Abstract
Purpose To evaluate outcome after fractionated stereotactic radiotherapy (FSRT) and concomitant daily temozolomide (TMZ) in patients with recurrent gliomas. Materials and Methods Twenty-five patients with recurrent or progressive gliomas were treated with FSRT in combination with TMZ at the Department of Radiation Oncology, University of Heidelberg. Histologic classification at primary diagnosis included low-grade astrocytoma in 7 patients (28%), grade III gliomas in 10 patients (40%) and glioblastoma in 8 patients (32%). All patients had undergone at least one neurosurgical resection, which was complete in 5 patients (20%), subtotal in 13 patients (52%) and a biopsy only in 7 patients (28%). Nineteen patients (76%) had undergone neurosurgical resection for tumor recurrence. All patients had received radiation therapy with a median dose of 60 Gy. The median time interval between primary RT and re-irradiation was 36 months. Using FSRT, we applied a median total dose of 36 Gy in a median fractionation of 5 × 2 Gy/week. Chemotherapy with TMZ was applied in a median dose of 50 mg/m2. Results Median overall survival was 59 months. Median survival from re-irradiation was 8 months. Actuarial survival rates at 6 and 12 months were 81% and 25%. Median PFS was 5 months; actuarial PFS rates at 6 and 12 months were 48% and 16%. Treatment could be completed in all patients as scheduled without interruptions >3 days. No severe treatment-related side effects could be observed. Conclusion Re-irradiation and TMZ is safe and effective in a subgroup of patients with recurrent gliomas. Further evaluation of radiochemotherapy regimens for recurrent or progressive gliomas is warranted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Salvage treatment options for patients with recurrent gliomas are often restricted. Due to the infiltrative nature of the disease, neurosurgical resection is frequently limited due to a high risk for surgery-related side effects (1, 2). A number of chemotherapeutic substances are prescribed for tumor recurrence, however, most show only modest benefit. A review analysis performed by Wong et al. determined a median progression-free survival time (PFS) of 10 weeks, with 21% of the patients progression-free at 6 months (PFS-6), these data were obtained from eight consecutive phase II trials including 225 patients with recurrent gliomas. The implementation of temozolomide (TMZ), an orally applicable alkylating substance, has improved outcome for patients with recurrent gliomas. PFS-6 after treatment of recurrent gliomas with TMZ alone was 46% (3). Only recently, alternative dosing schedules of TMZ leading to more prolonged exposure were shown to be safe and very effective. Wick et al. reported a PFS-6 of 43.8%, with a 1-year survival rate from progression of 23% (4).
In the past, a second course of radiation therapy (RT) was considered to be only of modest benefit while being associated with a high risk of treatment-related side effects using conventional RT techniques (5). However, the advent of stereotactic RT such as Stereotactic Radiosurgery (SRS) and Fractionated Stereotactic Radiotherapy (FSRT) have enabled the delivery of high local doses while sparing surrounding normal tissue. For recurrent gliomas, good efficacy and safety could be demonstrated for both techniques (6, 7).
For primary glioblastoma, standard-of-care after primary diagnosis currently is radiochemotherapy (RCHT) with TMZ (8, 9). In the past, only few studies have evaluated RCHT for tumor recurrence (10–13). Therefore, transfer of the concomitant TMZ-concept into the situation of tumor recurrence seems to be a promising strategy. Thus, in the present manuscript, we report outcome of re-irradiation as RCHT using FSRT with TMZ in 25 patients with recurrent gliomas.
Materials and methods
Twenty-five patients with recurrent or progressive gliomas were treated with FSRT at the Department of Radiation Oncology, University of Heidelberg.
Histologic classification at primary diagnosis included low-grade astrocytoma in 7 patients (28%) grade III gliomas in 10 patients (40%) and glioblastoma in 8 patients (32%). All patients had undergone at least one neurosurgical resection, which was complete in 5 patients (20%), subtotal in 13 patients (52%) and a biopsy only in 7 patients (28%). Nineteen patients (76%) had undergone a neurosurgical resection for tumor recurrence. Pathologic classification was glioblastoma in all 19 patients after neurosurgical re-resection, of which 5 patients had been diagnosed with glioblastoma at primary diagnosis, 4 with anaplastic oligodendroglioma, and 5 each with anaplastic astrocytoma and WHO Grade II astrocytoma. Detailed patients’ characteristics are provided in Table 1.
All patients had received radiation therapy at some time after primary diagnosis with a median dose of 60 Gy (range 54–63 Gy). The median time interval between primary RT and re-irradiation was 36 months (range 5–180 months). Six patients had received RCHT with TMZ after primary diagnosis for glioblastoma; in 2 patients, TMZ had been prescribed for tumor recurrence. One patient had received carmustine (BCNU) prior to re-irradiation. All patients demonstrated contrast-enhancing lesions on the T1-weighted MRIs as a correlation for tumor recurrence and/or secondary malignisation.
For treatment planning, an individual fixation head mask made of Scotch cast (3 M, St. Paul, MN, USA) was manufactured, enabling precise patient positioning for treatment planning as well as realignment for each fraction. The fixation system allowing 1–2 mm repositioning accuracy was implemented as published previously (14, 15). Three-dimensional treatment planning was based on contrast-enhanced CT- and MR-images performed in mask fixation with the stereotactic localization system attached to a stereotactic base frame. After stereotactic image fusion, the treatment volume was delineated on each 3 mm slice of the three-dimensional data cube. Treatment planning was performed using the three dimensional treatment planning system Voxelplan (dkfz Heidelberg, Germany) using the beam’s eye view technique for field optimization. We defined the area of contrast-enhancement on MRI as the gross tumor volume (GTV), and added a safety margin of 0.5–1 cm as the planning target volume (PTV). The median PTV size was 50 ml (range 16–149 ml).
The dose for re-irradiation was prescribed with respect to the previous treatment portals, previous RT dose, size and location of the lesion, with special respect to organs at risk such as optic nerves, chiasm and brain stem. For dose delivery, 3–4 irregular non-coplanar fields formed with a midsize multi-leaf collimator with a leaf thickness of 5 mm at isocenter were chosen; we applied a median total dose of 36 Gy (range 25–45 Gy) in a median fractionation of 5 × 2 Gy/week with a 6 MV linear accelerator (Primus, Siemens, Erlangen, Germany). The defined PTV was encompassed by the 90% isodose line.
Chemotherapy with TMZ was applied in a median dose of 50 mg/m2 on each day of irradiation. It was administered orally early in the morning at approximately the same time of each day. Prophylaxis against Pneumocystis carinii was not prescribed. For antiemesis, metoclopramide, alizaprid or ondansetron medication was given.
Seventeen patients were treated with adjuvant cycles of TMZ.
All patients were seen for a first follow-up visit 6 weeks after completion of FSRT, thereafter in three-months intervals or as needed clinically. All visits included a thorough clinical-neurological assessment as well as contrast-enhanced MR-imaging. Additional diagnostic procedures, including positron-emission tomography (PET), single photon emission computed tomography imaging as well as MRI spectroscopy were scheduled as required. The median follow-up time was 8 months (range 2–14 months).
For tumor progression, chemotherapy was applied in 4 patients with nimustine (n = 3) and PCV (procarbacine, carmustine, vincristine; n = 1).
Primary endpoint of this analysis was survival. Overall survival (OS) was calculated from primary diagnosis of the tumor, survival (S-RT) from re-irradiation was determined from the initiation of RT. Progression-free survival (PFS) was calculated from the initiation of RT for recurrence until tumor progression or death (by any cause), whichever happened first. OS, S-RT and PFS were determined using the Kaplan–Meier-method (16, 17). Influence of prognostic factors on outcome was evaluated using the univariate Cox proportional regression model. Statistical analyses were performed using the software Statistica (StatSoft, Hamburg, Germany).
Results
Overall survival (OS)
Median OS was 59 months (range 15–192 months). Age (P = 1.0), gender (P = 0.72) as well as extent of neurosurgical resection (P = 1.0), were not significantly associated with OS. Primary histology was no prognostic factor for OS (P = 0.95). In 19 patients, re-operation was performed, and in all of these patients the second histology was glioblastoma. Between these 19 patients and the 6 patients in which no second surgery was performed, overall survival was not statistically significant (P = 0.73).
Survival from RCHT (S-RT)
Median S-RT was 8 months (range 3–14 months). Actuarial survival rates at 6 and 12 months were 81% and 25% (Fig. 1). No significant influence S-RT of age (P = 1.0), gender (P = 1.0), extent of neurosurgical resection (P = 0.9) or histologic classification (P = 0.66) was observed. No difference in S-RT between TMZ-naïve patients and patients pre-exposed to TMZ was observed (P = 0.7). There was no statistically significant difference between patients treated with re-operation (n = 19) and patients treated with re-irradiation without a second course of surgery (n = 6; P = 0.72).
Progression-free survival (PFS)
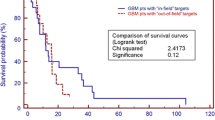
Median PFS was 5 months (range 2–14 months); actuarial PFS rates at 6 and 12 months were 48% and 16% (Fig. 2). No significant prognostic factors of PFS including histology (P = 0.6), age (P = 0.44), gender (P = 0.45) or extent of neurosurgical resection (P = 0.25) could be calculated. PFS was not different between TMZ-naïve patients and patients pre-exposed to TMZ was observed (P = 0.7). 82% of the recurrences occurred within the high-dose irradiation field or at the field borders, 18% were outfield recurrences. PFS was not different in the group of patients treated with a second course of surgery (n = 19; P = 0.19):
Figure 3 shows radiologic outcome after RCHT with TMZ as re-irradiation 14 months after treatment.
Radiographic outcome after FSRT and concomitant TMZ: MRI for treatment planning in stereotactic setup (a) and follow-up examination 14 months after re-irradiation (b) in a female patient diagnosed with WHO grade II astrocytoma at the age of 54. After stereotactic biopsy at primary diagnosis, postoperative RT was performed up to a total dose of 60 Gy. Thirteen years after RT, tumor recurrence developed as seen in A; the patient had developed progressive focal seizures. We treated her with FSRT to a dose of 36 Gy and concomitant TMZ, followed by adjuvant cycles of TMZ. Fourteen months after re-irradiation, the patient is clinically as well as radiologically recurrence-free (b)
Toxicity
Treatment could be completed in all patients as scheduled without interruptions >3 days. Minor side effects included alopecia, headaches and nausea/vomiting, which could be controlled effectively by antiemetic medication. Hematological side effects were only mild.
No severe treatment-related side effects could be observed.
Discussion
This study demonstrates that RCHT performed as re-irradiation with FSRT and concomitant application of TMZ is safe and seems so be effective in a subgroup of patients with recurrent gliomas. PFS-6 is 48% and superior to most data on the treatment of recurrent gliomas found in the literature. Treatment is well tolerated with low toxicity.
Achievement of local control is crucial to improve outcome in patients with recurrent gliomas, since the majority of recurrences occur locally, within the primary tumor region of in close proximity to the tumor site (18, 19). Therefore, effective local treatment is essential not only after primary diagnosis, but also for the treatment of recurrences. However, most patients have already undergone at least one neurosurgical resection, and have been exposed to high doses of RT before presenting with a recurrence. Therefore, treatment options are limited in most cases, mostly due to the fear of severe treatment related side effects.
Besides neurosurgical resection, which should be evaluated for each patient, chemotherapy is probably the most frequent salvage therapy employed for recurrent malignant gliomas, leading to median survival times of about 20 weeks (20); newer substances, such as the oral alkylating agent TMZ, have increased outcome in patients with recurrent gliomas, especially more recently with intensified dose regimens (3, 4, 21).
A second course of radiation therapy can be considered, at least in a subgroup of patients. Re-irradiation using conventional external beam techniques was associated with only modest palliative and survival benefits, and treatment toxicity outweighed outcome in most studies (5). Using modern precision RT techniques, such as FSRT or SRS, prolongation of survival with low toxicity rates can be achieved (6, 7). Previously, we could show that treatment outcome and toxicity of FSRT for recurrent gliomas is a safe and effective treatment alternative (6): Survival for patients with glioblastoma from re-irradiation was 8 months, and 12 and 22 months for anaplastic and low-grade gliomas, respectively.
On the basis of the work performed by the EORTC and other groups concurrent radiation and TMZ has become the standard of care for patients with newly diagnosed GBM (8, 9, 22). Therefore, it seemed promising to evaluate this regimen for patients with recurrent gliomas, since lesions were either recurrent malignant gliomas or considered as secondary malignisation in patients initially diagnosed with low-grade gliomas. Based on the excellent results obtained in our institution with a dose of 50 mg/m2 TMZ during RCHT for primary glioblastoma (9), this dosing was considered to be a safe dose in combination with re-irradiation. While this study reports the first results on RCHT using TMZ for recurrent gliomas, other groups have evaluated a number of substances in combination with RT for this patient population.
Arcicasa et al. treated 31 patients with external beam RT in combination with lomustine (CCNU) prescribing a median RT dose of 34.5 Gy; median survival after re-irradiation was 13.7 months, with moderate acute toxicity (10). Lomustine was applied orally at a dose of 130 mg/m2 at the beginning of RT, then every 6 weeks until tumor progression. Cisplatin was assessed by Glass et al. in combination with hypofractionated FSRT in 20 patients with recurrent gliomas. The RT dose applied ranged between 35 Gy and 42 Gy (12). One of the largest groups treated with RCHT for recurrent gliomas is published by Lederman et al.; 88 patients were treated with paclitaxel and hypofractionated FSRT with RT doses between 18 Gy and 36 Gy (13). Median survival after RT was 7 months. Topotecan in combination with hypofractionated FSRT was evaluated by Wurm et al.; the Berlin group reports median survival of 21.3 months for patients with anaplastic gliomas (n = 5), and 7.9 months for patients with glioblastoma (n = 20). Topotecan was applied as continuous infusion at a dose of 1.1 mg/m2/d, and toxicity was acceptable (11). The present data on re-irradiation as RCHT with temozolomide are comparable to the different reports in the literature, however, treatment results of the different studies show large differences with respect to OS and PFS. This is most probably due to the heterogeneous patient population at the time point recurrence and different inclusion criteria into the analyses.
Comparing the results from this analysis with outcome data on FSRT for tumor recurrence, outcome is largely comparable (6). Patients’ characteristics and treatment data including median dose and PTV resemble in both analyses. However, the small patient collective treated with RCHT represents a more heterogeneous group with respect to tumor histology and prior treatments. Thus, without randomized controlled trials, it is difficult to conclude if at all or which chemotherapy offers the most benefit in this situation.
One argument against TMZ for RCHT might be that nowadays most patients have been pre-exposed to chemotherapy with TMZ, either as RCHT after primary diagnosis, or as first-line chemotherapy for recurrence. Franceschi et al. have investigated the efficacy of TMZ in prior TMZ responders and have shown that repeat use of TMZ is effective: PFS-6 was 36%, and the objective response or stable disease rate was 43% (23). The notion, that patients presenting with stable disease for a longer time after primary TMZ may profit from another prolonged stabilization after a second course of TMZ, was shown by a German study on dose intensified TMZ (4). In the present study, no difference in outcome between TMZ-naïve patients and patients pre-exposed to TMZ was observed.
Based on the results from the present analysis, RCHT with TMZ for recurrent gliomas is a safe and effective treatment alternative. However, it must kept in mind that the results are based on a small patient collective with a number of different histologies at primary diagnosis. Therefore, further evaluation in a larger group of patients in a prospective trial is needed. Perhaps, application of novel dosing schedules, such as dose-intensified TMZ, or novel RT modalities such as carbon ion RT, might further improve outcome. Future randomized trials are warranted to further improve outcome in patients with recurrent gliomas. Novel pharmaceutical substances and innovative radiation techniques and qualities such as carbon ion RT might offer promising alternatives.
References
Dirks P, Bernstein M, Muller PJ, Tucker WS (1993) The value of reoperation for recurrent glioblastoma. Can J Surg 36:271–275
Harsh GR, Levin VA, Gutin PH, Seager M, Silver P, Wilson CB (1987) Reoperation for recurrent glioblastoma and anaplastic astrocytoma. Neurosurgery 21:615–621
Yung WK, Prados MD, Yaya-Tur R, Rosenfeld SS, Brada M, Friedman HS et al (1999) Multicenter phase II trial of temozolomide in patients with anaplastic astrocytoma or anaplastic oligoastrocytoma at first relapse. Temodal Brain Tumor Group. J Clin Oncol 17:2762–2771
Wick A, Felsberg J, Steinbach JP, Herrlinger U, Platten M, Blaschke B et al (2007) Efficacy and tolerability of temozolomide in an alternating weekly regimen in patients with recurrent glioma. J Clin Oncol 25:3357–3361
Bauman GS, Sneed PK, Wara WM, Stalpers LJ, Chang SM, McDermott MW et al (1996) Reirradiation of primary CNS tumors. Int J Radiat Oncol Biol Phys 36:433–441
Combs SE, Thilmann C, Edler L, Debus J, Schulz-Ertner D (2005) Efficacy of fractionated stereotactic reirradiation in recurrent gliomas: long-term results in 172 patients treated in a single institution. J Clin Oncol 23:8863–8869
Combs SE, Widmer V, Thilmann C, Hof H, Debus J, Schulz-Ertner D (2005) Stereotactic radiosurgery (SRS): treatment option for recurrent glioblastoma multiforme (GBM). Cancer 104:2168–2173
Stupp R, Mason WP, Van den Bent MJ, Weller M, Fisher B, Taphoorn MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Combs SE, Gutwein S, Schulz-Ertner D, van Kampen M, Thilmann C, Edler L et al (2005) Temozolomide combined with irradiation as postoperative treatment of primary glioblastoma multiforme. Phase I/II study. Strahlenther Onkol 181:372–377
Arcicasa M, Roncadin M, Bidoli E, Dedkov A, Gigante M, Trovo MG (1999) Reirradiation and lomustine in patients with relapsed high-grade gliomas. Int J Radiat Oncol Biol Phys 43:789–793
Wurm RE, Kuczer DA, Schlenger L, Matnjani G, Scheffler D, Cosgrove VP et al (2006) Hypofractionated stereotactic radiotherapy combined with topotecan in recurrent malignant glioma. Int J Radiat Oncol Biol Phys 66:S26–S32
Glass J, Silverman CL, Axelrod R, Corn BW, Andrews DW (1997) Fractionated stereotactic radiotherapy with cis-platinum radiosensitization in the treatment of recurrent, progressive, or persistent malignant astrocytoma. Am J Clin Oncol 20:226–229
Lederman G, Wronski M, Arbit E, Odaimi M, Wertheim S, Lombardi E et al (2000) Treatment of recurrent glioblastoma multiforme using fractionated stereotactic radiosurgery and concurrent paclitaxel. Am J Clin Oncol 23:155–159
Menke M, Hirschfeld F, Mack T, Pastyr O, Sturm V, Schlegel W (1994) Photogrammetric accuracy measurements of head holder systems used for fractionated radiotherapy. Int J Radiat Oncol Biol Phys 29:1147–1155
Schulz-Ertner D, Frank C, Herfarth KK, Rhein B, Wannenmacher M, Debus J (2002) Fractionated stereotactic radiotherapy for craniopharyngiomas. Int J Radiat Oncol Biol Phys 54:1114–1120
Clark TG, Bradburn MJ, Love SB, Altman DG (2003) Survival analysis part IV: further concepts and methods in survival analysis. Br J Cancer 89:781–786
Clark TG, Bradburn MJ, Love SB, Altman DG (2003) Survival analysis part I: basic concepts and first analyses. Br J Cancer 89:232–238
Park I, Tamai G, Lee MC, Chuang CF, Chang SM, Berger MS et al. (2007) Patterns of recurrence analysis in newly diagnosed glioblastoma multiforme after three-dimensional conformal radiation therapy with respect to pre-radiation therapy magnetic resonance spectroscopic findings. Int J Radiat Oncol Biol Phys
Sneed PK, Gutin PH, Larson DA, Malec MK, Phillips TL, Prados MD et al (1994) Patterns of recurrence of glioblastoma multiforme after external irradiation followed by implant boost. Int J Radiat Oncol Biol Phys 29:719–727
Brandes AA, Fiorentino MV (1996) The role of chemotherapy in recurrent malignant gliomas: an overview. Cancer Invest 14:551–559
Yung WK, Albright RE, Olson J, Fredericks R, Fink K, Prados MD et al (2000) A phase II study of temozolomide vs. procarbazine in patients with glioblastoma multiforme at first relapse. Br J Cancer 83:588–593
Mirimanoff RO, Gorlia T, Mason W, Van den Bent MJ, Kortmann RD, Fisher B et al (2006) Radiotherapy and temozolomide for newly diagnosed glioblastoma: recursive partitioning analysis of the EORTC 26981/22981-NCIC CE3 phase III randomized trial. J Clin Oncol 24:2563–2569
Franceschi E, Omuro AM, Lassman AB, Demopoulos A, Nolan C, Abrey LE (2005) Salvage temozolomide for prior temozolomide responders. Cancer 104:2473–2476
Conflict of interest
SEC, DSE and JD received research grants from Schering-Plough. SEC served on advisory boards and received speakers’ honoraria from Schering-Plough.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Combs, S.E., Bischof, M., Welzel, T. et al. Radiochemotherapy with temozolomide as re-irradiation using high precision fractionated stereotactic radiotherapy (FSRT) in patients with recurrent gliomas. J Neurooncol 89, 205–210 (2008). https://doi.org/10.1007/s11060-008-9607-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-008-9607-4