Abstract
Little is known about the cytogenetic and molecular genetic events that lead to the formation of paediatric astrocytoma. We have analysed 57 paediatric astrocytoma (WHO grades I–IV) using comparative genomic hybridisation in order to identify common regions of abnormality. Large regions of copy number alterations were infrequent with 71% of tumours demonstrating no genomic imbalance. Furthermore, the most frequent aberrations (including gain of 6q, 2q, and 7q, and loss of 16 and 12q) occurred in only a subset of cases. High-copy number amplification was seen in five tumours at 12 different regions. The presence of copy number alterations was significantly associated with increasing grade of malignancy, and gain of 12q and the presence of high-copy number amplification were associated with a poor outcome in patients with malignant astrocytoma (P = 0.0039 and 0.0085, respectively). FISH analysis confirmed loss of 1p36 identified by CGH. There was no evidence of amplification of EGFR, CDK4, MET, CDK6, c-myc, or MDM2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system tumours are a leading cause of cancer-related deaths in children. The most prevalent type of brain tumour in the paediatric population is astrocytoma, which constitutes approximately two-fifths of this group of tumours. Astrocytoma commonly manifests as World Health Organisation (WHO) grade I pilocytic astrocytoma (PA) (0.83 cases/100,000 head of population/year), followed by WHO grade IV glioblastoma multiforme (GBM) (0.13 cases/100,000 head of population/year), WHO grade III anaplastic astrocytoma (AA) (0.09 cases/100,000 head of population/year), and WHO grade II diffuse astrocytoma (DA) (0.05 cases/100,000 head of population/year) [1]. Tumour grade is the most powerful predictive factor, and prognosis for these patients becomes increasingly poor with progressive grades of malignancy. The long-term outcome is excellent for children with PA and survival of 100% has been reported in some studies [2–5]. In contrast, five-year survival of 55% has been observed in patients with diffuse astrocytoma [6] and children with malignant astrocytoma have an even poorer prognosis, with two-year survival of only 33% being reported in one study [4]. In addition, the extent of surgical resection is favourably associated with length of survival whereas brainstem involvement is an adverse prognostic factor [7–13]. However, little is known about the genetic pathogenesis of paediatric astrocytoma and reliable molecular prognostic markers have yet to be identified.
In contrast, many of the genetic aberrations which are involved in the development of adult astrocytoma been characterised. Primary GBM may develop de novo without a clinical history of a pre-existing low-grade tumour and are characterised by amplification or overexpression of EGFR and MDM2 and homozygous deletion of p16 INK4A [14]. In contrast, secondary GBM progress from lower grade tumours and have a high incidence of p53 mutations and overexpression of PDGFR [15]. The incidences of RB loss and/or mutation and CDK4 amplification are comparable in both primary and secondary GBM (25 and 15% of cases, respectively). Similarly, deletions on chromosome 10 are very common in both types of GBM although mutations of PTEN occur almost exclusively in primary GBM. However, extensive analyses have been unable to demonstrate many of these patterns of genetic change in paediatric astrocytoma [16]. From published data, normal karyotypes have been observed in approximately 70% of PA, 55% of DA, 38% of AA, and 25% of GBM (21–31). Numerical and structural abnormalities of chromosomes 1, 2, 3, 7, 8, 17, 18 and 22 have been reported in a subset of cases but novel non-random aberrations have not yet been identified [17–26].
Cytogenetic and molecular genetic investigations in paediatric astrocytoma have been hindered by the comparative rarity of these tumours, and the difficulty in producing sufficient numbers of metaphase spreads of adequate quality for cytogenetic analysis. In addition, the tumours are often sited in deep-seated and/or functionally important areas of the brain, which, together with the increased use of stereotactic surgery, results in small biopsies and limited amounts of tissue available for molecular analysis. We have overcome these obstacles by applying comparative genomic hybridisation (CGH) to identify consistent regions of genomic imbalance in a series of 57 paediatric astrocytoma. We have also used fluorescent in-situ hybridisation (FISH) to investigate the copy number of genes mapping to areas of genomic gain on chromosomes 7, 8, and 12. Probes were used to detect EGFR, MET, CDK6, CDK4, and MDM2 in order to determine whether commonly amplified genes in adult astrocytoma are also targets in childhood tumours. FISH analysis of C-myc (8q24.1) was also included because gains of 8q and elevated expression of c-myc have been reported previously in paediatric malignant astrocytoma [27]. We have combined the CGH data generated in this study with those from an earlier publication [27] in order to identify potential prognostic markers.
Materials and methods
Tumour samples and patient characteristics
The clinical features of the 57 patients included in this study are summarised in Table 1, together with details of previously published cases from our laboratory (numbers 2*–12*). The mean age at presentation was 7.98 years (range 0.75–17 years) with a male/female ratio of 28/29. Most of the patients in this study received surgery at first presentation (25/57 macroscopic removal, 22/57 partial removal, 5/57 stereotactic biopsy, 1/57 temporal lobectomy, four unknown). Following surgical resection of the primary tumour approximately 30% of patients received adjuvant therapy (12 radiotherapy only, 2 chemotherapy only) according to either the Baby Brain Protocol (UKCCSG CNS9204) or the Low Grade Glioma Protocol (UKCCSG CNS9702). All tumour samples were obtained with informed consent and were graded according to WHO criteria [28]. There were 35 PA, 6 DA, 4 AA, 1 gliomatosis cerebri (WHO grade III), and 11 GBM. Thirty-one samples were fresh frozen material collected directly from the operating theatre and 26 were short-term cultures (at passage level < 8), prepared as described by Lewandowicz et al. [29]. All tumour samples were directly adjacent to tumour tissue processed for routine histological evaluation and were first examined macroscopically to ensure that no frankly normal tissue was included in either culture preparation or DNA extraction.
DNA extraction and labelling
For fresh frozen biopsies, DNA was extracted using a QIAmp isolation kit (Qiagen, Hilden, Germany). DNA was isolated from short-term cell cultures and from normal blood from ten healthy donors for controls using Qiagen Genomic Tip 100/g columns. Tumour and control DNA was labelled by nick translation with either SpectrumGreen dUTP or SpectrumRed dUTP (Vysis, Downers Grove, IL, USA) to provide fragments 300–3,000 bp in length.
Comparative genomic hybridisation
CGH was performed as described previously [30, 31]. Briefly, 400 ng SpectrumGreen-labelled tumour DNA was co-hybridised with 200 ng SpectrumRed total female genomic reference DNA (Vysis) and 10 μg human COT-1 DNA to denatured normal metaphase slides (Vysis) for 72 h at 37°C. Slides were then washed and counterstained with 4,6-diamidino-2-phenylindole (DAPI) in antifade solution (Vysis). Control CGH experiments using normal DNA alone were performed with each set of tumour samples. All tumour hybridisations were repeated at least once.
Metaphase images with uniform hybridisation were acquired with a Olympus BX41 epifluorescence microscope equipped with a Hamamatsu ORCA-ER digital camera. Mean ratios of SpectrumGreen to SpectrumRed signal intensities were calculated with Quips Karyotyper software (Digital Scientific, Cambridge, UK). Between 10 and 20 metaphases were analysed and averaged to yield CGH profiles for each tumour. Upper and lower thresholds values of >1.2 and <0.8 were used to interpret gain or loss of chromosomal material, and high-copy-number amplifications (HCNAs) were defined by a tumour/reference ratio of >1.4. For the normal blood controls, the mean green-to-red ratios remained between 1.2 and 0.8 along the whole length of all chromosomes. Copy number changes were scored only if they were present in repeat hybridisations, Particular care was taken to ensure that imbalances at the G–C rich regions at 1p32-36, 16p, 19, and 22 were not artifacts. Imbalances at these regions were scored only if they were also present in a reverse hybridisation experiment using SpectrumRed-labelled tumour DNA and SpectrumGreen total female genomic reference DNA.
Fluorescence in-situ hybridisation
Touch preparations of biopsy samples were digested in 0.25 mg/ml proteinase K solution for between 2 and 5 min before use. Samples were evaluated for sufficient digestion by counterstaining with propidium iodide (2.5 μg/ml) and viewing using a FITC/propidium Iodide filter set. Appropriately digested tissue had little background fluorescence, nuclei evenly and brightly stained with PI, and clearly defined nuclear borders. Short-term cell cultures at low passage numbers were harvested for chromosomal preparations according to standard procedures.
Bacterial artificial chromosome (BAC) clones for CDK6 (RP11-345K8), MDM2 (RP11-755J10) and CDK4 (RP11-571M6) were purchased as LB agar stab cultures from BACPAC resources (Children’s Hospital, Oakland, CA, http://bacpac.chori.org). DNA was extracted using a plasmid midi kit according to the supplier’s instructions (Qiagen) and labelled by nick translation with SpectrumGreen dUTP (Vysis). Commercial probes for detection of 1p36, EGFR (7p12), MET (D7S522, 7q31), and c-myc (8q24), and centromere probes for chromosomes 1, 7, 8, and 12 were purchased from Vysis. Slides were denatured for 2 min in 70% formamide, 2X SSC for 5 min at 73°C followed by dehydration through a 70, 85, and 100% alcohol series for 1 min each. Gene probes were cohybridised with the appropriate differentially labelled centromere probe to denatured slides for 24 h according to the suppliers’ recommendations. Slides were washed in 0.4X SSC/0.3% NP-40 at 73°C for 2 min and 2X SSC/0.1% NP-40 at room temperature for 1 min and counterstained with DAPI in antifade solution (Vysis). For each sample, hybridisation signals from a minimum of 100 nuclei were evaluated.
Statistical analysis
Univariate and multivariate statistical analyses were performed to compare the incidence of chromosomal gains and losses between different histological and clinical subgroups of tumours and to assess the effects of clinicopathological variables (patient age, sex, tumour histology, tumour location, and extent of surgical resection) and genomic aberrations on outcome. Association in contingency tables was assessed by Fisher’s exact test. Estimates of overall survival were calculated using the Kaplan–Meier method and statistical analyses were performed using the log-rank test. A P value of <0.05 was considered to be statistically significant at the 95% confidence level.
Results
CGH analysis
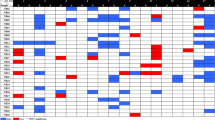
CGH analysis was successfully carried out on all 57 samples. There was no difference in the frequency of aberrations observed between fresh frozen tissue and short-term cell cultures (P = 1.000, RR 0.9 95% CI 0.39–2.06). The cumulative chromosomal losses and gains are summarised in Fig. 1 and Table 1. Regions of genomic imbalance were detected in 17 tumours (29%). Multiple copy number alterations (CNAs) were observed, ranging from 1 to 22 per tumour (mean 6.05). In cases where HCNA was seen in addition to low-level gain on a chromosome arm, they were classified as two separate changes. With the exception of the Y chromosome, all chromosomes were involved at least once in CNAs. In the overall sample group, the most common regions of gain involved chromosome arms 6q (six cases, 10.3%), 2q and 7q (five cases, 8.6%), and 1p, 1q, 12q and 18q (four cases, 6.8%). The most common regions of loss included chromosome arm 16p (six cases, 10.3%) and 12q and 16q (four cases, 6.8%). Four tumours had sole abnormalities comprising gain 1p12-qter, gain 6q, gain 7q, and loss 18p11-q21. Twelve independent regions of HCNA were observed in five tumours comprising 1p32-34, 1q21, 2q24-32, 7p11-14, 7q22-31, 7q31-33, 9q32-34, 12p11.2, 13q21-31, 17p, 19q, and 20.
Summary of copy number changes in 57 paediatric astrocytoma, detected by comparative genomic hybridisation. Vertical boxes to the right of chromosome represent gains, vertical boxes to the left represent losses and bold regions represent high copy number amplification. Grey-shaded boxes represent gains pilocytic astrocytoma, empty boxes represent diffuse astrocytoma, checked boxes represent anaplastic astrocytoma and black boxes represent glioblastoma multiforme
Pilocytic astrocytoma
CNAs were infrequent in PA with 5/35 (14.3%) tumours having alterations. IN2466 had a sole abnormality (gain of 6q) and IN2017 showed gain of the long arm of chromosome 7 (including HCNA at 7q22-31) only. HCNA was also seen in IN1524 at 13q21-31. Gain of 6q11-23 was present in three tumours and gain of 7q22-31 and 12q14-21 were each seen in two tumours. Loss of 1p31-pter and 16p were observed in two tumours.
Diffuse astrocytoma
Three of six (50%) DA showed regions of loss ranging from 2 to 4 per tumour (mean 2.66) and each alteration was seen in only one tumour. No regions of gain or HCNA were observed in DA.
Anaplastic astrocytoma/gliomatosis cerebri
There were five tumours in this study corresponding to WHO grade III, two of which had CNAs. IN3180 (gliomatosis cerebri) had a sole region of gain at 1p12-qter (Fig. 2). IN3032 had eight regions of imbalance including two regions of HCNA at 7p11-14 and 12p11.2.
a Three-colour digital image of CGH analysis of paediatric gliomatosis cerebri IN3180 after hybridisation of SpectrumGreen-labelled tumour DNA with SpectrumRed-labelled normal DNA. Chromosome 1 is indicated showing increased green fluorescence on the q arm. b Ratio profiles of CGH analysis in IN3180 showing gain of 1q
Glioblastoma multiforme
Seven of 11 (63.6%) GBM had CNAs, ranging from 1 to 22 per tumour (mean 9.7). Two tumours had regions of HCNA: IN2240 had two amplicons at 2q24-32 and 7q31-33, and IN699 had six amplicons encompassing 1p32-34, 1q21, 9q32-34, 17p, 19q, and 20q. The most common alterations in GBM were gain of 1q and 18q (four cases, 36%). Gain of 1p and 6q were seen in three cases (27%). The most common regions of loss were 12q23-qter, and monosomy 16 (3 cases, 27%).
FISH analysis
Results of FISH analysis are summarized in Table 2.
Chromosome 1
A 1p36-specific probe was used to validate regions of loss at 1p observed in three tumours by CGH analysis. IN2003 had a predominant population (74%) with fewer copies of the 1p36 probe compared with the centromere probe (Fig. 3). In addition, 55% of the nuclei counted in 6* and 63.5% in 12* also showed fewer copies of the 1p36 probe than the centromere, suggesting that loss of the 1p region often seen in CGH analysis is not experimental artifact but genuine genomic loss.
a Ratio profile of chromosome 1 in paediatric pilocytic astrocytoma IN2003, showing a region of loss at 1p35-pter. b Three-colour digital image of chromosome 1 in IN2003, showing a red region (indicating loss) on 1p. c Fluorescence in-situ hybridisation of IN2003 demonstrating two copies of chromosome 1 centromere probe (red) and only one copy of the 1p36 specific probe (green)
Chromosome 7
The copy number status of three genes (EGFR, CDK6, and Met) were investigated on chromosome 7. CGH analysis demonstrated IN699 to have a region of gain spanning 7p11-21 and additional copies of EGFR (7p12) were present in 36% of nuclei compared with the Cep 7 centromere probe in IN699. Extra copies of CDK6 (7q21-22) were identified in IN1524 (58% of nuclei), IN699 (39% of nuclei), and IN2017 (39.5% of nuclei) compared with the Cep 7 centromere probe. These three samples had shown gain of 7q, and IN2017 had an amplicon at 7q22-31. IN2017 had additional copies of Met (7q31) in 56.6% of nuclei. Despite having a region of gain at 7q22-31, most nuclei (53%) in IN1524 showed no extra copies of Met. There was no evidence of amplification of any of the chromosome 7 genes examined.
Chromosome 8
C-myc (8q24) copy number status was assessed in four tumours (IN699, 6*, 11* and 12*). Additional copies of c-myc compared with the Cep 8 centromere probe were observed in IN699 and sample 6*. Sample 12* appeared to have two populations of cells present, those with extra copies of c-myc (36%) and a population which had equal numbers of Cep 8 and c-myc (42%). There was no evidence of amplification of c-myc in these samples.
Chromosome 12
Extra copies of CDK4 (12q14) were seen in IN699 (67% of nuclei) and 6* (51% of nuclei). Sample 8* showed most nuclei (65%) to have equal numbers of gene probe and centromere probe. Sample 11* showed 53.5% of nuclei to have loss of the CDK4 probe compared with the centromere probe—this sample had demonstrated loss of 12q by CGH analysis. Only one sample was seen to have extra copies of MDM2 (12q14.3-q15). Fifty-seven percent of IN699 nuclei had more copies of gene probe than centromere probe. Sample 11* again showed the most nuclei (62.6%) to have loss of this gene probe. Samples 6* and 8* both had equal copies of centromere and gene probe present (51.5 and 58%, respectively). There was no evidence of amplification of CDK4 or MDM2 in these samples.
Correlation of CNAs with clinicopathological criteria
Because of the small number of tumours with CNAs, we combined the CGH data from this investigation with those from our previous study in order to increase the statistical power of our analysis [27]. Follow-up data was available for 51 of the patients in this study and seven from our earlier study [27]. Overall survival was 78% at 5 years and 74% at 10 years. There was a significant adverse relationship between grade of malignancy and outcome (log-rank test, P ≤ 0.0001) (Fig. 4a). Survival at 5 years was 100% for patients with PA and DA, 60% for patients with AA, and 20% for patients with GBM. The extent of surgical resection also affected survival. Those patients who underwent partial resection had a poorer prognosis than patients who had macroscopic removal of tumour. The 5-year survival for patients with macroscopic removal was 96% compared with 65% for patients having partial resection. This finding was statistically significant, P = 0.0310 (hazard ratio 0.2171, 95% CI of ratio 0.082 to 0.8873) but was not independent of tumour grade. Outcome was not affected by patient sex, age at diagnosis (<3 years vs. >3 years), or tumour location (intracranial vs. brainstem).
a Survival of paediatric astrocytoma patients is dependent on tumour grade (P ≤ 0.0001); b The presence of copy number aberrations is associated with poor prognosis in paediatric astrocytoma patients (P = 0.0005) but is not independent of tumour grade; c Gain on 12q is associated with poor survival in paediatric patients with malignant astrocytoma (AA and GBM) (P = 0.0039); d The presence of HCNA is associated with poor outcome in paediatric patients with malignant astrocytoma (P = 0.0085)
In the overall group of tumours, there was no association between alterations on individual chromosome arms and any clinicopathological criteria. However, the presence of CNAs was significantly associated with increasing grade of malignancy (P ≤ 0.0001). The 5-year survival of patients with tumours which had CNAs was 44% compared with 88% in patients with tumours which had no aberrations (Fig. 4b). Although this finding was statistically significant (P = 0.0009, hazard ratio = 5.596, 95% CI of ratio 2.203–21.71), it was not independent of tumour grade by multivariate analysis.
The association of individual CNAs with outcome in patients with low-grade astrocytoma could not be determined because of the small number of aberrations and the near 100% survival of patients with PA and DA. In malignant astrocytoma (AA and GBM), gain of 12q and the presence of HCNA were significant adverse prognostic factors (Fig. 4c, d). Patients who had tumours with gain of 12q had a shorter overall survival than those patients with no gain on 12q (P = 0.0039, hazard ratio = 4.377, 95% CI of ratio 2.245–68.23). Similarly, patients with HCNA had a shorter survival than patients with CNAs or those with no abnormalities (P = 0.0496 hazard ratio = 3.381, 95% CI of ratio 1.003–34.56).
Discussion
To our knowledge, this study represents the largest series to date of paediatric astrocytoma analysed by CGH. This study was biassed towards PA because of the rarity of the more malignant grades of tumour in the paediatric population and also because of the previous publication of data pertaining to malignant astrocytoma from our laboratory [27]. This latest study found large regions of genomic imbalance to be infrequent events in paediatric astrocytoma; 71% of the tumours had no detectable aberrations. In agreement with previous cytogenetic studies, the presence of CNAs was significantly associated with increasing grade of malignancy (14.3% of PA, 50% of DA, 40% AA and 63.6% GBM). Individual cytogenetic studies have shown wide variation in the frequency of tumours with normal karyotypes. In PA normal karyotypes have been observed in 50, 75, or as many as 100% of tumours [22, 24, 32]. In DA reported rates range from 50 to 100% [18, 19, 22, 33, 34]. AA have been reported to have normal karyotypes in the range 0–100% of tumours analysed [16–18, 22, 23, 34, 35] and normal karyotypes have been reported in 0–50% of GBM [16–19, 22–24, 34, 35]. Combining the results from all the published data shows genomic aberrations occur in approximately 22% of PA, 31% of DA, 62% of AA, and 80% of GBM (21–31). It is possible that the frequency of copy number aberrations is under-reported in this study, because there are a number of limitations in CGH analysis of metaphase chromosomes, not least of which is the sensitivity. Copy number changes will only be detected if they are present in >50% of cells and, hence, aberrations present in a clonal subset will not be identified. Similarly, contamination of the tumour specimen with normal cells will reduce sensitivity. The resolution of analogue CGH is restricted to approximately 5–10 Mbp and, furthermore, CGH analysis will only detect loss and/or gain of DNA sequences not balanced translocations, inversions, and intragenic rearrangements.
There is still widespread debate regarding the use of cultured cells in the genetic analysis of tumours. Adult glioma short-term cultures have shown the same cytogenetic alterations in early passage (<3) and late passage cells (5–170) [36]. This suggests that aberrations are maintained in cell culture and, because these are often associated with the early stage of disease, it would indicate that alterations are not induced by the in-vitro environment. In contrast, De Witt Hamer et al. [37] reported genetic discordance between the parental tumour and derived cell cultures in 4/8 cases of glioma, using higher-resolution array CGH technology. However, a recent study analysing copy number changes in various types of GBM tumour samples has concluded that whilst HCNA of oncogenes is often lost during in-vitro culture, primary and established cell lines are superior to primary tumours for identification of genomic deletions [38]. In most of the cell cultures used in our study, DNA extraction was carried out after a relatively short time in culture (passage 4) and we found no statistical difference in the frequency of aberrations observed between fresh frozen tissue and short-term cell cultures. Importantly, HCNAs were also preserved in one cell culture (IN699). However, it is possible that some changes, particularly HCNAs, may be under-represented in the cell cultures.
The findings of this study are comparable with the small number of previous studies of paediatric astrocytoma using CGH. We have shown that fewer than 20% of PA have aberrations compared with frequencies of 22% [39], 37.5% [40], and 50% [32] in the 57 cases previously described in the literature. In our study and that of Shlomit et al. [32] multiple aberrations were seen in some tumours with gain of 6q being the most common alteration. This is in contrast with the study by Sanoudou et al. [39], which found only sole abnormalities, with frequent gains of chromosomes 6 and 7. There is a single report of CGH analysis in paediatric DA in which 2/5 (40%) cases had multiple alterations [33]. Similarly, alterations were present in 40% of samples in our study. In addition to the previous paper from our laboratory describing CGH analysis in malignant astrocytoma, one other study has reported a higher frequency of copy number aberrations in these tumours; 100% in AA and 85% in GBM [16].
The most common chromosomal imbalances in this study were gains of 2q, 6q, and 7q, and loss of 12q23-24 and 16. Gain of 2q was seen in five tumours, with the minimum overlapping region spanning 2q22-32. Gain of chromosome two has been reported previously in five paediatric AA and five GBM [17–19, 22, 34, 35]. CGH analyses have shown gain of chromosome 2 in <20% of PA and malignant astrocytoma [27, 32]. Only one structural alteration, der(2)t(1;2)(q22;q37), has been reported in a brainstem GBM [23]. There are a number of candidate genes that map within this region of gain at 2q22-32 including, I-TRAF, FRZB-1, and GRB14 [41, 42, 43].
Gain of 6q was seen in six tumours, with a minimum overlapping region of 6q12-21. Trisomy 6 has been observed at low frequency in all grades of paediatric astrocytoma [17, 18, 22, 23, 34, 35, 39, 40, 44, 45] and gain of 6q12-16 has been reported in PA, AA, and GBM [16, 27, 32, 43]. Gain of 6q was seen to be the most frequent alteration (50% of cases) in a previous study of PA with a minimum overlapping region of 6q14-16 [32]. Structural abnormalities involving 6q have also been observed in paediatric astrocytoma including, t(6;9)(q16;q22), t(6;17)(q21;p11.2), and t(6;8)(q27;q21.3) [17, 23].
Gain of 12q was seen in four cases in this study with a minimum overlapping region of 12q14-22. Overrepresentation of chromosome 12 has been observed in previous studies of paediatric astrocytoma, although at low frequencies [17, 22, 23, 26, 35, 45]. Gain of 12q has been identified in conjunction with HCNA at 12q13-pter and 12q15-21 in paediatric malignant astrocytoma [16, 27].
Loss of 12q22-24 was seen in four tumours in this study. In previous cytogenetic studies loss of 12 was reported in 2/7 GBM and a del 12(q22q23) in 1/3 AA [35]. CGH analyses have shown loss of 12q21-qter in 1 PA, 3 AA, and 3 GBM [16, 27, 32]. Single nucleotide polymorphic allele array (SNP array) has shown LOH of 12q in 38% paediatric GBM but not in other grades of paediatric astrocytoma [46]. Apaf-1 is an apoptotic protease activating factor in the p53-mediated apoptosis pathway. It is located at 12q22-23 and is broadly expressed in a number of tissue types, including brain. Recently around 40% of adult GBM have been shown to have LOH of 12q22-23 [47].
Loss of 16p was the most frequently observed deletion in this study, in six tumours. No minimum region of loss could be estimated, because the deletion appeared to span the entire short arm of the chromosome. Cytogenetic analyses of paediatric astrocytoma have reported monosomy 16 at very low frequency in all grades of tumour [17, 18, 20, 35, 48]. Previous CGH studies have observed both monosomy 16 and loss of 16p in around 20% of paediatric malignant astrocytoma [16, 27]. This region of deletion at 16p includes the tuberous sclerosis gene, TSC2, at 16p13.3. The TSC2 gene product is tuberin, which may regulate cell growth by decreasing rap-1 induced cell proliferation.
There was little evidence of the characteristic changes that have been reported in adult astrocytoma in the tumours in this series. Loss of 9p encompassing CDKN2A/B was only seen in two tumours and loss of 13 and the RB1 locus was only seen in one case. Loss of 10q was seen in one case of diffuse astrocytoma (IN380), where the region of deletion was distal to the location of the PTEN/MMAC1 gene at 10q23. Monosomy 10 was also observed in one case of GBM. Loss of 17p, the location of the p53 gene was also only seen in two tumours in this series (IN2003 and IN3032). Amplification at 7p11-14, which includes the locus of EGFR, was seen in one AA. Although some studies have found no evidence for alterations of EGFR in paediatric malignant astrocytoma [49–51], amplification of EGFR has been observed in 30% of paediatric GBM [52–54] and positive immunoreactivity has been noted in approximately 80% of paediatric malignant astrocytoma [54, 55]. SNP loci at 7p have been reported to be highly amplified in paediatric GBM and amplification of EGFR has been confirmed by semi-quantitative real-time PCR [46]. In our study, no amplification of EGFR was observed. Gain of 7q was seen in four tumours including two cases which had HCNA at 7q22-31 and 7q31-33. CDK6 maps to 7q21-22 and complexes with members of the cyclin D family. Overexpression of CDK6 may mimic mutation of p16/p15 inhibitors and override their function [56]. Three samples in our study had large proportions of cells with extra copies of the CDK6 gene probe compared with the centromere probe but there was no evidence of gene amplification. Amplification of 7q31 has been reported previously in paediatric malignant astrocytoma [16, 27]. MET, located at 7q31, encodes a transmembrane growth factor receptor tyrosine kinase whose ligand is the hepatocyte growth/scatter factor and is amplified in 20% of adult GBM [57]. However, in the samples analysed in this study there was no evidence of amplification of this gene. Amplification and overexpression of multiple genes at 12q13-14, including MDM2, GLI, SAS, CDK4, and A2MR, have been reported in a subset of adult astrocytoma [58, 59] although there have been no reports of amplification of either MDM2 or CDK4 in paediatric astrocytoma [52, 60–62]. The FISH analysis in this study confirms that neither MDM2 nor CDK4 is the target of chromosome 12 amplification in this group of tumours. DYRK2, a gene involved in cellular growth and development is located at 12q14.3-15 and has been shown to be gained and amplified in adult GBM [63].
In common with previous reports, tumour grade was the most powerful predictor of outcome in this study and patients with malignant tumours had a much poorer outcome than those with PA or DA [4, 5]. Although extent of resection had a significant impact on patient survival, it was not independent of tumour grade. Patient age did not affect outcome. Tumour progression has been associated with infant patients [4] and some studies have reported earlier recurrences in children <5 years of age at diagnosis [64, 65]. Other studies have shown no difference in survival or the risk of progression between infants and older children [2, 5, 66]. Within the malignant tumours, the presence of regions of HCNA was significantly associated with shorter survival, a finding which has not been previously reported in paediatric astrocytoma. Gain of 12q was also associated with a poor outcome in patients with malignant tumours. Gain of 12q22 has been associated with poor prognosis in fibrosarcoma [67] and with some forms of adult GBM [68]. However, there have been no previous reports of a correlation between outcome and 12q gain in paediatric malignant astrocytoma. Gain of 1q has previously been shown to be associated with shorter survival in children with AA compared to those with GBM [16]. There was no association between outcome and the presence of gain of 1q in the patients in this study.
In summary, this study has shown paediatric astrocytoma to have a low frequency of genetic alterations that differ significantly from those seen in adult astrocytoma. The presence of chromosome aberrations is associated with increasing tumour malignancy. The data from this study and our earlier publication have indicated several factors which might be useful as potential prognostic markers, including the presence of high-copy number amplification and gain of chromosome 12q in malignant astrocytoma. FISH analysis has confirmed loss of 1p36 in a subset of these tumours and has shown no amplification of genes commonly associated with adult astrocytoma namely, EGFR, MET, CDK4, c-myc, CDK6, and MDM2. This study provides further evidence that the pattern of genetic aberrations in paediatric astrocytoma is markedly different from those reported in adult tumours.
References
Davis FG, Freels S, Grutsch J, Barlas S, Brem S (1998) Survival rates in patients with primary malignant brain tumours stratified by patient age and tumour histological type: an analysis based on surveillance, epidemiology, and end results (SEER) data, 1973–1991. J Neurosurg 88:1–10
Pollack IF, Claassen D, Al-Shboul Q, Janosky JE, Deutsch M (1995) Low grade gliomas of the cerebral hemispheres in children: an analysis of 71 cases. J Neurosurg 82:536–547
Wallner K, Gonzales M, Edwards M, Wara W, Sheline G (1988) Treatment results of juvenile pilocytic astrocytoma. J Neurosurg 69:171–176
Vinchon M, Ruchoux MM, Soto-Ares G, Nicolas R, Dhellemmes P (2001) Cerebellar gliomas in infants: specificity, pathology and outcome. Childs Nerv Syst 17:31–36
Fisher BJ, Leighton CC, Vujovic O, MacDonald DR, Stitt L (2001) Results of a policy of surveillance alone after surgical management of pediatric low-grade gliomas. Int J Radiat Oncol Biol Phys 51:704–710
Orr LC, Fleitz J, McGavran L, Wyatt-Ashmead HM, Foreman NK (2002) Cytogenetics in paediatric low-grade astrocytomas. Med Pediatr Oncol 38:173–177
Albright A, Guthkelch A, Packer R (1986) Prognostic factors in pediatric brain-stem gliomas. J Neurosurg 65:751–755
Kretschmar C, Tarbell N, Barnes P (1993) Pre-irradiation chemotherapy and hyperfractionated radiation therapy 66 Gy for children with brain stem tumours. A phase II study of the Pediatric Oncology Group. Protocol 8833. Cancer 72:1404–1413
Littman P, Jarret P, Bilanuk L (1982) Pediatric brainstem gliomas. Cancer 45:2787–2792
Pencalet P, Maixner W, Sainte-Rose C, Lellouch-Tubiana A, Cinalli G, Zerah M, Pierre-Kahn A, Hoppe-Hirsch E, Bourgeois M, Renier D (1999) Benign cerebellar astrocytomas in children. J Neurosurg 90:265–273
Packer RJ (1994) Diagnosis and treatment of pediatric brain tumours. Curr Opin Neurol 7:484–491
Schneider JH, Raffel C, McComb JG (1992) Benign cerebellar astrocytomas of childhood. Neurosurgery 30:58–62
Strange P, Wohlert L (1982) Primary brainstem tumours. Acta Neurochir 62:219–232
Smith J, Tachibana I, Passe S, Huntley B, Borell T, Iturria N, O’Fallon J, Schaefer P, Scheithauer B, James C, Buckner J, Jenkins R (2001) PTEN mutation, EGFR amplification and outcome in patients with anaplastic astrocytoma and glioblastoma multiforme. J Natl Cancer Inst 93:1246–1256
Ichimura K, Bolin MB, Goike HM, Schmidt EE, Moshref A, Collins VP (2000) Deregulation of the p14ARF/MDM2/p53 pathway is a prerequisite for human astrocytic gliomas with G1-S transition control gene abnormalities. Cancer Res 60:417–424
Rickert CH, Strater R, Kaatsch P, Wassman H, Jurgens H, Dockhorn-Dworniczak B, Paulus W (2001) Pediatric high grade astrocytomas show chromosomal imbalances distinct from adult cases. Am J Pathol 158:1525–1532
Agamanolis DP, Malone JM (1995) Chromosomal abnormalities in 47 pediatric brain tumours. Cancer Genet Cytogenet 81:125–134
Bhattacharjee MB, Armstrong DD, Vogel H, Cooley LD (1997) Cytogenetic analysis of 120 primary pediatric brain tumours and literature review. Cancer Genet Cytogenet 97:39–53
Fujii Y, Hongo T, Hayashi Y (1994) Chromosome analysis of brain tumours in childhood. Genes Chromosom Cancer 11:205–215
Griffin CA, Hawkins AL, Packer RJ, Rorke LB, Emanuel BS (1988) Chromosome abnormalities in pediatric brain tumours. Cancer Res 48:175–180
Griffin CA, Long PP, Carson BS, Brem H (1992) Chromosome abnormalities in low grade central nervous system tumours. Cancer Genet Cytogenet 60:67–73
Karnes PS, Tran TN, Cui MY, Raffel C, Gilles FH, Barranger JA, Ying KL (1992) Cytogenetic analysis of 39 paediatric central nervous system tumours. Cancer Genet Cytogenet 59:12–19
Neumann E, Kalousek DK, Norman MG, Steinbok P, Cochrane DD, Goddard K (1993) Cytogenetic analysis of 109 pediatric central nervous system tumours. Cancer Genet Cytogenet 71:40–49
Sainati L, Bolcato S, Montaldi A, Celli P, Stella M, Leszl A, Silvestro L, Perilongo G, Cordero di Montezemolo L, Basso G (1996) Cytogenetics of pediatric central nervous system tumours. Cancer Genet Cytogenet 91:13–27
Sawyer JR, Swanson CM, Roloson GJ, Longee DC, Chadduck WM (1992) Cytogenetic findings in a case of pediatric glioblastoma. Cancer Genet Cytogenet 64:75–79
Vagner-Capodano AM, Gentet JC, Gambarelli D, Pellissier JF, Gouzien M, Lena G, Genitori L, Choux M, Raybaud C (1992) Cytogenetic studies in 45 pediatric brain tumours. Pediatr Haematol Oncol 9:223–235
Warr T, Ward S, Burrows J, Harding B, Wilkins P, Harkness W, Hayward R, Darling J, Thomas D (2001) Identification of extensive genomic loss and gain by comparative genomic hybridisation in malignant astrocytoma in children and young adults. Genes Chromosom Cancer 31:15–22
Kleihues P, Burger PC, Scheithauer BW (1993) The new WHO classification of brain tumours. Brain Pathol 3:255–268
Lewandowicz GM, Harding B, Harkness W, Hayward R, Thomas DG, Darling JL (2000) Chemosensitivity in childhood brain tumours in vitro: evidence of differential sensitivity to lomustine (CCNU) and vincristine. Eur J Cancer 36:1955–1964
Kallioniemi A, Kallioniemi OP, Piper J, Isola J, Waldman FM, Gray JW, Pinkel D (1994) Optimizing comparative genomic hybridisation for analysis of DNA sequence copy number changes in solid tumours. Genes Chromosom Cancer 10:231–243
Kallioniemi A, Kallioniemi OP, Sudar D, Rutovitz D, Gray JW, Waldman F, Pinkel D (1992) Comparative genomic hybridisation for molecular cytogenetic analysis of solid tumours. Science 258:818–821
Shlomit R, Ayala AG, Michal D, Ninett A, Frida S, Boleslaw G, Gad B, Gideon R, Shlomi C (2000) Gains and losses of DNA sequences in childhood brain tumours analysed by comparative genomic hybridisation. Cancer Genet Cytogenet 121:67–72
Hirose Y, Aldape K, Chang S, Lamborn K, Berger M, Feuerstein B (2003) Grade II astrocytomas are subgrouped by chromosome aberrations. Cancer Genet Cytogenet 142:1–7
Roberts P, Chumas PD, Picton S, Bridges L, Livingstone JH, Sheridan E (2001) A review of the cytogenetics of 58 pediatric brain tumours. Cancer Genet Cytogenet 131:1–12
Bigner SH, McLendon RE, Fuchs HE, McKeever PE, Friedman HS (1997) Chromosomal characteristics of childhood brain tumours. Cancer Genet Cytogenet 97:125–134
Westphal M, Hansel M, Hamel W, Kunzmann R, Holzel F (1994) Karyotype analyses of 20 human glioma cell lines. Acta Neurochir 126:17–26
De Witt Hamer PC, Van Tilborg AAG, Eijk PP, Troost D, Van Noorden CJF, Ylstra B, Leenstra S (2008) The genomic profile of human malignant glioma is altered early in primary cell culture and preserved in spheroids. Oncogene 27:2091–2096
Solomon DA, Kim J-S, Ressom HW, Sibenaller Z, Ryken T, Jean W, Bigner D, Yan H, Waldman T (2009) Sample bias in the analysis of cancer genomes. Cancer Res 69: 5630–5633
Sanoudou D, Tingby O, Ferguson-Smith MA, Collins VP, Coleman N (2000) Analysis of pilocytic astrocytoma by comparative genomic hybridisation. Br J Cancer 82:1218–1222
Schrock E, Blume C, Meffert MC, du Manoir S, Bersch W, Kiessling M, Lozanowa T, Thiel G, Witkowski R, Ried T, Cremer T (1996) Recurrent gain of chromosome arm 7q in low grade astrocytic tumours studied by comparative genomic hybridisation. Genes Chromosom Cancer 15:199–205
Rothe M, Xiong J, Shu HB, Williamson K, Goddard A, Goeddel DV (1996) I-TRAF is a novel TRAF-interacting protein that regulates TRAF-mediated signal transduction. Proc Natl Acad Sci USA 93:8241–8246
Leyns L, Bouwmeester T, Kim SH, Piccolo S, de Roberts EM (1997) Frzb-1 is a secreted antagonist of Wnt signaling expressed in the spemann organizer. Cell 88:747–756
Shen R, Fan J-B, Campbell D, Chang W, Chen J, Doucet D, Yeakley J, Bibikova M, Wickham Garcia E, McBride C, Steemers F, Garcia F, Kermani B, Gunderson K, Oliphant A (2005) High-throughput SNP genotyping on universal bead arrays. Mutat Res 573:70–82
Kucerova H, Stejskalova E, Vicha A, Tichy M, Chanova M, Sumerauer D, Koutecky J, Eckschlager T (2000) Gene aberrations in childhood brain tumours. Folia Biol (Praha) 46:187–190
White FV, Anthony DC, Yunis EJ, Tarbell NJ, Scott RM, Schofield DE (1995) Nonrandom chromosomal gains in pilocytic astrocytomas of childhood. Hum Pathol 26:979–986
Wong K, Tsang Y, Chang Y-M, Su J, Di Francesco A, Meco D, Riccardi R, Perlaky L, Dauser R, Adesna A, Bhattacharjee M, Chintagumpala M, Lau C (2006) Genome-wide allelic imbalance analysis of pediatric gliomas by single nucleotide polymorphic allele array. Cancer Res 66:11172–11178
Watanabe T, Hirota Y, Arakawa Y, Fujisawa H, Tachibana O, Hasegawa M, Yamashita J, Hayashi Y (2003) Frequent LOH at chromosome 12q22-23 and Apaf-1 inactivation in glioblastoma. Brain Pathol 13:431–439
Wernicke C, Thiel G, Lozanova T, Vogel S, Witkowski R (1997) Numerical aberrations of chromosomes 1, 2 and 7 in astrocytomas studied by interphase cytogenetics. Genes Chromosom Cancer 19:6–13
Cheng Y, Ng HK, Zhang SF, Ding M, Chung-Sean Pang J, Zheng J, Poon WS (1999) Genetic alterations in pediatric high grade astrocytomas. Hum Pathol 30:1284–1290
Raffel C, Frederick L, O’Fallon JR, Atherton-Skaff P, Perry A, Jenkins RB, James CD (1999) Analysis of oncogene and tumour suppressor gene alterations in pediatric malignant astrocytomas reveals reduced survival for patients with PTEN mutations. Clin Cancer Res 5:4085–4090
Sung T, Miller DC, Hayes RL, Alonso M, Yee H, Newcomb EW (2000) Preferential inactivation of the p53 tumour suppressor pathway and lack of EGFR amplification distinguish de novo high grade paediatric astrocytomas from de novo adult astrocytomas. Brain Pathol 10:249–259
Von Deimling A, Fimmers R, Schmidt MC, Bender B, Fassbender F, Nagel J, Jahnke R, Kaskel P, Duerr E, Koopman J, Maintz D, Steinbeck S, Wick W, Platten M, Mueller DJ, Przkora R, Waha A, Blumcke B, Wellenreuther R, Meyer-Puttlitz B, Schmidt O, Mollenhauer J, Poustka A, Stangl AP, Lenartz D, Von Ammon K, Henson JW, Schramm J, Louis DN, Wiestler OD (2000) Comprehensive allelotype and genetic analysis of 466 human nervous system tumours. J Neuropathol Exp Neurol 59:544–558
Rasheed BKA, McLendon RE, Herndon JE, Friedman HS, Friedman AH, Bigner DD, Bigner SH (1994) Alterations of the TP53 gene in human gliomas. Cancer Res 54:1324–1330
Bredel M, Pollack IF, Hamilton RL, James CD (1999) Epidermal growth factor receptor expression and gene amplification in high-grade non-brainstem gliomas of childhood. Clin Cancer Res 5:1786–1792
Maruno M, Ninomiya H, Muhammad A, Hirata M, Kato A, Yoshimine T (2000) Whole genome analysis of human astrocytic tumours by comparative genomic hybridisation. Brain Tumor Pathology 17:21–27
Kleihues P, Davis RL, Ohgaki H, Burger PC, Westphal MM, Cavenee WK (2000) Diffuse astrocytoma. In: Kleihues P, Cavenee WK (eds) Pathology and genetics of tumours of the nervous system. IARC Press, Lyon, pp 22–26
Fischer U, Mueller H, Sattler H, Feiden K, Zang K, Meese E (1995) Amplification of the MET gene in glioma. Genes Chromosom Cancer 12:63–65
Reifenberger G, Liu L, Ichimura K, Schmidt EE, Collins VP (1993) Amplification and overexpression of the MDM2 gene in a subset of human malignant gliomas without p53 mutations. Cancer Res 53:2736–2739
Reifenberger J, Reifenberger G, Liu L, James CD, Wechsler W, Collins VP (1994) Molecular genetic analysis of oligodendroglial tumours shows preferential allelic deletions on 19q and 1p. Am J Pathol 145:1175–1190
Kraus JA, Felsberg J, Tonn JC, Reifenberger G, Pietsch T (2002) Molecular genetic analysis of the TP53, PTEN, CDKN2A, EGFR, CDK4 and MDM2 tumour-associated genes in supratentorial primitive neuroectodermal tumours and glioblastomas of childhood. Neuropathol Appl Neurobiol 28:325–333
Biernat W, Dębiec-Rychter M, Liberski P (1998) Mutations of TP53, amplification of EGFR, MDM2 and CDK4, and deletions of CDKN2A in malignant astrocytomas. Pol J Pathol 49:267–271
Di Sapio A, Morra I, Pradotto L, Guido M, Schiffer D, Mauro A (2002) Molecular genetic changes in a series of neuroepithelial tumours of childhood. J Neurooncol 59:117–122
Maher E, Brennan C, Wen P, Durso L, Ligon K, Richardson A, Khatry D, Feng B, Sinha R, Louis D, Quackenbush J, McL.Black P, Chin L, DePinho R (2006) Marked genomic differences characterize primary and secondary glioblastoma subtypes and identify two distinct molecular and clinical secondary glioblastoma entities. Cancer Res 66:11502–11513
Davis C, Joglekar V (1981) Cerebellar astrocytomas in children and young adults. J Neurol Neurosurg Psychiatry 44:820–828
Ilgren E, Stiller C (1987) Cerebellar astrocytomas: clinical characteristics and prognostic indices. J Neurooncol 4:293–308
Smoots DW, Geyer JR, Lieberman DM, Berger MS (1998) Predicting disease progression in childhood cerebellar astrocytoma. Childs Nerv Syst 14:636–648
Schmidt H, Taubert H, Würl P, Kappler M, Lange H, Bartel F, Bache M, Holzhausen H-J, Hinze R (2002) Gains of 12q are the most frequent genomic imbalances in adult fibrosarcoma and are correlated with a poor outcome. Genes Chromosom Cancer 34:69–77
Weber RG, Sommer C, Albert FK, Kiessling M, Cremer T (1996) Clinically distinct subgroups of glioblastoma multiforme studied by comparative genomic hybridisation. Lab Investig 74:108–119
Acknowledgements
Supported by the Samantha Dickson Brain Tumour Trust and Brain Tumour UK. We thank Digital Scientific UK for assistance with digital imaging.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ward, S.J., Karakoula, K., Phipps, K.P. et al. Cytogenetic analysis of paediatric astrocytoma using comparative genomic hybridisation and fluorescence in-situ hybridisation. J Neurooncol 98, 305–318 (2010). https://doi.org/10.1007/s11060-009-0081-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-009-0081-4