Abstract
Several single nucleotide polymorphisms (SNPs) affecting DNA repair capacity and modifying cancer susceptibility have been described. We evaluated the association of SNPs Arg194Trp, Arg280His, and Arg399Gln in the X-ray cross-complementing group 1 (XRCC1) and Thr241Met in the X-ray cross-complementing group 3 (XRCC3) DNA repair genes with the risk of brain tumors. The Caucasian study population consisted of 701 glioma (including 320 glioblastoma) cases, 524 meningioma cases, and 1,560 controls in a prospective population-based case–control study conducted in Denmark, Finland, Sweden, and the UK. The studied SNPs were not significantly associated with the risk of brain tumors. The highest odds ratios (ORs) for the associations were observed between the homozygous variant genotype XRCC1 Gln399Gln and the risk of glioma (OR = 1.32; 95% confidence interval, CI, 0.97–1.81), glioblastoma (OR = 1.48; 95% CI, 0.98–2.24), and meningioma (OR = 1.34; 95% CI, 0.96–1.86). However, in pair-wise comparisons a few SNP combinations were associated with the risk of brain tumors: Among others, carriers of both homozygous variant genotypes, i.e., XRCC1 Gln399Gln and XRCC3 Met241Met, were associated with a three-fold increased risk of glioma (OR = 3.18; 95% CI, 1.26–8.04) and meningioma (OR = 2.99; 95% CI, 1.16–7.72). In conclusion, no significant association with brain tumors was found for any of the polymorphisms, when examined one by one. Our results indicated possible associations between combinations of XRCC1 and XRCC3 SNPs and the risk of brain tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is a disease of multifactorial etiology, caused by the interaction of several inherited and environmental factors. Despite decades of research, the etiology of human brain tumors is poorly understood. In addition to hereditary syndromes, the only established risk factor for glioma and meningioma is radiotherapy to the head [1, 2]. However, as both the inherited disorders and irradiation are rare exposures, they account for only a minority of brain neoplasms. In recent years, it has been shown that variability in DNA repair capacity plays a role as a modifier of cancer risk. Increased risks of various cancer types have been associated with single nucleotide polymorphisms (SNPs) within the DNA repair genes (reviewed in 3, 4). We analyzed SNPs in the X-ray cross-complementing group 1 (XRCC1) and group 3 (XRCC3) genes, which belong to the DNA repair gene family.
The XRCC1 gene (located at chromosome 19q13.2) produces an enzyme involved in the base excision repair (BER) pathway, amending small lesions such as single-strand breaks (SSBs), non-bulky adducts, oxidative damage, alkylation, and methylation. Recently, the XRCC1 complex has also been described as part of an alternative route of DNA double-strand break (DSB) nonhomologous end-rejoining, i.e., PARP1–dependent end-joining of DSBs [5]. The XRCC1 protein is essential for mammalian viability and XRCC1-deficient cells are genetically unstable and sensitive to DNA damaging agents. Three common SNPs (variant allele frequency > 0.05) lead to amino acid substitutions in XRCC1 at codons 194 (exon 6, C → T, Arg → Trp), 280 (exon 9, G → A, Arg → His), and 399 (exon 10, G → A, Arg → Gln) [6].
The XRCC3 gene (located at chromosome 14q32.3) codes for an enzyme functioning in the homologous recombination (HR) repair of DNA cross-links [7] and DSBs [8]. The role of XRCC3 in HR is not entirely clear, but the XRCC3 gene is a member of the RAD51 family. It interacts with RAD51 and is required for its focus formation and catalyzing of DNA strand exchange in HR repair [9]. XRCC3 deficient cell lines display reduced HR [10] and they are hypersensitive to ionizing radiation, UV radiation, genotoxic alkylating agents, and cross-linking agents [11]. The main SNP in the XRCC3 gene leads to an amino acid substitution at codon 241 (exon 8, C → T, Thr → Met) [6].
Despite the fact that XRCC1 and XRCC3 SNPs have been widely examined and related to several types of cancer, their role in brain carcinogenesis has not been established. Only three studies have so far investigated the association of brain tumors with XRCC1 and XRCC3 SNPs: two in glioma [12, 13] and one in meningioma [14]. Therefore, we evaluated the possible association of XRCC1 and XRCC3 SNPs and the risk of developing glioma, glioblastoma, or meningioma in a large, prospective case–control study of brain tumors. In the present analysis, we included all four common non-synonymous SNPs in the coding regions of these two genes.
Materials and methods
Study subjects and data collection
Study subjects with primary brain tumors were recruited in closely coordinated population-based case–control studies in Denmark, Finland, Sweden, and the UK. Samples and clinico-pathological information from patients were obtained with informed consent and ethical review board approval in accordance with the tenets of the Declaration of Helsinki. The brain tumor cases were identified from oncology, neuropathology, neurosurgery, and neurology centers as well as from cancer registries. The studies covered the whole of Denmark; all regions of Finland except Northern Lapland and Åland; the Stockholm, Lund, Gothenburg, and Umeå regions of Sweden; and the Thames regions of Southeast England. All the study centers followed the core protocol of the INTERPHONE Study (coordinated by the International Agency for Research on Cancer) [15] with some extensions to the study design, such as a wider age range, an extended questionnaire, and the collection of blood samples.
The eligible cases were patients diagnosed with primary glioma (International Classification of Diseases (ICD), 10th Revision, code C71; and International Classification of Diseases for Oncology (ICD-O), 3rd Edition, codes 9380–9384, 9390–9394, 9400, 9401, 9410, 9411, 9420–9424, 9430, 9440–9443, 9450, 9451, and 9505) or meningioma (ICD, 10th Revision, code C70; ICD-O, 3rd Edition, codes 9530–9539). The most common form of glioma, glioblastoma (ICD-O, 3rd Edition, codes 9440–9442), was also analyzed separately. In addition to the primary brain cancer diagnosis, the eligible cases had to be resident in the study region at the time of diagnosis and aged between 20 and 69 years at diagnosis in the Nordic countries and from 18 to 59 years in the UK. Case ascertainment was based on histological (in 94% of glioma and 89% of meningioma cases) or radiological verification of diagnosis during the study period from September 2000 to February 2004 (the exact dates within this period varied by country).
The controls were randomly selected from population registers in the Nordic countries and from general practitioner’s practice lists in the UK. They were frequency-matched to the cases by 5-year age group, sex, and geographical area and had never been diagnosed with a brain tumor (in Denmark any cancer).
The eligible study subjects consisted of 2,160 glioma cases, 1,339 meningioma cases, and 6,062 controls. All cases and controls were first contacted by letter as soon as possible after identification and invited to participate in the study. When needed, a reminder was sent or contact was made by telephone.
Of the invited study subjects, 1,243 (58%) glioma cases, 1,004 (75%) meningioma cases, and 2,951 (51%) controls gave their informed consent for participation and they were interviewed. Information on medical history (e.g., diseases, including tumors, and radiotherapy), occupational exposures, smoking habits, and family history of cancer as well as ethnicity and country of birth, was obtained from in-person interviews conducted by trained nurses or medical students. At the end of the interview, the study subjects were asked to give their consent for blood sampling and genotyping and to donate a blood sample. In Finland, the number of patients and controls to be sampled was determined prior to the study, and blood was drawn from patients in three hospitals and from controls living in the area served by these hospitals. During the data collection period, all eligible Finnish participants were asked to donate a blood sample.
Blood sample collection and DNA extraction were performed according to standard procedures in each of the participating countries, with the exception that blood samples from Denmark were sent to Sweden for DNA extraction.
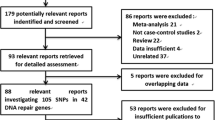
Of the interviewed study subjects, DNA was derived from 728 glioma (including 325 glioblastoma) and 549 meningioma cases, as well as from 1,610 controls. These DNA samples were shared among the participating centers, thus facilitating the examination of specific SNPs from all study samples in the same laboratory. In order to obtain a homogeneous study population, non-Caucasians (21 glioma cases, 21 meningioma cases, and 40 controls) were excluded from the study. The mean ages of the genotyped glioma, glioblastoma, and meningioma cases were 48.2, 53.0, and 53.1 years respectively and the mean age for the controls was 51.8 years. The age and sex distributions of the interviewed and successfully genotyped Caucasian study subjects were similar as seen in Table 1.
SNP selection and genotyping
In the present study, the investigations were conducted on SNPs that have been associated with cancer predisposition in the Genetic Association Database (2004) (Center for Information Technology. http://geneticassociationdb.nih.gov) in the DNA damage repair genes XRCC1 and XRCC3. We included SNPs showing functional repair deficiency in the XRCC1 (Arg399Gln; dbSNP ID# rs25487) and in the XRCC3 (Thr241Met; rs861539) as well as a SNP (XRCC1 Arg194Trp; rs1799782) having limited alterations in repair activities [16]. A third variant (Arg280His; rs25489) within XRCC1 was examined in order to study intragenic associations.
The chosen SNPs were examined in a 96-well format using a polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) based method previously described [17]. Each 96-well plate contained negative (no template) controls as well as positive controls for all genotypes (wild-type/wild-type, wild-type/variant, and variant/variant; see Table 2). Genotypes of positive controls were verified by sequencing. For quality control on each studied SNP, 30% of the samples were randomly chosen for repeated analyses, which were verified to be identical to the original results. Furthermore, all genotypes were individually interpreted by two geneticists from coded DNA samples.
Statistical analysis
Each SNP was tested for deviation from the Hardy-Weinberg equilibrium (HWE) among controls by comparing the observed and expected genotype frequencies using the χ2 test.
The associations between the SNPs and the risk of brain tumors were studied using conditional logistical regression, with frequency matched strata defined by age category (10-year age group), sex, and geographical region. Glioma (including glioblastoma), glioblastoma, and meningioma were analyzed separately. Odds ratios (ORs) and 95% confidence intervals (95% CIs) were estimated for each studied SNP and all combinations of the genotypes. Due to the relatively low frequencies of the XRCC1 variant alleles 194Trp and 280His (0.057 and 0.049, respectively), these genotypes were also modeled as a dichotomous variable (carriers versus non-carriers, i.e., wild-type/wild-type vs. wild-type/variant + variant/variant). The statistical tests were performed two-sided and P values < 0.05 were considered statistically significant. These statistical analyses were performed using Stata Statistical Software (STATA release 9.0; Stata Corporation, College Station, TX).
The possible associations between the XRCC1 haplotypes and risk of glioma, glioblastoma, and meningioma were tested using a score test developed by Schaid et al [18]. This was performed using the “haplo.stats” package version 1.2.1 (Mayo Clinic. http://mayoresearch.mayo.edu/mayo/research/schaid_lab/software.cfm) implemented for the R programming language.
Results
The successfully genotyped Caucasian study subjects comprised 701 glioma (including 320 glioblastoma) cases, 524 meningioma cases, and 1,560 controls. The genotype distribution and variant allele frequencies of the XRCC1 Arg194Trp, Arg280His, and Arg399Gln SNPs and the XRCC3 Thr241Met SNP did not differ significantly between the cases and controls (Table 2).
The genotype frequencies of the XRCC1 Arg194Trp, Arg280His, and Arg399Gln SNPs were consistent with the Hardy-Weinberg equilibrium (HWE) at the 0.05 level among the controls. However, HWE could not be demonstrated for the XRCC3 Thr241Met SNP among the controls (χ2 = 7.42; P = 0.006). When the study population was divided into national cohorts, the HWE disequilibrium was observed among the Danish controls and therefore the Danish data were excluded from the XRCC3 Thr241Met analyses. The estimated ORs were consistent between the countries in all the single and pair-wise comparisons of SNPs. Therefore, the combined material from Denmark, Finland, Sweden, and the UK was used in the data analyses.
Studied single SNPs in the XRCC1 and XRCC3 genes were not significantly associated with the risk of brain tumors. The homozygous variant genotype XRCC1 Gln399Gln showed an association close to statistical significance with the risk of all brain tumor types, i.e., glioma (OR = 1.32; 95% CI, 0.97–1.81), glioblastoma (OR = 1.48; 95% CI, 0.98–2.24), and meningioma (OR = 1.34; 95% CI, 0.96–1.86) (Table 3). The heterozygous variant genotype XRCC3 Thr241Met was associated with a decreased risk of glioblastoma (OR = 0.71; 95% CI, 0.52–0.98). However, a tendency of increased risk was seen for the homozygous carriers of the 241Met allele. There were no significant differences in the risk of brain tumors between the carriers and non-carriers of the rare variant alleles 194Trp and 280His in XRCC1.
The effect of different SNP combinations on the risk of brain tumors was also evaluated. Odds ratios of brain tumors for pair-wise combinations of variant and wild-type alleles in the SNPs XRRC1 Arg399Gln and XRCC3 Thr241Met are presented in Table 4. No significant associations were observed in the remaining pair-wise comparisons and are thus not reported. The combination of the homozygous variant genotypes XRCC1 Gln399Gln and XRCC3 Met241Met was associated with a three-fold increased risk of glioma and meningioma (OR = 3.18; 95% CI, 1.26–8.04 and OR = 2.99; 95% CI, 1.16–7.72, respectively). Subjects with the homozygous variant genotype XRCC1 Gln399Gln combined with the homozygous wild-type genotype XRCC3 Thr241Thr had a two-fold increased risk of glioblastoma (OR = 2.22; 95% CI, 1.08–4.57) and meningioma (OR = 1.90; 95% CI, 1.02–3.57).
To elucidate further the relevance of the variant alleles in XRCC1, haplotypes for the three SNPs (Arg194Trp, Arg280His, and Arg399Gln) were constructed using the HAPLO.STAT package. Altogether six XRCC1 haplotypes were detected in glioma, but two haplotypes (i.e., 194Arg/280His/399Gln and 194Trp/280Arg/399Gln) were very infrequent among the study subjects. Only five haplotypes were detected in glioblastoma and meningioma as the haplotype 194Arg/280His/399Gln was missing. The rare variant alleles in XRCC1, i.e., 194Trp and 280His, did not share a haplotype. The results showed that the haplotype effects reflected the effect of the XRCC1 399Gln allele. None of the six haplotypes yielded a significant association with the risk of glioma, glioblastoma, or meningioma (results not presented).
Information on the exposure of the subjects to radiotherapy and the existence of brain tumor cases among first-degree relatives was also obtained through interview. However, in the present study, 0.6% of brain tumor cases and 0.0% of controls had a history of previous radiotherapy. Moreover, among the study subjects 0.6% of cases and 0.3% of controls reported having a relative with a glioma and none reported meningiomas among their relatives. Therefore, we could not meaningfully analyze the interrelationship of these exogenous factors with the XRCC1 and XRCC3 SNPs.
Discussion
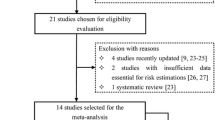
We investigated the associations of brain tumors with SNPs in one major gene (XRCC1) involved in base excision repair (BER) of single-strand breaks (SSBs) and another (XRCC3) functioning in homologous recombination repair (HR) of double-strand breaks (DSBs). No significant association with brain tumors was found for any of the SNPs (Arg194Trp, Arg280His, and Arg399Gln in the XRCC1 and Thr241Met in the XRCC3), when examined one by one. These SNPs have been extensively studied in several other cancer sites, but the results are inconsistent (reviewed in 3, 4). To date, only three published studies have examined the association between XRCC1 and XRCC3 SNPs and the risk of brain tumors. All these three studies are consistent with our results. Wang et al. [12] studied 309 glioma cases and 342 controls representing non-Hispanic Caucasians from the USA. The XRCC1 Arg399Gln and XRCC3 Thr241Met SNPs were not significantly associated with the risk of glioma. Felini et al. [13] established the XRCC1 Arg399Gln genotypes of 366 white glioma cases and 427 controls from the USA. They found no evidence of an association between the XRCC1 Arg399Gln genotypes and glioma. Sadetzki et al. [14] studied 219 meningioma cases and 216 controls from Israel of mixed ethnicity (mainly of African and Asian origin). The XRCC3 Thr241Met SNP was not associated with the risk of meningioma either in homozygous or heterozygous carriers.
However, indications of possible associations between combinations of the studied SNPs and increased risk of glioma, glioblastoma, or meningioma emerged from our results. The carriers of the combination of the homozygous variant genotype XRCC1 Gln399Gln and the homozygous wild-type genotype XRCC3 Thr241Thr showed an increased risk of glioblastoma and meningioma. The carriers of the two homozygous variant genotypes (XRCC1 Gln399Gln and XRCC3 Met241Met) appeared to have a substantially increased risk of glioma and meningioma. These results are in line with earlier studies where the variant allele 241Met in XRCC3 has been associated primarily with cancers unrelated to smoking, particularly in combination with other variants such as the 399Gln variant in XRCC1 or the NAT-2 slow acetylator genotype [19, 20].
Although genetic susceptibility analyses have the potential to provide novel information regarding the development of cancer, reproducibility of the results, i.e., frequent failure to replicate previous findings, has emerged as a major issue [21, 22]. False positive findings are always possible especially when multiple groups are tested. For glioma and glioblastoma, the proportion of statistically significant findings was 5% or less and for meningioma between 5% and 10% in the present study.
Few risk factors have been established for brain tumors and confounding by known factors is unlikely to affect our results because few subjects had earlier radiotherapy or a family history of brain tumors and their exclusion did not affect the findings. Population admixture is a known potential confounding factor in a population-based association analysis [23] and therefore we included only Caucasians in the statistical analysis. We were able to conduct a population-based study with frequency matching for age, sex, and geographical region. Comprehensive population rosters were available as sources of controls, thus ensuring representative identification. Misclassification of the disease status was minimized by histological confirmation of diagnosis and misclassification of exposure by quality control of genotyping and a low failure rate.
In the present study, we used prospective case ascertainment with rapid enrolment of cases (in glioma cases, the median lag between the diagnosis and interview was two months in Denmark, less than one month in Finland, three months in Sweden, and four months in the UK). A short lag between the diagnosis, ascertainment, and blood sample collection is especially important with malignant brain tumors with the rapid loss of cases due to poor outcome. A particular concern in studies of genetic factors is possible bias due to genes affecting prognosis, which may cause an imbalance if participants represent patients with favorable prognoses. Wrensch et al. [24] have demonstrated that glioma and glioblastoma survival was poorer with the XRCC1 Arg280His SNP, whereas it was not associated with the XRCC1 Arg399Gln SNP. However, the distribution of the XRCC1 Arg280His and Arg399Gln genotypes were not different between the cases and controls in the present study and thus it is not likely that the results were affected by differences in prognosis.
In addition, selection bias could have played a role since about 60–70% of the interviewed cases in Denmark, Sweden, and UK were genotyped in the present study. In addition, only a predetermined number of interviewed cases were genotyped in Finland. However, there were no obvious differences in the characteristics of those donating a blood sample from those who only responded to the study questionnaire. Selection bias could also have interfered with the Hardy-Weinberg equilibrium in the XRCC3 Thr241Met SNP among the control subjects. Therefore, the Danish study subjects causing this disequilibrium were excluded from our statistical analysis in order to remove this source of bias. However, an alternative analysis that included also the Danish group gave similar results.
In conclusion, a lack of overall effect, i.e., no association between any of the single polymorphisms or haplotypes and the risk of glioma, glioblastoma, or meningioma was observed in this study. However, this is the first study to demonstrate possible associations between combinations of XRCC1 and XRCC3 SNPs and the risk of brain tumors. Our results indicate that reduced DNA repair capacity may play a role in brain carcinogenesis when the function of both the XRCC1 and XRCC3 genes, which are involved in different DNA repair pathways, is reduced. Although the present study includes the largest series of glioma, glioblastoma, and meningioma cases with well-characterized diagnoses and homogenic ethnic composition described thus far, the results should be considered preliminary and validated in other similar studies.
References
Ron E, Modan B, Boice JD Jr et al (1988) Tumors of the brain and nervous system after radiotherapy in childhood. N Engl J Med 319:1033–1039
Sadetzki S, Chetrit A, Freedman L et al (2005) Long-term follow-up for brain tumour development after childhood exposure to ionising radiation for tinea capitis. Radiat Res 163:424–432
Goode EL, Ulrich CM, Potter JD (2002) Polymorphisms in DNA repair genes and associations with cancer risk. Cancer Epidemiol Biomarkers Prev 11:1513–1530
Hung RJ, Hall J, Brennan P et al (2005) Genetic polymorphisms in the base excision repair pathways and cancer risk: a HuGE review. Am J Epidemiology 162:925–942
Audebert M, Salles B, Calsou P (2004) Involvement of poly(ADP-ribose)polymerase-1 and XRCC1/DNA ligase III in an alternative route for DNA double-strand breaks rejoining. J Biol Chem 279:55117–55126
Shen MR, Jones IM, Mohrenweiser H (1998) Nonconservative amino acid substitution variants exist at polymorphic frequency in DNA repair genes in healthy humans. Cancer Res 58:604–608
Thompson LH, Schild D (2002) Recombinational DNA repair and human disease. Mutat Res 509:49–78
Khanna KK, Jackson SP (2001) DNA double-strand breaks: signaling, repair, and the cancer connection. Nat Genet 27:247–254
Bishop DK, Ear U, Bhattacharyya A et al (1998) XRCC3 is required for assembly of Rad51 complexes in vivo. J Biol Chem 273:21482–21488
Pierce AJ, Johnson RD, Thompson LH et al (1999) XRCC3 promotes homology-directed repair of DNA damage in mammalian cells. Genes Dev 23:2633–2638
Caldecott K, Jeggo P (1991) Cross-sensitivity of gamma-ray-sensitive hamster mutants to cross-linking agents. Mutat Res 255:111–121
Wang L-E, Bondy ML, Shen H et al (2004) Polymorphisms of DNA repair genes and risk of glioma. Cancer Res 64:5560–5563
Felini MJ, Olshan AF, Schroeder JC et al (2007) DNA repair polymorphisms XRCC1 and MGMT and risk of adult gliomas. Neuroepidemiology 29:55–58
Sadetzki S, Flint-Richter P, Starinsky S et al (2005) Genotyping of patients with sporadic and radiation-associated meningiomas. Cancer Epidemiol Biomarkers Prev 14:969–976
Cardis E, Richardson L, Deltour I et al (2007) The INTERPHONE study: design, epidemiological methods, and description of the study population. Eur J Epidemiol 22:647–664
Au WW, Navasumrit P, Ruchirawat M (2004) Use of biomarkers to characterize functions of polymorphic DNA repair genotypes. Int J Hyg Environ Health 207:301–313
Kiuru A, Lindholm C, Heilimo I et al (2005) Influence of DNA repair gene polymorphisms on the yield of chromosomal aberrations. Environ Mol Mutagen 46:198–205
Schaid DJ, Rowland CM, Tines DE et al (2002) Score tests for association between traits and haplotypes when linkage phase is ambiguous. Am J Hum Genet 70:425–434
Matullo G, Guarrera S, Carturan S et al (2001) DNA repair gene polymorphisms, bulky DNA adducts in white blood cells and bladder cancer in a case–control study. Int J Cancer 92:562–567
Smith TR, Miller MS, Lohman K et al (2003) Polymorphisms of XRCC1 and XRCC3 genes and susceptibility to breast cancer. Cancer Lett 190:183–190
Wacholder S, Chanock S, Garcia-Closas M et al (2004) Assessing the probability that a positive report is false: an approach for molecular epidemiology studies. J Natl Cancer Inst 96:434–442
Hattersley AT, McCarthy MI (2005) What makes a good genetic association study? Lancet 366:1315–1323
Wacholder S, Rothman N, Caporaso N (2000) Population stratification in epidemiologic studies of common variants and cancer: quantification of bias. J Natl Cancer Inst 92:1151–1158
Wrensch M, Wiencke JK, Wiemels J et al (2006) Serum IgE, tumor epidermal growth factor receptor expression, and inherited polymorphisms associated with glioma survival. Cancer Res 66:4531–4541
Lahkola A, Auvinen A, Raitanen J et al (2007) Mobile phone use and risk of glioma in 5 North European countries. Int J Cancer 120:1769–1775
Acknowledgements
The authors warmly thank all patients, controls, interviewers, and team collaborators in the study in all the participating countries, as listed in Lahkola et al. [25] for their invaluable contribution to this work. This research was supported by a grant from the Nordic Cancer Union. The INTERPHONE Study was supported by the European Commission Fifth Framework Program “Quality of Life and Management of Living Resources” (contract number QLK4-CT-1999–01563), and the International Union against Cancer (UICC; RCA/01/08). The UICC received funds for this study from the Mobile Manufacturers’ Forum and the Global System for Mobile Communications Association. Provision of funds to the INTERPHONE Study investigators via the UICC was governed by agreements that guaranteed INTERPHONE’s complete scientific independence. These agreements are publicly available at INTERPHONE site (2005) (International Agency for Research on Cancer. http://www.iarc.fr/ENG/Units/RCAd.html). Additional support was given by the Academy of Finland (grant number 71037), the Cancer Foundation of Northern Sweden, the Cancer Society of Finland, the Danish Cancer Society, the Emil Aaltonen Foundation, the Mobile Telecommunications and Health Research (MTHR) Program, the Swedish Cancer Society, and the Swedish Research Council. The views expressed in this paper are not necessarily those of the funders.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kiuru, A., Lindholm, C., Heinävaara, S. et al. XRCC1 and XRCC3 variants and risk of glioma and meningioma. J Neurooncol 88, 135–142 (2008). https://doi.org/10.1007/s11060-008-9556-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-008-9556-y