Abstract
Bevacizumab is effective for the treatment of non-small cell lung cancer (NSCLC). Ongoing trials are exploring the safety of bevacizumab in patients with inactive, previously treated brain metastases. However, bevacizumab safety and efficacy in the treatment of active brain metastases is unknown. Bevacizumab received accelerated FDA approval for progressive glioblastoma, a primary brain tumor, because of high response rates and low incidence of intracranial hemorrhage. We retrospectively identified patients treated with bevacizumab for active (treatment naïve or progressive) central nervous system (CNS) metastases from NSCLC. MRI scans performed at least 6 weeks after initiating bevacizumab were assessed for response. There were six patients, four women and two men with a median age of 60 years (range 59–77) at initiation of bevacizumab. Five patients had progressive CNS metastases despite prior treatment including surgery, radiotherapy, and/or chemotherapy; one patient had treatment-naïve brain metastases. Two patients had leptomeningeal metastases, isolated or coexistent with parenchymal brain metastases in one patient each. Bevacizumab was administered alone to one patient and in combination with various cytotoxic chemotherapies in the others. Toxicity included an asymptomatic (Grade 1) intra-tumoral hemorrhage which occurred in one of three patients receiving concurrent anticoagulation with bevacizumab. There was no recurrent CNS bleeding in two patients with a prior history of such hemorrhage. Best CNS response (RECIST) was partial in two, stable disease in three, and progression in one. Median progression-free survival (PFS) was 7.8 months and median overall survival (OS) was 14.1 months following initiation of bevacizumab. Clinical benefit was also observed in the form of improved symptoms and reduced corticosteroid requirements. Bevacizumab should be used with caution in patients with active CNS metastases pending additional safety data. This series suggests bevacizumab may be safe and effective for progressive brain metastases from NSCLC and deserves further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment options are limited for patients with brain metastases from non-small cell lung cancer (NCSLC). Bevacizumab is a monoclonal antibody that binds VEGF-b, inhibiting angiogenesis. It is used in the treatment of multiple tumor types including NCSLC. Concerns about the risk of intracranial hemorrhage initially precluded use in patients with brain metastases. However, bevacizumab recently gained accelerated FDA approval for progressive primary brain tumors (glioblastoma) with a low rate (approximately 3%) of intratumoral hemorrhage [1].
Recent data suggest bevacizumab is safe in patients with treated, quiescent NSCLC brain metastases [2–5]. There are also anecdotal retrospective reports of bevacizumab given with therapeutic intent for brain metastases from breast [6] and colorectal [7] cancers. However, safety and efficacy in patients with active (progressive or untreated) central nervous system (CNS) metastases from NSCLC are unknown. Therefore, we retrospectively identified six patients with active CNS metastases from NCSLC and report results.
Methods
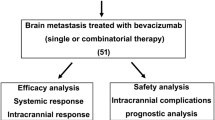
Using Institutional Review Board approved departmental databases, we retrospectively identified patients treated with bevacizumab-containing chemotherapy regimens for active CNS metastases, either untreated or progressive after at least one prior therapy. MRI scans to assess CNS radiographic response (RECIST) were reviewed by two neuro-oncologists (KCD, ABL) and discrepancies adjudicated by a neuro-radiologist (AIH). Survival was calculated by the Kaplan–Meier method. Clinical data was updated as of 12/21/2009.
Results
Patients
There were four women and two men (Table 1) with a median age of 60 years (range 59–77) at initiation of bevacizumab. Five patients had 1 to >10 brain metastases, one of whom had coexistent leptomeningeal metastases; one had isolated leptomeningeal disease. One patient had treatment-naïve brain metastases and five had progressive CNS disease despite prior surgery (n = 2), whole brain radiotherapy (n = 3), stereotactic radiosurgery (n = 2), and chemotherapy with temozolomide (n = 2), pemetrexed (n = 2), and intrathecal cytarabine (n = 1). Bevacizumab was administered as monotherapy to one patient and was combined with other agents in five.
Efficacy
Best CNS response was partial (Fig. 1) in two, stable disease (Fig. 2) in three, and progression in one. The radiographic response rate was 33% (2/6) and the disease control rate (complete/partial response + stable disease) was 83% (5/6). At initiation of bevacizumab, 5 patients had co-existent extra-CNS metastases; best response extracranially was stable disease in 4 (80%) and progression in 1 (20%). Of note, both patients with progressing extra-CNS disease at initiation of bevacizumab stabilized. After initiating bevacizumab, the median progression-free survival (PFS) was 7.8 months and the median overall survival (OS) was 14.1 months. Two of four patients who were neurologically symptomatic at baseline improved during bevacizumab-based therapy, and two of three were able to reduce corticosteroid dependence. Reasons for discontinuation of bevacizumab included toxicity (1), medical comorbidities precluding further therapy (1), CNS progression only (2), non-CNS progression only (1), and both CNS and non-CNS progression (1).
Partial response (patient 2 in Table 1). (a) Gadolinium-enhanced T1-weighted MRI of the brain 16 days prior to commencement of treatment with bevacizumab demonstrated a metastasis involving the left side of the pons with leptomeningeal spread along the fifth cranial nerve. (b) The fluid attenuation inversion recovery (FLAIR) sequence demonstrated extensive associated edema. Multiple follow up scans demonstrated almost complete resolution of the enhancement (c) and edema (d)
Stable disease (patient 1 in Table 1). (a) Gadolinium-enhanced T1-weighted MRI of the brain 13 days prior to commencement of treatment with bevacizumab demonstrated a brightly enhancing metastasis in the right quadrigeminal plate. (b) Two months following commencement of bevacizumab monotherapy, the lesion is unchanged in size; however, it demonstrates essentially no enhancement. Enhancement of the choroid plexus in the temporal horns of the lateral ventricles demonstrates that the contrast dose was adequate. (c) Following radiological stability in the interim, the MRI performed over 11 months after commencement of bevacizumab demonstrated a slight increase in the size of the metastasis with new peripheral enhancement
Toxicity
Major bevacizumab related toxicity included chronic skin ulceration at the site of a pilonidal cyst, pulmonary embolus, and asymptomatic (Grade 1) CNS hemorrhage in one patient each. The hemorrhage occurred in one of three patients receiving concurrent therapeutic anticoagulation with bevacizumab. There was no recurrent bleeding in two patients with a prior history of CNS hemorrhage.
Discussion
Hemorrhage into a previously unrecognized intracranial lesion in a patient with hepatocellular carcinoma on a phase I study of bevacizumab led to safety concerns in patients with CNS disease [8]. A Phase II trial of bevacizumab for NSCLC also reported intracranial hemorrhage in patients developing cerebral metastasis during treatment, although the incidence was <1% (3 of 427) [9]. Subsequently, screening brain imaging became routine, and clinical trials of bevacizumab excluded patients with brain metastases. These events also led to reluctance to use bevacizumab in patients with brain metastases.
However, further experience treating patients with primary or metastatic brain tumors revealed that intracranial hemorrhage was rare. Subsequently, eligibility criteria for clinical trials of extracranial solid tumors were relaxed, allowing patients with previously treated, but inactive, brain metastases to participate. For example, the PASSPORT (A Study of Bevacizumab in Combination With First- or Second-Line Therapy in Subjects with Treated Brain Metastases Due to Non-Squamous NSCLC, AVF3752g) and ATLAS (Avastin and Tarceva in Lung with NSCLC, AVF3671g) studies permitted accrual of patients with stable, treated cerebral metastases. There were no grade ≥2 cerebral hemorrhages in 106 patients with brain metastases who received bevacizumab in PASSPORT [2] and 1 of 25 patients in ATLAS [3].
An analysis of data from multiple trials encompassing over 10,000 patients with various primary cancers also demonstrated no significant increase in the risk of intracranial hemorrhage in 639 patients with documented brain metastases treated with bevacizumab [5]. Another study also confirmed that the risk of cerebral hemorrhage into incidental or quiescent metastases did not significantly increase when bevacizumab was administered [4].
However, the efficacy and safety of bevacizumab used with therapeutic intent for active brain metastases, as opposed to treated and inactive CNS disease, is unknown. All of our patients had active CNS disease. Toxicity was consistent with expected events from bevacizumab, but there was no grade ≥2 CNS hemorrhage despite a prior history of spontaneous hemorrhage in two patients and therapeutic anticoagulation in three. Concurrent anticoagulation and bevacizumab also has reported safety in patients with glioma [10].
Although the disease control rate in our series was high (83%), conclusions regarding efficacy are limited by our small size and because reduced contrast enhancement on MRI in patients with brain tumors may not reflect a true tumor response [1, 11] (Fig. 2). However, radiographic disease control was associated with neurologic improvement and reduced corticosteroid dependence, both clinically meaningful benefits. In addition, one patient with leptomeningeal metastases lived for over one year and the other for close to five months, exceeding the median survival of approximately two months for that disease [12].
Bevacizumab should be used with caution in patients with active CNS metastases pending additional safety data. However, our series suggests that bevacizumab administered with therapeutic intent for treatment of active CNS metastases may be effective safe and effective, especially for small lesions that are less likely to hemorrhage [13]. Further study of bevacizumab is warranted in NSCLC and other solid tumors such as breast [6] and colorectal [7] cancers in which bevacizumab has extra-CNS activity.
References
Cloughesy TF, Prados MD, Wen PY, Mikkelsen T, Abrey LE, Schiff D, Yung WK, Maoxia Z, Dimery I, Friedman HS (2008) A phase II, randomized, non-comparative clinical trial of the effect of bevacizumab (BV) alone or in combination with irinotecan (CPT) on 6-month progression free survival (PFS6) in recurrent, treatment-refractory glioblastoma (GBM). J Clin Oncol 26(Suppl):Abstract 2010b, oral presentation update
Socinski MA, Langer CJ, Huang JE, Kolb MM, Compton P, Wang L, Akerley W (2009) Safety of bevacizumab in patients with non-small-cell lung cancer and brain metastases. J Clin Oncol 27:5255–5261
Akerley WL, Langer CJ, Oh Y, Strickland DK, Joo Royer S, Xia Q, Mu Y, Huang J, Socinski MA (2008) Acceptable safety of bevacizumab therapy in patients with brain metastases due to non-small cell lung cancer [abstract]. J Clin Oncol 26: Abstract 8043
Besse B, Lasserre SF, Compton P, Huang J, Augustus S, Rohr UP (2010) Bevacizumab safety in patients with central nervous system metastases. Clin Cancer Res 16:269–278
Carden CP, Larkin JM, Rosenthal MA (2008) What is the risk of intracranial bleeding during anti-VEGF therapy? Neuro Oncol 10:624–630
Labidi SI, Bachelot T, Ray-Coquard I, Mosbah K, Treilleux I, Fayette J, Favier B, Galy G, Blay JY, Guastalla JP (2009) Bevacizumab and paclitaxel for breast cancer patients with central nervous system metastases: a case series. Clin Breast Cancer 9:118–121
Bhaskara A, Eng C (2008) Bevacizumab in the treatment of a patient with metastatic colorectal carcinoma with brain metastases. Clin Colorectal Cancer 7:65–68
Gordon MS, Margolin K, Talpaz M, Sledge GW Jr, Holmgren E, Benjamin R, Stalter S, Shak S, Adelman D (2001) Phase I safety and pharmacokinetic study of recombinant human anti-vascular endothelial growth factor in patients with advanced cancer. J Clin Oncol 19:843–850
Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, Lilenbaum R, Johnson DH (2006) Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med 355:2542–2550
Nghiemphu PL, Green RM, Pope WB, Lai A, Cloughesy TF (2008) Safety of anticoagulation use and bevacizumab in patients with glioma. Neuro Oncol 10:355–360
van den Bent MJ, Vogelbaum MA, Wen PY, Macdonald DR, Chang SM (2009) End point assessment in gliomas: novel treatments limit usefulness of classical Macdonald’s Criteria. J Clin Oncol 27:2905–2908
DeAngelis LM, Posner JP (2009) Leptomeningeal metastases. In: DeAngelis LM, Posner JP (eds) Neurologic complications of cancer. Oxford University Press, Inc., New York, pp 240–281
Srivastava G, Rana V, Wallace S, Taylor S, Debnam M, Feng L, Suki D, Karp D, Stewart D, Oh Y (2009) Risk of intracranial hemorrhage and cerebrovascular accidents in non-small cell lung cancer brain metastasis patients. J Thorac Oncol 4:333–337
Acknowledgements
The authors thank Lisa M. DeAngelis, MD for critical review of the manuscript and Judith Lampron for her expert editorial assistance.
Disclaimers
Dr. Kris is listed on a patent application to use VEGF targeting agents to treat effusions. Dr. Lassman has consulted for Genentech on the use of bevacizumab to treat gliomas and received research support for clinical trials related to brain metastases from Novartis and Pfizer. No grants have been supplied by the NIH.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Braganca, K.C., Janjigian, Y.Y., Azzoli, C.G. et al. Efficacy and safety of bevacizumab in active brain metastases from non-small cell lung cancer. J Neurooncol 100, 443–447 (2010). https://doi.org/10.1007/s11060-010-0200-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-010-0200-2