Abstract
Objective We report our experience using gamma knife radiosurgery (GKR) for brain metastasis from thyroid cancer, which is extremely rare. Methods Between 1995 and 2007, 9 patients with 26 metastatic brain tumor(s) from thyroid cancer underwent GKR. The mean patient age was 58 years (range: 10–78). Seven patients had metastases from papillary thyroid cancer, and two from medullary thyroid cancer. Five patients had solitary tumors, and four patients had multiple metastases. Three patients who had multiple metastases also underwent whole brain radiation therapy (WBRT). The mean tumor volume was 2.4 cc (range: 0.03–14.0). A median margin dose of 18.0 Gy (range: 12–20) was delivered to the tumor margin. Results Tumor control was obtained in 25 out of 26 tumors (96%). The median progression-free period after GKR was 12 months (range: 4–53). The overall median survival after GKR was 33 months (range: 5–54). There were no procedure-related complications and six patients are still living 5–54 months after GKR. Conclusions Radiosurgery is an effective and minimally invasive strategy for management of brain metastases form thyroid cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stereotactic radiosurgery (SRS) for cerebral metastases is associated with high local control rates [1–11]. Even cerebral metastases considered resistant to whole brain radiation therapy can be successfully treated with SRS [2, 12, 13]. The response rate may differ depending on the tumor histology [9, 14]. Although thyroid cancer is a relatively common malignancy that may metastasize within the body, brain metastases from thyroid cancer are extremely rare [15]. The reported incidence is approximately 1% of all cases of thyroid carcinoma [15–18]. There are only rare reports on the management of cerebral metastases from thyroid cancer [15, 17, 19]. The role of SRS has not been defined for this pathology and only scattered cases have been reported [20–22].
We retrospectively studied the outcomes of gamma knife radiosurgery (GKR) for patients with cerebral metastases from thyroid cancer. The purposes in this study were 1) to define the role and effectiveness of GKR for this rare type of brain metastasis and 2) to identify potential factors that affect tumor control after for GKR.
Patients and methods
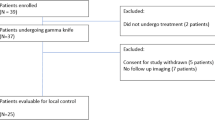
We first surveyed our total clinical experience using GKR for brain metastases (N = 2639). Between 1995 and 2007 we managed nine patients with metastatic brain thyroid cancer. The mean age of these 9 patients was 58 years (range: 10–78), and there were six male and three females (Table 1). Seven patients had papillary thyroid cancer, and two had medullary thyroid cancer. The length of time between initial thyroid cancer diagnosis and GKR varied from 6 months to 49 years (mean: 11.3 years). Previous treatment for their primary as well as any known systemic involvement began with thyroidectomy (N = 9) and Iodine-131 treatment (N = 6).
At the time of GKR, seven patients had other organ involvement including metastatic cancer in the lung, bone, liver, or gastrointestinal tract. One patient first underwent craniotomy and resection of a metastatic papillary thyroid cancer. The diagnosis of a metastatic brain cancer was diagnosed by contrast enhanced MRI or CT. Only one patient was symptomatic (gait disturbance and ipsilateral hearing impairment) due to a cerebellar metastasis with extension into the cerebellopontine angle (case 2).
Five patients had solitary cerebral metastasis at GKR, and four had multiple tumors. The total number of brain metatases managed initially was 21. Two patients underwent a second radiosurgery when they developed new metastatic tumors, and, in one of them, one recurrent tumor was also irradiated. Three of four multiple metastatic patients also underwent fractionated whole brain radiation therapy (WBRT).
Radiosurgery technique
The procedure began with rigid cranial fixation of an MRI compatible Leksell stereotactic frame (Elekta Instruments, Atlanta, GA, USA) using local anesthetic scalp infiltration (5% marcaine and 1% xylocaine), supplemented by mild intravenous conscious sedation. For stereotactic targeting a 3-D volume acquisition MRI using contrast-enhanced spoiled-Gradient Recalled Acquisition in Steady State (SPGR) images were acquired. For one patient, contrast CT was used because he had undergone bilateral stapes replacement. One patient subsequently developed a new skull base metastasis and underwent a second GKR. All patients had intracranial tumor(s) that showed contrast enhancement. A highly conformal and selective computer dose plan (Leksell Gamma Plan®) was created.
A total number of 21 tumors were treated initially. During follow-up, five new tumors were discovered and a second GKR was performed. The locations of the tumors were frontal (10), temporal (4), occipital (3), parietal (2), cerebellar hemisphere (4), cerebellar vermis (2), and clivus (1).
A total of 11 GKR procedures were performed for these 9 patients. The mean tumor volume was 2.4 cc (range: 0.03–14.0). A median margin dose of 18.0 Gy (range: 12–20) was prescribed at the tumor border. All patients received an intravenous dose of 40 mg of methylprednisolone at the conclusion of the procedure. The patients were observed for several hours and then discharged the same day. After GKR, all patients were followed with serial contrast enhanced MRI scans, which were requested at 3-month intervals.
Results
Imaging
After GKR, serial MRI evaluations were obtained in eight patients, and PET-CT was performed in one patient not eligible for MRI. The progression-free period after GKR varied from 4 months to 53 months (median: 12.0). In this study, we regarded tumor disappearance, reduction or no change in volumes as ‘tumor control’. An increased in volume by more than 20% was classified as ‘tumor progression’. Tumor control was obtained in 25 out of 26 tumors (96%). None of the treated tumors showed delayed hemorrhage (Fig. 1).
One tumor had delayed enlargement 45 months after GKR and was successfully managed by repeat radiosurgery. At the time of last follow-up (8 months) tumor control was maintained. Two patients underwent a second GKR for new tumor development. During the follow-up period, one small tumor showed minimal enlargement (< 20% by volume) 18 months after GKR, but then stabilized. The imaging changes were compatible with delayed radiation effect.
Clinical results
Patient survival GKR varied from 5 to 54 months (median: 33). During this time, there were no procedure-related complications. Adverse radiation effects were suspected in one patient who had transient symptoms that resolved with a short course of oral corticosteroids (case 1). The only symptomatic patient showed improvement in his gait disturbance (case 2).
The identified progression-free survival after GKR varied from 4 months to 53 months (median: 12.0). Six patients were alive at last follow-up. One patient died as a result of pulmonary metastasis progression. The cause of death was uncertain in two patients; however, their follow-up brain images showed control of their brain tumors prior to death.
Discussion
Although thyroid carcinoma is a relatively common malignancy that often metastasizes to other organs, spread to the brain is reported to occur in only 1% of patients [15–18]. As care is improved in systemic disease management, the potential for cerebral metastasis may become higher. Chiu et al. [17] reported 47 patients with brain metastases from thyroid cancer, but 23% had brain metastases discovered at postmortem examination.
Few studies have reported clinical outcomes for patients with metastatic thyroid brain cancer [15, 20, 22]. Surgical resection has been reported to be associated with a favorable outcome for patients with solitary metastasis [17]. McWilliams et al. [15] reported 16 cases of cerebral metastasis from thyroid cancer. They used GKR in four patients in combination with other treatment modalities such as resection, WBRT, and systemic Iodine-131. They suggested that either resection or radiosurgery are potentially beneficial [15].
In the present study, a high local control rate of 96% (25 out of 26 tumors) and prolonged progression free periods (mean: 14.6 months) was achieved. The overall median survival after GKR was 33 months with six of nine living at the conclusion of the follow-up interval. In our patients, GKR contributed to the high local control rates and longer survivals. This study only included patients with papillary and medullary thyroid cancers. None of our patients had follicular or poorly differentiated cancers. The small tumor volumes in this study (mean: 2.5 cc) often detected prior to the onset of clinical symptoms, may also improve the clinical outcome. Metastatic brain tumors with smaller volumes have better tumor control, in part because higher doses are feasible [9, 13].
Three patients underwent WBRT followed by GKR. In this retrospective study, it is impossible to determine whether WBRT provided additional benefits. In this experience, the only tumor that failed in local control had undergone both GKR and WBRT; this patient also developed new distant brain metastases despite WBRT. Currently, we advocate primary GKR for patients with ten or fewer metastases and add WBRT later if additional multiple metastases develop and they are unsuitable for repeat GKR. Because of the expectation for longer survival, we think it reasonable to defer WBRT in an attempt to reduce the chance for associated cognitive late deficits.
Four cases of hemorrhagic thyroid brain metastases have been reported [15, 23, 24]; all were from papillary cancers. None of the patients in this series had initial or delayed intratumoral hemorrhage.
Conclusion
GKR is valuable minimally invasive management strategy for patients with cerebral metastasis from thyroid cancer. Early detection using surveillance brain imaging facilitates treatment when the tumors are small. In such cases higher GKR doses enhance tumor control. We suspect that WBRT has a limited role in the management of brain metastases from thyroid cancer. Death is most likely caused by systemic disease progression as GKR achieves control of brain metastases in more than 90% of patients with thyroid cancer of brain.
Abbreviations
- GKR:
-
Gamma knife radiosurgery
- MRI:
-
Magnetic resonance imaging
- SPGR:
-
Spoiled-Gradient Recalled Acquisition in Steady State
- SRS:
-
Stereotactic radiosurgery
- WBRT:
-
Whole brain radiation therapy
References
Adler JR, Cox RS, Kaplan I, Martin DP (1992) Stereotactic radiosurgical treatment of brain metastases. J Neurosurg 76:444–449
Alexander E III, Moriarty TM, Davis RB et al (1995) Stereotactic radiosurgery for the definitive, noninvasive treatment of brain metastases. J Natl Cancer Inst 87:34–40. doi:10.1093/jnci/87.1.34
Buatti JM, Friedman WA, Bova FJ, Mendenhall WM (1995) Treatment selection factors for stereotactic radiosurgery of intracranial metastases. Int J Radiat Oncol Biol Phys 32:1161–1166. doi:10.1016/0360-3016(94)00461-S
Coffey RJ, Flickinger JC, Bissonette DJ, Lunsford LD (1991) Radiosurgery for solitary brain metastases using the cobalt-60 gamma unit: methods and results in 24 patients. Int J Radiat Oncol Biol Phys 20:1287–1295
Flickinger JC, Loeffler JS, Larson DA (1994) Stereotactic radiosurgery for intracranial malignancies. Oncology 8:81–86 Williston Park
Fuller BG, Kaplan ID, Adler J, Cox RS, Bagshaw MA (1992) Stereotaxic radiosurgery for brain metastases: the importance of adjuvant whole brain irradiation. Int J Radiat Oncol Biol Phys 23:413–418
Kihlstrom L, Karlsson B, Lindquist C, Noren G, Rahn T (1991) Gamma knife surgery for cerebral metastasis. Acta Neurochir Suppl (Wien) 52:87–89
Loeffler JS, Kooy HM, Wen PY et al (1990) The treatment of recurrent brain metastases with stereotactic radiosurgery. J Clin Oncol 8:576–582
Mehta MP, Rozental JM, Levin AB et al (1992) Defining the role of radiosurgery in the management of brain metastases. Int J Radiat Oncol Biol Phys 24:619–625
Sturm V, Kimmig B, Engenhardt R et al (1991) Radiosurgical treatment of cerebral metastases. Method, indications and results. Stereotact Funct Neurosurg 57:7–10. doi:10.1159/000099550
Williams J, Enger C, Wharam M, Tsai D, Brem H (1998) Stereotactic radiosurgery for brain metastases: comparison of lung carcinoma vs. non-lung tumors. J Neurooncol 37:79–85. doi:10.1023/A:1005958215384
Brown PD, Brown CA, Pollock BE, Gorman DA, Foote RL (2002) Stereotactic radiosurgery for patients with “radioresistant” brain metastases. Neurosurgery 51:656–665. doi:10.1097/00006123-200209000-00009
McDermott MW, Sneed PK (2005) Radiosurgery in metastatic brain cancer. Neurosurgery 57(Suppl):S45–S53. doi:10.1227/01.NEU.0000182741.82422.14
Smith ML, Lee JY (2007) Stereotactic radiosurgery in the management of brain metastasis. Neurosurg Focus 22:E5. doi:10.3171/foc.2007.22.3.6
McWilliams RR, Giannini C, Hay ID, Atkinson JL, Stafford SL, Buckner JC (2003) Management of brain metastases from thyroid carcinoma: a study of 16 pathologically confirmed cases over 25 years. Cancer 98:356–362. doi:10.1002/cncr.11488
Biswal BM, Bal CS, Sandhu MS, Padhy AK, Rath GK (1994) Management of intracranial metastases of differentiated carcinoma of thyroid. J Neurooncol 22:77–81. doi:10.1007/BF01058357
Chiu AC, Delpassand ES, Sherman SI (1997) Prognosis and treatment of brain metastases in thyroid carcinoma. J Clin Endocrinol Metab 82:3637–3642. doi:10.1210/jc.82.11.3637
Dinneen SF, Valimaki MJ, Bergstralh EJ, Goellner JR, Gorman CA, Hay ID (1995) Distant metastases in papillary thyroid carcinoma: 100 cases observed at one institution during 5 decades. J Clin Endocrinol Metab 80:2041–2045. doi:10.1210/jc.80.7.2041
Salvati M, Frati A, Rocchi G et al (2001) Single brain metastasis from thyroid cancer: report of twelve cases and review of the literature. J Neurooncol 51:33–40. doi:10.1023/A:1006468527935
Cha ST, Jarrahy R, Mathiesen RA, Suh R, Shahinian HK (2000) Cerebellopontine angle metastasis from papillary carcinoma of the thyroid: case report and literature review. Surg Neurol 54:320–326. doi:10.1016/S0090-3019(00)00306-2
Masiukiewicz US, Nakchbandi IA, Stewart AF, Inzucchi SE (1999) Papillary thyroid carcinoma metastatic to the pituitary gland. Thyroid 9:1023–1027
Ogawa Y, Sugawara T, Seki H, Sakuma T (2006) Thyroid follicular carcinoma metastasized to the lung, skull, and brain 12 years after initial treatment for thyroid gland-case report. Neurol Med Chir (Tokyo) 46:302–305. doi:10.2176/nmc.46.302
Isoda H, Takahashi M, Arai T et al (1997) Multiple haemorrhagic brain metastases from papillary thyroid cancer. Neuroradiology 39:198–202. doi:10.1007/s002340050393
Lin CK, Lieu AS, Howng SL (1999) Hemorrhagic cerebellar metastasis from papillary thyroid carcinoma. Kaohsiung J Med Sci 15:234–238
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, IY., Kondziolka, D., Niranjan, A. et al. Gamma knife radiosurgery for metastatic brain tumors from thyroid cancer. J Neurooncol 93, 355–359 (2009). https://doi.org/10.1007/s11060-008-9783-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-008-9783-2