Abstract
To determine the safety and tolerability of IV and oral levetiracetam monotherapy for seizures in brain tumor patients following resection. Brain tumor patients undergoing neurosurgery with ≥1 seizure within the preceding month prior to surgery were enrolled to receive intravenous levetiracetam for a minimum of 48 h, transitioned to oral levetiracetam at the same dose, and followed for 1-month after discharge. Patients were assessed daily in the hospital, provided with a seizure diary, and supplied with 30 days of levetiracetam upon discharge. Study patients were telephoned weekly to assess their cognitive status and seizure frequency. Of the 17 patients enrolled, the baseline seizure types were tonic clonic, partial, and complex partial with secondary generalization. The most common type of tumor was glioblastoma multiforme. Levetiracetam was well tolerated with no medication discontinuation during the study period. Adverse effects reported were somnolence, nausea/vomiting, headache, and insomnia. Eleven patients were evaluable for TICS scores (64.7%) with an average score of 33.3. Two patients were deemed to be cognitively impaired (18.2%). Eleven of twelve patients (91.7%) that completed the study period achieved a ≥50% reduction in their number of seizures. A total of 92 drug interactions were avoided (P = 0.0016) with dexamethasone, acetaminophen, and fentanyl being the most common. Levetiracetam monotherapy was found to be safe and tolerable in this patient population. Nearly all patients achieved a ≥50% reduction in seizure frequency post-op with levetiracetam monotherapy. Levetiracetam also has the potential for less drug interactions compared to phenytoin in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Seizures in patients with primary and metastatic brain tumors occur commonly. In the United States in 2000, an estimated 359,000 persons were living with a diagnosis of primary brain and central nervous system tumors, and the prevalence rate for these tumors was estimated to be 130.8 per 100,000 [1]. In 2004, more than 225,000 patients were newly diagnosed with primary and/or metastatic brain tumors, and this number has continued to climb annually [2–4]. The incidence of seizures varies from 20 to 70% depending on the type of tumor, with seizures being the presenting symptom of brain tumors in approximately 10–40% of this patient population [5, 6].
Treatment of seizures related to tumors has often been associated with an inadequate response that may be due to tumor growth, anticonvulsant resistance, and pharmacokinetic or pharmacodynamic drug interactions. Typical anticonvulsants (phenytoin, carbamazepine, phenobarbital, and valproic acid) have been associated with a large spectrum of drug–drug interactions. The aromatic anticonvulsants (phenytoin, carbamazepine, phenobarbital, and primidone) have been well known inducers of drug metabolism, which markedly reduces the effective serum concentrations of many of the chemo- and nonchemo-therapeutic agents used in the management of brain tumor patients.
Medication side effects and the sequelae of brain tumors complicate treatment of seizures in these patients. In addition to an inadequate response, brain tumor patients receiving antiepileptic medications experience an increased incidence of certain side effects, especially drug rashes. Clinical studies have reported that more than 20% of brain tumor patients treated with phenytoin and carbamazepine developed morbilliform rashes, with a small percentage progressing to Stevens-Johnson syndrome [7, 8]. The American Academy of Neurology recently reported that 23.8% of all brain tumor patients taking anticonvulsants will experience side effects severe enough to warrant a change in or discontinuation of therapy [9–14]. Nonetheless, these patients are often treated with the older, conventional antiepileptic medications (phenytoin, carbamazepine, and valproic acid) that require significant monitoring for therapeutic serum concentrations, can cause drug toxicity, and exhibit significant drug–drug interactions.
Levetiracetam, a relatively new antiepileptic medication, is currently indicated for adjunctive therapy in the treatment of partial onset seizures in adults and children 4 years of age and older with epilepsy. To date, clinical studies with levetiracetam have demonstrated the following: no serum drug concentration monitoring required, limited side effect profile, lack of known drug interactions, and 1:1 intravenous to oral conversions. Therefore, levetiracetam may be a very useful, alternative antiepileptic in patients with brain tumors following resection.
Methodology
Rationale for the study
This prospective, open label study proposed to assess the use of levetiracetam as monotherapy in the treatment of 20 brain tumor patients with seizures and document their clinical outcomes. Levetiracetam is being utilized as monotherapy in brain tumor patients; although, to date, there have only been a few reports of levetiracetam use (adjunctive and monotherapy) in this patient population. Methodist University Hospital is a center of excellence in the neurological sciences and is one of the top neurosurgical institutions in the United States. Since there is a large number of new brain tumors diagnosed at this institution yearly, this site provides a unique patient population to prospectively analyze levetiracetam monotherapy in patients with brain tumors following resection and seizures.
Objectives
The overall aim of this study was to determine the safety and tolerability of IV and oral levetiracetam, as monotherapy, for seizures in brain tumor patients following resection through adverse effect monitoring and cognitive functioning/impairment assessments (TICS—telephone interview for cognitive status). Secondary objectives were to evaluate the efficacy of IV and oral levetiracetam, as monotherapy, in brain tumor patients following neurosurgery and seizures, defined as a ≥50% reduction in baseline seizure activity or being seizure free, and to assess the number of possible drug interactions avoided through the use of IV and oral levetiracetam monotherapy in comparison with phenytoin as a theoretical therapeutic substitution for levetiracetam.
Study population
Through a database search performed by Health Information Management, an estimated 380 brain tumors are diagnosed at Methodist University Hospital each year. Of the estimated 380 brain tumor patients, 10–40% of these patients have concomitant seizures. A total of 20 patients with a diagnosis of a brain tumor that is operable and who have a history of seizures (≥1 witnessed seizure) were included in this study on an intention to treat basis. Patients were selected by a neurosurgery investigator based on the aforementioned diagnoses. Patients were screened for inclusion and exclusion criteria and had informed consent initiated by one of the IRB (Institutional Review Board) approved investigators (see Tables 1 and 2). This study was approved by the IRB.
Treatment
Baseline evaluations (prior to levetiracetam administration)
After patients were evaluated for enrollment according to study criteria and had signed voluntary informed consent, the following baseline information was collected: demographic data (age, race, gender); patient weight and height; medical, social (smoking, alcohol, illicit substances), and medication history.
Levetiracetam administration
If treated previously with other antiepileptic agents, patients were converted to levetiracetam monotherapy and all other agents discontinued prior to surgery. Following standard clinical practice, no washout period occurred prior to levetiracetam administration to prevent a potential increase in the risk of seizures during the transition period.
Within 6 h following surgery, patients previously untreated with levetiracetam were administered levetiracetam 500 mg IV twice daily as monotherapy for a minimum of 48 h (recommended starting dose per FDA approved package labeling). Patients receiving levetiracetam prior to surgery or as an outpatient received the same preoperative regimen as initial therapy. Dosage titrations of the IV formulation were made per physician, based on patient response to therapy and seizure frequency.
Patients were then converted to the same dose and frequency of oral levetiracetam, when tolerated, but not <48 h after IV levetiracetam initiation. Intravenous and oral doses were titrated on an individual basis by 500 mg/day increments per physician in response to patient’s seizure activity up to a maximum dose of 3,000 mg/day. Patients that required >3,000 mg/day of levetiracetam for seizure control or had intolerance to levetiracetam dose escalation were deemed candidates for concomitant therapy with another antiepileptic(s).
Patients were provided with a 1-month supply of levetiracetam oral tablets upon discharge from the hospital. Outpatient oral dosage titrations were made per physician based on patient response to therapy and seizure frequency. One week prior to discontinuation from the study, the primary physician was notified to determine the necessity of antiepileptics beyond the 4 week study period.
Daily assessments and procedures (during levetiracetam therapy)
While in the hospital, each patient was evaluated daily by an investigator to determine efficacy, safety, and tolerability of levetiracetam dosing, including the number and type of seizures and adverse effects.
As an outpatient, each patient was asked to record daily in a seizure diary the number and a description of seizures experienced. Each patient was also asked to record the schedule and daily doses of levetiracetam administered as an outpatient.
Weekly follow-up contacts
Upon discharge from the hospital on levetiracetam, patients had weekly telephone follow-up performed by a study investigator. The safety, tolerability, and efficacy of levetiracetam monotherapy were determined based on the reported information from each patient’s seizure diary. Adverse effects of levetiracetam were evaluated and recorded weekly and a questionnaire called the TICS was administered weekly to assess each patient’s cognitive function and mental status.
Statistical considerations and data analysis
All data was collected on a standardized data collection form by study investigators. Data was entered into a Microsoft Excel spreadsheet to group data for analysis. Demographic and baseline information were summarized. Descriptive statistics for continuous variables included N, mean, and range.
Mean and range were used to evaluate patient age, pre-op seizure frequency, and TICS scores. Descriptive analysis was performed on seizure type, antiepileptics prior to surgery, brain tumor type, brain tumor location, and medication adverse effects.
The secondary objectives evaluated the efficacy of IV and oral levetiracetam, as monotherapy, for seizures in brain tumor patients following resection and identified the number of drug interactions avoided through the use of IV and oral levetiracetam monotherapy. Per national guidelines, efficacy of antiepileptic treatment was determined by patients being seizure free or having a ≥50 reduction in their number of seizures. To assess the efficacy of levetiracetam monotherapy, a seizure type and quantitative seizure history, for 1-month prior to study enrollment, were documented. This baseline assessment was compared to the number and type of seizures each patient had post-surgically while being treated with levetiracetam monotherapy. Drug interactions avoided were determined by utilizing Micromedex Drug-Reax® system. Each patient’s medication profile was assessed daily while in the hospital and weekly after discharge for drug interactions with levetiracetam and compared to the potential drug interactions with phenytoin, as if it had been prescribed. The drug interactions avoided were attributed to the potential number of drug interactions phenytoin had with each patients’ medication profile compared to the actual drug interactions with levetiracetam. Drug interactions avoided were analyzed with paired student t test.
Results
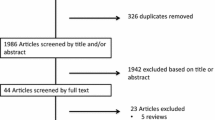
Enrollment began on August 9, 2007, and ended on November 1, 2008. Of the 20 patients anticipated for inclusion in this study, only 17 patients were enrolled for evaluation. Recruitment was ceased at the request of UCB Pharma due to difficulties in identifying and enrolling patients within the levetiracetam study protocol. Demographics of these patients were as follows: 8 male, 9 female; 12 Caucasian, 5 African American. The mean age of these patients was 56 y/o (range 27–77 y/o). The mean number of seizures pre-op per patient was 3.5 (range 1–22).
The types of seizure at baseline for patients enrolled are listed in Table 3. Most patients were receiving antiepileptic medications prior to study enrollment (see Table 4). A number of different types of tumors were identified upon surgery, but the most common type (glioblastoma multiforme) occurred in 7 patients (41.2%) (see Table 5). Tumor location also varied among the study population with 13 patients having a left-sided tumor and 4 patients having a right-sided tumor (see Table 6). Of the patients enrolled, 16 of 17 patients had gross total resections of their tumors.
Primary objective
All patients continued levetiracetam monotherapy throughout the entire study period with no decreases in dose due to adverse effects. A total number of 6 adverse effects were reported by levetiracetam study patients with somnolence being the most commonly reported (see Table 7). One patient did develop aphasia but this was deemed to be a consequence of disease progression and not an adverse effect of levetiracetam. Due to the effects of other antiepileptic medications on cognitive status, a TICS evaluation was performed on study patients to determine if levetiracetam had any adverse effect on cognitive status. Eleven patients (64.7%) were available for TICS evaluations. Two patients did not achieve the minimum score of 31 (18.2%) and were deemed cognitively impaired. All other patients achieved a score of 31 on each of their assessments (see Table 8).
Secondary objectives
Seizure control
Twelve patients completed the entire 4 week follow-up for determining a ≥50% reduction in seizure activity. Eleven (91.7%) of these twelve patients achieved this degree of seizure control with 10/12 patients achieving seizure freedom (83%) during the study period. Of the 17 patients enrolled, two patients had at least 1 seizure during the study period (see Table 9). The first of these patients had 2 tonic clonic seizures prior to surgery and 1 tonic clonic seizure during the 1st week of outpatient follow-up. The maintenance dose of levetiracetam was increased from 1,000 to 1,500 mg po daily. No further seizures occurred during the study period.
The second of these patients had 1 tonic clonic seizure prior to surgery and two seizures during the post-op study period. The first was a tonic clonic seizure hours after surgery was completed that was averted with lorazepam 2 mg IV. No levetiracetam dosage changes were made at that time. The second seizure was a partial seizure that occurred during the 4th week of follow-up. Per the clinic’s recommendation, the patient was advised to increase the levetiracetam dose by 500 mg that day to a total of 1,500 mg daily. Both of these patients had gross total resections of an oligodendroglioma. All other patients in the study were maintained on levetiracetam 500 mg po twice daily and had no further seizures while on monotherapy.
Drug–drug interactions
A significant number of potential drug interactions were avoided with the use of levetiracetam as compared to phenytoin. A total number of 92 drug interactions (62 inpatient, 30 outpatient) were avoided with the use of levetiracetam as compared to if patients had received phenytoin (P = 0.0016). The most common potential drug–drug interactions avoided were phenytoin/dexamethasone, phenytoin/acetaminophen, and phenytoin/fentanyl (see Table 10).
Discussion
Potential role for levetiracetam in brain tumor patients with seizures
Several studies have investigated the use of levetiracetam in various patient populations. VanLandingham and Radtke [15] examined the efficacy of levetiracetam in 38 patients with primary brain or metastatic tumors and uncontrolled partial seizures. Seizure frequency, along with side effects of the antiepileptic agents administered, was assessed at each patient visit. Initial doses of levetiracetam were 500 mg twice daily for 1 week and increased based on individual patient response and side effects. Fourteen patients received levetiracetam concurrently with phenytoin, at doses ranging from 200 to 400 mg/day. Mean and median doses of levetiracetam within the study were 1,826 and 1,750 mg/day, respectively. Follow-up between 2 and 18 months found 8 patients to be seizure free and 7 patients with a >90% reduction in their number of seizures. Six patients exhibited no significant improvement with 1 patient developing worsening of seizures. Three patients were maintained on levetiracetam monotherapy, one of which became seizure free. Of the 38 patients treated in this study, three patients required dose reductions or termination due to excessive sedation [15].
In 2002, Siddiqui et al. [16] published an abstract that reviewed levetiracetam therapy in 49 brain tumor patients. Levetiracetam was administered to 41 (23 female, 18 male; aged 24–78) of these patients for a minimum of 6 months. Two patients (4%) had no history of seizures, 32 (78%) had seizures post-surgery, and 23 (57%) had seizures upon presentation. Levetiracetam therapy was initiated in patients for seizure prophylaxis, with suboptimal seizure control, with sedation and fatigue adverse effects on previous antiepileptics, for neutropenia on previous antiepileptics, and on chemotherapy protocols that prohibited enzyme-inducing medications. Of these 41 patients, sixteen received levetiracetam monotherapy for a duration of 6–18 months. A total of 21 patients were seizure free, 11 patients had moderate seizure reduction, and 2 patients had no improvement. Adverse effects were limited to mood disturbances (drug discontinuation in 1 patient), fatigue, or sedation [16].
Within the 2 previously described studies, a significant number of brain tumor patients received levetiracetam for documented seizures lending to the design of our prospective evaluation of levetiracetam in brain tumor patients. Several of these patients were able to be maintained on levetiracetam monotherapy throughout the duration of their study periods. Although these 2 studies were conducted for significantly longer periods of time, similar results were discovered in seizure reductions or freedom and limited adverse effects that required dose adjustments or discontinuation compared to our prospective evaluation.
In a 2004 retrospective evaluation in Epilepsia, Penovich et al. [17] reviewed the efficacy of newer antiepileptics and chemotherapy medications in central nervous system (CNS) neoplasms that were responsible for new onset, adult seizures. Antiepileptic medications were chosen based on avoidance of drug interactions with chemotherapeutic agents being administered. Forty patients aged 18–77 with multiple types of tumors were included. Levetiracetam was administered as monotherapy in 22 patients and polytherapy in 5 patients. Gabapentin, oxcarbazepine, topiramate, and phenytoin were the other antiepileptics used as mono- and polytherapy. Of patients treated with levetiracetam, 77.8% had seizure freedom or experienced only simple partial seizures [17].
Levetiracetam was theorized to be an effective alternative antiepileptic in patients with CNS neoplasms due to its inability to invoke drug–drug interactions. Decreased serum concentrations or altered metabolism with chemotherapeutic agents can negatively effect tumor treatment when potent cytochrome inducing agents such as phenytoin, carbamazepine, and phenobarbital are utilized. Optimal effects and outcomes can be achieved with recommended dosing of chemotherapeutic agents when levetiracetam has been prescribed in lieu of phenytoin. Although our study analyzed the avoidance of drug–drug interactions, none of the patients were documented to have received chemotherapeutic agents during the study period. The potential for avoiding other vital drug–drug interactions with drugs such as dexamethasone, prescribed to decrease vasogenic edema and swelling, was significantly reduced with the use of levetiracetam instead of phenytoin in our study patients.
Another 2004 retrospective study in Epilepsia by Larson et al. [18] evaluated the efficacy and tolerability of levetiracetam in brain tumor patients with seizures. Fifteen patients (aged 24–76) with primary or metastatic tumors that had experienced a minimum of one simple partial, complex partial, or generalized seizure were included. The mean duration of therapy was 7.25 months on levetiracetam doses that ranged from 500 to 2,000 mg/day (mean = 1,016 mg/day). Six patients received levetiracetam as monotherapy with 9 patients receiving 1–3 concurrent antiepileptics. After a minimum follow-up of 3 months, all 6 patients receiving levetiracetam monotherapy were seizure free. Of the 9 patients receiving levetiracetam as adjunctive treatment, two had improved seizure control and 7 had no change in seizure control. Behavioral adverse effects requiring levetiracetam discontinuation occurred in 2 patients and required 1 patient to have the levetiracetam dose reduced [18].
In a 2005 Neurology supplement, Stevens et al. [19] reviewed 278 medical charts for patients with various brain tumor types treated with levetiracetam over a 3 year period. Each chart was reviewed for documentation of brain tumor type, seizure frequency, and drug therapy adverse effects. Levetiracetam was found to have a >50% reduction in seizure activity in 60% of patients. Of these patients, 70% were treated with levetiracetam as monotherapy. Only 10 patients (3.5%) required dosage reductions or discontinuation of levetiracetam due to behavioral-related adverse effects. The most frequently documented adverse effects were somnolence and fatigue [19].
As with our study, multiple brain tumor types and various types of seizures were analyzed in these two studies. Levetiracetam monotherapy was effective in these small populations, regardless of seizure type. No differences were stated in the ability of levetiracetam to be more effective in particular brain tumor types within these studies, but in our study, levetiracetam dosage increases were required in patients with an oligodendroglioma due to the occurrence of seizures. As discovered in the Stevens analysis, somnolence was the most common adverse effect in our study.
Historically, one of the major adverse effects and reasons for discontinuation of first generation antiepileptics has been alterations in cognitive function. In our study, we assessed each patient’s cognitive function weekly with the TICS. This simple test of global mental status was first validated as a tool for assessing cognitive function in the Alzheimer’s Disease population back in 1988 [20]. The TICS was discovered to be a reliable and valid alternative to the Mini Mental State Exam (MMSE) in a cross-sectional study of cognitive assessment in geriatric patients. Greater than 90% of cases that screened positive via the TICS also screened positive on the MMSE [21]. More recently, a TICS evaluation of patient cognitive function and outcomes, when exposed to phenytoin 14 days and 3 months after subarachnoid hemorrhage, was published in Stroke in 2005. Cognitive outcome testing with the TICS was stated as providing a sensitive method of detecting permanent disabilities and being highly predictive of cognition post subarachnoid hemorrhage [22]. We were able to employ the TICS evaluation tool to assess patients for declines in cognition during the 4 week follow-up period while on levetiracetam monotherapy. While location of tumor, degree of surgical debulking, and concomitant CNS altering medications were potential confounding factors, the TICS provided an objective measurement of cognitive changes within our patient population with data supporting its test–retest reliability [23].
Valeriano and Lane [24] retrospectively reviewed 25 adult patients treated with levetiracetam as monotherapy and presented their findings at the Meeting of the American Epilepsy Society in December 2005. These patients had a variety of seizure types including simple and complex partial seizures (with and without secondary generalization) and primary generalized seizures, including myoclonic seizures. Twenty-one of these patients had previously received one to six antiepileptics that were either ineffective or discontinued due to intolerable adverse effects. Initial treatment was levetiracetam 250 mg twice daily titrated to 500 mg twice daily after 1 week of therapy. All subsequent dosage titrations were dependent upon individual patient response and breakthrough seizures. Patients were followed for a minimum of 3 months up to >5 years (>1 year in 15 patients) [24].
Of the 25 patients, 21 had seizure freedom with levetiracetam monotherapy. The remaining 4 patients did have ≥50% decrease in seizure frequency although they did not achieve seizure freedom. Twenty-four patients were assessed utilizing the Global Clinical Impression Scale. A good or excellent rating was reported in 23 patients (95.8%) with the remaining patient reporting a fair rating. No adverse events were attributed to levetiracetam therapy in this retrospective review [24].
Two retrospective analyses were published in the Journal of Neuro-Oncology in 2006 [25] and 2007 [26] that included either primary and metastatic brain tumor patients or only metastatic brain tumor patients, respectively. Levetiracetam was utilized as monotherapy in 8/41 patients [25] and 6/13 patients [26] within each of these studies. In the 2006 analysis, levetiracetam reduced the median seizure frequency from 1 seizure per week at baseline to 0 per week when prescribed as adjunctive or monotherapy. A total of 59% of patients were documented to have achieved complete seizure control. Levetiracetam was well tolerated in this patient population with the most common adverse effect being somnolence in 37% of patients [25]. In the 2007 analysis, levetiracetam reduced the median seizure frequency from 1 ictal event every other day at baseline to 0 per week when prescribed as adjunctive or monotherapy. All patients had reductions of >50% in seizure frequency from their pre-levetiracetam baseline with a total of 77% achieving complete seizure control. The most common adverse effects discovered in this retrospective analysis was somnolence and headache in 23% of the population [26]. Both studies concluded that levetiracetam was effective and well tolerated in this patient population and could be considered as either an adjunctive or monotherapy antiepileptic [25, 26].
Although levetiracetam has been utilized effectively as a monotherapy antiepileptic in brain tumor patients, no study had been undertaken to prospectively analyze the safety and efficacy of both intravenous and oral levetiracetam in brain tumor patients with seizures. A recent publication by Rüegg et al. [27] described the use of weight-based dosing of intravenous levetiracetam in 50 critically ill patients. Of these patients, nine (18%) were diagnosed with a brain tumor. An initial dose of levetiracetam at 20 mg/kg body weight was administered intravenously with subsequent doses starting 6 h later at 15 mg/kg body weight. The mean duration of treatment with intravenous levetiracetam was 2.1 ± 1.22 days with a range of 1–5 days. Eighty-six percent of patients were either in status epilepticus (48%) or had an initial seizure (38%) prior to the initiation of levetiracetam. Twelve patients were administered levetiracetam as a first-line therapy with 11 becoming or remaining seizure free during the 7-day study period. The intravenous dosage form of levetiracetam was deemed both safe and effective in this broad, small population of patients [27].
Also, Chang et al. [28] retrospectively analyzed the seizure characteristics of 332 patients with low-grade gliomas following resection. Of these patients, 269 (81%) had experienced at least 1 seizure including generalized (33%), complex partial (16%), simple partial (22%), and combinations (29%). Cortical tumor location along with oligodendroglioma and oligoastrocytoma subtypes were more likely to be associated with seizures compared to deeper midline location and astrocytoma subtype (P = 0.017, P = 0.001). Pharmacoresistant seizures were present in 132 patients (49%) prior to surgery and most likely to be located in the temporal lobe and be simple partial in nature (P = 0.0089, P = 0.0005). The majority of patients became seizure free after surgery (67%), but other patients either experienced rare seizures (17%), meaningful improvement (8%), or no improvement/worsening (9%). Simple partial seizures (P = 0.004) and longer seizure history (P < 0.001) were more common in patients that had poor seizure control post-op. Gross total resections compared to subtotal resections or biopsies (OR 16, 95% CI 2.2–124, P = 0.0064) were predictors of improved seizure control post-op. Tumor progression was linked with seizure recurrence after patients had achieved initial seizure control post-operatively (P = 0.001) [28].
In our study population, patients were most likely to have a left-sided tumor in various lobes with the majority of tumors being identified as a GBM subtype. The majority of study patients achieved seizure freedom but one type of seizure was not seen more than another. No determinations could be made in seizure control for patients that had a gross total resection (16 patients) versus a biopsy (1 patient).
Milligan et al. [29] recently published a retrospective analysis of monotherapy with levetiracetam or phenytoin in supratentorial neurosurgical patients. Although only a small percentage of this patient population had seizures pre-operatively (levetiracetam group—31%, phenytoin group—21%), both intervention groups successfully prevented seizures within 7 days of surgery and had similar rates of patients developing epilepsy at 12 months (P = 0.17, P = 0.34, respectively). Adverse drug reactions during hospitalization that required antiepileptic therapy changes were less among patients in the levetiracetam group (P < 0.001). A larger percentage of patients were also maintained on levetiracetam monotherapy (64%) versus phenytoin monotherapy (26%) throughout the study period (P = 0.03). Both interventions had a low risk of early postoperative seizures and a moderate risk of developing epilepsy during the study. Levetiracetam was responsible for a significantly less number of adverse drug reactions and less discontinuations of medication compared to phenytoin during the 12-month follow-up [29].
In contrast to our study, Milligan actively compared monotherapy treatment with levetiracetam versus phenytoin in neurosurgical patients regardless of a history of pre-operative seizures. Our study design included only patients with pre-operative seizures with no comparator group. Even though the amount of published literature is limited in this patient population, Milligan et al. [29] noted that levetiracetam monotherapy was equally efficacious to phenytoin in neurosurgical patients for the prevention of seizures. These researchers had only 1 patient that received levetiracetam and required discontinuation due to adverse effects. Multiple patients required discontinuation of phenytoin due to adverse effects in this study [29]. A low incidence of adverse drug reactions occurred in our levetiracetam monotherapy study with no patients requiring medication discontinuation.
Finally, a similarly designed phase II pilot study was recently published in the Journal of Neuro-Oncology that described the safety and feasibility of switching from phenytoin to levetiracetam monotherapy for glioma-related seizure control following craniotomy [30]. As with our study, patients were required to have at least 1 seizure at baseline prior to the initiation of antiepileptics, but contrary to being a prospective levetiracetam study as with our design, this prospective pilot study randomized 29 patients over a 13-month period in a 2:1 ratio of levetiracetam to phenytoin. Initiating levetiracetam within 24 h of surgery varied slightly from our design of beginning intravenous levetiracetam in the first 6 h following neurosurgery. At 6 month follow-up, 87% of levetiracetam patients were seizure free compared to 75% of phenytoin patients. This rate of seizure freedom was comparable with our results of 83% of patients having seizure freedom (10/12 patients) at the end of study follow-up. Adverse effects reported with levetiracetam were similar with the most common in this study being depression (7%), lack of energy or strength (20%), insomnia (40%), and mood instability (7%). From this data, the authors concluded that patients with supratentorial gliomas having craniotomies could be safely transitioned from phenytoin to levetiracetam as a monotherapy antiepileptic [30].
Limitations
This study had several limitations. Study enrollment was a challenge with the unique patient population. Although the goal was to enroll 20 patients, the study was ceased early by the manufacturer. We had a small sample size of 17 patients which was not powered to detect differences among the population. This study was open label with no randomization or a placebo-controlled group. Sixteen of the study patients underwent gross total resection of their brain tumor. Potentially, the epileptogenic source may have been removed with this surgical procedure or had its epileptogenic capability greatly reduced negating the necessity for antiepileptic therapy. However, gross total resection is a confounding variable in all post-neurosurgery antiepileptic studies. Follow-up proved to be difficult in reaching patients after discharge from the hospital leading to deficiencies in documentation for the entire study period. Baseline cognition scores were unable to be obtained to detect deterioration in cognitive status over time while receiving levetiracetam. Although a valid evaluation tool for cognitive function, the TICS was unable to be performed in all patients and led to deficiencies in documentation when assessing each patient for changes in cognition. Some adverse effects were dependent on patient self-reporting and may not have represented the actual number experienced within this study period.
Conclusion
Levetiracetam, intravenous and oral, demonstrated both safety and efficacy for post-surgical brain tumor patients with seizures. The medication was well tolerated throughout the study period with no discontinuations. Nearly all patients achieved a ≥50% reduction in the number of seizures post-operatively compared to pre-operatively while in this study. A significant number of drug interactions were potentially avoided with the use of levetiracetam instead of phenytoin in this patient population. Although larger, placebo-controlled, clinical trials are warranted, levetiracetam appears to be an efficacious, monotherapy agent in neurosurgical brain tumor patients with seizures.
References
Central Brain Tumor Registry of the United States (2007–08) CBTRUS, Chicago
Posner JB (1992) Management of brain metastases. Rev Neurol (Paris) 148:477–487
Landis SH, Murray T, Bolden S, Wingo PA (1999) Cancer statistics, 1999. CA Cancer J Clin 49:8–31
Davis FG, Kupelian V, Freels S, McCarthy B, Surawicz T (2001) Prevalence estimates for primary brain tumors in the United States by behavior and major histology groups. Neuro-Oncology 3(3):152–158
Villemure JG, de Tribolet N (1996) Epilepsy in patients with central nervous system tumors. Curr Opin Neurol 9(6):424–428
Wen P (1997) The diagnosis and management of patients with brain tumors. In: Loeffler JS, Black PM (eds) Cancer of the nervous system. Blackwell Scientific, Boston, pp 106–127
Moots PL, Maciunas RJ, Eisert DR, Parker RA, Laporte K, Abou-Khalil B (1995) The course of seizure disorders in patients with malignant gliomas. Arch Neurol 52:717–724
Mamon HJ, Wen PY, Burns AC, Loeffler JS (1999) Allergic skin reactions to anticonvulsant medications in patients receiving cranial radiation therapy. Epilepsia 40:341–344
Mahaley MS, Dudka L (1981) The role of anticonvulsant medications in the management of patients with anaplastic gliomas. Surg Neurol 16:399–401
Hagen NA, Cirrincione C, Thaler HT et al (1990) The role of radiation therapy following resection of single brain metastasis from melanoma. Neurology 40:158–160
Hung S, Hilsenbeck S, Feun L (1999) Seizure prophylaxis with phenytoin in patients with brain metastases. Proc Am Soc Clin Oncol 10:A1151
Moots PL, Maciunas RJ, Eisert DR et al (1995) The course of seizure disorders in patients with malignant gliomas. Arch Neurol 52:717–724
Glantz MJ, Cole BF, Friedberg MH et al (1996) A randomized, blinded, placebo-controlled trial of divalproex sodium prophylaxis in adults with newly diagnosed brain tumors. Neurology 46:985–991
Forsyth PA, Weaver S, Fulton D et al (2003) Prophylactic anticonvulsants in patients with brain tumour. Can J Neurol Sci 30(2):89–90
VanLandingham KE, Radtke RA (2002) Use of levetiracetam in patients with brain tumors and intractable partial epilepsy. Epilepsia 43(7):202
Siddiqui F, Wen P, Dworetzky B, Cabello D, Broomfield EB (2002) Use of levetiracetam in patients with brain tumors. Epilepsia 43(7):297
Penovich PE, Dickens DL, Gates JR et al (2004) Treating seizures due to brain neoplasms: rational new choices. Epilepsia 45(7):311
Larson SE, Sirven JI, Drazkowski JF, Zimmerman RS (2004) Efficacy and tolerability of levetiracetam in patients with brain tumors and seizures. Epilepsia 45(7):124
Stevens GHJ, Vogelbaum MA, Suh JH, Peereboom DM, Barnett GH (2005) Levetiracetam use in brain tumor patients. Neurology 64(1):A47–A48
Brandt J, Spencer M, Folstein M (1988) The telephone interview for cognitive status. Neuropsychiatr, Neuropsychol Behav Neurol 1(2):111–117
Ferrucci L, Del Lungo I, Guralnik JM et al (1998) Is the telephone interview for cognitive status a valid alternative in persons who cannot be evaluated by the mini mental state examination? Aging 10(4):332–338
Naidech AM, Kreiter KT, Janjua N et al (2005) Phenytoin exposure is associated with functional and cognitive disability after subarachnoid hemorrhage. Stroke 36:583–587
Sanchez CE, Ogilvy CS, Carter BS (2007) Outcomes studies in cerebrovascular neurosurgery. Neurosurg Focus 22(3):1–21
Valeriano JP, Lane CL (2005) Clinical experience with levetiracetam monotherapy in the treatment of epilepsy. Epilepsia 46(8):191
Newton HB, Goldlust SA, Pearl D (2006) Retrospective analysis of the efficacy and tolerability of levetiracetam in brain tumor patients. J Neurooncol 78(1):99–102
Newton HB, Dalton J, Goldlust S, Pearl D (2007) Retrospective analysis of the efficacy and tolerability of levetiracetam in patients with metastatic brain tumors. J Neurooncol 84(3):293–296
Rüegg S, Naegelin Y, Hardmeier M, Winkler DT, Marsch S, Fuhr P (2008) Intravenous levetiracetam: treatment experience with the first 50 critically ill patients. Epilepsy Behav 12:477–480
Chang EF, Potts MB, Keles GE et al (2008) Seizure characteristics and control following resection in 332 patients with low-grade gliomas. J Neurosurg 108:227–235
Milligan TA, Hurwitz S, Bromfield EB (2008) Efficacy and tolerability of levetiracetam versus phenytoin after supratentorial neurosurgery. Neurology 71:665–669
Lim DA, Tarapore P, Chang E et al (2009) Safety and feasibility of switching from phenytoin to levetiracetam monotherapy for glioma-related seizure control following craniotomy: a randomized phase II pilot study. J Neurooncol 93(3):349–354
Acknowledgments
This research study was funded through a Young Investigator Research Grant provided by UCB Pharma.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Usery, J.B., Michael, L.M., Sills, A.K. et al. A prospective evaluation and literature review of levetiracetam use in patients with brain tumors and seizures. J Neurooncol 99, 251–260 (2010). https://doi.org/10.1007/s11060-010-0126-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-010-0126-8