Abstract
To determine the safety, tolerability, and report on secondary efficacy endpoints of motexafin gadolinium (MGd) in combination with whole-brain radiotherapy (WBRT) and stereotactic radiosurgery (SRS) for patients with ≤6 brain metastases. We conducted an international study of WBRT (37.5 Gy in 15 fractions) and SRS (15–21 Gy) with the addition of MGd (5 mg/kg preceding each fraction beginning week 2). The primary endpoint was to evaluate the rate of irreversible grade 3 or any grade ≥4 neurotoxicity and establish feasibility in preparation for a phase III trial. Sixty-five patients were enrolled from 14 institutions, of which 45 (69%) received SRS with MGd as intended and were available for evaluation. Grade ≥3 neurotoxicity attributable to radiation therapy within 3 months of SRS was seen in 2 patients (4.4%), including generalized weakness and radionecrosis requiring surgical management. Immediately following the course of MGd plus WBRT, new brain metastases were detected in 11 patients (24.4%) at the time of the SRS treatment planning MRI. The actuarial incidence of neurologic progression at 6 months and 1 year was 17 and 20%, respectively. The median investigator-determined neurologic progression free survival and overall survival times were 8 (95% CI: 5–14) and 9 months (95% CI: 6–not reached), respectively. We observed a low rate of neurotoxicity, demonstrating that the addition of MGd does not increase the incidence or severity of neurologic complications from WBRT with SRS boost.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain metastases represent the most common intracranial tumor in adults, occurring in approximately 25% of those with a cancer diagnosis. Primary tumors of the lung, breast, melanoma, and kidney demonstrate a strong predilection for dissemination to the brain. Intracranial metastatic disease is a major source of morbidity, neurocognitive decline, loss of functional independence, and mortality in these patients. The median survival with best supportive care only is approximately two months [1, 2].
Whole brain radiation therapy (WBRT) improves survival to approximately four months and is a commonly employed therapeutic strategy [3]. The addition of a stereotactic radiosurgery (SRS) boost has been shown to improve overall survival for patients with a single metastasis, although post-hoc subset analysis of the landmark RTOG trial was suggestive of improved survival in selected patients with up to three intracranial lesions. It also improves local control and functional autonomy, while decreasing steroid dependence in those with multiple brain metastases [4, 5]. Emerging, but controversial data suggest that the clinical benefits of SRS (other than survival) might extend to patients with 4 or more metastases; in these studies of patients with multiple lesions treated with SRS, the treatment volume appears to be more important than the absolute number of brain metastases [6].
Motexafin gadolinium (MGd) is an expanded metalloporphyrin that is active in intracellular redox cycling, and is also a specific inhibitor of ribonucleotide reductase (RNR), which is overexpressed in several malignancies, as a promoter of enhanced DNA synthesis [7]. MGd generates reactive oxygen species by catalyzing the oxidation of reducing metabolites, the primary target of which appears to be thioredoxin reductase and metallothioneins, both involved in repairing radiation-induced DNA damage [8, 9]. The resultant oxidative stress allows MGd to enhance the cytotoxicity of both ionizing radiation and chemotherapy. In addition, it may also be directly cytotoxic to tumor cells [10–15]. Its specific inhibitory effect on RNR is putatively one of the mechanisms for this direct cytotoxicity. The iron-dependent enzyme RNR, controls cellular concentrations of deoxyribonucleotides, and is therefore essential for DNA synthesis. It is absolutely essential for cell proliferation since the enzyme catalyses the de novo synthesis of deoxyribonucleotides. In lung cancer patients, the level of RNR is directly associated with response to gemcitabine and cisplatin [16].
MGd is preferentially taken up by malignant cells and, given its paramagnetic properties, has been shown to localize in tumors using magnetic resonance imaging (MRI) [17, 18]. A recent phase III trial demonstrated that MGd in combination with WBRT, when initiated within 28 days of the diagnosis of brain metastases, improves the interval to neurologic progression from 8 to 24 months in patients with non-small cell lung cancer [19].
The primary purpose of the current study, PCYC-0224, was to determine the safety, tolerability, and measure secondary efficacy endpoints of MGd in combination with WBRT followed by a SRS boost for patients with up to six brain metastases (although at entry, the cut-off was 4 metastases; see below for details); the exploratory objective was to evaluate feasibility in preparation for a potential phase III trial.
Patients and methods
Patients
Adult patients with a Karnofsky performance status ≥70, irrespective of dexamethasone use, and histologically confirmed malignancy with one to four brain metastases as determined by diagnostic gadolinium contrast-enhanced MRI were eligible for enrollment. The maximum tumor diameter was ≤4 cm for a solitary metastasis. In the presence of multiple lesions the maximum diameter could not exceed 3 cm. Institutional review board approval was obtained from each participating center and written informed consent from all patients in accordance with the Helsinki Declaration was required [20].
Patients who underwent resection were eligible for the study, provided that residual intracranial metastases met entry criteria. Patients were excluded if they underwent complete resection of all known brain metastases, received previous cranial radiation, had leptomeningeal or liver metastases, had clinical or radiologic evidence of progressive disease within 1 month prior to enrollment, had metastases involving the midbrain, pons, or medulla or within 10 mm of the optic apparatus. Patients with a history of porphyria, glucose-6-phosphate-dehydrogenase (G6PD) deficiency, HIV infection, or uncontrolled hypertension (defined as >160/110 on maximum medical therapy) were also excluded. Minimal laboratory requirements included: lactate dehydrogenase (LDH) <1.3 times the upper limit of normal, platelets >50,000/mm3, creatinine <2.0 mg/dl, absolute neutrophil count (ANC) >1,500/mm3, AST and ALT less than three times the upper limit of normal, and total bilirubin less than two times the upper limit of normal.
Treatment
WBRT was delivered to a total dose of 37.5 Gy in 15 once daily fractions of 2.5 Gy over 3 weeks, prescribed to midplane using opposed lateral fields and 4–8 MV photons. Alternate fractionation schedules or concurrent chemotherapy were not permitted. Patients received MGd 5 mg/kg IV infused over approximately 10–30 min once a day 2–5 h before each WBRT fraction for 10 days during weeks 2 and 3 of WBRT treatment. In addition, MGd 5 mg/kg was administered once during week 4 or 5, a minimum of 2–5 h before the SRS boost.
SRS was delivered within 14 days after completion of WBRT. A post-WBRT, pre-SRS contrast-enhanced MRI was obtained for SRS target volume delineation and isocenter determination. If more than 4 days had elapsed since the last dose of MGd, an additional dose of MGd was given before treatment-planning MRI. If obtained on the day of SRS, treatment-planning MRI was obtained after the infusion of the final dose of MGd. Radiosurgery was permitted for up to 6 lesions that met eligibility criteria, in the event that additional lesions were discovered at the time of SRS planning. Metastases demonstrating complete radiologic response were not targeted for radiosurgical boost. The total dose for single fraction SRS was determined by tumor diameter. Lesions ≤2.0 cm received 21 Gy; lesions 2.1–3.0 cm received 18 Gy, while those 3.1–4.0 cm received 15 Gy [21]. The dose was prescribed to the 50–90% isodose line that encompassed the target volume. The target volume was defined as the enhancing portion of the metastatic lesion, without volumetric expansion. The brainstem and optic chiasm/nerves could not exceed 15, and 8 Gy, respectively. The heterogeneity index (defined as the maximum dose/prescribed dose) was recommended ≤2, and could not exceed 2.5 for any lesion. The preferred conformality index (defined as the prescribed isodose volume/target volume) was between 1.0 and 2.0, but could not exceed 3.5. A central reviewer performed the final review of the SRS boost treatment for each patient.
Assessments
The primary endpoint was the rate of irreversible grade 3 or any grade ≥4 clinical (not radiographic only) neurotoxicity attributable to radiation occurring within three months of SRS boost. Secondary endpoints included the interval to neurologic progression, the interval to neurocognitive progression, survival, and change in lesion size and number between screening MRI and SRS treatment-planning MRI. The feasibility endpoint was observational, to determine the proportion of patients proceeding to SRS after enrollment, in other words, to assess the “drop-out” rate, in order to plan for future statistical powering of a Phase III trial. Predetermined exploratory endpoints included the interval to radiologic progression and radiologic response rate at three months. All patients who did not receive any MGd or did not receive MGd and SRS on the same day were discontinued from the study and were not evaluable. All toxicities in this trial were scored according to version 3.0 of the National Cancer Institute Common Toxicity Criteria Adverse Events (NCI CTCAE).
Patients were evaluated at the time of study entry, monthly for 9 months, then every three months thereafter. Follow-up concluded six months after the last patient was enrolled. Each follow-up visit included a thorough neurologic examination, with assessment of alertness, orientation, language, speech, cranial nerves, motor strength, sensory deficits, and cerebellar function. Formal cognitive testing using a previously developed test-battery was also performed before enrollment, within 14 days of WBRT completion, and at each follow-up visit employing standardized psychometric instruments for assessing cognitive functions affected by brain tumors and treatment, including the Hopkins’ Verbal Learning (HVLT) test for memory, Controlled Oral Word Association (COWA) for executive function, Trail Making Test (TMT) Part A for visual motor speed, and Trail Making Test (TMT) Part B for executive function. Neurocognitive progression was defined as a worsening of 2.0 or more in the z-scores from baseline neurocognitive assessment for each individual instrument. Radiologic progression, which was defined as the occurrence of new metastases, reappearance of old lesions, or an increase in the sum of lesion sizes by >25%, was assessed by post-treatment MRI at 3 months and every 3 months thereafter. Radiologic response was defined as a decrease in the size of all lesions by at least 50%, without the occurrence of new lesions.
The treating physician determined neurologic progression for all patients. Neurologic events were considered as either major or minor. Major criteria are findings that by themselves are most specific for acute deterioration caused by progressive brain tumors without further confirmation, including change in level of consciousness, aphasia/dysphasia, paralysis, new visual field defect, ataxia, and decline in executive function. The minor criteria are findings suggestive of tumor progression, but insufficient in isolation to make the diagnosis. These included change in orientation or motor strength, loss of sensation in a limb, facial weakness, abnormal papillary light reflex, dysarthria, papilledema, oculomotor palsy, impaired cerebellar function, decline in neurocognitive function, or new onset seizures. Any combination of 3 minor criteria were considered neurologic progression if they could subsequently be confirmed. Alterations in steroid dosing, unless initiated in response to either major or minor neurologic events, were not considered as evidence of progressive disease. Patients with evidence of neurologic, neurocognitive, or radiologic progression returned 2–3 weeks later for a confirmatory visit. If death occurred before the confirmatory visit, the patient was considered to have experienced death with neurologic progression.
Statistical methods
As an a priori designation, >40% was reported as an unacceptable rate of radiation toxicity, with an incidence of 10–20% designated as acceptable at the time of protocol design [21]. A sample size of 45 provides an approximately 80% probability that the 95% binomial confidence interval for the primary endpoint will fall below 40%. This calculation is based on a true neurologic toxicity rate of 20% and allows for a 10% non-evaluable rate. The time to neurologic progression, neurocognitive progression, radiologic progression and overall survival are plotted using the Kaplan–Meier method. With the exception of overall survival, all analyses censored patients for non-neurologic deaths.
Results
Patient characteristics
Sixty-five patients were enrolled between June 2005 and September 2006 from 14 institutions, including sites in the United States (n = 35, 53.8%) and Canada (n = 30, 46.2%). Patients who did not receive SRS boost (13 patients, 20%: 6 decline in health/disease progression, 4 patient refusal, 2 no longer SRS candidates, and 1 poor target delineation) or MGd on the day of SRS boost (7 patients, 11%: 5 patient/physician preference, 2 patient refusal) were excluded from the analysis, leaving 45 patients (69%) available for evaluation. These parameters for non-evaluability were pre-specified. Patient characteristics for evaluable patients are outlined in Table 1. The most common primary tumor site was lung (76%), followed by breast (11%), melanoma (7%), colorectal (4%), and renal (2%). Most patients were RTOG recursive partitioning analysis (RPA) class II (84.4%), which encompasses patients with uncontrolled primary tumors, age ≥65 years, or with extracranial metastases. The remaining (15.6%) were RPA class I, indicating KPS ≥70, primary site controlled, age <65 years, and no extracranial metastases [22]. The majority of patients (n = 37, 82%) demonstrated neurologic symptoms at the time of diagnosis of brain metastasis, while the remainder were detected by routine imaging for staging or restaging (n = 8, 18%). Sixty-three percent of evaluable patients had 1 or more sites of extra-cranial metastases.
The characteristics of treated brain metastases are listed in Table 2. The median number of brain metastases treated with SRS boost was 2, with 15 patients (33.3%) receiving treatment to 1 lesion, 16 patients (35.6%) to 2 lesions, 4 patients (8.9%) to 3 lesions, 6 patients (13.3%) to 4 lesions, 3 (6.7%) patients to 5 lesions, and 1 (2.2%) patient to 6 lesions. The total area of brain metastases treated with SRS, measured at the point of greatest cross-sectional diameter, ranged from 0.4 to 110.1 cm2, with a median of 3.3 cm2.
Treatment characteristics
The median time from diagnosis of brain metastasis to enrollment was 2.1 weeks. All of the 45 patients available for evaluation completed the 15 fraction course of WBRT, with 3 patients (6.7%) experiencing a >4 day interruption between fractions. Overall, 40 patients (88.9%) received all 11 planned doses of MGd followed by WBRT and SRS as intended, while 4 patients (8.9%) missed at least one scheduled dose of MGd (range 1–3 doses). The interval between the last fraction of WBRT to SRS boost ranged from 1 to 14 days, with a median of 7 days. The median heterogeneity index (maximum dose/prescription dose) for SRS treatments was 1.3 (range 1.0–2.1), with a median conformality index (prescription isodose volume/target volume) of 1.8 (range 0.5–4.6).
Adverse events
The incidence of irreversible grade 3 or any grade ≥4 neurotoxicity attributable to radiation therapy occurring within 3 months of SRS boost was 4.4%, occurring in two patients. One patient experienced generalized weakness and the second developed radionecrosis requiring resection and prolonged hospitalization.
Grade ≥3 toxicity that was potentially related to MGd treatment occurred in 10 patients (22.2%) and is outlined in Table 3. In addition to the neurotoxicity reported above, these included anemia in 1 patient (2.2%), atrial fibrillation 1 (2.2%), liver function test abnormality 1 (2.2%), deep venous thrombosis 3 (6.7%), and dermatitis 2 (4.4%). Observed grade 3 skin toxicity included allergic dermatitis and exfoliative dermatitis, both of which were out of the radiation treatment portals and presumably related to MGd administration. There was no grade ≥3 radiation dermatitis.
The most commonly observed adverse events related to MGd treatment were low grade. Grade 1 and 2 toxicities included green discoloration of the skin in 37 patients (82.2%), chromaturia 30 (66.7%), fatigue 15 (33.3%), nausea 10 (22.2%), diarrhea 10 (22.2%), headache 8 (17.8%), blisters 7 (15.6%), rash 6 (13.3%), liver function abnormalities 4 (8.9%), and arthralgias 4 (8.9%).
Secondary and exploratory efficacy endpoints
New brain metastases were detected in 11 patients (24.4%) at the time of SRS treatment planning MRI, following the complete course of MGd, in comparison to the screening MRI at the time of diagnosis. A single new lesion was discovered in 7 patients (15.6%), two lesions in 2 patients (4.4%), and three lesions in 2 patients (4.4%). The median area of newly detected lesions for each patient was 0.2 cm2, with a range of 0.0–1.2 cm2.
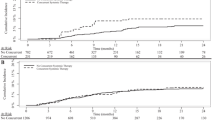
With a median follow-up of 7.5 months (range 38–578 days), the median interval to investigator-determined neurologic progression among all 45 evaluable patients had not been reached at the time of study completion (Fig. 1). The actuarial incidence of neurologic progression at 6 months and 1 year was 17 and 20%, respectively. Both the investigator-determined neurologic progression free survival and overall survival were 39% at 1 year. The median investigator-determined neurologic progression free survival and overall survival was 8 (95% CI: 5–14) and 9 months (95% CI: 6–unknown), respectively (Fig. 2).
Unadjusted Kaplan–Meier estimate of the time to investigator-determined CNS progression among all evaluable patients (n = 45). The median interval to neurologic progression had not been reached at the time of study completion. The estimated rates of freedom from neurologic progression at 6 months and 1 year were 83 and 80%, respectively. M months since the initiation of WBRT
The rates of neurocognitive progression by psychometric instruments at 6 months and 1 year were: COWA 5 and 5%, HVLT free recall 32 and 32%, TMT Part A 18 and 18%, TMT part B 26 and 26%, and HVLT delayed recall 47 and 55%. The median interval to neurocognitive progression according to HVLT Free Recall, COWA, TMT Part A, and TMT Part B tests was not reached. The median time to neurocognitive progression according to the HVLT Delayed Recall assessment was 8 months (95% CI: 4–not reached).
Radiologic follow-up (within approximately the 3-month follow-up time frame) was available for 43 of 45 evaluable patients. Surveillance MRI at the 3-month time point was available for 38 patients. The majority of patients (55.2%) demonstrated stable disease. There was one complete response (2.6%) and 13 partial responses (34.2%), for an overall response rate of 36.8% at three months. Radiologic evidence of progressive disease was seen in three patients (7.9%). The median interval to radiologic progression was not reached at the time of study termination.
Discussion
The addition of MGd to prompt WBRT has recently been shown to significantly improve the interval to neurologic and neurocognitive progression in non-small cell lung cancer patients with brain metastases [19]. In addition, the results of this recently reported phase III randomized trial demonstrated a substantial reduction in the need for salvage brain surgery or stereotactic radiosurgery with the addition of MGd [19]. That trial, however, did not allow for the inclusion of SRS as a component of initial therapy. The current trial, PCYC-0224, includes the first published results investigating the combination of MGd to WBRT followed by SRS boost.
The primary endpoint of this phase II trial was the rate of irreversible grade 3 or any grade ≥4 neurotoxicity attributable to radiation occurring within 3 months of SRS boost and was found to be acceptably low at 4.4% (2 patients). This is comparable to the previously published results of major trials investigating the combination of WBRT and SRS, suggesting that the addition of MGd does not increase the incidence or severity of neurologic complications from SRS [5, 21–23]. There were no other grade 3 or 4 adverse events related to MGd administration observed with an incidence of >10%. The majority of toxicities observed were grade 1 or 2 and consistent with the known and expected MGd side effect profile from previous trials, falling well within the statistical bounds proscribed at the time of trial initiation [19, 24–27]. The most common adverse event was reversible olive discoloration of the skin and urine (82%), related to MGd’s dark-green color. Others included fatigue, LFT abnormalities, hypertension, nausea, diarrhea, blisters and rash.
The feasibility endpoint was to evaluate the “dropout” rate to plan the appropriate sample size for a future phase III trial. Of 65 patients enrolled, 45 received WBRT and SRS with 7 or more of 11 planned doses of MGd, and MGd on the day of SRS; this represents a “dropout” rate of 20/65, or 31%, a significant number that would need to be accounted for in future trials; the primary reasons for this included the 13 patients who did not receive SRS boost (13 patients, 20%: 6 decline in health/disease progression, 4 patient refusal, 2 no longer SRS candidate, and 1 poor target delineation) or MGd on the day of SRS boost (7 patients, 11%: 5 patient/physician preference, 2 patient refusal). If future trials would allow inclusion of these latter 7 patients, the “drop-out” rate, would be approximately 20%, which could be built into a future phase III trial. The observed drop out rate of 13 patients (20%) who did not go on to receive SRS observed in the current trial is comparable to the 19% observed in the phase III trial RTOG 9508, which corroborates that the addition of MGd is well tolerated and is not causing undue toxicity that prevents patients from proceeding to SRS boost [5].
The median time to CNS progression had not been reached at the time of study closure. The median time to neurocognitive progression was not reached for 5 of the 6 formally tested instruments, with the exception of 8 months for the HVLT for Delayed Recall. This finding is consistent with previous reports employing the HVLT instrument in patients receiving WBRT, indicating there is a measurable impact on memory function in many patients [28]. However, the goal of preserving neurocognition is complex, as several reports suggest that intracranial tumor progression has a larger impact on neurocognitive decline in comparison to the effects of radiotherapy [29, 30].
It is important to point out that this was not an intention to treat analysis given that the study was designed to assess the primary endpoint of attributable neurologic toxicity for this novel combination of modalities with proven efficacy in the treatment of brain metastases. All patients who did not receive SRS or MGd and SRS on the same day were discontinued from the study and were not evaluable. For example, six patients did not go on to receive SRS due to health decline and/or disease progression. Assessment of neurologic progression and survival endpoints should be interpreted in this context, recognizing that trial design selected for patients with a more favorable prognosis and introduced bias into the efficacy assessment. Unbiased and conclusive efficacy testing should be the subject of further randomized investigation of WBRT and SRS with or without MGd.
The protocol enrolled patients with up to four brain metastases, but allowed for the treatment of up to six lesions to account for new lesions detected at the time of SRS. Ten patients (22%) on the study had 4 or more brain metastases. Given that only four patients had 5 or 6 lesions, the safety of this combination regimen for all patients with a large number of brain metastases has not been completely established. One of the more noteworthy findings from the study was the percentage of patients discovered to have new brain lesions at the time of SRS planning. One potential explanation is the accumulation of MGd in previously undetected, small metastases. MGd does not cross the intact blood–brain barrier, preferentially accumulates in tumors with prolonged retention, and is detectable on MRI [17, 18, 31].
The median area of newly detected metastases was only 0.2 cm2. One-fourth of all patients experienced an increase in the number of lesions to be treated with radiosurgery in comparison to what was expected based upon pretreatment MRI obtained at the time of diagnosis and study enrollment. An alternative explanation is the continued growth of small micrometastases that had previously not been detected. A final explanation is use of MRI techniques with better resolution and thinner slices for the SRS MRI. Unfortunately, the current study did not control for variations in MRI technique. Therefore, these data are inconclusive and a causal relationship has not been established. We do, however, believe it should be the subject of further, controlled investigation, as this finding represents a potential direct application and benefit for the radiosurgical management of brain metastases.
In conclusion, the combination of WBRT and SRS with MGd appears safe. In the current trial, we observed acceptable rates of neurotoxicity attributable to radiotherapy and post-treatment neurocognitive profiles consistent with previously published reports following WBRT. Future controlled investigation should focus on the potential role of MGd in improving the diagnostic yield of MRI in radiosurgery treatment planning.
References
Richards P, Mc KW (1963) Intracranial metastases. Br Med J 1:15–18
Lang EF, Slater J (1964) Metastatic brain tumors. Results of surgical and nonsurgical treatment. Surg Clin North Am 44:865–872
Borgelt B, Gelber R, Kramer S et al (1980) The palliation of brain metastases: final results of the first two studies by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 6:1–9
Kondziolka D, Patel A, Lunsford LD et al (1999) Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys 45:427–434
Andrews DW, Scott CB, Sperduto PW et al (2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 363:1665–1672
Bhatnagar AK, Flickinger JC, Kondziolka D et al (2006) Stereotactic radiosurgery for four or more intracranial metastases. Int J Radiat Oncol Biol Phys 64:898–903
Zahedi Avval F, Berndt C, Pramanik A et al (2009) Mechanism of inhibition of ribonucleotide reductase with motexafin gadolinium (MGd). Biochem Biophys Res Commun 379:775–779
Hashemy SI, Ungerstedt JS, Zahedi Avval F et al (2006) Motexafin gadolinium, a tumor-selective drug targeting thioredoxin reductase and ribonucleotide reductase. J Biol Chem 281:10691–106977
Magda D, Lecane P, Miller RA et al (2005) Motexafin gadolinium disrupts zinc metabolism in human cancer cell lines. Cancer Res 65:3837–3845
Amato RJ, Jac J, Hernandez-McClain J (2008) Motexafin gadolinium for the treatment of metastatic renal cell carcinoma: phase II study results. Clin Genitourin Cancer 6:73–78
Lecane PS, Karaman MW, Sirisawad M et al (2005) Motexafin gadolinium and zinc induce oxidative stress responses and apoptosis in B-cell lymphoma lines. Cancer Res 65:11676–11688
Magda D, Lepp C, Gerasimchuk N et al (2001) Redox cycling by motexafin gadolinium enhances cellular response to ionizing radiation by forming reactive oxygen species. Int J Radiat Oncol Biol Phys 51:1025–1036
Miller RA, Woodburn K, Fan Q et al (1999) In vivo animal studies with gadolinium (III) texaphyrin as a radiation enhancer. Int J Radiat Oncol Biol Phys 45:981–989
Miller RA, Woodburn KW, Fan Q et al (2001) Motexafin gadolinium: a redox active drug that enhances the efficacy of bleomycin and doxorubicin. Clin Cancer Res 7:3215–3221
Xu S, Zakian K, Thaler H et al (2001) Effects of Motexafin gadolinium on tumor metabolism and radiation sensitivity. Int J Radiat Oncol Biol Phys 49:1381–1390
Bepler G, Zheng Z, Gautam A et al (2005) Ribonucleotide reductase M1 gene promoter activity, polymorphisms, population frequencies, and clinical relevance. Lung Cancer 47:183–192
Rosenthal DI, Nurenberg P, Becerra CR et al (1999) A phase I single-dose trial of gadolinium texaphyrin (Gd-Tex), a tumor selective radiation sensitizer detectable by magnetic resonance imaging. Clin Cancer Res 5:739–745
Viala J, Vanel D, Meingan P et al (1999) Phases IB and II multidose trial of gadolinium texaphyrin, a radiation sensitizer detectable at MR imaging: preliminary results in brain metastases. Radiology 212:755–759
Mehta MP, Shapiro WR, Phan SC et al (2008) Motexafin gadolinium combined with prompt whole brain radiotherapy prolongs time to neurologic progression in non-small-cell lung cancer patients with brain metastases: results of a phase III trial. Int J Radiat Oncol Biol Phys 73:1069–1076
World Medical Association Declaration of Helsinki (2001) Ethical principles for medical research involving human subjects. Bull World Health Organ 79:373–374
Shaw E, Scott C, Souhami L et al (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90–05. Int J Radiat Oncol Biol Phys 47:291–298
Gaspar L, Scott C, Rotman M et al (1997) Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37:745–751
Aoyama H, Shirato H, Tago M et al (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491
Bradley KA, Pollack IF, Reid JM et al (2008) Motexafin gadolinium and involved field radiation therapy for intrinsic pontine glioma of childhood: a Children’s Oncology Group phase I study. Neuro Oncol 10:752–758
Ford JM, Seiferheld W, Alger JR et al (2007) Results of the phase I dose-escalating study of motexafin gadolinium with standard radiotherapy in patients with glioblastoma multiforme. Int J Radiat Oncol Biol Phys 69:831–838
William WN Jr, Zinner RG, Karp DD et al (2007) Phase I trial of motexafin gadolinium in combination with docetaxel and cisplatin for the treatment of non-small cell lung cancer. J Thorac Oncol 2:745–750
Mehta MP, Rodrigus P, Terhaard CH et al (2003) Survival and neurologic outcomes in a randomized trial of motexafin gadolinium and whole-brain radiation therapy in brain metastases. J Clin Oncol 21:2529–2536
Chang EL, Wefel JS, Hess KR et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet 10:1037–1044
Li J, Bentzen SM, Renschler M et al (2007) Regression after whole-brain radiation therapy for brain metastases correlates with survival and improved neurocognitive function. J Clin Oncol 25:1260–1266
Aoyama H, Tago M, Kato N et al (2007) Neurocognitive function of patients with brain metastasis who received either whole brain radiotherapy plus stereotactic radiosurgery or radiosurgery alone. Int J Radiat Oncol Biol Phys 68:1388–1395
Wu GN, Ford JM, Alger JR (2003) MRI measurement of the uptake and retention of motexafin gadolinium in glioblastoma multiforme and uninvolved normal human brain. J Neurooncol 77:95–103
Acknowledgments
Trial was sponsored and supported by Pharmacyclics Inc., Sunnyvale, CA.
Conflict of interest
1. Minesh Mehta serves on the Board of Directors of Pharmacyclics (paid, including stock options), Inc. and is a consultant for Schering-Plough, Genentech, Tomotherapy (including stock options), Bayer, and Adnexus. 2. Tarak Mody is a Senior Director for Development for Pharmacyclics, Inc. All additional authors report no conflicts of interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
This trial, PCYC-0224, is registered through the NIH at http://clinicaltrials.gov with an identifier of NCT00121420.
Rights and permissions
About this article
Cite this article
McHaffie, D.R., Chabot, P., Dagnault, A. et al. Safety and feasibility of motexafin gadolinium administration with whole brain radiation therapy and stereotactic radiosurgery boost in the treatment of ≤6 brain metastases: a multi-institutional phase II trial. J Neurooncol 105, 301–308 (2011). https://doi.org/10.1007/s11060-011-0590-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-011-0590-9