Abstract
Meningiomas account for approximately 20% of adult primary intracranial tumours. WHO I meningiomas are the most common and are generally benign, but can progress, recur or transform to WHO II or WHO III grades over many years. A systematic review of multiple independent shotgun proteomic analyses of meningioma was performed to provide insight into underlying disease pathways. Shotgun proteomics has been conducted in seven meningioma related studies but there is considerable variation in aims, methodology, statistical power and the use of control tissue between these studies. Fifteen proteins which are different between WHO I and WHO II meningiomas and nine proteins which are different between WHO II and WHO III meningiomas have been described but without a view of their biological significance. Network analysis of proteins different between WHO I and WHO II meningiomas provided a coherent hypothesis for the involvement of these proteins in meningioma. Western blot analyses of meningioma tissue provided a measure of support for a core component in the network (involving VDAC2, APOA1 and HNF4α) but highlighted intrinsic difficulty of proteomic and biochemical analysis of meningiomas (as a consequence of gross alterations in tissue composition). Systematic review of shotgun proteomics and network analysis provides insight into meningioma pathophysiology despite the many barriers and difficulties that are inherent to this type of study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Shotgun proteomics provides simultaneous assessment of multiple proteins expressed by a cell or tissue [1]. Traditionally, studying one targeted protein through methods such as immunohistochemistry and western blotting, depended on antibody availability, was time-consuming and gave little insight into the complex protein pathways that underpin neoplasia. With 2-dimensional gel electrophoresis (2DGE) combined with mass spectrometry, hundreds of proteins in a single tissue sample can be identified on a single gel phase (2DGE). Factors such as epigenetic phenomena, post-translational modification, modifications occurring from transcription to translation, protein trafficking and protein interactions can all affect the final protein levels within a cell [2]. Thus, proteomics has the potential to characterize the dynamic regulation or dysregulation of protein expression and function [2].
Primary brain tumours such as meningiomas and gliomas are currently characterized and classified histopathologically for purposes of diagnosis and treatment. The World Health Organisation (WHO) classifies meningiomas into three histological grades: benign (grade I), atypical (grade II) and anaplastic (grade III) that generally relate well to clinical prognosis [3–5]. Thus, in 90% of grade I meningiomas surgery would be deemed curative [5, 6]. Yet some grade I meningiomas show a propensity for progression (if not totally excised), recurrence (even if apparently totally excised) and occasionally transformation to higher grade tumours despite seemingly benign histological characteristics [3, 5]. Shotgun proteomics has been extensively employed in the study of gliomas [2, 8, 9], and systematic review of these data coupled to bioinformatics network analysis has provided insight to glioblastoma pathophysiology [9]. In contrast, no systematic analysis of shotgun proteomics in excised meningioma tissue or cells in culture has been performed. The major translational clinical benefit of proteomic studies in meningiomas would be realised if it was possible to identify the non-indolent WHO I meningiomas at diagnosis, so that adjuvant therapy could be offered to minimize recurrence and reduce morbidity and mortality. Additionally, proteomic studies could give pathophysiological insights into the oncological basis of WHO II and III tumours, possibly translating into prognostic, categoric or therapeutic benefit.
In the present report, we performed a systematic review of meningioma proteomics and critically evaluated the findings. All the proteins identified in meningioma proteomic studies were compared for commonality across studies. The list of proteins found to be differentially expressed between different WHO graded meningiomas were then assessed by network analysis (i.e. protein–protein interactions) using the ingenuity pathway analysis (IPA) bioinformatics database which identifies highly connected biochemical networks [10]. Secondly, the dependence of a meningioma protein network on a hub protein inserted by IPA, which has never before been described in meningiomas, was assessed (and confirmed), but the analyses highlighted gross changes in tissue composition between meningioma samples.
Methods
Systematic review of meningioma proteomics
The main search terms “proteomics” and “meningioma” were employed using the literature databases: Medline, Embase and Web of Science (WoS). Other more specific terms like “electrophoresis, gel, two-dimensional”, “nano liquid chromatography” and “meningeal neoplasms” were also tested. From each retrieved article, the year of publication, sample size (‘n’), WHO pathology grade, method of protein analysis, use of control tissue and differentially expressed protein names and accession numbers were extracted. A comprehensive spreadsheet was created containing all of the aforementioned data. Articles up to October 2010 were included.
Proteins altered in meningioma and their putative functional interactions
Ingenuity pathway analysis (IPA) software was used to investigate the existence of any functional protein–protein interactions amongst the proteins identified as differentially expressed between benign and atypical tumours by one of the reviewed papers [13]. IPA software comprises a huge manually curated knowledge database of protein information extracted from peer-reviewed literature [9–11]. Uniprot accession numbers of differentially expressed proteins in meningioma were uploaded to IPA, which categorised the proteins into biological networks and functional pathways containing direct protein–protein interactions. Generated IPA networks were ranked by statistical ‘score’ based upon the inclusion of as many proteins from the inputted list as possible. For more details on IPA network scores and features, please refer to references [11, 12] or Ingenuity Systems Ltd online help manual (https://analysis.ingenuity.com/pa/info/help/help.htm#ipa-help.htm). The strengths and limitations of IPA network analyses have recently been discussed in relation to glioma and cell death research [9, 11]. IPA also identified the biological functions and/or diseases that were most significantly overrepresented by the proteins differentially expressed in meningioma as determined by a right-tailed Fisher’s exact test.
Critical analysis of functional networks in meningioma using western blotting
Western blot analyses were performed to examine the proposed expression profiles of specific proteins within the meningioma network generated with IPA. Three inter-connected proteins at the core of the meningioma network were chosen for investigation: VDAC2, APOA1 and HNF4α. VDAC2 and APOA1 represent proteins that change bidirectionally from grade I to grade II meningiomas, up-regulated and down-regulated, respectively. HNF4α is an IPA inserted hub protein linking VDAC2 and APOA1, never before identified in meningioma samples. The presence of these proteins would confirm the biological relevance of IPA inserted proteins and also represent a novel protein pathway in meningioma pathophysiology.
All tissue was taken from first surgical operations of adult patients (age range 31–93 years) with informed written consent (Lothian Region Ethical Approval, LREC/2004/4/16). WHO I and WHO II meningioma tissue (defined independently by a specialist neuropathologist) was homogenised in a buffer consisting of 9 M urea, 4% CHAPS and complete protease inhibitor cocktail and centrifuged at 10,000 rpm for 10 min. The supernatant was recovered and stored at −80°C until required. Each sample was assayed for protein concentration using the Bradford method. Samples were denatured at 70°C for 10 min before being separated on 4–12% Bis–Tris gel (Invitrogen) at 80 V for 150 min. Proteins were electro-transferred (30 V, 1 h) on to nitrocellulose membrane (Biorad). After blocking (10 ml Odyssey blocking buffer, 10 ml Phosphate Buffered Saline), membranes were incubated overnight with blocking solution containing either rabbit polyclonal VDAC2 antibody (1:1000, Abcam, Cambridge, UK); mouse monoclonal APOA1 antibody (1:500, Santa Cruz); goat polyclonal HNF4α (1:500, Santa Cruz); with GAPDH or α tubulin as loading controls. After washing six times for 5 min in PBS/0.1% Tween-20 solution, the membranes were incubated for 1 h with the appropriate 680 and 800 IR dye secondary antibodies (1:50000, LI-COR Biosciences). The membranes were washed again in PBS/0.1% Tween-20 solution with a final wash carried out in PBS only. The membranes were imaged using Odyssey infrared imaging system, corrected for background, and analysed using Odyssey software (LI-COR Biosciences).
Results
Systematic review of meningioma proteomics
Five papers and two abstracts were identified in which differences in multiple protein expression between different subtypes of meningeal neoplasms were described [13–19]. There was considerable variation regarding aims, methodology, statistical power and use of control tissue between studies within this publication list (Table 1). For example, Okamoto et al. [13] compared differences between first resections of WHO I, II and III tumours. Agar et al. [14] characterised tumours similarly, but also included specimens that were recurrent and/or progressive. Wibom et al. [19] compared proteomes of invasive and infiltrative meningioma versus non invasive or non-infiltrative WHO I meningiomas. Boumrani et al. [15] investigated specifically, brain invasive and infiltrative behaviour in mostly WHO I meningiomas. Saydam et al. [17] compared findings in meningioma cell lines versus normal arachnoidal tissue. There was also variation in the way meningioma samples were prepared for proteomic analysis. Most studies used whole cell lysates, while two studies [13, 14] employed selective tissue microdissection to obtain purer populations of tumour cells. Sample sizes varied from 14 to 64, and a range of protein separation and identification methodologies were used, ranging from 2DGE and MALDI-TOF MS to alternatives such as Nano-LC MS/MS and SELDI-TOF MS (Table 1).
A list of proteins differentially expressed in meningioma was compiled. The list has limitations, for example, only two papers [13, 17] actually published lists of named proteins that were differentially up- or down-regulated, and of these, one paper [13] did not use ‘control’ tissue, and the other [17] compared meningioma cell lines versus primary arachnoidal cells. One abstract mention differentially expressed proteins but does not attempt to explain if they were up or down regulated [16]. One study named only a single protein of interest that they found as an intensity peak in the protein profile adequate in discriminating between non-infiltrative versus infiltrative or invasive tumours. This was a multi-phosphorylated form of vimentin [15]. Another study compared differentially expressed spectra intensities in the protein profiles, without establishing specific protein identification [19]. Out of the five papers and two abstracts, one study [19] and one abstract [18] used normal arachnoidal tissues from autopsies as control tissue. One other study [14] used ‘non tumourous’ brain samples from patients undergoing epilepsy and post-mortem tissue. The same study also used ‘healthy blood samples’ as controls. It is unclear how comparable the proteomic profile of blood samples would be with brain tissue samples. Other studies either did not have control tissue for comparison or compared the proteomic profiles of different histological subtypes of meningiomas with each other (Table 1) [13, 14, 16, 19].
Proteins altered in meningioma and their putative functional interactions
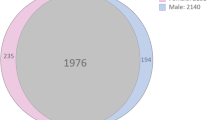
Only two papers published lists of identified proteins in meningioma. One study [17] found that there were 281 proteins that were differentially expressed between the meningioma cell line and normal arachnoidal tissue, 97 of which were exclusively expressed in meningiomas and 36 that were exclusively expressed in arachnoidal cells. In a study investigating the comparability of glioma cell lines and resected human glioblastoma, Vogel et al. [20] found there was a significant difference between these different tissues: 160 proteins were gained and 60 proteins lost on culture out of a total of about 500 protein spots identified [20]. This finding strongly suggests that caution should be taken when using cell lines followed by translation to functional analysis of human brain tumours. Okamoto et al. [13] listed two sets of proteins associated with different grades of meningiomas (Table 2). One set comprised of 15 proteins that were differentially expressed in benign WHO I versus atypical WHO II meningiomas. The other protein set showed nine proteins that were differentially expressed in atypical WHO II versus anaplastic WHO III meningiomas.
The extent to which direct functional interactions have been described from proteins associated with different grades of meningioma was assessed by network analysis (Ingenuity pathway analysis; IPA). For the 15 proteins differentially expressed in WHO I versus WHO II meningiomas, IPA network analysis yielded a high score of 41 (see reference [11]) with all 15 proteins included in the generated network. The top two biological functions ascribed to the network by IPA were ‘cancer’ (10 proteins) and ‘cellular growth and proliferation’ (9 proteins) (Table 3).
A second network of protein interactions was identified with the set of nine proteins found differentially expressed in WHO III versus WHO II tumours (Table 3). For this network, IPA network analysis yielded a lower score of 24 and the generated network did not appear to be directly related to neoplasia. Unfortunately, the Okamoto et al. [13] study did not analyse the proteins differentially expressed between WHO I and WHO III meningiomas.
Critical analysis of functional networks in meningioma
Network analysis, though persuasive and with a quantitative underpinning, provides a hypothesis for protein–protein interactions in meningioma. The database from which the network is derived is based on published protein–protein interactions irrespective of cell type, tissue, organ or species. The network may depend upon the insertion in the analysis of a “hub” protein, which may never have been described in the samples being studied. For example, HNF4α is an inserted hub protein in the meningioma network (Fig. 1) and we have demonstrated that it is present across all of our meningioma sample (WHO I and II) (Fig. 2). Although there was no evidence that HNF4α was altered in WHO 1 meningiomas relative to WHO II meningiomas, its presence (and not alteration) is sufficient to support the generated network.
Putative interactions of proteins altered in meningioma. The network of direct interactions between 15 proteins differentially expressed in benign WHO I versus atypical WHO II meningiomas [13] was generated from the IPA database of published interactions between proteins (derived from diverse species, organs and cell types). The 15 proteins altered in meningioma [13] have a coloured background: proteins in red (i.e. PRD2, PRD8, ATP5H, ALKAL, VDAC2, ACTA2, LGAL1, PSME2 and CRABP2) are upregulated and proteins in green (i.e. AHSA1, POA1, STRAP, RNH1, CNNi, and GC) are downregulated. Proteins with no background colour (for example, HNF4α) are proteins that have been inserted into the network by IPA to produce a highly connected network (see http:\\www.ingenuity.com) but which have not been shown to be altered (or even identified) in meningioma samples
Western analysis of individual proteins provides support for the protein–protein interaction network in Fig. 1. a The presence of HNF4α (a ‘hub’ protein in Fig. 1 inserted by IPA) in all patients with WHO I and WHO II meningiomas is described. Despite loading the same amount of protein in each lane (10 μg), there are marked differences in the GAPDH between samples. The sample from patient A (circled) was of overtly different composition from other samples (for example, solid at dissection and homogenized and solubilised with difficulty). b The protein VDAC2 was higher in 3 of the 4 patients (the exception being patient A) with atypical WHO II meningiomas compared to all 4 patients with benign WHO I tumours. Again despite loading the same amount of protein in each lane, there are marked differences in α-tubulin between samples. c The protein APOA1 was lower in 2 of the 4 patients (one of the exceptions being patient A) with atypical WHO II meningiomas compared to all four patients with benign WHO I tumours
The western analysis highlighted intrinsic challenges of meningioma proteomics. Despite meticulous assessment of protein concentrations, the levels of GAPDH and α-tubulin varied markedly among meningioma samples. The overt differences observed between samples during homogenization, provides further evidence of gross heterogeneity between meningioma samples. Notwithstanding this fundamental problem, western analysis offered some support for described protein alterations in meningioma. For example the expression of VDAC2 (which putatively interacts with HNF4α) was greater in 3 of 4 samples of WHO II than any of the WHO I samples. APOA1 (also shown to putatively interact with HNF4α) was less in 2 of 4 samples of WHO II than levels in the WHO I samples.
Discussion
Compared to proteomic research in gliomas [9, 21] there have been relatively few studies investigating meningiomas. There are several reasons for this. Firstly, in comparison to glioma where ‘control’ tissue is readily obtained from patients undergoing either epilepsy surgery or peri-lesional tissue from patients undergoing other lesional resection, it is difficult to obtain ‘control’ tissue (and indeed there is uncertainty as to what is the ideal ‘control’) for meningioma experiments. This is apparent in the various different types of control tissue and comparative study designs used in the reviewed papers. Meningiomas arise from arachnoidal cap cells which are found in arachnoid mater [3]. One way to obtain adequate arachnoidal tissue ethically would be from autopsy, and this in itself poses certain problems. Excision of normal dura during neurosurgery would also require ethical permission and it is debatable as to whether this would constitute an appropriate control. Thus, in the few papers reviewed, the lists of proteins either mentioned or recorded were not comparable due to the use of different ‘control’ tissues with different base-line protein profiles.
Another theoretical problem with meningioma proteomics is the potential lack of homogeneity in WHO I tissues, arising due to differences in histological tumour subtypes. There are nine histological variants recognised for WHO I meningiomas, the three commonest being meningothelial, fibroblastic and transitional [3, 4]. Heterogeneity of tissue samples used for our Western blot studies was also obvious, in terms of their physical characteristics within samples from the same meningioma grade. One particular WHO II sample (the outlier in Fig. 2) was firmer and more resistant to homogenization than the others. Such differences in the tissue consistency and firmness are obvious to all neurosurgeons who operate on meningiomas. Some tumours are extremely firm and resistant to removal by an ultrasonic aspirator, whilst others are soft and can be removed by simple suction. These differences in tissue consistency are frequently noticed even within the same tumour. Tissue heterogeneity may also explain the differences in basal expression levels of the two different “loading” controls used in this study (GAPDH—a metabolic marker; and alpha-tubulin—a structural marker). At present, little is known about how the different cyto-architectural patterns are represented by differences in proteomic profile. There are significant differentially expressed protein spectra between bone invasive and noninvasive fibrous and meningothelial WHO I subtypes [19]. Variation in the phosphorylation of vimentin in invasive meningiomas compared to non-invasive meningiomas further emphasizes potential proteomic differences related to biological tumour characteristics [14].
The relative scarcity of WHO II and III meningiomas is another methodological problem that will limit single centre studies since they comprise only about 10% of meningioma cases [3, 6]. The WHO derived grading system for meningiomas are dependent upon certain histological features. This can lead to subjectivity in classification particularly as these criteria are revised [3, 22]. In the latest revision, brain invasion was included as a criterion for atypia [3, 4]. Thus, histological WHO I tumours that are invading the brain are now classified as WHO II because they behave more aggressively. It is unclear if this is simply a result of parts of the tumour being left behind during resection or if there is something intrinsically aggressive about these tumours [3–5]. Molecular studies have shown that brain-invasive but histologically benign lesions do not display the genetic alterations characteristic of a higher grade meningioma [3, 5]. Clearly this is an area where proteomic research may help unravel the pathophysiology underlying aggressive tumour behaviour.
Another problem that will and does hamper translational research in meningioma research is the benign course of most meningiomas following Simpson grade 1 surgical resection. Therefore, it is not easy to do a prospective study between biomarkers and tumour recurrence as these tumours recur unpredictably and may take up to 10 years to do so [6, 7]. Additionally, at the time of recurrence, a WHO I meningioma may either still be a WHO I tumour or it may occasionally have transformed into either an atypical or malignant type [3, 5]. Ideally, one would want to compare the protein profiles of the first tumour and the recurring tumour in the same patient to determine if there are differentially expressed proteins that could predict later recurrence, progression and transformation. However, there exist logistical and practical limitations as to obtaining and storing histological samples of the first tumour for an extended period of time.
The protein–protein interaction network generated by IPA on one of the few specific datasets of differentially expressed proteins in meningiomas suggests that additional insight can be gained despite all the difficulties and various limitations of proteomic work on meningiomas. Confirmation of the presence in meningiomas of inserted hub protein HNF4α provides support for its insertion into the network (Fig. 1) [10]. IPA analysis extends pathophysiological insights beyond the limitations of extensive protein lists most commonly seen as the outcome of large scale proteomic studies. However, despite the apparent biological coherence of this analysis, there are limitations in the interpretation of IPA networks and shotgun proteomics [11]. Shotgun proteomics and IPA analyses are static in nature, they provide a snap shot of the proteins expressed at the time of tissue collection. There is therefore no demonstration of the temporal changes in protein expression seen throughout the progression of a dynamic, probably evolving oncogenic pathway. In addition, the databases from which the IPA software is derived are extensive and non-tissue specific in terms of information collated from publications [9]. Shotgun proteomics and IPA are powerful tools in generating hypotheses which must then be tested in subsequent studies for the tumour of interest.
Nonetheless, shotgun proteomics and IPA of meningiomas fit comfortably within the current concepts of tumour biology. VDAC channels are known to interact with many proteins, including those which are pro- and anti-apoptotic from the Bcl-2 family, as well as the apoptotic resistance enzyme hexokinase. It is hypothesised here that in tumour cells, hexokinase out compete pro-apoptotic proteins for interaction with VDAC, giving the cancer cells extensive proliferative capacity and apoptotic resistance [23]. Increased levels of VDAC2 in WHO II meningiomas (Figs. 2 and 3; and reference [13]) could represent more opportunity for hexokinase—VDAC interaction, a possible mechanism for conferring apoptotic resistance in atypical meningioma.
Putative VDAC2, APOA1 and HNF4α interaction—a possible mechanism for resistance to mitochondrial mediated apoptosis in atypical meningiomas. (a) Normal levels of APOA1 enable efficient cholesterol efflux from the cell. (b) In atypical meningioma cells, HNF4α reduces the expression levels of APOA1, reducing cholesterol efflux, causing an accumulation of this cholesterol in the mitochondrial membrane. (c) Excess cholesterol enhances the binding of anti-apoptotic hexokinase to VDAC2, out competing pro-apoptotic BCL2 proteins and changing the channel to an open conformation, preventing cytochrome c release through the mitochondrial swelling/rupture pathway. This effect will be exacerbated with the up regulation of VDAC2
Excess cholesterol enhances binding of hexokinase to VDAC channels, potentially increasing apoptotic resistance in malignant cancer cells [23]. Tissue culture experiments on macrophage cell lines have shown APOA1 to be essential for macrophage cholesterol efflux and cholesterol homeostasis [24]. It might therefore be hypothesised that in WHO II meningiomas, reduced levels of APOA1 result in reduced clearance of excess cholesterol from tumour cell membranes, enhancing the hexokinase—VDAC interaction, conferring apoptotic resistance. Cholesterol levels are found to be significantly increased in the mitochondria of hepatocarcinoma cells from human tissue. This increase in mitochondrial cholesterol conferred chemotherapy resistance upon these hepatocarcinoma cells [25]. Furthermore, murine studies investigating growth of gastric tumours have shown a negative correlation between APOA1 levels and gastric tumour development, with expression of APOA1 being lower in mice suffering larger tumours [26]. The fact that the trends in protein expression we have shown here in meningioma tissue are consistent with the pathological mechanisms underlying other cancer subtypes further validates the findings.
An important result from the western blot study is the demonstration that HNF4α is present in meningioma tissue and its apparent link between key proteins VDAC2 and APOA1. HNF4α has been implicated in the down regulation of the APOA1 gene in a human liver cancer cell line [27]. This finding suggests HNF4α is a crucial link between APOA1 and VDAC2 dysregulation which can confer mitochondrial mediated apoptotic resistance. A potential mechanism for the interaction of HNF4α, APOA1 and VDAC2 is summarised in Fig. 3.
Proteomic analysis within meningiomas is in its infancy, and further studies need to be performed. These studies will need careful, meticulous design to control for the many variables inherent in meningioma tissue. This review does, however, suggest pathophysiological pathways will be identified in these future studies. The challenge then is to translate the findings into therapeutic, categoric and prognostic variables.
References
Dhamoon A, Kohn E, Azad N (2007) The ongoing evolution of proteomics in malignancy. Drug Discov Today 12(17/18):700–708
Micallef J, Gajadhar A, Wiley J, DeSouza L, Siu K, Guha A (2008) Proteomics: present and future implications in neuro-oncology. Neurosurgery 62(3):539–555
Mawrin C, Perry A (2010) Pathological classification and molecular genetics of meningiomas. J Neurooncol 99(3):379–391
Perry A, Louis D, Scheithauer B, Budka H, Von Deimling A (2007) Meningiomas. In: Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds) WHO classification of tumours of the central nervous system. IARC press, Lyon, pp 164–172
Hanft S, Canoll P, Bruce J (2010) A review of malignant meningiomas: diagnosis, characteristics, and treatment. J Neurooncol 99(3):433–443
Whittle I, Smith C, Navoo P, Collie D (2004) Meningiomas. Lancet 363:1535–1543
Sughrue M, Kane A, Shangari G, Rutkowski M, McDermott M, Berger M, Parsa A (2010) The relevance of Simpson grade I and II resection in modern neurosurgical treatment of World Health Organization grade I meningiomas. J Neurosurg 113(5):1029–1035
Whittle I, Short D, Deighton R, Kerr L, Smith C, Mcculloch J (2006) Proteomic analysis of gliomas. Br J Neurosurg 21(6):576–582
Deighton R, McGregor R, Kemp J, McCulloch J, Whittle I (2010) Glioma pathophysiology: insights emerging from proteomics. Brain Pathol 1015–6305:1–13
Ingenuity systems citing guidelines. Last updated 2009. Available from http://www.ingenuity.com
Deighton R, Kerr L, Short D, Allerhand M, Whittle I, McCulloch J (2010) Network generation enhances interpretation of proteomic data from induced apoptosis. Proteomics 10:1–9
Deighton R, Short D, McGregor R, Gow A, Whittle I, McCulloch J (2009) The utility of functional interaction and cluster analysis in CNS proteomics. J Neurosci Methods 180(2):321–329
Okamoto H, Li J, Vortmeyet A, Jaffe H, Lee Y, Glasker S, Sohn T, Zeng W, Ikejiri B, Proescholdt M, Mayer C, Weil R, Oldfield E, Zhuang Z (2006) Comparative proteomic profiles of meningioma subtypes. Cancer Res 66(20):10199–10204
Agar N, Malcom J, Mohan V, Yang H, Johnson M, Tannenbaum A, Agar J, Black P (2010) Imaging of meningioma progression by MALDI-TOF MS. Anal Chem 82(7):2621–2625
Bouamrani A, Ramus C, Gay E, Pelletier L, Cubizolles M, Brugiere S, Wion D, Berger F, Issartel J (2010) Increased phosphorylation of vimentin in noninfiltrative meningiomas. PLoS ONE 5(2):e9238
Kim Y, Klotz M, Tholey A, Henn W, Schafer K, Feiden W (2009) Comparative proteome analyses of meningiomas of different grades in the identification of progression associated proteins. Acta Neuropathol 118:433–467 Abstract
Saydam O, Senol O, Schaaij-Visser T, Pham T, Piersma S, Stemmer-Rachamimov A, Wurdinger T, Peerdeman S, Jimenez C (2010) Comparative protein profiling reveals minichromosome maintenance (MCM) proteins as novel potential tumor markers for meningiomas. J Proteome Res 9:485–494
Scholz M (2006) Proteomics-based identification of differentially expressed proteins in human meningiomas. German medical science (Meeting Abstract)
Wibom C, Moren L, Aarhus M, Knappskof P, Lund-Johansen M, Antti H, Bergenheim A (2009) Proteomic profiles differ between bone invasive and noninvasive benign meningiomas of fibrous and meningothelial subtypes. J Neurooncol 94:321–331
Vogel T, Zhuang Z, Li J, Okamoto H, Furata M, Lee Y, Zeng W, Oldfield E, Vortmeyer A, Weil R (2005) Proteins and protein pattern differences between glioma cell lines and glioblastoma multiforme. Clin Cancer Res 11(10):3624–3632
Niclou S, Fack F, Rajcevic U (2010) Glioma proteomics: status and perspectives. J Proteomics 73(10):1823–1838
Willis J, Smith C, Ironside J, Erridge S, Whittle I (2005) The accuracy of meningioma grading: a 10 year audit. Neuropathol Appl Neurobiol 31:141–149
Pastorino J, Hoek J (2008) Regulation of hexokinase binding to VDAC. J Bioenerg Biomembr 40:171–182
Taylor J, Borthwick F, Bartholomew C, Graham A (2010) Overexpression of stroidogenic acute regulatory protein increases macrophage cholesterol efflux to apolipoprotein AI. Cardiovasc Res 86:526–534
Montero J, Morales A, Llacuna L, Lluis J et al (2008) Mitochondrial cholesterol contributes to chemotherapy resistance in hepatocellular carcinoma. Cancer Res 68:5246–5256
Chong P, Lee H, Zhou J, Liu S et al (2010) Reduced plasma APOA1 level is associated with gastric tumour growth in MKN45 mouse xenograft model. J Proteomics 73:1632–1640
Mogilenko D, Dizhe E, Shavva V, Lapikov I et al (2009) Role of the nuclear receptors HNF4α, PPARα, and LXRs in the TNFα-mediated inhibition of human apolipoprotein A-1 gene expression in HepG2 cells. Biochemistry 48:11950–11960
Acknowledgments
This work was partly supported by grants from the Chief Scientists Office, the Melville Trust, and The Brain Tumour Research Fund.
Author information
Authors and Affiliations
Corresponding author
Additional information
Herrmann A, Ooi J contributed equally
Rights and permissions
About this article
Cite this article
Herrmann, A., Ooi, J., Launay, S. et al. Proteomic data in meningiomas: post-proteomic analysis can reveal novel pathophysiological pathways. J Neurooncol 104, 401–410 (2011). https://doi.org/10.1007/s11060-010-0526-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-010-0526-9