Supported by National Institutes of Health grant nos. 1-P50-CA108786-01, NS20023 and CA11898 and by grant no. MO1 RR 30 through the General Clinical Research Centers Program, National Center for Research Resources, National Institutes of Health.
Abstract
Purpose
Recent reports demonstrate the activity of imatinib mesylate, an ATP-mimetic, tyrosine kinase inhibitor, plus hydroxyurea, a ribonucleotide reductase inhibitor, in patients with recurrent glioblastoma multiforme. We performed the current phase 2 study to evaluate this regimen among patients with recurrent WHO grade III malignant glioma (MG).
Patients and method
Patients with grade III MG at any recurrence, received imatinib mesylate plus hydroxyurea (500 mg twice a day) orally on a continuous, daily schedule. The imatinib mesylate dose was 500 mg twice a day for patients on enzyme inducing anti-epileptic drugs (EIAEDs) and 400 mg once a day for those not on EIAEDs. Clinical assessments were performed monthly and radiographic assessments were obtained at least every 2 months. The primary endpoint was 6-month progression-free survival (PFS) rate.
Results
Thirty-nine patients were enrolled. All patients had progressive disease after prior radiotherapy and at least temozolomide-based chemotherapy. The median number of episodes of prior progression was 2 (range, 1–7) and the median number of prior treatment regimens was 3 (range, 1–8). With a median follow-up of 82.9 weeks, 24% of patients were progression-free at 6 months. The radiographic response rate was 10%, while 33% achieved stable disease. Among patients who achieved at least stable disease at first evaluation, the 6-month and 12-month PFS rates were 53% and 29%, respectively. The most common grade 3 or greater toxicities were hematologic and complicated less than 4% of administered courses.
Conclusion
Imatinib mesylate plus hydroxyurea, is well tolerated and associated with anti-tumor activity in some patients with recurrent grade 3 MG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gliomas, the most common primary neoplasm of the CNS, constitute a complex spectrum of heterogeneous tumors. High-grade or malignant gliomas (MG), which include World Health Organization (WHO) grade III and IV neoplasms, account for the majority of glial neoplasms and remain essentially fatal diagnoses. Current standard therapy for patients with newly diagnosed grade III MG, including anaplastic astrocytoma (AA), anaplastic oligodendroglioma (AO) and anaplastic oligoastrocytoma (AOA), includes surgery, radiotherapy and chemotherapy [1–3]. In general, grade III MG respond more favorably to post-surgical therapy than grade IV MG [4–8], with grade III tumors that exhibit deletion of chromosomes 1p and 19q being the most responsive MG subtype [9–12]. However, the vast majority of grade III MG tumors lack these chromosomal changes. Following recurrence, most salvage therapies offer essentially palliative benefit [1, 13, 14].
WHO grade III MG tumors typically affect younger patients than grade IV MG tumors, with an average age at onset of 41 years [15]. Thus, in addition to greater overall years of lost life, grade III MG tumors frequently terminate promising professional careers abruptly and deprive young families of parents and spouses. Clearly, more effective therapies are desperately needed for patients afflicted with these tumors.
We recently reported that the regimen of imatinib mesylate (Gleevec®, Glivec®, formerly STI571, Novartis, Basel, Switzerland), a selective receptor tyrosine kinase inhibitor of Bcr-Abl, c-KIT, c-fms, and platelet-derived growth factor receptor (PDGFR), plus hydroxyurea, a ribonucleoside diphosphate reductase inhibitor, has significant activity in the treatment of patients with recurrent (GBM) glioblastoma multiforme [16]. These results were unexpected as neither agent has been effective for MG patients when used as either monotherapy or in other combinatorial regimens [8, 17–20]. We now report a single-arm, phase 2 study demonstrating that imatinib plus hydroxyurea is also active in the treatment of some patients with recurrent WHO grade III MG.
Patients and methods
Study objectives
The primary objective of this single-arm, single institution, open-labeled, phase 2 study was to determine the 6-month PFS of adults with recurrent WHO grade III malignant glioma treated with imatinib plus hydroxyurea. Secondary objectives included: (1) determination of median PFS, overall survival (OS) and radiographic response in this patient population and; (2) further evaluation of the toxicity of this regimen.
Patient eligibility
Patients were required to: (1) have a histologically confirmed diagnosis of recurrent/progressive anaplastic astrocytoma (AA), anaplastic oligodendroglioma (AO) or mixed anaplastic oligoastrocytoma (AOA); (2) be 18 years of age; (3) have evidence of measurable enhancing disease on contrast-enhanced MRI; (4) have an interval of at least 2 weeks between prior surgical resection or 4 weeks between prior radiotherapy (XRT) or chemotherapy (except nitrosoureas which require 6 weeks); (5) have a Karnofsky performance score (KPS) 60%, and; (6) be on a stable dose of corticosteroids for at least 1 week. Additional enrollment criteria included: hematocrit >29%, ANC >1,500 cells/l, platelet count >100,000 cells/l; and serum creatinine, BUN, AST and bilirubin <1.5 times the upper limit of normal; recovery from all expected toxicity related to previous therapy; and written informed consent as approved by the DUMC IRB. Patients with a prior history of low-grade glioma were eligible if their most recent histopathology evaluation revealed WHO grade III malignant glioma and they were previously treated with external beam radiotherapy. There was no restriction on the number of prior treatment regimens or episodes of progressive disease.
Patients were excluded for any of the following: prior progressive disease or toxicity grade ≥3 with hydroxyurea; prior treatment with imatinib; excessive risk of bleeding (defined as either stroke within the prior 6 months, history of CNS or intraocular bleed, or septic endocarditis, evidence of intratumoral hemorrhage on pretreatment diagnostic imaging except for stable post-operative grade 1 hemorrhage, or active systemic bleeding); female patients who were pregnant or breast feeding; adults of reproductive potential not employing an effective method of birth control; concurrent severe and/or uncontrolled cardiac disease, chronic renal disease, active uncontrolled infection and acute or chronic liver disease; confirmed diagnosis of HIV infection; impairment of gastrointestinal (GI) function or GI disease that may significantly alter the absorption of imatinib; concurrent therapy with Coumadin (warfarin sodium); and grade 2 or greater peripheral edema or central/systemic fluid collections (pericardial effusion; pulmonary effusion; ascites, etc.). In addition, patients diagnosed with another primary malignancy within the past 5 years and patients who were unwilling to or unable to comply with the protocol were excluded.
Treatment design
Both imatinib and hydroxyurea were given orally on a continuous dosing schedule. Imatinib was administered at 400 mg daily to patients not on CYP 3A-enzyme inducing anti-epileptic drugs (EIAED) (phenytoin, carbamazepine, oxcarbazepine, phenobarbitol, primidone) (stratum A) while those on EIAED (stratum B) received 500 mg twice a day. Hydroxyurea was administered to all patients at 500 mg twice a day. Each cycle included 28 days of therapy. Patients remained on study unless they withdrew consent or developed either unacceptable toxicity or tumor progression.
Dose modification and retreatment
Toxicity was graded according to the NCI CTC version 2.0 (NCI 2004). Imatinib was reduced by 100 mg/day for patients not on EIAED and by 200 mg/day for patients on EIAED, for related grade ≥3 non-hematologic or grade 4 hematologic toxicities. Hydroxyurea was reduced by 25% for grade 4 hematologic toxicity that developed following imatinib dose modification. Re-treatment required adequate hematologic, hepatic and renal laboratory parameters (defined in eligibility criteria) and resolution of any related grade ≥3 toxicity to grade ≤1.
Study evaluations
Patients underwent physical examinations and MRI scans within 2 weeks of enrollment and before every other cycle of therapy. A weekly CBC and monthly biochemistry profile were also performed. Patients recorded their weight biweekly and notified study personnel if they gained ≥10% of baseline weight.
Response evaluation
Response determination, performed by study investigators, included neurologic examination and comparison of baseline contrast-enhanced magnetic resonance imaging (MRI) with the MRI performed before every other cycle. A complete response (CR) was defined as disappearance of all enhancing tumor from baseline on consecutive MRIs at least 6 weeks apart, combined with corticosteroid discontinuation and neurologic stability or improvement. A partial response (PR) was defined as ≥50% reduction from baseline in size (product of largest perpendicular diameters) of enhancing tumor with neurologic stability or improvement and stable or reduced corticosteroid requirement. Progressive disease (PD) was defined as more than 25% increase in size of enhancing tumor from baseline or any new lesion on MRI. Stable disease (SD) was defined as any assessment not meeting CR, PR, or PD criteria.
Statistical considerations
The primary goal was to evaluate the 6-month PFS rate among patients with recurrent WHO grade III MG treated with imatinib plus hydroxyurea. We employed a single-stage, phase II design to differentiate between a 20% and 40% 6-month PFS rate with type I and II error rates of 0.089 and 0.090 respectively.
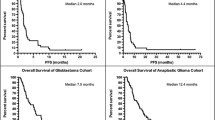
Time to progression (TTP) and overall survival (OS) were measured from treatment initiation and analyzed by the Kaplan-Meier (KM) method including 95% confidence intervals (CIs) [21]. Univariate logistic regression established whether covariates including age, KPS, EIAED use, number of prior progressions, and number of prior chemotherapy agents, was predictive of either PFS or OS. If the P-values was <0.25, then the characteristic was considered a possible multivariate Cox regression model covariate [22]. Relative risk was calculated for each variable with CIs.
Results
Patient characteristics
Thirty-nine patients with recurrent WHO grade III MG were enrolled at DUMC between March 2004 and January of 2005, including 32 patients with recurrent AA and 7 patients with recurrent AO. Twenty-one patients (54%) enrolled on stratum A and 18 (46%) on stratum B. Patient characteristics were comparable between both strata (Table 1).
All patients received prior external beam radiotherapy and chemotherapy that included at least temozolomide. Per patient, the mean number of prior treatment regimens (excluding surgery) was 3 (range, 1–8), and the median number of prior progressions was 2 (range, 1–7). The median time to study enrollment from original diagnosis was 137.6 weeks (range, 4.9–648 weeks).
Outcome
Thirty-seven patients were evaluable for survival. Two patients who discontinued therapy after less than 7 days (1 due to eligibility violation; 1 due to withdrawal of consent) were not included in the survival analysis. With a median follow-up of 82.9 weeks, the 6-month PFS rate for all patients, those on stratum A and those on stratum B were 24% (95% CI, 14–43%), 11% (95% CI, 3–39%) and 39% (95% CI, 22–69%), respectively (Table 2). The 12-month PFS rate for all patients, those on stratum A and those on stratum B were 14% (95% CI, 6–31%), 5% (95% CI, 1–36%) and 22% (95% CI, 9–53%), respectively. The median PFS for all patients, and for those on strata A and B were 10.9 weeks (95% CI, 8.1–15.9 weeks), 8.7 weeks (95% CI, 6.4–14.1 weeks) and 13.9 weeks (95% CI, 8.1–32.1 weeks) respectively (Fig. 1). Four patients (10%) remain on study in cycles 16, 17, 19 and 22 including three patients with AA and one patient with an AO. The median overall survival for all patients, those on stratum A and those on stratum B were 33.3 weeks (95% CI, 24.6-∞ weeks), 28.7 weeks (95% CI, 15.7-∞ weeks) and 67.9 weeks (95% CI, 24.6–∞ weeks), respectively. Given the small number of patients with histologic diagnosis of AO, a significant difference in outcome could not be identified between the two histologic subgroups. Specifically the 6-month PFS rate for patients with AO and AA were 29% and 23%, respectively; the 12-month PFS rate for AO and AA patients were 14% and 13%, respectively; and the median PFS was 8.0 weeks for patients with AO, compared to 10.9 weeks for those with AA.
Thirty-five patients were evaluable for radiographic response. Four patients were not evaluable due to violation of eligibility (n = 1), consent withdrawal (n = 1), and premature discontinuation of therapy (n = 2). The latter included one patient with grade 4 toxicity during cycle 1 and one patient with PD after only 9 days of therapy. Four patients achieved a partial response including one patient on stratum A and 3 patients on stratum B. No patient achieved a complete response. The overall response rate was 10%. Overall 13 patients (33%) achieved a best response of disease stabilization including 5 (24%) of stratum A and 8 (44%) of stratum B patients (Table 2). Therefore, a best radiographic response of either partial response or stable disease after at least two months of therapy was achieved in 43%. Among patients who achieved at least stable disease after 2 months of treatment, the median PFS was 26.9 weeks (95% CI, 14.1–61.3 weeks). The percentage of these patients remaining progression-free for six and twelve months was 53% (95% CI, 34–83%) and 29% (95% CI, 14–61%).
Prognostic implications
Although PFS, OS and the rate of radiographic disease control (PR or SD) were greater among stratum B patients compared to those on stratum A, none of these differences achieved statistical significance.
Analysis of prognostic factors was limited by small sample size. However, univariate analysis did not demonstrate age (>40 years vs <40 years), histology (AA vs AO) or KPS (≥90% vs <90%) to predict PFS. Although, statistical significance was not achieved, patients who received >1 prior chemotherapy trended toward poorer outcome compared to those who received only 1 prior chemotherapy (P = 0.07). Furthermore, a Cox regression model analysis revealed that patients who had >1 prior chemotherapy had a 3.3-fold greater risk of disease progression compared to patients who received only 1 prior chemotherapy (P = 0.04).
Toxicity
The most frequent grade 3–4 toxicities (Table 3) were hematologic. A total of 194 cycles of therapy were administered to study patients. Grade 3 and 4 neutropenia complicated 3% of courses. Grade 3 and 4 thrombocytopenia complicated 3% and <1% of courses, respectively. Non-hematologic grade 3 toxicities included thrombosis (n = 3), fatigue (n = 2) and pulmonary edema (n = 2). Single episodes of grade 3 edema, infection with normal absolute neutrophil count, hypokalemia, gastritis, vomiting and hyperglycemia were also noted. The only grade 4 non-hematologic toxicity observed in this study was an episode of infection that occurred in a patient with a normal neutrophil count. One death occurred on study and was attributed to intracranial hemorrhage at tumor progression.
Discussion
Therapeutic options for recurrent WHO grade III MG patients are limited. Furthermore, there is no established therapy for patients with progressive disease after conventional XRT and alkylator-based chemotherapy. In the current study, we report that the combination of imatinib mesylate plus hydroxyurea is well tolerated and associated with anti-tumor activity among some heavily pretreated patients with recurrent grade III MG patients after XRT and at least temozolomide chemotherapy.
Although the modest therapeutic benefit we report appears less than that described in two “benchmark” studies for this patient population, patients in the current study represented a greater challenge than those of these comparator studies due to heavier pretreatment. In the first benchmark, Yung reported that temozolomide achieved a radiographic response rate, median PFS and 6-month PFS rate of 35%, 21.6 weeks, and 46%, respectively, among 162 AA and AOA patients treated at first recurrence [23]. Although our outcomes are clearly inferior to those achieved by temozolomide, nearly all patients in the current study had two or more prior episodes of progression and all had failed prior temozolomide therapy. In the second benchmark, Wong reported that the radiographic response rate, median PFS and 6-month PFS rate achieved among 150 recurrent AA patients treated on 8 consecutive salvage regimens, were 14%, 13 weeks, and 31%, respectively [24]. Although neither our study nor that of Wong restricted patient eligibility based on degree of prior treatment, patients enrolled in our study were more heavily pretreated than those reported by Wong. Specifically, 89% of the patients on the current study received 2 or more prior chemotherapy agents, compared to only 25% of those treated by Wong. In fact, 23% of those reported by Wong had not received any prior chemotherapy. Furthermore, all patients on the current study had progressive disease after temozolomide chemotherapy. In contrast, although not specified in the manuscript, it is likely that few, if any, of the patients reported by Wong had failed prior temozolomide because temozolomide was not widely available during the Wong study period (1986–1995).
Hence, the modest anti-tumor activity reported in our study is encouraging given the substantial degree of pretreatment of our patient population. The study primary endpoint, 6-month PFS, was successfully achieved in that 9 of the 39 study patients (24%) remained progression-free at 6 months. In fact, a best radiographic response of either partial response or stable disease was achieved in 43% of patients. Furthermore, among patients who achieved disease control after the first 2 months of treatment, the duration of tumor control was particularly encouraging. Specifically, the median PFS in this subset of patients was 26.9 weeks, and 53% of these patients remained progression-free for up to 6 months, while 29% remained progression-free for at least a year. Furthermore, a subset of patients achieved particularly noteworthy tumor control including 3 patients with a diagnosis of AA who continue on therapy for 16, 17, and 19 months, and one patient with an AO who remains on treatment for 22 months.
The combination of imatinib mesylate plus hydroxyurea was recently reported to have activity in the treatment of patients with recurrent GBM in two separate studies. First, Dresemann reported a radiographic response rate of 20% and a 6-month PFS of 32% among 30 GBM patients treated with 400 mg of imatinib per day and 500 mg of hydroxyurea twice a day following tumor progression after radiotherapy and temozolomide chemotherapy [25]. In our formal phase 2 study, we observed a radiographic response rate of 9% and a 6-month PFS of 27% [16]. The fact that grade III MG patients reported in the current study had a comparable outcome relative to our GBM study is somewhat surprising because grade III MG patients typically respond more favorably to active regimens than grade IV MG patients [4–8, 24]. However, patients treated on the current study were more heavily pretreated than patients treated on our GBM study with imatinib plus hydroxyurea. Furthermore it is possible that some patients enrolled in the current study may have transformed to grade IV MG prior to enrollment. Such transformation, a frequent event among glial tumors at recurrence, would not have been appreciated in the current study because eligibility required only a prior diagnosis of grade III MG and did not mandate confirmation of grade III MG pathology at study enrollment.
Despite the degree of pretreatment of the current study population, our results, coupled with the previous reports of this regimen among recurrent GBM patients, confirm that imatinib mesylate plus hydroxyurea is well tolerated among MG patients. The most common toxicity was hematologic, and was limited to grade 3 events in the majority of cases. A recent report raised a concern of possible cardiomyopathy associated with imatinib therapy [26]. Although no direct evidence of cardiomyopathy was observed among patients in the current study, 2 patients developed pulmonary edema that responded to medical intervention and dose modification of the study regimen.
The results of the current study, as well as the prior GBM studies suggest that a subset of patients will respond to imatinib mesylate plus hydroxyurea therapy. One intriguing clinical factor associated with response to this regimen appears to be concurrent use of CYP3A-inducing anti-epileptic drugs (EIAEDs). Regression analyses of patients treated on our recently published GBM study demonstrated that patients on EIAEDs had a 59% lower risk of recurrence than those not on EIAEDs. This finding was paradoxical given that patients on EIAEDs had lower imatinib exposures, despite a 2.5-fold higher administered dose compared to patients not on EIAEDs [16]. Patients on EIAEDs in the current study also trended toward better outcomes than those not on EIAEDs, although the differences did not achieve statistical significance. Nonetheless, Cox regression analysis demonstrated that, after adjusting for prior chemotherapy exposure, patients on EIAEDs in the current study had a 49% lower risk of progression than patients not on EIAEDs. Mechanisms underlying an improved response to imatinib mesylate plus hydroxyurea for patients on EIAEDs are unclear. Nonetheless, future studies should further evaluate whether concurrent administration of EIAEDs is associated with improved response to imatinib plus hydroxyurea. In addition, another important challenge for ongoing preclinical studies and future clinical trials will be to identify biologic factors predictive of response to this regimen. Unfortunately, limited availability of primary tumor specimens precluded an analysis of potential biomarkers among patients treated on the current study. Nonetheless, evaluation of such biomarkers in future studies should be considered. Possible candidates for such evaluations include the level of PDGF receptor and c-KIT expression in tumor specimens of treated patients.
The anti-tumor activity and low toxicity of imatinib mesylate plus hydroxyurea observed in the current study and in 2 recently reported independent recurrent GBM trials, suggest that this regimen warrants further evaluation for MG patients. The observation that patients on EIAEDs appear more responsive than patients not on EIAEDs is intriguing and also warrants further investigation in future studies. Particularly attractive features of this regimen are its tolerability and durability of disease control among a subset of patients who achieve tumor control at initial evaluation. These features suggest that further evaluation of this regimen is warranted among patients at recurrence following conventional therapy.
Abbreviations
- AA:
-
anaplastic astrocytoma
- AO:
-
anaplastic oligodendroglioma
- AOA:
-
anaplastic oligoastrocytoma
- CBC:
-
complete blood count
- CI:
-
confidence interval
- CNS:
-
central nervous system
- CR:
-
complete response
- DLT:
-
dose-limiting toxicity
- EIAED:
-
enzyme inducing anti-epileptic drugs
- 18FDG PET [18F]:
-
fluorodeoxyglucose positron emission tomography
- FDA:
-
Food and Drug Administration
- GBM:
-
glioblastoma multiforme
- G-CSF:
-
granulocyte colony stimulating factor
- GS:
-
gliosarcoma
- IRB:
-
institutional review board
- ITT:
-
intent-to treat
- KM:
-
Kaplan-Meier
- KPS:
-
Karnofsky performance status
- MG:
-
malignant glioma
- MRI:
-
magnetic resonance imaging
- MTD:
-
maximum-tolerated dose
- OS:
-
overall survival
- PD:
-
progressive disease
- PFS:
-
progression-free survival
- PR:
-
partial response
- SD:
-
stable disease
- TTP:
-
time to progression
- XRT:
-
external beam radiotherapy
References
See SJ, Gilbert MR (2004) Anaplastic astrocytoma: diagnosis, prognosis, and management. Semin Oncol 31:618–634
Engelhard HH, Stelea A, Mundt A (2003) Oligodendroglioma and anaplastic oligodendroglioma: clinical features, treatment, and prognosis. Surg Neurol 60:443–456
Lonardi S, Tosoni A, Brandes AA (2005) Adjuvant chemotherapy in the treatment of high-grade gliomas. Cancer Treat Rev 31:79–89
Fine HA, Dear KB, Loeffler JS, Black PM, Canellos GP (1993) Meta-analysis of radiation therapy with and without adjuvant chemotherapy for malignant gliomas in adults. Cancer 71:2585–2597
Stewart LA (2002) Chemotherapy in adult high-grade glioma: a systematic review and meta-analysis of individual patient data from 12 randomised trials. Lancet 359:1011–1018
Levin VA, Wilson CB, Davis R, Wara WM, Pischer TL, Irwin L (1979) A phase III comparison of BCNU, hydroxyurea, and radiation therapy to BCNU and radiation therapy for treatment of primary malignant gliomas. J Neurosurg 51:526–532
Buckner JC, Schomberg PJ, McGinnis WL, Cascino TL, Scheithauer BW, O’Fallon JR, Morton RF, Kuross SA, Mailliard JA, Hatfield AK, Cole JT, Steen PD, Bernath AM (2001) A phase III study of radiation therapy plus carmustine with or without recombinant interferon-alpha in the treatment of patients with newly diagnosed high-grade glioma. Cancer 92:420–433
Prados MD, Larson DA, Lamborn K, McDermott MW, Sneed PK, Wara WM, Chang SM, Mack EE, Krouwer HG, Chandler KL, Warnick RE, Davis RL, Rabbitt JE, Malec M, Levin VA, Gutin PH, Phillips TL, Wilson CB (1998) Radiation therapy and hydroxyurea followed by the combination of 6-thioguanine and BCNU for the treatment of primary malignant brain tumors. Int J Radiat Oncol Biol Phys 40:57–63
Smith JS, Perry A, Borell TJ, Lee HK, O’Fallon J, Hosek SM, Kimmel D, Yates A, Burger PC, Scheithauer BW, Jenkins RB (2000) Alterations of chromosome arms 1p and 19q as predictors of survival in oligodendrogliomas, astrocytomas, and mixed oligoastrocytomas. J Clin Oncol 18:636–645
Ino Y, Zlatescu MC, Sasaki H, Macdonald DR, Stemmer-Rachamimov AO, Jhung S, Ramsay DA, von Deimling A, Louis DN, Cairncross JG (2000) Long survival and therapeutic responses in patients with histologically disparate high-grade gliomas demonstrating chromosome 1p loss. J Neurosurg 92:983–990
Ino Y, Betensky RA, Zlatescu MC, Sasaki H, Macdonald DR, Stemmer-Rachamimov AO, Ramsay DA, Cairncross JG, Louis DN (2001) Molecular subtypes of anaplastic oligodendroglioma: implications for patient management at diagnosis. Clin Cancer Res 7:839–845
Cairncross JG, Ueki K, Zlatescu MC, Lisle DK, Finkelstein DM, Hammond RR, Silver JS, Stark PC, Macdonald DR, Ino Y, Ramsay DA, Louis DN (1998) Specific genetic predictors of chemotherapeutic response and survival in patients with anaplastic oligodendrogliomas. J Natl Cancer Inst 90:1473–1479
Behin A, Hoang-Xuan K, Carpentier AF, Delattre JY (2003) Primary brain tumours in adults. Lancet 361:323–331
DeAngelis LM (2001) Brain tumors. N Engl J Med 344:114–123
Kleihues P, Cavenee WK (2000) Pathology and Genetics of Tumours of the Nervous System. International Agency for Research on Cancer (IARC), Lyon, France
Reardon DA, Egorin MJ, Quinn JA, Rich JN Sr, Gururangan I, Vredenburgh JJ, Desjardins A, Sathornsumetee S, Provenzale JM, Herndon JE, 2nd. Dowell JM, Badruddoja MA, McLendon RE, Lagattuta TF, Kicielinski KP, Dresemann G, Sampson JH, Friedman AH, Salvado AJ, Friedman HS (2005) Phase II study of imatinib mesylate plus hydroxyurea in adults with recurrent glioblastoma multiforme. J Clin Oncol 23:9359–9368
Wen PY, Yung WK, Lamborn K, Peng B, Dahia P, Abrey L, Raiser J, Cloughesy T, Fink K, Gilbert M, Chang SM, Junck L, Schiff D, Lieberman F, Fine H, Mehta M, Robins HI, DeAngelis LM, Hess K, Groves M, Puduvalli VK, Levin VA, Conrad C, Kuhn J, Maher E, Hayes M, Silberman S, Letvak L, Capdeville R, Kaplan R, Murgo A, Stiles CD, Prados MD: Phase I/II study of imatinib mesylate (ST1571) for patients with recurrent malignant gliomas (NABTC 99–08). In: Bigner DD (ed) Society for Neuro-oncology Ninth Annual Meeting, Toronto, Canada
Van Den Bent MJ, Brandes AA, van Oosterom A, Dittrich C, Fumoleau P, Coudert B, Twelves C, de Balincourt C, Lacombe D, Raymond E: Multicentre phase II study of imatinib mesylate (Gleevec) in patients with recurrent glioblastoma: an EORTC NDDG/BTG intergroup study. In: Bigner DD (ed) Society for Neuro-Oncology Ninth Annual Meeting, Toronto, Canada, p 383
Geyer JR, Zeltzer PM, Boyett JM, Rorke LB, Stanley P, Albright AL, Wisoff JH, Milstein JM, Allen JC, Finlay JL, et al. (1994) Survival of infants with primitive neuroectodermal tumors or malignant ependymomas of the CNS treated with eight drugs in 1 day: a report from the Childrens Cancer Group. J Clin Oncol 12:1607–1615
Levin VA (1992) The place of hydroxyurea in the treatment of primary brain tumors. Semin Oncol 19:34–39
Brookmeyer R, Crowley J (1982) A confidence interval for the median survival time. Biometrics 38:29–41
Cox DR (1972) Regression models and life-tables (with discussion). J Roy Stat Soc B 34:187–220
Yung WK, Prados MD, Yaya-Tur R, Rosenfeld SS, Brada M, Friedman HS, Albright R, Olson J, Chang SM, O’Neill AM, Friedman AH, Bruner J, Yue N, Dugan M, Zaknoen S, Levin VA (1999) Multicenter phase II trial of temozolomide in patients with anaplastic astrocytoma or anaplastic oligoastrocytoma at first relapse. Temodal brain tumour group. J Clin Oncol 17:2762–2771
Wong ET, Hess KR, Gleason MJ, Jaeckle KA, Kyritsis AP, Prados MD, Levin VA, Yung WK (1999) Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. J Clin Oncol 17:2572–2578
Dresemann G (2005) Imatinib and hydroxyurea in pretreated progressive glioblastoma multiforme: a patient series. Ann Oncol 16:1702–1708
Kerkela R, Grazette L, Yacobi R, Iliescu C, Patten R, Beahm C, Walters B, Shevtsov S, Pesant S, Clubb FJ, Rosenzweig A, Salomon RN, Van Etten RA, Alroy J, Durand JB, Force T (2006) Cardiotoxicity of the cancer therapeutic agent imatinib mesylate. Nat Med 12:908–916
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Desjardins, A., Quinn, J.A., Vredenburgh, J.J. et al. Phase II study of imatinib mesylate and hydroxyurea for recurrent grade III malignant gliomas. J Neurooncol 83, 53–60 (2007). https://doi.org/10.1007/s11060-006-9302-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-006-9302-2