Abstract
Introduction
Between surgery and radiotherapy patients with a malignant glioma may encounter a number of psychosocial issues that could invoke an anxious or depressive response. This study explored the frequency, severity and cause of anxiety and depression in patients with presumed malignant brain tumours in the period between their surgery and radiotherapy.
Methods
A prospective study of 51 patients used mixed methods to measure anxiety and depression at three time points; post surgery, three weeks post surgery and pre radiotherapy. Analysis was undertaken using statistical and content analysis of the Hospital Anxiety and Depression (HAD) scores and unstructured interviews respectively.
Results
Analysis of HAD scores indicated a heightened level of anxiety in patients pre radiotherapy. This anxiety is more prevalent in younger patients and is not related to the patients change in functional state. Five patients had a significant depression at one or more time points between surgery and radiotherapy. Four of the five patients who reported scores consistent with depression had past histories of depression. Content analysis of unstructured interviews indicated that the HAD scores underestimated the presence of anxiety and depression amongst this group of patients.
Conclusion
Anxiety was more common in younger patients. Anxiety was slightly more frequent pre-radiotherapy. A past medical history of depression is a predictor of significant depression in the post-operative period. The HAD scale although useful is not an adequate measurement tool for detecting anxiety and depression amongst all patients and health care professionals should adopt other means to monitor for these signs and symptoms.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The functional and psychosocial issues experienced by patients with malignant brain tumours in the period between surgery and radiotherapy has never been investigated in much detail. Interestingly, although many studies have investigated treatment, fewer studies have investigated the impact of the diagnosis on patient’s lives [1, 2]. It is widely acknowledged that psychosocial issues experienced by patients who have been given a diagnosis of malignant glioma requires further attention [1–5]. Although previous studies do not explicitly explore the period between surgery and radiotherapy, their findings provide us with some insight to what may induce psychosocial issues during this time.
Between surgery and radiotherapy, patients who have malignant glioma may encounter many stressors that could invoke an anxious or depressive response [6–8]. The prevalence of anxiety and, to a lesser extent, depression in patients with different types of common cancer is well documented. In one study the incidence of anxiety amongst breast cancer patients was recorded at 83% [6]. Although a study in patients with brain tumours reported a relatively low level of anxiety (30%) and depression (16%) before and after surgery [9]. The differences between the results of these two studies can be partially explained by methodological differences. Anxiety was present in 83% of patients after diagnosis when qualitative reporting measures were used amongst patients who were told of their diagnosis prior to surgery. Whereas significant levels of depression were not detected when the HAD scale was used in a group of brain tumour patients who had not been informed of their diagnosis [9].
Giovagnali (1999) studied quality of life in 57 brain tumour patients and compared it to the quality of life scores of 24 patients with other chronic neurological disease [10]. It was concluded that anxiety was common in the later stages of the disease (after radiotherapy and on commencement of chemotherapy). Using the State Trait Anxiety Inventory and unstructured interviews, Oberst and James (1985), examined the ‘post discharge’ period of 40 patients and their spouses [11]. Uncertainty and anxiety was present in over 50% of these patients within 60 days of their discharge. In some patients frequency of anxiety increased after this time. Interestingly, in another study comparing the anxiety of patients with breast cancer and their spouses at three time points: pre surgery, post surgery, and at three months, 83% of patients indicated they were most anxious pre surgery [6].
Maunsell et al (1992) studied 235 patients at two time points after their surgical treatment for breast cancer (three and 18 months) using the Psychiatric Symptom Index (PSI) and Unstructured Interviews [12]. The PSI scores were the primary outcome measure and analysis indicated that past stressful events and a history of depression were all strong indicators of poor psychological adjustment.
For these reasons we decided to use both the HAD scale and unstructured interviews to explore the frequency, severity and cause of anxiety and depression in patients with presumed malignant brain tumours in the period between their surgery and radiotherapy.
Materials and methods
Design
A prospective study was undertaken of all patients referred with a history, examination and cranial imaging consistent with a diagnosis of a malignant brain tumour in a Regional Neuroscience Unit (catchment 1.6 million).
The study inclusion criteria were:
-
Age > = 18
-
Able to give informed consent (no significant dysphasia)
-
Scan consistent with a single intracerebral tumour, likely to be a malignant glioma
Patients were excluded if:
-
They were previously known to have a brain tumour (e.g. not first presentation)
-
They had previous cranial irradiation (e.g. prophylactic cranial irradiation for small cell lung cancer/leukaemia)
-
They were already involved in another research study using experimental therapy
Data collection tools
We used mixed methods to explore the research questions because we considered that rating scales for anxiety and depression alone may not provide sufficient depth of information to inform the study.
To screen for anxiety and depression, patients were asked to complete the HAD scale at three time points during the study period; post surgery, three weeks after surgery and final follow up (pre radiotherapy for the patients who received it). The HAD scale is a test of psychological well being [13]. It consists of 14 questions divided into two sub scales––one for anxiety one for depression––of seven questions each. Each question is rated by the patient on a four point scale. The score for each item represents the degree of distress suffered by the patient (0 = none, 4 = unbearable). Items for each sub scale are summated. A score of 11+ on either scale is taken to indicate a definite case of anxiety and/or depression.
Over a one year period n = 51 patients were recruited. Each patient was interviewed weekly by a semi structured telephone interview to detect any reasons for anxiety and/or depressive thoughts. Additionally four (n = 4) patients were selected for an unstructured interview after commencement of their radiotherapy. Questions relating to anxiety and depression were open ended. Patients were asked “How have you been feeling over the past week?” If necessary the patients were asked to elaborate on the response they gave.
The analysis of the HAD data in conjunction with weekly telephone interviews and unstructured interviews were used to provide detail to the severity and aetiology of anxiety and depression within the study.
Ethical considerations
Ethical approval for this study was obtained from the Regional Ethical Committee (Application 1702/98/4/104).
Data analysis
The HAD scores were analysed using a t test. The transcripts of the weekly interviews were analysed using content analysis [14, 15]. Anxiety and Depression were identified as priori categories for the analysis of the interview transcripts. These categories were systematically applied to the transcripts to gain insight into the anxious and depressive symptoms described by the patients.
Results
Subjects
Fifty-one patients were recruited from a potential 65 patients within the 12 months of the study. Twenty eight males (n = 28) and 23 females (n = 23) consented to participate in the study. The median age was 55 (range 22–80). Forty (78%) of the patients were married, three (6%) were single, three (6%) were divorced, four (8%) were widowed and one (2%) was living with their partner. All had a surgical procedure for confirmation of diagnosis. Fourteen patients were omitted from the study as they were lost to follow upFootnote 1(n = 10) or their confirmed diagnosis was not as anticipated (n = 4) e.g. cerebral abscess. Forty six patients (90%) were offered radiotherapy after histological confirmation of the diagnosis and discussion with the Radiation Oncologist. However, only 38 patients who were offered radiotherapy, received it as six patients deteriorated while awaiting radiotherapy and were subsequently felt to be unsuitable and two patients later refused treatment. Table 1 indicates the demographic details of the patients receiving surgery, radiotherapy and dexamethasone therapy throughout the study period. The mean length of time in days between surgery and radiotherapy for the patients was 41 days (SD 13.6) with the median length of time being 38 days.
Quantitative results
Hospital anxiety and depression questionnaire
The HAD scale scores of anxiety and depression were measured in 38/51 (74%) patients post surgery, 20/51 (40%) three weeks after their surgery and 35/51 (69%) at final data collection point. Twenty three out of thirty five (65%) of the patients who completed the HAD at two time points (post surgery and at final data collection point) improved physically functionally during the period between surgery and radiotherapy, 9/25 (36%) showed no change and 3/37 (8%) deteriorated. Sixteen out of fifty one (31%) patients failed to complete the HAD scale. Patients were less likely to complete the HAD scale if they had physically or cognitively deteriorated. Therefore the results discussed can only be applicable to patients who improve or functionally remain the same between surgery and radiotherapy since 6/11 (55%) patients who deteriorated between surgery and radiotherapy did not complete the HAD scale. If anxiety and depression is associated with physical disability this finding indicates that these results may underestimate the frequency of anxiety and depression.
Due to the small sample size and the small change in anxiety and depression levels noted between patients at the two time points no significant change in these scores could be measured using a t test (P = 0.05). However, simple descriptive analysis of the data did reveal some interesting findings (see Table 2 and 3).
The mean score of anxiety and depression over the three study time points (post operatively, three weeks post operatively and final point of data collection) are all significantly below the level that indicates a case of anxiety or depression (score ≥11). Patients who improve or functionally remain the same between surgery and radiotherapy do not report a high level of anxiety and depression on the HAD questionnaire.
Frequency and severity of anxiety between surgery and radiotherapy
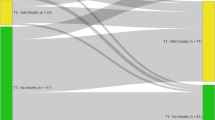
The HAD scale detected that n = 5 (13%) patients were anxious after their surgery, and four (11%) of these continued to be anxious throughout the period of time between surgery and radiotherapy. Eight (22%) patients were anxious prior to their radiotherapy. Five (62%) of these patients had not been significantly anxious post surgery. The HAD scale demonstrated a heightened level of anxiety in patients prior to their radiotherapy. Anxiety was more common in younger patients between surgery and radiotherapy (see Table 2).
Overall 13 (35%) patients were detected to be suffering from anxiety by the HAD. The level of anxiety that was detected by the HAD scale does not reflect the level of anxiety prevalent amongst all patients within the study that was apparent from analysis of the interview transcripts.
Changes in depression
The HAD scale detected that only five patients had significant depression (defined by HAD) at one or more times between surgery and radiotherapy (see Table 3). Two (6%) patients had significant depression post surgery and one (3%) of these patients continued to report a high depression score pre radiotherapy. Four of the patients (80%) who reported heightened level of depression between surgery and radiotherapy had a past medical history of depressive illness. The other patient who became depressed also deteriorated functionally between surgery and radiotherapy. Patients who clinically deteriorated completed the HAD scale less often and therefore the frequency of depression reported may be an underestimate.
Qualitative results
From the weekly telephone interviews it was apparent that there were a number of factors that were causing anxiety and depression amongst the patients. Content analysis of the qualitative data demonstrated a frequency of anxiety in 36 (61%) of patients. The source of this anxiety was firstly, the forthcoming treatment and secondly, the effect of the brain tumour. Depressive thoughts appear to be less prevalent than anxiety although 25 (50%) patient indicated feeling low in mood at one point during the study period.
Content analysis of the interview data concluded that one of the main sources of this anxiety was waiting for the impending radiotherapy treatment. People were anxious as they did not know when their radiotherapy would start. They also were unsure of what it would involve.
36 (75%) of respondents highlighted during the telephone interviews that the lack of information about their start date for radiotherapy was concerning them.
The uncertainty of what radiotherapy would entail was causing 18 (35%) of patients to feel anxious about the whole experience. However, when this was further explored during the interviews it was interesting to note that some of the patients and carers who identified their need for more information about the radiotherapy had actually sought it out themselves from a number of sources.
Many patients resolved some of their uncertainties about radiotherapy treatment by asking the researcher questions during the telephone interviews:
Three (17%) patients’ held mistaken ideas about the effects, side effects and benefits of radiotherapy. Was she going to get her hair cut off so that she could get a good fitting wig prior to radiotherapy that she could wear after?
Another source of anxiety expressed by 30 (58%) of the patients was related to the fear that the tumour in their head was growing and spreading and would continue to do so until the start of their radiotherapy.
Eighteen (46%) patients mentioned to the researcher, during the telephone interview, that they were concerned about changes in their physical state. Forty two (82%) patients would describe problems that were obviously related to dexamethasone therapy. e.g. heart burn, oral thrush, insomnia, night sweats, urine frequency and excessive eating, but their concern was that this was tumour rather than dexamethasone related.
Some of the comments made by patients about their mood indicated that they could be having depressive symptoms in the period between surgery and radiotherapy. In response to the question ‘How are you feeling?’ over 50% of the patients on at least two occasions stated they were feeling ‘low in mood’ or ‘fed up’.
The cause of this low mood could only be ascertained for a few of the patients, but these patients associated their low mood to their hair loss, weight gain, tiredness and/or poor functional state.
Discussion
It is understandable why patients may be anxious or depressed in the time between neuro-surgical intervention and initiation of radiation therapy. There is a lot to think about and a lot of uncertainty regarding the diagnosis, prognosis, the side effects and effectiveness of treatment (surgery or radiation therapy) and when it will start. There are also issues of how the person, family and perhaps work will manage in their absence, either organizationally or financially. It is a time when there is consideration of mortality and it will clearly be a time of stress. When the patient is discharged from hospital and the initial active intervention, which has often been performed expeditiously, is over, thoughts may move on to what the next stage holds and when will it start. It may also be a time when general information about the tumour type may be sought from official or non-official sources (friends, family, internet). Doubts and uncertainties increase and patients may consider; Why have some symptoms not settled? What do new symptoms mean? Therefore this is an important time to assess peoples feelings in the most scientifically valid way possible, accepting that scientific methodology may have to be relaxed in favor of clinically sound person-centred evaluation. For example, it is not feasible to perform a full psychiatric interview at different time points in all patients during this time to classify any psychiatric condition and decide whether treatment would be valuable.
Our study has shown the limitation of using a screening tool such as the HAD to study the presence and record the severity of anxiety or depression. Especially if the cut off to define anxiety is high. It is stated that the HAD is a reliable self assessment tool, that can be utilised outwith and within the hospital setting [9, 13, 16]. In comparison to other tools utilised to screen psychological disorders e.g. General Health Questionnaire, the HAD separates the concept of anxiety and depression, assesses the degree of change and is user friendly for the researcher and the participant [13]. The level of anxiety prevalent amongst patients during the study period was underestimated by the HAD measurement scale with a cut off ≥ 11. Patients who deteriorated functionally within the study period did not complete the HAD scale and consequently only 69% of patients scores were analysed. Analysis of the HAD scores indicated that anxiety was only present in 13–22% of patients, whereas, content analysis of the telephone and unstructured interview transcripts indicated that 75% of people were anxious about aspects of their radiotherapy and 58% were anxious about their tumour growing. These contrasting findings may help explain some of the discrepancies that exist within the literature regarding the prevalence of anxiety after a malignant diagnosis [9, 17]. Different measurement tools for the same dependent variable can produce significantly different results and this was highlighted throughout the data analysis stage of this study. Contrasting results were found within the measurement of all the dependent variables that were measured using a self completion questionnaire and a form of interview between the researcher and the patient.
The HAD scale detected significant depression in 2–3% of patients. However, depressive symptoms such as feeling ‘low in mood’ were recorded in over half of the patient transcripts. The cause of these depressive symptoms could not be established for all patients from the transcripts but some patients did associate their feelings to their physical functional state, hair loss, weight gain and/or tiredness. People with a history of depressive illness were more likely to report a depressive state post operatively.
Adelbratt and Strang (2000) and Curren (2001) detected denial, anger, fear, anxiety and guilt within the first three months after diagnosis of a brain tumour amongst [18, 19]. This study found that patients had anxieties and fears about their tumour growing (58%) and their radiotherapy treatment (35%). The researchers belief that lack of information may have contributed to these feelings. Thirty Five percent of patients were asking questions about radiotherapy indicating that they were unclear of what it would entail, its effects and response. Shaw (1999) states that the information people have regarding their situation affects the way they construct their representation of it [20]. In the initial stages of diagnosis patients require information about proposed therapy, sequence of future events, side effects of treatment, symptom management and prognosis [21]. According to the results of this study some (35–58%) patients awaiting radiotherapy did not have sufficient information and this caused them heightened anxiety and fear.
At the outset of this study the researchers believed that marital status would influence patients coping behavior as from their personal experience patients with close spouses tended to cope better. Northouse (1989) provided some findings to support this anecdotal evidence but within this study the only patient characteristic that statistically influenced any of the findings was age [6]. The age of patients has been associated with the frequency of anxiety and the coping behavior elicited by patients in other studies [20, 22, 23]. It is suggested from the current study that younger patients with a malignant glioma may report heightened anxiety between surgery and radiotherapy, but, the difference in anxiety levels reported within this study were not statistically significant. However, as many of the patients who encounter a malignant glioma are aged ≤61, it is worth examining this finding further as it may provide the basis for future research. According to Shaw (1999) patients assess a situation by determining the threat they perceive the illness to have on their life commitments e.g. family role and work life [20]. As many younger patients are more likely to have an active work, family and social life than older patients, one could hypothesis that the level of threat that an illness has on their lives is greater than perceived by older individuals [20]. This study would be supportive of this theory.
This study also found that people who had suffered from depressive illness in the past were more likely to exhibit depression in the period between surgery and radiotherapy. These findings concur with the findings of Maunsell et al. (1992) [12].
The analysis of the data had limitations due to the small sample size, limitations in patient recruitment, limitations in obtaining complete data or detailed data from serial measures, which makes statistical analysis fraught with difficulty. Nevertheless, on balance we believe that the results reflect the occurrence and development of anxiety and depression in a representative group of patients attending a regional neuro-oncology centre who would be suitable for and eventually receive radiation therapy for malignant brain tumour.
Recommendations
Between surgery and radiotherapy some patients may suffer from anxiety and depression. Only a small percentage of patients have significant anxiety and depression as graded by the HAD. However, the HAD scale although useful is not an adequate measurement tool for detecting anxiety and depression amongst all patients and health care professionals should adopt other means to monitor for these signs and symptoms. Particular attention should be paid to patients with a past medical history of depressive illness between surgery and radiotherapy. Recurrence of significant depression is likely to occur in this stressful period. Younger patients may be at heightened risk of suffering from signs of anxiety between surgery and radiotherapy but further research is required to validate this finding.
Lack of or conflicting information about radiotherapy and delays in treatment are likely to increase patients’ anxiety. Patients need simple and specific sources of information about their tumour type, their symptoms and, more specifically, the planning and delivery of their radiotherapy treatment in the period between surgery and radiotherapy. This information must be readily accessible following surgery shortly after their discharge from the treatment hospital.
Notes
There were three reasons why the study only approached 65 patients of a potential 100–150 patients: Despite best efforts not all patients admitted to the study centre were referred to the researcher, the researcher was on holiday at three time points during data collection period and patients in concurrent trials (of which there were three at the time of this study) were not eligible for inclusion.
References
Salander P, Bergenheim T, Henriksson R (1996) The creation of protection and hope in patients with malignant brain tumours. Soc Sci Med 42(7):985–996
Gupta T, Sarin R (2002) Poor prognosis high grade gliomas: evolving an evidence based standard of care. Lancet Oncol 3:557–564
Gregor A, Cull A (1996) Radiotherapy for malignant glioma. Br Med J 313:1500–1501
Lovely MP (1998) Quality of life of brain tumour patients. Semin Oncol Nurs 14(1):73–80
Huang ME, Wartella J, Kreutzer J, Broaddus W, Lyckholm L (2001) Functional outcomes and quality of life in patients with brain tumours–a review of the literature. Brain Inj 15(10):843–856
Northouse L (1989) The impact of breast cancer on patients and husbands. Cancer Nurs 12(5):276–284
Halm M, Titler M, Kleiber C, et al (1993) Behavioural responses of family members during critical illness. Clin Nurs Res 2(4):414–437
Northouse L, Jeffs M, Caraway A, Lampman L, Dorris G (1995) Emotional distress reported by women and husbands prior to breast surgery. Nurs Res 44(4):196–201
Pringle AM, Taylor R, Whittle IR (1999) Anxiety and depression in patients with and intracranial neoplasm before and after tumour surgery. Br J Neurosurg 13(1):46–51
Giovagnoli AR (1999) Quality of life in patients with stable disease after surgery, radiotherapy and chemotherapy for malignant brain tumour. J Neurol Neurosurg Psychiatry 67:358–363
Oberst M, James R (1985) Going home: patient and spouse adjustment following cancer surgery. Top Clin Nurs 7(1):46–57
Maunsell E, Brisson J, Duchenes L (1992) Psychological distress after initial treatment of breast cancer. Cancer 70(1):121–125
Zigmond AS, Snaith RP (1983) The Hospital anxiety & depression scale. Acta Psychiatry 67:361–370
Downe-Wambolt B (1992) Content analysis: methods, applications and issues. Health Care Women Int 13:313–321
Silverman D (ed) (2004) Qualitative Research Theory, Method & Practice 2nd Edition, Sage Publications, London, Thousand Oaks, New Delhi
Grant R, Whittle IR, Gregor A, Kaar G, Mathew P (1999) A prospective study of the Royal College of Physicians Guidelines for the management of malignant glioma. Unpublished results of paper submitted to Scottish Executive, December
Zabora J, Brintzenhofeszoc K, Curbow B, Hooker C, Plantadosi S (2001) The prevalence of psychological distress by cancer site. Psycho Oncology 10(1):19–28
Adelbratt S, Strang P (2000) Death anxiety in brain tumour patients and their spouses. Palliat Med 14:499–507
Curren JR (2001) Support needs of brain tumour patients and their carers: the place of a telephone service. Int J Palliat Nurs 7(7):331–337
Shaw C (1999) A framework for the study of coping, illness behaviour and outcomes. J Adv Nurs 29(5):1246–1255
Adams M (1991) Information and education across the phases of cancer care. Semin Oncol Nurs 7:105–111
Morris T, Greer S, Pettingale RW, Watson M (1981) Patterns of Expression & Anger and Psychological Correlates in women with breast cancer, London
Hughson AVM, Cooper AF, McArdle C, Smith DC (1988) Psychological morbidity in patients awaiting breast biopsy. J Psychosom Res 32(2):173–180
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kilbride, L., Smith, G. & Grant, R. The frequency and cause of anxiety and depression amongst patients with malignant brain tumours between surgery and radiotherapy. J Neurooncol 84, 297–304 (2007). https://doi.org/10.1007/s11060-007-9374-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-007-9374-7