Abstract
Objective
The immunological mechanisms behind different mucosa against candidiasis are largely unknown. In this study, we investigate the natural protective mechanisms and local cytokine responses of C. albicans-infected oral and vaginal epithelial cells.
Method
The cell lines (Leuk-1 and VK2/E6E7) were cultured with C. albicans (SC5314, Δals3, and Δssa1) in indicated ratio, respectively. The morphological changes and colony growth of C. albicans were observed to evaluate the fungicidal ability of epithelial cells, and the cellular morphological changes and LDH activity measurements were used to assess cell damage. Further, we assess the production of cytokines and chemokines in co-culture supernatants using enzyme-linked immunosorbent assay (ELISA).
Result
Our results show that the oral and vaginal epithelial cells use different strategies to combat this pathogen. Infected oral epithelial cells are adept at the production of cytokines (GM-CSF, IL-1α, and IL-1β) and chemokines (IL-8, MIP-3α, and RANTES), and yet, vaginal cells are more proficient at direct fungal killing. However, both epithelial cells play only a minor role in adaptive immunity to C. albicans. Further, C. albicans Als3p and Ssa1p genes also participate in local immune response since deletion of ALS3 or SSA1 causes reduction in cytokine and chemokine levels in both oral and vaginal cells. The dramatic decreases in both fungal % of cytotoxicity and the secretion of such cytokines as GM-CSF, MIP-3α, and RANTES in Δssa1-infected oral cells were consistent with a delayed germination process in that mutant.
Conclusion
Human oral and vaginal epithelial cells performed different host response to C. albicans by fungal killing ability or secreting cytokines and chemokines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Candida albicans, a commensal organism of the gastrointestinal and female lower reproductive tracts, is the most common pathogen of mucosal candidiasis, leading to oropharyngeal candidiasis (OPC) in immunocompromised patients and to vulvovaginal candidiasis (VVC) in immunocompetent individuals [1]. OPC is commonly seen in patients with human immunodeficiency virus (HIV) infections, or patients undergoing or having undergone chemotherapy or allogeneic transplantation when peripheral T cells are defective. On the other hand, VVC commonly causes mucosal inflammation in healthy women of fertile age [2]. Given the differences in clinical progress and distinction infection sites, the mechanisms behind the body’s defense against mucosal candidiasis are largely unknown.
Cell-mediated immunity (CMI) by Th1-type CD4+T cells is considered the predominant host defense mechanism against mucosal C. albicans infections [3]. However, CMI shows no vaginal protection from Candida because women suffering from recurrent VVC can sustain normal levels of Candida-specific systemic Th1-type CMI [4]. Anti-Candida activity of epithelial cells has been recognized lately since epithelial cells can inhibit the growth of C. albicans in vitro [5, 6], and HIV-infected persons with OPC and women with VVC have impaired epithelial cell activity against C. albicans [7]. More evidences have been emerged lately indicating that epithelial cells are playing a more important role in host responses to the fungus such as immunity, commensal/pathogen discrimination, and damage repair. Moyes et al. [8] have demonstrated that oral and vaginal epithelial cells responded to yeast or hyphal form of C. albicans via the bi-phasic MAPK (mitogen-activated protein kinase) pathways, which may regulate the expression levels of various immune effectors including IL-6, IL-8, IL-1a, G-CSF, GM-CSF, and CCL20 epithelial cells [9]. The epithelial cells at the outmost surfaces of the mucosa are the first host cells that contact with pathogens, taking a charge of the recognition process and C. albicans invasion. The virulent factors of the C. albicans on the other side are also the contributors of mucosal candidiasis for its pathogenesis, which include Als3p and Ssa1p. As a GPI-anchored glycoprotein, Als3p is responsible for the adherence of C. albicans to the oral epithelial cells, followed by an immune response [10]. Yang et al. [11] identified the second adhesin of C. albicans Ssa1p for epithelial cells reorganization. As a member of Hsp70 family, Ssa1p on the surface of blastospores and hyphae acts as the same of Als3p to lead endocytosis after binding to host cell cadherin [12].
The discrimination of host immune responses to fungus is not just limited to the initial parts of host–pathogen interaction via either epithelial or myeloid-originated immune cells. Given the fact that oral candidiasis tends to affect immunocompromised HIV+ or AIDS patients and vaginal infection has a tendency of immunocompetent individual, one would, however, expect some degree of difference existing in immunological responses that result from an interplay among epithelial cells and Candida in each infected location. On the other hand, despite those general responses of the host to C. albicans, some of C. albicans genes reacted in a niche-specific manner, for example, SAP gene family [13]. In order to better understand the epithelial roles in site immunity, we assess the capability of fungal killing and cytokines response in vitro using human oral- and vaginal-originated epithelial cells. Meanwhile, both innate immune responses are also studied in the absence of ALS3 or SSA1 to correlate these two virulent factors with site immunity.
Materials and Methods
Human Epithelial Cell Lines and Cell Culture
Two human epithelial cell lines were used. Immortalized human oral mucosal epithelial (Leuk-1) cell line was gifted from Dr. Wang (see acknowledgment). VK2/E6E7 kindly gifted from Dr. Raina Fichorova (see acknowledgment) is an epithelial cell line derived from the vaginal mucosa of a healthy premenopausal female undergoing vaginal repair surgery, following immortalization by human papillomavirus VK6/E6E7. Both cell lines were maintained and passaged in keratinocyte serum-free medium (Gibco, USA) supplemented with 50 μg/ml of bovine pituitary extract and 0.1 ng/ml of epidermal growth factor in a humidified incubator with 5% CO2 at 37 °C.
Candida albicans Strains and Growth
Candida albicans SC5314 was used for all assays as a wild-type and mutant strain Δals3 or Δssa1 which has both alleles of gene deleted. All of C. albicans strains were routinely grown in liquid YPD (1% yeast extract, 2% bactopeptone, 2% d-glucose) medium at 30 °C in a shaking incubator overnight. For maintenance of strains on solid media, 2% agar was added. Prior to use in experiments, C. albicans cells diluted at 1:20 ratio into fresh liquid YPD medium allow a log phase growth for another 2–4 h at 30 °C. The fungal cells were collected, washed with phosphate-buffered saline, and then counted in a hemocytometer and adjusted to the desired concentration in cell culture medium immediately prior to the experiments.
Strains Morphological Analysis
C. albicans yeast cells of SC5314 (WT), Δals3, and Δssa1 were added into a 24-well plate, respectively, containing 1 ml KSFM and grown at 37 °C with 5% CO2 for 2 h. The germ tube formation was then examined. The differential interference contrast (DIC) microscopy was used to image 8–10 fields for each experiment randomly. MShot Image Analysis System was applied to measure the length of germ tube.
Epithelial Cells Infection
C. albicans strains were inoculated into Leuk-1 and VK2/E6E7 monolayer cultures at a multiplicity of infection (MOI = Candida cell/epithelial cell ratios) of 0.01–10 for cytokine analysis in all the experiments below. All the mixtures of cell monolayer and fungal cells post-infection were incubated at 37 °C with 5% CO2 for 24 h as previously described [9]. Non-infected controls contained cell culture medium (KSFM) alone.
Detection of Fungicidal Ability of Epithelial Cells
Oral and vaginal cells were prepared and seeded into a 96-well plate cultured for 12 h at 37 °C with 5% CO2 prior to infection (there were about 1 × 104 cells/well). The overnight cultures of each fungal strain were diluted accordingly. A 50 µl aliquot was added into the first column of the plate to mix with epithelial cells (the initial concentration of each strain is also about 1 × 104 cells/well and the MOI was 1:1) and then serially diluted at 1:2 for six times. Strains incubated without cells were diluted in parallel manner. All the plates were incubated for 24 h and 48 h at 37 °C in a 5% CO2 atmosphere. Colonies in each well were counted under microscopy. The survival rate of each strain was calculated as the numbers of colonies with epithelial cells were divided by the number of colonies in the absence of cells × 100%. Each experiment was duplicated and repeated three times.
Cell Damage Assay
For epithelial cell damage assays, a total of 106 oral and vaginal cells was seeded into a 6-well plate cultured overnight and then mixed with the Candida cells as of MOI of 0.01 for 24 h; 0.2% trypan blue was used to stain dead cells and photographed.
Epithelial cell damage was also determined at 24 h by measuring lactate dehydrogenase (LDH) activity in the culture supernatants with the MOI from 0.01 to 10. The experiment was performed using the CytoTox 96 Non-Radioactive Cytotoxicity Assay kit (Promega, USA) according to the manufacturer’s protocol. For cell death calculation, the formula is as follows: % cytotoxicity = (experimental–effector spontaneous–target spontaneous)/(target maximum–target spontaneous) × 100%.
Assessment of Cytokine and Chemokine in Co-culture Supernatants
Supernatants were assayed for pro-inflammatory (G-CSF, GM-CSF, IL-1a, IL-1β), Th1 and Th2 immunoregulatory (IL-12 and IL-4), and chemotactic (MIP-3α, RANTES, IL-8) cytokines by enzyme-linked immunosorbent assay (ELISA) using commercially available capture and biotinylated detection antibodies, coupled with the Luminex 100TM machine according to the manufacturer’s protocol (the MOI values of the experimental groups were 0.01, 0.1, 1, 10, respectively). The trimmed median value was used to derive the standard curve in order to calculate the concentrations of cytokines in the samples.
Statistical Analysis
Statistical analyses were performed using SPSS 16.0. The results above were analyzed by the independent samples t test or one-way ANOVA. Significant differences were defined with a P value less than 0.05.
Results
The Fungal Killing Efficiency of Epithelial Cells
In order to assess the relative contributions of the oral and vaginal cells in host defense mechanisms against C. albicans, we first explore the difference of fungal killing between two epithelial cells under different MOI infections. Using wild type of C. albicans, oral and vaginal cells showed the significant differences in fungal killing at MOI of 1 and 10. When the Leuk-1 (oral) and VK2/E6E7 (vaginal) were infected triplicate with an MOI of 1 (Fig. 1a, b), the fungal CFU (colony-forming unit) decreased in VK2/E6E7 after 24 h (Fig. 1a) and 48 h (Fig. 1b) compared to control wells (Candida cells only). In contrast to vaginal epithelial cells, the fungal killing abilities of Leuk-1 could not be seen until 48-h incubation at MOI of 1 (P > 0.05) (Fig. 1b). With more Candida cells in the culture (MOI of 10), vaginal cells still have higher capacity to suppress CFU than oral cells at 24 h and 48 h (P < 0.05, P < 0.01, respectively). Oral cells again had no effects on fungal killing at both 24 h and 48 h. These results demonstrate that fungal killing by the vaginal cells appears earlier and stronger than that of oral cells.
Fungal CFUs are calculated after epithelial cells Leuk-1 (oral) and VK2/E6E7 (vaginal) were infected with wild type of Candida cells for 1 d (a) and 2 d (b) with MOI = 1. The CFUs are also measured from both epithelial cell lines after incubation with Candida cells for 1 d (c) and 2 d (d) at MOI = 8. Data represent mean values ± SEM and are representative of three independent experiments. *P < 0.05; **P < 0.01
Epithelial Cell Damages Induced by C. albicans
To better understand the invasive mechanism of C. albicans on epithelial tissues, epithelial cell damages were assessed in each epithelial cell line after cultivation with wild type of C. albicans. Two gene deletion mutants, ∆als3 and ∆ssa1, are also included in this study to determine the virulent roles of each gene on epithelial tissue. The viability of both epithelial cell lines was evaluated by trypan blue staining as shown in Fig. 2. Under microscopy, the injured epithelial cells were prone to aggregate or distribute alone with the hyphae of wild-type and mutant strain (Fig. 2a1), as we have seen in a higher magnification (Fig. 2a2). Both ∆als3 and ∆ssa1 mutants have reduced infectivity to the oral and vaginal cells at 24 h with MOI of 0.01 when compared to wild type (Fig. 2a1). With less fungal infectivity, morphologic changes on both epithelial cells were subtle, particularly in ∆ssa1 mutant-infected samples.
Cell damage of mucosal cells cultivated by different strains. a Oral and vaginal cells are stained by trypan blue 24 h post-infected with wild type, ∆als3 and ∆ssa1 mutants at MOI of 0.01. Morphology was assessed by DIC microscopy at × 4 (a1) and × 200 (a2). b The cytotoxicity of oral and vaginal cells infected by wild type and two mutants at different MOI for 24 h. b1 Cytotoxic effects of each strain at different MOI condition; b2 comparison of cytotoxic effects between oral and vaginal cells with three strains. Data represent mean values ± SEM and are representative of a minimum of three independent experiments. Statistical analysis was performed using the unpaired, two-tailed t test. *P < 0.05; **P < 0.01; ***P < 0.001 present the comparison between wild type and each mutant with each MOI infection
The epithelial cell damages were further assessed with three fungal strains at various MOI mixtures and calculated by LDH activity. As shown in Fig. 2b, the cytotoxicity increased as the fungal burden was increased in both oral and vaginal cells no matter what fungal strain had been used. The overall cytotoxicity of vaginal cells in this study is higher than that of oral cells (P < 0.05). The ∆ssa1 mutant shows less cytotoxic roles than that of wild type and ∆als3 mutant, especially in oral cell infection (Fig. 2b1). For vaginal cells, compared to a low cytotoxicity rate of ∆ssa1, ∆als3 mutant seems to slightly increase the vaginal cell cytotoxicity when fungal burden was same to the WT in regard to LDH release. This enhanced cytotoxicity of ∆als3 is consistent with a stronger trypan staining as shown in Fig. 2a1 when MOI was used at 0.01. These results suggest that Ssa1p is required for both oral and vaginal cells invasion and damage, but not Als3p, at least in vaginal cells.
Germ Tube Delayed Only in ∆ssa1 Strain
In correspondence with a less cytotoxic effect of ∆ssa1 in both oral and vaginal cells, germ tube formation is delayed in this mutant when cultured in vitro. Compared to C. albicans wild type (SC5314) and ∆als3, the average length of germ tubes of ∆ssa1 is 4.2 ± 1.8 µm when cultivated in culture media KSFM for 2 h at 37 °C in 5% CO2, which was obtained by taking 8 ~ 10 image fields at random with 10 cells in each field under the microscope. The germ tube formation was defective in ∆ssa1 with approximately 30–40% reduction compared to other two strains (Fig. 3a). However, the morphology of the germ tubes in both mutants could not be distinguished from the wild-type strain (Fig. 3b). The ability to form hyphae and colony of Δssa1 strain was significantly different from WT and als3Δ strains when they were co-cultured with oral and vaginal cells at 24 h with MOI of 0.01, which is shown in Fig. 2a1.
Germ tubes formation of C. albicans wild type and mutants. The average length of germ tube formed by wild type, ∆als3 and ∆ssa1 mutants was measured after incubated in KSFM at 37 °C with 5% CO2 for 2 h (a). The morphology of germ tube was assessed by DIC microscopy at × 200 (b). The length of germ tube in 8 ~ 10 fields was acquired using the MShot Image Analysis System. Data represent mean values ± SEM and are representative of two independent experiments. The scale bar in B is 10 microns. ***P < 0.001 compared to wild type and ∆als3, respectively
The Inflammatory Responses of Epithelial Cells Following Exposure to C. albicans Strains
The cytokine and chemokine production of two types of epithelial cells is also assessed upon infected by different strains of C. albicans to distinguish the likely defense mechanisms of each type of epithelial cells against mucosal candidiasis. The induction of immune response can be effectively induced at the highest MOI of 10 in vaginal cells while at the MOI of 1 in oral cells as reported previously. In this study, we tested fungal burden at MOI of 0.01, 0.1, 1, and 10 for either wild type or mutant of C. albicans with cell medium alone as the control. Supernatants collected at 24 h were assayed for pro-inflammatory (G-CSF, GM-CSF, IL-1a, and IL-1β), chemotactic (MIP-3a, IL-8, and RANTES), Th1 (IL-12p70), and Th2 immunoregulatory (IL-4) cytokines.
In our study, the overall strength of two types of epithelial cells in the production of pro-inflammatory cytokines was firstly tested in wild-type C. albicans. The results shown in Fig. 4 indicate that oral Leuk-1 cells are able to release measured amounts of GM-CSF (Fig. 4a) and G-CSF (Fig. 4b) even under uninfected condition (average 53.52 pg/ml of GM-CSF and 316.7 pg/ml of G-CSF). In comparison with oral cell line, such baseline levels of both cytokines are much less in VK2/E6E7 cells with average 0.24 pg/ml of GM-CSF and 44.38 mg/ml of G-CSF (P < 0.001). No matter what type of cell line we used in this experiment, some degree of correlation exists between the secretion of GM-CSF and fungal burden (Fig. 4a). At MOI of 0.01, the concentration of GM-CSF reached the highest level of 528.5 pg/ml in Leuk-1 cells that is significantly higher than 114.5 pg/ml in VK2/E6E7 cells (P < 0.001). For G-CSF secretion, the difference between two cell lines is much smaller (Fig. 4b). Unlike GM-CSF, the highest secretion peak for G-CSF in both cell lines appeared at MOI of 0.1 with 1988 pg/ml in Leuk-1 and 1772 pg/ml in VK2/E6E7 (P < 0.05). These results suggest that oral cells can maintain both pro-inflammatory cytokines effectively than vaginal cells and temporal expression of GM-CSF or G-CSF may be required for mucosal defense when dealing with variant population of fungal burden. The similar results were also found in IL-1α and IL-1β measurement. As shown in Fig. 4c & d, the certain amount of IL-1α and IL-1β in both epithelial cells was detected, with a higher amount from Leuk-1 than that from VK2/E6E7 in the presence of wild type of C. albicans in the culture (P < 0.05). Then, the production of IL-1α and IL-1β in two cell types further induced when infected with Candida cells with highest at MOI of 1. However, the IL-1α production in VK2/E6E7 cells seems to be higher than that of Leuk-1 cells when MOI is ≥ 1 (higher fungal burden), while IL-1β levels are all lower in VK2/E6E7 cells than that of Leuk-1 cells.
Activation of inflammatory cytokines in Leuk-1 and VK2/E6E7 cells upon C. albicans infection. Yeast cells were added to oral and vaginal epithelial cell monolayers and incubated under standard conditions for 24 h. The concentration of fungal cells in culture mixture ranges from 0.01 to 10 MOI (fungal/epithelial cells). Cell culture medium was collected, and GM-CSF (a), G-CSF (b), IL-1a (c), and IL-1β (d) levels were measured. Data represent mean values ± SEM and are representative of three independent experiments. *P < 0.05; **P < 0.01; ***P < 0.001 obtained when compared with the uninfected group
The Roles of Epithelial Cells on Chemotactic Cytokines
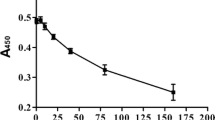
The C. albicans-induced chemotactic roles of each epithelial cell type were estimated by the production of RANTES, MIP-3α, and IL-8, as shown in Fig. 5. At the uninfected status, RANTES level is barely seen (Fig. 5a) and no MIP-3α can be detected (Fig. 5b) from vaginal cells, while oral cells are still able to secrete both chemokines (P < 0.05). The production of RANTES, MIP-3α, and IL-8 from oral cells all reached their peak points at MOI of 0.01, suggesting that these chemotactic effects may function only when small population of fungal cells present in the local environment. The VK2/E6E7 cells seem to response differently from Leuk-1 cells in RANTES level (remaining low at all tested MOIs) and MIP-3α (sustaining when MOI > 0.1) when infected (Fig. 5a, b) with wild type of C. albicans. The overall chemokines produced from vaginal cells are less than that of oral cells, especially seen in IL-8 (Fig. 5c) and RANTES production.
Activation of chemokines and pro-inflammatory cytokines induced by C. albicans in Leuk-1 and VK2/E6E7 cells. The fungal cells at MOIs from 0.01 to 10 were added to oral and vaginal epithelial cell monolayers and incubated under standard conditions for 24 h. Cell culture medium was collected, and RANTES (a), MIP-3α (b), IL-8 (c) IL-12P70 (d), and IL-4 (e) levels were measured. Data represent mean values ± SEM and are representative of three independent experiments. *P < 0.05; **P < 0.01; ***P < 0.001 obtained when compared with the uninfected group
Pro-inflammatory Cytokines for Adaptive Immunity are not Affected by Epithelial Cells
The T cell response for adaptive immunity to C. albicans depends on the cytokine milieu during its activation such as IL-12/IFNγ for Th1 cells and IL-4 for Th2 cells. To elucidate the roles of epithelial cells on T cell subset polarization, we measure the C. albicans-induced IL-12P70 and IL-4 levels in both epithelial cell lines in the absence of dendritic cells and T cells environment. As shown in Fig. 5d and e, both cytokines are not only so low at their baselines (uninfected) but also remained low levels throughout the 24-h culture period with the C. albicans. For IL-4 response, vaginal cells reacted only when high concentration of C. albicans was added, but the absolute concentration is only 2.8 pg/ml.
Adhesins Als3p and Ssa1p are Required for the Production of Pro-inflammatory Cytokines from Epithelial Cells
The importance of Als3 and Ssa1p for C. albicans virulence has long been recognized as adhesins to guide an endocytosis. The interaction between these adhesins and epithelial cells initiates the following fungal invasion in the tissue. The outcome of which is either to destroy the host cells or cause fungal death by recruiting more immune cells. To investigate whether cytokine induction is correlated with recognition event, we measured all the cytokines that mentioned above from epithelial cells infected with gene deletion mutants (∆als3 and ∆ssa1). The results shown in Fig. 6a–g indicate that both genes play the minor roles for pro-inflammatory cytokine and chemokine secretion in VK2/E6E7 cells except IL-α in ∆als3 (Fig. 6c), reflected by similar levels of each cytokine in mutant strains compared to that of wild type. On the other hand, most of these cytokine and chemokine levels are decreased in Leuk-1 cells when they are infected by either ∆als3 or ∆ssa1 compared to wild type, such as GM-CSF (Fig. 6a), IL-1α (Fig. 6c), IL-1β (Fig. 6d), IL-8 (Fig. 6e), and MIP-3α (Fig. 6f) (P < 0.001–0.05). In regard to the individual function of each gene on cytokine activation, we observed a certain degree of diversity between two mutant strains on the oral epithelial cells. For example, GM-CSF (Fig. 6a), IL-8 (Fig. 6e), MIP-3α (Fig. 6f), and RANTES (Fig. 6g) chemokines are significantly reduced in ∆ssa1 infection. When ∆ssa1-infected vaginal cells remain a wild-type level of G-CSF, secretion of this cytokine is inversely increased in ∆ssa1-infected oral epithelial cells (Fig. 6b).
Effects of Als3p and Ssa1p on cytokine activation. The fungal cells at MOIs from 0.01 to 10 were added to oral and vaginal epithelial cell monolayers and incubated under standard conditions for 24 h. The pro-inflammatory cytokine (a–d) and chemokine (e–g) activation is shown. *P < 0.05; **P < 0.01; ***P < 0.001 compared with the WT group
Discussion
Despite our increasing knowledge of immune cell and fungal interactions, the relative importance of epithelial cells in determining the course of mucosal infection is still unclear. Most antifungal immunity studies have focused on how immune cells such as macrophages, dendritic cells, and neutrophils combat the pathogens. With the discovery of a number of Toll-like receptors (TLRs) (dectin-1, dectin-2, and others) on these immune cells, molecules on the fungal cell surface such as phospholipomannan and β-glucan that correspond to each host receptor have also been identified and characterized. However, these fungal wall polysaccharides are not able to induce a cytokine response in oral epithelial cells or in skin keratinocytes [14], even though most receptors for immune cells are also found in epithelial cells [15]. These results may imply that epithelial cells use different mechanisms for host response either by utilizing different host receptors or by utilizing different fungal moieties for downstream immune activation.
To better understand the roles of epithelial cells against C. albicans, we investigate possible distinctions that may be made in the immune roles of epithelial cells originating from oral and vaginal locations. Our results are consistent with others that epithelial cells play a far more active role in combating fungal infection. We also find that cells of oral origin and vaginal origin carry out significantly different strategies in defending against this pathogen. In this experiment, we used two human epithelial cell lines: Leuk-1 is an immortalized human oral mucosal epithelial cell line, and VK2/E6E7 is obtained by immortalization of primary vaginal cells. Both cells have been used for oral/vaginal pathological studies by others [16, 17]. Early studies on the fungicidal activity of oral and vaginal epithelial cells suggest that both types of cells can inhibit but not kill C. albicans. By CFU recovery, we find that oral cells can hardly inhibit the formation of fungal colonies, but the fungal population can be significantly repressed by epithelial cells of vaginal origin until the fungal load is increased to about 10 times that of epithelial cells (MOI of 10). As murine vaginal cells were using in this early study, the fungal killing capability demonstrated in our study may be partially reflected by the human vaginal cells we used.
The interaction between C. albicans and epithelial cells includes adherence and invasion that the former requires C. albicans adhesins such as Als3 and Ssa1 for host recognition, and the subsequent invasion is accomplished by a receptor-mediated endocytosis of epithelial cells. Along with engulfment, C. albicans can secrete tissue-degrading enzymes, such as proteases and phospholipase to pierce the epithelial barrier. To test the outcome of this degrading process, we also examine the cell damage of each epithelial cell type by lactate dehydrogenase release. Consistent with their high fungal killing rate, infected vaginal cells are also easily damaged. These results suggest that both fungal killing and the dying of vaginal epithelial cells may enhance the shedding of fungal burden from vaginal locations.
Filamentation and active penetration appear to be involved in epithelial damage [18], which is further indicated by the presence of mostly dead cells around the fungal hyphal elements, as seen under trypan blue staining. Fungal Ssa1 and Als3 have been linked to the same pathway to induce fungal endocytosis via binding to E-cadherin receptor present in epithelial cells. As host endocytosis was attenuated in Δssa1 and Δals3 mutant, respectively, their effects on host cell damage are different here. We find that deletion of SSA1 reduces infectivity and results in markedly less damage to oral epithelial cells and vaginal cells as well, while Δals3 seems to produce similar changes or even more in vaginal cells when compared to wild type. Consistent with the observation of less host cell damage, germ tube formation in Δssa1 is also delayed in vitro. These results point out the relationship between the particular host defense mechanism and putative virulence factors in each infected location.
Mucosal epithelial cells can release cytokines in response to pathogen infection [19, 20]. The key T cell subsets most strongly associated with adaptive immunity in candidiasis are Th1 and Th17. In contrast to high levels of pro-inflammatory cytokines and chemokines induced by Candida infection, both oral and vaginal epithelial cells barely produce detectable levels of IL-12, indicating that epithelial cells do not contribute to adaptive immunity but are important for innate immunity for mucosal candidiasis. The basal levels of pro-inflammatory cytokines and chemokines from epithelial cells suggest that these cytokines may be in some sort of homeostasis and are critical for preserving mucosal hygiene.
The cytokines explored in this study were selected based on the fact that they are important regulatory, pro-inflammatory, or chemotactic cytokines and subset T cell effectors. We demonstrate that an initial difference of cytokine products exists between oral and vaginal cells. Under similar conditions, the cytokine production is higher in oral cells as reported previously than in vaginal cells, indicating that oral cells have a stronger innate immunity to Candida infection despite the fact that the optimal concentration of fungal cells can be slightly different between the two cell types for some cytokines. Cytokine type is also somewhat limited in vaginal cells compared to oral cells, as seen in GM-CSF and RANTES. Using MOIs of 0.01, 0.1, 1, and 10, the peak production of GM-CSF, IL-8, RANTES, and MIP-3α is induced by an MOI of 0.01 infection, while optimal MOI is 0.1 for G-CSF and 1 for IL-1α and IL-β in both cell lines. Such cytokine profile diversity suggests that a temporal expression of each cytokine effector may depend directly on fungal burden in oral and vaginal locations, which is likely necessary for the anti-Candida mechanism at the different stages of the disease and is in turn directly related to the severity of the illness. For example, the higher level of G-CSF at higher MOI compared to GM-CSF and IL-8 may imply that the former plays an important role when fungal burden is increased and the latter acts at an earlier stage of infection. In other words, while IL-8 and GM-CSF recruit the immune cells, a sustained high level of G-CSF in variant of fungal burden maintains persistent responses at the two mucosal sites.
These cytokines and chemokines of innate immunity in response to Candida infection have been well established for recruiting and activation of a variety of immune cells, including neutrophils, dendritic cells, and T cells. IL-1α and IL-1β are the two major pro-inflammatory family of cytokines, which act mainly at expression of integrins on leukocytes and endothelial cells [21, 22]; the latter provokes an inflammatory response via the NF-KB pathway. Compared to higher levels of GM-CSF and G-CSF, the absolute volume of IL-1α and IL-1β is lower, but the secretion persists from MOIs of 0.01–10. We observe that all four pro-inflammatory cytokines are higher in oral cells than those of vaginal cells, except IL-1α (equally between two cell lines) after exposure to Candida. The functional difference between IL-1α and IL-1β has recently been proposed by others. IL-1α often remains in the cells but is released outside when activated, while IL-1β is only stimulated by the presence of inflammasomes [23]. Also, Rider et al. [24] have shown that IL-1α released from dying cells can initiate inflammation by recruiting neutrophils, whereas IL-1β promotes the recruitment and retention of macrophages. The new evidence further demonstrates that IL-1α retained within the nucleus as a mechanism to prevent inflammation and preserve immune tolerance [25]. In agreement with these observations, our data on infected vaginal cells with compatible IL-1α support this IL-1α requirement for fungal tolerance in vaginal mucosa. Also, the higher release of IL-1β by oral cells tends to recruit more macrophages in oral location for defeating Candida infection.
The chemokines are significant contributors in inflammatory response. IL-8 release can recruit and activate neutrophils to the site of mucosal infection [26]. MIP-3α (CCL20/macrophage inflammatory protein-3α) is expressed constitutively by keratinocytes to trigger an adaptive immune response. This chemokine can attract immature dendritic cells to the site of inflammation and therefore form a bridge between the innate and adaptive immune response. RANTES, a member of the β or CC family of chemokines, can chemoattract activated T cells (particularly Th1 cells), dendritic cells, and monocytes to the infected sites as well [27]. In this study, the IL-8 and MIP-3α response is significantly stronger in oral cells than that in vaginal cells at an MOI of 0.01, but MIP-3α response is better when MOI was ≥ 1. Meanwhile, RANTES in vaginal cells remains very low no matter if Candida cells are present suggesting that RANTES chemoattraction is less necessary for vaginal sites.
The overall reduction in cytokines and chemokines in ∆als3 and ∆ssa1 compared to wild type demonstrates that cytokine response is correlated with Candida adhesion and invasion. The further reduced GM-CSF, MIP-3α, and RANTES and increased G-CSF levels in ∆ssa1-infected oral cells are also companied with the decrease in epithelial killing for this mutant, and as a consequence, we suspect that these four cytokines are more closely related to Ssa1p for an epithelial cytotoxicity. By the same token, Als3p is more important to maintain the healthy levels of IL-1α and RANTES in vaginal cells.
In summary, epithelial cells in oral and vaginal origins are actively response to kill and secrete cytokines and chemokines upon Candida infection, in which adhesins—Als3 and Ssa1—are required for an effective immune response. Oral cells can produce more cytokines when vaginal cells have a higher capability to kill fungal cells, a requisite for maintaining a healthy mucosal barrier for individual mucosal location. This may explain why the esophageal candidiasis is common in HIV or AIDS patients, since cytokine production is defective in this situation. On the other hand, the vaginal cells produce fewer cytokine, but are prone to shedding, leading to mild inflammation, but the incidence of vaginal candidiasis is higher. As this study is a two-dimensional model between epithelial cells and pathogen, the diversity of immune response in two mucosal locations will be further examined in an animal model in the presence of immune cells.
References
Calderone RA. Candida and candidiasis. Washington, DC: ASM Press; 2002.
Sobel JD. Vulvovaginal candidiasis. Lancet. 2007;369:1961–71.
Cenci E, Mencacci A, Spaccapelo R, Tonnetti L, Mosci P, Enssle KH, et al. T helper cell type 1 (Th1)- and Th2-like responses are present in mice with gastric candidiasis but protective immunity is associated with Th1 development. J Infect Dis. 1995;171:1279–88.
Fidel PL Jr, Lynch ME, Redondo-Lopez V, Sobel JD, Robinson R. Systemic cell-mediated immune reactivity in women with recurrent vulvovaginal candidiasis. J Infect Dis. 1993;168:1458–65.
Fidel PL Jr, Cutright J, Steele C. Effects of reproductive hormones on experimental vaginal candidiasis. Infect Immun. 2000;68:651–7.
Steele C, Leigh J, Swoboda R, Fidel PL Jr. Growth inhibition of Candida by human oral epithelial cells. J Infect Dis. 2000;182:1479–85.
Barousse MM, Steele C, Dunlap K, Espinosa T, Boikov D, Sobel JD, et al. Growth inhibition of Candida albicans by human vaginal epithelial cells. J Infect Dis. 2001;184:1489–93.
Moyes DL, Runglall M, Murciano C, Shen C, Nayar D, Thavaraj S, et al. A biphasic innate immune MAPK response discriminates between the yeast and hyphal forms of Candida albicans in epithelial cells. Cell Host Microbe. 2010;8:225–35.
Moyes DL, Murciano C, Runglall M, Islam A, Thavaraj S, Naglik JR. Candida albicans yeast and hyphae are discriminated by MAPK signaling in vaginal epithelial cells. PLoS ONE. 2011;6:e26580.
Murciano C, Moyes DL, Runglall M, Tobouti P, Islam A, Hoyer LL, et al. Evaluation of the role of Candida albicans agglutinin-like sequence (Als) proteins in human oral epithelial cell interactions. PLoS ONE. 2012;7:e33362.
Yang W, Yan L, Wu C, Zhao X, Tang J. Fungal invasion of epithelial cells. Microbiol Res. 2014;169:803–10.
Sun JN, Solis NV, Phan QT, Bajwa JS, Kashleva H, Thompson A, et al. Host cell invasion and virulence mediated by Candida albicans Ssa1. PLoS Pathog. 2010;6:e1001181.
Kumamoto CA. Niche-specific gene expression during C. albicans infection. Curr Opin Microbiol. 2008;11:325–30.
de Koning HD, Rodijk-Olthuis D, van Vlijmen-Willems IM, Joosten LA, Netea MG, Schalkwijk J, et al. A comprehensive analysis of pattern recognition receptors in normal and inflamed human epidermis: upregulation of dectin-1 in psoriasis. J Invest Dermatol. 2010;130:2611–20.
Weindl G, Naglik JR, Kaesler S, Biedermann T, Hube B, Korting HC, et al. Human epithelial cells establish direct antifungal defense through TLR4-mediated signaling. J Clin Invest. 2007;117:3664–72.
Wang WM, Ye P, Qian YJ, Gao YF, Li JJ, Sun FF, et al. Effects of whole cigarette smoke on human beta defensins expression and secretion by oral mucosal epithelial cells. Tob Induc Dis. 2015;13:3.
Anukam KC, Reid G. In vitro evaluation of the viability of vaginal cells (VK2/E6E7) and probiotic Lactobacillus species in lemon juice. Sex Health. 2009;6:67–74.
Wachtler B, Wilson D, Haedicke K, Dalle F, Hube B. From attachment to damage: defined genes of Candida albicans mediate adhesion, invasion and damage during interaction with oral epithelial cells. PLoS ONE. 2011;6:e17046.
Dongari-Bagtzoglou A, Fidel PL Jr. The host cytokine responses and protective immunity in oropharyngeal candidiasis. J Dent Res. 2005;84:966–77.
Steele C, Fidel PL Jr. Cytokine and chemokine production by human oral and vaginal epithelial cells in response to Candida albicans. Infect Immun. 2002;70:577–83.
Carmi Y, Voronov E, Dotan S, Lahat N, Rahat MA, Fogel M, et al. The role of macrophage-derived IL-1 in induction and maintenance of angiogenesis. J Immunol. 2009;183:4705–14.
Apte RN, Voronov E. Is interleukin-1 a good or bad ‘guy’ in tumor immunobiology and immunotherapy? Immunol Rev. 2008;222:222–41.
Rider P, Carmi Y, Guttman O, Braiman A, Cohen I, Voronov E, et al. IL-1alpha and IL-1beta recruit different myeloid cells and promote different stages of sterile inflammation. J Immunol. 2011;187:4835–43.
Cohen I, Rider P, Carmi Y, Braiman A, Dotan S, White MR, et al. Differential release of chromatin-bound IL-1alpha discriminates between necrotic and apoptotic cell death by the ability to induce sterile inflammation. Proc Natl Acad Sci U S A. 2010;107:2574–9.
Godaly G, Bergsten G, Hang L, Fischer H, Frendeus B, Lundstedt AC, et al. Neutrophil recruitment, chemokine receptors, and resistance to mucosal infection. J Leukoc Biol. 2001;69:899–906.
Homey B, Dieu-Nosjean MC, Wiesenborn A, Massacrier C, Pin JJ, Oldham E, et al. Up-regulation of macrophage inflammatory protein-3 alpha/CCL20 and CC chemokine receptor 6 in psoriasis. J Immunol. 2000;164:6621–32.
Luster AD. Chemokines–chemotactic cytokines that mediate inflammation. N Engl J Med. 1998;338:436–45.
Acknowledgement
This work was supported by National Key Basic Research Program of China (2013CB531605), National Natural Science Foundation of China (No. 81071332), and Jiangsu Provincial Special Program of Medical Science (BL2012003). We thank Professor Li Mao for providing Leuk-1 cell line, Dr. Raina Fichorova for kindly providing cell lines VK2/E6E7, and Dr. Scott G Filler for kindly gift of mutant strains shown in this study. We also would like to thank Professor Wantao Chen for his kind help to our experiment.
Author information
Authors and Affiliations
Corresponding author
Additional information
Handling Editor: A. Vecchiarelli.
Rights and permissions
About this article
Cite this article
Gao, Y., Liang, G., Wang, Q. et al. Different Host Immunological Response to C. albicans by Human Oral and Vaginal Epithelial Cells. Mycopathologia 184, 1–12 (2019). https://doi.org/10.1007/s11046-018-0301-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-018-0301-6