Abstract
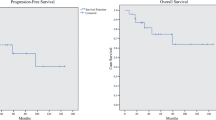
Background Infratentorial ependymoma is a common central nervous system tumor of childhood and in patients >1 year of age is treated with maximally feasible surgical resection and radiotherapy. Because of this tumor typically arises within the 4th ventricle and can invade the brainstem, patients are at risk for significant neurological impairment. Purpose To characterize the incidence, evolution, and persistence of neurologic impairment in children with infratentorial ependymoma following maximal safe surgery and conformal or intensity-modulated radiation therapy (CRT/IMRT). Patients and Methods After surgical resection, 96 children with non-metastatic infratentorial ependymoma were enrolled on a phase II study of image-guided radiation therapy and were prospectively followed with interval comprehensive neurological examinations. Late adverse neurological severity was graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE), version 3.0. Results The most common deficits detected at baseline examination were limb dysmetria, cranial nerve VI/VII palsy, limb paresis, dysphagia, and truncal ataxia/hypotonia. When present, gait dysfunction and dysphagia were often severe. Oculomotor dysfunction, facial paresis, dysphagia, and gait impairment improved over time. With the exception of hearing loss, in the survivor cohort, very few severe late effects (CTCAE Grade 3/4/5) were present at 60 months survival. Conclusion In general, neurological deficits were maximal in the post-operative period and either remained stable or improved during radiation and the post-treatment evaluation period. With the exception of hearing, the majority of chronic residual neurological deficits in this at-risk population are mild and only minimally intrude upon daily life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Each year in the United States, approximately 200 children, most of whom are <4 years old, are diagnosed with ependymoma [1, 2]. Although this tumor is derived from ependymal cells that traverse the central nervous system, in the pediatric age group, ependymomas typically arise within and grow to fill the 4th ventricle. Concurrent brainstem invasion and tumor extension through the foramina of Luschka to involve cranial nerves, pyramidal, and cerebellar tracts are common.
Treatment of non-metastatic infratentorial ependymoma in children >1 year of age consists of surgical resection followed by local irradiation. Because the degree of resection has proven to be an important prognostic factor, complete tumor extirpation is advocated whenever possible [3]. The optimal dose of radiation remains unknown; however, survival is presumed to correlate with a larger prescription dose [3]. Given the invasive nature of ependymoma within the brainstem and the need for an aggressive therapeutic approach, these patients are at risk to develop significant neurological deficits that may negatively impact daily function.
Over the past decade, CRT/IMRT has become the principal method to deliver therapeutic radiation in cooperative group treatment trials for pediatric intracranial ependymoma [4]. CRT/IMRT limits normal tissue exposure and presumably mitigates the risk of untoward morbidity by conforming the prescription radiation dose to a well defined intracranial target. Despite its widespread use, long-term neurological outcome in children treated with CRT/IMRT has not been well established. To better characterize neurological morbidity after maximal safe surgery and CRT/IMRT in children with non-metastatic infratentorial ependymoma, we reviewed longitudinal neurological examinations that were prospectively completed as part of an institutional phase II treatment trial. Based on our clinical experience, we hypothesized that neurological deficits would be maximum in the post-operative period and in most children severity would either stabilize or improve over time. Additionally, we did not expect the severity of persistent neurological morbidity in long-term survivors to be excessive or significantly impact daily life.
Patients and methods
Patients
From August 11, 1997 to February 8, 2006, 98 children with non-metastatic infratentorial ependymoma were enrolled on an institutional phase II study of image-guided radiation therapy with quantification of radiation-related CNS effects. Criteria for enrollment on this institutional review board approved trial have been published previously [5]. One patient died of tumor related complications after enrollment but before a baseline neurologic examination was performed. A second patient was determined to have metastatic tumor shortly after enrollment and was therefore ineligible for protocol treatment. Thus, 96 patients comprised this study’s cohort.
Extent of resection defined
All patients underwent surgical resection before radiation therapy. Gross-total resection was defined as resection after which the only tumor cells that remained were visible with the use of the operating microscope; patients for whom this type of resection was achieved had no evidence of disease on postoperative neuroimaging. Near-total resection was defined as resection after which only residual tumor <5-mm thick was visible on postoperative neuroimaging. Subtotal resection was defined as resection that left behind residual tumor >5-mm thick on postoperative neuroimaging. Further surgery was systematically applied to maximize the extent of resection before irradiation.
Conformal radiation therapy
The gross tumor volume (GTV) encompassed the tumor bed, residual tumor, or both. The clinical target volume (CTV) contained the GTV with an additional margin of 10 mm, which was included so that subclinical microscopic disease beyond the GTV could be treated. The CTV was anatomically confined; that is, it was limited by normal tissue structures through which tumor extension was unlikely. The planning target volume included the CTV surrounded by an additional margin of 3–5 mm expanded in three dimensions to account for uncertainty in patient positioning and image registration. Conventional fractionation (1.8 Gy per day) was used to treat all patients, and the prescribed dose was 59.4 Gy (except in children <18 months; prescribed dose = 54.0 Gy).
Prospective assessment of neurological morbidity
A comprehensive neurological examination was scheduled at baseline (defined as within 3 months of CRT) and every 6–12 months thereafter until reaching 120 months following the start of CRT. All examinations were performed by a board-certified neurologist and/or their designee. Using a 4-point severity scale (provided in Table 3), a total of 37 neurological functions were assessed with each visit: cranial nerves (CN) III–VII (left/right), CN IX–XII (left/right), muscle strength, tone, and reflexes in upper and lower extremities (left/right), axial tone and motor control, plantar reflexes (left/right), gross sensory function in upper and lower extremities (left/right), coordination in upper and lower extremities (left/right), ocular pursuit (including an assessment for nystagmoid or saccadic eye movements), speech, swallow, station, and gait. Initial hand dominance was not routinely assessed in this predominantly infant cohort. If a patient was taken off-protocol (progressive disease, family or physician preference), further examinations were excluded from the analysis.
Analysis of neurologic morbidity
Neurological morbidity was characterized with regard to individual deficits and clinically relevant functional impairments. The first objective was to estimate the incidence and evolution of specific neurologic deficits observed within the entire cohort (n = 96). A deficit was defined as any abnormal neurological sign demonstrated on examination. Total number of neurological deficits noted at each examination from baseline to the 60 months post-RT examination was compiled. Neurological deficits were defined as abnormal neurological signs on examination (see above). For analysis, 21 of the 37 neurologic functions routinely tested were utilized: CN III (left versus right), CN IV (left versus right), CN VI (left versus right), ocular pursuit, CN VII (left versus right), swallowing function (CN IX, CN X), speech, muscle strength in upper and lower extremities (left versus right; upper versus lower), limb coordination (left versus right; upper versus lower), station (truncal tone, truncal coordination), and gait. Speech and gait were not assessed in patients who were younger than 2.0 years at time of evaluation. With regard to reporting total number of deficits, a score of 0 was assumed in 34 evaluations for speech and gait in the 23 patients whose age was less than 2 years at time of evaluation. Based on 495 neurologic follow up exams from baseline to 60 months after the start of RT, we used linear mixed effects model with random coefficients [6] to describe the trend of number of deficits; exponential decay, simple linear function, and non-parametric function [7] were considered for the relationship between average number of deficits and time, and simple linear regression function was chosen based on model validity and simplicity. The intercept of the simple linear function represents the average number of deficits at start of RT, and the slope the average changing rate post-radiation. Comparisons between patient groups utilized Pearson and exact Pearson chi-square tests.
The second objective of this study was to characterize the incidence and evolution of specific neurologic impairments over time. Neurological impairments were defined by grouping individual neurological deficits (when applicable) into eight clinically evaluable categories: oculomotor dysfunction (CN III, IV, VI, and ocular pursuit), facial paresis (CN VII), dysphagia (CN IX, CN X), dysarthria, limb paresis (irrespective of arm vs. leg or laterality), limb dysmetria (irrespective of arm versus leg or laterality), truncal ataxia/hypotonia, and gait dysfunction. Because patient enrollment decreased over time, only a subset of the entire cohort completed a baseline, 36 months, and 60 months post-RT examination (N = 42). Descriptive statistics were used to characterize impairment.
The third objective was to characterize the severity of residual neurologic deficits in long-term survivors of pediatric infratentorial ependymoma. Forty-eight patients survived ≥60 months and contribute to this analysis. These late adverse neurological effects were defined as neurological deficits persisting or occurring ≥60 months after tumor diagnosis and, similar to other late effects studies in pediatric cancer [8, 9], severity was graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE), version 3.0. Although hearing (CN VIII) was not routinely assessed during neurological examinations, all patients periodically received a formal audiometric study [10], and the results of the most recent assessment are included within this analysis.
All analyses were performed by using SAS® (SAS® Institute, Cary, NC).
Results
Cohort characteristics
The clinical and treatment characteristics of the study cohort are presented in Table 1. The median total radiation dose for this cohort was 59.4 Gy (54–59.4 Gy). Fourteen children younger than 18 months and three children older than 18 months (physician’s discretion) received 54.0 Gy after gross-total resection of tumor.
Neurological examination participation
Cohort status is current to March 2008. The number of patients assessed for individual neurologic impairments at protocol-specified time points is shown in Table 2. Of the 96 patients who were initially enrolled, 40 patients (42%) did not complete a neurological examination within the 12 month period that preceded analysis: 31 patients (78%) were off-protocol because of either tumor progression (n = 23), study completion (n = 3), or patient/parent/physician preference (n = 5). Nine patients (23%) were still enrolled on protocol but did not have a neurologic examination in the last 12 months because of scheduling conflicts or reasons unaccounted. The overall rate of compliance for neurological assessment at the specific time intervals was 66% and the median interval from initiation of RT to last neurologic evaluation was 49.2 months (range −0.4 to 98.7 months).
Baseline incidence and evolution of neurologic deficits and impairments
No neurological deficits were detected at any time in 20 patients (21%). Among these patients, seven had survived ≥60 months, seven had not yet reached 60 months survival, and six were off-study at time of analysis (one completed study, one non-compliance, and four progressive disease). When the clinical and demographic characteristics of these 20 patients are compared with the 76 patients who had at least one morbidity, the presence of hydrocephalus (P = 0.015) and a history of ventricular shunt placement (P = 0.009) were significantly associated with the latter group. In contrast, achievement of GTR (.043) was significantly associated with the 20 patients without any morbidity. Not surprisingly, majority of these patients had midline tumors that rarely advanced into the lateral recesses where cranial nerves would be most vulnerable.
For the entire cohort (N = 96), at the baseline examination, the average number of neurological deficits per patient was 3.6. The most common deficits detected at baseline were limb dysmetria (37 patients, 55%), CN VI palsy (35 patients, 51%), CN VII palsy (34 patients, 50%), limb paresis (27 patients, 40%), dysphagia (25 patients, 39%), and truncal ataxia and/or hypotonia (16 patients, 24%). Seventeen patients had at least one deficit characterized as severe and, of these, 11 patients had 2–4 concurrent severe deficits and one patient had six concurrent severe deficits on baseline exam. Gait (nine patients, 18%) and swallowing (six patients, 9%) were the most common severely compromised functions at baseline.
Overall, the number of neurological deficits per patient decreased over time on an average rate of 0.28 per year (0.024 per month). The average number of neurological deficits at 60 months was 2.2. Of the 17 patients with at least one severely compromised function, 15 were examined at a later time point (other two patients had early progression and came off-study) and 13 had improved neurological status. Severe dysphagia was the function most resistant to improvement over time; no improvement was evident in 33% of these patients. Of note, 27 patients (28%) had a gastrostomy tube (G-tube) placed because of severe dysphagia. The G-tube remained in place for a median of 234 days (range = 17–2453 days). On a similar note, 15 patients (16%) required a tracheotomy for a median of 473 days (range = 68–2196 days).
Of the 48 patients who had survived ≥60 months since diagnosis of tumor, 42 patients (88%) had a neurological evaluation at baseline, 36 months post-CRT, and 60 months post-CRT. The characterization of severity and incidence of impairment within this group is provided in Table 3. Overall, this group tended to have mild or no detected neurological impairment from baseline to 60 months post-RT examination. The number of outliers with more severe impairment decreased in almost all categories. Baseline limb paresis and limb dysmetria was generally mild but did not improve over time. Facial paresis, dysphagia, and gait impairment improved within 36 months and then remained stable. Oculomotor dysfunction continued to improve at 60 months. Bilateral neurological impairment was noted in some patients at baseline: oculomotor dysfunction (7.1%), facial paresis (2.4%), limb paresis (11.9%), and limb dysmetria (23.8%). At the time of the 60 month post-RT examination, the incidence of bilateral impairment had decreased within the following categories: oculomotor dysfunction (4.8%), limb paresis (0%), and limb dysmetria (9.5%). The incidence of bilateral facial paresis remained stable over 60 months.
Late neurological effects in long-term survivors of pediatric infratentorial ependymoma
At the time of analysis, 48 patients had survived ≥60-months (median = 84.7; range 56–108.3 months) from diagnosis. The incidence and impact upon daily life of late neurological effects as measured by CTCAE criteria are presented in Table 4. With the exception of hearing loss sufficient to indicate therapeutic intervention, very few severe late effects (Grade 3/4/5) were present. Mild (Grade 1/2) residual neurological deficits that do not interfere with daily functions included impaired eye abduction (CN VI), facial paresis (CN VII), limb paresis, and limb dysmetria. Given the lack of clinically significant late effects in this population, further covariate analyses using pertinent medical risk factors (Table 1) were not attempted.
Discussion
Improvements in therapeutic radiation technique as well as advancements in diagnostic imaging, neurosurgical technique, and supportive patient care measures over the past 3 decades have resulted in an increased 5-year survival rate for children diagnosed with CNS tumors [1, 2]. With improved survival, systematic characterization of the long-term sequelae affecting these patients is important as this information may inform future treatment trials and help to identify patient groups who require closer surveillance and/or specific interventions to limit disability. Characterization of neurological outcomes in brain tumor patients may be particularly important as these patients are reported to potentially have a higher risk for mortality from accidental trauma due to underlying neurosensory/neuromotor deficits [11, 12].
In general, neurological impairment (as differentiated from neuro-cognitive or neuro-endocrine function) in pediatric brain tumor patients is poorly described. The literature is devoid of any prospective series that track the evolution of neurological deficits over time. With respect to chronic neurologic outcomes, more literature is available. The largest cohort of pediatric brain tumor patients with available neurological outcomes is from the Childhood Cancer Survivor Study [13]. This report demonstrated childhood brain tumor survivors have excess risk for chronic neurosensory deficits, focal neurological dysfunction, and epilepsy. Unfortunately, the characterization of neurological impairment in this cohort is limited because outcomes are based upon the patient’s own recall of events and their ability to interpret relevant neurologic symptoms or signs. Also, like much of the available literature, the cohort is from an era dominated by whole-brain megavoltage radiotherapy. This may not represent more contemporary patients treated with advanced multi-modal therapy.
Another deficiency of the existent literature is that risk factors for chronic neurological impairment in pediatric brain tumor patients are often not well characterized with respect to individual tumor type or location [13–22]. More recently, treatment strategies for pediatric brain tumors have become more diversified and are now often customized with respect to underlying tumor histopathology, tumor molecular profile, tumor location, and/or individual patient characteristics. Because treatment exposure and attendant risk for untoward morbidity will vary, it is no longer tenable to aggregate childhood brain tumor patients when reporting treatment outcomes.
Given the paucity of literature that characterizes neurological impairment in contemporary pediatric brain tumor patients, this longitudinal study of neurological function in pediatric infratentorial ependymoma patients treated with maximal safe surgery and CRT/IMRT is notable. To our knowledge, this report is the first to describe the evolution of neurological impairment from treatment initiation to achievement of long-term survival in a cohort of pediatric brain tumor patients. Because neurological function is such an important consideration for clinicians and parents, these findings should provide some reassurance and assist treatment decision-making in pediatric infratentorial ependymoma patients.
As hypothesized, in most patients, neurological deficits were maximal in the post-operative period and either remained stable or improved during radiation and the post-treatment evaluation period. Presence of hydrocephalus and history of shunt placement was associated with increased morbidity. Even those deficits characterized as severe typically improved over time. Need for G-tube and tracheotomy placement was rare. When placed, both were generally required for about 1 year. With the exception of hearing, the majority of chronic residual neurological deficits in this at-risk population is mild and only minimally intrudes upon daily life. The primary impairments noted 5-years after start of radiation include impaired ocular motility, facial weakness, mild hemiparesis, and limb dysmetria. With respect to radiation-related morbidity, within the first 5 years after irradiation, no patient experienced untoward radiation necrosis or radiation induced neurological decline. Although the maximally-tolerated dose of small volume fractionated irradiation to the brainstem in children is unknown, the prescribed dose 59.4 Gy appears to be generally safe with regard to cranial nerves and white matter bundles subserving motor and sensory functions travelling within or near the 4th ventricle. Despite these optimistic findings, it is pertinent to note that the majority of children are pre-adolescent at time of 5-year follow-up (median age 7.7 years) and with age and additional social pressures, these survivors may develop further impairments such as peer rejection because of facial asymmetry or inability to obtain drivers permit because of motor difficulties. Continued monitoring of this population with particular attention to quality of life is thereby required.
When interpreting the results of this study, several limitations should be considered. With regard to patient participation, overall rate of compliance to mandated examinations at specific intervals was moderate (66%). Unfortunately, the challenge in reconciling often complex patient schedules (multiple competing clinical appointments, extended sedation for irradiation or surveillance scans, prolonged post-sedation effects, etc.) to the limited availability of neurological subspecialty appointments largely contributed to this deviance. However, because most patients underwent multiple examinations (median number of examinations per patient = 7, range = 1–14) risk for referral bias was believed to be minimal. On a similar note, given the reduced flexibility in scheduling, neurological examinations were not performed by a single neurologist and, thus, inter-rater reliability may be of concern. Also, the interpretation of neurological impairment from clinical notes was retrospective and subject to additional bias. Furthermore, the severity scale for deficits/impairments was an “in-house” measure and has not been validated at this juncture. Although validated clinical severity scales exist for some for some deficits of interest, these were not assessed prospectively and therefore were not utilized for this study. St. Jude Children’s Research Hospital serves as a national referral center and our pediatric neurosurgeons have experience that only several institutions in the United States can equal. Therefore, our rate and degree of neurological morbidity after maximal safe surgery may not be well generalized to all patients. Because of the potential risk of harm in removing infratentorial ependymoma, resection by an experienced neurosurgeon is highly advised. Finally, there is growing optimism that radiotherapy using protons rather than photons may provide additional protection to normal brain structure in pediatric brain tumor patients. It is unclear whether the results of this study will be applicable to a growing population of patients receiving proton therapy.
References
CBTRUS 1/22/08. Selected primary (malignant and non-malignant) brain and central nervous system tumor age-specific incidence rates by age at diagnosis, CBTRUS 1998–2002. http://wwwcbtrusorg/2005-2006/tables/2006table12pdf Accessed 22 Jan 2008
Gurney JGSM, Bunin GR (1999) CNS and miscellaneous intracranial and intraspinal neoplasms. National Cancer Institute, SEER Program, Bethesda, MD. NIH Pub. No. 99-4649 Report
Bouffet E, Perilongo G, Canete A et al (1998) Intracranial ependymomas in children: a critical review of prognostic factors and a plea for cooperation. Med Pediatr Oncol 30(6):319–329. doi:10.1002/(SICI)1096-911X(199806)30:6<319::AID-MPO1>3.0.CO;2-H (discussion 329–331)
Phase A II trial of conformal rt for pediatric patients with localized ependymoma, chemotherapy prior to 2nd surgery for incompletely resected ependymoma and observations for completely resected, differentiated, supratentorial ependymoma. https://members.childrensoncologygroup.org/prot/ProtInfo.asp?ProtocolNum=ACNS0121&Disease=CNS. Children’s Oncology Group Accessed
Merchant TE, Mulhern RK, Krasin MJ et al (2004) Preliminary results from a phase II trial of conformal radiation therapy and evaluation of radiation-related CNS effects for pediatric patients with localized ependymoma. J Clin Oncol 22(15):3156–3162. doi:10.1200/JCO.2004.11.142
Littell RCMG, Stroup WW, Wolfinger RD (1996) SAS system for mixed models. SAS Institute Inc, Cary, NC
Liang H (2006) A new method of evaluating antitumor activity from measured tumor volumes. Contemp Clin Trials 27(3):269–273. doi:10.1016/j.cct.2005.11.004
Spunt SL, Sweeney TA, Hudson MM et al (2005) Late effects of pelvic rhabdomyosarcoma and its treatment in female survivors. J Clin Oncol 23(28):7143–7151. doi:10.1200/JCO.2005.12.096
Oeffinger KC, Mertens AC, Sklar CA et al (2006) Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 355(15):1572–1582. doi:10.1056/NEJMsa060185
Hua C, Bass JK, Khan R et al (2008) Hearing loss after radiotherapy for pediatric brain tumors: effect of cochlear dose. Int J Radiat Oncol Biol Phys 72(3):892–899
Hawkins MM, Kingston JE, Kinnier Wilson LM (1990) Late deaths after treatment for childhood cancer. Arch Dis Child 65(12):1356–1363. doi:10.1136/adc.65.12.1356
Mertens AC, Yasui Y, Neglia JP et al (2001) Late mortality experience in five-year survivors of childhood and adolescent cancer: the childhood cancer survivor study. J Clin Oncol 19(13):3163–3172
Packer RJ, Gurney JG, Punyko JA et al (2003) Long-term neurologic and neurosensory sequelae in adult survivors of a childhood brain tumor: childhood cancer survivor study. J Clin Oncol 21(17):3255–3261. doi:10.1200/JCO.2003.01.202
Bamford FN, Jones PM, Pearson D et al (1976) Residual disabilities in children treated for intracranial space-occupying lesions. Cancer 37(2 (Suppl)):1149–1151. doi:10.1002/1097-0142(197602)37:2+<1149::AID-CNCR2820370825>3.0.CO;2-C
Butler DF, Jose BO, Paris KJ et al (1999) An analysis of the late effects of radiotherapy in pediatric central nervous system tumors. J Ky Med Assoc 97(10):465–471
Chapman CA, Waber DP, Bernstein JH et al (1995) Neurobehavioral and neurologic outcome in long-term survivors of posterior fossa brain tumors: role of age and perioperative factors. J Child Neurol 10(3):209–212. doi:10.1177/088307389501000308
Foreman NK, Faestel PM, Pearson J et al (1999) Health status in 52 long-term survivors of pediatric brain tumors. J Neurooncol 41(1):47–53. doi:10.1023/A:1006145724500
Lannering B, Marky I, Lundberg A et al (1990) Long-term sequelae after pediatric brain tumors: their effect on disability and quality of life. Med Pediatr Oncol 18(4):304–310. doi:10.1002/mpo.2950180410
Macedoni-Luksic M, Jereb B, Todorovski L (2003) Long-term sequelae in children treated for brain tumors: impairments, disability, and handicap. Pediatr Hematol Oncol 20(2):89–101. doi:10.1080/0880010390158595
Sonderkaer S, Schmiegelow M, Carstensen H et al (2003) Long-term neurological outcome of childhood brain tumors treated by surgery only. J Clin Oncol 21(7):1347–1351. doi:10.1200/JCO.2003.08.009
Spunberg JJ, Chang CH, Goldman M et al (1981) Quality of long-term survival following irradiation for intracranial tumors in children under the age of two. Int J Radiat Oncol Biol Phys 7(6):727–736
Syndikus I, Tait D, Ashley S et al (1994) Long-term follow-up of young children with brain tumors after irradiation. Int J Radiat Oncol Biol Phys 30(4):781–787
Acknowledgements
Financial Support: This work was supported by the Cancer Center Support (CORE) Grant P30 CA 21765 from the National Institutes of Health and by the American Lebanese Syrian Associated Charities (ALSAC).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brannon Morris, E., Li, C., Khan, R.B. et al. Evolution of neurological impairment in pediatric infratentorial ependymoma patients. J Neurooncol 94, 391–398 (2009). https://doi.org/10.1007/s11060-009-9866-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-009-9866-8