Abstract
Purpose The hypothesis addressed by this study is that a glutamine synthetase (GS) deficiency in neoplastic astrocytes is a possible molecular basis associated with seizure generation in glioblastoma multiforme (GBM). Methods Quantitative Western blot analysis of GS was performed in 20 individuals operated for malignant glioma. Results The levels of GS in patients with GBM and epilepsy were significantly lower (range 0.04–1.15; mean 0.35 ± 0.36; median 0.25) than in non-epileptic GBM individuals (range 0.78–3.97; mean 1.64 ± 0.99; median 1.25; P = 0.002). No relationship has been found between histological features (i.e. necrosis, gliosis, stroma, inflammatory cells, giant cells, and haemosiderine) and GS expression or epilepsy. Discussion Even though the epileptogenesis in glioma is multifactorial, it is conceivable that a down-regulation of GS may have an important pro-epileptogenic role in GBM, through the slowing of glutamate-glutamine cycle. This study suggests that seizures in GBM are coupled with a highly localized enzyme deficiency. The manipulation of GS activity might constitute a novel principle for inhibiting seizures in patients with glioma epilepsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The epileptic neuronal activity is characterized by abnormal synchronization, excessive glutamate excitation and/or inadequate GABA inhibition, affecting small or large neuronal aggregates (ictogenesis) [1]. Although neurons play a prominent role in the initiation and the propagation of a seizure in time and space, increasing evidence suggests that astrocytes are critically involved in the biochemical/histological process of initiation and maturation of an “epileptogenic focus” (epileptogenesis) [1–5]. Gliosis is, in fact, a constant feature in the otherwise normal appearing tissue of epileptic patients [6]. Astrocytes guarantee extracellular homeostasis by removing extracellular K+ and, via the enzyme glutamine synthetase (GS), they protect neurons against excitotoxicity by taking up ammonia and glutamate in excess and converting the latter into glutamine [7]. Glutamine synthetase is an enzyme mainly present in glial cells [8] and its distribution and expression are more pronounced in the brain regions where glutamic acid-transmitting synapses are abundant [9–11]. Glutamine synthetase is present in normal, reactive, and neoplastic astrocytes and its increase during astrocyte maturation indicates that enzyme activity is associated with astrocyte differentiation [10, 12, 13]. In fact, all astrocytoma show positive reaction to GS with an inverse correlation between histological malignancy and the degree of GS expression [14, 15].
A loss of GS has been reported in mesial temporal sclerosis hippocampus with epilepsy [16] and in the brain of seizure-prone gerbils compared with animals not prone to seizures [17], suggesting that a GS deficiency in astrocytes may be a possible molecular basis for extracellular glutamate accumulation and seizure generation [18].
Even though the epileptogenesis in glioma is multifactorial [19], it is conceivable that a down-regulation of GS in astrocytes may have an important pro-epileptogenic role, through the slowing of glutamate–glutamine cycle [20] and glutamate accumulation [21].
The hypothesis addressed by this study is that a GS deficiency in neoplastic astrocytes is a possible molecular basis associated with seizure generation in glioblastoma multiforme (GBM).
Methods
Central nervous system samples were obtained from 20 individuals (10 males and 10 females) operated for malignant glioma and prospectively followed for 2 years from 1 April 2004 at the Department of Neurosurgery, Bolzano, Italy. Age at the GBM diagnosis ranged from 33 to 69 years (mean 56 ± 11). Symptoms at the onset of GBM were: epilepsy (9 patients, 45%), headache (4, 20%), focal motor neurological deficit (3, 15%), psychiatric symptoms (1, 5%), visual deficit (1, 5%), and cognitive impairment (2, 10%). The epilepsy diagnosis was made on the basis of clinical and electroencephalographic criteria. Patients were followed through clinical and MRI examinations every 3 months or less, if necessary. At the last evaluation, recurrence of GBM was radiologically and/or clinically evident in 13 (65%) individuals. Symptoms at the GBM recurrence were: epilepsy in 1 (8%) case, focal motor neurological deficit in 6 (46%), and none (only radiological evidence) in 6 (46%). On the basis of the epilepsy diagnosis, patients were divided into two groups: (1) Group A with epilepsy (10 patients); (2) Group B without epilepsy (10 patients). Epilepsy characteristics are reported in Table 1.
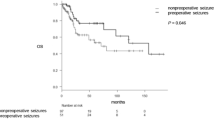
At the last evaluation, eight patients died in Group A (mean duration of disease, 11.7 months) and four in Group B (mean duration of disease, 12.4 months). Histological diagnosis was blindly re-evaluated, according to the WHO 2000 Classification and every case was scored for necrosis, gliosis, haemosiderine, giant cells, stroma, and inflammatory cells (++ = abundant, + = present; − = absent). Histological changes are summarized in Table 2.
Western blot analysis was blindly performed to quantify the expression of GS and actin in surgical specimens. A careful blinded microscopic evaluation was performed on frozen sections to distinguish between normal and neoplastic tissue; the latter was then randomly chosen and isolated on 20 consecutive sections, homogenized and sonicated in homogenization buffer [50 mM 3-(N-morpholino) propanesulphonic acid/HCl, 2 mM dithiothretiol, 0,5 mM magnesium acetate, 0,32 mM sucrose and Protease Inhibitor Complete; all from Sigma-Aldrich]. White matter was also obtained from age-matched human healthy subjects succumbed from non-neurological conditions; samples were homogenized and sonicated as described above. Each step was performed in ice to avoid protein degradation. Protein concentration was estimated according to the Bradford assay method: after creating a standard curve with serially diluted BSA (1–10 μg/ml), 1 ml of Bradford Reagent (Sigma-Aldrich) was added to each sample for 30 min. The absorbance at 595 nm was measured with a microplate reader (2550 EIA; BioRad Laboratories). The protein concentration of each sample was determined by comparing the absorbance values with the standard curve. Based on this result, appropriate amounts of homogenates from each patient were mixed with sample loading buffer (20% sucrose, 4% sodium dodecyl sulphate, 10% β-mercaptoethanol, 125 mM Tris-HCl, 0.01% bromophenol blue; all from Sigma-Aldrich), heat-denatured and loaded (4 μg protein per lane). The proteins were separated by electrophoresis on 12% polyacrylamide gels (Bio-Rad Laboratories) and transferred onto nitrocellulose membranes (Amersham Biosciences). After blocking, the membranes were incubated overnight with GS and actin (both 1:25000; Sigma-Aldrich) primary antibodies. After washing, anti-rabbit IgG-HRP conjugated (1:5000; Amersham Biosciences) was added, followed by ECL Advanced Detection kit. All samples were tested for GS and actin in the same western blotting session and each sample was tested at least twice. The GS antibody gave a single band at 45 kDa, whereas the actin signal was evident at 42 kDa (Fig. 1). The substitution of the primary antibodies with normal serum cancelled the staining completely.
Western blot of glutamine synthetase in epileptic (group A) and non-epileptic (group B) glioma patients. Each lane corresponds to a patient’s sample, numbered as in Table 1. A band corresponding to glutamine synthetase (GS) is visible at about 45 kDa, while that of actin (ACT) at 42 kDa. In both cases, bands visible at lower MW represents degradation products
Each radiographic film was digitalized using a computing densitometer (Power Look 1120, UMAX) and a global background subtraction was performed. After zooming until individual pixels were visible, the bands were traced manually and subsequently the values of each band were calculated. The relative expression of GS of a given sample was obtained dividing the value of GS by actin.
Results
The histological diagnosis was GBM (14 patients, 70%), giant cell GBM (2, 10%) and GBM with oligodendroglial component (4, 20%). Glioblastoma multiforme localization was: frontal in 6 patients, fronto-temporal in 2, temporal in 7, temporo-occipital in 2, fronto-parietal in 1, parietal in 1, and parieto-occipital in 1.
No relationship has been found between the frequency of epilepsy and GBM lateralization (Group A: 7/10 right hemisphere; Group B: 8/10 right hemisphere) or GBM localization or p53 and EGRF expression (Table 3).
Interestingly, the relative expression of GS according to Western blot analysis in the samples from GBM patients with epilepsy (range 0.04–1.15; mean 0.35 ± 0.36; median 0.25) was significantly lower than in the group without epilepsy (range 0.78–3.97; mean 1.64 ± 0.99; median 1.25; P = 0.002), whereas the mean of GS expression in normal control was 2.9 ± 0.3.
No relationship has been found between the different histological features considered (i.e. necrosis, gliosis, stroma, inflammatory cells, giant cells, and haemosiderine) and GS expression or epilepsy (Table 2).
Discussion
Epilepsy incidence in gliomas ranges between 30 and 80% and GBMs are less epileptogenic than the more benign brain tumors [22]. This may be due to the usually brief duration of disease in GBM patients, who do not have enough time to develop epilepsy. Furthermore, the incessant and constant astrocyte growth might prevent the development and/or the stability of the “epileptogenic focus”. However, when present, seizures in GBM are usually more difficult to control with the common antiepileptic drugs (AED) [23]. Despite a vast literature on epilepsy and gliomas, it is still unknown if prognostic factors may indicate which glioma patients will develop seizures. For that reason, it is current practice at several Centers to treat glioma patients with AED even in the absence of seizure, although it is known that AEDs do not prevent epileptogenesis [24, 25] and most of them may also reduce antitumoral drug levels and chemotherapy efficacy [26].
The knowledge of both epilepsy prognostic factors and epileptogenesis mechanisms in gliomas may help to recognize patients with the highest seizure risk, limiting the use of AED to those cases.
Even though the epileptogenesis in glioma is multifactorial, an important role of the astrocytes can be reasonably hypothesized [19].
Experimental evidence indicates that gliosis is not only a response to seizure-induced neuronal damage, but also plays an active role in seizure development and maintenance. In the genetic absence epilepsy rats from Strasbourg model (GAERS), gliosis appears before the spike and wave abnormalities and seizures [27], and in the EL mice epilepsy model, gliosis is present in the hippocampus even in the absence of neuronal loss [28]. This shows that astrocytic modifications are not just an adaptive response to seizures, but they may be involved in the neuronal processes leading to epileptic seizures.
Astrocytes may be critically involved in epileptogenesis through their role in cellular homeostasis and in the catabolism of glutamate [2–5]. In fact, glial cells remove extracellular K+ and, via the GS enzyme, protect neurons from glutamate excitotoxicity [7]. In gliomas, GS is an astrocyte specific marker and may be of diagnostic value in cases with poor astrocytic differentiation [29]. Indeed, all astrocytomas display positive staining with GS, whose degree is related to the extent of differentiation, as the lower the degree of GS the higher will be the histological malignancy [15]. Hence, the histological malignancy-related expression of GS in astrocytomas represents a useful functional marker of tumor-composing cells [14].
We provide the evidence of a correlation between low levels of GS in tumor samples and the presence of epilepsy in GBM patients. Glutamine synthetase deficiency in astrocytes may represent a possible molecular basis for extracellular glutamate accumulation and seizure generation.
On the other hand, a loss of GS has also been found in mesial temporal sclerosis hippocampus with epilepsy, particularly in areas of neuronal loss and astroglial proliferation, such the CA1, CA3, and dentate hilus [16].
The role of GS in epilepsy is also confirmed in experimental models; in fact, GS is also deficient in the brain of seizure-prone gerbils compared with animals not prone to seizures [17]. Moreover, in the GAERS model, both a slight decrease of GS and reactive astrocytes in the thalamus are already found before the development of absence seizures [27].
In our study, significant lower levels of GS in brain tumor were present in epileptogenic GBMs as compared with non-epileptogenic GBMs. Moreover, in line with literature data [16, 17], GS deficiency was independent from gliosis. Epilepsy frequency was not related to glioma localization and other histological features (neuronal loss, haemosiderine, giant cells, inflammatory cells, stroma).
This study suggests that seizures in GBM are coupled with a localized enzyme deficiency. If this is a causal relation, a GS western blot analysis might help to identify the patient with a high risk of epilepsy who should be treated with AED. Moreover, manipulation of GS activity might constitute a novel principle for inhibiting seizures in patients with glioma epilepsy.
References
Lothman EW (1996) Basic mechanisms of seizure expression. Epilepsy Res Suppl 11:9–16
Bordey A, Sontheimer H (1998) Properties of human glial cells associated with epileptic seizure foci. Epilepsy Res 32:286–303. doi:10.1016/S0920-1211(98)00059-X
Najm I, Ying Z, Janigro D (2001) Mechanisms of epileptogenesis. Neurol Clin 19:237–250. doi:10.1016/S0733-8619(05)70017-7
Steinhäuser C, Seifert G (2002) Glial membrane channels and receptors in epilepsy impact for generation and spread of seizure activity. Eur J Pharmacol 447:227–237. doi:10.1016/S0014-2999(02)01846-0
Vessal M, Dugani CB, Solomon DA, McIntyre Burnham W, Ivy GO (2005) Might astrocytes play a role in maintaining the seizure-prone state? Brain Res 1044:190–196. doi:10.1016/j.brainres.2005.02.058
Khurgel M, Ivy GO (1996) Astrocytes in kindling: relevance to epileptogenesis. Epilepsy Res 26:163–175. doi:10.1016/S0920-1211(96)00051-4
Suárez I, Bodega G, Fernández B (2002) Glutamine synthetase in brain: effect of ammonia. Neurochem 41:123–142. doi:10.1016/S0197-0186(02)00033-5
Martinez-Hernandez A, Bell KP, Norenberger MD (1977) Glutamine synthetase: glial localization in brain. Science 195:1356–1358. doi:10.1126/science.14400
Patel AJ, Hunt A, Gordon RD, Balázs R (1982) The activities in different neural cell types of certain enzymes associated with the metabolic compartmentation of glutamate. Dev Brain Res 8:31–37. doi:10.1016/0165-3806(83)90154-2
Patel AJ, Hunt A, Tahoyrdin CSM (1983) Regional development of glutamine synthetase activity in the rat and its association with the differentiation of astrocytes. Dev Brain Res 8:31–37. doi:10.1016/0165-3806(83)90154-2
Fages C, Khelil M, Rolland B, Bridoux AM, Tardy M (1988) Glutamine synthetase: a marker of an astroglial subpopulation in primary cultures of defined brain areas. Dev Neurosci 10:47–56. doi:10.1159/000111955
Caldani M, Rolland B, Fages C, Tardy M (1982) Glutamine synthetase during mouse brain development. Experientia 38:1199–1202. doi:10.1007/BF01959739
Mearow KM, Mill JF, Vitkovic L (1989) The ontogeny and localization of glutamine synthetase gene expression in rat brain. Brain Res Mol Brain Res 6:223–232. doi:10.1016/0169-328X(89)90068-5
McCormick D, McQuaid S, McCusker C, Allen IV (1990) A study of glutamine synthetase in normal human brain and intracranial tumours. Neuropathol Appl Neurobiol 16:205–211. doi:10.1111/j.1365-2990.1990.tb01157.x
Akimoto J (1993) Immunohistochemical study of glutamine synthetase expression in normal human brain and intracranial tumors. No To Shinkei 45(4):362–368
Eid T, Thomas MJ, Spencer DD, Rundén-Pran E, Lai JCK, Malthankar GV, Kim JH, Danbolt NC, Ottersen OP (2004) Loss of glutamine synthetase in the human epileptogenic hippocampus: possible mechanism for raised extracellular glutamate in mesial temporal lobe epilepsy. Lancet 363:28–37. doi:10.1016/S0140-6736(03)15166-5
Laming PR, Cosby SL, O’Neill JK (1989) Seizures in the Mongolian gerbil are related to a deficiency in cerebral glutamine synthetase. Comp Biochem Physiol C 94:399–404. doi:10.1016/0742-8413(89)90088-1
Hertz L, Dringen R, Schousboe A, Robinson SR (1999) Astrocytes: glutamate producers for neurons. J Neurosci Res 57(4):417–428. doi:10.1002/(SICI)1097-4547(19990815)57:4<417::AID-JNR1>3.0.CO;2-N
Schaller B, Rüegg SJ (2003) Brain tumor and seizures: pathophysiology and its implications for treatment revisited. Epilepsia 44(9):1223–1232. doi:10.1046/j.1528-1157.2003.05203.x
Petroff OA, Errante LD, Rothman DL, Kim JH, Spencer DD (2002) Glutamate-glutamine cycling in the epileptic human hippocampus. Epilepsia 43:703–710. doi:10.1046/j.1528-1157.2002.38901.x
During MJ, Spencer DD (1993) Extracellular hippocampal glutamate and spontaneous seizure in the conscious human brain. Lancet 341:1607–1610. doi:10.1016/0140-6736(93)90754-5
Wrensch M, Minn Y, Chew T, Bondy M, Berger MS (2002) Epidemiology of primary brain tumors: current concepts and review of the literature. Neuro-oncol 4:278–299. doi:10.1215/15228517-4-4-278
Lund M (1952) Epilepsy in association with intracranial tumours. Acta Psychiatr Neurol Scand, Suppl 81:1–149
Glantz MJ, Cole BF, Friedberg MH, Lathi E, Choy H, Furie K, Akerley W, Wahlberg L, Lekos A, Louis S (1996) A randomized, blinded, placebo-controlled trial of divalproex sodium prophylaxis in adults with newly diagnosed brain tumours. Neurology 46:985–991
Glantz MJ, Cole BF, Forsyth PA, Recht LD, Wen PY, Chamberlain MC, Grossman SA, Cairncross JG (2000) Practice parameter: anticonvulsant prophylaxis in patients with newly diagnosed brain tumours. Report of the Quality Standard Subcommittee of the American Academy of Neurology. Neurology 54:1886–1893
Vecht CJ, Wagner GL, Wilms EB (2003) Treating seizures in patients with brain tumors: drug interactions between antiepileptic and chemotherapeutic agents. Semin Oncol 30(6(suppl. 19)):49–52. doi:10.1053/j.seminoncol.2003.11.030
Dutuit M, Didier-Bazès M, Vergnes M, Mutin M, Conjard A, Akaoka H, Belin MF, Touret M (2000) Specific alteration in the expression of glial fibrillary acid protein, glutamate deydrogenase, and glutamine synthetase in rats with genetic absence epilepsy. Glia 32:15–24. doi:10.1002/1098-1136(200010)32:1<15::AID-GLIA20>3.0.CO;2-#
Drage MG, Holmes GL, Seyfried TN (2002) Hippocampal neurons and glia in epileptic EL mice. J Neurocytol 31(8–9):681–692. doi:10.1023/A:1025747813463
Pilkington GL, Lantos PL (1982) The role of glutamine synthetase in the diagnosis of cerebral tumours. Neuropathol Appl Neurobiol 8(3):227–236. doi:10.1111/j.1365-2990.1982.tb00277.x
Author information
Authors and Affiliations
Corresponding author
Additional information
All Authors confirm that they have read the Journal’s position on issues involved in ethical publication and affirm that the work is consistent with those guidelines. All Authors disclose non conflict of interest. All Authors have been substantively involved in the study and/or the preparation of manuscript. All Authors have seen and approved the submitted version of the paper and accept responsibility for its content.
Rights and permissions
About this article
Cite this article
Rosati, A., Marconi, S., Pollo, B. et al. Epilepsy in glioblastoma multiforme: correlation with glutamine synthetase levels. J Neurooncol 93, 319–324 (2009). https://doi.org/10.1007/s11060-008-9794-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-008-9794-z