Abstract
In colorectal cancer and breast cancer a high TIMP-1 level has been shown to correlate with a shorter overall patient survival and it has been suggested that TIMP-1 is involved in tumour invasion, proliferation and apoptosis in different types of cancers. TIMP-1 is known to be expressed in gliomas but whether TIMP-1 is a prognostic marker in gliomas has not previously been investigated. In the present study, the TIMP-1 expression was investigated immunohistochemically in 112 formalin-fixed paraffin embedded astrocytomas and related to tumour grade and overall patient survival by scoring the TIMP-1 immunoreactivity of both tumour cells and blood vessels. Moreover, TIMP-1 in situ hybridisation was performed on ten of the glioblastomas. In the vast majority of the tumours TIMP-1 protein was expressed in both tumour cells and blood vessels. In situ hybridisation for TIMP-1 mRNA on glioblastomas confirmed the immunohistochemical expression of TIMP-1. The percentage of TIMP-1 positive tumour cells and blood vessels as well as the staining intensity varied between tumours of the same grade, but the total staining score increased with tumour grade. The multivariate Cox regression test showed that glioblastoma patients with the lowest TIMP-1 expression had a significantly longer overall survival (HR (95% CI) = 3.2 (1.5–6.7), P = 0.004) when compared to the patients with higher TIMP-1 protein expression. In conclusion, this study showed that low TIMP-1 immunohistochemical expression predicts longer overall survival in glioblastoma patients, suggesting a role for TIMP-1 as a biomarker in glioblastoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Matrix metalloproteinases (MMPs) and their inhibitors (TIMPs) are known for their role in remodelling of the extracellular matrix (ECM), thus playing important roles in both tumour invasion and metastasis [1, 2]. Among the four known TIMPs characterised so far, most focus has been on TIMP-1. TIMP-1 is a naturally occurring inhibitor of most of the MMPs, a family of zinc dependent endopeptidases essential for degrading components of the ECM. TIMP-1 is found either as a precursor, a free unbound protein, or in a complex with the active site of a MMP. It can also be found in a complex with proMMP9 and thereby prevent this pro-protein from becoming an active proteinase [3–5]. Over the years it has become clear that TIMP-1 is not only a MMP inhibitor but more likely a multipotent protein with other important functions in cancer as well. It has thus been suggested that TIMP-1 may stimulate cell growth [6–9], regulate angiogenesis [10, 11] and inhibit apoptosis [12–15].
Recent studies have shown that high levels of TIMP-1 in both plasma and tumour are associated with a poor prognosis in breast cancer [16–18], colorectal cancer [19], gastric cancer [20, 21] and ovarian cancer [22], indicating that TIMP-1 contribute to the progression of different types of cancer. Only a few studies on the expression of TIMP-1 in astrocytomas are published showing however different results. An immunohistochemical study on astrocytomas thus indicated that TIMP-1 expression in anaplastic astrocytomas and glioblastomas was almost similar [23], while a Western Blot study found the highest TIMP-1 densities in grade one astrocytomas and glioblastomas with diffuse and anaplastic astrocytomas showing the lowest densities [24]. However, a quantitative polymerase chain reaction (qPCR) study showed a correlation between glioma grade and TIMP-1 mRNA levels [25].
The aim of this study was to investigate the TIMP-1 expression in astrocytomas by immunohistochemistry and relate this expression to overall patient survival, which to our knowledge has not been done before. In this study we used the new and well-characterised TIMP-1 antibody VT7. The VT7 TIMP-1 antibody recognises a linear epitope, which may not be particularly accessible unless denaturation of the antigen is performed [26, 27]. Using this new antibody we found that glioblastoma patients with the lowest TIMP-1 expression had a significantly longer overall survival. In contrast, patients with the highest TIMP-1 expression had the shortest overall survival suggesting that TIMP-1 is a negative prognostic biomarker.
A preliminary report of this study has appeared in abstract form [28].
Materials and methods
Patients
This is a retrospective study on archive tumour material obtained from 112 patients who underwent initial surgery of diffuse astrocytoma (23 patients) and anaplastic astrocytoma (17 patients) between 1995 and 2005, and glioblastoma (72 patients) between 2001 and 2005 at Odense University Hospital, Denmark. The patients had received no prior treatment to the craniotomy. Table 1 describes the characteristics of the 112 patients included in the present study. In order to assure a sufficient and representative amount of tumour tissue and thereby reliable results, we defined a number of exclusion criteria. Recurrent tumours which are known to change expression of a number of proteins [29, 30] were thus excluded. Studies have shown that although improving the diagnostic evaluation of gliomas [31], glioma tissue removed by ultrasonic aspiration displayed varying degrees of degeneration [32, 33]. Consequently, tissue removed by ultrasonic aspiration was excluded. In keeping with this, astrocytomas where all the material had been frozen before paraffin embedding were excluded since the morphology of frozen tissue is compromised compared to the morphology of paraffin embedded tissue [34]. Finally, in heterogeneous tumours like astrocytomas, it is not optimal to assess the TIMP-1 expression in small biopsy specimens. Biopsies with a diameter of less than 4 mm were thus excluded.
Preparation of tissue
Fresh tissue biopsies from all astrocytoma patients were fixed in 4% neutral buffered formalin and paraffin embedded. Three micrometer sections were cut on a microtome and stained routinely with haematoxylin eosin to define representative tumour regions. All samples were classified according to World Health Organization guidelines 2007 [35].
TIMP-1 immunohistochemistry
Paraffin sections of all astrocytomas were stained using the TIMP-1 antibody VT7 [26, 27]. The immunostainings were performed using a Dako Autostainer Universal Staining System (Dako, Glostrup, Denmark). All reagents were obtained from Dako A/S, Denmark and used as described by manufacturer’s instructions. Paraffin sections were deparaffinised and endogenous peroxidase activity was quenched by immersion in 1.5% hydrogen peroxide followed by heat-induced epitope retrieval in 10 mM citrate buffer (pH 6). The sections were subsequently incubated for 60 min with the VT7 TIMP-1 monoclonal antibody (1:4000). The detection of the antigen–antibody complex was performed using anti-mouse PowerVision followed by visualisation with diaminobenzidine (DAB) as chromogen. Finally, the sections were counterstained with Mayer’s haematoxylin. Using paraffin sections with human prostate tissue as positive controls, intense and specific TIMP-1 positive epithelial cells were found in the glandular structure of hyperplastic prostate in accordance with previous findings [27]. No staining was observed using primary antibody omission as negative control. When staining normal brain tissue fixed in 4% neutral-buffered formalin for 24 h according to the protocol described above, TIMP-1 positive purkinje cells of the cerebellum were detected. No other cell types or blood vessels showed positive TIMP-1 immunoreactivity in the normal brain tissue. Using glioblastoma tissue sections fixed in 4% neutral-buffered formalin for 1, 3, 6, 24 and 48 h, no differences were detected in the intensity of the immunohistochemical reaction (data not shown).
Scoring of the TIMP-1 staining
The immunohistochemical score was based on the average percentage of TIMP-1 positive cells and blood vessels and their average staining intensity for the whole tissue section (Table 2). Regarding the percentage of positive tumour cells, the score 0 corresponds to 0% to <2% positive cells, score 1 to 2% to <15% positive cells, score 2 to 15% to <40% positive cells and score 3 to 40% to 100% positive cells. Regarding the tumour cell staining intensity, the score 0 corresponds to no staining, score 1 to faint staining, score 2 to moderate staining and score 3 to intense immunostaining. The percentage of positive tumour blood vessels and the blood vessel staining intensity were assessed in the same way. The necrotic areas of the glioblastomas were not included when the tumours were scored. Moreover, the invasion zones were not included as they were assessed separately in the same way as described above.
In order to include all four scores per tumour in one total value, the four scores for each tumour were summed. Thus a maximum score of 12 points could be reached for a tumour. For comparison with overall patient survival, the tumours were divided into four groups according to increasing total scores. Group one: total scores 0–5, group two: total scores 6–7, group three: total scores 8–9, and group four: total scores 10–12.
TIMP-1 in situ hybridisation
In situ hybridisation was performed using the probe described in a previous study [36]. Three μm paraffin sections from ten selected glioblastomas were deparaffinised in xylene and hydrated using ethanol/water solutions followed by proteinase K (10 mg/ml) treatment at 37°C for 5 min. The sections were washed 2× 5 min at 37°C in phosphate buffered saline (PBS), dehydrated and air-dried. A mixture of 5 μl digoxigenin labelled probe (10 ng/μl) and 20 μl hybridisation mix was applied to each section followed by hybridisation overnight at 42°C. The following day the sections were washed in 2× saline-sodium citrate (SSC) buffers containing 0.1% sodium dodecyl sulphate (SDS) at 55°C for 1 h followed by 30 min in 0.5× SSC containing 0.1% SDS. Sections were then RNase A treated for 10 min to remove non-specifically bound riboprobe followed by a final wash in 0.1× SSC containing 0.1% SDS for 30 min at 37°C. The sections were blocked with 5% BSA in 0.1 M Tris, 0.15 M NaCl, pH 7.5 containing 0.1% Triton X-100 for 30 min. Alkaline phosphatase-labelled anti-digoxigenin antibody (1:500, Roche Diagnostics GmbH, Mannheim, Germany) was then applied to the sections for 2 h. The reaction was visualised by incubation of the sections with NBT/BCIP (Roche, Switzerland) overnight in the dark. Finally, the sections were washed in TE-buffer followed by wash in water, counterstained with Mayer’s hematoxylin and mounted with Glycergel (Dako, Denmark). Sense probe was added to a section as a negative control and a section with human mamma carcinoma known to contain TIMP-1 mRNA was used as a positive control.
Statistical analysis
For comparison of TIMP-1 scores with increasing tumour grades, ANOVA with Bonferroni correction was used.
Overall patient survival was defined from the day of initial surgery until death of the patient. For each tumour grade, the TIMP-1 immunohistochemical scores corresponding to the percentage of TIMP-1 positive tumour cells and blood vessels and their staining intensity (0–3) were compared with overall patient survival in a Kaplan–Meier plot using the log rank test. Furthermore, the patients were stratified into four groups based on the total TIMP-1 score (0–5; 6–7; 8–9; 10–12) for comparison with overall patient survival in the same way. When performing the analysis, nine patients with diffuse astrocytoma, one patient with anaplastic astrocytoma, and one patient with glioblastoma were still alive. These patients were therefore censored. The multivariate Cox regression model was used to adjust for age and gender and P < 0.05 was considered significant. The statistical analyses were performed using SPSS 16.0 software (Statistical Package for the Social Sciences, SPSS, Denmark).
Results
TIMP-1 expression in diffuse astrocytomas
In diffuse astrocytomas two different cytoplasmatic staining patterns were observed as diffuse astrocytomas with a gemistocytic pattern showed distinct TIMP-1 positive gemistocytic tumour cells (Fig. 1a–b), whereas diffuse astrocytomas with a fibrillary pattern showed a more diffuse TIMP-1 staining (Fig. 1c). Moreover, in some gemistocytic tumour cells TIMP-1 seemed to be located to the membrane surrounding the characteristic copious cytoplasm (Fig. 1b). In the blood vessels, TIMP-1 was mainly detected in the periphery of the tumour vessels corresponding to the supposed localisation of the basal endothelial membrane (Fig. 1d). TIMP-1 positive tumour cells were detected in 96% of the diffuse astrocytomas, whereas TIMP-1 positive blood vessels were detected in 88% of the tumours (Table 3).
TIMP-1 immunohistochemically stained paraffin sections of diffuse astrocytomas. Tumours with a gemistocytic pattern showed distinct TIMP-1 positive gemistocytic tumour cells (a–b, arrows), whereas tumours with a fibrillary pattern showed a more diffuse TIMP-1 staining (c). In some of the tumours TIMP-1 staining was detected in the periphery of blood vessels (d, arrow). Scalebar 50 μm (a, c), 10 μm (b), 30 μm (d)
TIMP-1 expression in anaplastic astrocytomas
In anaplastic astrocytomas, a specific TIMP-1 labelling of the gemistocytic tumour cells was observed (Fig. 2a), but also areas with a more diffuse staining were found (Fig. 2b). In a few tumours, the TIMP-1 staining of the blood vessels was similar to that found for diffuse astrocytomas however, in most of the anaplastic astrocytomas, the blood vessels were found with TIMP-1 staining of the cytoplasm of some of the endothelial cells (Fig. 2c). TIMP-1 positive tumour cells were detected in 88% of the anaplastic astrocytomas, whereas TIMP-1 was detected in tumour blood vessels in 82% of the tumours (Table 3).
TIMP-1 immunohistochemically stained paraffin sections of anaplastic astrocytomas showed areas with distinctly TIMP-1 positive tumour cells (a) as well as areas with a more diffuse staining (b). Endothelial cells in some tumour blood vessels were TIMP-1 labelled (c, arrow) and TIMP-1 positive cells were also detected in the invasion zone (d) showing both positive cells with a tumour cell-like morphology as well as positive pyramidal shaped neurons. The insert shows the invasive zone in low magnification. Scalebar 50 μm
In four of the tumour biopsies, invasion zones were present. In all of these zones, diffusely putative invading TIMP-1 positive tumour cells were detected. Furthermore, TIMP-1 positive pyramidal shaped neurons were seen (Fig. 2d).
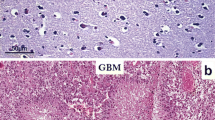
TIMP-1 expression in glioblastomas
In glioblastomas, TIMP-1 positive tumour cells showed a clear cytoplasmatic staining in both the smaller fusiform and stellate shaped tumour cells as well as in the multinucleated giant cells (Fig. 3a–c). TIMP-1 positive blood vessels were detected in most of the glioblastomas, often located in relation to TIMP-1 positive tumour cells (Fig. 3e–f), although other patterns were also recognised (Fig. 3c–d). In a few tumours, no blood vessel staining was detected in relation to the TIMP-1 positive tumour cells (Fig. 3c), whereas in other tumours TIMP-1 positive blood vessels were detected in relation to TIMP-1 negative tumour cells (Fig. 3d). In addition, tumour areas with both negative blood vessels and tumour cells were also recognised (Fig. 3g). In contrast to diffuse astrocytomas, TIMP-1 protein was detected mainly in the cytoplasm of the endothelial cells (Fig. 3d). TIMP-1 positive tumour cells were detected in 97% of the glioblastomas, whereas TIMP-1 positive blood vessels were detected in 92% of the tumours (Table 3).
TIMP-1 immunohistochemically stained paraffin sections of glioblastomas. TIMP-1 expression was detected in the cytoplasm of both the smaller fusiform and stellate shaped tumour cells as well as in the multinucleated giant cells (a–c). Blood vessel staining varied between tumours as some tumour blood vessels showed no TIMP-1 expression (c, arrows), while other tumour blood vessels showed a marked TIMP-1 staining of the endothelial cells (d, arrow). In most tumours a diffuse staining of the necrotic areas was seen (e–f), but tumours without staining of the necrotic areas were also seen. In general, a high TIMP-1 staining intensity was detected in tumour cells and tumour blood vessels close to the necrotic areas (e–f). Tumours with no TIMP-1 expression in tumour cells or in blood vessels were also found (g, arrow). TIMP-1 positive cells were also detected in the invasion zone (h) showing positive cells with a tumour cell-like morphology as well as positive pyramidal shaped neurons. Scalebar 100 μm (e, h), 50 μm (a, c, d, f, g), 30 μm (b)
The percentages and staining intensities of TIMP-1 positive tumour cells and blood vessels were generally high close to the large necrotic areas (Fig. 3e–f). The necrotic areas themselves showed a diffuse staining (Fig. 3e–f) similar to what is seen with other antibodies as well. In contrast to tumour cells and blood vessels close to these large necrotic areas, the spindle shaped tumour cells in the pseudopalisade formations delineating necrosis, which is one of the hallmarks of glioblastomas, did not express TIMP-1 (not shown).
In 22 of the glioblastoma biopsies (30.5%), invasion zones were present. In 20 of these 22 glioblastomas (90%) diffusely putative invading TIMP-1 positive tumour cells were detected as well as positive pyramidal shaped neurons (Fig. 3h). In the invasion zones, most tumours had TIMP-1 negative blood vessels, with only a few of the tumours having a faint TIMP-1 expression in the blood vessels.
TIMP-1 in situ hybridisation in glioblastomas
TIMP-1 in situ hybridisation confirmed that TIMP-1 mRNA was localised in both tumour cells and tumour blood vessels (Fig. 4a). The areas where TIMP-1 mRNA was detected using in situ hybridisation corresponded to the areas where TIMP-1 protein was detected using immunohistochemistry (Fig. 4b). In general, more TIMP-1 positive tumour cells and blood vessels were detected with immunohistochemistry than with in situ hybridisation.
Comparison of TIMP-1 scores
For both the percentage of TIMP-1 positive tumour cells and blood vessels, the highest score 3 was most often given to glioblastomas (Fig. 5a–d). For the total TIMP-1 score (Fig. 5e), the scores 8–9 and 10–12 were most often given to glioblastomas, whereas the scores 0–5 and 6–7 most often were given to diffuse astrocytomas.
Distribution of diffuse astrocytomas, anaplastic astrocytomas and glioblastomas according to the TIMP-1 immunohistochemical scores corresponding to the percentage of positive tumour cells (a), tumour cell staining intensity (b), percentage of positive blood vessels (c) and blood vessel staining intensity (d) as well as the distribution of all tumours according to the total score (e). Note that in all four categories, the highest score 3 was most often given to glioblastomas (a–d). Using the total score (e), glioblastomas most often received the scores 8–9 and 10–12, whereas diffuse astrocytomas most often received the scores 0–5 and 6–7. Data is shown as the percentage of diffuse astrocytomas (n = 23), anaplastic astrocytomas (n = 17) and glioblastomas (n = 72) given the scores 0, 1, 2 or 3 (a–d) or given the total scores 0–5, 6–7, 8–9 and 10–12 (e)
The TIMP-1 scores representing the percentages of TIMP-1 positive tumour cells were similar for all three tumour grades (Fig. 6a), whereas the TIMP-1 tumour cell staining intensity scores and the scores representing the percentage of TIMP-1 positive blood vessels increased with tumour grade (Fig. 6b–c). The TIMP-1 scores representing blood vessel staining intensity were similar for diffuse and anaplastic astrocytomas, whereas the score was significantly higher for glioblastomas (Fig. 6d). The total TIMP-1 scores increased with tumour grade, although being only significantly higher for glioblastomas compared with diffuse astrocytomas (Fig. 6e) similar to what was found for TIMP-1 tumour cell staining intensity and the percentage of TIMP-1 positive blood vessels (Fig. 6b–c).
Comparison of TIMP-1 immunohistochemical scores in diffuse astrocytomas, anaplastic astrocytomas and glioblastomas. The comparison was made for scores corresponding to the percentage of positive tumour cells (a), tumour cell staining intensity (b), percentage of positive blood vessels (c) blood vessel staining intensity (d) and for the total TIMP-1 score incorporating all four parameters (e). Note that the scores corresponding to the TIMP-1 tumour cell staining intensity (b), percentage of positive blood vessels (c) blood vessel staining intensity (d) as well as the total score (e) increased with tumour grade, whereas the percentage of positive tumour cells appeared to be similar for all three tumour grades. Data shown as mean scores + SEM for diffuse astrocytomas (n = 23), anaplastic astrocytomas (n = 17) and glioblastomas (n = 72). ANOVA with Bonferroni correction was used for comparison of the different tumour grades
Comparison of TIMP-1 protein expression and overall patient survival
For glioblastomas, patients with the lowest total TIMP-1 score (score 0–5; n = 12) had a significantly longer overall survival when compared to the patient groups with higher TIMP-1 scores using the multivariate Cox regression model adjusting for age and gender (P = 0.004, hazard ratio (95% confidence interval) = 3.2 (1.5–6.7)) (Fig. 7e). The percentage of TIMP-1 positive tumour cells (P = 0.018), the TIMP-1 tumour cell staining intensity (P = 0.035) and the TIMP-1 blood vessel staining intensity (P = 0.029) all affected overall patient survival (Fig. 7a–b, d). The percentage of TIMP-1 positive blood vessels did not affect overall patient survival when using the Cox regression model (Fig. 7c).
Kaplan–Meier survival plot for 72 glioblastoma patients grouped according to the TIMP-1 immunohistochemical score corresponding to the percentage of positive tumour cells (a), tumour cell staining intensity (b), percentage of positive blood vessels (c) blood vessel staining intensity (d) and according to the total TIMP-1 immunohistochemical score (e). Note that the percentage of positive tumour cells (a), the tumour cell staining intensity (b) and the blood vessel staining intensity (d) all are significantly associated with overall patient survival, whereas the percentage of positive blood vessels is not (c). When grouped according to the total score, the group with the scores 0–5 has a significantly longer overall survival than groups with higher scores (e). Differences were analysed by a multivariate Cox regression model adjusted for age and gender
For diffuse and anaplastic astrocytomas, we did not find any significant correlation between the TIMP-1 expression and overall patient survival when comparing the percentage of TIMP-1 positive tumour cells, tumour cell staining intensity, percentage of TIMP-1 positive blood vessels, blood vessel staining intensity or the total score with the overall patient survival (data not shown).
Discussion
The present study shows for the first time that a low immunohistochemical TIMP-1 protein expression in glioblastomas is associated with a longer overall patient survival when using the monoclonal antibody VT7 [26]. This is in accordance with results found in other human cancers such as breast [16], colorectal [19] and ovarian cancer [22]. In breast cancer, high tumour tissue levels of TIMP-1 measured by ELISA have been shown to have a negative effect on patient prognosis [16] and it has been shown by immunohistochemistry that a high TIMP-1 level detected in stromal cells was associated with a higher rate of distant metastases [37]. The majority of studies on colorectal cancer have focused on TIMP-1 plasma levels [38–40] showing that a high preoperative plasma level is associated with a shorter overall patient survival [19, 38, 39]. Furthermore, preoperative TIMP-1 serum levels in ovarian cancer have been shown to be associated with a more aggressive tumour behaviour and thereby to a poorer patient prognosis [22]. Taken together these studies suggest that TIMP-1 may play an important role in the biology in different types of cancer.
In the present study, we found that the TIMP-1 level increased with the malignancy grade for astrocytomas (WHO grade II–IV) (Fig. 6). This supports the theory of TIMP-1 being a negative prognostic marker in astrocytomas as well as in other cancers as described above. For both the TIMP-1 tumour cell staining intensity, the percentage of TIMP-1 positive blood vessels and the TIMP-1 blood vessel staining intensity, the immunohistochemical scores increased with grade of malignancy. Surprisingly, the percentage of TIMP-1 positive tumour cells was similar for all grades, whereas the grade-dependent increase in the percentage of TIMP-1 positive tumour blood vessels was in accordance with the well known higher blood vessel density in glioblastomas. Although significant results were found by comparison of TIMP-1 protein expression and malignancy grade, a certain variation was seen in the percentage of TIMP-1 positive tumour cells and blood vessels as well as in the staining intensities between tumours of the same grade. This might be due to the large degree of heterogeneity in astrocytomas and suggests that a high number of tumours must be included when quantifying and comparing staining characteristics in astrocytomas. In this study we included 23 anaplastic astrocytomas, 17 diffuse astrocytomas, and 72 glioblastomas. This is in contrast to a previous immunohistochemical study where no differences were found in TIMP-1 protein expression between six anaplastic astrocytomas and five glioblastomas. Furthermore, no TIMP-1 expression was found in four low grade astrocytomas [23]. In line with this, a Western Blot study detected the highest TIMP-1 densities in five pilocytic astrocytomas and ten glioblastomas, with five diffuse astrocytomas and ten anaplastic astrocytomas showing the lowest densities [24]. However, similar to our results a qRT-PCR study showed correlation between TIMP-1 mRNA level and astrocytoma grade [25] when comparisons were made for three low-grade astrocytomas, four anaplastic astrocytomas and nine glioblastomas.
In the present study, TIMP-1 protein and mRNA were detected in glioblastomas in both tumour cells and tumour endothelial cells. According to the stainings, TIMP-1 protein was more widely distributed compared to TIMP-1 mRNA which might be expected since mRNA is rapidly degraded compared to the more stable proteins. Similar to our observations, TIMP-1 protein was located in the cytoplasm of tumour cells in neuroendocrine cancers like parathyroid carcinoma [41] and Merkel cell carcinoma [42]. However, in colorectal cancers and breast cancers, TIMP-1 was mostly expressed in the myofibroblasts rather than in the epithelial cancer cells themselves [43, 44]. Expression of TIMP-1 protein in tumour endothelial cells has only been described in a few studies, where a faint endothelial expression was detected by immunohistochemistry e.g. in laryngeal carcinoma and papillary thyroid carcinoma [45, 46]. In contrast to these studies, we detected an intense endothelial TIMP-1 staining in glioblastoma. The present study is to our knowledge the first, where the expression of TIMP-1 protein in tumour blood vessels has been assessed and compared with grade of malignancy and overall patient survival. Our results suggest that TIMP-1 protein expression in tumour blood vessels increases with tumour grade (Fig. 6c–d). In addition, there appeared to be an association between a low tumour blood vessel TIMP-1 protein expression and a prolonged overall patient survival in glioblastomas (Fig. 7c–d) being however only significant for TIMP-1 blood vessel staining intensity. Investigating the presence of blood vessels in the glioblastomas, no differences were found between glioblastomas receiving a low versus a high TIMP-1 score.
TIMP-1 has recently been recognised as an anti-apoptotic protein besides its involvement in regulation of MMPs, stimulation of proliferation and regulation of angiogenesis [6–15, 47]. Davidsen et al. [48] established a TIMP-1 gene deficient fibrosarcoma cell line demonstrating that TIMP-1 gene deficient cells were considerably more sensitive to chemotherapy-induced apoptosis compared to the corresponding wild-type cells, thereby suggesting that TIMP-1 plays an important role in inhibition of chemotherapy-induced apoptosis. Using three different chemotherapeutic agents, it was moreover demonstrated that the protection was independent of the mechanism of action of the drug. Previously Li et al. [49] demonstrated that TIMP-1 could inhibit cell death induced by hydrogen peroxide, the chemotherapeutic drug adriamycin and radiation. Since both radiation and chemotherapy induce apoptosis, the high expression of TIMP-1 in both tumour cells and tumour blood vessels in glioblastomas may contribute to the therapeutic resistance of these tumours. Interestingly, Davidsen et al. [48] demonstrated the existence of a saturation level of TIMP-1 concerning the protection against apoptosis indicating that a higher level of TIMP-1 expression did not result in increased protection. This may explain why a longer overall survival in our study was only found for patients with the lowest TIMP-1 expression, whereas the three other survival curves corresponding to a higher total TIMP-1 expression were almost similar (Fig. 7e). Moreover, a certain level of TIMP-1 may be necessary for TIMP-1 to have an anti-apoptotic action, thereby possibly explaining why the TIMP-1 expression in diffuse and anaplastic astrocytomas did not seem to influence survival. Playing an anti-apoptotic role in cancer, the results obtained in the present study seem to reveal TIMP-1 as a potential new therapeutic target in glioblastomas. In order to elucidate a possible therapeutic role of TIMP-1 in glioblastomas, further investigations in vitro as well as in vivo are needed. An alternative target might be the putative TIMP-1 receptor CD63 [50]. It has been demonstrated by Jung et al. that TIMP-1 can bind to the cell surface protein CD63 present on the human breast epithelial cell line MCF10A and this interaction could be important in the TIMP-1 anti-apoptotic pathway since CD63 down-regulation has been shown to prevent the anti-apoptotic effect of TIMP-1 [50].
In conclusion, our results show that TIMP-1 immunohistochemical expression was significantly associated with overall survival in glioblastoma patients, suggesting that TIMP-1 might be used as a new biomarker in this type of cancer. The shorter survival of glioblastoma patients with a high tumour TIMP-1 level may be explained by the anti-apoptotic effect of TIMP-1 preventing apoptosis induced by radiation and chemotherapy. Accordingly, TIMP-1 or TIMP-1 interacting proteins may represent new targets in future development of anti-cancer therapies.
References
Jiang Y, Goldberg ID, Shi YE (2002) Complex roles of tissue inhibitors of metalloproteinases in cancer. Oncogene 21:2245–2252. doi:10.1038/sj.onc.1205291
Chirco R, Liu XW, Jung KK, Kim HR (2006) Novel functions of TIMPs in cell signaling. Cancer Metastasis Rev 25:99–113. doi:10.1007/s10555-006-7893-x
Carmichael DF, Sommer A, Thompson RC, Anderson DC, Smith CG, Welgus HG, Stricklin GP (1986) Primary structure and cDNA cloning of human fibroblast collagenase inhibitor. Proc Natl Acad Sci USA 83:2407–2411. doi:10.1073/pnas.83.8.2407
Stricklin GP, Welgus HG (1983) Human skin fibroblast collagenase inhibitor. Purification and biochemical characterization. J Biol Chem 258:12252–12258
Welgus HG, Stricklin GP, Eisen AZ, Bauer EA, Cooney RV, Jeffrey JJ (1979) A specific inhibitor of vertebrate collagenase produced by human skin fibroblasts. J Biol Chem 254:1938–1943
Hayakawa T, Yamashita K, Tanzawa K, Uchijima E, Iwata K (1992) Growth-promoting activity of tissue inhibitor of metalloproteinases-1 (TIMP-1) for a wide range of cells. A possible new growth factor in serum. FEBS Lett 298:29–32. doi:10.1016/0014-5793(92)80015-9
Chesler L, Golde DW, Bersch N, Johnson MD (1995) Metalloproteinase inhibition and erythroid potentiation are independent activities of tissue inhibitor of metalloproteinases-1. Blood 86:4506–4515
Wang T, Yamashita K, Iwata K, Hayakawa T (2002) Both tissue inhibitors of metalloproteinases-1 (TIMP-1) and TIMP-2 activate Ras but through different pathways. Biochem Biophys Res Commun 296:201–205. doi:10.1016/S0006-291X(02)00741-6
Porter JF, Shen S, Denhardt DT (2004) Tissue inhibitor of metalloproteinase-1 stimulates proliferation of human cancer cells by inhibiting a metalloproteinase. Br J Cancer 90:463–470. doi:10.1038/sj.bjc.6601533
Cornelius LA, Nehring LC, Harding E, Bolanowski M, Welgus HG, Kobayashi DK, Pierce RA, Shapiro SD (1998) Matrix metalloproteinases generate angiostatin: effects on neovascularization. J Immunol 161:6845–6852
Yoshiji H, Harris SR, Raso E, Gomez DE, Lindsay CK, Shibuya M, Sinha CC, Thorgeirsson UP (1998) Mammary carcinoma cells over-expressing tissue inhibitor of metalloproteinases-1 show enhanced vascular endothelial growth factor expression. Int J Cancer 75:81–87. doi:10.1002/(SICI)1097-0215(19980105)75:1<81::AID-IJC13>3.0.CO;2-G
Boudreau N, Sympson CJ, Werb Z, Bissell MJ (1995) Suppression of ICE and apoptosis in mammary epithelial cells by extracellular matrix. Science 267:891–893. doi:10.1126/science.7531366
Guedez L, Stetler-Stevenson WG, Wolff L, Wang J, Fukushima P, Mansoor A, Stetler-Stevenson M (1998) In vitro suppression of programmed cell death of B cells by tissue inhibitor of metalloproteinases-1. J Clin Invest 102:2002–2010. doi:10.1172/JCI2881
Lambert E, Boudot C, Kadri Z, Soula-Rothhut M, Sowa ML, Mayeux P, Hornebeck W, Haye B, Petitfrere E (2003) Tissue inhibitor of metalloproteinases-1 signalling pathway leading to erythroid cell survival. Biochem J 372:767–774. doi:10.1042/BJ20030187
Liu XW, Bernardo MM, Fridman R, Kim HR (2003) Tissue inhibitor of metalloproteinase-1 protects human breast epithelial cells against intrinsic apoptotic cell death via the focal adhesion kinase/phosphatidylinositol 3-kinase and MAPK signaling pathway. J Biol Chem 278:40364–40372. doi:10.1074/jbc.M302999200
Schrohl AS, Holten-Andersen MN, Peters HA, Look MP, Meijer-van Gelder ME, Klijn JG, Brünner N, Foekens JA (2004) Tumor tissue levels of tissue inhibitor of metalloproteinase-1 as a prognostic marker in primary breast cancer. Clin Cancer Res 10:2289–2298. doi:10.1158/1078-0432.CCR-03-0360
Wu ZS, Wu Q, Yang JH, Wang HQ, Ding XD, Yang F, Xu XC (2008) Prognostic significance of MMP-9 and TIMP-1 serum and tissue expression in breast cancer. Int J Cancer 122:2050–2056
Kuvaja P, Wurtz SO, Talvensaari-Mattila A, Brünner N, Paakko P, Turpeenniemi-Hujanen T (2007) High serum TIMP-1 correlates with poor prognosis in breast carcinoma—a validation study. Cancer Biomark 3:293–300
Holten-Andersen M, Christensen IJ, Nilbert M, Bendahl PO, Nielsen HJ, Brünner N, Fernebro E (2004) Association between preoperative plasma levels of tissue inhibitor of metalloproteinases 1 and rectal cancer patient survival. A validation study. Eur J Cancer 40:64–72. doi:10.1016/j.ejca.2003.09.019
Joo YE, Seo KS, Kim HS, Rew JS, Park CS, Kim SJ (2000) Expression of tissue inhibitors of metalloproteinases (TIMPs) in gastric cancer. Dig Dis Sci 45:114–121. doi:10.1023/A:1005421713137
Yoshikawa T, Tsuburaya A, Kobayashi O, Sairenji M, Miyagi Y (2006) Protein levels of tissue inhibitor of metalloproteinase-1 in tumor extracts as a marker for prognosis and recurrence in patients with gastric cancer. Gastric Cancer 9:106–113. doi:10.1007/s10120-006-0362-y
Rauvala M, Puistola U, Turpeenniemi-Hujanen T (2005) Gelatinases and their tissue inhibitors in ovarian tumors; TIMP-1 is a predictive as well as a prognostic factor. Gynecol Oncol 99:656–663. doi:10.1016/j.ygyno.2005.07.009
Nakagawa T, Kubota T, Kabuto M, Sato K, Kawano H, Hayakawa T, Okada Y (1994) Production of matrix metalloproteinases and tissue inhibitor of metalloproteinases-1 by human brain tumors. J Neurosurg 81:69–77
Kachra Z, Beaulieu E, Delbecchi L, Mousseau N, Berthelet F, Moumdjian R, Del MR, Beliveau R (1999) Expression of matrix metalloproteinases and their inhibitors in human brain tumors. Clin Exp Metastasis 17:555–566. doi:10.1023/A:1006760632766
Nuttall RK, Pennington CJ, Taplin J, Wheal A, Yong VW, Forsyth PA, Edwards DR (2003) Elevated membrane-type matrix metalloproteinases in gliomas revealed by profiling proteases and inhibitors in human cancer cells. Mol Cancer Res 1:333–345
Møller SN, Dowell BL, Stewart KD, Jensen V, Larsen L, Lademann U, Murphy G, Nielsen HJ, Brünner N, Davis GJ (2005) Establishment and characterization of 7 new monoclonal antibodies to tissue inhibitor of metalloproteinases-1. Tumour Biol 26:71–80. doi:10.1159/000085588
Sørensen IV, Fenger C, Winther H, Foged NT, Lademann U, Brünner N, Usher PA (2006) Characterization of anti-TIMP-1 monoclonal antibodies for immunohistochemical localization in formalin-fixed, paraffin-embedded tissue. J Histochem Cytochem 54:1075–1086. doi:10.1369/jhc.5A6896.2006
Aaberg-Jessen C, Christensen K, Schrøder HD, Offenberg H, Brünner N, Kristensen BW (2008) Low tissue inhibitor of metalloproteinases-1 (TIMP-1) protein expression in glioblastoma predicts longer patient survival, AACR Annual Meeting, Abstract # 5541
Graham DI, Lantos PL (2002) Tumours of the nervous system. In: Graham DI, Lantos PL (eds) Greenfield’s Neuropathology, vol 2. Arnold, Great Britain, pp 768–1052
Kleihues P, Cavenee WK (2000) Pathology and genetics of tumours of the nervous system. IARC Press, Lyon
Neckelmann K, Kristensen BW, Schrøder HD (2004) Improved histopathological evaluation of gliomas using tissue fragments obtained by ultrasonic aspiration. Clin Neuropathol 23:47–52
Silverman JF, Jones FD, Unverferth M, Berns L (1989) Cytopathology of neoplasms of the central nervous system in specimens obtained by the Cavitron Ultrasonic Surgical Aspirator. Acta Cytol 33:576–582
Malhotra V, Malik R, Gondal R, Beohar PC, Parkash B (1986) Evaluation of histological appearance of tissues removed by cavitron ultrasonic surgical aspirator (CUSA). Acta Neurochir (Wien) 81:132–134. doi:10.1007/BF01401235
Shi SR, Liu C, Pootrakul L, Tang L, Young A, Chen R, Cote RJ, Taylor CR (2008) Evaluation of the value of frozen tissue section used as “gold standard” for immunohistochemistry. Am J Clin Pathol 129:358–366. doi:10.1309/7CXUYXT23E5AL8KQ
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (2007) WHO Classification of Tumours of the Central Nervous System. International Agency for Research on Cancer, Lyon
Usher PA, Sieuwerts AM, Bartels A, Lademann U, Nielsen HJ, Holten-Andersen L, Foekens JA, Brünner N, Offenberg H (2007) Identification of alternatively spliced TIMP-1 mRNA in cancer cell lines and colon cancer tissue. Mol oncol 1:205–215
Vizoso FJ, Gonzalez LO, Corte MD, Rodriguez JC, Vazquez J, Lamelas ML, Junquera S, Merino AM, Garcia-Muniz JL (2007) Study of matrix metalloproteinases and their inhibitors in breast cancer. Br J Cancer 96:903–911. doi:10.1038/sj.bjc.6603666
Holten-Andersen MN, Stephens RW, Nielsen HJ, Murphy G, Christensen IJ, Stetler-Stevenson W, Brünner N (2000) High preoperative plasma tissue inhibitor of metalloproteinase-1 levels are associated with short survival of patients with colorectal cancer. Clin Cancer Res 6:4292–4299
Yukawa N, Yoshikawa T, Akaike M, Sugimasa Y, Rino Y, Masuda M, Imada T (2007) Impact of plasma tissue inhibitor of matrix metalloproteinase-1 on long-term survival in patients with colorectal cancer. Oncology 72:205–208. doi:10.1159/000112827
Waas ET, Hendriks T, Lomme RM, Wobbes T (2005) Plasma levels of matrix metalloproteinase-2 and tissue inhibitor of metalloproteinase-1 correlate with disease stage and survival in colorectal cancer patients. Dis Colon Rectum 48:700–710. doi:10.1007/s10350-004-0854-y
Tomita T (1997) Matrix metalloproteinases and tissue inhibitors of metalloproteinases in thyroid C-cells and medullary thyroid carcinomas. Histopathology 31:150–156. doi:10.1046/j.1365-2559.1997.2160834.x
Massi D, Franchi A, Ketabchi S, Paglierani M, Pimpinelli N, Santucci M (2003) Expression and prognostic significance of matrix metalloproteinases and their tissue inhibitors in primary neuroendocrine carcinoma of the skin. Hum Pathol 34:80–88. doi:10.1053/hupa.2003.51
Holten-Andersen MN, Hansen U, Brünner N, Nielsen HJ, Illemann M, Nielsen BS (2005) Localization of tissue inhibitor of metalloproteinases 1 (TIMP-1) in human colorectal adenoma and adenocarcinoma. Int J Cancer 113:198–206. doi:10.1002/ijc.20566
Jones JL, Glynn P, Walker RA (1999) Expression of MMP-2 and MMP-9, their inhibitors, and the activator MT1-MMP in primary breast carcinomas. J Pathol 189:161–168. doi:10.1002/(SICI)1096-9896(199910)189:2<161::AID-PATH406>3.0.CO;2-2
Sawatsubashi M, Mizokami H, Tokunaga O, Shin T (1998) Expression of MMP-1, TIMP-1, and type I collagen in laryngeal carcinoma. Mod Pathol 11:878–885
Maeta H, Ohgi S, Terada T (2001) Protein expression of matrix metalloproteinases 2 and 9 and tissue inhibitors of metalloproteinase 1 and 2 in papillary thyroid carcinomas. Virchows Arch 438:121–128. doi:10.1007/s004280000286
Liu XW, Taube ME, Jung KK, Dong Z, Lee YJ, Roshy S, Sloane BF, Fridman R, Kim HR (2005) Tissue inhibitor of metalloproteinase-1 protects human breast epithelial cells from extrinsic cell death: a potential oncogenic activity of tissue inhibitor of metalloproteinase-1. Cancer Res 65:898–906
Davidsen ML, Wurtz S, Rømer MU, Sørensen NM, Johansen SK, Christensen IJ, Larsen JK, Offenberg H, Brünner N, Lademann U (2006) TIMP-1 gene deficiency increases tumour cell sensitivity to chemotherapy-induced apoptosis. Br J Cancer 95:1114–1120. doi:10.1038/sj.bjc.6603378
Li G, Fridman R, Kim HR (1999) Tissue inhibitor of metalloproteinase-1 inhibits apoptosis of human breast epithelial cells. Cancer Res 59:6267–6275
Jung KK, Liu XW, Chirco R, Fridman R, Kim HR (2006) Identification of CD63 as a tissue inhibitor of metalloproteinase-1 interacting cell surface protein. EMBO J 25:3934–3942. doi:10.1038/sj.emboj.7601281
Acknowledgments
We are grateful to Ole Nielsen for collaboration on the immunohistochemical protocol. Thanks are also due to Professor Werner Vach for help with the statistical survival analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aaberg-Jessen, C., Christensen, K., Offenberg, H. et al. Low expression of tissue inhibitor of metalloproteinases-1 (TIMP-1) in glioblastoma predicts longer patient survival. J Neurooncol 95, 117–128 (2009). https://doi.org/10.1007/s11060-009-9910-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-009-9910-8