Abstract
Oral cavity is inhabited by more than 25,000 different bacterial phylotypes; some of them cause systemic infections in addition to dental and periodontal diseases. Emergence of multiple antibiotic resistance among these bacteria necessitates the development of alternative antimicrobial agents that are safe, stable, and relatively economic. This review focuses on the significance of metal oxide nanoparticles, especially zinc oxide and titanium dioxide nanoparticles as supplementary antimicrobials for controlling oral infections and biofilm formation. Indeed, the ZnO NPs and TiO2 NPs have exhibited significant antimicrobial activity against oral bacteria at concentrations which is not toxic in in vivo toxicity assays. These nanoparticles are being produced at an industrial scale for use in a variety of commercial products including food products. Thus, the application of ZnO and TiO2 NPs as nanoantibiotics for the development of mouthwashes, dental pastes, and other oral hygiene materials is envisaged. It is also suggested that these NPs could serve as healthier, innocuous, and effective alternative for controlling both the dental biofilms and oral planktonic bacteria with lesser side effects and antibiotic resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The oral microbiome is a complex ecosystem consisting of about 25,000 different bacterial phylotypes as revealed by deep sequencing of human oral microbiome, traditional cultivation, and cloning approaches (Jenkinson et al. 2011; Keijser et al. 2008; Liu et al. 2012; Paster et al. 2006). The proliferation of pathogenic bacteria within the mouth gives rise to periodontitis, an inflammatory disease, which also constitutes a risk factor for other systemic diseases (Zbinden et al. 2012) such as endocarditis and colorectal cancer (Han and Wang 2013). Therefore, one of the most urgent and important biomedical challenges of our times is to clarify the role of microbial communities in human health (Belda-Ferre et al. 2011; Turnbaugh et al. 2007; Ximénez-Fyvie et al. 2000). Unfortunately, the antibiotic therapies have rendered these bacteria resistant to traditional antibiotics (Leistevuo et al. 2000; Sweeney et al. 2004). Therefore, it has been envisaged that the metal oxide nanoparticles with antimicrobial activity (nanoantibiotics) could offer a good alternative to abate and/or control the growth of bacteria in oral cavity (Allaker 2010). This review discusses briefly the impact of oral cavity bacteria on oral and other systemic diseases and emphasizes the role and mechanism of metal oxide nanoparticles, particularly ZnO NPs and TiO2 NPs in impeding the growth and biofilm formation activity of oral bacterial.
Oral bacteria: a health concern
Oral cavity is one of the most densely populated regions of human microbiome, where the heterogeneity of tissue types in the oral cavity, such as teeth, tongue, and mucosa, provides diverse ecological niches for the colonization of niche-specific microorganisms resulting in tongue coating, supragingival, and subgingival plaques (Fig. 1; Takahashi 2005; Kolenbrander and London 1993; Takahashi et al. 1997; Takahashi and Schachtele 1990). However, Streptococcus mutans and Porphyromonas gingivalis have received considerable attention due to their role in dental caries and periodontitis, respectively (Loesche 1986; Hayashi et al. 2010).
Dental caries, periodontal diseases, and microbes
Dental and periodontal diseases have multiple etiologies, but are largely caused by bacteria. Oral microbiome is one of the most extensively studied human microbiomes both for normal and diseased subjects (Nasidze et al. 2009; Wang et al. 2013a). Bacterial species belonging to 11 different phyla (Actinobacteria, Bacteroidetes, Chloroflexi, Firmicutes, Fusobacteria, Proteobacteria, Spirochetes, Synergistetes, Tenericutes, SR1, and TM7) inhabit the oral cavity (Aas et al. 2005; Dewhirst et al. 2010; Munson et al. 2004; Paster et al. 2001). High diversity of salivary microbiome within and between individuals has also been reported (Nasidze et al. 2009). Dental caries starts with the disturbance in the microbial homeostasis of the oral cavity and biofilm formation on the surface of the teeth. Bacteria initiate the biofilm formation by attaching firmly and irreversibly on dental surface and by evading the host defense system. Clarke identified S. mutans as one of the most important organisms causing dental caries, back in 1924. Lately, Socransky et al. (1998) have defined the red complex of bacteria (Treponema denticola, P. gingivalis, and Tannerella forsythia) associated with diseased site, and their collective ability to interfere with host defense mechanism. Among the primary colonizers that initiate the biofilm formation are S. oralis, S. mitis, S. sanguinis, S. parasanguinis, S. gordonii, Actinomyces, Veillonella, Gemella, Abiotrophia, Granulicatella, and Lactobacillus (Darveau 2010; Hojo et al. 2009; Komoria et al. 2012; Kolenbrander et al. 2010; Socransky et al. 1998). These primary colonizers produce various biomolecules to overcome the host defense system such as leucotoxins (Höglund et al. 2014), proteases like immunoglobulin A1 protease, IL-8 protease (Cole et al. 1994; Frandsen et al. 1986; Kolenbrander et al. 2002; Zinkernagel et al. 2008), and glycosidases (Bradshaw et al. 1994) in addition to the substances required for their binding on oral surfaces such as exopolysaccharides, environmental DNA, proteins, and lipoproteins. Once the first layer of colonizers is established, secondary colonizers start binding on the surface of these primary colonizers. Binding of secondary colonizers quickly and effectively on a preformed Streptococcus biofilm has been demonstrated by Skopek et al. (1993). Among secondary colonizers are P. gingivalis, P. intermedia, T. denticola, F. nucleatum, A. actinomycetemcomitans, and Lactobacillus (Fig. 2). The biofilm utilizes dietary sugars and continuously produces acids causing demineralization of enamel and bone loss.
Oral bacteria and systemic diseases
Oral infections, specifically periodontitis, influence the progression and pathogenesis of many systemic diseases, including the cardiovascular disease, bacterial pneumonia, diabetes mellitus, and low birth weight (Ali et al. 2011; Bascones-Martinez et al. 2011; Teles and Wang 2011; Li et al. 2000). A detailed list of oral bacteria associated with various systemic infections is given in Table 1. Oral infections affect the host’s susceptibility to systemic disease by causing transient bacteremia and metastatic injuries due to microbial toxins (Li et al. 2000). Lipopolysaccharides (LPS) from subgingival biofilms induce the vascular responses (Marcus and Hajjar 1993; Mattila 1989; Williams and Offenbacher 2000) and up-regulate the expression of endothelial cell adhesion molecules and secretion of interleukin-1 (IL-1), tumor necrosis factor alpha (TNF-α), and thromboxane. These mediators in circulation result in platelet aggregation and adhesion, formation of lipid-laden foam cells, deposits of cholesterol, preterm labor, and low birth weight infants (Herzberg and Meyer 1996; Han et al. 2010). F. nucleatum one of the predominant bacteria involved in adverse pregnancy outcomes has been isolated from fetal membranes, amniotic fluid, neonatal gastric aspirates, and fetal lung (Han et al. 2010; Han and Wang 2013). It has also been demonstrated that these F. nucleatum originated from mother’s subgingival plaque (Han et al. 2010; Han and Wang 2013). F. nucleatum has also been associated with a number of other systemic diseases (Table 1), and its pathogenicity can be attributed to its ability to adhere to cell surface through FadA adhesin. FadA binds to VE-cadherin receptors on the surface of endothelial cells increasing their permeability thus allowing the penetration of bacteria into the cells (Fardini et al. 2011). Following penetration into the cell, F. nucleatum stimulates TLR4-mediated inflammatory response. F. nucleatum also promotes colorectal cancer by recruiting tumor-infiltrating immune cells and creating a microenvironment conducive for colorectal neoplasia progression (Kostic et al. 2013).
Another important bacterium involved in a number of systemic diseases is P. gingivalis. This bacterium can actively adhere to and invade endothelial cells including human umbilical vein endothelial cells (Deshpande et al. 1998). Its mechanism of pathogenicity and involvement in cardiovascular disease and atherosclerosis has been comprehensively reviewed (Hayashi et al. 2010). P. gingivalis often induces a local chronic inflammatory response by modulating complement system resulting in oral inflammation and bone destruction. Toll-like receptors play an important role in the initiation of this inflammatory response. One of the unique characters of P. gingivalis through which it manifests its pathogenicity is peptidylarginine deiminase.
Resistance to antimicrobial agents among oral bacteria
Resistance to some antibiotics commonly prescribed for oral infections (Beta-lactams, macrolides, tetracyclines, lincosamides, and nitroimidazoles) is widespread among oral bacteria even among healthy children (Dar-Odeh et al. 2010; Ready et al. 2003; Sweeney et al. 2004). Leistevuo et al. (2000) reported resistance to cefuroxime, penicillin, and tetracycline in 839 strains of S. mutans. In another study, β-Lactamase-producing strains including Prevotella intermedia, P. denticola, and F. nucleatum were isolated from patients with dental caries (Fosse et al. 1999). Remarkably 80 % of the β-lactamase-producing F. nucleatum exhibited an MIC value as high as 8 mg/L (Nyfors et al. 2003). Greater resistance against the antibiotics clindamycin, metronidazole, and amoxicillin has been reported in P. gingivalis and A. actinomycetemcomitans associated with periodontal disease (Ardila et al. 2010). Significantly, higher incidence of resistance against spiramycin and metronidazole has been reported in periodontal A. actinomycetemcomitans strains (Madinier 1999). Even oral bacteria that are not directly involved in dental and/or periodontal diseases exhibit resistant to antimicrobial agents (Kouidhi et al. 2011; Villedieu et al. 2004). Rôças and Siqueira (2012) have reported a widespread distribution of antibiotic resistance genes in bacteria isolated from infected root canals. The most prevalent genes were β-lactamases bla TEM (17 %), followed by tetracycline tetW (10 %) and macrolide erythromycin ermC (10 %). The prevalence of tetQ (tetracycline), cepA(β-lactamase), and cblA(β-lactamase) genes has also been documented (Kirchner et al. 2013). Moreover, bacteria in oral biofilms are more resistant to antibiotics than in planktonic form (Mah and O’Toole 2001) due to the inability of antimicrobial agents to penetrate through the polymeric matrix secreted by the bacteria.
Nanoantibiotics: an alternative approach to combat antibiotic resistance
Pen (project on emerging nanotechnologies) project lists about 1824 commercial products including biomedicine that use nanomaterials (Berube et al. 2010). Plethora of biomedical applications has also been proposed for nanoparticles based on their unique physico-chemical properties. Their roles in hyperthermia treatment of cancer (Banobre-López et al. 2013), surgery (Ou et al. 2014), therapeutics (Zhang et al. 2008), biosensors (Luo et al. 2006), imaging (Drummen 2010), as drug carriers (De Jong and Borm 2008), and as anticancer (Cai et al. 2008) and antimicrobial agents (Marambio-Jones and Hoek 2010) are extensively reviewed. Nano-based drugs such as Emend, Rapamune, and Estrasorb are already approved by USFDA (Zhang et al. 2008) and are being marketed. One such nano-based product is nanoantibiotics. Nanomaterials that either exhibit antimicrobial activity per se or augment the efficacy and safe delivery of the antibiotics are called “nanoantibiotics” (Abeylath and Turos 2008; Huh and Kwon 2011; Kim et al. 2007). Nanoantibiotics offer significant benefits and advances in addressing the problems in treating infectious disease and hence are emerging as promising alternative antimicrobial agents. Some nanoparticles could be cost-effective (Li et al. 2008; Seyedmahmoudi et al. 2015), and are stable for long-term storage with a prolonged shelf-life (Weir et al. 2008). In addition, some NPs can withstand harsh conditions, such as high temperature sterilization, in comparison to conventional antibiotics (Applerot et al. 2012).
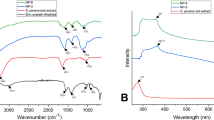
Mechanisms by which NPs exhibit their antimicrobial activity against bacteria include (i) disruption of bacterial cell membrane integrity (Xi and Bothun 2014), (ii) induction of oxidative stress by free radical formation (von Moos and Slaveykova 2014), (iii) mutagenesis (Ahmad et al. 2012), (iv) protein and DNA damage (Li et al. 2013), (v) inhibition of DNA replication by binding to DNA (Li et al. 2013), and (vi) respiratory chain disruption (Choi et al. 2008). Figure 3 depicts the plausible mechanisms by which metal or metal oxide NPs exhibit toxicity against bacteria and bacterial biofilm. The antimicrobial property of NPs largely arises and depends on their shape (Pal et al. 2007), size (Azam et al. 2012; Raghupathi et al. 2011), and the ability to form free biocidal metal ions (Song et al. 2010; Wang et al. 2010). Conversely, the sensitivity of bacteria to these NPs depends on their biochemical nature and composition, such as cell wall composition and growth rates. Baek and An (2011) reported that Gram-negative bacteria Escherichia coli are highly susceptible, whereas Gram-positive Staphylococcus aureus and Bacillus subtilis are less susceptible to CuO NPs, a trend that corresponds with our findings on silver nanoparticles (Khan et al. 2014a). It has also been demonstrated that the fast-growing bacteria are more susceptible than slow-growing bacteria to antibiotics and nanoparticles (Brown et al. 1988; Sheng and Liu 2011). Most likely, the tolerance of slow-growing bacteria is related to the expression of stress response genes (Stewart 2002).
Plausible mechanisms of NP-mediated antimicrobial and antibiofilm activities against oral bacteria. a Shows the inhibition of glucosyl transferase by NPs leading to the reduced exopolysaccharide production and biofilm formation. b Shows NP-mediated biochemical changes occurring at cellular level either in the planktonic cells or within the individual cells of the dental biofilm (e.g., ROS generation, DNA binding, enzyme inhibition). c Shows the changes taking place at the membranes of individual cells such as disruption of cell membrane, inhibition of cytochrome oxidase involved in the bacterial respiration
Several metals and metal oxides, carbon-based nanomaterials, and surfactant-based nanoemulsion have been reported to exhibit antibacterial activity (Huh and Kwon 2011; Li et al. 2008). However, the metallic NPs are regarded as promising candidates for overcoming bacterial resistance (Allaker 2010; Allaker and Memarzadeh 2014; Hajipour et al. 2012; Huh and Kwon 2011). Antimicrobial activity of NPs, including zinc oxide, silver, copper oxide, nickel, nickel oxide, tungsten trioxide, gold nanoparticles against oral bacteria, has been documented (Eshed et al. 2012; Espinosa-Cristóbal et al. 2012; Khan et al. 2013a, b; Lu et al. 2013), and is detailed in Table 2.
Metal oxide nanoparticles as potential antimicrobial agents with special reference to ZnO and TiO2 NPs
Among the different types of NPs tested for antimicrobial activity, the Ag NPs and CuO NPs have been shown to exhibit excellent antimicrobial potential (Bondarenko et al. 2013). However, their global production is much lower than that of ZnO and TiO2 NPs (Piccinno et al. 2012). ZnO NPs are the third largest produced NPs with a global annual production of ~550 tons per year (Piccinno et al. 2012, Keller et al. 2013). The production cost of ZnO NPs is also lesser than Ag NPs (Dastjerdi and Montazer 2010). Besides their use in cosmetics and paints (Piccinno et al. 2012), ZnO NPs are known for their excellent antimicrobial activity against pathogens (Allaker 2010; Allaker and Memarzadeh 2014; Jin et al. 2009; Liu et al. 2009). With regard to dental hygiene, ZnO NPs exhibited remarkable antimicrobial activity against a number of oral bacteria including S. mutans (Eshed et al. 2012), Streptococcus sobrinus (Aydin-Sevinç and Hanley 2010), P.intermedia, P. gingivalis, Fusobacterium nucleatum, Aggregatibacter actinomycetemcomitans (Vargas-Reus et al. 2012), Rothia dentocariosa, and Rothia mucilaginosa (Khan et al. 2014b). Both, the ZnO and TiO2 are comparatively less toxic to humans than CuO and Ag NPs (Bondarenko et al. 2013; Yu and Li 2011, Sect. 8.0). Therefore, ZnO NPs and TiO2 NPs are being utilized as drug carriers, in food packaging, cosmetics ingredients, and medical filling materials (Akbar and Kumar, 2014; Berube et al. 2010; Yu and Li 2011). Our earlier studies (Khan et al. 2013a, 2014b) suggest the possible application of ZnO NPs in oral pastes or mouth washes at concentration >100 µg/ml. Use of these nanoparticles in toothpastes is also reported by other authors (Yu and Li 2011; Vandebriel and De Jong 2012). ZnO NPs with an average size of 35 nm exhibit good antimicrobial activity against total oral bacteria at 70 µg/ml in vitro (Khan et al. 2013a; Fang et al. 2006). In addition to the desired antimicrobial and antibiofilm formation activities, ZnO NPs are also known to inhibit dentine demineralization (Takatsuka et al. 2005).
Several studies have suggested the inverse relationship between the size of NPs and their antimicrobial activity (Pal et al. 2007; Raghupathi et al. 2011; Lu et al. 2013; Adams et al. 2014). Khan et al. (2013a) demonstrated the IC50 value of 70.5 µg/ml with polygonal ZnO NPs (35 nm) against total oral bacteria. Aydin-Sevinç and Hanley (2010) reported the antimicrobial activity of 40–100 nm ZnO NPs against S. sobrinus with an MIC of 50 µg/ml against planktonic form of the bacteria. ZnO NPs with a size between 10 and 70 nm exhibited an MIC value of 250 µg/ml against P. gingivalis, F. nucleatum, A. actinomycetemcomitans, and an MIC value of 1.0 mg/ml against P. intermedia under anaerobic condition (Vargas-Reus et al. 2012). However, exposure to larger ZnO NPs with an average size of 125 nm has been shown to exhibit MIC/MBC value of 500 μg/ml against S. mutans (Hernández-Sierra et al. 2008), while still larger ZnO NPs (120–180 nm) do not inhibit the growth of S. mutans even up to a concentration of 1.0 mg/ml (Eshed et al. 2012). In addition to size, the shape of ZnO NPs also influences their antimicrobial activity. For instance, flower-shaped ZnO NPs with more sharp edges show higher antimicrobial activity against E. coli and S. aureus than relatively smoother rod- and sphere-shaped NPs (Talebiana et al. 2013). ZnO whiskers exhibited the MIC values of 78.1 and 312.5 µg/ml against A. viscosus and S. mutans, respectively (Fang et al. 2006).
One of the important factors that contributes in bacterial growth inhibition could be the release of zinc ions from ZnO NPs (Fukui et al. 2012). ZnO NPs also manifest their toxicity via generation of reactive oxygen species, such as hydrogen peroxide (Eshed et al. 2012). Leakage of intracellular content, cell wall, and membrane disruption by ZnO NPs in E. coli has been demonstrated using scanning electron microscopy and transmission electron microscopy (Liu et al. 2009). Also, the change in expression levels of genes involved in pathogenesis, oxidative stress responses, toxin production, and motility following exposure to ZnO NPs in Campylobacter jejuni has been studied (Xie et al. 2011). The expression of general stress response gene (dnaK) and oxidative stress genes (ahpC and katA) is reported to increase by 17-, 7-, and 52-fold, respectively, following the exposure to ZnO NPs, clearly demonstrating that ZnO NPs induced oxidative stress in bacteria. Cellular uptake of ZnO NPs in E. coli resulted in glutathione depletion and DNA damage (Kumar et al. 2011). However, most of these studies report only the MIC or IC50 values and the detailed studies of the possible interference of NPs with microbial processes resulting in their antimicrobial activities are lacking.
TiO2 NPs are one of the most abundant NPs produced globally with some studies estimating a global production of 3000 tons per year (Piccinno et al. 2012; Keller et al. 2013). TiO2 NPs are being extensively used even in food products; according to some findings, a typical US adult is already exposed to 1 mg/kg body weight per day of titanium, as it is used in a number of food products including chewing gums, candies and sweets with a code E171 (Weir et al. 2012). TiO2 NPs demonstrate significant antimicrobial activity against a number of microorganisms including E. coli, S. aureus, P. aeruginosa, E. faecium, B. subtilis, and Klebsiella pneumonia (Rajakumar et al. 2012; Kühn et al. 2003). The MIC value of the TiO2 NPs (62–74 nm) against these bacteria has been reported to be in the range of 40–80 µg/ml. However, the TiO2 NPs with an average size of 21 nm exhibit an MIC value of 1 mg/ml against S. sobrinus (Saito et al. 1992). Konishi (1987) demonstrated the growth inhibition of oral bacteria including S. mutans HS-6 and A. viscosus ATCC 19246 by TiO2 NPs at a concentration of 0.1 % (w/v). In another study, the mean MIC value of TiO2 NPs against important oral biofilm-forming bacteria P. intermedia, P. gingivalis, F. nucleatum, and A. actinomycetemcomitans was found to be 1187.5 µg/ml (Vargas-Reus et al. 2012). The plausible mechanism of action of TiO2 NPs against the bacteria could be ROS generation, DNA damage after internalization, peroxidation of membrane phospholipids, and inhibition of respiration (Kumar et al. 2011; Tsuang et al. 2008). Photoactivation of TiO2 NPs also remarkably increased its antimicrobial activity against Bacteroides fragilis, E. coli, E. hire, P. aeruginosa, S. typhimurium, and S. aureus (Maness et al. 1999).
Nanoantibiotics and their antibiofilm activity with focus on ZnO and TiO2
Biofilms are complex microbial communities adhered to solid surfaces by the secretion of extracellular matrix (containing extracellular polysaccharide, proteins, pili, flagella, adhesive fibers, and extracellular DNA), which cocoons the bacterial cell community. Bacteria in biofilms behave differently from their planktonic forms, forming complex 3D macroscopic structures containing channels and pores thus acting like multicellular organisms (Davey and O’Toole 2000; Costerton et al. 1995). These 3D, multicellular structures formed by pathogenic bacteria act as a protective shield against toxicants and antibiotics resulting in the development of chronic and recurring infections. Such biofilms exhibit significantly greater resistance to toxicants and antibiotic than the planktonic cells (Gilbert et al. 1997; Mah et al. 2003). Therefore, a good antibiofilm agent should have the ability to effectively penetrate through the biofilm in addition to possessing significant antimicrobial activity. In case of oral biofilms, an effective antiplaque agent should penetrate through the plaque and should reach enamel. Metal oxide NPs are emerging as propitious antimicrobial agents as discussed above. However, a few studies have demonstrated the antibiofilm activity of these nanoparticles and the molecular mechanism underlying their antibiofilm activity remains largely unexplained. Fabrega et al. (2011) demonstrated the inhibition of marine biofilm by Ag NPs, and reported a concentration-dependent reduction in biofilm formation. Although the mechanism of antibiofilm activity is not known, an important role of electrostatic attractions has been suggested. Positive charge of silver ions facilitates electrostatic attraction between the metal and the negatively charged bacterial membrane, augmenting uptake and antimicrobial activity (Kim et al. 2007). Ag+ ions are known to inhibit DNA replication, expression of ribosomal subunit proteins, enzymes necessary for ATP production (Yamanaka et al. 2005), and membrane-bound respiratory enzymes (Bragg and Rainnie 1974). Antibiofilm activity of nitric oxide (NO)-releasing silica nanoparticles on the biofilms formed by P. aeruginosa, E. coli, S. aureus, and S. epidermidis has also been reported (Hetrick et al. 2009). The NO was shown to rapidly diffuse through the biofilms providing enhanced penetration resulting in the death of over 99 % cells from each type of biofilm. In a related study, considerable capability of magnetic NPs to penetrate into biofilms, using external magnetic fields, has been demonstrated (Park et al. 2011). ZnO NPs and CuO NPs when tested for the prevention of biofilm formation activity by a mixed oral bacterial population on artificial dental surfaces and on the surface of polystyrene plates show significant antibiofilm activity at concentrations lesser than 100 µg/ml (Khan et al. 2013a). A new class of multimodal NPs comprising a magnetic core and a silver ring with a ligand gap was engineered for the eradication of biofilm (Mahmoudi and Serpooshan 2012). These nanoparticles exhibited high antibacterial and antibiofilm activity and thus their use in theranosis has been proposed (Mahmoudi and Serpooshan 2012). Several studies on the coating of various surfaces such as glass, polyacrylic teeth, and catheters with nanoparticles with an aim to prevent and/or minimize the biofilm formation have been reported. Eshed et al. (2012) demonstrated 85 % reduction in biofilm formation activity of S. mutans on the surface of artificial teeth coated with ZnO NPs, as compared to control uncoated teeth. Coating of ZnO NPs on glass surfaces produces reactive oxygen species (ROS), which interferes with the E. coli and S. aureus biofilm formation (Applerot et al. 2012). ZnO NPs also show marked inhibition of biofilm formation and hemolytic activity of P. aeruginosa, besides inhibition of pyocyanin, Pseudomonas quinolone signal (PQS), and pyochelin production. Transcriptome analyses of ZnO NPs exposed P. aeruginosa showed that ZnO nanoparticles induce the zinc cation efflux pump czc operon and several important transcriptional regulators including porin gene opdT and type III repressor ptrA (Lee et al. 2014). Comparative analysis of the inhibitory effect of Ni NPs (41 nm) and NiO NPs (35 nm) on biofilm formation activity of mixed oral bacteria revealed greater effect of Ni NPs compared to NiO NPs (Khan et al. 2013b). Engineered TiO2 NPs impede the biofilm formation by Shewanella oneidensis (Maurer-Jones et al. 2013). However, another study shows that the coating of surface by TiO2 does not affect the biofilm formation activity of two early colonizers of the oral cavity, namely S. sanguinis and A. naeslundii (Fröjd et al. 2011). Chun et al. (2007) demonstrated the bactericidal effect of TiO2 NP-coated orthodontic wires on S. mutans and P. gingivalis, besides significant prevention of bacterial biomass deposition on their surface. Suketa et al. (2005) have suggested the photobactericidal effect of TiO2 NPs layered metallic titanium on A. actinomycetemcomitans and F. nucleatum, with significant decrease in the viability of bacteria under UVA illumination within 120 min.
Hybrid nanocomposites and their antimicrobial activity
One of the most noticeable contributions of nanotechnology to oral hygiene and health is the nanoparticle-based dental materials with improved antimicrobial properties such as nanofillers, nanocomposites, and nanoparticle-based polymers (Cheng et al. 2012; Dwivedi et al. 2013; Hule and Pochan 2007). Development of such antimicrobial dental materials is a challenge as the addition of antimicrobial agents to these materials may adversely affect their physico-chemical properties including hardness and mechanical strength (Hanemann and Szabó 2010). On the contrary, nanoparticle-based dental materials offer esthetic and strength advantages over conventional micro-filled and hybrid resin-based composite (RBC) systems besides possessing strong antimicrobial activity and remineralizing capabilities (Saunders 2009). These materials are also advantageous in terms of smoothness, polishability and precision of shade characterization, flexural strength, and micro-hardness, as compared to resin-based composites (Saunders 2009; Cheng et al. 2012).
Tavassoli-Hojati et al. (2013) developed resin composites containing various concentrations of ZnO NPs (0–5 wt%) and evaluated their physico-chemical properties and antimicrobial activity against S. mutans. The antimicrobial activity of resins increased with the concentration of ZnO NPs incorporated without any change in the flexural strength and compressive modulus. On the contrary, compressive strength and flexural modulus of the resins improved significantly. Aydin-Sevinç and Hanley (2010) have also reported the synthesis of resins with different concentrations of ZnO NPs and suggested that ZnO NPs at a concentration of 10 % in these resins effectively inhibit the biofilm formation by S. sobrinus. The composite resins also showed significant inhibitory activity against the biofilm formed by S. oralis, S. gordonii, and A. naeslundii under anaerobic conditions (Aydin-Sevinç and Hanley 2010).
Incorporation of silver nanoparticles at a concentration of <1 % (w/v) in orthodontic bracket-bonding cement is reported to prevent the attachment and growth of the cariogenic bacterium S. mutans, without altering the physical properties of the cement (Allaker and Memarzadeh 2014). Similarly, silver complexes of poly(amidoamine) (PAMAM) dendrimers and silver-PAMAM dendrimer nanocomposite solutions have displayed considerable antimicrobial activity against S. aureus, P. aeruginosa, and E. coli (Balogh et al. 2001).
Nanotoxicology perspective
Indeed, there is a multitude of challenges in translating nanotechnology and nanoantibiotics, in particular, for clinical use. Toxicity of these NPs needs a careful and balanced evaluation before successful clinical translations. Key factors determining the toxicity of NPs include nature and extent of interactions of NPs with cells, tissues, and organs, and their proper routes of administration for desired therapeutic effects (Sandhiya et al. 2009; Suri et al. 2007). As the use of ZnO NPs and TiO2 NPs in toothpastes and mouthwashes is proposed, the possibility of their ingestion warrants the evaluation of their toxicity on intestinal epithelial cells both in vivo and in vitro. Exposure of RKO and Caco-2 human colon carcinoma cells to ZnO NPs with a size of 8–10 nm has been shown to yield changes in chaperonin proteins, metal metabolism, and protein-folding genes but did not show a pro-inflammatory signature (Moos et al. 2011). It has also been demonstrated in the same study that ZnO NPs (8–10 nm) and TiO2 NPs (5 nm) both show minimal toxicity below 100 μg/cm2. Exposure of the LoVo human colon carcinoma cell line to 11.5 µg/ml of ZnO NPs (50–70 nm) for 24 h resulted in decreased viability, increased \({\text{H}}_{ 2} {\text{O}}_{ 2} /{\text{OH}}^{ \cdot }\), decreased O2 −, and glutathione depolarization of the inner mitochondrial membrane, apoptosis, and IL-8 release (De Berardis et al. 2010). Musarrat et al. (2009) also suggested the genotoxic potential of ZnO NPs (19.82 nm) at a higher concentration range of 100–400 μg/ml and their ability to perturb the mitochondrial membrane potential, possibly through oxidative mechanism on human lymphocytes. Bondarenko et al. (2013) in their review have compared the toxicity of 3 different NPs, namely Ag, CuO, and ZnO NPs. Based on 25 different in vitro studies on human cell lines, the median LE/LC50 value of ZnO NPs has been calculated to be 43 µg/ml, which is 4 times higher than that of silver (11.3 µg/ml), a well-known metal used in dentistry (Peng et al. 2012), which clearly shows that ZnO is safer than Ag NPs. Vandebriel and De Jong (2012) in their review of mammalian toxicity of ZnO NPs have concluded that genotoxicity of ZnO NPs was only observed in in vitro and not in vivo studies and the toxicity in in vitro assays was largely due to the oxidative stress. Warheit et al. (2007) investigated in vivo and in vitro toxicity of ultrafine TiO2 (140 nm) and concluded that this form of oxide exhibited low hazard potential in aquatic and mammalian species/cell lines following acute exposure. In another in vivo study on terrestrial isopods Valant et al. (2012) found that ingestion of TiO2 nanoparticles exhibits toxic effects only at a high concentration of 1000–2000 µg/g of feed.
Thus, the proposed application of ZnO NPs and TiO2 NPs in toothpastes and mouthwashes, as supplementary antibacterial agents, may not exert the acute adverse effects to human cells, due to short exposure time and at proposed non-toxic doses (>100 µg/ml). Nevertheless, it remains crucial to determine the actual doses of the nano-based formulations, to which the oral cavity is exposed, and possibly reach the gastrointestinal tract by accidental ingestion, and to assess the in vivo toxicity of these doses.
Conclusion
The increasing evidence of the involvement of oral bacteria in a number of systemic diseases and the development of antibiotic resistance among oral bacteria is a matter of serious concern. Metal oxide nanoparticles especially ZnO and TiO2 NPs exhibit good antimicrobial activity against the oral bacteria, and therefore offer a good alternative for traditional antibiotics. However, their applications in oral hygiene are still in infancy. Therefore, systematic and mechanistic studies are required to understand the impact of these NPs in combating the oral infections and biofilm formation.
References
Aas JA, Paster BJ, Stokes LN, Olsen I, Dewhirst FE (2005) Defining the normal bacterial flora of the oral cavity. J Clin Microbiol 43:5721–5732
Abeylath SC, Turos E (2008) Drug delivery approaches to overcome bacterial resistance to β-lactam antibiotics. Expert Opin Drug Deliv 5:931–949
Adams PC, Walker KA, Obare SO, Docherty KM (2014) Size-dependent antimicrobial effects of novel palladium nanoparticles. PLoS ONE 9(1):e85981
Ahmad J, Dwivedi S, Alarifia S, Al-Khedhairy AA, Musarrat J (2012) Use of β-galactosidase (lacZ) gene α-complementation as a novel approach for assessment of titanium oxide nanoparticles induced mutagenesis. Mutat Res 747:246–252
Ahn J, Chen CY, Hayes RB (2012) Oral microbiome an oral and gastrointestinal cancer risk. Cancer Cause Control 23:399–404
Akbar A, Kumar A (2014) Zinc oxide nanoparticles loaded active packaging, a challenge study against Salmonella typhimurium and Staphylococcus aureus in ready-to-eat poultry meat. Food Control 38:88–95
Ali J, Pramod K, Tahir MA, Ansari SH (2011) Autoimmune responses in periodontal diseases. Autoimmun Rev 10:426–431
Allaker RP (2010) The use of nanoparticles to control oral biofilm formation. J Dent Res 89:1175–1186
Allaker RP, Memarzadeh K (2014) Nanoparticles and the control of oral infections. Int J Antimicrob Agents 43:95–104
Applerot G, Lellouche J, Perkas N, Nitzan Y, Gedanken A, Banin E (2012) ZnO nanoparticle-coated surfaces inhibit bacterial biofilm formation and increase antibiotic susceptibility. RSC Adv 2:2314–2321
Ardila CM, López MA, Guzmán IC (2010) High resistance against clindamycin, metronidazole and amoxicillin in Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans isolates of periodontal disease. Med Oral Patol Oral Cir Bucal 15:e947–e951
Aydin-Sevinç AB, Hanley L (2010) Antibacterial activity of dental composites containing zinc oxide nanoparticles. J Biomed Mater Res B 94:22–31
Azam A, Ahmed SA, Oves M, Khan MS, Memic A (2012) Size-dependent antimicrobial properties of CuO nanoparticles against Gram-positive and -negative bacterial strains. Int J Nanomed 7:3527–3535
Baek YW, An YJ (2011) Microbial toxicity of metal oxide nanoparticles (CuO, NiO, ZnO, and Sb2O3) to Escherichia coli, Bacillus subtilis, and Streptococcus aureus. Sci Total Environ 409:1603–1608
Balogh L, Swanson DR, Tomalia DA, Hagnauer GL, McManus AT (2001) Dendrimer-silver complexes and nanocomposites as antimicrobial agents. Nano Lett 1:18–21
Bañobre-López M, Teijeiro A, Rivas J (2013) Magnetic nanoparticle-based hyperthermia for cancer treatment. Rep Pract Oncol Radiother 18:397–400
Bascones-Martinez A, Matesanz-Perez P, Escribano-Bermejo M et al (2011) Periodontal disease and diabetes-review of the literature. Med Oral Patol Oral Cir Bucal 16:e722–e729
Belda-Ferre P, Alcaraz LD, Cabrera-Rubio R et al (2011) The oral metagenome in health and disease. ISME J 6:46–56
Berube DM, Searson EM, Morton TS, Cummings CL (2010) Project on emerging nanotechnologies—consumer product inventory evaluated. Nanotechnol Law Bus 7:152–163
Bondarenko O, Juganson K, Ivask A, Kasemets K, Mortimer M, Kahru A (2013) Toxicity of Ag, CuO and ZnO nanoparticles to selected environmentally relevant test organisms and mammalian cells in vitro: a critical review. Arch Toxicol 87:1181–1200
Bradshaw DJ, Homer KA, Marsh PD, Beighton D (1994) Metabolic cooperation in oral microbial communities during growth on mucin. Microbiol 140:3407–3412
Bragg PD, Rainnie DJ (1974) The effect of silver ions on the respiratory chain of Escherichia coli. Can J Microbiol 20:883–889
Brown MR, Allison DG, Gilbert P (1988) Resistance of bacterial biofilms to antibiotics: a growth-rate related effect? J Antimicrob Chemother 22:777–780
Byrne GI, Kalayoglu MV (1999) Chlamydia pneumoniae and atherosclerosis: links to the disease process. Am Heart J 138:S488–S490
Cai W, Gao T, Hong H, Sun J (2008) Applications of gold nanoparticles in cancer nanotechnology. Nanotechnol Sci Appl. doi:10.2147/NSA.S3788
Castellarin M, Warren RL, Freeman JD et al (2012) Fusobacterium nucleatum infection is prevalent in human colorectal carcinoma. Genome Res 22:299–306
Cheng L, Weir MD, Xu HH et al (2012) Effect of amorphous calcium phosphate and silver nanocomposites on dental plaque microcosm biofilms. J Biomed Mater Res B 100:1378–1386
Choi O, Deng KK, Kim NJ et al (2008) The inhibitory effects of silver nanoparticles, silver ions, and silver chloride colloids on microbial growth. Water Res 42:3066–3074
Chun MJ, Shim E, Kho EH et al (2007) Surface modification of orthodontic wires with photocatalytic titanium oxide for its antiadherent and antibacterial properties. Angle Orthod 77:483–488
Clarke JK (1924) On the bacterial factor in the etiology of dental caries. Br J Exp Pathol 5:141–147
Cole MF, Evans M, Fitzsimmons S et al (1994) Pioneer oral Streptococci produce immunoglobulin A1 protease. Infect Immun 62:2165–2168
Costerton JW, Lewandowski Z, Caldwell DE et al (1995) Microbial biofilms. Annu Rev Microbiol 49:711–745
Dar-Odeh NS, Abu-Hammad OA, Al-Omiri MK, Khraisat AS, Shehabi AA (2010) Antibiotic prescribing practices by dentists: a review. Ther Clin Risk Manag 6:301–306
Darveau PR (2010) Periodontitis: a polymicrobial disruption of host homeostasis. Nat Rev Microbiol 8:481–490
Dastjerdi R, Montazer M (2010) A review on the application of inorganic nanostructured materials in the modification of textile: focus on antimicrobial properties. Colloids Surf B 79:5–18
Davey ME, O’Toole GA (2000) Microbial biofilms: from ecology to molecular genetics. Microbiol Mol Biol Rev 64:847–867
De Berardis B, Civitelli G, Condello M et al (2010) Exposure to ZnO nanoparticles induces oxidative stress and cytotoxicity in human colon carcinoma cells. Toxicol Appl Pharmacol 246:116–127
De Jong WH, Borm PJA (2008) Drug delivery and nanoparticles: applications and hazards. Int J Nanomedicine 3:133–149
Deshpande RG, Khan MB, Genco CA (1998) Invasion of aortic and heart endothelial cells by Porphyromonas gingivalis. Infect Immun 66:5337–5343
Dewhirst FE, Chen T, Izard J et al (2010) The human oral microbiome. J Bacteriol 192:5002–5017
Dietrich T, Sharma P, Walter C et al (2013) The epidemiological evidence behind the association between periodontitis and incident atherosclerotic cardiovascular disease. J Periodontol 84:S70–S84
Drummen GPC (2010) Quantum dots—from synthesis to applications in biomedicine and life sciences. Int J Mol Sci 11:154–163
Dwivedi P, Narvi SS, Tewari RP (2013) Application of polymer nanocomposites in the nanomedicine landscape: envisaging strategies to combat implant associated infections. J Appl Biomater Funct Mater 11:129–142
Eshed M, Lellouche J, Matalon S et al (2012) Sonochemical coatings of ZnO and CuO nanoparticles inhibit Streptococcus mutans biofilm formation on teeth model. Langmuir 28:12288–12295
Espinosa-Cristóbal FA, Martínez-Castañóna GA, Téllez-Déctorb EJ et al (2012) Adherence inhibition of Streptococcus mutans on dental enamel surface using silver nanoparticles. Mater Sci Eng C 33:2197–2202
Fabrega J, Zhang R, Renshaw JC, Liu WT, Lead JR (2011) Impact of silver nanoparticles on natural marine biofilm bacteria. Chemosphere 85:961–966
Fang M, Chen JH, Xu XL, Yang PH, Hildebr HF (2006) Antibacterial activities of inorganic agents on six bacteria associated with oral infections by two susceptibility tests. Int J Antimicrob Agents 27:513–517
Fardini Y, Wang X, Temoin S et al (2011) Fusobacterium nucleatum adhesin FadA binds vascular endothelial cadherin and alters endothelial integrity. Mol Microbiol 82:1468–1480
Fosse T, Madinier I, Hitzig C, Charbit Y (1999) Prevalence of beta-lactamase-producing strains among 149 anaerobic Gram-negative rods isolated from periodontal pockets. Oral Microbiol Immunol 14:352–357
Frandsen EV, Theilade E, Ellegaard B, Kilian M (1986) Proportions and identity of IgA1-degrading bacteria in periodontal pockets from patients with juvenile and rapidly progressive periodontitis. J Periodontal Res 21:613–623
Fröjd V, Linderbäck P, Wennerberg A, Chávez de Paz L, Svensäter G, Davies JR (2011) Effect of nanoporous TiO2 coating and anodized Ca2+ modification of titanium surfaces on early microbial biofilm formation. BMC Oral Health 11:8
Fukui H, Horie M, Endoh S et al (2012) Association of zinc ion release and oxidative stress induced by intratracheal instillation of ZnO nanoparticles to rat lung. Chem Biol Interact 198:29–37
Gilbert P, Das J, Foley I (1997) Biofilm susceptibility to antimicrobials. Adv Dent Res 11:160–167
Hajipour MJ, Fromm KM, Ashkarran AA et al (2012) Antibacterial properties of nanoparticles. Trends Biotechnol 30:499–511
Han YW, Wang X (2013) Mobile microbiome: oral bacteria in extra-oral infections and inflammation. J Dent Res 92:485–491
Han YW, Fardini Y, Chen C et al (2010) Term stillbirth caused by oral Fusobacterium nucleatum. Obstet Gynecol 115:442–445
Hanemann T, Szabó DV (2010) Polymer-nanoparticle composites: from synthesis to modern applications. Materials 3:3468–3517
Hayashi C, Gudino CV, Gibson FCIII, Genco CA (2010) Review: pathogen-induced inflammation at sites distant from oral infection: bacterial persistence and induction of cell-specific innate immune inflammatory pathways. Mol Oral Microbiol 25:305–316
Hernández-Sierra JF, Ruiz F, Pena DC et al (2008) The antimicrobial sensitivity of Streptococcus mutans to nanoparticles of silver, zinc oxide, and gold. Nanomedicine 4:237–240
Herzberg MC, Meyer MW (1996) Effects of oral flora on platelets: possible consequences in cardiovascular disease. J Periodontol 67:1138–1142
Hetrick EM, Shin JH, Paul SH, Schoenfisch MH (2009) Anti-biofilm efficacy of nitric oxide-releasing silica nanoparticles. Biomaterials 30:2782–2789
Höglund ÅC, Haubek D, Kwamin F, Johansson A, Claesson R (2014) Leukotoxic activity of Aggregatibacter actinomycetemcomitans and periodontal attachment loss. PLoS One 9(8):e104095
Hojo K, Nagaoka S, Ohshima T, Maeda N (2009) Bacterial interactions in dental biofilm development. J Dent Res 88:982–990
Huh AJ, Kwon YJ (2011) “Nanoantibiotics”: a new paradigm for treating infectious diseases using nanomaterials in the antibiotics resistant era. J Controlled Release 156:128–145
Hule RA, Pochan DJ (2007) Polymer nanocomposites for biomedical applications. MRS Bull 32:354–358
Ismail Y, Mahendran V, Octavia S et al (2012) Investigation of the enteric pathogenic potential of oral Campylobacter concisus strains isolated from patients with inflammatory bowel disease. PLoS ONE 7:e38217
Jenkinson HF (2011) Beyond the oral microbiome. Environ Microbiol 13:3077–3087
Jin T, Sun D, Su JY, Zhang H (2009) Antimicrobial efficacy of zinc oxide quantum dots against Listeria monocytogenes, Salmonella enteritidis and E. coli O157:H7. J Food Sci 74:46–52
Kamer AR, Dasanayake AP, Craig RG, Glodzik-Sobanska L, Bry M, de Leon MJ (2008) Alzheimer’s disease and peripheral infections: the possible contribution from periodontal infections, model and hypothesis. J Alzheimers Dis 13:437–449
Keijser BJF, Zaura E, Huse SM et al (2008) Pyrosequencing analysis of the Oral microflora of healthy adults. J Dent Res 87:1016–1020
Keller AA, McFerran S, Lazareva A, Suh S (2013) Global life cycle releases of engineered nanomaterials. J Nanopart Res 15:1692
Khan ST, Ahmad M, Al-Khedhairy AA, Musarrat J (2013a) Biocidal effect of copper and zinc oxide nanoparticles on human oral microbiome and biofilm formation. Mater Lett 97:67–70
Khan ST, Ahamed M, Alhadlaq HA, Musarrat J, Al-Khedhairy AA (2013b) Comparative effectiveness of NiCl2, Ni- and NiO-NPs in controlling oral bacterial growth and biofilm formation on oral surfaces. Arch Oral Biol 58:1804–1811
Khan M, Khan ST, Khan M et al (2014a) Antibacterial properties of silver nanoparticles synthesized using Pulicaria glutinosa plant extract as a green bioreductant. Int J Nanomed 9:3551–3565
Khan ST, Ahamed M, Musarrat J, Al-Khedhairy AA (2014b) Antibiofilm and antibacterial activities of zinc oxide nanoparticles against the oral opportunistic pathogens Rothia dentocariosa (Ora-7) and Rothia mucilaginosa (Ora-16) isolates. Eur J Oral Sci 122:397–403
Kim JS, Kuk E, Yu KN et al (2007) Antimicrobial effects of silver nanoparticles. Nanomedicine 3:95–101
Kirchner M, Mafura M, Hunt T, Card R, Anjum MF (2013) Antibiotic resistance gene profiling of faecal and oral anaerobes collected during an antibiotic challenge trial. Anaerobe 23:20–22
Kolenbrander PE, London J (1993) Adhere today, here tomorrow: oral bacterial adherence. J Bacteriol 175:3247–3252
Kolenbrander PE, Andersen RN, Blehert DS, Egland PG, Foster JS, Palmer RJ Jr (2002) Communication among oral bacteria. Microbiol Mol Biol Rev 66:486–505
Kolenbrander PE, Palmer RJ, Periasamy S, Jakubovics NS (2010) Oral multispecies biofilm development and the key role of cell–cell distance. Nat Rev Microbiol 8:473–480
Komoria R, Sato T, Yamamotoa T, Takahashi N (2012) Microbial composition of dental plaque microflora on first molars with orthodontic bands and brackets, and the acidogenic potential of these bacteria. J Ora Biosci 54:107–112
Konishi K (1987) Antibacterial effect of the powdered semiconductor titanium oxide on the viability of oral microorganisms. Shika Igaku 50:119–125
Koren O, Spor A, Felin J et al (2011) Human oral, gut, and plaque microbiota in patients with atherosclerosis. PNAS 108:4592–4598
Kostic AD, Chun E, Robertson L et al (2013) Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell Host Microbe 14:207–215
Kouidhi B, Zmantar T, Mahdouani K, Hentati H, Bakhrouf A (2011) Antibiotic resistance and adhesion properties of oral Enterococci associated to dental caries. BMC Microbiol 11:155
Kühn KP, Cahberny IF, Massholder K et al (2003) Disinfection of surfaces by photocatalytic oxidation with titanium dioxide and UVA light. Chemosphere 53:71–77
Kumar A, Pandey AK, Singh SS, Shanker R, Dhawan A (2011) Engineered ZnO and TiO2 nanoparticles induce oxidative stress and DNA damage leading to reduced viability of Escherichia coli. Free Radic Biol Med 51:1872–1881
Lee HR, Jun HK, Kim HD, Lee SH, Choi BK (2012) Fusobacterium nucleatum GroEL induces risk factors of atherosclerosis in human microvascular endothelial cells and ApoE(−/−) mice. Mol Oral Microbiol 27:109–123
Lee JH, Kim YG, Cho MH, Lee J (2014) ZnO nanoparticles inhibit Pseudomonas aeruginosa biofilm formation and virulence factor production. Microbiol Res 169:888–896
Leistevuo J, Järvinen H, Österblad M, Leistevuo T, Huovinen P, Tenovuo J (2000) Resistance to mercury and antimicrobial agents in Streptococcus mutans isolates from human subjects in relation to exposure to dental amalgam fillings. Antimicrob Agents Chemother 44:456–457
Li X, Kolltveit KM, Tronstad L, Olsen I (2000) Systemic diseases caused by oral infection. Clin Microbiol Rev 13:547–558
Li Q, Mahendra S, Lyon DY et al (2008) Antimicrobial nanomaterials for water disinfection and microbial control: potential applications and implications. Water Res 42:4591–4602
Li K, Zhao X, Hammer BK, Du S, Chen Y (2013) Nanoparticles inhibit DNA replication by binding to DNA: modeling and experimental validation. ACS Nano 7:9664–9674
Liu Y, He L, Mustapha A, Li H, Hu ZQ, Lin M (2009) Antibacterial activities of zinc oxide nanoparticles against Escherichia coli O157:H7. J Appl Microbiol 107:1193–1201
Liu B, Faller LL, Klitgord N et al (2012) Deep sequencing of the oral microbiome reveals signatures of periodontal disease. PLoS ONE 7(1–16):e37919
Loesche WJ (1986) Role of Streptococcus mutans in human dental decay. Microbiol Rev 50(4):353–380
Lu Z, Rong K, Li J, Yang H, Chen R (2013) Size-dependent antibacterial activities of silver nanoparticles against oral anaerobic pathogenic bacteria. J Mater Sci Mater Med 24:1465–1471
Luo Morrin A, Killard AJ, Smyth MR (2006) Application of nanoparticles in electrochemical sensors and biosensors. Electroanalysis 18:319–326
Madinier IM (1999) Resistance profile survey of 50 periodontal strains of Actinobacillus actinomycetemcomitans. J Periodontol 70:888–892
Mah TFC, O’Toole GA (2001) Mechanisms of biofilm resistance to antimicrobial agents. Trends Microbiol 9:34–39
Mah TF, Pitts B, Pellock B, Walker GC, Stewart PS, O’Toole GA (2003) A genetic basis for Pseudomonas aeruginosa biofilm antibiotic resistance. Nature 426:306–310
Mahmoudi M, Serpooshan V (2012) Silver-coated engineered magnetic nanoparticles are promising for the success in the fight against antibacterial resistance threat. ACS Nano 6:2656–2664
Maness PC, Smolinski S, Blake DM, Huang Z, Wolfrum EJ, Jacoby WA (1999) Bactericidal activity of photocatalytic TiO2 reaction: toward an understanding of its killing mechanism. Appl Environ Microbiol 65:4094–4098
Marambio-Jones C, Hoek EMV (2010) A review of the antibacterial effects of silver nanomaterials and potential implications for human health and the environment. J Nanopart Res 12:1531–1551
Marcus AJ, Hajjar DP (1993) Vascular transcellular signaling. J Lipid Res 34:2017–2031
Mattila KJ (1989) Viral and bacterial infections in patients with acute myocardial infarction. J Intern Med 225:293–296
Maurer-Jones MA, Gunsolus IL, Meyer BM, Christenson CJ, Haynes CL (2013) Impact of TiO2 nanoparticles on growth, biofilm formation, and flavin secretion in Shewanella oneidensis. Anal Chem 85:5810–5818
Moos PJ, Olszewski K, Honeggar M et al (2011) Responses of human cells to ZnO nanoparticles: a gene transcription study. Metallomics 3:1199–1211
Morris JF, Sewell DL (1994) Necrotizing pneumonia caused by mixed infection with Actinobacillus actinomycetemcomitans and Actinomyces israelii: case report and review. Clin Infect Dis 18:450–452
Munson MA, Banerjee A, Watson TF, Wade WG (2004) Molecular analysis of the microflora associated with dental caries. J Clin Microbiol 42:3023–3029
Musarrat J, Saquib Q, Azam A, Naqvi SAH (2009) Zinc oxide nanoparticles-induced DNA damage in human lymphocytes. Int J Nanopart 2:402–415
Nasidze I, Li J, Quinque D, Tang K, Stoneking M (2009) Global diversity in the human salivary microbiome. Genome Res 19:636–643
Nyfors S, Könönen E, Syrjänen R, Komulainen E, Jousimies-Somer H (2003) Emergence of penicillin resistance among Fusobacterium nucleatum populations of commensal oral flora during early childhood. J Antimicrob Chemother 51:107–112
Ou KL, Chu JS, Hosseinkhani H, Chiou JF, Yu CH (2014) Biomedical nanostructured coating for minimally invasive surgery devices applications: characterization, cell cytotoxicity evaluation and an animal study in rat. Surg Endosc 28(7):2174–2188
Pal S, Tak YK, Song JM (2007) Does the antibacterial activity of silver nanoparticles depend on the shape of the nanoparticle? A study of the Gram-negative bacterium Escherichia coli. Appl Environ Microbiol 73:1712–1720
Park H, Park HJ, Kim JA et al (2011) Inactivation of Pseudomonas aeruginosa PA01 biofilms by hyperthermia using superparamagnetic nanoparticles. J Microbiol Methods 84:41–45
Paster BJ, Boches SK, Galvin JL et al (2001) Bacterial diversity in human subgingival plaque. J Bacteriol 183:3770–3783
Paster BJ, Olsen I, Aas JA, Dewhirst FE (2006) The breadth of bacterial diversity in the human periodontal pocket and other oral sites. Periodontol 2000 42:80–87
Peng JJ, Botelho MG, Matinlinna JP (2012) Silver compounds used in dentistry for caries management: a review. J Dent 40:531–541
Piccinno F, Gottschalk F, Seeger S, Nowack B (2012) Industrial production quantities and uses of ten engineered nanomaterials for Europe and the world. J Nanopart Res 14:1109–1120
Raghupathi KR, Koodali RT, Manna AC (2011) Size-dependent bacterial growth inhibition and mechanism of antibacterial activity of zinc oxide nanoparticles. Langmuir 27:4020–4028
Rajakumar G, Rahuman AA, Roopan SM et al (2012) Fungus-mediated biosynthesis and characterization of TiO2 nanoparticles and their activity against pathogenic bacteria. Spectrochim Acta A 91:23–29
Ready D, Bedi R, Spratt DA, Mullany P, Wilson M (2003) Prevalence, proportions, and identities of antibiotic-resistant bacteria in the oral microflora of healthy children. Microb Drug Resist 9:367–372
Rôças IN, Siqueira JF Jr (2012) Antibiotic resistance genes in anaerobic bacteria isolated from primary dental root canal infections. Anaerobe 18:576–580
Saito T, Iwase T, Horie J, Morioka T (1992) Mode of photocatalytic bactericidal action of powdered semiconductor TiO2 on mutans streptococci. J Photochem Photobiol B 14:369–379
Sandhiya S, Dkhar SA, Surendiran A (2009) Emerging trends of nanomedicine—an overview. Fundam Clin Pharmacol 23:263–269
Saunders SA (2009) Current practicality of nanotechnology in dentistry. Part 1: Focus on nanocomposite restoratives and biomimetics. Clin Cosmet Investig Dent 1:47–61
Seyedmahmoudi SH, Harper SL, Weismiller MC, Haapala KR (2015) Evaluating the use of zinc oxide and titanium dioxide nanoparticles in a metalworking fluid from a toxicological perspective. J Nanopart Res 17:104
Sheng Z, Liu Y (2011) Effects of silver nanoparticles on wastewater biofilms. Water Res 45:6039–6050
Skopek RJ, Liljemark WF, Bloomquist CG, Rudney JD (1993) Dental plaque development on defined Streptococcal surfaces. Oral Microbiol Immunol 8:16–23
Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL Jr (1998) Microbial complexes in subgingival plaque. J Clin Periodontol 25:134–144
Song W, Zhang J, Guo J et al (2010) Role of the dissolved zinc ion and reactive oxygen species in cytotoxicity of ZnO nanoparticles. Toxicol Lett 199:389–397
Stewart PS (2002) Mechanisms of antibiotic resistance in bacterial biofilms. Int J Med Microbiol 292:107–113
Suketa N, Sawase T, Kitaura H et al (2005) An antibacterial surface on dental implants, based on the photocatalytic bactericidal effect. Clin Implant Dent Relat Res 7:105–111
Suri SS, Fenniri H, Singh B (2007) Nanotechnology-based drug delivery systems. J Occup Med Toxicol 2:16
Sweeney LC, Dave J, Chambers PA, Heritage J (2004) Antibiotic resistance in general dental practice—a cause for concern? J Antimicrob Chemother 53:567–576
Takahashi N (2005) Microbial ecosystem in the oral cavity: metabolic diversity in an ecological niche and its relationship with oral diseases. Int Congr Ser 1284:103–112
Takahashi N, Schachtele CF (1990) Effect of pH on growth and proteolytic activity of Porphyromonas gingivalis and Bacteroides intermedius. J Dent Res 69:1244–1248
Takahashi N, Saito K, Schachtele CF, Yamada T (1997) Acid tolerance of growth and neutralizing activity of Porphyromonas gingivalis, Prevotella intermedia and Fusobacterium nucleatum. Oral Microbiol Immunol 12:323–328
Takatsuka T, Tanaka K, Iijima Y (2005) Inhibition of dentine demineralization by zinc oxide: in vitro and in situ studies. Dent Mater 21:1170–1177
Talebiana N, Amininezhada SM, Doudi M (2013) Controllable synthesis of ZnO nanoparticles and their morphology-dependent antibacterial and optical properties. J Photochem Photobiol 120:66–73
Tavassoli-Hojati S, Alaghemand H, Hamze F et al (2013) Antibacterial, physical and mechanical properties of flowable resin composites containing zinc oxide nanoparticles. Dent Mater 29:495–505
Teles R, Wang CY (2011) Mechanisms involved in the association between periodontal diseases and cardiovascular disease. Oral Dis 17:450–461
Témoin S, Chakaki A, Askari A et al (2012) Identification of oral bacterial DNA in synovial fluid of patients with arthritis with native and failed prosthetic joints. J Clin Rheumatol 18:117–121
Tsuang YH, Sun JS, Huang YC et al (2008) Studies of photokilling of bacteria using titanium dioxide nanoparticles. Artif Organs 32:167–174
Turnbaugh P, Ley R, Hamady M, Fraser-Liggett C, Knight R, Gordon JI (2007) The human microbiome project. Nature 449:804–810
Valant J, Drobne D, Novak S (2012) Effect of ingested titanium dioxide nanoparticles on the digestive gland cell membrane of terrestrial isopods. Chemosphere 87:19–25
Vandebriel RJ, De Jong WH (2012) A review of mammalian toxicity of ZnO nanoparticles. Nanotechnol Sci Appl 5:61–71
Vargas-Reus MA, Memarzadeh K, Huang J, Ren GG, Allaker RP (2012) Antimicrobial activity of nanoparticulate metal oxides against peri-implantitis pathogens. Int J Antimicrob Agents 40:135–139
Villedieu A, Diaz-Torres ML, Roberts AP et al (2004) Genetic basis of erythromycin resistance in oral bacteria. Antimicrob Agents Chemother 48:2298–2301
von Moos N, Slaveykova VI (2014) Oxidative stress induced by inorganic nanoparticles in bacteria and aquatic microalgae—state of the art and knowledge gaps. Nanotoxicology 8:605–630
Wang Z, Lee YH, Wu B et al (2010) Antimicrobial activities of aerosolized transition metal oxide nanoparticles. Chemosphere 80:525–529
Wang J, Qi J, Zhao H et al (2013a) Metagenomic sequencing reveals microbiota and its functional potential associated with periodontal disease. Sci Rep 3:1843
Wang X, Buhimschi CS, Temoin S, Bhandari V, Han YW, Buhimschi IA (2013b) Comparative microbial analysis of paired amniotic fluid and cord blood from pregnancies complicated by preterm birth and early-onset neonatal sepsis. PLoS ONE 8:e56131
Warheit DB, Hoke RA, Finlay C et al (2007) Development of a base set of toxicity tests using ultrafine TiO2 particles as a component of nanoparticle risk management. Toxicol Lett 171:99–110
Weir E, Lawlor A, Whelan A, Regan F (2008) The use of nanoparticles in anti-microbial materials and their characterization. Analyst 133:835–845
Weir A, Westerhoff P, Fabricius L, von Goetz N (2012) Titanium dioxide nanoparticles in food and personal care products. Environ Sci Technol 46:2242–2250
Whitmore SE, Lamont RJ (2014) Oral bacteria and cancer. PLoS Pathog 10:e1003933
Williams RC (2000) Offenbacher S (2000) Periodontal medicine: the emergence of a new branch of periodontology. Periodontol 23:9–156
Xi A, Bothun GD (2014) Centrifugation-based assay for examining nanoparticle-lipid membrane binding and disruption. Analyst 139:973–981
Xie Y, He Y, Irwin PL, Jin T, Shi X (2011) Antibacterial activity and mechanism of action of zinc oxide nanoparticles against Campylobacter jejuni. Appl Environ Microbiol 77:2325–2331
Ximénez-Fyvie LA, Haffajee AD, Socransky SS (2000) Comparison of the microbiota of supra- and subgingival plaque in health and periodontitis. J Clin Periodontol 27:648–657
Yamanaka M, Hara K, Kudo J (2005) Bactericidal actions of a silver ion solution on Escherichia coli, studied by energy-filtering transmission electron microscopy and proteomic analysis. Appl Environ Microbiol 71:7589–7593
Yu JX, Li TH (2011) Distinct biological effects of different nanoparticles commonly used in cosmetics and medicine coatings. Cell Biosci 1:19
Zbinden A, Mueller NJ, Tarr PE et al (2012) Streptococcus tigurinus, a novel member of the Streptococcus mitis group, causes invasive infections. J Clin Microbiol 50:2969–2973
Zhang L, Gu FX, Chan JM, Wang AZ (2008) Nanoparticles in medicine: therapeutic applications and developments. Clin Pharmacol Ther 83(5):761–769
Zinkernagel AS, Timmer AM, Pence MA et al (2008) The IL-8 protease SpyCEP/ScpC of group A Streptococcus promotes resistance to neutrophil killing. Cell Host Microbe 4:170–178
Acknowledgments
This project was funded by the National Plan for Science, Technology and Innovation (MAARIFAH), King Abdul Aziz City for Science and Technology, Kingdom of Saudi Arabia Award Number (12-NAN-2490-2).
Conflict interest
The authors declare no conflict of interest whatsoever.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khan, S.T., Al-Khedhairy, A.A. & Musarrat, J. ZnO and TiO2 nanoparticles as novel antimicrobial agents for oral hygiene: a review. J Nanopart Res 17, 276 (2015). https://doi.org/10.1007/s11051-015-3074-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11051-015-3074-6