Abstract
Purpose
The optimal therapy of oligodendrogliomas remains uncertain. Although chemosensitive, these tumors are not chemocurable. We investigated whether chemotherapy delays the need for radiation therapy (RT) without decreasing length and quality of survival.
Methods and materials
Among 89 patients treated for oligodendrogliomas at the Centre Léon Bérard of Lyon from 1982 to 1999, 59 patients fitted inclusion criteria, having had centrally reviewed pure oligodendroglioma requiring treatment. According to the WHO’s classification 35 patients had Grade III and 24, Grade II oligodendrogliomas.
Results
According to the intent to treat, patients were retrospectively classified in three groups as exclusive RT (Group 1), radio-chemotherapy (Group 2), or exclusive chemotherapy (Group 3). Median progression-free survival (PFS): was 47 months [95% confidence interval (CI) 39–56], and median overall survival (OS) was 109 months (95% CI 83–134). In univariate analysis, PFS was correlated with frontal location and WHO classification; OS was correlated with frontal location and Post-operative Karnosky performans status both appearing as independent prognostic factors for OS in multivariate analysis. There was no significant difference between the treatment groups with regard to PFS (P = 0.82) and OS (P = 0.64). In the group of patients treated with exclusive chemotherapy the 5-year PFS and OS rates were 44 and 71%, respectively.
Conclusion
Front-line exclusive chemotherapy results in prolonged OS in patients with confirmed pure oligodendroglioma. Whether this strategy improves quality of life remains debatable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The optimal therapy of gliomas is unclear [1]. Five randomized concordant studies demonstrate that radiotherapy of high-grade gliomas increases survival [2–6]. Two concordant meta-analyses show a 10% survival advantage at 1 and 2 years for patients receiving nitrosoureas compared to those who do not [7, 8]. However, in these studies, high-grade oligodendrogliomas were not segregated from high-grade astrocytomas. No clear guideline exists for the treatment of high-grade oligodendrogliomas.
For low-grade gliomas, the situation is even less clear. The European Organization for Research and Treatment of Cancer (EORTC) randomized trial [9] showed no overall difference in 5-year survival comparing therapy comprising post-operative irradiation of 54 Gy with irradiation at recurrence. Median survival was 7.4 years in the radiotherapy group and 7.2 years in the control group [HR 0.97, 95% confidence interval (CI) 0.71–1.34; P = 0.872]. However, median progression-free survival (PFS) was 5.3 years in the group receiving early radiotherapy versus 3.4 years in the control group (HR 0.59 and 95% CI 0.45–0.77; P < 0.0001). Randomized prospective trials conducted by the EORTC [10] and Radiation Therapy Oncology Group (RTOG) [11] demonstrated lower-dose radiotherapy (45 and 50.4 Gy) to be as effective as higher doses (59.4 and 64.8 Gy). Again, oligodendrogliomas were not segregated from other gliomas. Neither optimal timing nor optimal dose of radiation is clearly defined in treatment of low-grade gliomas. Nor is there a randomized study evaluating the role of chemotherapy in these low-grade glial tumors.
Oligodendrogliomas demonstrate better prognoses than other gliomas. With equivalent treatment, patients with oligodendrogliomas survive longer than those with astrocytomas. In a review of the RTOG 83-02, Donahue et al. reported a median survival of 7.3 years in patients with anaplastic oligodendrogliomas or anaplastic mixed tumors versus 3.4 years for those with pure anaplastic astrocytomas P = 0.019 [12].
Cairncross et al. showed that LOH foci on 1p and 19q were predictors of good response to chemotherapy in anaplastic oligodendrogliomas [13]. In adults, combined 1p and 19q deletion has been observed in 83% of pure oligodendrogliomas, 63% of anaplasic oligodendroglioma, 56% of mixed low-grade glioma and 52% of anaplastic mixed oligoastrocytoma. Those patients also had longer overall survival (OS) (172 months vs. 105 months without deletions) [14].
Oligodendrogliomas are considered chemosensitive tumors irrespective of grade [15–25], but the optimal timing and final contribution of chemotherapy to OS remains unknown. Addition of chemotherapy to radiotherapy in first-line treatment of oligodendrogliomas increased disease-free survival (DFS) but had no impact on OS [26, 27]. No study in the current literature evaluates the impact of front-line radiotherapy in the subgroup of oligodendrogliomas that respond to chemotherapy. So, is it possible to treat a subgroup of patients exclusively with chemotherapy?
Prospective trials with baseline cognitive testing have shown small but measurable incidence of cognitive deficits after focal moderate dose radiotherapy, and therefore efforts to delay the possibility of this late toxicity are reasonable [28–30]. Thus, to determine if radiotherapy could be post-poned without adversely affecting survival, the authors’ retrospectively analyzed three types of first-line strategies used in one oncology center in 59 centrally reviewed pure oligodendrogliomas requiring treatment. The first group underwent radiotherapy alone; the second, radiotherapy followed by chemotherapy; and the third, exclusive chemotherapy.
Methods and materials
Patients
We retrospectively reviewed the records of all patients with oligodendrogliomas who received adjuvant treatment at Centre Léon Bérard from 1982 to 1999. Only patients followed with modern imaging techniques [computed tomography (CT) and/or magnetic resonance (MR) imaging]. Most patients were operated in one of the neuro-surgical units and most initial pathology was examined in the Department of Neuropathology of Hôpital Wertheimer (Lyon, France), and central review for all patients was performed by an experienced neuropathologist (AJ). The Neuro-oncology Committee of the Centre Léon Bérard designed post-operative treatment. Active treatment was undertaken in two situations. High-grade oligodendrogliomas (Grade III according to WHO’s classification) were treated directly after pathological diagnosis, but in Grade II tumors, active treatment was undertaken in case of clinical progression (deficit and/or resistant epilepsy) and/or radiological progression (increase in volume and/or apparition on contrast enhancement). In the latter group, there was usually no new histological proof of grading. Radiotherapy was delivered in the Radiotherapy and Neuro-oncology Unit of Centre Léon Bérard. Regular follow-up was performed either by the neuro-oncology team of Centre Léon Bérard or by a member of the ONCORA network. The response evaluation to chemotherapy is based on MacDonald’s criteria [31].
Radiation therapy
Involved field radiotherapy was administered at 60 Gy in 2.0 Gy, 5 days a week using a technique with multiple fields. All patients had CT planning and provisional dosimetry. Planning target volume (PTV) varied according to date of treatment. From 1982 to 1994, the gross target volume (GTV) was defined by CT; after 1994, by MR imaging. Patients were discharged home after 1-week hospital stay or as soon as feasible thereafter. Concomitant prevention of edema was delivered as required using steroids and/or mannitol.
Chemotherapy
Patients were scheduled to receive six cycles of PCV chemotherapy that included CCNU (110 mg/m²) or BCNU (150 mg/m²) on day 1; procarbazine (60 mg/m²) on days 8–21; and vincristine (1.4 mg/m², maximum dose: 2 mg) on days 8 and 28. The cycles were scheduled at 6-week intervals. Concomitant edema prevention using both steroids and/or mannitol was delivered as required.
The grouping of patients depended on the initial intention to treat. In the group treated with either exclusive radiation therapy (RT) or combined radio-chemotherapy (RT-CT), failure was defined as recurrence of tumor during or after therapy. In the group receiving exclusive CT the intent to treat was to discontinue treatment only in those patients who showed complete disappearance of contrast enhancement after 4–6 courses of chemotherapy. The strategy was considered to have failed if contrast enhancement persisted after chemotherapy, and these patients received immediate radiotherapy.
Review of histology
The pathology was reviewed centrally by an experienced neuro-pathologist using different classifications. Hematoxylin and eosin-stained slides of paraffin-embedded tumor tissue were examined for the presence of oligodendroglial and astrocytic components. Mixed oligoastrocytomas were excluded. Mixed oligoastrocytomas are defined as tumors witch contained both neoplastic oligodendroglial and astrocytic elements, with neoplastic astrocytic elements comprising at least 25% of the mixed glioma. Tumors were also graded as either low-grade or malignant, based on the presence or absence of elevated mitotic activity, significant nuclear pleomorphism, vascular neogenesis, and necrosis. In the identification of high-grade tumors, great emphasis was placed upon the presence or absence of vascular neogenesis. Vascular neogenesis was identified in all tumors designated malignant, with the exception of two small tumor samples containing few blood vessels, but displaying marked nuclear pleomorphism and significantly elevated mitotic activity. Ancillary diagnostic techniques, including immunohistochemistry, were selectively employed.
Statistical analysis
The end point of interest was survival time, with two criteria, PFS and OS. PFS was defined as the time from the date of start of treatment to the date of disease progression or death or to the date of last follow-up for patients alive with no indication of disease progression. OS was defined as the time from the date of start of treatment to the date of death or to the date of last follow-up for patients alive at last contact. Follow-up was completed in April 2006; median follow-up was 81 months. Survival curves were estimated using the Kaplan–Meier method [32] and compared with the log-rank test.
Univariate analysis
To evaluate the relation between survival and baseline characteristics, variables were included in univariate Cox proportional hazard regression models [33]. Age was included in the models as a dichotomous variable with the value zero for patients under 45 years (median value of the series) or one otherwise.
Multivariate analysis
Independent prognostic variables of PFS and OS were, respectively, identified by Cox regression analysis using a backward stepwise procedure to eliminate non-influential variables. We used a stepwise modeling algorithm with a significance level of 0.10 for entering and of 0.05 for removing explanatory variable.
Results
Eighty-nine patients fit inclusion criteria. Review of pathology excluded 30 patients. Of these 30, no slides were available for 20 patients; the diagnosis was changed for five patients (one case each, chordoid glioma, ependymoma, cavernoma, meningioma, and astrocytoma); and the diagnosis after histology review was mixed tumor for five patients. Thus, the diagnosis of pure oligodendroglioma was confirmed in 59 cases, and analysis was restricted to these 59 patients Characteristic of those 59 patients are described in Table 1 (Table 1).
Patients were 29 men and 30 women. Median age at diagnosis was 45 years (21–72 years). Thirty-three patients presented with only seizure at diagnosis, nine with headache, five with headache and seizure, and 12 with focal deficit. The predominant localization was frontal (25 patients), followed by occipital (14), temporal (10), parietal (6), thalamic (3), and brainstem (1). Sixteen underwent total gross removal (surgeon’s description) of the tumor, whereas 43 underwent biopsy or incomplete resection.
According to the WHO classification [34] determined at the time of histological review, 35 patients had Grade III and 24 Grade II oligodendrogliomas. Among the 24 Grade II oligodendrogliomas, nine patients with inoperable tumors were treated because of symptoms and five patients with inoperable tumors were treated because of contrast enhancement. Seven were treated at the time of unresectable recurrence with no new biopsy. Two patients were treated after surgery because of contrast enhancement on preoperative MRI. One patient was treated with chemotherapy for a tumor classified Grade II according to WHO classification. He was treated after multidisciplinary discussion because of an elevated mitotic activity in a small part of the tumor. After central review this tumor remains classified Grade II.
Twenty-one were treated after 12 or more months of observation after diagnosis of oligodendroglioma.
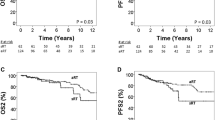
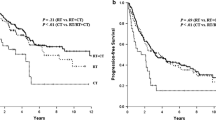
According to current knowledge and to neuro-oncology multidisciplinary decisions, the intent to deliver adjuvant therapy varied with time. Group 1 included 11 patients treated between 1982 and 1996 with exclusive radiotherapy. Group 2 included 16 patients treated between 1988 and 1999 with chemotherapy followed by radiotherapy. Group 3 included 32 patients treated between 1994 and 1999 with exclusive chemotherapy. The median PFS and OS for the series were 47 and 109 months, respectively (Fig. 1). In univariate analysis, PFS was correlated with frontal location and WHO classification and OS was correlated frontal location and Post-operative Karnosky performans status (KPS) (Table 2). After multivariate analysis, these factors appear as independent prognostic factors for PFS and OS (Table 3).
The 5-year PFS was 32% in Group 1 (RT); 41% in Group 2 (RT-CT), and 44% in Group 3 (CT). The difference is not significant (P = 0.67; Fig. 2). In addition, there was no significant difference between the three groups with regard to OS. Five-year OS was 51% for Group 1, 68% for Group 2, and 71% for Group 3 (P = 0.86; Fig. 3).
Kaplan–Meier curves for progression-free survival according among patients in the three treatment groups. The tick marks represent censored data on patients who were alive without progression of disease. Large dotted line represents group 1 (exclusive radiotherapy), small dotted line group 2 (chemotherapy followed by radiotherapy), and solid line group 3 (exclusive chemotherapy). P = 0.67 for the comparison among the groups
Kaplan–Meier curves for overall survival according among patients in the three treatment groups. The tick marks represent censored data on patients who were alive at last follow-up. Large dotted line represents group 1 (exclusive radiotherapy), small dotted line group 2 (chemotherapy followed by radiotherapy), and solid line group 3 (exclusive chemotherapy). P = 0.86 for the comparison among the groups
Patient characteristics (gender, age, frontal localization, complete surgery, and time from diagnosis to treatment) were well balanced between the three groups (Table 1). However, the histological type and Karnofsky index were more favorable in group 3 (CT). The rate of Grade III tumors according to WHO classification was only 41% in group 3 (CT) compared to 81% in the groups 1 and 2 (receiving radiation).
In Group 1 (RT), all 11 patients completed radiotherapy and experienced no tumor progression while on radiotherapy. Two remain non-progressive (9 and 3 years after treatment). Tumor recurred in nine patients, eight of whom required a second-line treatment because of tumoral evolution and the ninth receiving no second-line treatment because of low Karnofsky performance status at the time of recurrence. Second-line treatment was PCV in five patients, fotemustine (Muphoran®) in two patients, eight drugs in 1 day in one patient. Two patients were alive 24 and 108 months after recurrence, and six patients died 2, 3, 10, 42, 46, and 57 months after recurrence.
In Group 2 (CT + RT) all 16 patients completed intended treatment. Six remain non-progressive, four had no second-line treatment because of low-performance status, and six had second-line treatment, consisting of further surgery plus chemotherapy in two patients, chemotherapy in four patients. Chemotherapy comprised (Temodal®), in two patients, Muphoran (fotemustine), in four patients. One of whom is alive 2 months after recurrence and the others died 8, 13, 36, 48, and 50 months after recurrences.
In Group 3 (CT), three of 32 patients had progression during or immediately after first-line treatment and received RT as salvage treatment. Nine patients did not relapse. Four patients had no treatment at the time of tumor recurrence because of poor performance status. Nineteen patients required a second-line treatment for tumor evolution. Four patients received exclusive chemotherapy (comprised Temodal), two of whom were alive 24, and 36 months after recurrence and the others died 24 and 30 months after recurrence. Of 15 patients receiving radiotherapy for recurrence eight patients were alive, respectively, 24, 36, 42, 48 (three patients), 60, and 66 months after recurrence, and seven patients died 4, 6, 13 (two patients), 24, 28, and 36 months after radiation. In the group 3 (CT), 19 patients were treated for low-grade oligodendrogliomas according to WHO classification, and 13 were treated for High-grade oligodendrogliomas. In the group 3 (CT) the 5 years OS for low-grade is 66% (CI 95% 52–80); and 62% for high grade (CI 95% 47–75). The 5 years PFS for low grade is 32% (CI 95% 21–43); and 38% for high grade (CI 95% 25–51). Those differences are not statistically significant. Sixteen patients of group 3 were treated with exclusive chemotherapy after 12 or more months of observation after diagnosis of oligodendroglioma. Five-year PFS is 42% (CI 95% 29–55) compared to 35% (CI 95% 21–49) for patients receiving chemotherapy <1 year before diagnosis. Five-year OS is 66% (CI 95% 52–80) compared to 63% (CI 95% 48–78) for patients receiving chemotherapy <1 year before diagnosis.
Discussion
Any study reporting on a cohort of oligodendrogliomas has its own biases. Our study was designed to deal with a population as homogeneous as possible. Central review for all patients was performed by an experienced neuro-pathologist. Patients younger than 18 years were excluded because of differences in survival between patients according to age [35–40]. Inclusion criteria were the need for treatment in patients with confirmed oligodendrogliomas and included only pure oligodendrogliomas confirmed after review. According to WHO classification this study includes Grade III, and clinical aggressive Grade II. Clinical aggression was defined as increasing symptoms or tumor size or occurrence of contrast enhancement. Such inclusion criteria are similar to that used by Abrey et al. [41].
The prognostic factors in this series were consistent with those reported in the literature. In the present series Karnofsky index was prognostic factor for survival. Higher survival was associated with frontal location and grade of tumor according to WHO classification as reported in other series [42, 43] and absence of neuro-logical symptoms [44–49].
Demonstration of the unique chemosensitivity of oligodendrogliomas has opened the way to considerable research and hope. Cairncross and MacDonald and their colleagues were the first to report on a high-response rate of 75% to PCV chemotherapy for patients with enhancing recurrent oligodendroglioma [50, 51]. Genetic alterations were shown to correlate significantly with chemosensitivity and OS of oligodendroglioma in several uncontrolled or retrospective studies, but also in two recent phase III prospective trials [52–56]. The PCV chemotherapy regimen has been the standard treatment in case of recurrence after radiotherapy. Taliansky-Aronov et al. reported a series of 20 patients treated with Temozolomide for newly diagnosed anaplastic oligodendrogliomas. Clinical improvement was observed in 60% of the patients and objective radiological response in 75% of the patients [57]. Several phase II trials investigated the role of Temozolomide (Temodal) in patients with recurrent anaplastic oligodendroglioma after prior RT. In the study EORTC 26971 High-response rates of 53% (26% complete responses) were observed with first-line chemotherapy [58]. In contrast Temozolomide has demonstrated response rates of 25–43% in second-line studies after prior radiotherapy and PCV [59, 60]. Most patients who responded to second-line treatment had also responded to first-line PCV chemotherapy, but some patients who do not respond to PCV may still respond to TMZ [61]. Triebel reported a 50% PFS after PCV in Temozolomide resistant oligodendrogliomas [62]. Franceschi et al. evaluate Temozolomide for prior Temozolomide responders. Objective response or stable disease was achieved in 43% patients [63]. A second line of chemotherapy may also be discussed for patients relapsing after first line. In case of low grade Oligodendroglioma response have been published [64, 22].
In the present series, patients receiving exclusive chemotherapy as first-line treatment, the 5-year PFS and OS rates were 44 and 71%, respectively. When analysis is limited to the 13 patients treated for Grade III oligodendroglioma (according to the WHO’s classification), the 5 years OS and DFS are, respectively, 62 and 38%.
To our knowledge, there is no publication assessing the role of exclusive chemotherapy in high-grade oligodendrogliomas naïve of radiotherapy. Abrey et al. reported a series of 69 newly diagnosed oligodendroglioma treated with first-line chemotherapy including PVC and thiotepa high dose in case of response to PVC. Thirty-nine above 69 patients received thiotepa high dose; their 2 years DFS is 78% [65].
In the present series patients receiving exclusive radiotherapy as first-line treatment, the 5-year PFS and OS rates were 32 and 51%, respectively, study. OS are reported in literature between 50 and 83% [66–68]. In the retrospective series reported by Celli et al. RT helped the 65 patients with neuro-logic signs (5-year survival rate, 11% vs. 53%; P = 0.002) [69]. Lindergaard et al. found that irradiation appears not to be of benefit after “total” removal. In this series patients with partly removed lesions appeared to benefit from post-operative radiotherapy; the median survival period after subtotal tumor resection was 37 months with and 26 months without radiotherapy (P = 0.0089) [70]. Shaw et al. analyzed of the subset of 63 patients who underwent subtotal resection alone or with RT showed that the median survival was 2 years for the eight patients with subtotal resection alone; 4 and 7 years for the 26 patients with surgery and low-dose (<5,000 cGy) RT; and 7.9 years for the 29 patients receiving surgery and high-dose RT (≥5,000 cGy) [71, 72]. In similar retrospective studies post-operative radiotherapy increased survival for several authors [73, 74] and had no impact [75, 76].
The respective indications for RT and chemotherapy are not well defined. Two multiinstitutional randomized trials have been performed to determine the contribution of PCV to OS and PFS of patients with newly diagnosed high-grade oligodendrogliomas. The RTOG 9402 study compared exclusive radiotherapy to dose-intensive PCV administered immediately before radiotherapy. The EORTC 26591 investigated the value of six cycles of PCV after radiotherapy compared with exclusive radiotherapy. In both studies PFS is better after association of radiotherapy and chemotherapy but OS is not significantly modified [21, 22]. In both studies 80% of patients assigned to the radiotherapy only group received chemotherapy at recurrence. The absence of benefit in OS may be a result of the efficacy of chemotherapy at the time of recurrence. It is regrettable that these randomized trials did not include an arm using exclusive chemotherapy, with OS and quality-of-life end points. In fact, these patients may well respond to RT, which, for small-volume tumors, may be the simpler therapeutic choice [77].
The EORTC 22845 [78] experience with low-grade gliomas has led to important conclusions: because radiotherapy delays progression, delaying radiotherapy results in lower PFS. However, radiotherapy delivered at relapse results in equivalent OS. It remains to be proven that delaying radiotherapy does not extend the field of radiation. It will be crucial to understand if delaying radiotherapy improves quality of life. Only Q-TWIST analysis in a randomized setting may be able to answer such a question [79].
In this series, PFS and OS did not differ significantly among the three treatment groups. As usual for retrospective studies, there are obvious biases. Initial prognostic factors were less favorable in the group of patients treated with exclusive RT. They had higher tumor grades. In all groups, second-line treatment was delivered at time of relapse, suggesting a similar philosophy of successive medical teams.
Our findings of 5-year OS of 71% and 5-year PFS of 44% after exclusive chemotherapy suggest that exclusive front-line chemotherapy is an efficient treatment. Exclusive chemotherapy with careful follow-up did not seem to reduce survival in our patients. First-line exclusive chemotherapy with PCV was advised as an option in the French “standard option and recommendations” [1]. Delaying radiotherapy with careful follow up seems possible but RT is a major treatment of oligodendroglioma. The search for 1p 19q deletion that was not available during the period of our study, may modify such conclusions in the future: selection of patients with molecular biology may isolate subgroups that would benefit more of this strategy.
Therefore, it may be suggested that, despite inevitable biases, this study may serve as a foundational randomized study for further strategies.
References
Frappaz D, Chinot O, Bataillard A, Ben Hassel M, Capelle L, Chanalet S et al (2003) Summary version of the standards, options and recommendations for the management of adult patients with intracranial glioma (2002). Br J Cancer 89(Suppl 1):S73–S83
Andersen AP (1978) Postoperative irradiation of glioblastomas. Results in a randomized series. Acta Radiol Oncol Radiat Phys Biol 17(6):475–484
Kristiansen K, Hagen S, Kollevold T, Torvik A, Holme I, Nesbakken R et al (1981) Combined modality therapy of operated astrocytomas grade III and IV. Confirmation of the value of postoperative irradiation and lack of potentiation of bleomycin on survival time: a prospective multicenter trial of the Scandinavian Glioblastoma Study Group. Cancer 47(4):649–652
Sandberg-Wollheim M, Malmstrom P, Stromblad LG, Anderson H, Borgstrom S, Brun A et al (1991) A randomized study of chemotherapy with procarbazine, vincristine, and lomustine with and without radiation therapy for astrocytoma grades 3 and/or 4. Cancer 68(1):22–29
Walker MD, Alexander E Jr, Hunt WE, MacCarty CS, Mahaley MS Jr, Mealey J Jr et al (1978) Evaluation of BCNU and/or radiotherapy in the treatment of anaplastic gliomas. A cooperative clinical trial. J Neurosurg 49(3):333–343
Walker MD, Green SB, Byar DP, Alexander E Jr, Batzdorf U, Brooks WH et al (1980) Randomized comparisons of radiotherapy and nitrosoureas for the treatment of malignant glioma after surgery. N Engl J Med 303(23):1323–1329
Fine HA, Dear KB, Loeffler JS, Black PM, Canellos GP (1993) Meta-analysis of radiation therapy with and without adjuvant chemotherapy for malignant gliomas in adults. Cancer 71(8):2585–2597
Stewart LA (2002) Chemotherapy in adult high-grade glioma: a systematic review and meta-analysis of individual patient data from 12 randomised trials. Lancet 359(9311):1011–1018
Karim AB, Afra D, Cornu P, Bleehan N, Schraub S, De Witte O et al (2002) Randomized trial on the efficacy of radiotherapy for cerebral low-grade glioma in the adult: European organization for research and treatment of cancer study 22845 with the medical research council study BRO4: an interim analysis. Int J Radiat Oncol Biol Phys 52(2):316–324
Karim AB, Maat B, Hatlevoll R, Menten J, Rutten EH, Thomas DG et al (1996) A randomized trial on dose-response in radiation therapy of low-grade cerebral glioma: European organization for research and treatment of cancer (EORTC) study 22844. Int J Radiat Oncol Biol Phys 36(3):549–556
Shaw E, Arusell R, Scheithauer B, O’Fallon J, O’Neill B, Dinapoli R et al (2002) Prospective randomized trial of low- versus high-dose radiation therapy in adults with supratentorial low-grade glioma: initial report of a north central cancer treatment group/radiation therapy oncology group/eastern cooperative oncology group study. J Clin Oncol 20(9):2267–2276
Donahue B, Scott CB, Nelson JS, Rotman M, Murray KJ, Nelson DF et al (1997) Influence of an oligodendroglial component on the survival of patients with anaplastic astrocytomas: a report of radiation therapy oncology group 83-02. Int J Radiat Oncol Biol Phys 38(5):911–914
Cairncross JG, Ueki K, Zlatescu MC, Lisle DK, Finkelstein DM, Hammond RR et al (1998) Specific genetic predictors of chemotherapeutic response and survival in patients with anaplastic oligodendrogliomas. J Natl Cancer Inst 90(19):1473–1479
Smith JS, Perry A, Borell TJ, Lee HK, O’Fallon J, Hosek SM et al (2000) Alterations of chromosome arms 1p and 19q as predictors of survival in oligodendrogliomas, astrocytomas, and mixed oligoastrocytomas. J Clin Oncol 18(3):636–645
Cairncross G, Macdonald D, Ludwin S, Lee D, Cascino T, Buckner J et al (1994) Chemotherapy for anaplastic oligodendroglioma. National cancer institute of Canada clinical trials group. J Clin Oncol 12(10):2013–2021
Cairncross JG (1994) Aggressive oligodendroglioma: a chemosensitive tumor. Recent Results Cancer Res 135:127–133
Chinot OL, Honore S, Dufour H, Barrie M, Figarella-Branger D, Muracciole X et al (2001) Safety and efficacy of temozolomide in patients with recurrent anaplastic oligodendrogliomas after standard radiotherapy and chemotherapy. J Clin Oncol 19(9):2449–2455
Hoang-Xuan K, Capelle L, Kujas M, Taillibert S, Duffau H, Lejeune J et al (2004) Temozolomide as initial treatment for adults with low-grade oligodendrogliomas or oligoastrocytomas and correlation with chromosome 1p deletions. J Clin Oncol 22(15):3133–3138
Mason WP, Krol GS, DeAngelis LM (1996) Low-grade oligodendroglioma responds to chemotherapy. Neurology 46(1):203–207
Paleologos NA, Macdonald DR, Vick NA, Cairncross JG (1999) Neoadjuvant procarbazine, CCNU, and vincristine for anaplastic and aggressive oligodendroglioma. Neurology 53(5):1141–1143
Soffietti R, Ruda R, Bradac GB, Schiffer D (1998) PCV chemotherapy for recurrent oligodendrogliomas and oligoastrocytomas. Neurosurgery 43(5):1066–1073
Stege EM, Kros JM, de Bruin HG, Enting RH, van H, I, Looijenga LH et al (2005) Successful treatment of low-grade oligodendroglial tumors with a chemotherapy regimen of procarbazine, lomustine, and vincristine. Cancer 103(4):802–809
Stupp R, Hegi ME, van den Bent MJ, Mason WP, Weller M, Mirimanoff RO et al (2006) Changing paradigms—an update on the multidisciplinary management of malignant glioma. Oncologist 11(2):165–180
Taliansky-Aronov A, Bokstein F, Lavon I, Siegal T (2006) Temozolomide treatment for newly diagnosed anaplastic oligodendrogliomas: a clinical efficacy trial. J Neurooncol 79(2):153–157
Triebels VH, Taphoorn MJ, Brandes AA, Menten J, Frenay M, Tosoni A et al (2004) Salvage PCV chemotherapy for temozolomide-resistant oligodendrogliomas. Neurology 63(5):904–906
Cairncross G, Berkey B, Shaw E, Jenkins R, Scheithauer B, Brachman D et al (2006) Phase III trial of chemotherapy plus radiotherapy compared with radiotherapy alone for pure and mixed anaplastic oligodendroglioma: intergroup radiation therapy oncology group trial 9402. J Clin Oncol 24(18):2707–2714
van den Bent MJ, Carpentier AF, Brandes AA, Sanson M, Taphoorn MJ, Bernsen HJ et al (2006) Adjuvant procarbazine, lomustine, and vincristine improves progression-free survival but not overall survival in newly diagnosed anaplastic oligodendrogliomas and oligoastrocytomas: a randomized European organisation for research and treatment of cancer phase III trial. J Clin Oncol 24(18):2715–2722
Brown PD, Buckner JC, O’Fallon JR, Iturria NL, Brown CA, O’Neill BP et al (2003) Effects of radiotherapy on cognitive function in patients with low-grade glioma measured by the folstein mini-mental state examination. J Clin Oncol 21(13):2519–2524
Kiebert GM, Curran D, Aaronson NK, Bolla M, Menten J, Rutten EH et al (1998) Quality of life after radiation therapy of cerebral low-grade gliomas of the adult: results of a randomised phase III trial on dose response (EORTC trial 22844). EORTC radiotherapy co-operative group. Eur J Cancer 34(12):1902–1909
Torres IJ, Mundt AJ, Sweeney PJ, Llanes-Macy S, Dunaway L, Castillo M et al (2003) A longitudinal neuropsychological study of partial brain radiation in adults with brain tumors. Neurology 60(7):1113–1118
Macdonald DR, Cascino TL, Schold SC Jr, Cairncross JG (1990) Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8(7):1277–1280
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Cox DR (1972) Regression models and life tables (with discussion). J R Stat Soc Ser B 34:187–202
Burger PC (1995) Revising the world health organization (WHO) blue book—’Histological typing of tumours of the central nervous system’. J Neurooncol 24(1):3–7
Hamlat A, Saikali S, Chaperon J, Le Calve M, Gedouin D, Ben Hassel M et al (2005) Oligodendroglioma: clinical study and survival analysis correlated with chromosomal anomalies. Neurosurg Focus 19(5):E15
Nijjar TS, Simpson WJ, Gadalla T, McCartney M (1993) Oligodendroglioma. The princess margaret hospital experience (1958–1984). Cancer 71(12):4002–4006
Shaw EG, Scheithauer BW, O’Fallon JR, Tazelaar HD, Davis DH (1992) Oligodendrogliomas: the Mayo clinic experience. J Neurosurg 76(3):428–434
Hamlat A, Saikali S, Chaperon J, Le Calve M, Gedouin D, Ben Hassel M et al (2005) Oligodendroglioma: clinical study and survival analysis correlated with chromosomal anomalies. Neurosurg Focus 19(5):E15
Nijjar TS, Simpson WJ, Gadalla T, McCartney M (1993) Oligodendroglioma. The princess margaret hospital experience (1958–1984). Cancer 71(12):4002–4006
Shaw EG, Scheithauer BW, O’Fallon JR, Tazelaar HD, Davis DH (1992) Oligodendrogliomas: the Mayo clinic experience. J Neurosurg 76(3):428–434
Abrey LE, Childs BH, Paleologos N, Kaminer L, Rosenfeld S, Salzman D et al (2006) High-dose chemotherapy with stem cell rescue as initial therapy for anaplastic oligodendroglioma: long-term follow-up. Neurooncology 8(2):183–188
Nijjar TS, Simpson WJ, Gadalla T, McCartney M (1993) Oligodendroglioma. The princess margaret hospital experience (1958–1984). Cancer 71(12):4002–4006
Shaw EG, Scheithauer BW, O’Fallon JR, Tazelaar HD, Davis DH (1992) Oligodendrogliomas: the Mayo clinic experience. J Neurosurg 76(3):428–434
Celli P, Nofrone I, Palma L, Cantore G, Fortuna A (1994) Cerebral oligodendroglioma: prognostic factors and life history. Neurosurgery 35(6):1018–1034
Gannett DE, Wisbeck WM, Silbergeld DL, Berger MS (1994) The role of postoperative irradiation in the treatment of oligodendroglioma. Int J Radiat Oncol Biol Phys 30(3):567–573
Celli P, Nofrone I, Palma L, Cantore G, Fortuna A (1994) Cerebral oligodendroglioma: prognostic factors and life history. Neurosurgery 35(6):1018–1034
Gannett DE, Wisbeck WM, Silbergeld DL, Berger MS (1994) The role of postoperative irradiation in the treatment of oligodendroglioma. Int J Radiat Oncol Biol Phys 30(3):567–573
Celli P, Nofrone I, Palma L, Cantore G, Fortuna A (1994) Cerebral oligodendroglioma: prognostic factors and life history. Neurosurgery 35(6):1018–1034
Gannett DE, Wisbeck WM, Silbergeld DL, Berger MS (1994) The role of postoperative irradiation in the treatment of oligodendroglioma. Int J Radiat Oncol Biol Phys 30(3):567–573
Cairncross G, Macdonald D, Ludwin S, Lee D, Cascino T, Buckner J et al (1994) Chemotherapy for anaplastic oligodendroglioma. National cancer institute of Canada clinical trials group. J Clin Oncol 12(10):2013–2021
Macdonald DR, Gaspar LE, Cairncross JG (1990) Successful chemotherapy for newly diagnosed aggressive oligodendroglioma. Ann Neurol 27(5):573–574
Cairncross G, Berkey B, Shaw E, Jenkins R, Scheithauer B, Brachman D et al (2006) Phase III trial of chemotherapy plus radiotherapy compared with radiotherapy alone for pure and mixed anaplastic oligodendroglioma: intergroup radiation therapy oncology group trial 9402. J Clin Oncol 24(18):2707–2714
Felsberg J, Erkwoh A, Sabel MC, Kirsch L, Fimmers R, Blaschke B et al (2004) Oligodendroglial tumors: refinement of candidate regions on chromosome arm 1p and correlation of 1p/19q status with survival. Brain Pathol 14(2):121–130
Ino Y, Betensky RA, Zlatescu MC, Sasaki H, Macdonald DR, Stemmer-Rachamimov AO et al (2001) Molecular subtypes of anaplastic oligodendroglioma: implications for patient management at diagnosis. Clin Cancer Res 7(4):839–845
Smith JS, Perry A, Borell TJ, Lee HK, O’Fallon J, Hosek SM et al (2000) Alterations of chromosome arms 1p and 19q as predictors of survival in oligodendrogliomas, astrocytomas, and mixed oligoastrocytomas. J Clin Oncol 18(3):636–645
van den Bent MJ, Carpentier AF, Brandes AA, Sanson M, Taphoorn MJ, Bernsen HJ et al (2006) Adjuvant procarbazine, lomustine, and vincristine improves progression-free survival but not overall survival in newly diagnosed anaplastic oligodendrogliomas and oligoastrocytomas: a randomized European organisation for research and treatment of cancer phase III trial. J Clin Oncol 24(18):2715–2722
Taliansky-Aronov A, Bokstein F, Lavon I, Siegal T (2006) Temozolomide treatment for newly diagnosed anaplastic oligodendrogliomas: a clinical efficacy trial. J Neurooncol 79(2):153–157
van den Bent MJ, Taphoorn MJ, Brandes AA, Menten J, Stupp R, Frenay M et al (2003) Phase II study of first-line chemotherapy with temozolomide in recurrent oligodendroglial tumors: the European organization for research and treatment of cancer brain tumor group study 26971. J Clin Oncol 21(13):2525–2528
Chinot OL, Honore S, Dufour H, Barrie M, Figarella-Branger D, Muracciole X et al (2001) Safety and efficacy of temozolomide in patients with recurrent anaplastic oligodendrogliomas after standard radiotherapy and chemotherapy. J Clin Oncol 19(9):2449–2455
van den Bent MJ, Chinot O, Boogerd W, Bravo MJ, Taphoorn MJ, Kros JM et al (2003) Second-line chemotherapy with temozolomide in recurrent oligodendroglioma after PCV (procarbazine, lomustine and vincristine) chemotherapy: EORTC brain tumor group phase II study 26972. Ann Oncol 14(4):599–602
van den Bent MJ, Chinot O, Boogerd W, Bravo MJ, Taphoorn MJ, Kros JM et al (2003) Second-line chemotherapy with temozolomide in recurrent oligodendroglioma after PCV (procarbazine, lomustine and vincristine) chemotherapy: EORTC brain tumor group phase II study 26972. Ann Oncol 14(4):599–602
Triebels VH, Taphoorn MJ, Brandes AA, Menten J, Frenay M, Tosoni A et al (2004) Salvage PCV chemotherapy for temozolomide-resistant oligodendrogliomas. Neurology 63(5):904–906
Franceschi E, Omuro AM, Lassman AB, Demopoulos A, Nolan C, Abrey LE (2005) Salvage temozolomide for prior temozolomide responders. Cancer 104(11):2473–2476
Mason WP, Krol GS, DeAngelis LM (1996) Low-grade oligodendroglioma responds to chemotherapy. Neurology 46(1):203–207
Abrey LE, Childs BH, Paleologos N, Kaminer L, Rosenfeld S, Salzman D et al (2006) High-dose chemotherapy with stem cell rescue as initial therapy for anaplastic oligodendroglioma: long-term follow-up. Neurooncology 8(2):183–188
Allam A, Radwi A, El Weshi A, Hassounah M (2000) Oligodendroglioma: an analysis of prognostic factors and treatment results. Am J Clin Oncol 23(2):170–175
Gannett DE, Wisbeck WM, Silbergeld DL, Berger MS (1994) The role of postoperative irradiation in the treatment of oligodendroglioma. Int J Radiat Oncol Biol Phys 30(3):567–573
Nijjar TS, Simpson WJ, Gadalla T, McCartney M (1993) Oligodendroglioma. The princess margaret hospital experience (1958–1984). Cancer 71(12):4002–4006
Celli P, Nofrone I, Palma L, Cantore G, Fortuna A (1994) Cerebral oligodendroglioma: prognostic factors and life history. Neurosurgery 35(6):1018–1034
Lindegaard KF, Mork SJ, Eide GE, Halvorsen TB, Hatlevoll R, Solgaard T et al (1987) Statistical analysis of clinicopathological features, radiotherapy, and survival in 170 cases of oligodendroglioma. J Neurosurg 67(2):224–230
Shaw EG, Scheithauer BW, O’Fallon JR, Tazelaar HD, Davis DH (1992) Oligodendrogliomas: the Mayo clinic experience. J Neurosurg 76(3):428–434
Shaw EG, Scheithauer BW, O’Fallon JR, Tazelaar HD, Davis DH (1992) Oligodendrogliomas: the Mayo clinic experience. J Neurosurg 76(3):428–434
Gannett DE, Wisbeck WM, Silbergeld DL, Berger MS (1994) The role of postoperative irradiation in the treatment of oligodendroglioma. Int J Radiat Oncol Biol Phys 30(3):567–573
Allison RR, Schulsinger A, Vongtama V, Barry T, Shin KH (1997) Radiation and chemotherapy improve outcome in oligodendroglioma. Int J Radiat Oncol Biol Phys 37(2):399–403
Kros JM, Pieterman H, van Eden CG, Avezaat CJ (1994) Oligodendroglioma: the Rotterdam-Dijkzigt experience. Neurosurgery 34(6):959–966
Bullard DE, Rawlings CE III, Phillips B, Cox EB, Schold SC Jr, Burger P et al (1987) Oligodendroglioma. An analysis of the value of radiation therapy. Cancer 60(9):2179–2188
Stupp R, Hegi ME, van den Bent MJ, Mason WP, Weller M, Mirimanoff RO et al (2006) Changing paradigms—an update on the multidisciplinary management of malignant glioma. Oncologist 11(2):165–180
Karim AB, Afra D, Cornu P, Bleehan N, Schraub S, De Witte O et al (2002) Randomized trial on the efficacy of radiotherapy for cerebral low-grade glioma in the adult: European organization for research and treatment of cancer study 22845 with the medical research council study BRO4: an interim analysis. Int J Radiat Oncol Biol Phys 52(2):316–324
Sloan JA, Sargent DJ, Lindman J, Allmer C, Vargas-Chanes D, Creagan ET et al (2002) A new graphic for quality adjusted life years (Q-TWiST) survival analysis: the Q-TWiST plot. Qual Life Res 11(1):37–45
Acknowledgments
We are indebted to the neuro-oncology division of the Oncology Rhône-Alpes Network (ONCORA). Acknowledgement to Rosalyn Vu for Editing of this manuscript. Preliminary results were presented as a poster at the October 2001 meeting of the American Society of Radiotherapy (ASTRO).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sunyach, M.P., Jouvet, A., Perol, D. et al. Role of exclusive chemotherapy as first line treatment in oligodendroglioma. J Neurooncol 85, 319–328 (2007). https://doi.org/10.1007/s11060-007-9422-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-007-9422-3