Abstract
We retrospectively studied the efficacy of gamma knife surgery (GKS) for metastatic brain tumors from renal cell carcinoma (RCC). To evaluate the efficacy of GKS for control of peritumoral edema, we retrospectively studied 280 consecutive metastatic brain tumors (100 from lung cancers, 100 from breast cancers, and 80 from RCC) associated with peritumoral edema. In addition, this study included 11 patients with metastatic brain tumors from RCC who underwent direct surgery. The tumor growth control rate of GKS was 84.3%. The extent of edema of RCC metastases was significantly larger than those from lung and breast cancer. Primary site (renal or not renal) and delivered marginal dose (25 Gy or more) were significantly correlated with control of peritumoral edema. All tumors treated by direct surgery were more than 2 cm in maximum diameter. Peritumoral edema at surgery was extensive but disappeared within 1–3 months, and neurological symptoms also improved in many cases. Total removal of brain metastases from RCC was easy with little bleeding in most cases. Our results suggest that GKS is effective for growth control of metastatic brain tumors from RCC. Higher marginal dose such as 25 Gy or more is desirable to obtain peritumoral edema control, so GKS is not suitable for control of symptomatic peritumoral edema associated with relatively large tumors. Tumor removal of RCC metastases is relatively easy and rapidly reduces peritumoral edema. Treatment strategy for metastatic brain tumors from RCC depends on tumor size, number of tumors, and presence of symptomatic peritumoral edema.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumor growth control is the most important objective in treatment of metastatic brain tumors, but consideration of peritumoral edema is also very important because of resultant symptoms such as motor weakness, epilepsy, visual field defects, and aphasia, which may threaten activities of daily living in patients with generally limited life expectancy. Stereotactic radiosurgery has recently become widely used as a treatment modality for metastatic brain tumors [1–4]. However, control of peritumoral edema following gamma knife surgery (GKS) is not so well understood.
Renal cell cancer (RCC) metastasizes to the brain in about 10% of cases [5] and is radioresistant [6, 7]. Whole-brain radiotherapy (WBRT) is less effective against metastatic brain tumors from RCC [8], but radiosurgery may provide effective tumor control [9–17]. Previously, we described the efficacy of GKS against metastatic brain tumors from RCC [18]. We recently reported the efficacy of GKS for peritumoral edema control during management of metastatic brain tumors [19].
The present study updates the results of GKS for metastatic brain tumors from RCC [18], combined with the efficacy of GKS for peritumoral edema control [19], and retrospectively studied the results of direct surgery for metastatic brain tumors from RCC, to propose treatment strategy for control of both tumor growth and peritumoral edema.
Patients and methods
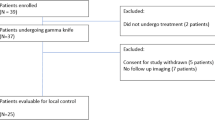
Analysis of tumor growth control following GKS
This study updates our previous analysis [18] to include 105 patients with metastatic brain tumors from RCC (77 men and 28 women; aged 45–85 years, mean 64.1 years), who underwent GKS at our hospital using the Leksell gamma unit (model B; Elekta Instrument AB, Stockholm, Sweden) and Gamma Plan treatment software or KULA (Elekta). Of these 105 patients, 36 patients were newly included in this study. Data of the other 69 patients were reported in our previous paper [18], and further follow-up findings were added in this study. The retrospective analysis included calculated tumor volume, prescription dose to the tumor margin, and change in tumor size on follow-up magnetic resonance (MR) imaging for each tumor. Change in tumor size was defined by the same method previously reported by us [18], summarized as complete remission (complete disappearance of the tumor), partial remission (decrease in tumor size of more than 25% but not disappearance), no change (no apparent change in size), and progression (increase in tumor size of more than 25% or decrease followed by increase in tumor size). Statistical analyses were carried out by using the StatView 5.0 statistical software package (SAS Institute, Cary, NC, USA). Logistic regression analysis was used to analyze significant factors affecting tumor growth control following GKS. A p value of <0.05 was defined as statistically significant.
Analysis of peritumoral edema control by GKS
Our previous analysis [19] retrospectively studied 280 consecutive metastatic brain tumors (100 from lung cancers, 100 from breast cancers, and 80 from RCC) which met the following criteria. The tumor was associated with apparent peritumoral edema at time of GKS on MR images, and was followed up on MR imaging for at least 6 months after GKS. No patient had a history of WBRT or craniotomy. No patient with multiple lesions had overlapping edema areas. The peritumoral edema index was measured as A × B × C, where A (cm) is the maximum diameter of the peritumoral edema on the axial MR image, B (cm) is the maximum diameter perpendicular to A, and C (cm) is the maximum diameter on the coronal image (Fig. 1). One-way analysis of variance followed by the Bonferroni/Dunn procedure was used to analyze differences in the edema index. Logistic regression analysis was used to analyze significant factors affecting peritumoral edema control following GKS.
Magnetic resonance images showing peritumoral edema index measured as A × B × C, where A (cm) is the maximum diameter of the peritumoral edema, B (cm) is the maximum diameter perpendicular to A, and C (cm) is the maximum diameter on the coronal image. In this example, edema index is A (3.1 cm) × B (1.3 cm) × C (2.0 cm) = 8.06 cm3
Analysis of patient survival and peritumoral edema control after direct surgery
This study included 11 patients with 12 metastatic brain tumors from RCC (9 men and 2 women; aged 53–74 years, mean 61.1 years), who underwent direct surgery at our hospital (Table 1). The retrospective analysis included tumor size, extent of peritumoral edema and neurological symptoms before and after direct surgery, survival time, and cause of death.
Results
Tumor growth control following GKS
The 105 patients underwent a total of 153 GKS procedures (mean 1.5). Only two patients received conventional external radiation therapy. The mean calculated volume of the tumors was 1.6 cm3 (range 0.1–22.6 cm3). The mean prescription dose at the tumor margin was 22.0 Gy (range 8–30 Gy), and the mean maximum dose was 37.3 Gy (range 14–55.6 Gy). Five of the 105 patients had tumor hemorrhage before GKS. GKS was canceled in one patient because of massive hemorrhage. Two patients suffered hemorrhage after GKS, and both underwent tumor removal.
A total of 444 tumors were treated by GKS (mean 2.9 tumors per procedure). Of these, 191 tumors were followed up by neuroimaging to monitor change following GKS. Mean duration of neuroimaging follow-up was 7.0 months (range 3–39 months). Apparently newly developed peritumoral edema following GKS was observed in only 5 of the 104 tumors not associated with peritumoral edema at the time of GKS. No apparent radionecrosis was detected by follow-up imaging, and no permanent morbidity associated with GKS. The outcome was complete remission (CR) in 71 of the 191 tumors (37.2%), partial remission (PR) in 52 (27.2%), no change (NC) in 38 (19.9%), and progression in 30 (15.7%). Therefore, the tumor growth control rate (CR + PR + NC) was 84.3%. Factors affecting tumor growth control are shown in Table 2. Tumor volume and delivered peripheral dose were significantly correlated with tumor growth control on univariate and multivariate analysis. Overall median survival time was 12 months (range 0.1–44.0 months). These results were almost the same as previously reported [18].
Peritumoral edema control by GKS
This is a summary of our previously published study [19]. Edema index of RCC metastases at time of GKS was significantly larger than those of lung and breast cancer metastases (p < 0.01) (Table 3). Edema index of RCC metastases at final imaging was also larger than those of lung (p < 0.05) and breast (p < 0.01) cancer metastases (Table 3). Controlled peritumoral edema was defined as decrease in edema index on final follow-up imaging to less than half of the pretreatment edema index. Peritumoral edema control was obtained for 82% of lung cancer metastases, 83% of breast cancer metastases, and 63.8% of RCC metastases. Primary site (renal or not renal, p < 0.01) and delivered marginal dose (25 Gy or more, p = 0.04) were significantly correlated with control of peritumoral edema on multivariate analysis. Details of the efficacy of GKS for peritumoral edema control associated with metastatic brain tumors are described elsewhere [19].
Patient survival and peritumoral edema control after direct surgery
The period between diagnosis of primary RCC and identification of brain metastases varied from 2 months to 6 years (mean 1.8 years). RCC was diagnosed after treatment of two brain metastases, both of which were removed, in one patient. All tumors were more than 2 cm in maximum diameter (range 2–5 cm, mean 3.5 cm). Peritumoral edema at surgery was extensive and symptomatic in many patients but disappeared within 1–3 months after surgery, and neurological symptoms such as motor weakness, aphasia, and disorientation improved (Table 1; Fig. 2). Tumors were all solid, except for one cystic tumor. The solid tumors were relatively hard in nine cases and soft in two. Most tumors were well demarcated and easily totally removed, except for one huge tumor (case 10), which required subsequent GKS to treat residual tumor. Our experience suggests that total removal of brain metastases from RCC is easy, with little bleeding in most cases with meticulous dissection technique. Resection was followed by external radiotherapy in 3 of the 12 resected tumors. Nine tumors were treated by only surgery, and three of these nine tumors recurred around the removal cavity and needed GKS. Therefore, the local control rate with only surgery was 66.7% in our series. Newly developed metastatic tumor was found in three patients after surgery (cases 4, 7, and 10), all treated by subsequent GKS. Three patients survived and eight patients had died at time of data collection. Median survival time was 11 months after surgery. Cause of death was progressive systemic disease in all eight patients.
A 56-year-old female with renal cell carcinoma. T1-weighted magnetic resonance (MR) image with gadolinium-diethylenetriaminepenta-acetic acid, showing a metastatic tumor with severe peritumoral edema in the temporal lobe (left). MR image about 1 month after surgical resection, demonstrating complete disappearance of peritumoral edema (right)
Discussion
Radiosurgery can achieve good tumor growth control for radioresistant tumors such as RCC and melanoma [1]. Tumor growth control of more than 90% has been reported (Table 4). Our experience also showed good tumor growth control by GKS for metastatic brain tumors from RCC, with a satisfactory growth control rate of 84.3%. This control rate is apparently lower compared with previous studies, but Table 4 shows small numbers of patients, as low as 30. Our study contains the largest number of patients, so we think our results may suggest the true control rate by GKS.
Peritumoral edema control presents another problem. Edema control around brain metastases from RCC by GKS has not been well described. Peritumoral edema improved in 8 of 16 patients following GKS, but the details were not shown [12]. Our previous study showed that brain edema around metastatic brain tumors from RCC was more extensive at time of GKS and at final imaging compared with lung and breast cancer metastases. In addition, multivariate analysis showed that primary site (not RCC) and higher delivered peripheral dose (25 Gy or more) were significantly correlated with good control of peritumoral edema. This new finding that RCC metastasis is a poor prognostic factor in peritumoral edema control is very important in discussing the treatment strategy for metastatic brain tumors from RCC.
GKS must deliver a marginal dose of 20 Gy to achieve tumor growth control, but 25 Gy or more is desirable to control peritumoral edema. We suggest that the optimal doses for tumor growth control and brain edema control may differ for metastatic brain tumors, especially from RCC. Such difficulty in edema control may be characteristic of GKS for brain metastases from RCC. The delivered dose depends mainly on the tumor volume. Marginal doses of 25 Gy or more are not recommended for tumors of more than 2 cm diameter. Therefore, the treatment strategy differs according to tumor volume and presence of symptomatic peritumoral edema.
The present study analyzed the results of direct surgery as well. Surgical removal of brain metastases from RCC was relatively easy in most of our cases, because of the well-demarcated boundaries and hardness of the tumors. Hypervascularity of RCC is well known, but little bleeding was encountered during surgery in most of our cases. Therefore, the risk associated with surgery was not high in patients with good general condition. In addition, surgery had a clear advantage in rapidly reducing peritumoral edema after tumor removal, as shown in Table 1 and Fig. 2. Although the survival benefit of tumor removal remains unclear, we recommend tumor removal if possible for patients with metastatic brain tumor from RCC of more than 2 cm in diameter associated with symptomatic peritumoral edema, to obtain rapid decrease of edema and improvement of neurological symptoms. Tumor removal by craniotomy and adjuvant WBRT are common treatment methods for metastatic brain tumors [20–22], but the efficacy of WBRT for RCC brain metastases is controversial [8, 23], and considering the low sensitivity of RCC to conventional radiotherapy, we recommend close MR imaging follow-up after removal of metastasis from RCC without subsequent WBRT.
Patients with metastatic brain tumors from RCC treated by combination of WBRT and radiosurgery survived longer than patients treated by only radiosurgery [10], as better local control was achieved [12, 23, 24]. However, the high growth control rate of RCC allows the use of only GKS [14, 18]. On the other hand, new development of metastases following GKS is common [9]. No preventive effect of WBRT was found on the new development of metastases from RCC [12]. Distant metastasis to the brain occurred in 39% of patients, and 16 of 69 patients received repeat GKS (2–3 times) [12]. Late distant metastasis occurred in about half of patients, but death from progression of brain disease was mainly avoided [12]. The present and previous studies indicate that repeat GKS should be performed for further metastases after the initial GKS [12, 16, 18].
GKS has been recommended for patients with up to three or four metastases [12, 16, 23], but some studies suggest that 20-25 small lesions are treatable by only GKS in one session [13, 25–27]. However, treatment time may be very long for such patients. Therefore, we recommend treatment in one or two sessions for patients with fewer than 20–25 metastatic brain tumors from RCC. Recently, some observations have suggested that inhibitors of tyrosine kinase receptors such as sorafenib and sunitinib are suitable for treatment of multiple brain metastases from RCC [28, 29].
The recommended treatment strategy for metastatic brain tumors from RCC is shown in Fig. 3. This strategy depends on tumor size, toleration of general anesthesia, presence of symptomatic peritumoral edema, and number of tumors. Fractionated stereotactic radiotherapy is indicated for unresectable large (more than 3 cm in diameter) tumors in patients with poor general condition [30], although the advantage of fractionation remains unclear for low-alpha/beta lesions such as RCC. Recently, good results were reported using three-stage stereotactic radiotherapy for large metastatic brain tumors with a 2-week interfraction interval [31]. A dose of 10 Gy was delivered in three fractions, and local tumor control rates of 89.8% and 75.9% were obtained at 6 and 12 months, respectively. Although this study included only 3 cases of metastatic brain tumors from RCC, 14 of 43 patients harbored colon cancer, which is known to be relatively radioresistant. We also recommend the same method to deliver 30 Gy in three fractions with a 2-week interval.
Conclusions
GKS is an effective treatment for metastatic brain tumors from RCC. The rate of complete remission on follow-up MR imaging is relatively low, but the tumor growth control rate is high. On the other hand, RCC metastasis is a poor prognostic factor for peritumoral edema control. Higher marginal doses such as 25 Gy or more are desirable to obtain peritumoral edema control. Therefore, control of symptomatic peritumoral edema associated with a relatively large tumor of more than 2 cm diameter is difficult. Surgical removal of RCC metastases is relatively easy in general because the tumor is well demarcated and hard, and bleeding is not so great. In addition, surgery has a clear advantage in rapid decrease of peritumoral edema after tumor removal. Treatment strategy for metastatic brain tumors from RCC depends on tumor size (less or more than 2 cm), toleration of general anesthesia, number of tumors, and presence of symptomatic peritumoral edema.
References
Flickinger JC, Kondziolka D, Lunsford LD et al (1994) A multi-institutional experience with stereotactic radiosurgery for solitary brain metastasis. Int J Radiat Oncol Biol Phys 28:797–802
Mehta MP, Rozental JM, Levin AB et al (1992) Defining the role of radiosurgery in the management of brain metastases. Int J Radiat Oncol Biol Phys 24:619–625
Shuto T, Fujino H, Asada H et al (2003) Gamma knife radiosurgery for metastatic tumours in the brain stem. Acta Neurochir (Wien) 145:755–760. doi:10.1007/s00701-003-0034-1
Shuto T, Fujino H, Inomori S et al (2004) Repeated gamma knife radiosurgery for multiple metastatic brain tumours. Acta Neurochir (Wien) 146:989–993. doi:10.1007/s00701-004-0306-4
Saitoh H (1981) Distant metastasis of renal adenocarcinoma. Cancer 48:1487–1491
Halperin EC, Harisiadis L (1983) The role of radiation therapy in the management of metastatic renal cell carcinoma. Cancer 51:614–617
Onufrey V, Mohiuddin M (1985) Radiation therapy in the treatment of metastatic renal cell carcinoma. Int J Radiat Oncol Biol Phys 11:2007–2009
Cannady SB, Cavanaugh KA, Lee SY et al (2004) Results of whole brain radiotherapy and recursive partitioning analysis in patients with brain metastases from renal cell carcinoma: a retrospective study. Int J Radiat Oncol Biol Phys 58:253–258. doi:10.1016/S0360-3016(03)00818-6
Amendola BE, Wolf AL, Coy SR et al (2000) Brain metastases in renal cell carcinoma: management with gamma knife radiosurgery. Cancer J 6:372–376
Hernandez L, Zamorano L, Sloan A et al (2002) Gamma knife radiosurgery for renal cell carcinoma brain metastases. J Neurosurg 97(5 Suppl):489–493. doi:10.3171/jns.2002.97.supplement5.0489
Hoshi S, Jokura H, Nakamura H et al (2002) Gamma-knife radiosurgery for brain metastasis of renal cell carcinoma: results in 42 patients. Int J Urol 9:618–626. doi:10.1007/s11060-007-9458-4
Mori Y, Kondziolka D, Flickinger JC et al (1998) Stereotactic radiosurgery for brain metastasis from renal cell carcinoma. Cancer 83:344–353. doi:10.1002/(SICI)1097-0142(19980715)83:2<344:AID-CNCR19>3.0.CO;2-T
Muacevic A, Kreth FW, Mack A et al (2004) Stereotactic radiosurgery without radiation therapy providing high local tumor control of multiple brain metastases from renal cell carcinoma. Minim Invasive Neurosurg 47:203–208. doi:10.1055/s-2004-818511
Noel G, Valery CA, Boisserie G et al (2004) LINAC radiosurgery for brain metastasis of renal cell carcinoma. Urol Oncol 22:25–31. doi:10.1016/S1078-1439(03)00104-2
Schoggl A, Kitz K, Ertl A et al (1998) Gamma-knife radiosurgery for brain metastases of renal cell carcinoma: results in 23 patients. Acta Neurochir (Wien) 140:549–555. doi:10.1007/s007010050139
Sheehan JP, Sun MH, Kondziolka D et al (2003) Radiosurgery in patients with renal cell carcinoma metastasis to the brain: long-term outcomes and prognostic factors influencing survival and local tumor control. J Neurosurg 98:342–349. doi:10.3171/jns.2003.98.2.0342
Wowra B, Siebels M, Muacevic A et al (2002) Repeated gamma knife surgery for multiple brain metastases from renal cell carcinoma. J Neurosurg 97:785–793. doi:10.3171/jns.2002.97.4.0785
Shuto T, Inomori S, Fujino H et al (2006) Gamma knife surgery for metastatic brain tumors from renal cell carcinoma. J Neurosurg 105:555–560. doi:10.3171/jns.2006.105.4.555
Shuto T, Matusnaga S, Inomori S et al (2008) Efficacy of gamma knife surgery for control of peritumoral edema associated with metastatic brain tumors. J Neurol Neurosurg Psychiatry 79:1061–1065. doi:10.1136/jnnp.2007.130534
Bindal RK, Sawaya R, Leavens ME et al (1993) Surgical treatment of multiple brain metastases. J Neurosurg 79:210–216. doi:10.3171/jns.1993.79.2.0210
Mandell L, Hilaris B, Sullivan M et al (1986) The treatment of single brain metastasis from non-oat cell lung carcinoma. Surgery and radiation versus radiation therapy alone. Cancer 58:641–649
Patchell RA, Tibbs PA, Walsh JW et al (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322:494–500
Goyal LK, Suh JH, Reddy CA et al (2000) The role of whole brain radiotherapy and stereotactic radiosurgery on brain metastases from renal cell carcinoma. Int J Radiat Oncol Biol Phys 47:1007–1012. doi:10.1016/S0360-3016(00)00536-8
Brown PD, Brown CA, Pollock BE et al (2002) Stereotactic radiosurgery for patients with “radioresistant” brain metastases. Neurosurgery 51:656–667. doi:10.1227/01.NEU.0000023713.44940.20
Serizawa T, Iuchi T, Ono J et al (2000) Gamma knife treatment for multiple metastatic brain tumors compared with whole-brain radiation therapy. J Neurosurg 93(Suppl 3):32–36. doi:10.3171/jns.2000.93.supplement3.0032
Yang CC, Ting J, Wu X et al (1998) Dose volume histogram analysis of the gamma knife radiosurgery treating twenty-five metastatic intracranial tumors. Stereotact Funct Neurosurg 70(Suppl 1):41–49. doi:10.1159/000056405
Yamamoto M, Ide M, Nishio S et al (2002) Gamma knife radiosurgery for numerous brain metastases: Is this a safe treatment? Int J Radiat Oncol Biol Phys 53:1279–1283. doi:10.1016/S0360-3016(02)02855-9
Koutras AK, Krikelis D, Alexandrou N et al (2007) Brain metastasis in renal cell cancer responding to sunitinib. Anticancer Res 27:4255–4257
Valcamonico F, Ferrari V, Amoroso V et al (2009) Long-lasting successful cerebral response with sorafenib in advanced renal cell carcinoma. J Neurooncol 91:47–50. doi:10.1007/s11060-008-9676-4
Ikushima H, Tokuuye K, Sumi M et al (2000) Fractionated stereotactic radiotherapy of brain metastases from renal cell carcinoma. Int J Radiat Oncol Biol Phys 48:1389–1393. doi:10.1016/S0360-3016(00)00804-X
Higuchi Y, Serizawa T, Nagano O et al (2009) Three-staged stereotactic radiotherapy without whole brain irradiation for large metastatic brain tumors. Int J Radiat Oncol Biol Phys 74:1543–1548. doi:10.1016/j.ijrobp.2008.10.035
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shuto, T., Matsunaga, S., Suenaga, J. et al. Treatment strategy for metastatic brain tumors from renal cell carcinoma: selection of gamma knife surgery or craniotomy for control of growth and peritumoral edema. J Neurooncol 98, 169–175 (2010). https://doi.org/10.1007/s11060-010-0170-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-010-0170-4