kit (Dako, CA). Briefly, deparaffinized sections were incubated with 3 % H2O2 to eliminate endogenous peroxidase activity for 30 min, followed by blocking with 5 % normal goat serum. Primary antibodies including anti-p53 (clone BP53-12, dilution 1:500; Sigma, USA), anti-endostatin (ab15685, dilution 1:200; Abcam, USA), anti-CD34 (dilution 1:100; Changdao, China), anti-dimethyl-histone H3K79me2 (ab46154, dilution 1:200; Abcam, USA), and anti-5-hydroxymethylcytosine (dilution 1:1,000; Active Motif, Carlsbad, CA) were incubated at 37 °C for 1 h. Phosphate-buffered saline (PBS) was used as negative control. Secondary antibody was then applied and incubated at 37 °C for 1 h; sections were developed with diaminobenzidine (DAB) kit and stopped with water.
Image analysis
To quantify the IHC-positive cells in glioma samples, five areas (173 μm2 each) were randomly selected from each sample and microscopically examined and analyzed by an experienced neuropathologist. Images were captured using a charge-coupled device (CCD) camera and analyzed using Motic Images advanced software (version 3.2; Motic China Group Co. Ltd.). Cells showing either positive cytoplasmic or nuclear signals (brown) were counted as positive signal and located automatically, while negative cells showed either no signal or weak signal close to background. The positive percentage of each field was obtained by dividing the positive area by the total area.
Tumor blood vessel density was determined by calculating the area of tumor vessels (μm2) per high-power field (173 μm2) in sections stained with antibodies against CD34 from five highly vascularized areas.
IHC statistics
All values were calculated as mean ± standard deviation (SD). Statistical analysis was performed with using SPSS 11.5. Statistical methods included one-way analysis of variance (ANOVA) test, Tukey–Kramer multiple-comparison test, and Pearson’s χ 2 test. Linear correlation analysis was used to examine the relation of nominal variables referring to absence or presence of genetic alterations within distinct tumor groups.
Results
IDH1 mutations in Chinese astroglioma samples
Among 253 astroglioma samples, 106 were detected to hold IDH1 mutations (Supplementary Table 1). All mutant samples bore heterozygous R132H (CGT → CAT) mutations. Notably, one case was found to have IDH1 and IDH2 mutations simultaneously. The IDH2 mutation in this case was a heterozygous R172K (AGG → AAG) mutation. IDH1 mutations were more frequent in low-grade diffuse astrocytoma (78.7 %) and anaplastic astrocytomas (66.7 %), while in glioblastoma their occurrence was significantly lower (20 %) (Table 1). GBM patients with IDH1 mutations averaged 40.56 ± 14.85 years old and were significantly younger than GBM patients without IDH1 mutations, who averaged 51.33 ± 13.74 years old (P < 0.01) (Table 2). However, no differences were observed among the ages of patients suffering from diffuse astroglioma (WHO grade II) and anaplastic astroglioma (WHO grade III) with or without IDH1 mutations. IHC results also showed that the p53-positive immunostaining rate in glioma samples bearing IDH1 mutations was significantly higher (73/106, 68.87 %) than those having wild-type enzymes (71/147, 48.29 %, P < 0.01) (Table 2). Pathological analysis showed that samples bearing IDH1 mutations were more frequently found in the frontal lobe (57/106, 55.37 %), while this location preference was not found in gliomas with wild-type IDH1, suggesting a previously unreported, yet interesting, feature for IDH1 mutations in gliomas (Table 2). The location of the tumors was determined by preoperative magnetic resonance imaging (MRI). The sample with both IDH1 and IDH2 mutations corresponded to a 38-year-old male with diagnosis of diffuse astrocytoma, WHO grade II, located in the left front lobe (Supplementary Table 1).
Primary glioma samples with IDH1 mutations have decreased endostatin levels
Parenchyma of normal brain showed very low endostatin immunoreactivity. In glioma tissue, endostatin was detected both in the cytoplasm with a homogeneous labeling pattern and in the extracellular matrix with a dot-like pattern. In gliomas with no IDH1 mutations, expression of endostatin showed a positive correlation with malignant astrocytoma grades (P = 0.001, correlation coefficient, r = 0.391), while in gliomas bearing IDH1 mutations, expression of endostatin showed no difference among malignant grades (P = 0.127, correlation coefficient, r = −0.180). However, the overall positive expression of endostatin in glioma samples bearing IDH1 mutations was significantly decreased when compared with those without IDH1 mutations at the same malignancy grade (P < 0.05) (Fig. 1a–c). These results show that IDH1 mutations directly lead to a decrease in the levels of endostatin in primary glioma samples.
IDH1-mutation-bearing glioma samples have decreased endostatin levels and elevated angiogenesis. a, b. Representative endostatin staining in glioma samples without (a) or with (b) IDH1 mutations at the same malignancy grades. c IDH1 mutation inhibited endostatin generation. Endostatin levels in glioma samples of different malignancy grades and with or without IDH1 mutation were quantified and compared. d, e Representative CD34 staining in glioma samples without (d) or with (e) IDH1 mutations at the same malignancy grades. f. IDH1-mutated gliomas have elevated angiogenesis. Intensity of CD34 staining in glioma samples of different malignancy grades and with or without IDH1 mutation was quantified and compared. Tumors for IHC included: diffuse astrocytoma WHO grade II (A II, 61 cases), anaplastic astrocytoma WHO grade III (A III, 42 cases), and glioblastomas WHO grade IV (GBM, 150 cases). Mean ± standard error of mean (SEM) is shown, *P < 0.05. One-way ANOVA test and further Tukey–Kramer multiple-comparison test were used for statistical analysis
Activated angiogenesis is observed in primary glioma samples with IDH1 mutations
Given that decreased endostatin would contribute to enhanced angiogenesis [17], we further wanted to confirm the difference in tumor blood vessel density between the IDH1 wild-type and mutated groups at different malignancy grades. When blood vessels were stained with an anti-CD34 antibody, we observed that blood vessel density (expressed as vessels/field) positively correlated with glioma malignancy regardless of IDH1 mutation status (IDH1-mutated cases: P = 0.000, correlation coefficient, r = 0.531; IDH1 wild-type cases: P = 0.000, correlation coefficient, r = 0.285), consistent with the reported positive correlation between angiogenesis and glioma grade [24]. However, vessel density in the IDH1-mutated samples was significantly higher than in IDH1 wild-type cases at the same malignancy grade (P < 0.05, Fig. 1d–f).
The correlation between endostatin expression and tumor blood vessel density was negative in glioma tissues (P = 0.045, correlation coefficient, r = −0.224), especially in IDH1-mutated grade IV gliomas (P = 0.013, correlation coefficient, r = −0.559). In contrast, wild-type cases showed no correlation between endostatin and tumor blood vessel density (P = 0.627, correlation coefficient, r = −0.058). These results indicate that IDH1 gene mutations alter the expression of endostatin and further influence blood vessel density in astrogliomas.
H3K79me2 levels are elevated in primary glioma samples with IDH1 mutations
Histone demethylases are also αKG-dependent dioxygenases. Since changes in histone methylation levels have direct, broad impact in gene transcription and contribute to tumorigenesis, it is important to find out whether gliomas harboring IDH1 mutations have changes in histone demethylation. An anti-H3K79me2 antibody detected different methylation levels in samples with and without IDH1 mutations, with average H3K79me2 histone levels of IDH1-mutated samples being significantly higher (P < 0.05). However, no positive correlation was found between H3K79me2 levels and malignant grades, either among samples bearing IDH1 mutations or among those with wild-type IDH1 (Fig. 2a–c). These results suggest that H3K79me2 levels in glioma cells are solely determined by IDH1 gene mutation status rather than by malignancy grades.
Elevated H3K9me2 levels and decreased 5hmC levels in IDH1-mutation-bearing gliomas. a, b Representative H3K9me2 staining in glioma samples with (a) or without (b) IDH1 mutations. c IDH1-mutated gliomas have elevated H3K9me2 levels. H3K9me2 levels in glioma samples of different malignancy grades and with or without IDH1 mutation were quantified and compared. d, e Representative 5hmC staining in glioma samples with or without IDH1 mutations. f IDH1-mutated gliomas have decreased 5hmC level. 5hmC levels in glioma samples of different malignancy grades and with or without IDH1 mutations were quantified and compared. Tumors for IHC included: diffuse astrocytoma WHO grade II (A II, 61 cases), anaplastic astrocytoma WHO grade III (A III, 42 cases), and glioblastoma WHO grade IV (GBM, 150 cases). Mean ± SEM is shown, *P < 0.05. One-way ANOVA test and further Tukey–Kramer multiple-comparison test were used for statistical analysis
5hmC levels are decreased in primary glioma samples with IDH1 mutations
We also found that, in the absence of IDH1 gene mutations, expression of 5hmC was similar among astrogliomas at different malignancy grades. Glioma samples harboring mutant IDH1 displayed significantly lower levels of 5hmC compared with those containing wild-type IDH1 (P < 0.05, Fig. 2d–f). These results provide in vivo evidence that IDH1 mutations directly reduce the levels of 5hmC.
Discussion
Similarly to other sequencing reports, we found a high frequency of IDH1 mutations in low-grade diffuse astrocytoma (78.7 %) and anaplastic astrocytoma (66.7 %), while in glioblastoma the occurrence was significantly lower (20 %). Furthermore, we also found that both IDH1 and IDH2 can coexist in the same patient. According to Parsons et al. [1] and Balss et al. [22], NADP+ IDH1 mutations can be used as a molecular marker for secondary GBM. Therefore, even though there was no clinical evidence indicated preexistence of a less malignant precursor lesion, NADP+ IDH1-mutated GBM in our experiment could be diagnosed as secondary GBM.
We also found that those cases with IDH1 mutations were more frontal lobe located, which is in accordance with Lai et al. [23]. Also, IDH1-mutated cases showed higher p53 immunopositivity, consistent with the previous sequencing finding that TP53 gene mutations were closely associated with IDH1 mutations [2].
Two distinct outcomes arise from IDH1 mutations: a decrease of αKG and an accumulation of d-2-HG [6]. Although Dang et al. [7] found that αKG was not decreased in IDH1 mutant tumors, Xu et al. [15] described that IDH1 mutations are capable of inhibiting dioxygenases, and this effect, since 2-HG and αKG are structurally similar, may be due to 2-HG binding to and functioning as a competitive inhibitor of αKG-dependent dioxygenases. These results integrate the loss of function model previously proposed by Zhao et al. [6] with the gain of catalytic function model proposed by Dang et al. [7].
Angiogenesis is recognized as a key event in the natural progression of gliomas. Neovascularization in brain tumors correlates directly with their biological aggressiveness, degree of malignancy, and clinical recurrence, and inversely with the postoperative survival of patients with gliomas [24]. In this study, we confirmed that an angiogenic-related factor, endostatin, was changed to a state that facilitates angiogenesis in IDH1-mutated cases. Our results showed that, in IDH1 wild-type cases, the levels of endostatin had a positive correlation with malignancy grade, which confirms previous observations [25]. On the contrary, in IDH1-mutated cases, no differences were observed among different malignancy grades. Comparing cases with the same malignancy grade, endostatin expression was lower in the IDH1-mutated cases than in the IDH1 wild-type cases, from astroglioma malignant grade II to grade IV. These results indicate that IDH1 gene mutations inhibited expression of endostatin and that high malignancy levels would not eliminate this effect. This makes pathological sense, because endostatin is only dependent on the degree of inhibition of CP4H, i.e., on the degree of decrease of αKG and accumulation of d-2-HG caused by IDH1 mutations, but not dependent on malignancy grade. Despite the fact that a variety of factors might influence expression of endostatin, in this work we verified that IDH1 mutations could inhibit its expression, which may facilitate angiogenesis in IDH1-mutated cases. For IDH1 wild-type cases, other factors such as extracellular matrix degradation may indirectly modulate levels of endostatin in tumor tissues. Also, angiogenesis is regulated by the highly coordinated function of various proteins with pro- and antiangiogenic functions. Proangiogenic factors include vascular endothelial growth factor (VEGF), fibroblast growth factor, platelet-derived growth factor, insulin-like growth factor, transforming growth factor, angiopoietins, and several chemokines, while antiangiogenic factors include thrombospondin-1, angiostatin, and endostatin [26]. Therefore, the mechanisms that determine blood vessel density in tumors may be complicated. IDH1 mutations were just partly involved in angiogenesis in astroglioma.
H3K79 methylation levels were significantly increased in IDH1-mutated cases compared with wild-type IDH1 cases and did not differ among malignancy grades in cases either with or without IDH1 mutations. The decrease of 5hmC expression was also solely determined by the NADP+ IDH1 status without any correlation with tumor malignancy. IDH1 gene mutations were therefore involved in the epigenetic regulation of histone methylation, which might further play an important role in controlling the expression of genetic information through transcriptional changes [25].
The mammalian genome is methylated predominantly at the C5 position of cytosine bases within CpG dinucleotides [27, 28]. 5mCs, especially when clustered, are important transcriptional silencers at gene promoters and endogenous retrotransposons in the genome [29]. Cytosine methylation is catalyzed by a family of DNA methyltransferases (DNMTs) [30]. 5hmC has been hypothesized as a potential intermediate for active DNA demethylation, and TET1 plays an important role through conversion of 5mC into 5hmC, which may further promote active DNA demethylation in mammalian cells. Here, we showed that IDH1 mutations are involved in the molecular mechanism underlying dynamic changes of DNA methylation in astroglioma. As DNA methylation plays an important role in tissue-specific gene expression, X chromosome inactivation, genomic imprinting, and nuclear reprogramming [31, 32], we hypothesized that, by influencing DNA methylation levels, IDH1 mutations also play critical roles in gene expression in astroglioma.
Overall, our results show that IDH1 mutation occurred frequently in low grades of astrocytomas. IDH1-mutated cases were more frontal lobe located and p53 positive than IDH1 wild-type cases. The finding that the influence of IDH mutations is wide is particular exciting for us. By inhibiting endostatin expression, IDH1 mutations could indirectly promote angiogenesis in glioma. IDH1 mutations could also influence the epigenetic regulation of both histone and DNA methylation, which were not suppressed as the malignancy level progressed, suggesting an early role of IDH1 mutations in astrocytoma tumorigenesis.
References
Parsons DW, Jones S, Zhang X, Lin JC, Leary RJ, Angenendt P, Mankoo P, Carter H, Siu IM, Gallia GL, Olivi A, McLendon R, Rasheed BA, Keir S, Nikolskaya T, Nikolsky Y, Busam DA, Tekleab H, Diaz LA Jr, Hartigan J, Smith DR, Strausberg RL, Marie SK, Shinjo SM, Yan H, Riggins GJ, Bigner DD, Karchin R, Papadopoulos N, Parmigiani G, Vogelstein B, Velculescu VE, Kinzler KW (2008) An integrated genomic analysis of human glioblastoma multiforme. Science 321:1807–1812. doi:10.1126
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, Kos I, Batinic-Haberle I, Jones S, Riggins GJ, Friedman H, Friedman A, Reardon D, Herndon J, Kinzler KW, Velculescu VE, Vogelstein B, Bigner DD (2009) IDH1 and IDH2 mutations in gliomas. N Engl J Med 360:765–773. doi:10.1056/NEJMoa0808710
Ward PS, Patel J, Wise DR, Abdel-Wahab O, Bennett BD, Coller HA, Cross JR, Fantin VR, Hedvat CV, Perl AE, Rabinowitz JD, Carroll M, Su SM, Sharp KA, Levine RL, Thompson CB (2010) The common feature of leukemia-associated IDH1 and IDH2 mutations is a neomorphic enzyme activity converting alpha-ketoglutarate to 2-hydroxyglutarate. Cancer Cell 17:225–234. doi:10.1016/jccr201001020
Kang MR, Kim MS, Oh JE, Kim YR, Song SY, Seo SI, Lee JY, Yoo NJ, Lee SH (2009) Mutational analysis of IDH1 codon 132 in glioblastomas and other common cancers. Int J Cancer 125:353–355. doi:10.1002/ijc.24379
Hartong DT, Dange M, McGee TL, Berson EL, Dryja TP, Colman RF (2008) Insights from retinitis pigmentosa into the roles of isocitrate dehydrogenases in the Krebs cycle. Nat Genet 40:1230–1234. doi:10.1038/ng.223
Zhao S, Lin Y, Xu W, Jiang W, Zha Z, Wang P, Yu W, Li Z, Gong L, Peng Y, Ding J, Lei Q, Guan KL, Xiong Y (2009) Glioma-derived mutations in IDH1 dominantly inhibit IDH1 catalytic activity and induce HIF-1alpha. Science 324:261–265. doi:10.1126/science.1170944
Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM, Fantin VR, Jang HG, Jin S, Keenan MC, Marks KM, Prins RM, Ward PS, Yen KE, Liau LM, Rabinowitz JD, Cantley LC, Thompson CB, Vander Heiden MG, Su SM (2009) Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature 462:739–744. doi:10.1038/nature08617
Rzem R, Veiga-da-Cunha M, Noël G, Goffette S, Nassogne MC, Tabarki B, Schöller C, Marquardt T, Vikkula M, Van Schaftingen E (2004) A gene encoding a putative FAD-dependent L-2-hydroxyglutarate dehydrogenase is mutated in L-2-hydroxyglutaric aciduria. Proc Natl Acad Sci U S A 101:16849–16854. doi:10.1073/pnas.0404840101
Topçu M, Jobard F, Halliez S, Coskun T, Yalçinkayal C, Gerceker FO, Wanders RJ, Prud’homme JF, Lathrop M, Ozguc M, Fischer J (2004) L-2-Hydroxyglutaric aciduria: identification of a mutant gene C14orf160, localized on chromosome 14q22.1. Hum Mol Genet 13:2803–2811. doi:10.1093/hmg/ddh300
Aghili M, Zahedi F, Rafiee E (2009) Hydroxyglutaric aciduria and malignant brain tumor: a case report and literature review. J Neurooncol 91:233–236. doi:10.1007/s11060-008-9706-2
Annunen P, Helaakoski T, Myllyharju J, Veijola J, Pihlajaniemi T, Kivirikko KI (1997) Cloning of the human prolyl 4-hydroxylase alpha subunit isoform alpha(II) and characterization of the type II enzyme tetramer. The alpha(I) and alpha(II) subunits do not form a mixed alpha(I)alpha(II) beta2 tetramer. J Biol Chem 272:17342–17348. doi:10.1074/jbc.272.28.17342
Falnes PØ, Johansen RF, Seeberg E (2002) AlkB-mediated oxidative demethylation reverses DNA damage in Escherichia coli. Nature 419:178–182. doi:10.1038/nature01048
Hirsilä M, Koivunen P, Günzler V, Kivirikko KI, Myllyharju J (2003) Characterization of the human prolyl 4-hydroxylases that modify the hypoxia-inducible factor. J Biol Chem 278:30772–30780. doi:10.1074/jbc.M304982200
Hirsilä M, Koivunen P, Günzler V, Kivirikko KI, Myllyharju J (2004) Catalytic properties of the asparaginyl hydroxylase (FIH) in the oxygen sensing pathway are distinct from those of its prolyl 4-hydroxylases. J Biol Chem 279:9899–9904. doi:10.1074/jbc.M312254200
Xu W, Yang H, Liu Y, Yang Y, Wang P, Kim SH, Ito S, Yang C, Wang P, Xiao MT, Liu LX, Jiang WQ, Liu J, Zhang JY, Wang B, Frye S, Zhang Y, Xu YH, Lei QY, Guan KL, Zhao SM, Xiong Y (2011) Oncometabolite 2-hydroxyglutarate is a competitive inhibitor of α-ketoglutarate-dependent dioxygenases. Cancer Cell 19:17–30. doi:10.1016/j.ccr.2010.12.014
Kivirikko KI, Myllylä R, Pihlajaniemi T (1989) Protein hydroxylation: prolyl 4-hydroxylase, an enzyme with four cosubstrates and a multifunctional subunit. FASEB J 3:1609–1617. doi:10.1074/jbc.M312254200
O’Reilly MS, Boehm T, Shing Y, Fukai N, Vasios G, Lane WS, Flynn E, Birkhead JR, Olsen BR, Folkman J (1997) Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell 88:277–285. doi:S0092-8674(00)81848-6
Krane SM (2008) The importance of proline residues in the structure, stability and susceptibility to proteolytic degradation of collagens. Amino Acids 35:703–710. doi:10.1007/s00726-008-0073-2
Klose RJ, Kallin EM, Zhang Y (2006) JmjC-domain-containing proteins and histone demethylation. Nat Rev Genet 7:715–727. doi:10.1038/nrg1945
Krivtsov AV, Feng Z, Lemieux ME, Faber J, Vempati S, Sinha AU, Xia X, Jesneck J, Bracken AP, Silverman LB, Kutok JL, Kung AL, Armstrong SA (2008) H3K79 methylation profiles define murine and human MLL-AF4 leukemias. Cancer Cell 14:355–368. doi:10.1016/j.ccr.2008.10.001
Suzuki MM, Bird A (2008) DNA methylation landscapes: provocative insights from epigenomics. Nat Rev Genet 9:465–476. doi:10.1038/nrg2341
Balss J, Meyer J, Mueller W, Korshunov A, Hartmann C, von Deimling A (2008) Analysis of the IDH1 codon 132 mutation in brain tumors. Acta Neuropathol 116:597–602. doi:10.1007/s00401-008-0455-2
Lai A, Kharbanda S, Pope WB, Tran A, Solis OE, Peale F, Forrest WF, Pujara K, Carrillo JA, Pandita A, Ellingson BM, Bowers CW, Soriano RH, Schmidt NO, Mohan S, Yong WH, Seshagiri S, Modrusan Z, Jiang Z, Aldape KD, Mischel PS, Liau LM, Escovedo CJ, Chen W, Nghiemphu PL, James CD, Prados MD, Westphal M, Lamszus K, Cloughesy T, Phillips HS (2011) Evidence for sequenced molecular evolution of IDH1 mutant glioblastoma from a distinct cell of origin. J Clin Oncol 29:4482–4490
Fischer I, Gagner JP, Law M, Newcomb EW, Zagzag D (2005) Angiogenesis in gliomas: biology and molecular pathophysiology. Brain Pathol 15:297–310
Morimoto T, Aoyagi M, Tamaki M, Yoshino Y, Hori H, Duan L, Yano T, Shibata M, Ohno K, Hirakawa K, Yamaguchi N (2002) Increased levels of tissue endostatin in human malignant gliomas. Clin Cancer Res 8:2933–2938 http://clincancerres.aacrjournals.org/content/8/9/2933.long
Sakurai T, Kudo M (2011) Signaling pathways governing tumor angiogenesis. Oncology 81:24–29. doi:10.1159/000333256
Bernstein BE, Mikkelsen TS, Xie X, Kamal M, Huebert DJ, Cuff J, Fry B, Meissner A, Wernig M, Plath K, Jaenisch R, Wagschal A, Feil R, Schreiber SL, Lander ES (2006) A bivalent chromatin structure marks key developemtal genes in embryonic stem cells. Cell 125:315–326. doi:10.1016/j.cell.2006.02.041
Zhu JK, Active DNA (2009) Demethylation mediated by DNA glucosylases. Annu Rev Genet 43:143–166. doi:10.1146/annurev-genet-102108-134205
Jaenisch R, Bird A (2003) Epigenetic regulation of gene expression: how the genome intergrates intrinsic and environmental signals. Nat Genet suppl 33:245–254. http://dx.doi.org/10.1038/ng1089
Ooi SK, Bestor TH (2008) The colorful history of active DNA demethylation. Cell 133:1145–1148. doi:10.1016/j.cell.2008.06.009
Bonasio R, Tu S, Reinberg D (2010) Molecular dignals of epigenetic states. Science 330:612–616. doi:10.1126/science.1191078
Feng J, Fan G (2009) The roles of DNA methylation in the central nervous system and neuropsychiatric disorders. Int Rev Neurobiol 89:67–84. doi:10.1016/S0074-7742(09)89004-1
Acknowledgments
We thank Professor Xue Xiong for critical suggestions on the manuscript. This work was support by Chinese National Science Foundation grants (30500189), Shanghai Nature Science Foundation Grants (12ZR1403200).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, Y., Jiang, W., Liu, J. et al. IDH1 mutations inhibit multiple α-ketoglutarate-dependent dioxygenase activities in astroglioma. J Neurooncol 109, 253–260 (2012). https://doi.org/10.1007/s11060-012-0914-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-012-0914-4