Abstract
Background As breast cancer patients live longer with control of systemic disease, survival after the diagnosis of brain metastases (BM) also appears to be improving. Methods The authors conducted a retrospective review of 112 breast cancer patients diagnosed with BM from 1997 to 2007 and correlated clinical and pathologic characteristics including hormone receptor (HR) and Her2/neu status with outcomes. Findings Median time to BM diagnosis (TTBM) was 38 months (range, 0–204 months). TTBM was shorter for patients with HR− versus HR+ disease (median 28.8 vs. 61.2 months, P < 0.001, Wilcoxon test). No difference in TTBM was observed for patients with HER2− versus HER2+ disease (median 37.4 vs. 34.9 months, P = 0.81). Median survival after the diagnosis of BM was 14.4 months. There was no significant difference in median survival after BM diagnosis for patients with HR+ versus HR− cancers (19.9 vs. 11.0 months, P = 0.18, log rank) or for patients with HER2+ versus HER2− disease (23.1 vs. 13.3 months, P = 0.11, log rank). Survival was significantly longer in patients with stable or responding systemic disease at BM diagnosis compared to patients with progressing systemic disease (31 vs. 6.3 months, P < 0.001). Multivariate analysis revealed that HR positivity, age <50, Karnofsky Performance Score (KPS) ≥80, and stable or responding systemic disease at BM diagnosis were associated with improved survival. Interpretation Subsets of patients with breast cancer BM are surviving longer. Control of systemic disease was most strongly associated with improved outcomes, and HER2/neu overexpression did not shorten survival after the diagnosis of BM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain metastases (BM) are a frequent complication in patients with metastatic breast cancer. A review of the natural history of breast cancer suggests that up to 16% of patients with metastatic disease develop clinically apparent central nervous system (CNS) disease [1], while autopsy series indicate that the incidence of BM in breast cancer patients may be as high as 30% [2]. More recently, the development of CNS metastases has been reported to be as high as 48% in patients receiving trastuzumab-based therapy [3]. Retrospective studies have reported that the median survival of patients with BM is less than 1 month if left untreated, 6–8 weeks if treated with steroids alone, and 3–6 months when treated with whole brain radiation therapy (WBRT) [4, 5]. Single institution studies have shown that patients with a single brain metastasis amenable to treatment with surgery followed by radiation therapy have a significantly better prognosis, with median survival in the range of 10–18 months, or much longer in some cases [6, 7].
As breast cancer patients with systemic disease live longer due to an increase in the number and efficacy of treatment options, there appears to be an increase in the diagnosis of BM in certain populations of patients [3, 8, 9]. Furthermore, the diagnosis of clinically asymptomatic BM is now commonplace with more frequent use of contrast enhanced magnetic resonance imaging (MRI) [10, 11]. With current treatment options, patients with BM appear to have improved survival, and often die from their systemic disease rather than from progression of disease in the CNS. We hypothesized that patient or disease specific characteristics or treatment related factors might correlate with survival, and might then be used to direct treatment or predict prognosis in the future. In this analysis, we describe the outcomes of patients with breast cancer brain metastases who have received treatment at the University of California San Francisco (UCSF) Comprehensive Cancer Center, and we explore clinical and biological characteristics and treatment factors that may impact survival.
Methods
Approval from the UCSF Committee on Human Research was obtained to perform this retrospective chart review. Patients who developed BM between 1997 and January 2007 and who were seen for at least one clinic visit at the UCSF Breast Care Center were identified by ICD-9 codes and through review of UCSF Radiation Oncology patient logs and medical oncology clinic schedules.
A total of 112 breast cancer patients with parenchymal BM were evaluated. Data were collected from clinic charts and from electronic records. Pathology information including primary tumor size, grade, and lymph node status was recorded from original surgical pathology reports when available. Hormone receptor (HR) status and Her2/neu status were obtained from reports on the primary tumor whenever available or from subsequent biopsies of metastatic sites. Tumors were considered Her2/neu+ if they were scored as 3+ by immunohistochemistry or had an amplification of >2.0 by fluorescence in situ hybridization. Clinical information was reviewed on all patients and included: (1) date of primary diagnosis; (2) age at diagnosis; (3) date of diagnosis of metastatic disease; (4) sites involved at diagnosis of metastatic disease; (5) date of diagnosis of BM; (6) Karnofsky performance status (KPS) at the time of diagnosis of BM; (7) reason for ordering imaging that led to brain metastasis diagnosis; (8) number of BM identified at initial diagnosis; (9) chemotherapy and hormonal therapies for primary tumor and for metastatic disease; (10) use of trastuzumab for metastatic disease; (11) treatment modalities for BM; and (12) and date of death. Status of systemic disease at the time of diagnosis of BM was recorded as responding, stable, or progressing based on review of CT scans, bone scans, and other diagnostic tests that were in most cases obtained within 14–28 days of diagnosis of BM. Primary cause of death was characterized as due to disease progression in the CNS, systemic progression outside the CNS, or both, and was assessed independently by two authors (M. Melisko and H. Rugo) based on review of scans, blood tests, clinic notes, and hospital discharge summaries obtained within several weeks of the patient’s death. For patients who received additional care at outside facilities, date of death and information supporting cause of death was collected from the patients’ primary treating oncologist.
Statistical analysis
Since all patients in the study had BM, the Wilcoxon rank test was used to test the effects of factors on time to BM. Univariate and multivariate analyses, using a Cox proportional hazards model, were performed to evaluate clinical and biological factors impacting survival following diagnosis of BM. The multivariate model was defined by including all factors that were significant at P < 0.10 in univariate Cox proportional hazard models and then eliminating them, one-at-a-time in a stepwise fashion. The elimination was based on the P-value for each factor and the one with the largest P-value was eliminated at each step. This continued until only those factors that were mutually significant at P < 0.05 remained in the model.
Median survival times were calculated based on Kaplan–Meier method for patients according to HR and HER2/neu status, number of BM at diagnosis, presence or absence of concurrent leptomeningeal disease (LMD), age at BM diagnosis, KPS at BM diagnosis, Recursive Partitioning Analysis (RPA) Class and status of systemic disease at BM diagnosis. Number of BM was divided into the following categories: (1) one (solitary); (2) two or three; (3) four to ten; (4) eleven to twenty; and (5) greater than twenty (including “military” or “too numerous to count”). Treatment for BM was divided into categories: (1) WBRT only; (2) WBRT followed by stereotactic radiosurgery (SRS) salvage; (3) initial treatment with SRS with or without WBRT salvage; (4) surgical resection with or without SRS and/or WBRT at any time; (5) No treatment (steroids/palliation only). Median survivals were compared using log rank statistics. All calculations were performed in STATA version 9.2.
Results
A total of 112 breast cancer patients with parenchymal BM diagnosed between 1997 and 2007 were identified; 20 of these patients had concurrent LMD. Characteristics of the patients and primary tumors are presented in Table 1. At last follow-up, 28 patients were still alive with median follow-up time of 18 months (range, 1.7–93 months) since the first diagnosis of brain metastasis. One patient presented with BM as the initial presentation of breast cancer, and 24 patients presented with BM as one of their first sites of metastatic disease. All patients were diagnosed with BM after imaging that was ordered to evaluate a neurological symptom. No patients were diagnosed with BM as a result of screening in asymptomatic patients or for clinical trial eligibility. Her2/neu or HR status was unknown in 12 and 7% of patients respectively, either because their primary breast cancer surgery occurred in the distant past or in another country, and therefore no primary tumor tissue was available for testing, or because there was no metastatic site amenable to biopsy. Table 2 shows the distribution of the number of BM at initial diagnosis, where scans or reports were available for review in 106 of 112 patients.
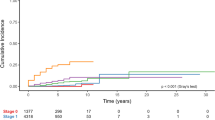
The median time from initial diagnosis of breast cancer to the development of BM was 38 months (range, 0–204 months). Time to development of BM (TTBM) from primary diagnosis was shorter for patients with HR− vs. HR+ disease (median 28.8 vs. 61.2 months, P < 0.001, Wilcoxon test, see Fig. 1), but there was no difference in TTBM for patients with HER2− vs. HER2+ disease (median 37.4 vs. 34.9 months, P = 0.81).
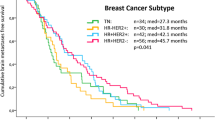
The median survival for the entire group after the diagnosis of BM was 14.4 months. Cause of death is listed in Table 3. There was no significant difference in median survival after the diagnosis of BM for patients with HER2+ (n = 53) compared to those with HER2− disease (n = 46), (23.1 vs. 13.3 months, P = 0.11, log rank test), although the survival curves in Fig. 2 demonstrate a trend towards longer survival in patients with HER2+ disease. Median survival for patients with HR+ disease (n = 56) was 19.9 months compared to 11.0 months for patients with HR− disease (n = 48), (P = 0.18) as seen in Fig. 3. Median survival for patients with both HR− and HER2− disease was extremely poor compared to the rest of the group (6.3 vs. 22.2 months, P = 0.002). Presence of concurrent LMD did not impact survival after diagnosis of BM, with median survival of 14.4 months in patients with LMD (n = 20) compared to 14.2 months without LMD (n = 92), (P = 0.50). The number of BM at initial diagnosis was not associated with survival in univariate analysis and therefore was not included in the multivariate analysis. Median survival was calculated by RPA class, with RPA Class I patients surviving a median of 55.6 months, RPA Class II 17.9 months, and RPA Class III only 1.1 month. Since only 3 patients were RPA Class I and 6 patients were RPA Class III, it appears that RPA classification does not separate this patient population into useful subsets.
Fifty percent of the patients had stable or responding systemic disease at the time of developing BM, and survival was significantly longer in these patients compared to patients with progression of systemic disease at the time of BM diagnosis (median 31 vs. 6.3 months, P < 0.001, Fig. 4). Patients younger than 50 survived longer than patients older than 50 at BM diagnosis (median 17.5 vs. 13.0 months, P = 0.015). A multivariate analysis (Table 4) that included 98 patients with all data available revealed that HR positivity, age <50, KPS ≥80, and stable or responding systemic disease at time of BM diagnosis were associated with improved survival.
Eleven patients underwent one or more surgical resections of BM along with other therapies including WBRT and/or SRS. The median survival of this group is 37.7 months, and four of these patients remained alive at 6, 22, 33, and 46 months after their diagnosis of BM. Of the eleven patients, one patient had surgery only, two patients had SRS first and then surgery as salvage, two patients underwent surgical resection then WBRT only, and six patients underwent surgical resection, WBRT and then SRS as salvage. Fifty six patients received WBRT alone and their median survival was 7.7 months. Seventeen patients underwent WBRT first, then had SRS as salvage, and their median survival was 22.2 months. Eighteen patients received SRS one or more times as their only treatment for BM and seven patients underwent SRS as initial therapy followed by WBRT as salvage. The median survival for these two groups combined was 18.1 months. There was no statistical difference in survival between the patients that received WBRT and then SRS as salvage compared to the patients that received SRS alone or as initial treatment and then WBRT salvage. Three patients received steroids or palliative support only, and their median survival was 0.8 months.
Patients received a median of 3 (range 0–11) chemotherapy regimens for metastatic disease. Patients with estrogen and/or progesterone receptor positive tumors received a median of 2 hormonal therapies (range 1–4). Seven patients underwent autologous bone marrow or stem cell transplant as treatment of systemic disease prior to diagnosis of BM, and 28 patients participated in a clinical trial of one or more novel chemotherapies, immunotherapies, or biologic agents during the course of their treatment. All patients whose cancers were known to overexpress HER2/neu received trastuzumab after 1998 when it became commercially available, and were continued on trastuzumab after the diagnosis of BM if they did not have contraindication such as a drop in their cardiac function.
Discussion
Our report describes the characteristics and outcomes for a group of breast cancer patients with BM followed at a single institution over the past 10 years. In a multivariate analysis of this dataset, patients with HR+ disease, patients who were age <50, with stable or responding systemic disease, or with a KPS ≥80 when diagnosed with BM had significantly longer survival. These criteria could be used to identify patients who are expected to have a better prognosis, and therefore may benefit from aggressive initial and/or salvage treatment of BM.
HER2 overexpressing breast cancers were over-represented in this group of patients with BM. Several studies have observed that HER2+ breast cancer is associated with a higher incidence of subsequent BM. Gabos et al. analyzed a cohort of newly diagnosed breast cancer patients. With a median follow-up of 3.9 years, BM were identified in 9% (27 patients) with HER2− overexpressing breast cancer compared with only 1.9% (7 patients) in the HER2− patients (hazard ratio 4.23 [1.84–9.74], P = 0.0007). In the Gabos cohort, hormone-receptor negativity was also an independent prognostic factor for the development of BM [12]. In our series, 54% (56/104) of patients in this series with tissue available for review had HR− tumors, corroborating the finding that this tumor biology may be associated with a higher risk of developing BM in the metastatic setting [13, 14].
The overall median survival for the entire group was 14.4 months, which is longer than described in larger series of patients identified through a multicenter database [15], but similar to survival estimates published for breast cancer patients at a single institution who developed BM while being treated with trastuzumab [8]. In our series, median survival after the diagnosis of BM was longer in patients with HER2 overexpressing tumors but this did not reach statistical significance, possibly due to the sample size. Our results support previous data indicating that overall survival is not compromised in patients with HER2+ disease who develop BM [16], and our outcomes are similar to those of Kirsch et al. [17] who reported a median survival of 22.4 months after diagnosis of BM in patients with HER2 overexpressing tumors compared to 9.4 months in patients with HER2− disease.
In the current series, median survival was 7.7 months in patients who received WBRT only. Survival was similar between patients who received WBRT as initial treatment and then were candidates for SRS as salvage (22.2 months), and patients who received SRS either as their only treatment or as primary therapy then had salvage WBRT (18.1 months). These results are consistent with previous retrospective studies in which survival after WBRT is in the range of 6 months and after SRS is 13–17 months [18, 19]. There is likely a selection bias as well as biological differences between patients who present with bulky or extensive CNS disease requiring WBRT and those patients who present with a small number of low volume BM and are candidates for SRS as their initial treatment. However, in our series, the number of BM at diagnosis was not correlated with survival in univariate analysis. It appears that patients who are initially treated with and respond to WBRT obtain benefit if they are followed carefully for the development of new lesions in the brain and then treated with SRS as salvage. The results from this series also suggest that initial treatment with SRS may be reasonable in selected patients since many of these patients will still have the option to receive salvage WBRT or further SRS as needed, and a small number may be spared WBRT altogether without compromising survival. All of these impressions should be considered with great caution given the likely influence of selection bias on our retrospective results. Prospective randomized trials are needed to determine the benefits of and indications for upfront and salvage SRS or WBRT in breast cancer patients.
Over 50% of patients developed BM at a time when their systemic disease was stable or responding, adding support to the widely held idea that most conventional chemotherapies and trastuzumab do not protect from or treat disease in the CNS. The majority of patients received ongoing systemic therapy with multiple sequential regimens, even after the diagnosis of BM. Despite aggressive treatments including experimental therapies in some cases, almost half of the patients died from progression of their systemic disease rather than from their BM.
The majority of patients who died of uncontrolled BM without evidence of leptomeningeal involvement had a large disease burden in the brain at diagnosis and often presented with more profound neurologic symptoms such as motor weakness, visual changes, or seizures. Most of these patients were not candidates for surgery or SRS and were treated with WBRT alone. Since the prognosis after WBRT alone remains quite dismal, a number of radiosensitizing agents including RSR13 (efaproxiral) and motexafin gadolinium have been investigated in combination with WBRT [20, 21]. A 368 patient, randomized, open-label Phase 3 study was conducted to evaluate the safety and efficacy of WBRT with supplemental oxygen with or without efaproxiral in breast cancer patients with BM. This study failed to achieve its primary endpoint of demonstrating an improvement in overall survival in patients receiving efaproxiral plus WBRT, compared to patients receiving WBRT alone [22]. The outcome of this study is disappointing, and further reinforces that additional therapies need to be developed for patients who are candidates only for WBRT. Patients who fail to respond initially or experience progression in brain have limited retreatment options other than additional SRS. More recently, data has been presented suggesting that lapatinib, an oral tyrosine kinase inhibitor targeting the epidermal growth factor (EGF) and HER2/neu pathways, has some activity in patients with HER2 overexpressing BM that have recurred or progressed after radiation [23].
Our single institution experience suggests that breast cancer patients with BM are surviving longer than has been described historically. Improvements in survival after the diagnosis of BM may be explained by a number of factors. Earlier detection of smaller, more treatable lesions through more frequent use of MRI, as well as advances in technology of MRI scanning, may be part of the explanation. In addition, prolonged survival after BM may be related to improved control of systemic disease due to increasing treatment options including newer chemotherapies, trastuzumab, and other experimental therapies. Based on the small number of patients who participated in clinical trials of CNS directed therapies such as lapatinib, temozolomide, or efaproxiral, it is not yet possible to estimate the impact that these treatment options may have had on survival.
Given the high percentage of patients who underwent SRS, either as initial treatment or as salvage therapy after WBRT or surgery, it is possible that more frequent and routine utilization of this modality provided benefit and extended survival in a number of patients. At the UCSF Comprehensive Cancer Center, SRS is offered to patients with a limited number of lesions (median number of lesions was 3, with a range of 1–13 in this series) and for lesions up to approximately 3 cm in diameter. Sixteen patients in this series underwent multiple SRS treatments (up to 4 sessions) to treat new or recurring lesions, suggesting that retreatment with this modality is an option for many patients. The long term safety and complications associated with repeat sessions of SRS is not yet known.
Feasibility of treatment with SRS depends on the diagnosis of BM that are few in number and small in size. Therefore, it is possible that a screening program to detect BM earlier in high risk patients may be beneficial. This series, and previous reports [9, 13, 15], suggest that patients with HER2+ and/or HR− disease are more likely to develop BM. Identification of clinical characteristics and/or novel biological markers in primary breast tumors that predict the development of BM, as well as the characteristics of these metastases, would greatly assist in selection of patients who would benefit most from a screening program, or from treatment with new chemotherapeutic or biologic agents that are known to cross the blood brain barrier. In the future, this information could also be used to recommend preventive strategies.
References
DiStefano A, Yong Yap Y, Hortobagyi GN, Blumenschein GR (1979) The natural history of breast cancer patients with brain metastases. Cancer 44:1913–1918
Tsukada Y, Fouad A, Pickren JW, Lane WW (1983) Central nervous system metastasis from breast carcinoma. Autopsy study. Cancer 52:2349–2354
Lai R, Dang CT, Malkin MG, Abrey LE (2004) The risk of central nervous system metastases after trastuzumab therapy in patients with breast carcinoma. Cancer 101:810–816
Boogerd W, Vos VW, Hart AA, Baris G (1993) Brain metastases in breast cancer; natural history, prognostic factors and outcome. J Neurooncol 15:165–174
Sneed PK, Larson DA, Wara WM (1996) Radiotherapy for cerebral metastases. Neurosurg Clin N Am 7:505–515
Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS, Young B (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322:494–500
Pieper DR, Hess KR, Sawaya RE (1997) Role of surgery in the treatment of brain metastases in patients with breast cancer. Ann Surg Oncol 4:481–490
Bendell JC, Domchek SM, Burstein HJ, Harris L, Younger J, Kuter I, Bunnell C, Rue M, Gelman R, Winer E (2003) Central nervous system metastases in women who receive trastuzumab-based therapy for metastatic breast carcinoma. Cancer 97:2972–2977
Evans AJ, James JJ, Cornford EJ, Chan SY, Burrell HC, Pinder SE, Gutteridge E, Robertson JF, Hornbuckle J, Cheung KL (2004) Brain metastases from breast cancer: identification of a high-risk group. Clin Oncol (R Coll Radiol) 16:345–349
Miller KD, Weathers T, Haney LG, Timmerman R, Dickler M, Shen J, Sledge GW Jr (2003) Occult central nervous system involvement in patients with metastatic breast cancer: prevalence, predictive factors and impact on overall survival. Ann Oncol 14:1072–1077
Schellinger PD, Meinck HM, Thron A (1999) Diagnostic accuracy of MRI compared to CCT in patients with brain metastases. J Neurooncol 44:275–281
Gabos Z, Sinha R, Hanson J, Chauhan N, Hugh J, Mackey JR, Abdulkarim B (2006) Prognostic significance of human epidermal growth factor receptor positivity for the development of brain metastasis after newly diagnosed breast cancer. J Clin Oncol 24:5658–5663
Slimane K, Andre F, Delaloge S, Dunant A, Perez A, Grenier J, Massard C, Spielmann M (2004) Risk factors for brain relapse in patients with metastatic breast cancer. Ann Oncol 15:1640–1644
Stewart JF, King RJ, Sexton SA, Millis RR, Rubens RD, Hayward JL (1981) Oestrogen receptors, sites of metastatic disease and survival in recurrent breast cancer. Eur J Cancer 17:449–453
Tham YL, Sexton K, Kramer R, Hilsenbeck S, Elledge R (2006) Primary breast cancer phenotypes associated with propensity for central nervous system metastases. Cancer 107:696–704
Lower EE, Drosick DR, Blau R, Brennan L, Danneman W, Hawley DK (2003) Increased rate of brain metastasis with trastuzumab therapy not associated with impaired survival. Clin Breast Cancer 4:114–119
Kirsch DG, Ledezma CJ, Mathews CS, Bhan AK, Ancukiewicz M, Hochberg FH, Loeffler JS (2005) Survival after brain metastases from breast cancer in the trastuzumab era. J Clin Oncol 23: 2114–2116; author reply 2116–2117
Firlik KS, Kondziolka D, Flickinger JC, Lunsford LD (2000) Stereotactic radiosurgery for brain metastases from breast cancer. Ann Surg Oncol 7:333–338
Petrovich Z, Yu C, Giannotta SL, O’Day S, Apuzzo ML (2002) Survival and pattern of failure in brain metastasis treated with stereotactic gamma knife radiosurgery. J Neurosurg 97:499–506
Shaw E, Scott C, Suh J, Kadish S, Stea B, Hackman J, Pearlman A, Murray K, Gaspar L, Mehta M, Curran W, Gerber M (2003) RSR13 plus cranial radiation therapy in patients with brain metastases: comparison with the Radiation Therapy Oncology Group Recursive Partitioning Analysis Brain Metastases Database. J Clin Oncol 21:2364–2371
Mehta MP, Rodrigus P, Terhaard CH, Rao A, Suh J, Roa W, Souhami L, Bezjak A, Leibenhaut M, Komaki R, Schultz C, Timmerman R, Curran W, Smith J, Phan SC, Miller RA, Renschler MF (2003) Survival and neurologic outcomes in a randomized trial of motexafin gadolinium and whole-brain radiation therapy in brain metastases. J Clin Oncol 21:2529–2536
Allos Therapeutics Reports Results for Phase 3 Enrich Study of Efaproxyn in Women With Brain Metastases Originating From Breast Cancer. Press Release (http://www.allos.com): Allos Therapeutics, Inc, 2007
Lin NU, Winer EP (2007) Brain metastases: the HER2 paradigm. Clin Cancer Res 13:1648–1655
Acknowledgment
This research was funded in part by a Career Development Award from the Bay Area Breast Cancer Translational Research Program P50 CA58207.
Author information
Authors and Affiliations
Corresponding author
Additional information
Contributors: M. Melisko and H. Rugo conceived the study idea. All co-authors participated in the design of the study. M. Melisko, P. Sneed, and J. De Franco collected and compiled the clinical and pathological data on the cancer patients. D. Moore organized and directed the statistical analyses. M. Melisko wrote the first draft of the paper and all co-authors participated in the subsequent revisions of the paper.
Rights and permissions
About this article
Cite this article
Melisko, M.E., Moore, D.H., Sneed, P.K. et al. Brain metastases in breast cancer: clinical and pathologic characteristics associated with improvements in survival. J Neurooncol 88, 359–365 (2008). https://doi.org/10.1007/s11060-008-9578-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-008-9578-5